Abstract
Introduction
The main cause for developing periapical lesions (PA) is the root canal infection. The mentioned causes may play a role in not controlling it but are not a “true” cause.
Objective
To determine apical status and prevalence of endodontic treated tooth using radiograph assessment in relation to quality of root canal treatment and clinical factors among Saudi adults in the Eastern province.
Patients and methods
This prospective case series study included 2161 patients who received root canal treatment (RCT) at Dammam Specialized Dental Center, Dammam Medical Complex, Ministry of Health, Saudi Arabia, between October 21, 2019 and April 22, 2020, after getting ethical approval from the Institutional Research Board (IRB). Saudi natives of either gender, age ≥ 18, with at least one fixed bridge or single dental crown evaluated on a clear, high-quality radiography image were recruited for the study. To determine the periapical state of root canal-filled teeth, the 'periapical index' (PAI) was used. All pertinent patient information was analyzed in SPSS verion-20 (IBM product, Chicago).
Results
Out of 2161 cases, a PA lesion was present in 756 (35.0%). The prevalence of periapical lesions in endodontically treated teeth was 31.2%. PA lesion was associated with molar involvement (50.8% vs. 36.6%, p = 0.001), poor RCT quality (85.2% vs. 51.0%, p = 0.001), and smoking (13.6% vs. 10.5%, p = 0.028). According to logistic regression model, female gender, molar tooth, and poor RCT quality were more likely to expose PA lesion 1.5 times, 1.8 times, and 5 times, respectively.
Conclusion
It is concluded that approximately 1/3rd of endodontically treated teeth are susceptible to the occurrence of periapical lesions in radiographic assessment, which are significantly associated with females, molars, and poor RCT quality, indicating a challenge for endodontists to improve their root canal assessment accuracy.
Keywords: Periapical lesion, Prevalence, Endodontics, Radiograph, Treatment failure
1. Introduction
1.1. Prevalence of periapical lesion
Endodontic treatment is becoming more popular in dental practice to prevent apical periodontitis, particularly in healthy and growing adults (Hamasha and Hatiwsh, 2013, Alvarez et al., 2015). This is due to the significantly higher prevalence of dental caries worldwide (Kim et al., 2012).
A recent study to determine the prevalence of root-filled teeth in the age adult population revealed that 82.5% of patients with previously endodontically treated teeth had root-filled teeth (Dydyk and Hrynyshyn, 2020). However, the quality of root canal treatment remains debatable, owing to an increase in periapical lesions in endodontically treated teeth (Burry et al., 2016, Kielbassa et al., 2017).
Prospective researches are instructive to identify the burden and pattern of diseases and associated risk in a community (Eriksen et al., 2020). The removal of micro-organisms from root canals and the placement of a root filling that totally obturates the remaining space, followed by a restoration that produces an adequate coronal seal, form the basis of root canal treatment (Meirinhos et al., 2020, Tabassum and Khan, 2016).
1.2. Relationship of PA lesion with quality of endodontically treated tooth
Several studies in a systematic review comprising of sixteen articles involving different geographical populations have constantly confirmed the detrimental causes of poor quality root canal obturation on the survival of root canal treated teeth (Jakovljevic et al., 2020). Apical periodontitis (AP) is defined as a radiolucency around the root apex or at various levels along the root surface in lateral or furcation areas depending on the portals of exit (Kim et al., 2012, Nair, 2002) and is identified as a radiolucency around the root apex or at various levels along the root surface in lateral or furcation areas depending on the portals of exit (Huumonen and Orstavik, 2002) of periapical or periradicular lesions is also higher among one-half of endodontically treated teeth (Gheorghe et al., 2019). Therefore, the persistence of AP in endodontically treated teeth after a certain period may be considered a sign of root canal treatment failure. In a systematic review comprising of 10 published studies, they couldn’t get sufficient evidence to figure out the actual cause of endodontic complications and recommended more prospective studies (Dawson et al., 2015).
1.3. Aim of study
This study was designed to determine the apical status and prevalence of endodontically treated teeth using radiograph assessment in relation to the quality of root canal treatment and clinical factors among Saudi adults in the Eastern province. It was anticipated to estimate the magnitude of root canal treatment failure and leading causes of periapical lesions would cause an increase in the burden on dental health centers due to patients’ retention.
2. Material and method
2.1. Study design and subjects selection
This prospective case series study based on 2161 patients who underwent endodontic treatment in Dammam Specialized Dental Center, Dammam Medical Complex, Ministry of Health, Saudi Arabia was conducted during the period of 6 months from 21-10-2019 to 22-04-2020. The ethical approval from the Institutional Research Board (IRB) was obtained prior to the commencement of the study. The eligible patients for the study were Saudi nationals of either gender, over 18 years of age, with all the permanent teeth having at least one fixed bridge or single dental crown, and a clear, good quality radiographic image in which the complete periapical region is clearly visible were recruited in the study by using a non-probability consecutive sampling technique. Patients with third molar teeth, implant supported fixed bridge, removable prosthetics and those of other nationalities were excluded from the study. Assuming a 49.8% prevalence of periapical lesions in root canal treated teeth (Gheorghe et al., 2019), a 5% relative precision error (α = 0.05), and a 95% confidence interval, the minimum required sample size to cover a large cluster was 1550 patients.
2.2. Radiographic evaluation of endodontically treated tooth
All of the radiographs were obtained by the same radiographer using a digital orthopantomography (OPG) unit (Veraviewpocs, J. Morita; Kyoto, Japan). The presence of patients' consent statements was assured. Further, all digital images were independently examined by two reliability-calibrated endodontists using Adobe Photoshop (Adobe; San Jose, CA, USA) on a Dell personal computer (Austin, TX, USA). A blinding technique about the patient’s details was used for radiographic evaluations. Inter-observer reliability was calculated based on a sample of 20 evaluations (5% of the whole sample) randomly by using Cohan’s kappa reliability coefficient k = 0.792, which revealed a high inter-observer reliability. For each radiograph, the following information was recorded: 1) the total number of existing teeth (excluding third molars) on the dental arches; 2) the location of the root canal-filled teeth (sextant); and 3) the presence or absence of AP. The “periapical index” (PAI), proposed by Orstavik et al. (Orstavik et al., 1986), was used to assess the periapical status of root canal-filled teeth. Based on this index, each root was classified as having one of the following: 4) Periodontitis with clearly defined radiolucent areas; and 5) Severe periodontitis with exacerbating features. The PAI uses a reference set of radiographs with corresponding line drawings and their associated scores on a photographic print or computer file (Fig. 1). It was determined that a PAI score of 1 would represent a healthy periapex, and all other PAI scores (PAI > 1) would indicate AP (Orstavik et al., 1986). Panoramic radiograph in comparison of CBCT image has high diagnostic accuracy (71.3%) for detection of endodotically treated apical periodontitis, positive predictive value (88.6%) and 93.8% specificity (Nardi et al., 2018).
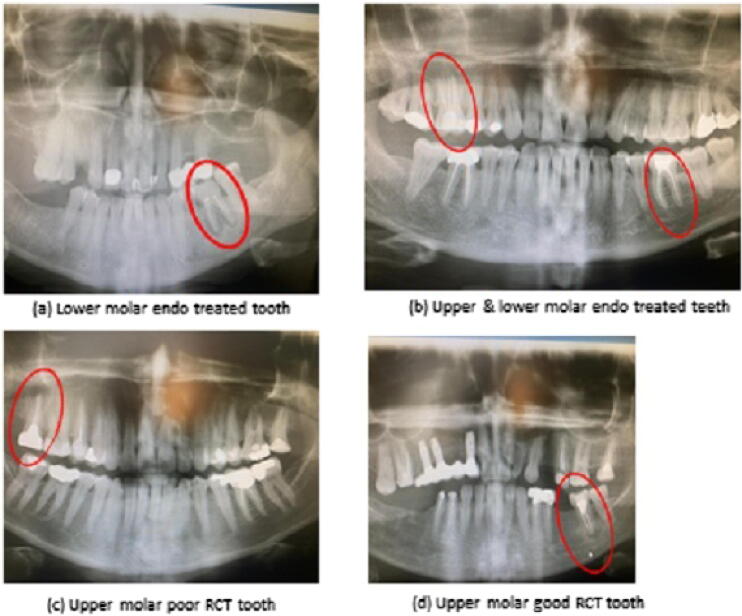
Fig. 1.
Radiographic evaluation of periapical lesion. Radiographic images contain red-colored circles to indicate particular characteristics in the figures. (a): An OPG radiographic image of lower molar tooth number 36 shows substandard endo treatment with a large periapical lesion. b): An OPG radiographic image of an upper molar tooth reveals substandard root canal treatment with a large PA lesion in tooth number 16. The lower molar OPG radiograph reveals that tooth number 36 has good root canal treatment and normal apical tissue. (c): OPG radiographic image of upper molar shows tooth number 17 with substandard root canal treatment and a large PA lesion. (d): An OPG radiographic image of the lower molar tooth reveals that tooth # 37 has received good root canal treatment and had a large PA lesion.
2.3. Data collection
Gender, age, tooth position, quality of root canal treatment, smoking status, sickle cell anemia, DMA1 + Q1 were considered independent variables and presence of periapical lesion was the dependent variable. All relevant data were recorded in a spread sheet.
2.4. Statistical analysis
Patient’s data were entered according to defined variables into SPSS version-20 (IBM product, Chicago) for statistical analysis. Mean and standard deviation were calculated to present numeric variable age. The aforementioned categorical were presented by frequencies and percentages. To compare the correlation of PA lesion with radiographic evaluation of endo treatment, Chi square test was used. Logistic regression analysis was employed by taking PA lesion as a dependent binary variable and radiographic evaluation of endo treatment as independent covariates to evaluate correlation with PA lesion. Statistical significance was considered if p-value ≤ 0.05.
3. Results
3.1. Prevalence of periapical lesion
Total 2161 radiographic images of endo treatments were reviewed. Age and gender information was missing in 200 (9.3%) cases. Out of total 1961 cases, there were 800 (40.8%) males and 1161 (59.2%) females (M: F ratio = 1: 1.5). The mean age of the patients was 41.56 ± 12.85 (ranging from 17 to 81 years). Majority of the patients were between 41 and 45 years i.e. 847 (43.2%). Out of 2161 cases, PA lesion was present in 756 (35.0%). There were total 2034 patients with root canal treatment and periapical lesion was found in 634 (31.2%), thus represents the prevalence of periapical lesion in endodontically treated teeth.
3.2. Relationship of periapical lesion with radiographic evaluation of quality of RCT
Periapical status have shown that the proportion of molar’s involvement was significantly higher in patients with periapical lesion (50.8% vs. 36.6%, p < 0.001). Although, there were majority of the patients with RCT treatment (93.4%). Patients without PA lesion had a significantly higher proportion of RCT-treated teeth than those with PA lesion (99.6% vs. 83.9%). Contrarily to this fact, there was significantly higher proportion of non RCT than RCT treated patients with PA lesion (16.1% vs. 0.4%, p < 0.001). Among 127 non RCT patients, 25 (19.7%) were smokers and 22 (17.3%) were DMA1 + Q1. However, the proportion of poor quality of RCT was significantly higher in PA lesion (85.2% vs. 51.0%, p < 0.001) as presented in Table 1.
Table 1.
Relationship of periapical lesion with the radiographic evaluation of root canal treatment.
| Evaluation of RCT | Total |
Periapical lesion |
P-value | |
|---|---|---|---|---|
| Present (n = 756) |
Absent (n = 1405) |
|||
| Tooth position | ||||
|
498 (23.0) | 149 (19.7) | 349 (24.8) | <0.001 |
|
765 (35.4) | 223 (29.5) | 542 (38.6) | |
|
898 (41.6) | 384 (50.8)* | 514 (36.6) | |
| RCT treated | ||||
|
2034 (93.2) | 634 (83.9) | 1400 (99.6) | <0.001 |
|
127 (6.8) | 122 (16.1)* | 5 (0.4) | |
| Quality of RCT | ||||
|
1256 (61.8) | 540 (85.2)* | 716 (51.0) | <0.001 |
|
778 (38.2) | 94 (14.8) | 684 (49.0) | |
The numeric expressions presented in parentheses are percentages. *Shows significant difference of proportion at 5% level of significance.
3.3. Relationship of periapical lesion with clinical causes
The relationship of smoking was found significant with PA lesion (13.6% vs. 10.5%, p = 0.028), but no correlation with sickle cell anemia (p = 0.341). There was significant proportion of DMA1 + Q1 in PA lesion patients (18% vs. 14%, p = 0.014) as detailed in Table 2.
Table 2.
Relationship of periapical lesion with patient’s clinical features.
| Clinical features | Total |
Periapical lesion |
P-value | |
|---|---|---|---|---|
| Present (n = 756) |
Absent (n = 1405) |
|||
| Smoking status | ||||
|
250 (11.6) | 103 (13.6)* | 147 (10.5) | 0.028 |
|
1911 (88.4) | 653 (86.4) | 1258 (89.5) | |
| Sickle cell anemia | ||||
|
15 (0.7) | 7 (0.9) | 8 (0.6) | 0.341 |
|
2146 (99.3) | 749 (99.1) | 1397 (99.4) | |
| DMA1 + Q1 | ||||
|
332 (15.4) | 136 (18.0)* | 196 (14.0) | 0.014 |
|
1829 (84.6) | 620 (82.0) | 1209 (86.0) | |
The numeric expressions presented in parentheses are percentages. *Shows significant difference of proportion at 5% level of significance.
Logistic regression analysis was performed by taking PA lesion as dependent binary variable and a penal of 6 covariates was evaluated for possible correlation with PA lesion. RCT or non RCT treatment variable was excluded from the model due to presence of smoking and DMA1 + Q1 effect modifiers in non RCT PA lesions. There were found three predictor of PA lesion including female gender, molar tooth and poor quality of RCT (Table 3). Adjusted odd ratio after age adjustment were also presented in Table 3.
Table 3.
Predictors of periapical lesion in relation to radiographic evaluation of Endodontic treatment.
| Factors | cOR (95% CI) | aOR (95% CI) | Sig. |
|---|---|---|---|
| Gender (Female) | 1.45 (1.15 – 1.78) | 1.28 (1.06 – 1.54) | 0.011* |
| Age (31–45 years) | 1.33 (1.14 – 1.54) | 1.05 (0.87 – 1.27) | 0.607 |
| Molar tooth | 1.79 (1.50 – 2.14) | 1.70 (1.32 – 2.17) | <0.001* |
| Poor quality of RCT | 5.49 (4.30 – 7.00) | 5.60 (4.37 – 7.17) | <0.001* |
| Active smoker | 1.35 (1.03 – 1.77) | 0.88 (0.65 – 1.20) | 0.408 |
| DMA1 + Q1 | 1.35 (1.06 – 1.71) | 0.80 (0.61 – 1.04) | 0.799 |
Shows significant at 5% level of significance. cOR: Crude Odd ratio, aOR: Adjusted Odd ratio.
4. Discussion
4.1. Salient findings of study
Primary findings of our study have shown a 31.2% prevalence of periapical lesions in endodontically treated teeth, which is a very high percentage compared to a cross-sectional study (Balto et al., 2010) done among the Saudi population (6.16%). It is, however, consistent with the prevalence of 37.99% reported in the Turkish adult population (Ozbas et al., 2011), and comparatively less than the reported prevalence of 68.13% in the Romanian adult population (Gheorghe et al., 2019). In a recent local study, the prevalence of PA (6.2%) was reported by AlNazhan S, who examined 25,028 teeth in their study (Al-Nazhan et al., 2017). Nevertheless, our study suggests validating the burden of endodontic disease in the general population and determining the actual magnitude and major reasons for endodontic treatment failure in this population.
4.2. Study outcomes in context of reported literature
We experienced that molars were the most frequently root-filled teeth among endodontically treated teeth (Eriksen et al., 2020). In a recent study (Dydyk and Hrynyshyn, 2020), similar findings were made that the commonest root-filled maxillary teeth were the first molars and second premolars, at 26.7% and 20.4%, respectively. A much lower rate of endodontic treatment was considered in the lower mandibular incisors and canines (0.7%, 0.9%, and 1.5%, respectively). Our study found the prevalence of root-filled molar teeth more likely to be 2 times (OR = 1.79: 95% CI = 1.5–2.14). Other reports have found that the mandibular first molar was the most often endodontically treated tooth, with 13.7% (Peak et al., 2001) and 3.2 percent (Balto et al., 2010) of the treated teeth. They reported that this was probably because of their early eruption in the oral cavity and the complexity of the anatomical surfaces of their crowns and occlusal surfaces (Peak et al., 2001).
In the analysis of the quality of endo treatment, we found that 778 (38.2%) were adequately treated, and 1256 (61.8%) were inadequately treated. The result is similar to Mukhaimer et al (Mukhaimer et al., 2012), where they found the majority of endodontically treated teeth (74.5%) were performed inadequately and Mirjana et al (Ilic et al., 2014) 55.9%. Our study matches with the general range (30–50%) of the most other published studies summarized by Connert T et al. in their discussion (Connert et al., 2019).
In poor quality RCTs, the frequency of PA lesion was significantly higher (85.2% vs. 51.0%, p < 0.001). is slightly higher than the value from a previously reported study in the Saudi population (22.3%) (Eriksen et al., 2020); 52%(Peak et al., 2001) and (40.0%) (Balto et al., 2010). However, 72.2% (Ilic et al., 2014) is closer to the reported study. There is sufficient evidence to prove a significant correlation between the presence of AP and poorly executed root canal fillings (Balto et al., 2010, Mukhaimer et al., 2012, Ilic et al., 2014). Of 179 endodontically treated teeth in a local study, 68 (37.99%) had periapical lesions, and the presence of severe curvatures was more significant among under-filled teeth (P < 0.001). None of the studies has shown the relationship between the presence of PA lesion and the absence of root canal treatment. We found there was a significantly higher proportion of non-RCT than RCT-treated patients with PA lesion (16.1% vs. 0.4%, p 0.001). In addition we found three predictors of PA lesion: female gender, molar tooth, and poor RCT quality.
4.3. Strengths of study
In our study, digital ortopantomographies (OPG) were used for standard assessment techniques for evaluation of apical status and quality of root canal, likewise to the reported studies (Dydyk and Hrynyshyn, 2020, Eriksen et al., 2020, Balto et al., 2010, Mukhaimer et al., 2012, Ilic et al., 2014). Though the OPG technique is considered effective for assessing root-filled teeth in even limited resource settings, an incorrect or inefficient assessment of OPG may be a misleading cause of endodontic treatment failure. Thus, our study has provided an opportunity for clinicians to enhance their accuracy of root canal assessment to reduce common measurement errors that cause endodontic treatment failure in their future practice.
4.4. Limitations of study
One of the limitations of our study was the absence of dentist’s profile, whether student, general dentist, or specialist, which may provide an overview about the skills and perfection of the clinician who performed endodontic treatment. Another limitation associated with endo treatment was the use of root filling material and its uniformity in the sampled subjects.
A limitation of our study is also the use of traditional radiographic imaging instead of cone beam computed tomography (CBCT), which may provide more promising results and an accurate magnitude of periapical status and prevalence (Pereira et al., 2020). We disregard unclear radiographic images may present increased prevalence of periapical lesion. Implant supported crowns were also excluded from the study, as in a recent study (Baruwa et al., 2022), prevalence of PA lesion in tooth supported and/or implant supported crowns was higher than non-adjacent teeth (p = 0.001), which indicates higher magnitude of overall prevalence of PA lesion.
5. Conclusion
It is concluded that approximately 1/3rd of endodontically treated teeth are susceptible to the occurrence of periapical lesions in radiographic assessment, which are significantly associated with females, molars, and poor RCT quality, indicating a challenge for endodontists to improve their root canal assessment accuracy and rule out the common mistakes that lead to endodontic treatment failure in their future practice.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Khalaf A. Al-Awasi, Email: kal-wasi@moh.gov.sa.
Ghada A. Altaroti, Email: ga-altaroti@moh.gov.sa.
Abeer Assaf Alshammari, Email: Abasalshammari@moh.gov.sa.
Tarek Ezzeldin, Email: tezzeldin@moh.gov.sa.
Intisar Ahmad Siddiqui, Email: iasiddiq@iau.edu.sa.
References
- Al-Nazhan S.A., Alsaeed S.A., Al-Attas H.A., Dohaithem A.J., Al-Serhan M.S., Al-Maflehi N.S. Prevalence of apical periodontitis and quality of root canal treatment in an adult Saudi population. Saudi Med. J. 2017;38(4):413–421. doi: 10.15537/smj.2017.4.16409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarez L., Liberman J., Abreu S., Mangarelli C., Correa M.B., Demarco F.F., Lorenzo S., Nascimento G.G. Dental caries in Uruguayan adults and elders: findings from the first Uruguayan National Oral Health Survey. Cad. SaudePublica. 2015;31:1663–1672. doi: 10.1590/0102-311X00132214. [DOI] [PubMed] [Google Scholar]
- Balto H., Al Khalifah S., Al Mugairin S., Al Deeb M., Al-Madi E. Technical quality of root fillings performed by undergraduate students in Saudi Arabia. Int. Endod. J. 2010;43:292–300. doi: 10.1111/j.1365-2591.2009.01679.x. [DOI] [PubMed] [Google Scholar]
- Baruwa A.O., Martins J.N.R., Pereira B., Meirinhos J., Ordinola-Zapata R., Souza E.M., Ginjeira A. Prevalence of periapical lesions, root canal treatments and restorations in teeth adjacent to implant-or tooth-supported crowns: A multi-centre cross-sectional study. Int. Endod. J. 2022;55:30–37. doi: 10.1111/iej.13651. [DOI] [PubMed] [Google Scholar]
- Burry J.C., Stover S., Eichmiller F., Bhagavatula P. Outcomes of Primary Endodontic Therapy Provided by Endodontic Specialists Compared with Other Providers. J. Endod. 2016;42(5):702–705. doi: 10.1016/j.joen.2016.02.008. [DOI] [PubMed] [Google Scholar]
- Connert T., Truckenmuller M., ElAyouti A., Eggmann F., Krastl G., Lost C., Weiger R. Changes in periapical status, quality of root fillings and estimated endodontic treatment need in a similar urban German population 20 years later. Clin. Oral Investig. 2019;23(3):1373–1382. doi: 10.1007/s00784-018-2566-z. [DOI] [PubMed] [Google Scholar]
- Dawson V.S., Amjad S., Fransson H. Endodontic complications in teeth with vital pulps restored with composite resins: a systematic review. Int. Endod. J. 2015;48(7):627–638. doi: 10.1111/iej.12364. [DOI] [PubMed] [Google Scholar]
- Dydyk N., Hrynyshyn O. Prevalence of root filled teeth in an adult population (lviv, ukraine) found on digital panoramic radiographs. WiadLek. 2020;73(4):691–695. [PubMed] [Google Scholar]
- Eriksen H.M., Kirkevang L.L., Petersson K. Endodontic epidemiology and treatment outcome: general considerations. Endod. Topics. 2020;2:1–9. [Google Scholar]
- Gheorghe A.G., Mercut V., Popescu S.M., Banica A.C., Ionescu M., Gheorghița L.M., Farcaș-Berechet C., Diaconu O.A., Țuculina M.J., Moraru A. Frequency of endodontic treatment and prevalence of apical periodontitis in abutment teeth – a radiological study. Romanian J. Oral Rehabilitat. 2019;11(1):11–20. [Google Scholar]
- Hamasha A.A., Hatiwsh A. Quality of life and satisfaction of patients after nonsurgical primary root canal treatment provided by undergraduate students, graduate students and endodontic specialists. IntEndod J. 2013;46(12):1131–1139. doi: 10.1111/iej.12106. [DOI] [PubMed] [Google Scholar]
- Huumonen S., Orstavik D. Radiological aspects of apical periodontitis. Endod. Topics. 2002;1:3–25. [Google Scholar]
- Ilic J., Vujaskovic M., Tihacek-Sojic L., Milic-Lemic A. Frequency and quality of root canal fillings in an adult Serbian population. SrpArhCelokLek. 2014;142(11–12):663–668. doi: 10.2298/sarh1412663i. [DOI] [PubMed] [Google Scholar]
- Jakovljevic A., Nikolic N., Jacimovic J., Pavlovic O., Milicic B., Beljic-Ivanovic K., Miletic M., Andric M., Milasin J. Prevalence of Apical Periodontitis and Conventional Nonsurgical Root Canal Treatment in General Adult Population: An Updated Systematic Review and Meta-analysis of Cross-sectional Studies Published between 2012 and 2020. J Endod. 2020;46(10):1371–1386. doi: 10.1016/j.joen.2020.07.007. [DOI] [PubMed] [Google Scholar]
- Kielbassa A.M., Frank W., Madaus T. Radiologic assessment of quality of root canal fillings and periapical status in an Austrian subpopulation – An observational study. PLoS One. 2017;12(5):e0176724. doi: 10.1371/journal.pone.0176724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.K., Baker L.A., Seirawan H., Crimmins E.M. Prevalence of oral health problems in U.S. adults, NHANES 1999–2004: exploring differences by age, education, and race/ethnicity. Spec Care Dentist. 2012;32:234–241. doi: 10.1111/j.1754-4505.2012.00280.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meirinhos J., Martins J.N.R., Pereira B., Baruwa A., Gouveia J., Quaresma S.A., Monroe A., Ginjeira A. Prevalence of apical periodontitis and its association with previous root canal treatment, root canal filling length and type of coronal restoration - a cross-sectional study. IntEndod J. 2020;53(4):573–584. doi: 10.1111/iej.13256. [DOI] [PubMed] [Google Scholar]
- Mukhaimer R., Hussein E., Orafi I. Prevalence of apical periodontitis and quality of root canal treatment in an adult Palestinian sub-population. Saudi Dent J. 2012;24(3–4):149–155. doi: 10.1016/j.sdentj.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair P.N.R. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit. Rev. Oral Biol. Med. 2002;15(348):381. doi: 10.1177/154411130401500604. [DOI] [PubMed] [Google Scholar]
- Nardi C., Calistri L., Grazzini G., Desideri I., Lorini C., Occhipinti M., Mungai F., Colagrande S. Is Panoramic Radiography an Accurate Imaging Technique for the Detection of Endodontically Treated Asymptomatic Apical Periodontitis? J. Endodont. 2018;44(10):1500–1508. doi: 10.1016/j.joen.2018.07.003. [DOI] [PubMed] [Google Scholar]
- Orstavik D., Kerekes K., Eriksen H.M. The periapical index:a scoring system for radiographic assessment of apicalperiodontitis. Endod. Dent. Traumatol. 1986;2:20–34. doi: 10.1111/j.1600-9657.1986.tb00119.x. [DOI] [PubMed] [Google Scholar]
- Ozbas H., Asci S., Aydın Y. Examination of the prevalence of periapical lesions and technical quality of endodontic treatment in a Turkish subpopulation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011;112(1):136–142. doi: 10.1016/j.tripleo.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Peak J.D., Hayes S.J., Bryant S.T., Dummer P.M. The outcome of root canal treatment. A retrospective study within the armed forces (Royal Air Force) Br. Dent. J. 2001;190:140–144. doi: 10.1038/sj.bdj.4800907. [DOI] [PubMed] [Google Scholar]
- Pereira B., Martins J.N.R., Baruwa A.O., Meirinhos J., Gouveia J., Quaresma S.A., Monroe A., Ginjeira A. Association between endodontically treated maxillary and mandibular molars with fused roots and periapical lesions: A cone-beam computed tomography cross-sectional study. J. Endod. 2020;46(6):771–777. doi: 10.1016/j.joen.2020.03.003. [DOI] [PubMed] [Google Scholar]
- Tabassum S., Khan F.R. Failure of endodontic treatment: The usual suspects. Eur. J. Dent. 2016;10(1):144–147. doi: 10.4103/1305-7456.175682. [DOI] [PMC free article] [PubMed] [Google Scholar]