Abstract
Background:
Telehealth has been declared an accepted method of occupational therapy (OT) service delivery and has been shown to be effective. However, studies done before the outbreak of coronavirus disease (COVID-19) show that most occupational therapists didn’t use it.
Aim:
The aim of this exploratory study was to examine the perceptions of occupational therapists regarding remote delivery of service following the COVID-19 outbreak.
Material and methods:
An online survey, including 11-item five-point Likert scale, and 2 open-ended questions were distributed to occupational therapists.
Results:
Responses were received from 245 Israeli occupational therapists. The majority of the participants (60%) strongly agreed that remote delivery allows an ecological and effective intervention, while 76% strongly agreed that an ideal treatment is one that would combine telehealth with in-person intervention. Qualitative findings indicated that the most significant advantage was providing care in the natural environment and improving accessibility to the service. The most salient barriers were limitations of the therapeutic relationship and threats on clinical reasoning.
Conclusion:
The study results highlight the complexity of telehealth. Findings indicate that overall occupational therapists perceive remote care as an effective and legitimate service delivery method that cannot be used as an alternative to in-person treatment. These findings can help in developing intervention programs for remote treatment, and their implementation.
Keywords: Telerehabilitation, Israel, accessibility, COVID-19, health policy, intervention out-patient rehabilitation
Introduction
Telehealth is defined as the application of evaluative, consultative, preventative, and therapeutic services delivered through information and communication technology. 1 Telehealth commonly interchanged with other related terms (eg, telemedicine telehealth, telerehabilitation, teletherapy, telecare, telepractice, etc.) and describes the delivery of care to patients through synchronous videoconferencing, asynchronous telephone calls and store-and-forward imaging, or remote monitoring. 2 Telehealth is growing rapidly and has the potential to transform the delivery of health care for millions of people. It emerges as a viable strategy that can enable individuals with disabilities to gain access to effective services, regardless of any limitations imposed by geography and local resource capabilities. In addition it can help to overcome physical accessibility barriers and assist in cases of isolation due to extreme weather, war zone, or epidemic. 3
Over the past 2 decades, OT practice has been increasingly influenced by technological advances that have offered increasing opportunities to support telehealth. 1 A remote delivery of OT to a client who is in a different physical location than the therapist has the potential to improve functional outcomes, enhance communication and continuity of care, enhance management of chronic diseases, and promote health and wellness. 4 OT delivered remotely has proven to be highly acceptable and effective for individuals with a variety of health conditions across their life-span. 5 Efficacy had also been established in multiple studies analyzing interventions for varying populations such as children with autism, 6 adolescents with myelomeningocele, 7 adults cancer-survivors,8,9 and people with acquired brain injury.10,11
The World Federation of Occupational Therapists affirmed the efficacy of telehealth for the delivery of rehabilitation and OT services, stating its use “leads to similar or better clinical outcomes when compared to conventional in-person interventions.” 12 However, despite the encouraging declarations,13,14 and the robust research evidence that showed its effectiveness, 15 studies done before the outbreak of coronavirus disease (COVID-19) shows that most occupational therapists in Israel as well as around the world did not use it in their routine clinical practice.16,17 The slow implementation of remote delivery of service is also influenced by the lack of provider’s acceptance and clinicians’ hesitation to embrace this changing delivery model.18,19 Indeed occupational therapists reported little utilization and low self-efficacy with telehealth technology20,21 and were not ready to adopt new technological systems due to increased workload. 22 In addition, the main barriers perceived by the therapists was their inability to diagnose patients and perform an evaluation process. 23
The rapid spread of the COVID-19 overwhelmed health care systems worldwide. 24 One of the most important challenge during COVID-19 pandemic seems to be its high transmissibility, necessitations social distancing as a strong defense. 25 The requirement to stay at home for extended periods of time put a strain on the health care system. Specifically, it had a profound impact on rehabilitation services causing increasing difficulties in providing in-person rehabilitation care. The unavoidable need to communicate virtually thrust health care practitioners into the use of a telehealth service delivery model. Suddenly, telehealth was on the front lines offering patients the opportunity to get the care they needed via telecommunications.15,26
A recent study conducted at a large medical center in Israel found that 87% of clinicians (physicians, psychologists, dietitians, speech therapists, social workers, and nurses) recognized the benefit of telehealth via video consultations for patients during the COVID-19 pandemic. However only 68% of the clinicians supported continuation of the service after the pandemic. 27 After the outbreak of the epidemic, there have been several studies conducted among occupational therapists. 18 These studies found overall positive perceptions toward telehealth, whereas most respondents were satisfied and perceived telehealth to be an effective delivery model for OT services.5,28-30 The overarching aim of this study is to examine the perceptions of Israeli occupational therapists regarding remote delivery of service following the COVID-19 outbreak and to explore the perceived benefits and barriers.
Material and Methods
Procedures and participants
This online cross-sectional exploratory study used design analyzing qualitative and quantitative data. All occupational therapists who have a license from the Israeli Ministry of Health were eligible to participate. The study was approved by the ethics committee of the Faculty of Medicine at The Hebrew University of Jerusalem. The survey was anonymous and no identification data was collected. Their participation was voluntary, completion of the questionnaire was considered to be consent for participation in the survey and no incentives were offered. The survey was built using a free online survey tool (Google Forms). Snowball sampling was used to recruit Israeli occupational therapists through institutional and personal networks, mailing lists, and in closed groups related to occupational therapy on social media platforms (eg, Facebook). The web link was available for 30 days in July 2020, this timeframe corresponding to the period of time between the first and second strict lockdown periods due to COVID-19 and the beginning of the de-escalation phase in Israel. Because participants joined via social media, it is impossible to determine an accurate response rate.
The recommended sample size using a power analysis for generalizability for a population of 5000 registered occupational therapists, using a 5% margin of error with a 95% confidence level, was 234 completed surveys. 31
Instrument
For the current study we developed an online self-administered questionnaire aimed to investigate the perceptions of Israeli occupational therapists toward remote delivery treatment. The questionnaire items were chosen based on a survey used in previous research, 32 a literature review,15,33-39 and input from 4 occupational therapists experienced in telehealth.
The final version of the questionnaire was comprised of 3 sections: (1) a short demographic questionnaire whose purpose was to collect basic information regarding the participants’ gender, years of experience, age, and field of work, (2) 11 quantitative questions aiming to captured information regarding the perceptions toward different aspects of remote delivery of OT. The respondents were asked to grade their level of agreement on a 5-point Likert scale ranging from 1 (slightly agree) to 5 (strongly agree), and (3) 2 open-ended questions about the main advantages and disadvantages of remote delivery to glean more in-depth information. The open-ended questions provided the participants with the opportunity to reflect on the quantitative-response questions, and further describe thoughts, concerns, feelings, and experiences, in writing. Expected duration for completing the online survey was about 5 minutes.
Data analysis
Descriptive statistical analysis was used with frequency distributions to describe the demographic characteristics of the sample and to analyze the survey results. Percentages were calculated based on the number of respondents for each question. Internal consistency within the subscale was calculated using Cronbach’s alpha. Spearman’s rank correlation coefficient was used to assess the association between years of experience and the perceptions, each individually and average of all together, toward remote delivery of OT. P < .05 denoted the presence of a statistically significant difference.
Qualitative content analysis of the 2 open-ended questions provided more in-depth insights to the advantages and disadvantages of telehealth care. Answers to the open-ended questions were analyzed using established methods for deductive content analysis through the following steps: (1) selecting the textual unit of analysis, (2) developing a codebook of mutually exclusive categories, (3) data coding, and (4) reporting the data by category. 40 The research team compiled the responses to the open-ended questions in Excel, then used open coding to generate codes from the responses, then categories and subcategories. The research team has reached a consensus about codes, categories and subcategories through discussion. Categories that have been noted most appear first.
The questions were answered in Hebrew and direct quotes were translated into English for this report by a bilingual member of the research team.
Results
This study includes a convenience sample of 245 occupational therapists, represents approximately 4% of the occupational therapists workforce in Israel (There were 5961 registered occupational therapists in Israel in 2019). 41 Table 1 lists the characteristics of the current sample population. The participants were mostly female within a large range of years of experience. The majority of the sample work in the pediatric field, with only 9 occupational therapists working in other areas that including assistive technology and adults with ADHD.
Table 1.
Demographic characteristics of the sample (n = 245).
| Variable | M (SD), range |
|---|---|
| Age | 34.76 (8.52), 24-68 |
| Years of experience | 9.14 (8.12), 1-40 |
| n (%) | |
| Gender (% females) | 243 (99.2) |
| Fields of clinical work a | |
| 1. Pediatric | 161 (66) |
| 2. Geriatric | 34 (13.9) |
| 3. Physical | 49 (20.1) |
| 4. Mental health | 35 (14.3) |
| 5. Other | 9 (3.6) |
Multiple responses per participant were allowed.
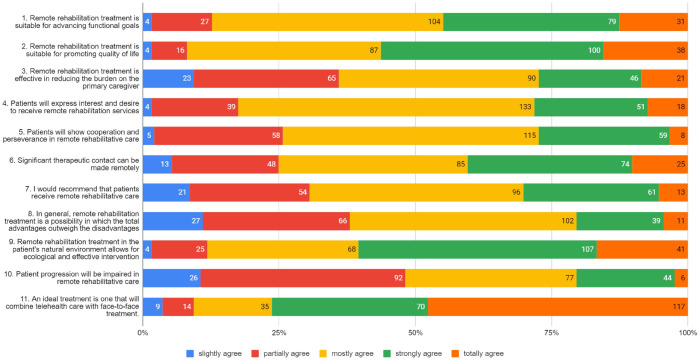
Figure 1 lists the respondents’ perceptions collected for the 11 items which were graded on a Likert scale between 1 (slightly agree) to 5 (strongly agree). Internal reliability for the quantitative questions was tested in the current study using Cronbach’s Alpha and found α = .837. The 2 items which received highest scores were: (1) an ideal treatment is one that will combine remote delivery with in-person treatment (M = 4.11, ±1.08) and (2) remote rehabilitation treatment in the patient’s natural environment allows an ecological and effective intervention (M = 3.64, ±0.94). The 2 items which received the lowest scores: (1) remote delivery of service is an option whose overall advantages outweigh its disadvantages (M = 2.76, ±0.99); and (2) patient progression will be impaired in remote rehabilitative care (M = 2.64, ±0.98).
Figure 1.
Occupational therapists perceptions toward remote delivery treatment (N = 245).
Spearman test was performed to examine the relationship between therapist perceptions toward remote delivery of service and years of experience. No significant correlation was found with any of the statements.
Content analysis
A summary of participant responses to the 2 open-ended questions are provided in Table 2. All answers regarding the advantages and disadvantages of telehealth care were divided into 2 broad categories, clinical and logistical. Subcategories are sorted in the order of their frequency. The n refer to the number of participants that mentioned the topic in their response, since multiple responses per participant were allowed, the percentages are summed above 100.
Table 2.
Perceived advantages and disadvantages of remote delivery of OT (N = 226).
| Logistical | Clinical | |
|---|---|---|
| Advantage | Improve accessibility to the service | Providing ecological care in the natural environment |
| Time and money saving (n = 35, 15%) | Treatment in the patients’ natural environment (n = 116, 51%) | |
| Accessibility for patient who cannot leave their home (n = 52, 23%) | Maintaining therapeutic contact and continuity of care (n = 31, 14%) | |
| Familiarity with the patient’s environment (n = 23, 10%) | ||
| Treatment is possible in times of emergency situations (n = 34, 15%) | Involvement of primary caregiver (n = 22, 10%) | |
| Disadvantage | Operational difficulties | Threats on clinical reasoning |
| Difficulties with technology (n = 52, 23%) | Limitations of the therapeutic relationship (n = 101, 45%) | |
| Limited ability in the use of hands-on intervention techniques (n = 91, 40%) | ||
| Inadequacy in home environment infrastructure (n = 32, 14%) | Dependence on the primary caregiver (n = 46, 20%) | |
| Inadequacy for specific populations (n = 21, 9%) |
Providing ecological care in the patients’ natural environment
Treatment in the natural environment
The main advantages that were mentioned by 51% of the respondents is that remote treatment takes place in the natural environment of the patients. Therefore, it promotes transfer of training, and leading efficient treatment in terms of functional gains. For example, one respondent shared that “. . . (telehealth is) an opportunity to transfer and generalize the treatments in a natural way.” A second respondent described the uniqueness of working in the natural environment allowing the clinician to “enter the house through the screen and work with the family and equipment that are there.”
Maintaining continuity of care
Remote delivery of OT allows the maintenance of the therapeutic relationship in circumstances where in-person contact cannot occur, enabling continuity of care toward promoting goals, preventing deterioration, and encouraging guided therapeutic practice. As one of the respondents noted, the main advantage of remote delivery of care is “the ability to maintain a sequence of treatments even in challenging situations such as corona or physical inaccessibility of treatment.” Another added: “The possibility to continue treatment when it is not possible to take place in person, preservation of condition and monitoring of changes and needs.”
Familiarity with the patient’s environment
Remote intervention was also perceived as an opportunity to get to know the patient’s human and physical environment. The familiarity with the environment can guide a more precise treatment. For example, one respondent commented: “An additional perspective on the patient and his family allows us to get to know his environment better. . ..” Another respondent stated “. . .The advantage in the pediatric field is seeing the natural environment, the human and physical environment which makes it possible to get real-time information about the contexts.” A third respondent commented: “Treatment in the natural environment makes it possible to identify strengths and weaknesses in daily functioning by observing during real-time, compared to observing in a clinic.”
Presence and involvement of the main caregiver
Remote service requires higher engagement of family members, parents, or primary caregiver in treatment. This was noted as a significant advantage by several respondents since it enables optimal utilization of the environmental resources. This collaborative work, was also seen as an opportunity to understand the needs of the primary caregiver or family. One respondent stated for example: “If a caregiver will implement and continue what is being done even later, there may be an advantage treating in the patient’s home and regular environment. Also the patient may feel safer in his natural environment.” Another participant commented: “the possibility to incorporate the caregiver in the treatment (is a significant advantage).”
Improve accessibility to the service
Accessibility for patient who cannot leave their home
Approximately 23% of the respondents noted that remote delivery of service allows patients to receive treatment they otherwise would not have been able to receive at all, due to long distance between the clinic and the patients’ residency or mobility restriction reasons which are usually permanent causes. One respondent summed up: “Accessibility; For those living in the periphery or anywhere that is not close or accessible to treatments, home remedies, people with poor immune systems. . .”
Time and money saving
Respondents indicated that another advantage is the time and money saved for both the patient and therapist while using remote delivery of service as there is no need to travel. In addition, time and money are being saved due to the possibility of simultaneous treatment for several people together using remote treatment platform. One respondent stated “(the main advantage is) cost savings of travel and time for the customer and his family. . ..” Another respondent added: “Efficiency; and savings in patient and caregiver travel time. Sometimes it is even possible to treat several patients at the same time. . ..” A third respondent defined simply “(remote care) makes it easier for the therapist and patient in terms of mobility.”
Treatment is possible in times of emergencies
The issue of accessibility to treatment during various temporary emergency situations for example COVID-19, war and extreme weather conditions was a benefit reported by 15% of the respondents. As a respondent noted: “the possibility of reaching a person even when it is difficult to leave the house because of a physical or mental reason, or when it is difficult to reach him for example, the current situation during the corona time. . ..”
Threats on clinical reasoning
A limited therapeutic relationship
Approximately 45% of the respondents strongly agreed that the unmediated connection between OT and patient cannot be replaced. They thought remote care may impact interpersonal components of the treatment and lead to a reduction of essential elements such as therapeutic relationship, trust, cooperation, perseverance, commitment, and lack of human warmth. As one respondent wrote, “In my opinion, there is no substitute to a close relationship in terms of recruiting the patient for treatment and his commitment to his personal advancement, creating a non-verbal relationship, and a more comprehensive look at the patient. All of these are more difficult to perform remotely.” Another respondent well defined the complexity of therapeutic relationship: “(a main disadvantage is) negative influence on personal contact, (and difficulty) catching nuances that cannot be seen through a screen.”
Limited ability in the use of hands-on intervention techniques
Over 40% of the respondents, stated the main disadvantage of remote delivery of OT is the absence of physical touch and the limitation on the use of treatment techniques that require it. Lack of physical contact may challenge tests of motor skills such as strength and range of motion and impede intervention that require direct touch such as passive activation of limbs. In addition, absence of a therapist standing close by might be problematic in terms of safety and may even endanger the patients. One respondent commented: “(While providing remote delivery of care it is) Difficult to perform assessment and treatment, passive and manual sessions in some cases, or practice functional tasks among patients with balance difficulties due to the danger of falls.”
Dependency on the primary caregiver
Some respondents (20%) noted that remote care may be perceived as burden on the primary caregiver, which is usually the parents in cases where the patient is a child. Remote intervention mostly requires their physical presence, investment of additional time, physical effort, and active collaboration beyond what is required in in-person sessions. One of the participants referred to the remote care of children who study in the special education system and honestly shared “With children being cared within the educational system, online care requires effort from the parents and often makes the treatments difficult instead of appreciated. . ..” Another respondent noted that remote care requires additional resources from the family: “The parent’s ability emotionally, technologically and financially is critical in the process.”
Inadequacy for specific populations
A smaller percentage of respondents (9%) noted that the main disadvantage is the inadequacy of remote OT for certain populations. For example, elderly population or people with cognitive decline might have difficulty operating the technology independently, or people with significant visual impairment or hearing loss, who will have a hard time seeing or hearing the OT through the screen, are less suitable for remote care. One respondent noted: “(remote delivery of service is) not suitable for everyone and very much depends on the physical and cognitive state of the patient. It is less suitable for cognitive therapy or for younger children.” Another respondent added: “It is less appropriate for someone with significant sensory impairment (hearing and vision).”
Logistical difficulties
Difficulties with technology
About 23% of the respondents commented that various technological problems are the biggest drawback of remote delivery. These divided to 2 main issues: First, some patients are inexperienced and have limited knowledge in operation. The second, the technological means, some of which are complicated, are not suitable for people with disabilities and require equipment and internet infrastructure that does not always exist. One of the respondents summed it up: “(Remote delivery sometimes leads to) Technological difficulties with technological products or of the patient ability to get along with the technology.”
Inadequacy in home environment infrastructure
The physical and human environment at home are often different from the existing conditions at the clinic, which therapists control to a greater extent. Several respondents (14%) indicated that the natural home environment leads to various challenges beyond technology, such as missing or unsuitable equipment, lack of infrastructure and noise. In addition there might be poor conditions in the physical environment such as small and crowded houses, lack of privacy, and other people around. One respondent noted: “The patient’s environment doesn’t always allow treatment. For example, there might be noise and different distractions.”
Discussion
This exploratory study investigated the perceptions of 245 occupational therapists regarding specific elements related to the remote delivery of service during the COVID-19 outbreak in Israel. Collectively, the responses to the survey questions indicate a subjective positive attitude toward remote delivery care. However, participants identified several benefits and barriers. The results of this survey have a number of implications for the implementation of remote OT practice initiative since therapists’ perceptions will have a significant effect after the epidemic is over too.30,42 In addition, these findings add to existing research by identifying aspects of telehealth services that need to be considered when evaluating whether telehealth is an appropriate form of service delivery, as well as identifying aspects that may need to be adapted in order to increase feasibility and effectiveness of telehealth services.
A majority of participants in this survey, in line with previous studies, perceived remote delivery of care as a suitable method for promoting functional goals (M = 3.43 ± 0.91) and quality of life (M = 3.68 ± 0.88), leading to greater independence.4,43,44 However, the item that offers an ideal treatment is a combination of remote care with in-person treatment that was rated highest (M = 4.11 ± 1.08) while the item stated that remote rehabilitation treatment is a possibility in which the total advantages outweigh the disadvantages, was rated lowest (M = 2.76 ± 0.99) on the Likert scale.
Therapeutic techniques that require touch cannot be used without modifications in remote service and was reported by respondents as one of its limitations. This is in line with a previous study, that reported that even if it is possible to compensate on some hands-on activities that cannot be done, participants value being in the clinic. 45 However, the ecological aspect of the intervention was rated second to highest (M = 3.64 ± 0.93) on the Likert scale and been noted by many of the respondents as the main advantage in the open-ended question. The participants in the current study highlighted the benefit of intervention that meet the clients beyond the simulated clinic setting in his/her “real life,” and specifically at home. These findings are in line with a previous study 46 that aimed to explore what occupational therapists perceive to be the values of OT. They found that one of the values perceived by occupational therapists is the ecological approach considering their clients’ environments and allowing interventions in the client’s natural milieu. It reflects the ultimate goal of OT to apply an intervention to promote life roles, routines, and occupational functioning in natural contexts and take into account the dynamic clients’ environments, and the bidirectional influences that exists between individuals and their environment. 47
The therapeutic relationship has emerged as a complex issue. On the one hand the participants in the current survey were concerned that remote delivery of care threatens the ability to create and maintain a therapeutic relationship. This is in line with previous reports that found health care providers considered telehealth to be a barrier in developing and maintaining a therapeutic relationship. Including difficulties with the therapists’ verbal and nonverbal communication abilities.45,48,49 Moreover, occupational therapists are concerned about the potential negative impact of remote care on the therapeutic relationship.50,51 On the other hand, most occupational therapists agreed that it is possible to develop a therapeutic contact remotely, and the Likert scale question on this issue was rated fairly high (M = 3.2 ± 1.04). This result supports a recent study which found that developing and maintaining a therapeutic relationship is feasible also in a remote mode of delivery. 8
Mixed results were also obtained regarding the influence of remote delivery of service on the primary caregiver. On average, the participants did not view remote delivery as a way to reduce the burden on the primary caregiver and this item was rated second to lowest. Moreover, burden on the parents or primary caregiver, was noted by several participants as a main disadvantage. These findings suggest that remote programs must be carefully developed to avoid increasing caregiver burden. 52 However, the necessary presence of primary caregiver, or family member, during remote sessions was perceived by some of the respondents’ as a main advantage too. The presence requirement enables collaborative working, increased motivation, and better opportunity to understand the needs of the primary caregiver and the family. Indeed, previous studies have demonstrated the potential of remote delivery of services to decrease caregiver burden, depression, stress and anxiety and increase caregivers perceived self-efficacy for caregiving skills, and social support among primary caregivers of dementia patients.53-55 These findings show that when the treatment focuses on the primary caregiver, or alternatively provides dedicated information, it can alleviate the burden placed on his shoulders. Our conclusion joins the call to consider the impact of the intervention on caregivers, in order to reduce and not increase, the burden on them. This can be achieved by giving direct attention to them and their needs.
Additional issues to consider are technological difficulties patients and therapists have to cope with during remote delivery care. Technical issues such as internet connectivity, software availability, limited knowledge, and experience in operation were noted by respondents in this current study as main barriers of telehealth. These findings are consistent with previous studies which had found that technological difficulties cause frustration among patients and providers, and constitute a disadvantage of remote rehabilitation.5,11,45 Remote delivery service should take the technology into account and make efforts to make it accessible to all. Moreover, training on how to use videoconferencing and other technology to deliver effective rehabilitation interventions should integrate curriculum for all health providers. 56
One might hypothesize that younger people including younger therapists are highly knowledgeable in technology and therefore feel more convenient with using technology as a means for their clinical practice.57,58 Surprisingly, no correlations were found between years of experience, and perceptions toward telehealth. The results of this current study suggest that the perceptions toward telehealth are not related to experience, but depend on the specific individual and targeted trainings he has undergone. 59 Therefore, the assumption which our results doubt, that young clinicians are technologically capable, and therefore hold positive attitudes toward telehealth compared to older clinicians, still needs empirical evidence. 60
Telehealth has been gaining traction as a service delivery method across healthcare professions worldwide and COVID-19 rapidly expanded the exposure of occupational therapists to remote delivery of care. This exploratory study results highlight the complexity of telehealth, although findings indicate that, overall, occupational therapists perceive remote care as an effective and legitimate service delivery method. The results point out significant benefits for both therapists and patient such as improving accessibility to the service, allowing the saving of time and money, providing ecological care in the natural environment and maintaining therapeutic contact and continuity of care. Nevertheless respondents noted several barriers, such as difficulties with technology, dependence on the primary caregiver, limitations of the therapeutic relationship, and limited ability in the use of hands-on intervention techniques.
Several limitations of this study that should be addressed in future studies can be identified. Firstly, it should be taken into account that the survey examined the perceptions of occupational therapists only, without obtaining additional information which would have enhanced our understanding, such as previous experience in remote care delivery before and during the COVID-19 or the availability of established telehealth infrastructure. The use of telehealth in Israel before the COVID-19 outbreak was rare and the transition to telehealth accrued during the first lockdown was minor and disorganized based on personal initiative and equipment. Therefore it would be reasonable to hypothesize that most on the participants did not have any significant previous experience with telehealth. Secondly, although attempts were made to obtain a representative sample, the therapists who voluntarily participated in the survey through snowball sampling may have been biased toward either a positive or negative view of telehealth depending on their previous experience. Non-respondent bias may limit the generalizability of the results, as respondents with strong beliefs were more likely to participate. Moreover, the focus of the current work was on the occupational therpist’s perspective relative to telehealth integration. A fundamental pillar of evidence-based practice in health care is the patient’s values and preferences. We encourage investigators to assess the patient’s experience with telehealth to see if the improved aspects of care from the provider’s perspective reflect the patient’s experiences. In addition, the survey was adapted for occupational therapists in Israel, who speak Hebrew, and excluded the minority in Israel who do not speak Hebrew. It is recommended in the future to adapt the survey for a sample that represents a wider population worldwide, using a variety of languages.
In conclusion, these findings are in alignment with the latest position paper published by the Israeli and the American Occupational Therapy Societies, which recommends providing remote services according to the patient’s preferences and needs14,61 as an adjunct to traditional in-person contact. 30 These results reflect that, overall, therapists hold the position that in-person treatment is preferable compared to remote delivery care, and the latter should not stand on its own and should at least be integrated with in-person treatment. These results indicate that the perceptions toward remote delivery care is not a dichotomy, rather a complex issue which needs to be addressed in accordance with every patient. Given that telehealth seems to be here to stay, the perceived benefits and barriers as experienced by occupational therapists in this study may inform future training initiatives and ongoing telehealth use in occupational therapy.
Acknowledgments
Our sincere gratitude to the participants who voluntarily participated in this study. In addition we wish to express our great appreciation to Sari Gross for the linguistic editing.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: TA contributed to the study design, data collection, and initial data analysis as well as writing the first draft of the manuscript. YG was responsible for conceptualizing the project, developing the methodology, writing, supervising, and administering the project. All authors reviewed and approved the final manuscript.
Data Availability Statement: The data that support the findings of this study are available on request from the corresponding author.
ORCID iD: Yafit Gilboa  https://orcid.org/0000-0002-0734-3626
https://orcid.org/0000-0002-0734-3626
References
- 1. Cason J, Hartmann K, Richmond T. Telehealth in occupational therapy. Am J Occup Ther. 2018;72:1-18. [Google Scholar]
- 2. Mechanic OJ, Persaud Y, Kimball AB. Telehealth Systems. StatPearls Publishing. 2017. [PubMed] [Google Scholar]
- 3. Portnoy J, Waller M, Elliott T. Telemedicine in the era of COVID-19. J Allergy Clin Immunol Pract. 2020;8:1489-1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cason J. Telehealth opportunities in occupational therapy through the Affordable Care Act. Am J Occup Ther. 2012;66:131-136. [DOI] [PubMed] [Google Scholar]
- 5. Abbott-Gaffney CR, Gafni-Lachter L, Cason J, et al. Toward successful future use of telehealth in occupational therapy practice: what the COVID-19 rapid shift revealed. Work. 2022;71:385-394. [DOI] [PubMed] [Google Scholar]
- 6. Little LM, Wallisch A, Pope E, Dunn W. Acceptability and cost comparison of a telehealth intervention for families of children with autism. Infants Young Child. 2018;31:275-286. [Google Scholar]
- 7. Steinhart S, Raz-Silbiger S, Beeri M, Gilboa Y. Occupation based telerehabilitation intervention for adolescents with myelomeningocele: a pilot study. Phys Occup Ther Pediatr. 2021;41:176-191. [DOI] [PubMed] [Google Scholar]
- 8. Maeir T, Nahum M, Makranz C, et al. The feasibility of a combined model of online interventions for adults with cancer-related cognitive impairment. Br J Occup Ther. 2021;84:430-440. [Google Scholar]
- 9. Lai LL, Player H, Hite S, et al. Feasibility of remote occupational therapy services via telemedicine in a breast cancer recovery program. Am J Occup Ther. 2021;75:75022050301-75022050309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Beit Yosef A, Jacobs JM, Shames J, Schwartz I, Gilboa Y. A performance-based teleintervention for adults in the chronic stage after acquired brain injury: an exploratory pilot randomized controlled crossover study. Brain Sci. 2022;12:213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beit Yosef A, Jacobs JM, Shenkar S, et al. Activity performance, participation, and quality of life among adults in the chronic stage after acquired brain injury – the feasibility of an occupation-based telerehabilitation intervention. Front Neurol. 2019;10:1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Federation Occupational Therapists. World federation of occupational therapists’ position statement on Telehealth. Int J Telerehabil. 2014;6:37-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rortvedt D, Jacobs K. Perspectives on the use of a telehealth service-delivery model as a component of school-based occupational therapy practice: designing a user-experience. Work. 2019;62:125-131. [DOI] [PubMed] [Google Scholar]
- 14. ISOT Position Paper. Telehelth in occupational therapy (in Hebrew). 2020. [Google Scholar]
- 15. Sarsak HI. Telerehabilitation services: a successful paradigm for occupational therapy clinical services? Int J Phys Med Rehabil. 2020;5:93-98. [Google Scholar]
- 16. Ninnis K, Van Den Berg M, Lannin NA, George S, Laver K. Information and communication technology use within occupational therapy home assessments: a scoping review. Br J Occup Ther. 2019;82:141-152. [Google Scholar]
- 17. Shahrabani S, Mizrachi Y. Factors affecting compliance with use of online healthcare services among adults in Israel. Isr J Health Policy Res. 2016;5:15-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hermes SS, Rauen J, O’Brien S. Perceptions of school-based telehealth in a rural state: moving forward after COVID-19. Int J Telerehabil. 2021;13:e6370-e6370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Serwe KM. The provider’s experience of delivering an education-based wellness program via telehealth. Int J Telerehabil. 2018;10:73-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cole B, Pickard K, Stredler-Brown A. Report on the use of telehealth in early intervention in Colorado: strengths and challenges with Telehealth as a service delivery method. Int J Telerehabil. 2019;11:33-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hersch G, Kao B, Melton L, Pancheri K. Telehealth usage by occupational therapy practitioners. Am J Occup Ther. 2015;69:69115100381-69115100381. [Google Scholar]
- 22. Corey T. Perspectives of Occupational Therapy Practitioners on Benefits and Barriers on Providing Occupational Therapy Services Via Telehealth. University of St Augustine for Health Sciences; 2019. [Google Scholar]
- 23. Tyagi S, Lim DSY, Ho WHH, et al. Acceptance of tele-rehabilitation by stroke patients: perceived barriers and facilitators. Arch Phys Med Rehabil. 2018;99:2472-2477.e2. [DOI] [PubMed] [Google Scholar]
- 24. Ren L-L, Wang Y-M, Wu ZQ, et al. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin Med J. 2020;133:1015-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. WHO. COVID-19 strategy update. 2020. [Google Scholar]
- 26. Gefen N, Steinhart S, Beeri M, Weiss PL. Lessons learned during a naturalistic study of online treatment for pediatric rehabilitation. Int J Environ Res Public Health. 2021;18:6659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Barkai G, Gadot M, Amir H, Menashe M, Shvimer-Rothschild L, Zimlichman E. Patient and clinician experience with a rapidly implemented large-scale video consultation program during COVID-19. Int J Qual Health Care. 2021;33:mzaa165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dahl-Popolizio S, Carpenter H, Coronado M, Popolizio NJ, Swanson C. Telehealth for the provision of occupational therapy: reflections on experiences during the COVID-19 pandemic. Int J Telerehabil. 2020;12:77-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Delos Reyes RC, Linang TN, Magsombol HA, Nebres ME, Zoleta M. Experiences of Filipino pediatric occupational therapists in Batangas city on telehealth. World J Res Rev. 2021;12:1-5. [Google Scholar]
- 30. Hoel V, von Zweck C, Ledgerd R; World Federation of Occupational Therapists. Was a global pandemic needed to adopt the use of telehealth in occupational therapy? Work. 2021;68:13-20. [DOI] [PubMed] [Google Scholar]
- 31. Price JH, Daek JA, Murnan J, Dimmig J, Akpanudo S. Power analysis in survey research: importance and use for health educators. Am J Health Educ. 2005;36:202-209. [Google Scholar]
- 32. Beit Yosef A, Maeir T, Khalailh F, Gilboa Y. Perceived feasibility of an occupation-based telerehabilitation intervention for older adults with chronic health conditions in Israel. Hong Kong J Occup Ther. 2022;35:62-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Al Rajeh A, Steiner MC, Aldabayan Y, et al. Use, utility and methods of telehealth for patients with COPD in England and Wales: a healthcare provider survey. BMJ Open Respir Res. 2019;6:e000345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen P, Xiao L, Gou Z, Xiang L, Zhang X, Feng P. Telehealth attitudes and use among medical professionals, medical students and patients in China: a cross-sectional survey. Int J Med Inform. 2017;108:13-21. [DOI] [PubMed] [Google Scholar]
- 35. Kim E, Gellis Z, Brennan R. Perception and utilization of telehealth services among home health care agencies: a national survey. Innov Aging. 2017;1:1193. [Google Scholar]
- 36. Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25:40-44. [PubMed] [Google Scholar]
- 37. Gately ME, Trudeau SA, Moo LR. Feasibility of telehealth-delivered home safety evaluations for caregivers of clients with dementia. OTJR. 2020;40:42-49. [DOI] [PubMed] [Google Scholar]
- 38. Hung Kn G, Fong KN. Effects of telerehabilitation in occupational therapy practice: a systematic review. Hong Kong J Occup Ther. 2019;32:3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Johnston R. Caregiver Perspectives on Telehealth: A Service Delivery for Occupational Therapy. University of St Augustine for Health Sciences; 2019. [Google Scholar]
- 40. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107-115. [DOI] [PubMed] [Google Scholar]
- 41. (Israel) PMsO. Personnel Gaps in the Health Professions Physiotherapy, Speech Therapy and Occupational Therapy (in Hebrew). Prime Minister’s Office; 2021. [Google Scholar]
- 42. Connolly SL, Miller CJ, Lindsay JA, Bauer MS. A systematic review of providers’ attitudes toward telemental health via videoconferencing. Clin Psychol Sci Pract. 2020;27:e12311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tchero H, Tabue-Teguo M, Lannuzel A, Rusch E. Telerehabilitation for stroke survivors: systematic review and meta-analysis. J Med Internet Res. 2018;20:e10867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kairy D, Lehoux P, Vincent C, Visintin M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil Rehabil. 2009;31:427-447. [DOI] [PubMed] [Google Scholar]
- 45. Campbell J, Theodoros D, Russell T, Gillespie N, Hartley N. Client, provider and community referrer perceptions of telehealth for the delivery of rural paediatric allied health services. Aust J Rural Health. 2019;27:419-426. [DOI] [PubMed] [Google Scholar]
- 46. Drolet M-J, Désormeaux-Moreau M. The values of occupational therapy: perceptions of occupational therapists in Quebec. Scand J Occup Ther. 2016;23:272-285. [DOI] [PubMed] [Google Scholar]
- 47. Ikiugu MN, Ciaravino EA. Psychosocial Conceptual Practice Models in Occupational Therapy: Building Adaptive Capability. Elsevier Health Sciences; 2007. [Google Scholar]
- 48. Liu X, Sawada Y, Takizawa T, et al. Doctor-patient communication: a comparison between telemedicine consultation and face-to-face consultation. Intern Med. 2007;46:227-232. [DOI] [PubMed] [Google Scholar]
- 49. Swinton JJ, Robinson WD, Bischoff RJ. Telehealth and rural depression: physician and patient perspectives. Fam Syst Health. 2009;27:172-182. [DOI] [PubMed] [Google Scholar]
- 50. Jacobs K, Cason J, McCullough A. The process for the formulation of the international telehealth position statement for occupational therapy. Int J Telerehabil. 2015;7:21-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Laver K, Liu E, Clemson L, et al. Does telehealth delivery of a dyadic dementia care program provide a noninferior alternative to face-to-face delivery of the same program? A randomized, controlled trial. Am J Geriatr Psychiatr. 2020;28:673-682. [DOI] [PubMed] [Google Scholar]
- 52. Erler KS, Sullivan V, Mckinnon S, Inzana R. Social support as a predictor of community participation after stroke. Front Neurol. 2019;10:1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Boots LM, de Vugt ME, van Knippenberg RJ, Kempen GI, Verhey FR. A systematic review of Internet-based supportive interventions for caregivers of patients with dementia. Int J Geriatr Psychiatry. 2014;29:331-344. [DOI] [PubMed] [Google Scholar]
- 54. Parra-Vidales E, Soto-Pérez F, Perea-Bartolomé MV, Franco-Martín MA, Muñoz-Sánchez JL. Online interventions for caregivers of people with dementia: a systematic review. Actas Esp Psiquiatr. 2017;45:116-126. [PubMed] [Google Scholar]
- 55. Tyack C, Camic PM. Touchscreen interventions and the well-being of people with dementia and caregivers: a systematic review. Int Psychogeriatr. 2017;29:1261-1280. [DOI] [PubMed] [Google Scholar]
- 56. Hsu N, Monasterio E, Rolin O. Telehealth in pediatric rehabilitation. Phys Med Rehabil Clin. 2021;32:307-317. [DOI] [PubMed] [Google Scholar]
- 57. Ivy CC, Doerrer S, Naughton N, Priganc V. The impact of COVID-19 on hand therapy practice. J Hand Ther. 2021; 5:1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Naszay M, Stockinger A, Jungwirth D, Haluza D. Digital age and the public eHealth perspective: prevailing health app use among Austrian Internet users. Inform Health Soc Care. 2018;43:390-400. [DOI] [PubMed] [Google Scholar]
- 59. Aafjes-van Doorn K, Békés V, Prout TA. Grappling with our therapeutic relationship and professional self-doubt during COVID-19: will we use video therapy again? Couns Psychol Q. 2021;34:473-484. [Google Scholar]
- 60. Serrano KM, Mendes GHS, Lizarelli FL, Ganga GMD. Assessing the telemedicine acceptance for adults in Brazil. Int J Health Care Qual Assur. Published online December 24, 2020. doi: 10.1108/IJHCQA-06-2020-0098 [DOI] [PubMed] [Google Scholar]
- 61. Radley LC, Emily Rumery OTD. Ethical Telehealth practice. 2021. [Google Scholar]