Introduction
In the past decade, we have witnessed the introduction and dissemination of transoral robotic surgery for the treatment of tumors, mainly of the oropharynx and larynx. The use of robotic surgery improves visualization of the operative field due to its three-dimensional image and enhances the surgeon's dexterity due to bimanual control of the robotic arms. Furthermore, the assistant contributes with suction and tissue traction, which leads to the use of four instruments during surgery, something impossible during a transoral resection through laryngoscopy, for instance.1 Therefore, the technique makes the approach truly minimally invasive, especially in the case of supraglottic partial laryngectomy, in which the conventional open approach inevitably leads to protective tracheostomy and feeding tube use, sometimes for prolonged periods. The robotic access, however, allows for early feeding without the need of a tube, and also eliminates the need for tracheostomy in many cases, as the rates of aspiration, fistulas, or other complications are significantly reduced when compared with conventional surgery and with oncologic and functional results that are quite similar between the two techniques.2
Therefore, this study reports the first case of supraglottic partial laryngectomy performed by transoral robotic surgery in Brazil, as well as documents the late oncologic and functional results (Approved by the Research Ethics Committee under No. 228/14).
Case report
A 57-year-old female patient was evaluated for a four month complaint of odynophagia; she was a long-term smoker (30 pack-years) and a non-alcoholic. Physical examination revealed no lesions at the oroscopy and no palpable cervical lymph nodes. The nasofibrolaryngoscopy identified a large vegetating lesion affecting the entire epiglottis and extending to the left aryepiglottic fold, but not affecting the arytenoid fold or the left ventricular fold; both vocal folds were still mobile.
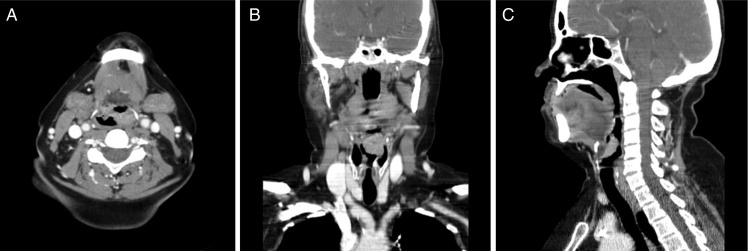
An incisional biopsy revealed that the lesion was a moderately differentiated squamous cell carcinoma (SCC). Assessment by computed tomography (Fig. 1) showed that the lesion had limits compatible with the laryngoscopy, without pre-epiglottic space involvement and without cervical lymph nodes suggestive of metastases. There was no evidence of pulmonary metastases; the search for a second primary tumor through high digestive endoscopy with chromoendoscopy was negative, and the cancer was staged as T2N0M0 (stage II).
Figure 1.
Computed tomography depicting a vegetative lesion in the epiglottis and affecting the left aryepiglottic fold in the axial (A), coronal (B), and sagittal (C) views.
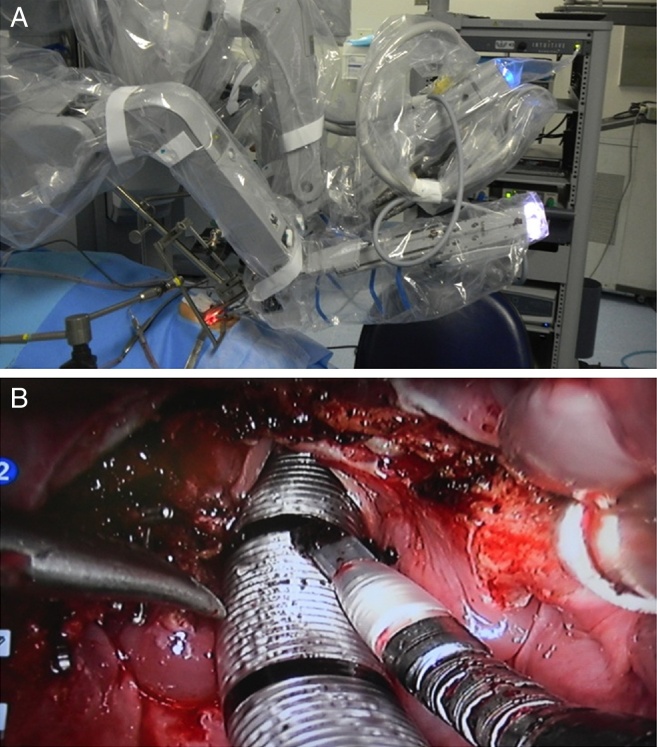
The patient then underwent a transoral robotic supraglottic partial laryngectomy using the daVinci SI Surgical System® (Intuitive Surgical®; Sunnyvale, California, United States) equipment (Fig. 2). The procedure was uneventful, lasted 158 minutes, had a 50-mL blood loss and the resection had clear intraoperative frozen section margins. There was no need for tracheostomy and the patient was extubated in the operating room under endoscopic view. Also, the use of a parenteral feeding tube was not necessary, and the patient received a thickened liquid diet on the second postoperative day, without evidence of aspiration. The length of hospital stay was three days. Definitive anatomopathological analysis disclosed a moderately differentiated SCC without perineural or angiolymphatic invasion with margins free of tumor.
Figure 2.
Intraoperative period. (A) Positioning of robotic arms and optical sensor; (B) surgical wound appearance after supraglottic laryngectomy.
After 24 postoperative days, the patient underwent uneventful selective cervical dissection of levels II, III, and IV bilaterally and histopathological analysis found no metastases in 57 dissected lymph nodes; she was discharged within 72 hours.
There was no indication for adjuvant treatment, and the patient remains on outpatient follow-up, with no evidence of disease, with a normal diet and no voice alterations at 42 months of follow-up.
Discussion
Since the first published work by Weinstein in 20073 with the description of the first three cases, other centers began to perform supraglottic laryngectomy using the transoral robotic approach, but the number of reported cases is still low. The largest series in the literature included 84 surgeries performed in seven French services.1 The authors demonstrated that the mean time of parenteral tube use was eight days and 24% of patients resumed oral intake 24 hours after the procedure. Only 24% of patients required a tracheostomy, but there was aspiration pneumonia in 23% of cases, including one death for that reason. Postoperative bleeding occurred in 15 patients and 51% of the patients required adjuvant radiotherapy due to the anatomopathological findings, but there is no description in this study of the oncologic outcomes in these patients.
Therefore, a systematic review in the Medline database until September 2015 (using the key words [“laryngectomy” and “robotic surgery”]) was performed, and it retrieved 11 articles,1, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 totaling 176 cases, in addition to the patient reported herein (Table 1). It was observed that most of the included patients had tumors at an early stage (stages I and II) and that the surgery was performed with free margins in most cases, with few complications. The need for tracheostomy and a parenteral feeding tube was variable, but brief, in most cases. The need for adjuvant therapy was low and oncologic results showed no cases of local recurrence, demonstrating the safety of the method.
Table 1.
Results of the systematic review of published cases of robotic supraglottic partial laryngectomy due to squamous cell carcinoma.
| Study | n | Age (years) | Primary lesion | cT | cN | Neck Dissection | Margins |
|---|---|---|---|---|---|---|---|
| Weinstein 20073 | 3 | 59 | Supraglottic | T2 | N0 | Yes | Free |
| 59 | T2 | N0 | Yes | Free | |||
| 69 | T3 | N0 | Yes | Free | |||
| Alon 20124 | 7 | 72 | Supraglottic | T2 | N1 | Yes | Free |
| 51 | T1 | N0 | Yes | Free | |||
| 45 | T3 | N0 | Yes | Free | |||
| 57 | T2 | N0 | Yes | Free | |||
| 67 | T2 | N2b | Yes | Free | |||
| 67 | T1 | N1 | Yes | Free | |||
| 71 | T2 | Yes | Free | ||||
| Ozer 201210 | 13 | 58 (mean) | EP (100%) | 1 T1 | 11 N0 | Yes (all) | Free (all) |
| AEF (76.9%) | 10 T2 | 2 N2b | |||||
| VF (23%) | 2 T3 | ||||||
| BT (23%) | |||||||
| EP (15.3%) | |||||||
| PS (15.3%) | |||||||
| Ansarin 20135 | 10 | 68 (mean) | Supraglottic | 2 T1 | 6 N0 | 40% | Positive in 40% of patients |
| 6 T2 | 4 N+ | ||||||
| 2 T3 | |||||||
| Lallemant 20138 | 10 | 64 | EP/AEF | T2 | N2c | Yes | Free |
| 67 | EP | T2 | N1 | Yes | Free | ||
| 75 | EP | T1 | N0 | Yes | Free | ||
| 63 | EP/AEF | T1 | N0 | Yes | Free | ||
| 60 | EP/AEF/BT | T2 | N2b | Yes | Free | ||
| 50 | VF | T1 | N0 | Yes | Free | ||
| 59 | AEF | T1 | N0 | Yes | Positive | ||
| 60 | AEF/VF/AT | T2 | N0 | Yes | Free | ||
| 67 | AT/AEF | T2 | N0 | Yes | Free | ||
| 51 | AEF/VF | T2 | N0 | Yes | Positive | ||
| Mendelsohn 20139 | 18 | ND | Supraglottic | 5 T3/4a | 6 NDis | Free in all cases | |
| 13 T1/2 | 12 SL | ||||||
| Park 201311 | 16 | 66 (mean) | 10 EP | 7 T1 | 9 N0 | Yes (No for 2 cases of EP T1N0) | Positive in 2 cases (12%) |
| 4 AEF | 5 T2 | 3 N1 | |||||
| 2 VF | 4 T3 | 3 N2b | |||||
| 3 N2c | |||||||
| Durmus 20146 | 1 | 45 | EP/VF | T2 | N0 | Yes | ND |
| Kayhan 20147 | 13 | 60 (mean) | Supraglottic | 4 T1 | 9 N0 | Yes (all) | Free in all cases |
| 9 T2 | 3 N2c | ||||||
| 1 N3 | |||||||
| Perez-Mitchel 201412 | 1 | 68 | VF | T2 | N0 | No | Positive |
| Razafindranaly 20151 | 84 | 59 (mean) | Supraglottic | 29 T1 | 54 N0 | 67 cases (80%) | Positive in 8 cases (9.5%) |
| 46 T2 | 11 N1 | ||||||
| 9 T3 | 4 N2a | ||||||
| 9 N2b | |||||||
| 5 N2c | |||||||
| 1 N3 | |||||||
| Study | Perioperative complications | TCT (days) | ENS/GTM (days) | Hospital length of stay (days) | Adjuvant treatment | Local recurrence |
|---|---|---|---|---|---|---|
| Weinstein 20073 | No | – | – | 3 | – | ND |
| No | – | – | 8 | – | ||
| No | – | – | 5 | CT + RT | ||
| Alon 20124 | No | – | – | ND | – | No |
| No | – | 56 | – | No | ||
| Burning | 4 | 38 | – | No | ||
| No | 45 | 45 | – | No | ||
| No | Dependent | GTM RT | RT | No | ||
| No | – | – | – | No | ||
| No | – | GTM RT | RT | No | ||
| Ozer 201210 | 1 conversion to negative margins | 17 (1 case) | 40 (1 case) | 3.9 (mean) | RT (2 cases N+) | No (median of 6.8 months) |
| Ansarin 20135 | None in 10 cases | 90% | 70% (mean 12 days) | 13 ± 6 days (mean) | 70% (5 CT + RT; 1 new surgery for free margins; 1 RT) | No (median of 5 months) |
| Lallemant 20138 | No | 4 | 5 | ND | CT+RT | No |
| No | – | 2 years | RT | No | ||
| No | – | 21 | – | No | ||
| No | – | – | – | No | ||
| No | – | 20 | CT+RT | No | ||
| Bleeding | – | – | – | No | ||
| No | – | 2 | RT | No | ||
| No | – | 8 | – | No | ||
| No | 3 | 5 | – | No | ||
| No | 3 | 4 | – | No | ||
| Mendelsohn 20139 | None in 18 cases | None | 0% GTM (ENS: ND) | 11 (median) | 10 CT+RT | No |
| Park 201311 | None | Yes (all cases; mean 11.2 days) | Yes (all cases; mean 8.3 days) | 13.5 (mean) | Yes in 8 cases (RT 3 cases, CT+RT 5 cases) | No (mean of 20.3 months) |
| Durmus 20146 | No | – | – | ND | – | ND |
| Kayhan 20147 | 2 cases of aspiration pneumonia | 1 case | Yes (all; mean 21.3 days) | Yes (all; mean 8 days) | 5 CT + RT | (mean of 14.1 months) |
| Perez-Mitchel 201412 | No | 3 (OTI) | 14 | 5 | – | No (median of 30 months) |
| Razafindranaly 20151 | 1 conversion | 24 cases (24%; mean 8 days; 1 case dependent on TCT) | 64 cases (76%; mean of 8 days; 1 case of permanent GTM) | 15.1 (mean) | CT+RT in 43 cases (51%) | ND |
| 16 cases of bleeding | ||||||
| 19 cases of aspiration pneumonia | ||||||
| 1 pharyngocutaneous fistula | ||||||
–, procedure not performed; AEF, aryepiglottic fold; AT, arytenoid; BT, base of tongue; CT, chemotherapy; ENS, Enteral nutrition support?; E.P, epiglottis; GTM, gastrostomy; NDis, neck dissection; ND, no data; OTI, orotracheal intubation; PS, pyriform sinus; RT, radiotherapy; SL, sentinel lymph node screening; TCT, tracheostomy; VF, ventricular fold; VF, vocal fold
In this case, some aspects are noteworthy and were later verified by other studies summarized here: the patient had an uneventful postoperative period, in addition to very satisfactory oncologic and functional results. The desire to provide the patient's late follow-up status led to the delay in reporting the present case.
Conclusion
This case describes the viability of supraglottic partial laryngectomy by transoral robotic approach, with good postoperative evolution and early rehabilitation. It is therefore a safe method, with very satisfactory oncologic and functional results.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Please cite this article as: Cernea CR, Matos LL, de Carlucci Junior D, Leonhardt FD, Haddad L, Walder F. Transoral robotic supraglottic partial laryngectomy: report of the first Brazilian case. Braz J Otorhinolaryngol. 2018;84:660–64.
Peer Review under the responsibility of Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial.
Contributor Information
Claudio Roberto Cernea, Email: cerneamd@uol.com.br.
Leandro Luongo Matos, Email: lmatos@amchan.com.br.
References
- 1.Razafindranaly V., Lallemant B., Aubry K., Moriniere S., Vergez S., De Mones E., et al. Clinical outcomes with transoral robotic surgery for supraglottic squamous cell carcinoma: experience of a French evaluation cooperative subgroup of GETTEC. Head Neck. 2015;(Suppl. 24):37–43. [PubMed] [Google Scholar]
- 2.Silver C.E., Beitler J.J., Shaha A.R., Rinaldo A., Ferlito A. Current trends in initial management of laryngeal cancer: the declining use of open surgery. Eur Arch Otorhinolaryngol. 2009;266:1333–1352. doi: 10.1007/s00405-009-1028-2. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein G.S., O’Malley B.W., Jr., Snyder W., Hockstein N.G. Transoral robotic surgery: supraglottic partial laryngectomy. Ann Otol Rhinol Laryngol. 2007;116:19–23. doi: 10.1177/000348940711600104. [DOI] [PubMed] [Google Scholar]
- 4.Alon E.E., Kasperbauer J.L., Olsen K.D., Moore E.J. Feasibility of transoral robotic-assisted supraglottic laryngectomy. Head Neck. 2012;34:225–229. doi: 10.1002/hed.21719. [DOI] [PubMed] [Google Scholar]
- 5.Ansarin M., Zorzi S., Massaro M.A., Tagliabue M., Proh M., Giugliano G., et al. Transoral robotic surgery vs transoral laser microsurgery for resection of supraglottic cancer: a pilot surgery. Int J Med Robot. 2014;10:107–112. doi: 10.1002/rcs.1546. [DOI] [PubMed] [Google Scholar]
- 6.Durmus K., Gokozan H.N., Ozer E. Transoral robotic supraglottic laryngectomy: surgical considerations. Head Neck. 2015;37:125–126. doi: 10.1002/hed.23645. [DOI] [PubMed] [Google Scholar]
- 7.Kayhan F.T., Kaya K.H., Yilmazbayhan E.D. Transoral robotic approach for schwannoma of the larynx. J Craniofac Surg. 2011;22:1000–1002. doi: 10.1097/SCS.0b013e3182101580. [DOI] [PubMed] [Google Scholar]
- 8.Lallemant B., Chambon G., Garrel R., Kacha S., Rupp D., Galy-Bernadoy C., et al. Transoral robotic surgery for the treatment of T1-T2 carcinoma of the larynx: preliminary study. Laryngoscope. 2013;123:2485–2490. doi: 10.1002/lary.23994. [DOI] [PubMed] [Google Scholar]
- 9.Mendelsohn A.H., Remacle M., Van Der Vorst S., Bachy V., Lawson G. Outcomes following transoral robotic surgery: supraglottic laryngectomy. Laryngoscope. 2013;123:208–214. doi: 10.1002/lary.23621. [DOI] [PubMed] [Google Scholar]
- 10.Ozer E., Alvarez B., Kakarala K., Durmus K., Teknos T.N., Carrau R.L. Clinical outcomes of transoral robotic supraglottic laryngectomy. Head Neck. 2013;35:1158–1161. doi: 10.1002/hed.23101. [DOI] [PubMed] [Google Scholar]
- 11.Park Y.M., Kim W.S., Byeon H.K., Lee S.Y., Kim S.H. Surgical techniques and treatment outcomes of transoral robotic supraglottic partial laryngectomy. Laryngoscope. 2013;123:670–677. doi: 10.1002/lary.23767. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Mitchell C., Acosta J.A., Ferrer-Torres L.E. Robotic-assisted salvage supraglottic laryngectomy. P R Health Sci J. 2014;33:88–90. [PubMed] [Google Scholar]