Abstract
This study aimed to compare the longitudinal change in depressive symptoms among healthcare professionals in Japan who are willing to receive novel coronavirus disease (COVID-19) vaccination and those who are unwilling to receive COVID-19 vaccination. The baseline survey was conducted in October 2020 (Survey time 1: T1); respondents in T1 were invited to participate in May 2021 (Survey time 2: T2). Depressive symptoms were assessed by the Patient Health Questionnaire-9 (PHQ-9). Group comparisons of the estimated mean of PHQ-9 score at T1 and T2 were estimated by the analysis of covariance. In T1, 597 participants (response rate: 4.4%) completed all questions. In T2, 211 participants (follow up rate: 35.3%) completed all questions. The group and time interaction effect was significant (F(1, 207)=3.9, p=0.049); depressive symptoms were worse among healthcare professionals who were unwilling to receive vaccination than among those who were willing to receive vaccination. This study showed that depressive symptoms were worse among healthcare professionals who were unwilling to receive COVID-19 vaccination than those who are willing to receive COVID-19 vaccination. This suggests that it is important to take care of healthcare professionals who are unwilling to receive vaccination to prevent mental health deterioration.
Keywords: Depressive symptoms, Healthcare professionals, Vaccine hesitancy, Vaccination, COVID-19
Introduction
Recently in some countries, the governments and several medical centers have made vaccination against the novel coronavirus disease (COVID-19) mandatory for healthcare professionals, which has led to a debate on whether this practice is ethical1, 2). Healthcare professionals in medical centers may be required to receive a vaccine against COVID-19 even if they have vaccine hesitancy, or they may be at a disadvantage because they refuse to receive the vaccine and have to change their workplace3). Vaccine hesitancy is defined as delayed acceptance, reluctance, or refusal of vaccination even though vaccination services are available4). In a systematic review of nationally representative samples that consisted of 58,656 participants from 13 countries, the proportion of vaccine hesitancy against COVID-19 was reported to be 20% (range: 13–29%)5). The vaccine confidence index in Japan has been one of the lowest worldwide6). A cross-sectional survey of the Japanese population showed that factors associated with hesitancy were the presence of severe psychological distress, female sex, living alone, and lower socioeconomic status7). In Japan, vaccinations began on 17 February 2021, and the first target group was healthcare professionals. On 9 July 2021, it was reported that 6,187,797 healthcare professionals had received their first dose of a vaccine against COVID-19, and 5,259,713 had received their second dose8).
It is well-known that mental health problems have occurred among healthcare professionals responding to COVID-199–11). Mental health problems have been reported to be associated with turnover, absenteeism, and job performance among healthcare professionals12). Prevention and countermeasures of mental health problems among healthcare professionals were important to maintain the healthcare system during the COVID-19 outbreak. Some previous studies have been published on the association between vaccination intentions and mental health among healthcare professionals and community residents13‒15). A previous study among healthcare professionals in Poland suggested that depression was significantly related to the willingness to get vaccinated13). Another study among 254 vaccinated community residents in Israel showed that higher levels of vaccine hesitancy were a risk factor for depression, peritraumatic stress and anxiety14). On the other hand, a previous study of the general adult population in Germany found that anxiety and depressive symptoms had no significant association with vaccine acceptance15). Thus, not enough studies have been done on vaccination hesitancy and mental health. In addition, only cross-sectional study designs have been reported, and the causal relationship between vaccination intention and mental health has not been clarified. Furthermore, no study has investigated longitudinal changes in mental health among healthcare professionals who are willing to receive the COVID-19 vaccination and those who are unwilling to receive the COVID-19 vaccination during the COVID-19 pandemic, respectively. Therefore, it is not clear whether there is a difference in longitudinal changes in mental health between healthcare professionals who are willing to receive the COVID-19 vaccination and those who are unwilling to receive the COVID-19 vaccination. It is important to examine changes in mental health among healthcare professionals who are willing to receive the COVID-19 vaccination and those who are unwilling to receive the COVID-19 vaccination, from before the start of vaccination to when vaccination has ended.
This study aimed to compare the longitudinal change in depressive symptoms among healthcare professionals in Japan who were willing to receive the COVID-19 vaccination and those who were unwilling to receive the COVID-19 vaccination, from before the start of vaccination (October 2020) to when vaccination had mostly ended during the pandemic (June 2021).
Subjects and Methods
Participants
Disaster Medical Assistance Team (DMAT) and Disaster Psychiatric Assistance Team (DPAT) are trained healthcare professionals with the mobility to work in an acute phase of a disaster. DMAT and DPAT members (physicians, nurses, and other healthcare professionals such as pharmacists and occupational therapists) usually work at their own base hospital. At the time of need, the national or prefectural government requests a deployment to disaster base hospitals. The selected members provide rescue efforts to the affected areas or accident sites for several days and return to their regular working hospital after the rescue activity. The recruited participants in this study included DMAT and DPAT members who met the following inclusion criteria: 1) aged 18 years or older, 2) native Japanese speaker or nonnative speaker with Japanese conversational abilities, 3) physically and psychologically capable of understanding and providing consent for study participation, 4) could receive an e-mail of the written guide for this study from the DMAT office or the DPAT office.
Study Design
Healthcare professionals belonging to DMAT or DPAT were recruited for this internet-based cohort survey. The baseline survey of this study was conducted from 23 October to 20 November, 2020 (Survey time 1: T1). The respondents in T1 were invited to participate in a follow-up survey from 21 May to 18 June, 2021 (Survey time 2: T2). For DMAT members, a written guide for this study was posted to the mailing list by the DMAT office, and for DPAT members by the DPAT office. The guide contained a written explanation of the study and the URL of a web page containing a consent form for this study and a questionnaire. Participants accessed the URL, read a detailed explanation of the study and responded online to a consent form and a questionnaire.
This study was ethically approved by the research ethics committee of the Graduate School of Medicine and Faculty of Medicine at the University of Tokyo (No. 2019164NI-(1)(2)(3)(4)) and the research ethics committee of the National Hospital Organization Disaster Medical Center (No. 2019-19). This study was ethically approved to use the information of DMAT and DPAT by the Ministry of Health, Labor and Welfare of Japan. Informed consent was obtained by reading an ethical document and completing a consent form on the Web page. This study was conducted in accordance with the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement16).
Measurements
Outcome: depressive symptoms
Depressive symptoms were assessed by the Patient Health Questionnaire-9 (PHQ-9), a self-reporting questionnaire designed to evaluate depressive symptoms, rating one’s condition for the last two weeks17). PHQ-9 consists of 9 items and uses a 4-point response format ranging from 0 (not at all) to 3 (nearly every day); the total score ranges from 0 to 27. The Japanese version of PHQ-9 was translated from English into Japanese, the developer of the PHQ used back translation to confirm the accuracy18). The validity and reliability of the Japanese version have been confirmed18). We used PHQ-9 to measure depressive symptoms at T1 and T2.
Independent variables
To the best of our knowledge, there was no Japanese version of the COVID-19 vaccine hesitancy scale that it’s reliability and validity were confirmed, at the time we were preparing the survey. Therefore, items about assessment of COVID-19 vaccine hesitancy and experience of vaccination against COVID-19 were originally developed by reviewing previous studies5, 13‒15), and through discussion between healthcare professionals and researchers (HA and DN) who engaged in mental health among healthcare professionals.
The question about assessment of COVID-19 vaccine hesitancy was asked at T2: “What do you think about vaccination against the novel coronavirus infection (COVID-19)?”. The participants answered by selecting one of the following four options: “I want to be vaccinated”, “I rather want to be vaccinated”, “I rather want not to be vaccinated” and “I don’t want to be vaccinated”. Those who answered “I want to be vaccinated” and “I rather want to be vaccinated” were defined as “willing to receive COVID-19 vaccination”, while those who answered “I rather want not to be vaccinated” and “I don’t want to be vaccinated” were defined as “unwilling to receive COVID-19 vaccination”. The question about the experience of vaccination against COVID-19 was asked at T2: “Have you received at least one dose of vaccine for the novel coronavirus infection (COVID-19)?”, and was answered in a binary (yes/no).
Demographic variables of sex, age, occupation and years of occupational experience were retrieved at the T2 survey.
Statistical Analysis
We analyzed the dataset of participants who completed all questions of both self-report questionnaires at T1 and T2. Participants were divided into two categories according to their answers to COVID-19 vaccine hesitancy at T2: healthcare professionals who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination. Group comparisons were estimated of the estimated mean of PHQ-9 scores at T1 and T2 between healthcare professionals who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination by the analysis of covariance (ANCOVA). Estimated mean scores were controlled by sex and age6, 7). Statistical significance was set as a two-sided p<0.05. All analyses were conducted using SPSS version 26.0 J for Windows (SPSS, Tokyo, Japan).
Results
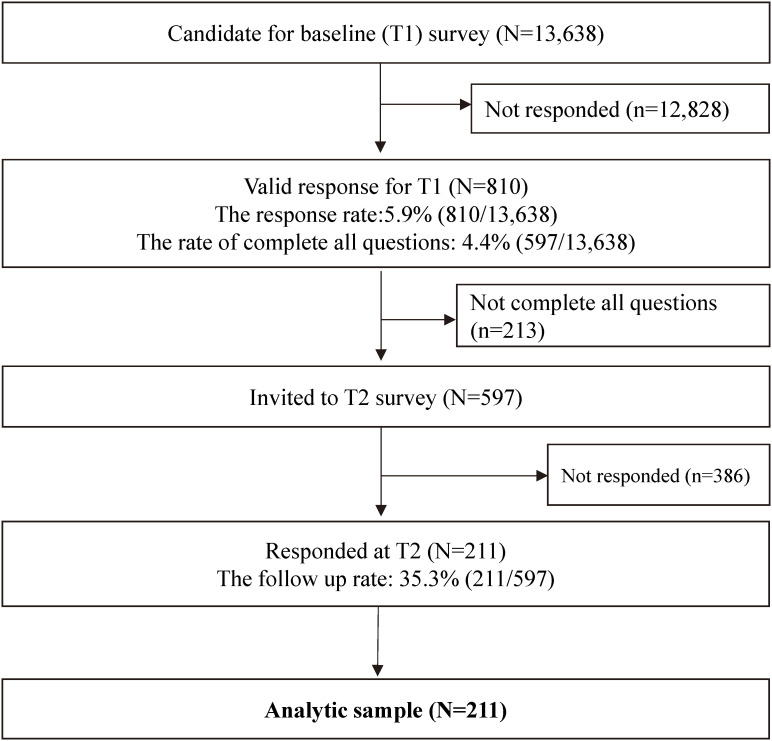
At T1, of 13,638 recruited DMAT and DPAT members, 810 (response rate: 5.9%) agreed to participate in this study, and 597 (4.4%) completed all questions. Among 597 completers of T1, 211 participants (follow-up rate: 35.3%) completed all questions at T2 (Fig. 1). The characteristics of participants are shown in Table 1. The mean age was 44.9 (SD=7.9), 58 participants (27.5%) were physicians, 71 participants (33.6%) were nurses and 82 participants (38.9%) were other healthcare professionals. 199 participants (94.3%) experienced at least one dose of COVID-19 vaccination. 174 participants (82.5%) were willing to receive the vaccine. Among 37 participants who were unwilling to receive vaccine against COVID-19, 30 participants had experienced at least one dose of COVID-19 vaccination and 7 participants did not receive a COVID-19 vaccination.
Fig. 1.
Flowchart of participant recruitment.
Table 1. Participants’ characteristics (N=211).
| n | % | mean | SD | |
| Sex | ||||
| Male | 149 | 70.6 | ||
| Female | 62 | 29.4 | ||
| Age (years) | 44.9 | 7.9 | ||
| Occupational experience (years) | 20.1 | 8.0 | ||
| Occupation | ||||
| Physicians | 58 | 27.5 | ||
| Nurses | 71 | 33.6 | ||
| Other healthcare professionals | 82 | 38.9 | ||
| Experience with at least one dose of the COVID-19 vaccination | 199 | 94.3 | ||
| Willingness to receive COVID-19 vaccine | ||||
| Willing to receive COVID-19 vaccine | 174 | 82.5 | ||
| Unwilling to receive COVID-19 vaccine | 37 | 17.5 | ||
| PHQ-9 at T1 (range: 0–27) | 3.1 | 3.9 | ||
| PHQ-9 at T2 (range: 0–27) | 3.8 | 4.2 |
COVID-19, Coronavirus disease 2019.
SD, standard deviation.
PHQ-9, Patient Health Questionnaire-9.
Sex, age occupational experience, occupation, experience with at least one dose of COVID-19 vaccination, willingness to receive the COVID-19 vaccine and PHQ-9 at T2 were measured at T2.
T1: October 2020, T2: May 2021.
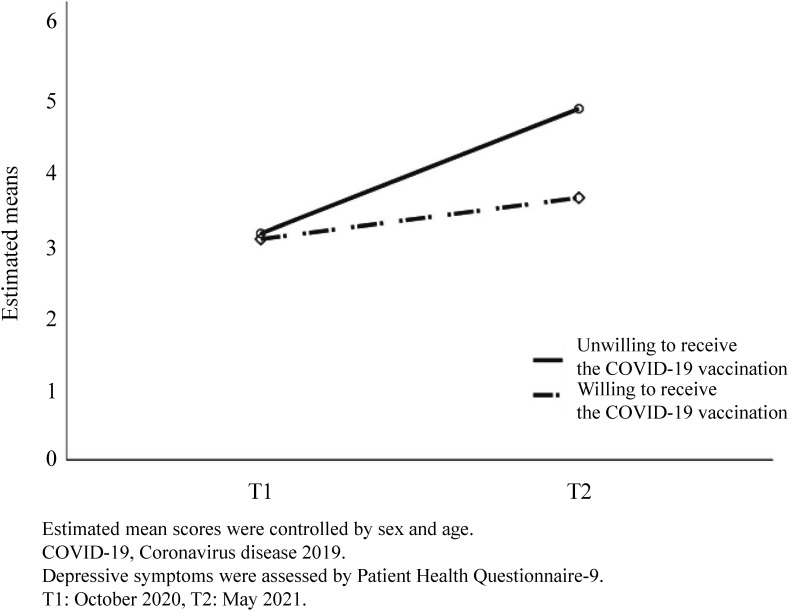
The results of the ANCOVA and the estimated mean of PHQ-9 scores at T1 and T2 between healthcare professionals who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination are shown in Table 2 and Fig. 2. The estimated mean of PHQ-9 score among healthcare professionals who were unwilling to receive COVID-19 vaccination was 3.4 (SE=3.8) at T1 and 5.0 (SE= 4.6) at T2. The estimated mean of PHQ-9 score among healthcare professionals who were willing to receive COVID-19 vaccination was 3.0 (SE=3.9) at T1 and 3.6 (SE=4.1) at T2. The group and time interaction effect was significant (F(1, 207)=3.9, p=0.049), and the change in the estimated mean of PHQ-9 score between healthcare professionals who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination was different.
Table 2. The estimated mean of PHQ-9 score at baseline (T1) and T2 among Japanese healthcare professionals: analysis of covariance (ANCOVA) (N=211).
| Estimated Means (SE)† | Interaction effect | p value | ||||
| Unwilling to receive the COVID-19 vaccination (n=37) | Willing to receive the COVID-19 vaccination (n=174) | |||||
|
| ||||||
| Outcomes | October 2020 |
May 2021 |
October 2020 |
May 2021 |
||
| PHQ-9 | 3.4 (3.8) | 5.0 (4.6) | 3.0 (3.9) | 3.6 (4.1) | F (1,207) = 3.9 | 0.049 |
† Estimated mean scores were controlled by sex and age.
COVID-19, Coronavirus disease 2019.
SE, standard error.
PHQ-9, Patient Health Questionnaire-9.
T1: October 2020, T2: May 2021.
Fig. 2.
The estimated mean of depressive symptoms at baseline (T1) and T2: analysis of covariance (N=211).
Discussion
This study showed the longitudinal change in depressive symptoms among healthcare professionals in Japan who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination, from before the start of vaccination (October 2020) until when vaccination had mostly ended (June 2021). The longitudinal changes in depressive symptoms differed among healthcare professionals who were willing to receive COVID-19 vaccination and those who were unwilling to receive COVID-19 vaccination: depressive symptoms were worse among those who were unwilling than among those who were willing to receive COVID-19 vaccination. To our knowledge, this is the first longitudinal study to examine the association of vaccine hesitancy with mental health.
As the results of the ANCOVA, the estimated mean of PHQ-9 score among healthcare professionals who were unwilling to receive COVID-19 vaccination was 3.4 (SE=3.8) at T1 and 5.0 (SE=4.6) at T2. The estimated mean of PHQ-9 score among healthcare professionals who were willing to receive COVID-19 vaccination was 3.0 (SE=3.9) at T1 and 3.6 (SE=4.1) at T2. The group and time interaction effect was significant (F(1, 207)=3.9, p=0.049). The estimated mean PHQ-9 score of healthcare professionals who were unwilling to receive COVID-19 vaccination increased significantly than the estimated mean PHQ-9 score of healthcare professionals who were willing to receive COVID-19 vaccination from T1 to T2. These results showed depressive symptoms were worse among healthcare professionals who were unwilling to receive vaccination than among those who were willing to receive vaccination, from before the start of vaccination (October 2020) to when vaccination had mostly ended during the pandemic (June 2021) in Japan. The result that COVID-19 vaccine hesitancy was positively associated with depressive symptoms was consistent with a previous cross-sectional studies13, 14). This longitudinal study might suggest the causal relationship between COVID-19 vaccination hesitancy and depressive symptoms, which previous studies has not been clarified.
Participants in this study who were unwilling to receive the vaccine consisted of those who had experienced at least one dose of COVID-19 vaccination and those who had not received a vaccination. The result that vaccine hesitation was positively associated with poor mental health among people who were vaccinated against COVID-19 was consistent with a previous cross-sectional study14). Healthcare professionals who were unwilling to receive COVID-19 vaccination but were vaccinated against COVID-19 might be depressed due to fears regarding the side effects and long-lasting effects of the vaccine against COVID-1914).
Among healthcare workers who were unwilling to receive COVID-19 vaccination and were not vaccinated against COVID-19, they might have been wondering whether to vaccinate, but might feel unable to confide their feelings in colleagues or might feel pressure to vaccinate. This study included 37 participants who were unwilling to receive vaccine against COVID-19, 30 participants had experienced at least one dose of COVID-19 vaccination and only 7 participants did not receive a COVID-19 vaccination, thus we were not able to conduct subgroup analyses. A study with a larger sample will be necessary in the future.
Recently in the United States, several medical centers announced a requirement for all healthcare professionals to be vaccinated against COVID-19; the question of whether to implement such a vaccination policy for healthcare professionals as a condition of employment is becoming clearer1). In some countries, such as Italy, the government has made vaccination against COVID-19 mandatory for healthcare professionals, which led to a debate on whether it is ethical2). These reports suggested that healthcare professionals who are unwilling to receive the COVID-19 vaccination were in the minority in the workplace and other settings, which might have a negative impact on their mental health. Given the results of the study, this issue may also need to be considered from a mental health perspective.
This study has several limitations. First, items about assessment of COVID-19 vaccine hesitancy were developed through discussion among authors. We could not use the COVID-19 vaccine hesitancy scale that it’s reliability and validity were confirmed in this study. Therefore, items about assessment of COVID-19 vaccine hesitancy are not fully evidence-based nor comprehensive. Second, items about assessment of COVID-19 vaccine hesitancy were measured at T2, the change in intention to receive vaccine from T1 was not examined. T1 was conducted in October 2020, and Japan had not yet decided on the COVID-19 vaccination schedule at this time. Therefore, we did not measure COVID-19 vaccine hesitancy at T1 because we did not think it was an appropriate time to ask about COVID-19 vaccine hesitancy. It is necessary to investigate the relationship between longitudinal change of COVID-19 vaccine hesitancy and longitudinal change of mental health during the COVID-19 pandemic in future studies. Third, approximately 95% of the participants in this study had received a vaccine against COVID-19, and the percentage of those who had not received a vaccine against COVID-19 was small. This difference in percentage may have affected the results. Fourth, motivated healthcare professionals are more likely to register as DMAT and DMAT members; thus, DMAT and DPAT members may not be representative of healthcare professionals in Japan. Fifth, we could not assess non-response bias. Participants who did not want to answer questions, such as COVID-19 vaccination hesitancy, may not have participated in the study. Sixth, we could not include quality assurance questions in the questionnaire. Thus, we might not be able to remove respondents who did not pay sufficient attention in this study. However, we did not assume that there would be respondents who did not pay sufficient attention, because we did not pay any rewards to the participants in our study, so we expect that those who did not want to participate did not participate. Finally, the response rate was low, which may limit the external validity of this study. Non-responders could be too stressed to respond or not at all stressed and therefore not interested in this survey. In the future, a survey with a larger sample and a higher response rate would be necessary.
Despite those limitations, to our knowledge, this study is the first longitudinal study to examine the association of COVID-19 vaccine hesitancy with depressive symptoms. This longitudinal study might suggest the causal relationship between vaccination intention and mental health, which previous studies has not been clarified. This study suggests that it is important to take care of healthcare professionals who are unwilling to receive vaccination to prevent mental health deterioration, from before the start of vaccination to when vaccination had mostly ended during the pandemic.
Conclusions
This study showed depressive symptoms was worse among healthcare professionals who were unwilling to receive COVID-19 vaccination than those who are willing to receive COVID-19 vaccination from before the start of vaccination (October 2020) to when vaccination had mostly ended among health care professionals (June 2021) in Japan. This suggests that it is important to take care of healthcare professionals who are unwilling to receive vaccination to prevent mental health deterioration. This study suggests the necessity to consider vaccine hesitancy from a mental health perspective, and further studies are needed.
Acknowledgments
The authors thank all participants in this study.
Conflict of Interest
All authors declare no relevant conflicts of interest in relation to the subject of the manuscript.
Funding/Support
This work was supported by Health and Labor Sciences Research Grants (19IA2014 to DN).
Authors’ Contributions
DN was in charge of this study, supervising the process and providing his expert opinion. HA and DN conceived and designed the study. HA, YKo, YKa, MI, YM, and DN contributed to creating questionnaires. YKa and MI recruited the participants. HA and DN developed the analysis plan. YKo managed the enrolment procedure and overall control of the study. HA wrote the first draft of the manuscript, and all other authors revised the manuscript critically. All authors approved the final version of the manuscript.
References
- 1).Talbot TR (2021) COVID-19 vaccination of health care personnel as a condition of employment: a logical addition to institutional safety programs. JAMA 326, 23–4. [DOI] [PubMed] [Google Scholar]
- 2).Paterlini M (2021) Covid-19: Italy makes vaccination mandatory for healthcare workers. BMJ 373, n905. [DOI] [PubMed] [Google Scholar]
- 3).Dyer C (2021) Covid-19: vaccination to become mandatory for care home staff and could extend to NHS. BMJ 373, n1576. [DOI] [PubMed] [Google Scholar]
- 4).Razai MS, Chaudhry UAR, Doerholt K, Bauld L, Majeed A (2021) Covid-19 vaccination hesitancy. BMJ 373. n1138. [DOI] [PubMed] [Google Scholar]
- 5).Robinson E, Jones A, Lesser I, Daly M (2021) International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine 39, 2024–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).de Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ (2020) Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet 396, 898–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Okubo R, Yoshioka T, Ohfuji S, Matsuo T, Tabuchi T (2021) COVID-19 vaccine hesitancy and its associated factors in Japan. Vaccines 9, 662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Japan Broadcasting Corporation. [Information of vaccination status in Japan]. 9 July 2020. https://www3.nhk.or.jp/news/special/coronavirus/vaccine/progress/#mokuji5 (in Japanese). Accessed 13 July, 2021.
- 9).DE Bloom J (2020) How to recover during and from a pandemic. Ind Health 58, 197–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Kisely S, Warren N, McMahon L, Dalais C, Henry I, Siskind D (2020) Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ (Clinical research ed.) 369, m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11).Johnston DA, Harvey SB, Glozier N, Calvo RA, Christensen H, Deady M (2019) The relationship between depression symptoms, absenteeism and presenteeism. J Affect Disord 256, 536–40. [DOI] [PubMed] [Google Scholar]
- 12).Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P (2020) Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 88, 901–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Szmyd B, Karuga F F, Bartoszek A, Staniecka K, Siwecka N, Bartoszek A, Błaszczyk M, Radek M (2021) Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines 9, 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Palgi Y, Bergman YS, Ben-David B, Bodner E (2021) No psychological vaccination: vaccine hesitancy is associated with negative psychiatric outcomes among Israelis who received COVID-19 vaccination. J Affect Disord 287, 352–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15).Bendau A, Plag J, Petzold MB, Ströhle A (2021) COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol 97, 107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16).von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg (London, England) 12, 1495–9. [DOI] [PubMed] [Google Scholar]
- 17).Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16, 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18).Muramatsu K, Miyaoka H, Kamijima K, Muramatsu Y, Tanaka Y, Hosaka M, Miwa Y, Fuse K, Yoshimine F, Mashima I, Shimizu N, Ito H, Shimizu E (2018) Performance of the Japanese version of the Patient Health Questionnaire-9 (J-PHQ-9) for depression in primary care. Gen Hosp Psychiatry 52, 64–9. [DOI] [PubMed] [Google Scholar]