Abstract
Introduction
With aging, the sensory systems suffer an accumulation of degenerative, infectious and/or traumatic processes that may hinder the body balance maintenance.
Objective
To assess the influence of sensory information on static body balance of elderly individuals with vestibular disorders.
Methods
Cross-sectional study of elderly individuals with vestibular disorders. The Clinical Test of Sensory Interaction and Balance and posturography integrated with virtual reality (Balance Rehabilitation Unit™) were used. Posturography parameters analyzed included center of pressure and velocity of body sway.
Results
123 individuals with mean age of 73.11 were assessed. Worst performance was observed in the Clinical Test of Sensory Interaction and Balance condition of visual dome-unstable surface. Differences between conditions were: firm surface-open eyes/firm surface-closed eyes, unstable surface-open eyes/unstable surface-closed eyes (p < 0.001), and unstable surface-closed eyes/unstable surface-visual dome. Considering center of pressure and velocity of body sway, significant differences were observed between the following conditions: firm surface-open eyes/firm surface-closed eyes: firm surface-saccadic stimulus/firm surface-vertical optokinetic stimulus; firm surface-optokinetic stimuli/firm surface-visual–vestibular interaction; and firm surface-visual–vestibular interaction/unstable surface. Worse performances were observed in conditions firm surface-closed eyes, firm surface-vertical optokinetic stimulus, F-visual–vestibular interaction, and unstable surface-closed eyes. There was a difference in the center of pressure between firm surface-closed eyes/firm surface-saccadic stimulus, with a worse performance in the condition of firm surface-closed eyes, and of velocity of body sway, between firm surface-saccadic stimulus/firm surface-horizontal optokinetic stimulus (p < 0.001).
Conclusion
Static body balance in elderly individuals with vestibular disorders is worse when the sensory conditions are more challenging, i.e. stable and unstable surfaces, visual stimuli, such as optokinetic and visual–vestibular interaction, and with the eyes closed.
Keywords: Aged, Postural balance, Rehabilitation, Dizziness, Vestibular diseases
Resumo
Introdução
Com o envelhecimento, o sistema sensorial sofre um acúmulo de processos degenerativos, infecciosos e/ou traumáticas que podem dificultar a manutenção do equilíbrio corporal.
Objetivo
Avaliar a influência das informações sensoriais no equilíbrio corporal estático de idosos vestibulopatas.
Método
Estudo transversal, cuja amostra foi constituída por idosos vestibulopatas. Empregaramse o Clinical Test of Sensory Interaction and Balance (CTSIB) e a posturografia integrada à realidade virtual (Balance Rehabilitation Unit.). Os parâmetros avaliados à posturografia foram: área do centro de pressão (COP) e velocidade de oscilação (VOC).
Resultados
Foram avaliados 123 idosos, com média etária de 73,11 anos. O pior desempenho ocorreu na condição cúpula visual-superfície instável (SI) do CTSIB. As diferenças entre as condições foram: superfície firme (SF)-olhos abertos (OA)/SF-olhos fechados (OF) e SI-OA/SI-OF (p < 0,001); SI-OF/SI-cúpula visual. Observou-se diferença da área do COP e da VOC entre as condições: SF-OA/SF-OF; SF-estímulo sacádico/SF-estímulo optocinético vertical; SF-estímulos optocinéticos/SF-interação visuo-vestibular (IVV); SF-IVV/SI, com pior desempenho nas condições SF-OF, SF-estímulo optocinético vertical, SF-IVV e SI-OF. Observou-se diferença do COP entre as condições SF-OF/SF-estímulo sacádico, com pior desempenho na condição SF-OF, e da VOC entre as condições SF-estímulo sacádico e SF-estímulo optocinético horizontal (p < 0,001).
Conclusão
O equilíbrio corporal estático de idosos vestibulopatas é pior à medida que as condições sensoriais são mais desafiadoras, ou seja, em SI e SE, estímulos visuais como os optocinéticos e interação visuovestibular e OF.
Palavras-chave: Idoso, Equilíbrio postural, Reabilitação, Tontura, Doenças vestibulares
Introduction
Body balance maintenance is influenced by the integration of sensory information from the vestibular, visual, and somatosensory systems. Any conflict between this information may cause changes in body balance.1
With aging, the sensory systems suffer an accumulation of degenerative, infectious and/or traumatic processes that hinder their adequate functioning. Although an isolated change in one system does not result in a major impact on the development of postural instability, a combination of such deficiencies is a key factor for body imbalance in the elderly.2, 3 Among these systems, the vestibular system deserves attention due to the high prevalence of vestibular disorders and dizziness with advancing age (11.0–36.0%).4, 5
Assessment of these systems by clinical and laboratory tests can be used to verify the involvement of sensory information in postural control.6 These tests simulate the demands involved in body balance through manipulation of sensory inputs, through changes in visual input, changes in surface, and reductions in the support base. The Clinical Test of Sensory Interaction and Balance (CTSIB) is a clinical test, whose purpose is to provide information about the individual's capacity to adapt and maintain body balance in the presence of sensory conflicts.7
Another way to assess the influence of sensory information on body balance is through laboratory tests involving force platforms, electromyography, and photo-filming systems. These evaluations primarily measure body sway, shifting the center of gravity and muscle activation.8 The Balance Rehabilitation Unit™ (BRU™) is a static posturography device that uses the technology of virtual reality to recreate environments and situations in order to measure the postural response of the individual in the presence of different stimuli.9
The knowledge of the deficits found in sensory conditions using the data from CTSIB and posturography and a comparison of the progression of difficulty imposed by the test conditions allows the identification of key information for body balance in elderly individuals with chronic vestibular dysfunction, and, thus provides valuable information for planning rehabilitation. This study aimed to evaluate the influence of sensory information on static body balance in elderly individuals with chronic vestibular dysfunction through clinical testing (CTSIB) and laboratory examination (BRU™).
Methods
This was a descriptive, analytical, cross-sectional study, approved by the Research Ethics Committee of the institution, Protocol No. 0356/2010.
The sample consisted of subjects aged 65 or older, male or female, who complained of dizziness for at least three months and had a diagnosis of chronic vestibular dysfunction. Elderly patients who met the inclusion criteria for the study were invited to participate and signed an informed consent.
Elderly individuals unable to understand and follow simple verbal commands; those unable to remain independently in the orthostatic position; those using gait-assistive devices; those with severe visual impairment or not compensated through the use of corrective lenses; insulin-dependent diabetics with orthopedic disorders that resulted in limited movement and use of prostheses in the lower limbs; individuals with neurological and/or psychiatric disorders; those who reported alcohol intake within 24 h before the assessment; those using medications that affect the central nervous or the vestibular system; and those that had undergone body balance rehabilitation in the last six months were excluded.
Elderly individuals with chronic vestibular dysfunction included in the study underwent evaluation consisting of clinical data, clinical test of sensory interaction through CTSIB, and laboratory testing through computed posturography integrated with virtual reality (BRU™).
Clinical data were collected: number of diseases, number of medications, history of falls in the last year, and type of dizziness (rotatory or vertigo, non-rotatory, and both).
The CTSIB assesses static balance in six sensory conditions: condition I, firm surface (FS) and open eyes; condition II, FS and closed eyes (CE); condition III, FS and visual conflict; condition IV, unstable surface and open eyes; condition V, unstable surface and CE; and condition VI, unstable surface and visual conflict. A stopwatch, foam (medium density), visual dome, and a blindfold were used to implement the CTSIB.8
The elderly patient was instructed to remain in each sensory condition for 30 s without making any steps to compensate for any instability; and to not move the upper limbs, heels, or feet. If the patient could not maintain stability with the above restrictions, time was stopped and the test was considered abnormal. The order of performance of conditions was randomized and the patient was allowed only one attempt to perform each condition. The base of support used was barefoot, with feet together, also called the Romberg position.8, 10 The result of the CTSIB was analyzed with respect to the time spent in seconds and the categorization as “normal” or “altered” for each sensory condition.
The BRU™ consists of a computer program for the analysis of postural control; a metal safety structure (protection support with straps and belt); force platform; virtual reality goggles; blindfold; accelerometer; and foam.9 It evaluates the individual's postural control under ten sensory conditions: (1) FS and eyes open; (2) FS with the eyes closed; (3) foam and eyes closed; (4) FS and saccadic stimulation; (5) FS and optokinetic stimulation in the horizontal direction from left to right; (6) FS and optokinetic stimulation in the horizontal direction from right to left; (7) FS and optokinetic stimulation with vertical direction downward; (8) FS and optokinetic stimulation with vertical direction upward; (9) FS and optokinetic stimulation with horizontal direction associated with slow and uniform head rotation movements; (10) FS and optokinetic stimulation with vertical direction associated with slow and uniform flexion–extension head movements.9
Sensory conditions 5 and 6, as well as 7 and 8, were grouped. Thus, there was a renaming of the conditions according with the sensory stimuli and the progression of difficulty in posturography, as shown in Table 1.
Table 1.
Conditions assessed by the Balance Rehabilitation Unit™ (BRU™), regrouped and renamed according to the stimuli involved and progression.
| Conditions | BRU™ conditions | Conditions | BRU™ conditions regrouped and renamed for the study |
|---|---|---|---|
| 1 | No stimulus, FS, OE | 1 | No stimulus, FS, OE |
| 2 | No stimulus, FS, CE | 2 | No stimulus, FS, CE |
| 3 | No stimulus, foam surface, OE | 6 | No stimulus, foam surface, CE |
| 4 | Saccadic, FS, OE | 3 | Saccadic, FS, OE |
| 5 | Optokinetic, Bars (to the right), FS, OE | 4 horizontal | Arithmetic mean Optokinetic, Bars (to the right), FS, OE and Optokinetic, Bars (to the left); FS, OE |
| 6 | Optokinetic, Bars (to the left); FS, OE | ||
| 7 | Optokinetic, Bars (downward): FS, CE | 4 vertical | Arithmetic mean Optokinetic, Bars (downward), FS, OE and Optokinetic, Bars (upward); FS, OE |
| 8 | Optokinetic, Bars (upward): FS, OE | ||
| 9 | Vestibular–visual interaction, Circular, Bars (horizontal direction), FS, OE | 5 horizontal | Vestibular–visual interaction, Circular, Bars (horizontal direction), FS, OE |
| 10 | Vestibular–visual interaction, Circular, Bars (vertical direction), FS, OE | 5 vertical | Vestibular–visual interaction, Circular, Bars (vertical direction), FS, OE |
FS, firm surface; OE, open eyes; CE, closed eyes.
The evaluation of each condition was carried for 60 s with the elderly individual in static posture, with arms along the side of the body. The support base used by posturography was barefoot, with a distance of 10° from the midline of the anterior portion of each foot on the platform, forming a 20° angle between the two great toes.6 The software uses the midpoint of the intermalleolar line as center of the standard border of the stability circle.
The parameters evaluated were: area of center of pressure (COP) displacement (elliptical area of COP with distribution of 95%) and velocity of body sway (VBS) (total distance divided by 60 s) in seconds for each sensory condition.9 In case of inability to maintain body balance in the standing position for the 60 s, the parameters of the interrupted condition were not recorded by the program.
Statistical analysis
Descriptive data analysis was performed to characterize the sample. To verify time differences in the CTSIB conditions of and between values of posturography evaluation parameters, according to the progression of sensory conditions of these tests, the Wilcoxon test was used for independent samples, in which the means of these conditions were compared two by two. The significance level for the statistical tests was 5% (α = 0.05). Statistical analyses were performed using the computer program SPSS 17.0.
Results
The sample consisted of 123 patients with chronic vestibular dysfunction, mostly females (n = 98; 79.7%), with a mean age of 73.11 ± 5.6 years. The elderly had on average 3.54 ± 1.71 diseases, used 3.75 ± 1.98 drugs, and 48.8% reported falls in the previous year. Regarding the type of dizziness, 39% of the sample reported having both types of dizziness, followed by 32.5% with vertigo and 28.5% with non-rotatory dizziness.
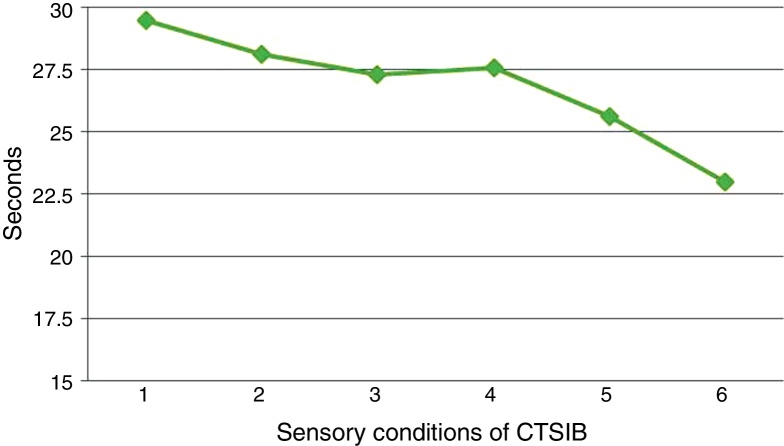
Most elderly with chronic vestibular disorders showed normality (ability to maintain stability for 30 s) under the conditions of the CTSIB. Sensory condition VI had the highest number of abnormal cases and the shortest average duration of time spent on the test (Table 2). Fig. 1 shows a comparative representation of the sensory condition means of CTSIB according to the test progression.
Table 2.
Frequencies and variability of conditions at the Clinical Test of Sensory Interaction and Balance (CTSIB) in elderly individuals with chronic vestibular disorders.
| CTSIB conditions | Cases | Mean (SD) | 95% CI | |
|---|---|---|---|---|
| I | N | 119 (96.7%) | 29.44 (3.26) | 28.86–30.0 |
| A | 4 (4.3%) | |||
| II | N | 107 (87.0%) | 28.11 (5.73) | 27.09–29.13 |
| A | 16 (13%) | |||
| III | N | 104 (84.6%) | 27.28 (7.26) | 25.99–28.58 |
| A | 19 (15.4%) | |||
| IV | N | 109 (88.6%) | 27.56 (7.04) | 26.30–28.82 |
| A | 14 (11.4%) | |||
| V | N | 91 (74.0%) | 25.01 (9.42) | 23.32–26.69 |
| A | 32 (26.0%) | |||
| VI | N | 82 (62.7%) | 22.99 (10.11) | 21.08–24.90 |
| A | 41 (33.3%) | |||
N, normal; A, altered.
Figure 1.
Sensory conditions of the Clinical Test of Sensory Interaction and Balance (CTSIB). Graph representation of the progression of time of sensory conditions of the CTSIB in elderly individuals with chronic vestibular dysfunction.
Regarding the CTSIB progression, there was a decrease in time spent in sensory conditions 1–2 (p = 0.001), 4–5 (p < 0.001), and 5–6 (p = 0.002). There was no significant difference from conditions 2 to 3 (p = 0.136) and 3 to 4 (p = 0.745).
Table 3 shows data from the COP area and the VBS of the BRU™ conditions. The results show that the highest mean of the COP area and VBS was found in condition 6. It was not possible to collect the parameters of three elderly in condition 6, but in the other conditions all subjects completed the time required for recording.
Table 3.
Sway velocity variability (cm/s) and the area of the center of pressure (cm2) of the Balance Rehabilitation Unit™ (BRU™) conditions in elderly individuals with chronic vestibular disorders.
| BRU™ conditions | VBS (cm/s) |
COP area (cm2) |
|||
|---|---|---|---|---|---|
| Mean (SD) | 95% CI | Mean (SD) | 95% CI | ||
| 1 FS/OA | 1.01 (0.40) | 0.94–1.08 | 3.88 (3.80) | 3.20–4.56 | |
| 2 FS/OF | 1.34 (0.57) | 1.23–1.44 | 4.90 (5.96) | 3.83–5.97 | |
| 3 FS/saccadic | 1.34 (0.50) | 1.25–1.43 | 2.93 (2.23) | 2.53–3.32 | |
| 4 | Horizontal | 1.23 (0.44) | 3.69 (3.53) | 3.69 (3.53) | 3.05–4.32 |
| Vertical | 1.31 (0.69) | 3.96 (3.47) | 3.96 (3.47) | 3.24–4.48 | |
| 5 | Horizontal | 1.75 (0.74) | 6.07 (4.87) | 6.07 (4.87) | 5.20–6.94 |
| Vertical | 1.74 (0.62) | 6.41 (4.10) | 6.41 (4.10) | 4.68–6.15 | |
| 6 | Foam/OF | 3.01 (1.24) | 15.00 (12.25) | 15.00 (12.25) | 12.78–17.22 |
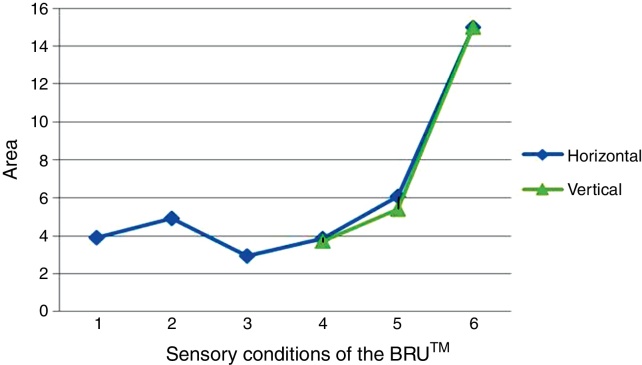
The comparative representation of the progression of the means of COP area at the sensory conditions of BRU™ is shown in Fig. 2.
Figure 2.
Sensory conditions of the Balance Rehabilitation Unit™ (BRU™). Graph representation of the progression of the means of the center of pressure area of the sensory conditions posturographic assessment of elderly individuals with chronic vestibular dysfunction.
When comparing the progress of the means of COP area in the BRU™ conditions, we observed, a significant increase from conditions 1 to 2 (p = 0.013), 3 to 4 vertical (p = 0.001), 4 to 5 horizontal (p < 0.001), 4 to 5 vertical (p < 0.001), 5 horizontal to 6 (p < 0.001), and 5 vertical to 6 (p < 0.001). There was a statistically significant decrease in the area from condition 2 to 3 (p = 0.001). From condition 3 to 4 horizontal (p = 0.053), there was a tendency to increase.
When comparing the COP area with respect to the stimulus direction, no statistical difference was observed between conditions 4 horizontal and 4 vertical (p = 0.479) and 5 horizontal and 5 vertical (p = 0.112).
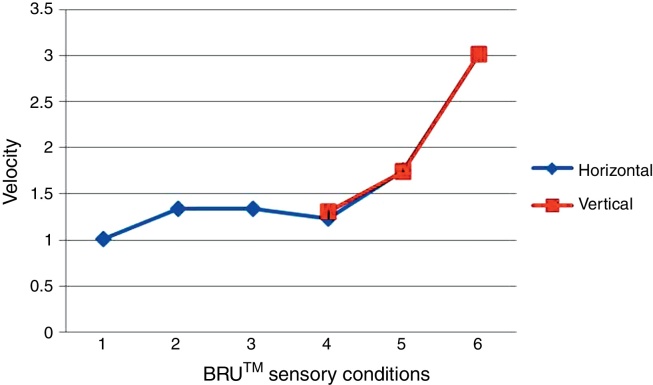
The comparative representation of the progression of means of VBS in the sensory BRU™ conditions is shown in Fig. 3.
Figure 3.
Progression of VOC means. Graph representation of the progression of the means of sway velocity of sensory conditions in posturographic assessment of elderly individuals with chronic vestibular dysfunction.
When comparing the progression of means of VBS conditions in the BRU™ conditions, a statistically significant increase was observed from condition 1 to 2 (p < 0.001), 4 to 5 horizontal (p < 0.001), 4 to 5 vertical (p < 0.001), 5 horizontal to 6 (p < 0.001), and 5 vertical to 6 (p < 0.001). There was a statistically significant decrease from condition 3 to 4 horizontal (p < 0.001) and 3 to 4 vertical (p = 0.007). There was no statistically significant difference in conditions 2 and 3 (p = 0.453).
When comparing VBS with respect to the direction of the stimulus, no statistical difference was observed between the 4 horizontal and 4 vertical conditions (p = 0.225) and 5 horizontal and 5 vertical conditions (p = 0.157).
Discussion
The clinical and laboratory assessments carried out in this study identified an impairment of sensory information that affects postural control in elderly patients, as these results differ from those of the elderly population in general.8
The composition of the sample in the present study was representative of the elderly population with vestibular disorders, i.e., mostly female and elderly. Women aged 65 years and older have a 1.81% greater chance of reporting problems related to dizziness when compared to men (95% CI: 1.38–2.38).4 Dizziness constitutes the second most prevalent symptom worldwide in individuals up to 65 years of age and its prevalence is approximately 80% in those aged 75 years or older.1
Falls in the elderly are the principal complication of disorders of body balance.11 There are several factors associated with falls, but dizziness of vestibular origin is noteworthy, as population studies show that the chance of falling increases by threefold (OR: 3.0; 95% CI: 1.9–5.0) in the presence of this complaint.12 This study, and others, showed a higher prevalence of falls in elderly patients with vestibular disorders5, 6 compared to elderly individuals from the same community without vestibular disorders.11
Our study noted the presence of both rotatory and non-rotatory dizziness in approximately 40.0% of patients, which is different from the study by Gazzola et al.11 One possible explanation for this finding is the concomitant involvement of other systems involved in body balance in conjunction with the vestibular system, suggesting a probable multifactorial sensory disorder.
We chose the CTSIB as our method of clinical assessment because it is easy to apply, is low in cost and can assist in the rehabilitation assessment. The results of this study using the CTSIB show that the performance of the elderly with vestibular disorders declines from condition I to II, i.e., when there is loss of visual information. Vision guides the body's position in relation to the surrounding environment and plays a key role in delayed stabilization of postural corrections and in the planning of anticipatory reactions.13
We previously reported a decrease in the time spent in condition II compared to condition I in elderly individuals from the community with a history of recurrent falls8 although we found no difference between these conditions for those without falls. In the case of elderly patients with a compromised system, the vestibular system or even a history of falls discloses the dependence on the visual system for body stabilization.
The absence of differences between conditions II, III, and IV indicates that when only two systems are active and one of them is the vestibular system, which was impaired in our elderly subjects, the remaining system, be it visual or proprioceptive, could not meet the necessary demands for postural control by itself.
The change from two systems (condition IV) to a single system (conditions V and VI) was even more challenging for our elderly subjects with vestibular disorders. In the last two conditions of the CTSIB, the vestibular system was the only accurate sensory source. Studies have shown that in conditions V and VI, performed with eyes closed, feet on an unstable surface, and with visual conflict, more than 50% of the elderly with a history of falls cannot successfully rely on exclusively vestibular information and interrupt the test before 30 s.14, 15
These results were even worse in the elderly patients with vestibular disorders in our study, since our patients had a previous limitation of the vestibular system. The data revealed these conditions to be the most challenging with respect to the time spent on the test by the elderly patients, showing the visual dependence of the elderly with chronic vestibular disorders on certain sensory conditions for static body balance. Conditions V and VI had the highest number of altered cases, 32 (26%) and 41 (33.3), respectively, and the lowest mean time spent on the test, 25.01 ± 9.42 and 22.99 ± 10.11 s, respectively.
Thus, the CTSIB can elucidate the difficulty individuals with vestibular disorders have in the most challenging conditions and can help direct rehabilitation through stimulation of the remaining systems.
Integrated virtual reality (BRU™) is a more sophisticated test that requires adequate equipment and is not always available in the clinical setting. Thus, computerized posturography complements conventional tests of otoneurological assessment, providing quantitative information about the influence of sensory systems on body balance control, in addition to promoting disruption of visual information through virtual reality stimuli to maintain body balance.16
In condition 1, the baseline condition of posturography evaluation, the COP area and the VBS showed no changes when compared to data from healthy elderly.6 These results are similar to the findings of other authors17, 18 who demonstrated normal values of COP and VBS for most patients with chronic vestibular dysfunction in this condition. This is because the visual and somatosensory cues for maintaining body balance are able to compensate for the inaccurate information from the vestibular system.
Thus, as in the CTSIB, computerized posturography showed a difference in the COP and VBS in conditions 1–2, documenting the dependence on the visual system in the presence of vestibular dysfunction in the elderly. In condition 2 of the posturography assessment (FS and CE), we observed differences in COP area between elderly subjects who were healthy and elderly patients with vestibular disorders whether they maintained stability or fell one or more times. We also observed differences on VBS scores between elderly patients with vestibular disorders who fell and healthy elderly subjects, and between elderly patients with vestibular disorders who did not fall and those who did fall. These results indicate that the use of visual information is very important for the control of body balance, especially in the elderly.6
Buatois et al. observed similar findings between groups (did not fall/history of one fall/history of two or more falls) of healthy and functionally active elderly on the balance score in condition 2 of the Sensory Organization Test (SOT), fixed surface and CE.19
With the introduction of visuo-vestibular stimuli, we found that condition 3 (saccade stimulus) added no difficulty to postural control, either by VBS or COP area, in contrast to conditions 4 and 5, which showed progressive difficulties.
Condition 3 used saccadic stimuli, related to rapid and small eye movements, which are intended to position the image and movement onto the fovea, and, thus, improve eyesight.16 In this study, the optokinetic stimuli appeared to stimulate and cause more dysfunction in elderly patients than saccadic stimuli. There are few studies on the influence of saccadic stimulation on postural control. In this third condition, the differences we saw in the COP area parameters were between elderly patients with vestibular disorders who fell and healthy elderly subjects, and between elderly patients with vestibular disorders who did not fall and those elderly patients with vestibular disorders who did fall, with the higher values observed for those who fell.
These findings were also identified, in the same condition, in a study that reported higher values of the COP area through posturography evaluation in a group of 57 subjects older than 65 years (67–82 years) with a history of instability and falls in the previous year, when compared to the postural responses of 46 healthy volunteers (aged 29–75 years) evaluated as a control group.20
Conditions 4 horizontal and 4 vertical use optokinetic stimulation, which combines saccadic and smooth pursuit mechanisms, produced by repeated movements through a stationary visual field to provide clear images for visual stimulation. The optokinetic stimuli are considered intense because the perception of neurovegetative symptoms can occur even without movement of the individual.21 The optokinetic stimuli can be more challenging for patients with vestibular dysfunction, as shown in the present study, and also in healthy elderly with a history of falls.20 However, the direction of the stimulus does not seem to influence postural control, since there was no statistically significant difference between conditions 4 horizontal and 4 vertical.
The conditions 5 horizontal and 5 vertical were even more challenging than condition 4. These conditions evaluate the performance of the vestibulo-ocular reflex (VOR) associated with optokinetic stimulation in the horizontal and vertical directions, associated with slow and uniform rotation or flexion–extension movements of the head. Again, it was shown that the difficulties imposed by the test do not depend on the stimulus direction. The study by Suarez et al.22 observed that elderly individuals with postural instability evaluated by BRU™ had a significant increase in COP and VBS in conditions of visual–vestibular interaction when compared to healthy elderly, probably because elderly with body imbalance have greater difficulty in stabilizing the retinal image, which infers VOR damage.
Among all the BRU™ conditions, the one that showed the highest degree of difficulty for both the VBS and the COP area was condition 6. This condition, in addition to suppression of visual stimuli, includes alteration of somatosensory information with the use of foam, causing individuals to depend more on vestibular function, which explains the difficulty in maintaining postural control by the elderly patients with vestibular disorder. This result is similar to that of the CTSIB.
Similar to the present study, other authors23 observed higher values of the VBS and COP area in relation to the other conditions. When comparing healthy elderly with young individuals, it has been shown that when proprioception is altered (unstable surface) and vision is removed (eyes closed), elderly subjects showed significantly higher sway than younger individuals.24
Therefore, both the clinical and laboratory tests showed that the condition on the foam surface with eyes closed is clearly the most challenging, particularly for elderly individuals with vestibular dysfunction, as the vestibular system cannot alone convey appropriate information for postural control.
Therefore, the findings of the present study can assist in the choice of conditions to be prioritized as a screening test in elderly patients with a complaint of dizziness and in the development of protocols that might include different stimuli (foam, virtual reality, visual occlusion, dome, proprioceptive boards, among others) according to the results of the sensory test.
Conclusions
The present study showed a decrease in static body balance in the elderly with chronic vestibular dysfunction as sensory conditions become more challenging, i.e., stable surface and visual stimuli such as optokinetic and visuovestibular interaction, and unstable surface.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Macedo C, Gazzola JM, Ricci NA, Doná F, Ganança FF. Influence of sensory information on static balance in older patients with vestibular disorder. Braz J Otorhinolaryngol. 2015;81:50–7.
References
- 1.Ganança M.M., Caovilla H.H. In: Princípios de otoneurologia. Série Distúrbios de Comunicação Humana. Ganança M.M., Vieira R.M., Caovilla H.H., editors. Atheneu; São Paulo: 1998. A vertigem e sintomas associados; pp. 3–5. [Google Scholar]
- 2.Tinetti M.E., Williams C.S., Gill T.M. Health, functional, and psychological outcomes among older persons with chronic dizziness. J Am Geriatr Soc. 2000;48:417–421. doi: 10.1111/j.1532-5415.2000.tb04700.x. [DOI] [PubMed] [Google Scholar]
- 3.Matsumura B.A., Ambrose A.F. Balance in the older elderly. Clin Geriatr Med. 2006;22:395–412. doi: 10.1016/j.cger.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Stevens K.N., Lang I.A., Guralnik J.M., Melzer D. Epidemiology of balance and dizziness in a national population: findings from the English Longitudinal Study of Ageing. Age Ageing. 2008;37:300–305. doi: 10.1093/ageing/afn019. [DOI] [PubMed] [Google Scholar]
- 5.Gassmann K.G., Rupprecht R. Dizziness in an older community dwelling population: a multifactorial syndrome. J Nutr Health Aging. 2009;13:278–282. doi: 10.1007/s12603-009-0073-2. [DOI] [PubMed] [Google Scholar]
- 6.Gazzola J.M. Universidade Federal de São Paulo; São Paulo: 2010. Controle postural de idosos vestibulopatas crônicos com e sem histórico de quedas submetidos à estimulação visual por realidade virtual. [Thesis] [Google Scholar]
- 7.Shumway-Cook A., Horak F.B. Assessing the influence of sensory interaction on balance. Suggestion from the field. Phys Ther. 1986;66:1548–1550. doi: 10.1093/ptj/66.10.1548. [DOI] [PubMed] [Google Scholar]
- 8.Ricci N.A., Gonçalves D.F.F., Coimbra A.M., Coimbra I.B. Sensory interaction on static balance: a comparison concerning the history of falls of community-dwelling elderly. Geriatr Gerontol Int. 2009;9:165–171. doi: 10.1111/j.1447-0594.2009.00516.x. [DOI] [PubMed] [Google Scholar]
- 9.BRU®. Unidade de reabilitação do equilíbrio. Manual do usuário. Versão 1.0.7. Versão do Software: 1.3.5.0. Uruguay: Medicaa; 2006.
- 10.Whitney S.L., Wrisley D.M. The influence of footwear on timed balance scores of the modified clinical test of sensory interaction and balance. Arch Phys Med Rehabil. 2004;85:439–443. doi: 10.1016/j.apmr.2003.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Gazzola J.M., Ganança F.F., Aratani M.C., Perracini M.R., Ganança M.M. Clinical evaluation of elderly people with chronic vestibular disorder. Braz J Otorhinolaryngol. 2006;72:515–522. doi: 10.1016/S1808-8694(15)30998-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaßmann K.G., Rupprecht R., Freiberger E. Predictors for occasional and recurrent falls in community-dwelling older people. Z Gerontol Geriat. 2009;1:3–10. doi: 10.1007/s00391-008-0506-2. [DOI] [PubMed] [Google Scholar]
- 13.Carvalho R.J., Almeida G.L. Aspectos sensoriais e cognitivos do controle postural. Rev Neurociênc. 2009;17:156–160. [Google Scholar]
- 14.Nascimento B.N., Duarte B.V., Antonini D.G., Borges S.M. Risco para quedas em idosos na comunidade; relação entre tendência e susceptibilidade. Rev Bras Clin Med. 2009;7:95–99. [Google Scholar]
- 15.Cohen H., Blatchly C.A., Gombash L.L. A study of the clinical test of sensory interaction and balance. Phys Ther. 1993;73:346–351. doi: 10.1093/ptj/73.6.346. [DOI] [PubMed] [Google Scholar]
- 16.Netto A.T.C., Colafemina J.F. Movimentos sacádicos em indivíduos com alterações cerebelares. Braz J Otorhinolaryngol. 2010;76:78–83. [Google Scholar]
- 17.Herdman S.J., Blatt P., Schubert M.C., Tusa R.J. Falls in patients with vestibular deficits. Am J Otol. 2000;21:847–851. [PubMed] [Google Scholar]
- 18.Pedalini M.E., Cruz O.L., Bittar R.S., Lorenzi M.C., Grasel S.S. Sensory organization test in elderly patients with and without vestibular dysfunction. Acta Otolaryngol. 2009;13:1–4. doi: 10.1080/00016480802468930. [DOI] [PubMed] [Google Scholar]
- 19.Buatois S., Gueguen R., Gauchard G.C., Benetos A., Perrin P.P. Posturography and risk of recurrent falls in healthy non-institutionalized persons aged over 65. Gerontology. 2006;52:345–352. doi: 10.1159/000094983. [DOI] [PubMed] [Google Scholar]
- 20.Suarez H., Arocena M., Geisinger D., Suarez A., Carrera X. In: Accidental falls: causes, preventions and interventions. Vincent M.L., Moreau T.M., editors. Nova Science; New York: 2008. Analysis of the role of virtual reality technology in the assessment and rehabilitation of Instability in the elderly population; pp. 107–120. [Google Scholar]
- 21.Cordeiro R.C. Universidade Federal de São Paulo/Escola Paulista de Medicina; São Paulo: 2002. Caracterização clínico-funcional do equilíbrio em idosos portadores de Diabetes Mellitus do tipo II. [Dissertation] [Google Scholar]
- 22.Suarez H., Geisinger D., Suarez A., Carrera X., Spiller P., Lapilover V. Postural strategies in normal subjects and in patients with instability due to central nervous system diseases after sudden changes in the visual flow. Acta Otolaryngol (Montevideo) 2008;128:398–403. doi: 10.1080/00016480701730018. [DOI] [PubMed] [Google Scholar]
- 23.Suarez H., Arocena M. Las alteraciones del equilibrio en el adulto mayor. Rev Méd Clín Condes. 2009;20:401–407. [Google Scholar]
- 24.Teasdale N., Stelmach G., Breuning A., Meeuwsen H. Age differences in visual sensory integration. Exp Brain Res. 1991;85:691–698. doi: 10.1007/BF00231755. [DOI] [PubMed] [Google Scholar]