Abstract
Objectives: To explore the clinical effect of electroacupuncture and scalp acupuncture combined with language rehabilitation training on cognitive and speech functions of patients with aphasia after craniocerebral injury. Methods: Seventy patients with aphasia after craniocerebral injury from January 2020 and January 2021 were retrospectively collected after filtering. Among them, 35 patients received language rehabilitation training and were included into a control group, and 35 patients who received electroacupuncture and scalp acupuncture combined with language rehabilitation training were included in a study group. Aphasia quotient score, Loewenstein occupational therapy cognitive assessment (LOTCA) score and Boston Diagnostic Aphasia Examination (BDAE) score of the two groups were compared. The relative risk factors of cognitive function and speech function in the patients were explored by multiple regression analysis. Results: The pretreatment aphasia quotient and LOTCA score between the two groups showed no obvious distinction (P>0.05). After treatment, the LOTCA and BDAE scores in the study group were obviously better than those in the control group (P<0.05). Conclusions: The effect of electroacupuncture and scalp acupuncture combined with language training is remarkable in treating aphasia after severe craniocerebral injury. This combined approach, which can improve the language and cognitive disorders of patients, has valuable application and research prospects in clinic.
Keywords: Electroacupuncture, scalp acupuncture, language rehabilitation training, cognitive function, speech function, craniocerebral injury
Introduction
Aphasia is the loss or damage of acquired language function caused by brain lesions, which can result from cerebrovascular accident, vascular malformation, brain tissue inflammation or brain injury [1]. Previous studies have pointed out that about 75% of patients with craniocerebral injury are accompanied by aphasia, and most of them have speech disorders, auditory processing disorders and receptive language disorders, which harshly affect the lives of patients and can cause a heavy burden on families and society [2,3]. For patients with aphasia after craniocerebral injury, timely diagnosis, effective treatment and functional training can improve their communication skills, which is crucial to restoring their confidence so that they can soon participate in societal activities again [4-6].
At present, the clinical treatment of aphasia after brain injury mainly focuses on rehabilitation training [7-9]. The overall treatment goal is to maximize the patients’ language ability and restore their normal life and work. Some studies have shown that electroacupuncture at brain functional areas and language areas can improve the blood circulation of patients with pathological changes and increase the supply of cerebral blood flow [10,11]. This treatment can also promote the cerebral cortex to produce a strong electrical tension and give full play to the overall treatment effect. In addition, stimulation with electroacupuncture and scalp acupuncture can create collateral circulation around the cerebral infarction or hemorrhage site, attenuate cerebrovascular resistance, increase glucose and blood oxygen supply, and reduce brain tissue damage [12,13].
It can be seen that electroacupuncture and scalp acupuncture have good clinical efficacy in treating brain injury related diseases. Here, we designed a case-control study to explore the clinical effect of electroacupuncture and scalp acupuncture combined with language rehabilitation training on cognitive and speech functions of patients with aphasia after craniocerebral injury.
Materials and methods
Clinical data
A total of 78 patients with aphasia after craniocerebral injury admitted to The Number Two Hospital of Baoding from January 2020 to January 2021 were collected retrospectively. After filtering, 70 patients were included. Among them, 35 patients received language rehabilitation training and were included in a control group, and 35 patients who received electroacupuncture and scalp acupuncture combined with language rehabilitation training were placed in a study group. All the patients voluntarily participated in this study and signed the informed consent form. This research protocol was approved by the ethics committee of The Number Two Hospital of Baoding (HX2022007).
Inclusion criteria
(1) Patients who were diagnosed with aphasia after craniocerebral injury according to the symptoms, signs and conditions, and the classification of language disorder level was 2-3. (2) Patients who had clear consciousness and basically stable conditions. (3) Patients who were over 18 years old. (4) Patients without hearing or visual impairment before onset.
Exclusion criteria
(1) Patients with dysfunction of heart, liver, kidney or lung. (2) Patients who were assessed to have dementia by Mini-Mental State Examination. (3) Patients with serious mental illness. (4) Patients with other complications after brain injury, such as epilepsy, hemiplegia, skull base fracture, hydrocephalus or subdural effusion. (5) Patients who did not complete the whole study or those with poor compliance. (6) Participants in other clinical studies.
Treatment
Treatment for the control group
The patients in the control group (n=35) were treated by language rehabilitation training. The language function of the patients was evaluated, and the training program was developed according to the language ability and aphasia degree of the patients. Targeted and step-by-step language rehabilitation training was given. The content mainly included mouth shape and pronunciation training, practice dialogue following audio, pronunciation muscle training, and individual or targeted training. Firstly, mouth shape and pronunciation training was to guide patients to practice pronunciation by controlling lip and tongue movement through mouth shaping and sound controlling. Also, differentiation training of vowels, initials and similar sounds were distinguished. Secondly, practice following audio was to record the daily-life phrases and sentences into audio, which usually started with a paragraph of encouraging and suggestive language. The patient was asked to repeat following the audio for language training. The rules are “easy first, difficult second” and “phrases first, sentences next”. Thirdly, pronunciation muscle training was to instruct patients to open, grin, close and pout the month, as well as to retract and forward-extend and lift the tongue, so as to strengthen the flexibility. Regular examination was carried out to regularly check the patient’s language function, so as to conduct targeted exercises to improve the pronunciation weaknesses. Individual strengthening exercises were guided if necessary. Targeted training was carried out for patients with different types of aphasia. To be specific, reading and expression were the main focuses for patients with sports aphasia, on oral address and words for patients with naming aphasia, and comprehension and listening for patients with complete aphasia. The language rehabilitation training was performed 30 minutes a day for 4 months.
Treatment for the study group
On the basis of the treatment in the control group, electroacupuncture and scalp acupuncture were given to the patients in the study group (n=35). Head areas, including motor area, sensory area and language area, were selected, and YaMen point, FengFu point and BaiHui point were taken as matching points. Then, 40 mm × 0.35 mm disposable filiform needles (Huatuo brand filiform needle) were inserted into the scalp at 30° to the cap like tendon sheath. The needles were connected to an electroacupuncture therapeutic instrument (Huatuo electroacupuncture therapeutic apparatus SDZ-II), with current intensity of 2 mA and frequency of 50 Hz. Electroacupuncture and scalp acupuncture combined with language rehabilitation training were performed 5 days continuously, then a two-day break, for a total of 4 months.
Evaluation indicators and criteria
The aphasia quotient scores of the 70 patients were evaluated with the Western Aphasia Battery [14]. The Loewenstein occupational therapy cognitive assessment (LOTCA) score (including 4 aspects, 20 items) of the patients were assessed to evaluate patients’ cognitive function in rehabilitation medicine, neurology and neurosurgery [15]. The Boston Diagnostic Aphasia Examination (BDAE) was used to score language function, including reading comprehension, repetition, writing and fluency, in order to quantitatively describe and classify the severity of aphasia [16].
Statistical processing
We employed SPSS 26.0 and GraphPad Prism 8.0 for data processing and visualization, respectively. The count data were described by the frequency (%) and compared using Chi-square test. The measurement data were described by (mean ± sd) and compared using independent t-test (intergroup) and paired t-test (intragroup, before and after treatment). Multiple regression analysis was utilized to explore the relative risk factors of cognitive and speech functions of the patients. The significance level was set at P<0.05.
Results
Baseline characteristics of the control and study groups
There was no statistical significance in age, sex and course of aphasia between the control and study groups (P>0.05) (Table 1).
Table 1.
Baseline characteristics of the control and study groups
| Index | Control group (n=35) | Study group (n=35) | t/χ2 | P |
|---|---|---|---|---|
| Age (years old) | 40.17±9.20 | 41.17±9.37 | -0.417 | 0.678 |
| Sex (female, %) | 16 (53.33%) | 17 (56.67%) | 0.067 | 0.795 |
| Course of aphasia (months) | 3.00±0.51 | 3.01±0.47 | -0.026 | 0.979 |
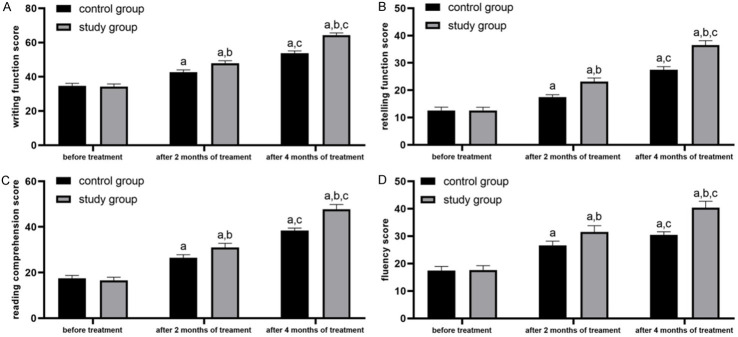
Comparison of aphasia quotient
Before treatment, there was no distinction in aphasia quotients between the two groups (P>0.05). After treatment, the aphasia quotients were improved in both groups (P<0.05). After 2 and 4 months of treatment, the aphasia quotients in the study group were better than those in the control group (P<0.05) (Figure 1).
Figure 1.
Comparison of aphasia quotient. Note: a represents P<0.05 compared with the same group before treatment; b represents P<0.05 compared with the control group; c represents P<0.05 compared with the same group after 2 months of treatment.
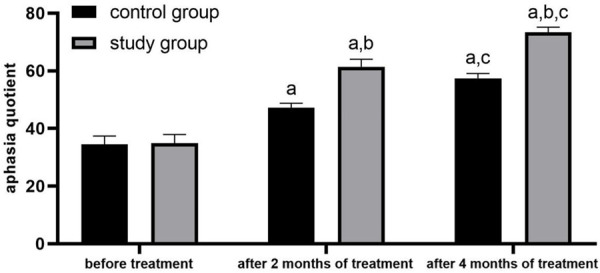
Comparison of LOTCA score
Before treatment, there was no obvious distinction in the LOTCA score between the two groups (P>0.05). After treatment, the scores were higher than those before treatment in both groups, and the score was obviously higher in the study group than that in the control group (P<0.05) (Figure 2).
Figure 2.
Comparison of LOTCA score. Note: LOTCA: Loewenstein occupational therapy cognitive assessment. a, b, c had the same meanings as those in Figure 1.
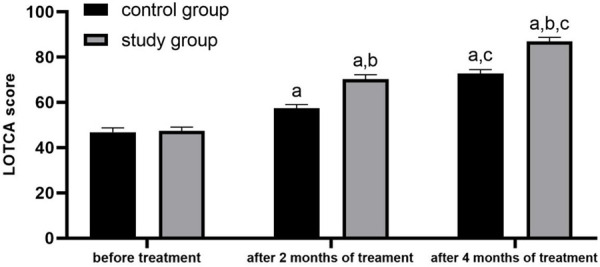
Comparison of BDAE
Before treatment, the writing function score, retelling function score, reading comprehension score, and fluency score were not obviously distinct between the control group and the study group (P>0.05). After 2 and 4 months of treatment, these four indexes were increased in both groups, and were significantly better in the study group than those in the control group (P<0.05). See Figure 3.
Figure 3.
Comparison of Boston Diagnostic Aphasia Examination (BDAE), including writing function score (A), retelling function score (B), reading comprehension score (C) and fluency score (D). Note: a, b, c had the same meanings as those in Figure 1.
Discussion
Human speech function is dominated by the dominant hemisphere of the brain, and most people will develop aphasia after damage in their dominant hemisphere [17]. The prevalence of aphasia after craniocerebral injury can be as high as 75%. Patients with aphasia have a reduced ability in understanding and expressing human communication symbols, including the expression and understanding of speech, grammar, vocabulary, language structure, as well as content and meaning [18,19]. The auditory processing disorder of aphasia can be manifested in the perception of phonemes, the understanding of vocabulary and semantics, and the understanding of syntax [20,21]. Based on the symptoms, aphasia can be divided into running aphasia, complete aphasia, thalamic aphasia, sensory aphasia, naming aphasia and mixed aphasia. At present, the clinical treatment for aphasia after brain injury mainly focuses on rehabilitation training [22], which tries to maximally restore patients’ language ability to help them return normal life and work.
Electroacupuncture and scalp acupuncture has the effect of filling the essence, supplementing blood, penetrating the vein and dredging the meridians through acupuncture points [23]. Acupuncture and moxibustion were performed on the head. The motor area, sensory area and language area were selected for treatment to directly act on the disease site and give full play to the overall treatment effect [24]. At the same time, Yamen point, Fengfu point and Baihui Point were selected. Baihui is the interactive point between foot and liver vein, which can replenish blood. Yamen is an important acupoint for aphasia, which can expel wind. Fengfu is an important acupoint for controlling wind, and it can clear customs, open orifices, and clear away heat and wind [25]. The functions of various regions of the cerebral cortex are closely related to the local blood flow. Most of the head acupoints have the effects of stimulating hypoglossal nerves, enhancing the flexibility of the tongue body and root, and correcting pronunciation [26]. Direct stimulation of head acupoints by electric needles can improve blood circulation, increase oxygen partial pressure in brain tissue, improve nutrition in tissues around lesions, accelerate metabolic recovery of brain tissue and cells, improve the supply and utilization of glucose and oxygen, change bioelectric activities in cerebral cortex and improve language function [27].
Previous studies have pointed out that stimulating patients with electroacupuncture can create collateral circulation around the cerebral infarction or cerebral hemorrhage site, attenuate cerebrovascular resistance, increase glucose and blood oxygen supply, and reduce brain tissue damage [28]. In this study, we found that the cognitive and speech functions in the study group were obviously better than those in the control group after treatment. This is because electroacupuncture on brain functional areas and language areas can improve the blood circulation of patients with pathological changes, increase the supply of cerebral blood flow and then improve aphasia [29]. Also, it can promote the cerebral cortex to produce a strong electrical tension and give full play to the overall treatment effect [30]. Some studies have shown that electroacupuncture and scalp acupuncture can regulate the secretion of neurotransmitters [31]. Specifically, serum serotonin is an important neurotransmitter in the body, which participates in the process of cognition and learning, and is related to the cognitive function of patients [32]. Brain derived neurotrophic factor can promote neuronal plasticity and survival, maintain cognitive memory function, and it shows low expression after brain injury [33]. Dopamine can cause cerebral vasospasm, lead to cerebral microcirculation disturbance, and aggravate the degree of hypoxia and ischemia of brain injury [34]. Based on these, regulating neurotransmitters may also be one of the reasons why electroacupuncture and scalp acupuncture can improve the language function and cognitive function of patients with aphasia after brain injury.
In conclusion, the combined application of electroacupuncture, scalp acupuncture and language training in patients with aphasia after craniocerebral injury is of significant value and worthy of further clinical application.
Disclosure of conflict of interest
None.
References
- 1.Jokel R. Maintenance and generalization of lexical items in primary progressive aphasia: reflections from the roundtable discussion at the 2021 clinical aphasiology conference. Am J Speech Lang Pathol. 2022:1–9. doi: 10.1044/2022_AJSLP-21-00275. [DOI] [PubMed] [Google Scholar]
- 2.Monroe P, Halaki M, Kumfor F, Ballard KJ. The effects of choral singing on communication impairments in acquired brain injury: a systematic review. Int J Lang Commun Disord. 2020;55:303–319. doi: 10.1111/1460-6984.12527. [DOI] [PubMed] [Google Scholar]
- 3.Wilmskoetter J, He X, Caciagli L, Jensen JH, Marebwa B, Davis KA, Fridriksson J, Basilakos A, Johnson LP, Rorden C, Bassett D, Bonilha L. Language recovery after brain injury: a structural network control theory study. J Neurosci. 2022;42:657–669. doi: 10.1523/JNEUROSCI.1096-21.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilbert C, Mooradian G, Citorik A, Gilmore N, Kiran S. Multi-level outcomes for young adults with acquired brain injury through a remote intensive cognitive rehabilitation approach: a pilot intervention study. Brain Inj. 2022;36:206–220. doi: 10.1080/02699052.2022.2034961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swenson TL, Roehmer C, Tran R, Plummer C. Donepezil for aphasia after severe traumatic brain injury: a clinical vignette. Am J Phys Med Rehabil. 2022;101:e54–e56. doi: 10.1097/PHM.0000000000001889. [DOI] [PubMed] [Google Scholar]
- 6.Peppel LD, Heijenbrok-Kal MH, Van Essen TA, De Ruiter GCW, Peul WC, Ribbers GM. A delphi procedure on rehabilitation outcome for patients with moderate to severe traumatic brain injury; first phase of the Neurotraumatology Quality Registry (NET-QURE) J Rehabil Med. 2022;54:jrm00249. doi: 10.2340/jrm.v53.760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.LeBlanc J, Seresova A, Laberge-Poirier A, Tabet S, Alturki AY, Feyz M, de Guise E. Cognitive-communication performance following mild traumatic brain injury: influence of sex, age, education, site of lesion and bilingualism. Int J Lang Commun Disord. 2021;56:130–144. doi: 10.1111/1460-6984.12589. [DOI] [PubMed] [Google Scholar]
- 8.Fabri TL, Stewart ML, Stevens SA. Informing pediatric rehabilitation: language-based neuropsychological profile following traumatic brain injury and stroke secondary to arteriovenous malformation. J Pediatr Rehabil Med. 2018;11:15–21. doi: 10.3233/PRM-160429. [DOI] [PubMed] [Google Scholar]
- 9.Gilmore N, Ross K, Kiran S. The intensive cognitive-communication rehabilitation program for young adults with acquired brain injury. Am J Speech Lang Pathol. 2019;28:341–358. doi: 10.1044/2018_AJSLP-17-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma C, Gan L, Wang H, Ren L, Lin Y, Zhao Y, Zhang S, Gong P, Lin X. Transcriptomic analysis of rat cerebral cortex reveals the potential mechanism of electroacupuncture opening blood brain barrier. Front Neurosci. 2022;16:834683. doi: 10.3389/fnins.2022.834683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li B, Deng S, Sang B, Zhu W, Zhuo B, Zhang M, Qin C, Lyu Y, Du Y, Meng Z. Revealing the neuroimaging mechanism of acupuncture for poststroke aphasia: a systematic review. Neural Plast. 2022;2022:5635596. doi: 10.1155/2022/5635596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang F, Ma T, Tong X, Liu Y, Cui P, Xu X, Shi J, Hu W, Lu W, Pei Z, Xu M, Li X, Xu C, Feng Y. Electroacupuncture improves metabolic and ovarian function in a rat model of polycystic ovary syndrome by decreasing white adipose tissue, increasing brown adipose tissue, and modulating the gut microbiota. Acupunct Med. 2022;40:347–359. doi: 10.1177/09645284211056663. [DOI] [PubMed] [Google Scholar]
- 13.Jiang Y, Yang Y, Xiang R, Chang E, Zhang Y, Zuo B, Zhang Q. Clinical study of post-stroke speech apraxia treated with scalp electric acupuncture under anatomic orientation and rehabilitation training. Zhongguo Zhen Jiu. 2015;35:661–664. [PubMed] [Google Scholar]
- 14.Rao LA, Roberts AC, Schafer R, Rademaker A, Blaze E, Esparza M, Salley E, Coventry C, Weintraub S, Mesulam MM, Rogalski E. The reliability of telepractice administration of the western aphasia battery-revised in persons with primary progressive aphasia. Am J Speech Lang Pathol. 2022;31:881–895. doi: 10.1044/2021_AJSLP-21-00150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen X, Liu F, Lin S, Yu L, Lin R. Effects of virtual reality rehabilitation training on cognitive function and activities of daily living of patients with poststroke cognitive impairment: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2022;103:1422–1435. doi: 10.1016/j.apmr.2022.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Fuentes B, de la Fuente-Gómez L, Sempere-Iborra C, Delgado-Fernández C, Tarifa-Rodríguez A, Alonso de Leciñana M, de Celis-Ruiz E, Gutiérrez-Zúñiga R, López-Tàppero J, Martín Alonso M, Pastor-Yborra S, Rigual R, Ruiz-Ares G, Rodríguez-Pardo J, Virués-Ortega J, Borobia AM, Blanco P, Bueno-Guerra N. DUbbing Language-therapy CINEma-based in Aphasia post-Stroke (DULCINEA): study protocol for a randomized crossover pilot trial. Trials. 2022;23:21. doi: 10.1186/s13063-021-05956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang H, Li S, Dai Y, Yu Q. Correlation between speech repetition function and the arcuate fasciculus in the dominant hemisphere detected by diffusion tensor imaging tractography in stroke patients with aphasia. Med Sci Monit. 2020;26:e928702. doi: 10.12659/MSM.928702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nakkawita SG, Duncan ES, Hartzheim DU. AAC apps for aphasia: a pilot study on the role of intuition and learning. Disabil Rehabil Assist Technol. 2021:1–11. doi: 10.1080/17483107.2021.1900932. [DOI] [PubMed] [Google Scholar]
- 19.Ramazanu S, Chisale MRO, Baby P, Wu VX, Mbakaya BC. Meta-synthesis of family communication patterns during post-stroke vascular aphasia: evidence to guide practice. Worldviews Evid Based Nurs. 2022;19:282–296. doi: 10.1111/wvn.12580. [DOI] [PubMed] [Google Scholar]
- 20.Knollman-Porter K, Brown JA, Hux K, Wallace SE, Crittenden A. Reading comprehension and processing time when people with aphasia use text-to-speech technology with personalized supports and features. Am J Speech Lang Pathol. 2022;31:342–358. doi: 10.1044/2021_AJSLP-21-00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Charalambous M, Phylactou P, Elriz T, Psychogios L, Annoni JM, Kambanaros M. Adaptation of The Scenario Test for Greek-speaking people with aphasia: a reliability and validity study. Int J Lang Commun Disord. 2022;57:865–880. doi: 10.1111/1460-6984.12727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zettin M, Bondesan C, Nada G, Varini M, Dimitri D. Transcranial direct-current stimulation and behavioral training, a promising tool for a tailor-made post-stroke aphasia rehabilitation: a review. Front Hum Neurosci. 2021;15:742136. doi: 10.3389/fnhum.2021.742136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shi S, Wang M, Liu X, Han S, Zhu P. Scalp electroacupuncture promotes angiogenesis after stroke in rats by activation of Wnt/β-catenin signal pathway. Evid Based Complement Alternat Med. 2022;2022:1649605. doi: 10.1155/2022/1649605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun TY, Ma LX, Mu JD, Zhang Z, Yu WY, Qian X, Tian Y, Zhang YD, Wang JX. Acupuncture improves the structure of spastic muscle and decreases spasticity by enhancing GABA, KCC2, and GABAAγ2 in the brainstem in rats after ischemic stroke. Neuroreport. 2022;33:399–407. doi: 10.1097/WNR.0000000000001798. [DOI] [PubMed] [Google Scholar]
- 25.Lin S, Zhu M, Chen W, Zhang Y, Lin J, Pu L, Chen S, Zhang Y, Liu X. “Acupuncture stimulation of Yamen (GV 15), Fengfu (GV 16), Baihui (GV 20), Shuigou (GV 26) and Hegu (LI 4) reduces brain microglia activation in a traumatic brain injury rat model”. J Tradit Chin Med. 2020;40:267–274. [PubMed] [Google Scholar]
- 26.Cui S, Yao S, Wu C, Yao L, Huang P, Chen Y, Tang C, Xu N. Electroacupuncture involved in motor cortex and hypoglossal neural control to improve voluntary swallowing of poststroke dysphagia mice. Neural Plast. 2020;2020:8857543. doi: 10.1155/2020/8857543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim YI, Kim SS, Sin RS, Pu YJ, Ri G, Rim KS. Study on the cerebral blood flow regulatory features of acupuncture at acupoints of the governor vessel. Med Acupunct. 2018;30:192–197. doi: 10.1089/acu.2018.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shi L, Cao HM, Li Y, Xu SX, Zhang Y, Zhang Y, Jin ZF. Electroacupuncture improves neurovascular unit reconstruction by promoting collateral circulation and angiogenesis. Neural Regen Res. 2017;12:2000–2006. doi: 10.4103/1673-5374.221156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Msigwa SS, Li Y, Cheng XL, Cao F. Combining electroacupuncture and transcranial direct current stimulation as an adjuvant therapy enhances spontaneous conversation and naming in subacute vascular aphasia: a retrospective analysis. J Integr Med. 2022;20:244–251. doi: 10.1016/j.joim.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Gu WJ, Bao CR, Xie HY, Chen B, Lin WQ, Wu Y, Wang NH. Effect of electroacupuncture invention on activities of PGC-1α/Irisin (FNDC5)/BDNF signaling in cerebral cortex, hippocampus and muscles in focal cerebral ischemic/reperfusion injury rats. Zhen Ci Yan Jiu. 2022;47:428–434. doi: 10.13702/j.1000-0607.20210495. [DOI] [PubMed] [Google Scholar]
- 31.Li Y, Yang M, Wu F, Cheng K, Chen H, Shen X, Lao L. Mechanism of electroacupuncture on inflammatory pain: neural-immune-endocrine interactions. J Tradit Chin Med. 2019;39:740–749. [PubMed] [Google Scholar]
- 32.Yuan XC, Yan XJ, Tian LX, Guo YX, Zhao YL, Baba SS, Wang YY, Liang LL, Jia H, Xu LP, Li L, Lin H, Huo FQ. 5-HT(7) receptor is involved in electroacupuncture inhibition of chronic pain in the spinal cord. Front Neurosci. 2021;15:733779. doi: 10.3389/fnins.2021.733779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pak ME, Ahn SM, Jung DH, Lee HJ, Ha KT, Shin HK, Choi BT. Electroacupuncture therapy ameliorates motor dysfunction via brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor in a mouse model of Parkinson’s disease. J Gerontol A Biol Sci Med Sci. 2020;75:712–721. doi: 10.1093/gerona/glz256. [DOI] [PubMed] [Google Scholar]
- 34.Torres-Rosas R, Yehia G, Peña G, Mishra P, del Rocio Thompson-Bonilla M, Moreno-Eutimio MA, Arriaga-Pizano LA, Isibasi A, Ulloa L. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20:291–295. doi: 10.1038/nm.3479. [DOI] [PMC free article] [PubMed] [Google Scholar]