Abstract
Background:
Fentanyl-related deaths continue to increase in the United States; however, most national studies focus on fatal overdose. More research, including data on nonfatal overdose, is needed.
Objective:
We examined trends in characteristics of fatal and nonfatal fentanyl-related poisonings (“exposures”) in the US.
Methods:
National Poison Control data were examined to estimate trends in characteristics of reported exposures between 2015 and 2021 (N = 15,391; 38.7% female). We also delineated correlates of experiencing a major adverse effect or death.
Results:
The proportion of exposures increased among all age groups between ages 13 and 39 (ps < .05) with the largest increase among those age 13–19 (a 127.8% increase). With respect to reasons for use, the proportion of cases involving fentanyl “abuse” increased by 63.8% (p < .001). The proportion involving fentanyl inhalation increased 427.6% from 5.7% to 29.9% and injection increased from 6.7% to 9.6%, a 42.3% increase (ps < .01). The proportion also increased for co-use of methamphetamine (by 669.0%), cocaine (by 374.0%), and heroin (by 159.5%). The proportion of major adverse effects increased from 15.5% to 39.6% (p < .001). In the multivariable model, “abuse”, suspected suicide attempts, and use via inhalation were risk factors for experiencing a major effect or death, and misuse, ingestion, dermal use, and co-use of methamphetamine were associated with lower risk.
Conclusion:
Poison Control data suggest that characteristics of individuals exposed to fentanyl continue to shift, with use via inhalation increasing and medical outcomes of nonfatal poisonings becoming more severe. These results complement mortality data and inform prevention and harm reduction efforts.
Keywords: Fentanyl, epidemiology, overdose, substance use, drug poisonings
Introduction
The opioid crisis in the United States (US) continues to worsen, with the number of opioid-related deaths continuing to rise. Increases in deaths have come in multiple waves. The first was overdoses related primarily to prescription opioid pills; the second was driven by heroin-related overdoses; and the third has been driven by overdoses due to use of illicitly manufactured fentanyl and its analogs (1). Deaths related to synthetic opioids other than methadone, primarily fentanyl and its analogs, have recently increased from 9,580 in 2015 to 36,359 in 2019 (2), and provisional counts from 2020 suggest that the number has continued to increase (3). Given that the opioid crisis has continued to shift, it is important for research to continue to examine trends related to fentanyl use and overdose in order to most effectively inform prevention and harm reduction efforts.
Centers for Disease Control and Prevention National Vital Statistics Systems (NVSS) mortality data have been the official source of information on opioid-related deaths in the US; however, results are typically lagged by about nine months (4). These data also tend to lack extensive information on characteristics or circumstances of overdoses, and information regarding nonfatal overdoses is not collected. In light of these limitations, alternate sources of national data could help further inform researchers and the public regarding characteristics of the ever-shifting opioid crisis which is currently driven by fentanyl use. Even though reports of fatal fentanyl exposures are exponentially higher via NVSS mortality data as these reports are believed to count all or almost all related deaths in the US (5), we believe Poison Control data can help complement this information. Specifically, Poison Control data are uploaded in almost real time and therefore, depending on data availability, they can be used as an informative source for surveillance (6). National Poison Control also collects more extensive data on circumstances of exposures (e.g., route of drug administration), and the majority of National Poison Control data are cases involving nonfatal overdoses – events that are currently lacking data at the national level. Therefore, National Poison Control data can elucidate risk factors for severity of fentanyl exposure outcomes, and determine how severity of outcomes and other circumstances of use shift over time.
In this analysis, we examine trends in characteristics of fentanyl exposures in the US using National Poison Control data and we also delineate correlates of cases experiencing major (severe) adverse effects or death. We intend for these analyses not only to complement national mortality data (e.g., NVSS) but also to inform prevention and harm reduction efforts as the opioid crisis continues to shift.
Methods
Procedure
This study is based on a collaboration through the National Institute on Drug “Abuse” National Drug Early Warning System (7) with the Researched “Abuse” Diversion and Addiction-Related Surveillance (RADARS) System. Poison Control data were obtained via the RADARS System Poison Center Program. Participating Poison Control Centers (PCCs) provided all cases involving pre-identified Micromedex codes to RADARS System staff who then reviewed select cases for accuracy. Poison Control provides treatment advice to the public and to healthcare staff treating people with suspected poisonings involving drugs, chemicals, and plants. Information about the patient and poisoning circumstances are recorded by individual PCCs as per standards set by the American Association of Poison Control Centers (AAPCC) and stored in an electronic database overseen by the National Poison Data System. RADARS System obtained data on poisonings reported to involve fentanyl (i.e., having fentanyl listed as a substance involved in the poisoning) between January 2015 and December 2021. Data were available from PCCs in all US states other than Utah prior to 2017 and North Carolina (all years).
Variables
With respect to patient characteristics, age and sex of the patient were obtained by PCC staff from the caller to the poison center, which may be the patient, health care provider, or other contact. With regard to characteristics of reported exposures, PCCs obtained information on the reason or intention for exposure, whether other drugs were co-used, the route(s) of administration, the management site, and severity of the outcome from the caller. Reasons for use included substance “abuse,” substance “misuse,” suspected suicide attempt, therapeutic error, and various other categories of intentional and unintentional exposure. Unintentional exposure does not involve intentional use of another drug (e.g., adulterated heroin) and typically refers to exposure among children. “Abuse” was defined by PCC as exposure resulting from intentional improper or incorrect use of a drug in which the patient was attempting to acquire a high, a euphoric effect, or some other psychotropic effect (8). “Misuse” was defined by PCC as intentional improper or incorrect, or otherwise nonmedical use but for reasons other than acquiring a psychotropic effect. Information on reason was collected by specialists in poison information (SPIs) from PCC contacts and reviewed by RADARS System staff. SPIs are instructed to determine whether the results were due to a purposeful action or not (intentional or unintentional). Based on coding guidelines provided by the AAPCC (9), they select the most appropriate reason for use within these categories. SPIs are instructed to record the rationale for this selection in case notes which are reviewed by RADARS System staff. In instances in which the patient is not conscious, this may impact the ability to obtain this information or create a bias due to reliance on other persons reporting.
Routes of administration included ingestion, dermal administration, injection, inhalation, and other method. It cannot be determined, however, whether inhalation referred to insufflation or smoking. Patients were able to report multiple routes. Co-drug use was also queried, and we focused on reported co-use of alcohol, cannabis, cocaine, methamphetamine, gabapentin, benzodiazepines, and prescription opioids (based on a list of 29 opioid formulations) (10). Drug use was based on self-report and toxicology test results were considered when available. All information recorded by PCC staff was reviewed for accuracy by trained RADARS System staff.
Management site was the site in which the call about the exposure to the PCC was made, and this was coded as taking place at a hospital center, on site (where the poisoning occurred), or patient referral. Finally, medical outcome was defined by PCC staff as none, mild, moderate, major, or death (6). Mild effects were defined as minimally bothersome effects, moderate effects were defined as more pronounced or prolonged effects, and major effects were defined as life-threatening or permanently disabling effects. Deaths indicate that the patient was believed to have died in relation to use of the drug. Specifically, exposure-related death was either directly determined by PCC staff involved with case management, or from death reports obtained from a medical examiner or other source (without PCC staff involved). In the latter case, an AAPCC faculty review team then judged whether deaths were in fact likely responsible or at least contributory regarding the reported exposure (6).
Analyses
First, we examined trends in characteristics of fentanyl exposures. We described the prevalence of characteristics of fentanyl exposures within each separate year and then calculated absolute and relative changes in prevalence between 2015 and 2021. We also estimated whether there werechanges in the proportion of each category of each covariate by time by examining whether there were linear, quadratic, or cubic trends using logistic regression. Next, we examined correlates of exposures resulting in a major effect or death. Covariates were fit into a multivariable generalized linear model using Poisson and log link to estimate adjusted prevalence ratios (aPRs) for each covariate. We imputed missing data for independent variables in the multivariable model. Multiple imputation was implemented via chained equations to handle missingness; predictors included all variables in the case-complete model. We imputed 10 datasets for the multivariable model and combined results using Rubin’s Rules (11).
We also conducted sensitivity tests in which we repeated all analyses excluding cases reported from Connecticut. This was done because beginning in 2018, Connecticut became the only state to mandate emergency medical service providers suspecting fentanyl overdoses to report such cases to local poison control (12). All statistics were conducted using Stata SE 17 (StataCorp, College Station, TX). This secondary analysis was exempt from review by New York University Langone Medical Center’s institutional review board.
Results
The aggregated sample was 38.7% female, and the mean age was 36.5 ± 16.7. There were 1,236 reported fentanyl-related exposures in 2015, 1,285 in 2016, 1,430 in 2017, 1,540 in 2018, 2,355 in 2019, 2,816 in 2020, and 4,729 in 2021 (aggregated N = 15,391). As such, the number of exposures increased 282.6% between 2015 and 2021. With respect to characteristics of exposures (Table 1), the proportion of exposures increased among all age groups between age 13 and 39 (ps < .05) with the largest increase among those age 13–19 (a 127.8% quadratic increase). The proportion of exposures decreased among ages greater than 39 (ps < .05). The proportion of males exposed also increased from 46.8% to 66.1%, a 41.4% cubic increase (p = .004). With respect to reasons for use, those reporting substance “abuse” increased in a cubic manner from 31.4% to 51.4% (a 63.8% increase, p < .001). Although less common, the proportion reporting withdrawal increased by 197.5%, the proportion reporting misuse increased by 26.2%, and the proportion reporting unintentional occupation exposure increased 206.8% (ps < .001). The proportion of most other reasons for use decreased. In particular, adverse reactions decreased by 81.3% between 2015 and 2021, therapeutic error decreased by 76.4%, and suspected suicide attempts decreased by 35.6% (ps < .05).
Table 1.
Trends in characteristics of fentanyl-related exposures, 2015–2021.
| 2015 % | 2016 % | 2017 % | 2018 % | 2019 % | 2020 % | 2021 % | Absolute Change % | Relative Change % | P (trend) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | ||||||||||
| ≤12 | 4.3 | 4.3 | 4.5 | 4.7 | 4.6 | 4.1 | 5.3 | 0.9 | 21.7 | 0.162a |
| 13–19 | 3.2 | 3.1 | 4.8 | 6.1 | 6.0 | 7.5 | 7.4 | 4.1 | 127.8 | 0.046b |
| 20–29 | 19.2 | 18.4 | 22.6 | 24.3 | 28.8 | 30.0 | 27.6 | 8.5 | 44.1 | <0.001c |
| 30–39 | 17.8 | 21.7 | 21.7 | 22.0 | 28.8 | 29.0 | 30.9 | 13.1 | 73.5 | <0.001a |
| 30–39 | 17.8 | 21.7 | 21.7 | 22.0 | 28.8 | 29.0 | 30.9 | 13.1 | 73.5 | <0.001a |
| 40–49 | 18.3 | 15.7 | 14.4 | 14.4 | 12.7 | 13.9 | 14.5 | −3.8 | −20.7 | <0.001b |
| 50–59 | 19.1 | 17.5 | 15.9 | 14.6 | 11.2 | 8.8 | 8.4 | −10.7 | −56.2 | <0.001a |
| 60–69 | 9.9 | 12.6 | 9.3 | 8.7 | 4.7 | 4.8 | 4.5 | −5.4 | −55.0 | <0.001c |
| 70–79 | 4.3 | 4.3 | 4.8 | 3.1 | 2.0 | 1.5 | 1.2 | −3.1 | −72.8 | 0.007b |
| ≥80 | 3.9 | 2.2 | 2.1 | 2.2 | 1.1 | 0.4 | 0.4 | −3.6 | −91.1 | 0.042b |
| Sex | ||||||||||
| Male | 46.8 | 51.0 | 53.4 | 59.7 | 63.4 | 67.2 | 66.1 | 19.4 | 41.4 | 0.004c |
| Female | 53.2 | 49.0 | 46.6 | 40.3 | 36.6 | 32.8 | 33.9 | −19.4 | −36.4 | 0.004c |
| Reason | ||||||||||
| Abuse | 31.4 | 33.4 | 37.1 | 39.4 | 48.3 | 55.0 | 51.4 | 20.0 | 63.8 | <0.001a |
| Suspected suicide attempt | 20.9 | 19.5 | 19.2 | 17.0 | 14.1 | 15.0 | 13.5 | −7.4 | −35.6 | <0.001a |
| Therapeutic error | 11.7 | 10.6 | 10.3 | 8.4 | 4.4 | 3.7 | 2.8 | −9.0 | −76.4 | 0.032c |
| Misuse | 10.4 | 10.0 | 7.7 | 9.8 | 11.1 | 9.3 | 13.1 | 2.7 | 26.2 | <0.001b |
| Adverse reaction | 9.1 | 8.6 | 5.0 | 4.4 | 3.0 | 2.2 | 1.7 | −7.4 | −81.3 | <0.001a |
| Intentional - unknown | 6.4 | 7.8 | 6.5 | 5.3 | 4.0 | 4.3 | 5.0 | −1.4 | −21.3 | <0.001c |
| Unintentional - general | 4.1 | 3.6 | 3.7 | 3.8 | 3.4 | 3.3 | 4.3 | 0.2 | 5.9 | 0.494a |
| Unknown reason | 4.4 | 3.0 | 4.3 | 3.3 | 3.1 | 3.0 | 2.6 | −1.8 | −40.0 | 0.001a |
| Unintentional - occupational | 0.7 | 0.7 | 3.1 | 6.9 | 4.9 | 1.7 | 2.2 | 1.5 | 206.8 | <0.001c |
| Withdrawal | 0.8 | 1.6 | 1.3 | 0.8 | 2.3 | 1.6 | 2.4 | 1.6 | 197.5 | <0.001a |
| Polydrug Use | ||||||||||
| Alcohol | 4.4 | 5.9 | 4.8 | 5.1 | 3.9 | 5.8 | 5.6 | 1.2 | 28.1 | 0.137a |
| Cannabis | 1.0 | 1.8 | 1.5 | 2.0 | 2.4 | 2.7 | 3.0 | 2.0 | 209.3 | <0.001a |
| Cocaine | 1.5 | 2.3 | 3.3 | 5.2 | 5.7 | 7.1 | 7.3 | 5.8 | 374.0 | 0.001b |
| Methamphetamine | 1.1 | 2.2 | 3.4 | 3.6 | 6.8 | 7.4 | 8.7 | 7.6 | 669.0 | 0.004b |
| Benzodiazepines | 18.2 | 17.1 | 13.2 | 12.7 | 9.3 | 10.9 | 9.5 | −8.7 | −47.6 | 0.019b |
| Prescription opioids | 29.4 | 28.0 | 24.4 | 15.6 | 12.1 | 13.3 | 11.8 | −17.6 | −59.9 | <0.001c |
| Heroin | 3.0 | 4.9 | 8.8 | 9.7 | 13.2 | 10.7 | 7.8 | 4.8 | 159.5 | <0.001b |
| Gabapentin | 3.5 | 3.8 | 2.9 | 2.3 | 2.1 | 1.7 | 1.8 | −1.7 | −49.4 | <0.001a |
| Route of Administration | ||||||||||
| Ingestion | 44.0 | 41.2 | 34.2 | 33.0 | 36.8 | 43.3 | 47.2 | 3.2 | 7.3 | <0.001b |
| Dermal | 40.2 | 37.1 | 32.6 | 28.6 | 15.3 | 8.8 | 5.7 | −34.5 | −85.8 | 0.013c |
| Injection | 6.7 | 8.0 | 11.2 | 11.7 | 12.2 | 14.1 | 9.6 | 2.8 | 42.3 | 0.012c |
| Inhalation | 5.7 | 8.0 | 13.2 | 15.0 | 21.3 | 27.1 | 29.9 | 24.2 | 427.6 | <0.001b |
| Other | 0.2 | 1.3 | 1.8 | 1.0 | 1.6 | 0.8 | 1.0 | 0.8 | 312.5 | 0.006c |
| Unknown | 4.5 | 6.3 | 9.8 | 11.3 | 8.7 | 14.0 | 15.5 | 11.0 | 243.0 | 0.005c |
| Management Site | ||||||||||
| Hospital center | 74.7 | 75.6 | 79.2 | 80.4 | 84.5 | 88.6 | 88.7 | 14.1 | 18.9 | 0.028c |
| On site | 14.2 | 14.0 | 14.2 | 12.3 | 10.2 | 6.2 | 6.2 | −8.0 | −56.4 | 0.041c |
| Patient referred | 11.2 | 10.4 | 6.6 | 7.3 | 5.4 | 5.2 | 5.1 | −6.1 | −54.6 | 0.025b |
| Region | ||||||||||
| Northeast | 20.6 | 19.8 | 18.8 | 18.2 | 21.8 | 26.2 | 22.5 | 1.9 | 9.4 | <0.001c |
| Midwest | 24.2 | 25.0 | 30.3 | 28.5 | 23.8 | 24.8 | 25.5 | 1.3 | 5.4 | <0.001c |
| South | 35.8 | 33.4 | 31.0 | 29.9 | 26.5 | 23.4 | 22.1 | −13.7 | −38.2 | <0.001a |
| West | 19.5 | 21.8 | 19.9 | 23.4 | 27.9 | 25.6 | 29.2 | 9.7 | 49.7 | <0.001a |
| Outcome | ||||||||||
| None | 12.4 | 12.1 | 13.5 | 13.0 | 14.6 | 9.3 | 10.6 | −1.8 | −14.2 | 0.007b |
| Mild | 27.4 | 26.5 | 21.1 | 19.7 | 16.6 | 14.4 | 16.1 | −11.3 | −41.2 | 0.007c |
| Moderate | 43.2 | 41.8 | 40.2 | 38.6 | 28.1 | 30.5 | 32.5 | −10.7 | −24.8 | <0.001c |
| Major | 15.5 | 18.2 | 23.4 | 27.0 | 39.3 | 44.4 | 39.6 | 24.1 | 155.4 | <0.001c |
| Death | 1.6 | 1.5 | 1.8 | 1.7 | 1.4 | 1.4 | 1.3 | −0.4 | −22.2 | 0.167a |
Absolute and relative change refers to changes between 2015 and 2021.
linear trend,
quadratic trend,
cubic trend
With respect to co-use of other drugs (Table 1 continued), the proportion of co-use of methamphetamine increased (from 1.1% to 8.7%—a 669.0% quadratic increase, p = .004), as did co-use of cocaine (which increased from 1.5% to 7.3%—a 374.0% quadratic increase, p < .001), cannabis (which increased from 1.0% to 3.0%—a 209.3% linear increase, p < .001), and heroin (which increased from 3.0% to 7.8%—a 159.5% quadratic increase, p < .001). Co-use of prescription opioids, however, decreased (by 59.9%), as did co-use of benzodiazepines (by 47.6%) and gabapentin (by 49.4%). Trends in co-use of heroin, cocaine, and methamphetamine are also presented in Figure 1. With regard to route of fentanyl administration, dermal use decreased in a cubic manner from 40.2% to 5.7% (an 85.8% decrease, p = .013). Inhalation increased exponentially from 5.7% to 29.9%, a 427.6% quadratic increase, p < .001). Injection use increased by 42.3% (p = .012) as did ingestion (a 7.3% quadratic increase, p < .001), and use by other or unknown methods each also more than tripled across years (ps < .01). Trends in route(s) of administration are also presented in Figure 2. On site care decreased by more than half (a 56.4% decrease, p = .041), and calls from hospital centers increased by 18.9% (p = .028). The proportion of exposures also increased in the West (by 49.7%), Northeast (by 9.4%), and Midwest (by 5.4%), and decreased in the South (by 38.2%) (ps < .001). Finally, with respect to medical outcomes, the proportion of major adverse events increased in a cubic manner from 15.5% to 39.6% (p < .001), and exposures leading to no effect, a mild effect, or moderate effect, decreased by 14,2%, 41.2%, and 24.8%, respectively (ps < .01).
Figure 1.
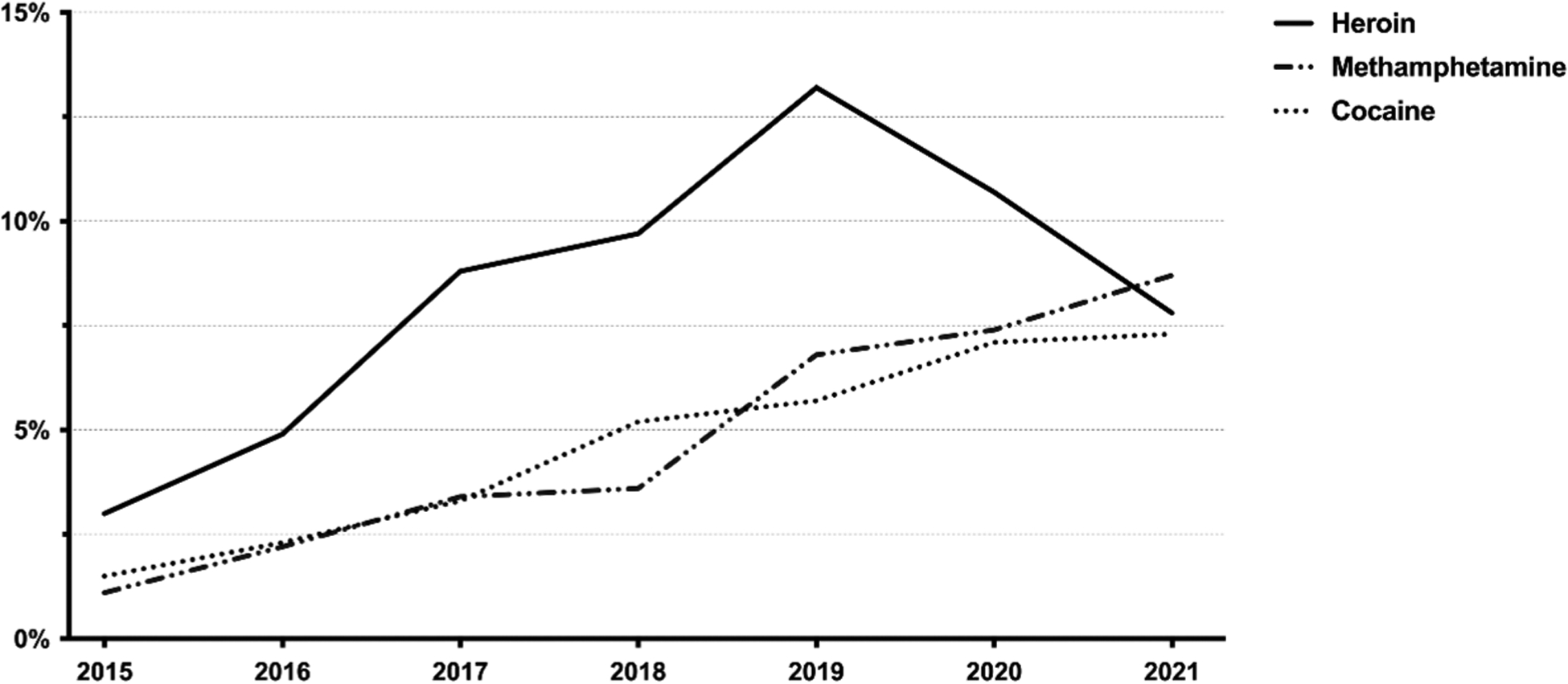
Trends in co-exposures of heroin, cocaine, and methamphetamine with fentanyl. The prevalence of co-exposure of fentanyl involving heroin increased between 2015 and 2021 from 3.0% to 7.8% (p< 0.001), as did the prevalence of co-exposure involving cocaine (increasing from 1.5% to 7.3%, p= 0.001), and methamphetamine (increasing from 1.1% to 8.7%, p= .004).
Figure 2.
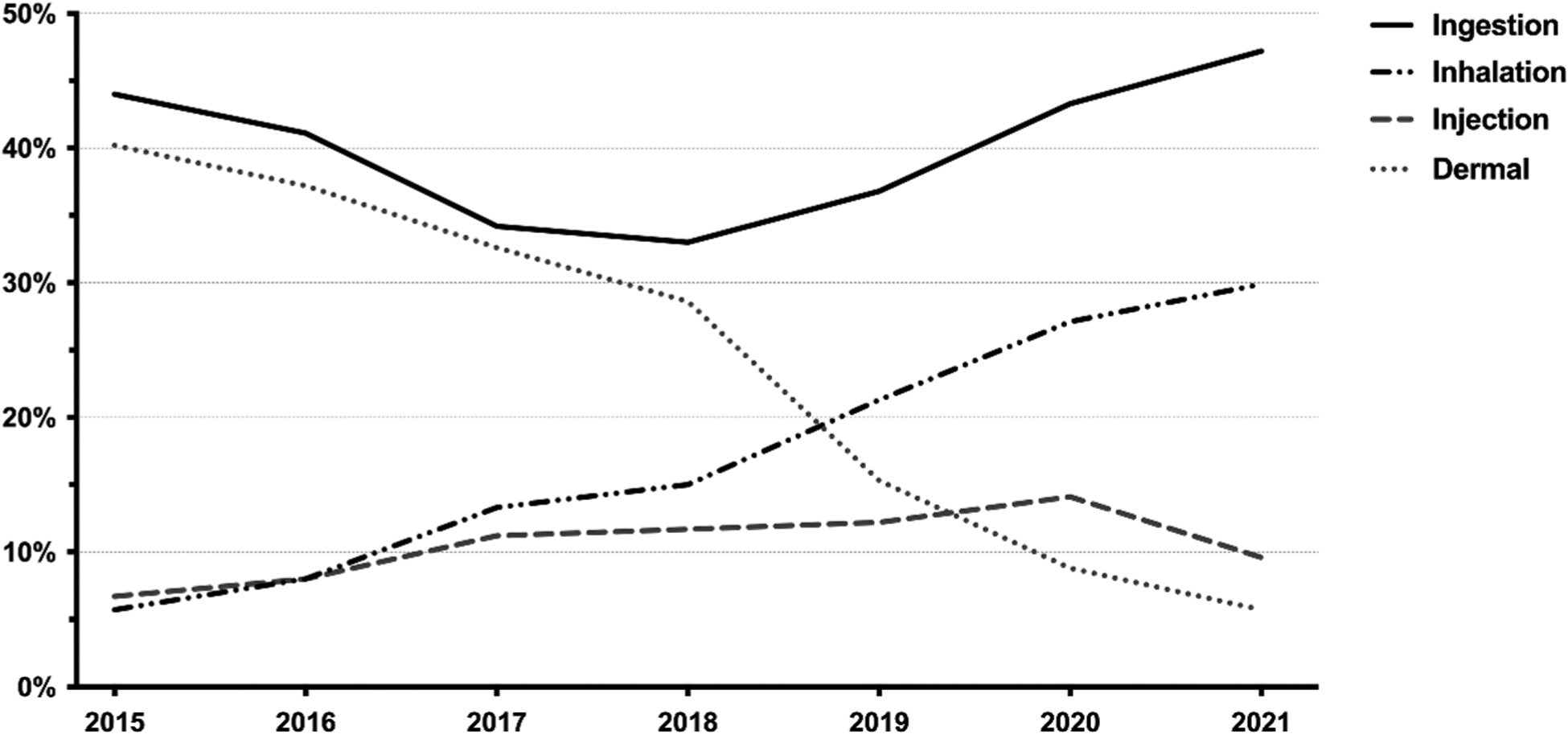
Trends in route(s) of fentanyl administration during exposure. The prevalence of ingestion increased between 2015 and 2021 between 44.0% and 47.2% (p< .001), as did the prevalence of injection (from 6.7% to 9.6%, p= .012), and inhalation (from 5.7% to 29.9%, p< .001). The prevalence of dermal route of administration, however, decreased from 40.2% to 5.7% (p= .013).
Table 2 presents correlates of an exposure resulting in a major adverse event or death (which was 35.6% of the sample). Of note, two thirds (67.0%) of major effects or death were linked to “abuse” compared to 39.6% of less severe effects being associated with “abuse”, and the prevalence of misuse was more than triple among those with less severe effects. With all else being equal, compared to those aged 20–29, those aged ≤12 (aPR = 1.49, 95% CI: 1.25–1.78), 13–19 (aPR = 1.22, 95% CI: 1.09–1.38), 50–59 (aPR = 1.19, 95% CI: 1.08–1.32), and 60–69 (aPR = 1.30, 95% CI: 1.14–1.48) were at higher risk of having a drug related major adverse outcome or death. Compared to those who reported reasons for use other than “abuse”, misuse, or suspected suicide, those who “abused” fentanyl (aPR = 1.72, 95% CI: 1.55–1.91) or who had a suspected suicide attempt (aPR = 1.21, 95% CI: 1.07–1.37) were at higher risk, and those who misused were at lower risk (aPR = 0.62, 95% CI: 0.52–0.74) of experiencing a major effect or death.
Table 2.
Correlates of major adverse effect or death.
| Full Sample % | Less Than Major Effect % | Major Effect or Death % | aPR (95% CI) | |
|---|---|---|---|---|
| Age | ||||
| ≤12 | 4.7 | 4.9 | 4.3 | 1.49 (1.25–1.78)c |
| 13–19 | 6.4 | 5.6 | 7.8 | 1.22 (1.09–1.38)b |
| 20–29 | 26.5 | 26.4 | 26.5 | 1.00 |
| 30–39 | 26.9 | 27.0 | 26.8 | 0.98 (0.91–1.07) |
| 40–49 | 14.4 | 14.5 | 14.2 | 1.02 (0.93–1.12) |
| 50–59 | 11.8 | 11.4 | 12.3 | 1.19 (1.08–1.32)b |
| 60–69 | 6.3 | 6.4 | 6.2 | 1.30 (1.14–1.48)c |
| 70–79 | 2.1 | 2.5 | 1.5 | 1.23 (0.95–1.59) |
| ≥80 | 1.0 | 1.3 | 0.4 | 0.93 (0.59–1.47) |
| Sex | ||||
| Male | 62.5 | 60.4 | 66.1 | 1.00 |
| Female | 37.5 | 39.6 | 33.9 | 1.02 (0.96–1.09) |
| Reason | ||||
| Other reason | 22.7 | 26.6 | 15.7 | 1.00 |
| Abuse | 49.3 | 39.6 | 67.0 | 1.72 (1.55–1.91)c |
| Suspected suicide attempt | 17.7 | 20.0 | 13.6 | 1.21 (1.07–1.37)b |
| Misuse | 10.3 | 13.9 | 3.8 | 0.62 (0.52–0.74)c |
| Polydrug Use | ||||
| Alcohol | 5.6 | 6.1 | 5.8 | 1.01 (0.89–1.14) |
| Cannabis | 2.6 | 2.3 | 3.0 | 1.01 (0.86–1.20) |
| Cocaine | 6.0 | 5.0 | 8.0 | 1.02 (0.92–1.14) |
| Methamphetamine | 6.3 | 7.4 | 4.2 | 0.79 (0.68–0.90)b |
| Benzodiazepines | 12.6 | 13.9 | 10.3 | 0.97 (0.88–1.07) |
| Prescription Opioids | 16.6 | 17.9 | 14.1 | 1.04 (0.95–1.13) |
| Heroin | 9.2 | 8.4 | 10.8 | 1.01 (0.92–1.11) |
| Gabapentin | 2.5 | 3.0 | 1.7 | 0.85 (0.68–1.07) |
| Route of Administration | ||||
| Ingestion | 42.5 | 47.0 | 34.2 | 0.89 (0.81–0.99)a |
| Dermal | 14.8 | 18.9 | 7.5 | 0.70 (0.60–0.82)c |
| Inhalation | 23.4 | 19.1 | 31.1 | 1.14 (1.02–1.27)a |
| Injection | 11.3 | 9.9 | 13.7 | 1.13 (1.00–1.27) |
| Unknown | 11.8 | 8.0 | 18.7 | 1.46 (1.31–1.63)c |
| Management Site | ||||
| Hospital center | 91.8 | 90.1 | 94.9 | 1.00 |
| On site | 4.9 | 5.6 | 3.7 | 0.80 (0.68–0.94)b |
| Patient referred | 3.3 | 4.3 | 1.4 | 0.52 (0.39–0.69)c |
| Region | ||||
| South | 25.7 | 26.2 | 24.7 | 1.00 |
| Northeast | 23.3 | 17.3 | 34.2 | 1.18 (1.09–1.28)c |
| Midwest | 27.0 | 30.1 | 21.2 | 0.84 (0.78–0.92)c |
| West | 24.0 | 26.3 | 19.9 | 0.86 (0.79–0.99)c |
Bivariable tests are based on case-complete data and the multivariable model is based on imputed data. The multivariable model controlled for year. aPR = adjusted prevalence ratio; CI = confidence interval. For the multivariable model:
p < .05,
p < .01,
p < .001
With regard to polydrug use (Table 2 continued), those who co-used methamphetamine were at lower risk for experiencing a major adverse effect or death compared to those who did not (aPR = 0.79, 95% CI: 0.68–0.90). Patients who used fentanyl via ingestion (aPR = 0.89, 95% CI: 0.81–0.99) or by dermal administration (aPR = 0.70, 95% CI: 0.60–0.82) were at decreased risk and those who inhaled (aPR = 1.14, 95% CI: 1.02–1.27) were at higher risk for a major effect or death, as were those with an unknown route of administration (aPR = 1.46, 95% CI: 1.31–1.63) compared to those who did not report the specific route of administration. Compared to those treated in a hospital center, those who were treated on site (aPR = 0.80, 95% CI: 0.68–0.94) or who were referred (aPR = 0.52, 95% CI: 0.39–0.69) were at lower risk of a major adverse effect or death. Finally, compared to those who lived in the South, those who lived in the Northeast (aPR = 1.18, 95% CI: 1.09–1.28) were at increased risk, and those who lived in the Midwest (aPR = 0.84, 95% CI: 0.78–0.92) or West (aPR = 0.86, 95% CI: 0.79–0.99) were at lower risk.
Sensitivity tests which excluded cases reported in Connecticut yielded similar results for all trend tests (e.g., regarding direction and significance), but some differences were detected in trends and in the multivariable model. Specifically, trends were significant for those age ≤12, those with general unintentional exposure, and for deaths. With respect to the model, ingestion and inhalation as routes of administration only approached significance as risk factors for experiencing a major adverse effect or death and injection was significant when it was not in the model focusing on the full sample.
Discussion
In this analysis of fatal and nonfatal fentanyl-related exposures reported to PCCs in the US, we detected significant shifts in characteristics of cases between 2015 and 2021. We also determined correlates of exposures resulting in major (severe) adverse effects or death.
There were many shifts in proportion of various age groups exposed across time. Exposures among individuals in all age groups between age 13 and 39 increased in proportion over time, especially adolescents (ages 13–19). We also determined that children, adolescents, and adults ages 50–69 were at higher risk for experiencing a major effect or death, suggesting these age groups are at particularly high risk for experiencing morbidity after exposure. The finding about increased exposures among children and adolescents is relatively unique. Although previous studies of mortality related to synthetic opioids suggest that there were increases among all age groups from 2011 through 2016, with a 93.9% increase among those age 15–24, increases were larger among those aged 35–44 (123.7%) and 25–34 (100.0%) (13). As such, our findings regarding children and adolescents being at increased risk for more severe outcomes may require more focus. Also, with respect to patient characteristics, the proportion of exposures increased among males. These results corroborate mortality data which suggests that since 2013, deaths related to use of synthetic opioids have increased at a faster rate then for females (13). In fact, in 2018, the rate of males who died from synthetic opioids was 14.2 per 100,000 compared to 5.5 per 100,000 females (14). Rates have remained at least 2.5 times higher among males since 2016 (13,14).
This is among the first national investigations to examine reasons for fentanyl exposure in a nuanced manner. With respect to route(s) of administration, dermal use decreased, and injection and inhalation in particular increased. Inhalation not only increased over four-fold, but this route was a risk factor for patients experiencing a major effect or death. This is the first national report on the increase in inhalation as a route of illicit fentanyl use. These results are difficult to compare to various other studies that queried route of administration but only reported injecting behavior (15,16). In addition, a limitation of Poison Control data is that we often cannot differentiate types of use that constitute inhalation; specifically, we cannot determine whether the patients insufflated, i.e., snorted, or smoked the substance. Our results appear to add to a national cross-sectional study of fentanyl-related deaths in 2016 which found evidence for snorting and smoking the drug in 52.4% and 17.9% of cases, respectively (17). A recent study in San Francisco found that there was a shift between injecting heroin to smoking fentanyl (18). This shift appeared to be largely rooted in harm reduction behavior; e.g., avoiding injection related risks of skin and soft tissue infections. Further, injection is associated with increased risk of overdose (19–20), although in our multivariable model, injection only approached significance as a risk factor for a major adverse outcome or death. Deaths involving opioids as recorded by the State Unintentional Drug Overdose Reporting System (SUDORS) in the first half of 2019 suggest that among deaths with a reported specific route of administration, injection (28.1–34.8%) was most common, followed by ingestion (12.0–16.6%), snorting/sniffing (11.5–12.5%), and smoking (5.1%–14.7%) (21). Indeed, snorting or smoking fentanyl is less common than injecting (22–24), but these methods appear to be becoming more prevalent among those who want to avoid injection or its associated risks (25–26). As such, research needs to continue to monitor shifts in route of administration as well as real or perceived changes in risk related to route.
Many Poison Control studies that examine drug exposures combine “abuse” and misuse into a single category, but we chose not to aggregate these reasons, which resulted in a more nuanced analysis. The proportion of cases involving “abuse” increased over time and represented the majority of cases in 2021. “Abuse” was also a major risk factor for patients experiencing a major effect or death. Misuse, which implies improper use of a legitimate medication, slightly decreased over time, and was actually inversely associated with patients experiencing a major effect or death. We believe this suggests higher call volume indicating use of illicitly manufactured fentanyl as opposed to use of pharmaceutical product. These results demonstrate the complexity of reasons for use which cannot be delineated in other datasets. Also, with respect to reasons for use, suspected suicide attempts decreased, although these cases were associated with higher risk of a major effect or death, possibly due to intentional high doses. Therapeutic error and adverse reactions decreased which we believe suggests stricter or more careful medical (or patient) oversight of prescribed fentanyl in recent years.
With regard to polydrug use, the proportion of cases involving methamphetamine and cocaine increased from 669.0% and 374.0%, respectively. This corroborates literature suggesting that co-use of fentanyl with stimulants is becoming more common (21 and 27), so much that it has been suggested that co-use of fentanyl and stimulants is now the “fourth wave” of the opioid overdose crisis (28). Despite increased co-use of methamphetamine, we found that this was actually a protective factor against experiencing a major adverse effect or death. The extent to which the drugs were directly combined, used en tandem, or merely used within the same day, is unknown. Given that some people use methamphetamine in attempt to prevent or reverse effects of opioids or other depressants (29) and others use in attempt to alleviate opioid withdrawal (30), more research is needed to determine contexts of such co-use in relation to severity of overdose risk. While the proportion of patients co-using heroin increased, we found that co-use of prescription opioids decreased. This finding adds to findings from mortality data which suggests that while deaths involving both prescription opioids and synthetic opioids increased from 2013 to 2017, deaths then leveled off from 2017 to 2019 (31). This decrease (or leveling off) may be indicative of the decline of the “first wave” of the opioid crisis which was largely driven by prescription opioid use (1). Further, nationally, nonmedical prescription opioid use and misuse has also been decreasing in the US (32 and 33). Although recent studies have found increasing rates of benzodiazepine use being involved in fentanyl-related deaths (34), we found that co-use of benzodiazepines actually decreased. A recent finding of a serious rise in seizures of counterfeit pills containing fentanyl (35) highlights concern about unbeknownst co-use.
The highest proportion of exposures (in 2021) occurred in the West, which is in contrast with other studies finding that most related deaths have occurred in the Northeast (13,31 and 36). With regard to the origin of calls, the proportion of calls to Poison Control centers increased from hospital centers and the proportion of calls made “on site,” typically referring to where the poisoning occurred, decreased. This suggests that it is primarily medical staff that call PCCs regarding fentanyl exposures, not patients or their caretakers. This perhaps demonstrates that while 911 emergency services are often called to respond to fentanyl overdoses, the public rarely calls PCCs for such cases. We also found that on site cases were less likely to experience a major outcome or death, although SUDORS data from the first half of 2019 suggest that the majority of fentanyl-related deaths occur at the decedent’s home (63.5–68.1%) followed by someone else’s home (16.9–19.0%) (21). Therefore, on site calls appear to be lacking using these data so more research is needed to focus on circumstances of nonfatal overdoses that occur in homes.
The increase in poisonings found in this study highlight the rising risk environment due to illicitly manufactured fentanyl (37) and point to the need for better prevention efforts. Improved drug supply surveillance is needed to better elucidate exposure risk (37) and this could include crime lab data (38), or data from the High Intensity Drug Trafficking Areas Performance Monitoring Program (35). The goal is timely data that can serve as an early warning system. Likewise, PCC data, with potentially timelier outcome data, can complement mortality data and aid in surveillance efforts. Drug checking for fentanyl, an intimate form of drug surveillance, is being explored to reduce the risk imposed by fentanyl (39–40). Further, wider distribution of naloxone is needed for more rapid response to fentanyl related overdose. For better household coverage, the US Food and Drug Administration is working on over-the-counter status for naloxone (41).
Limitations
We do not know definitively which cases involved prescribed, unprescribed, and/or illicitly manufactured fentanyl, although misuse tends to be associated with prescribed fentanyl (42). We did not present data on form of fentanyl reportedly used as this variable was missing for 64% of cases. However, results from a sub-analysis (data not presented) do indicate that 87.7% of patients who reported dermal use used fentanyl in patch form, suggesting that the vast majority of dermal use was in fact via patches. These data rely on caller or other contact information which may or may not include the patient. Some cases may rely on secondhand reporting, though this is not likely to have changed significantly over time and unlikely to have significantly biased trend estimates. Toxicology testing was not always conducted to confirm exposure to fentanyl or its analogs. Relatedly, given that fentanyl is a common adulterant in or replacement for drugs such as heroin, fentanyl exposures were likely underreported when people were unknowingly exposed. In fact, reporting of poisonings related to fentanyl is relatively rare compared to mortality studies. This is because calls to Poison Control are dependent on a patient or medical professional calling to report the poisoning or to ask for medical advice to treat a case. As such, these data are not generalizable to all poisonings; they are however, useful in informing other national studies. Exposures are also not generalizable to use or nonfatal overdose in the population as most cases reported involve adverse effects related to exposure and reporting exposures to PCCs is only voluntary. Finally, it is possible for medical outcomes to be misclassified, but in at least three quarters of cases involving fentanyl, exposure information is obtained from medical facilities that monitor patients and PCC staff follows up on cases to obtain the most accurate information possible before closing a case (6).
Conclusion
National Poison Control data suggest that characteristics of people exposed to fentanyl continue to shift, with use via inhalation increasing and medical outcomes of nonfatal poisonings becoming more severe. We believe results can be used to help monitor fentanyl exposure, to complement mortality data, and inform prevention and harm reduction efforts.
Acknowledgements
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Numbers U01DA051126, R01DA044207, and R01DA054190. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
The work was supported by the National Institute on Drug Abuse [R01DA044207,R01DA054190,U01DA051126]
Footnotes
Disclosure statement
Dr. Palamar has consulted for Alkermes. Dr. Ciccarone reports personal fees from Celero Systems and Motley Rice LLP outside the submitted work. The authors have no other potential conflicts to declare.
References
- 1.Ciccarone D The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183–88. doi: 10.1016/j.drugpo.2019.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hedegaard H, Miniño AM, Warner M. Drug overdose deaths in the United States, 1999–2019. NCHS Data Brief. 2020. 394:1–8. [PubMed] [Google Scholar]
- 3.Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics; 2021. [Google Scholar]
- 4.Spencer MR, Ahmad F. Timeliness of death certificate data for mortality surveillance and provisional estimates. National Center for Health Statistics; 2017. [Google Scholar]
- 5.Mallama CA, Trinidad JP, Swain RS, Zhao Y, Woods C, McAninch JK. A comparison of opioid-involved fatalities captured in the national poison data system to data derived from US death certificate literal text. Pharmacoepidemiol Drug Saf. 2019;28:1377–85. doi: 10.1002/pds.4869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Brooks DE, Dibert KW, Rivers LJ, Pham NPT, Ryan ML. 2019 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th Annual Report. Clin Toxicol. 2020;58:1360–541. doi: 10.1080/15563650.2020.1834219. [DOI] [PubMed] [Google Scholar]
- 7.O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths Involving Fentanyl, Fentanyl Analogs, and U-47700 – 10 States, July-December 2016. MMWR Morb Mortal Wkly Rep. 2017. Nov 3;66 (43):1197–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cottler LB, Goldberger BA, Nixon SJ, Striley CW, Barenholtz E, Fitzgerald ND, Taylor SM, Palamar JJ. Introducing NIDA’s new national drug early warning system. Drug Alcohol Depend. 2020;217:108286. doi: 10.1016/j.drugalcdep.2020.108286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zosel A, Bartelson BB, Bailey E, Lowenstein S, Dart R. Characterization of adolescent prescription drug abuse and misuse using the researched abuse diversion and addiction-related surveillance (RADARS) system. J Am Acad Child Adolesc Psychiatry. 2013;52:196–204.e192. doi: 10.1016/j.jaac.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gummin DD, Mowry JB, Beuhler MC, Spyker DA, Bronstein AC, Rivers LJ, Pham NPT, Weber J. 2020 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 38th annual report. Clin Toxicol. 2021;59:1282–501. doi: 10.1080/15563650.2021.1989785. [DOI] [PubMed] [Google Scholar]
- 11.Eluri M, Spiller HA, Casavant MJ, Chounthirath T, Conner KA, Smith GA. Analgesic-related medication errors reported to US poison control centers. Pain Med. 2018;19:2357–70. doi: 10.1093/pm/pnx272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley & Sons; 1987. [Google Scholar]
- 13.Canning P, Doyon S, Ali S, Logan SB, Alter A, Hart K, Coler R, Kamin R, Wolf SC, Soto K, et al. Using surveillance with near–real-time alerts during a cluster of overdoses from fentanyl-contaminated crack cocaine, Connecticut, June 2019. Public Health Rep. 2021;136:18s–23s. doi: 10.1177/00333549211015662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spencer MR, Warner M, Bastian BA, Trinidad JP, Hedegaard H. Drug overdose deaths involving fentanyl, 2011–2016. Natl Vital Stat Rep. 2019;68:1–19. [PubMed] [Google Scholar]
- 15.Wilson N, Kariisa M, Seth P, Smith HT, Davis NL. Drug and opioid-involved overdose deaths - United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69:290–97. doi: 10.15585/mmwr.mm6911a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kline A, Mattern D, Cooperman N, Williams JM, Dooley-Budsock P, Foglia R, Borys S. Opioid overdose in the age of fentanyl: risk factor differences among subpopulations of overdose survivors. Int J Drug Policy. 2021;90:103051. doi: 10.1016/j.drugpo.2020.103051. [DOI] [PubMed] [Google Scholar]
- 17.Foglia R 3rd, Cooperman N, Mattern D, Borys S, Kline A. Predictors of intentional fentanyl use: market availability vs consumer demand. Int J Drug Policy. 2021;95:103403. doi: 10.1016/j.drugpo.2021.103403. [DOI] [PubMed] [Google Scholar]
- 18.Kral AH, Lambdin BH, Browne EN, Wenger LD, Bluthenthal RN, Zibbell JE, Davidson PJ. Transition from injecting opioids to smoking fentanyl in San Francisco, California. Drug Alcohol Depend 2021;227:109003. doi: 10.1016/j.drugalcdep.2021.109003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shrestha S, Stopka TJ, Hughto JMW, Case P, Palacios WR, Reilly B, Green TC. Prevalence and correlates of non-fatal overdose among people who use drugs: findings from rapid assessments in Massachusetts, 2017–2019. Harm Reduct J. 2021;18:93. doi: 10.1186/s12954-021-00538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wallace B, Kennedy MC, Kerr T, Pauly B. Factors associated with nonfatal overdose during a public health emergency. Subst Use Misuse. 2019;54:39–45. doi: 10.1080/10826084.2018.1491051. [DOI] [PubMed] [Google Scholar]
- 21.O’-Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital signs: characteristics of drug overdose deaths involving opioids and stimulants - 24 states and the district of Columbia, January-June 2019. MMWR Morb Mortal Wkly Rep. 2020;69:1189–97. doi: 10.15585/mmwr.mm6935a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKnight C, Des Jarlais DC. Being “hooked up” during a sharp increase in the availability of illicitly manufactured fentanyl: adaptations of drug using practices among people who use drugs (PWUD) in New York City. Int J Drug Policy. 2018;60:82–88. doi: 10.1016/j.drugpo.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park JN, Tomko C, Silberzahn BE, Haney K, Marshall BDL, Sherman SG. A fentanyl test strip intervention to reduce overdose risk among female sex workers who use drugs in Baltimore: results from a pilot study. Addict Behav. 2020;110:106529. doi: 10.1016/j.addbeh.2020.106529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buresh M, Genberg BL, Astemborski J, Kirk GD, Mehta SH. Recent fentanyl use among people who inject drugs: results from a rapid assessment in Baltimore, Maryland. Int J Drug Policy. 2019;74:41–46. doi: 10.1016/j.drugpo.2019.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reed MK, Roth AM, Tabb LP, Groves AK, Lankenau SE. “I probably got a minute”: perceptions of fentanyl test strip use among people who use stimulants. Int J Drug Policy. 2021;92:103147. doi: 10.1016/j.drugpo.2021.103147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carroll JJ, Marshall BDL, Rich JD, Green TC. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: a mixed methods study. Int J Drug Policy. 2017;46:136–45. doi: 10.1016/j.drugpo.2017.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gladden RM, O’-Donnell J, Mattson CL, Seth P. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine - 25 states, July-December 2017 to January-June 2018. MMWR Morb Mortal Wkly Rep. 2019;68:737–44. doi: 10.15585/mmwr.mm6834a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ciccarone D The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34:344–50. doi: 10.1097/YCO.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daniulaityte R, Silverstein SM, Getz K, Juhascik M, McElhinny M, Dudley S. Lay knowledge and practices of methamphetamine use to manage opioid-related overdose risks. Int J Drug Policy. 2022;99:103463. doi: 10.1016/j.drugpo.2021.103463. [DOI] [PubMed] [Google Scholar]
- 30.Silverstein SM, Daniulaityte R, Getz K, Zule W. “It’s crazy what meth can help you do”: lay beliefs, practices, and experiences of using methamphetamine to self-treat symptoms of opioid withdrawal. Subst Use Misuse. 2021;56:1687–96. doi: 10.1080/10826084.2021.1949612. [DOI] [PubMed] [Google Scholar]
- 31.Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–07. doi: 10.15585/mmwr.mm7006a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnston LD, Miech RA, O’-Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the future national survey results on drug use 1975–2020: overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, University of Michigan; 2021. [Google Scholar]
- 33.Center for Behavioral Health Statistics and Quality. Results from the 2019 national survey on drug use and health: detailed tables. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2020. [Google Scholar]
- 34.Liu S, O’-Donnell J, Gladden RM, McGlone L, Chowdhury F. Trends in nonfatal and fatal overdoses involving benzodiazepines - 38 states and the district of Columbia, 2019–2020. MMWR Morb Mortal Wkly Rep. 2021;70:1136–41. doi: 10.15585/mmwr.mm7034a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palamar JJ, Ciccarone D, Rutherford C, Keyes KM, Carr TH, Cottler LB. Trends in seizures of powders and pills containing illicit fentanyl in the United States, 2018 through 2021. Drug Alcohol Depend. 2022;234:109398. doi: 10.1016/j.drugalcdep.2022.109398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hedegaard H, Bastian BA, Trinidad JP, Spencer MR, Warner M. Regional differences in the drugs most frequently involved in drug overdose deaths: United States, 2017. Natl Vital Stat Rep. 2019;68:1–16. [PubMed] [Google Scholar]
- 37.Ciccarone D Fentanyl in the US heroin supply: a rapidly changing risk environment. Int J Drug Policy. 2017;46:107–11. doi: 10.1016/j.drugpo.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosenblum D, Unick J, Ciccarone D. The rapidly changing US illicit drug market and the potential for an improved early warning system: evidence from Ohio Drug Crime Labs. Drug Alcohol Depend. 2020;208:107779. doi: 10.1016/j.drugalcdep.2019.107779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palamar JJ, Salomone A, Barratt MJ. Drug checking to detect fentanyl and new psychoactive substances. Curr Opin Psychiatry. 2020;33:301–05. doi: 10.1097/YCO.0000000000000607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sherman SG, Morales KB, Park JN, McKenzie M, Marshall BDL, Green TC. Acceptability of implementing community-based drug checking services for people who use drugs in three United States cities: Baltimore, Boston and Providence. Int J Drug Policy. 2019;68:46–53. doi: 10.1016/j.drugpo.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 41.U.S. Food and Drug Administration. Statement on continued efforts to increase availability of all forms of naloxone to help reduce opioid overdose deaths. 2019.
- 42.Land ME, Wetzel M, Geller RJ, Steck AR, Grunwell JR. Adult opioid poisonings by drug, intent, and resource use from the United States national poison data system from 2005–2018. Clin Toxicol. 2021;59:142–51. doi: 10.1080/15563650.2020.1781150. [DOI] [PubMed] [Google Scholar]


