Abstract
Background
During the COVID-19 pandemic, in-person cadaveric dissection laboratories for teaching anatomy were omitted by many schools around the world. While knowledge domains can be easily evaluated via remote exams, non-traditional discipline-independent skills such as those encouraged through reflection on the topic of death are often overlooked. This study investigated how different anatomy course formats played a role in initiating students’ reflections on death during the COVID-19 pandemic.
Method
In fall 2020, 217 medical, dental, premedical, and health sciences students from 13 international universities discussed differences in their anatomy courses online. Formats of anatomy courses ranged from dissection-based, prosection-based, hybrid (combination of dissection and prosection) to no laboratory exposure at all. Students’ responses to the question, “Did/does your anatomy course initiate your thinking about life's passing?” were collected, and they self-reported themes that were present in their reflections on death using a multiple-choice prompt. Statistical analyses to detect differences between students with and without exposure to cadavers were performed using the chi-squared test.
Results
When comparing students who had exposure to human anatomical specimens to those who had no exposure, the majority of students with exposure thought that the course did initiate thoughts about life’s passing, compared to students without exposure (P < 0.05). Reflection themes were consistent across groups.
Discussion
These findings indicate that anatomy dissection courses are important for the initiation of students’ feelings about the topic of death. Omission of cadaveric dissection- or prosection-based laboratories will decrease the likelihood that students initiate reflection on this topic and gain important transferable skills.
Keywords: Anatomy course, Dissection course, Students, Reflection on death, COVID-19, Peer interactions
Introduction
During the onset of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; COVID-19) pandemic, major changes in the delivery of anatomy teaching have been reported across the globe. Due to social distancing mandates, many programs underwent significant redesigns in the delivery of their anatomy teaching, as was necessary for remote education [1–4]. In many schools around the world, in-person cadaveric dissection was omitted, or time allotted to the cadaver laboratory was significantly reduced [1]. Concerns that these changes and the omission of cadaveric dissection would persist were raised by many in the anatomy education community [3, 5].
One aspect of anatomy education that instructors most feared would be lost in the transition to remote teaching was the benefits of the “hidden curriculum” associated with the cadaveric dissection laboratory [2]. The hidden curriculum in medical education is known to be an effective forum for teaching skills that are not explicit goals of the standard activities outlined in the curriculum [6]. In anatomy, the cadaver laboratory is one area that has long been shown to have a rich hidden curriculum, offering educational benefits outside of simply teaching anatomical facts [7].
Historically, dissection-based anatomy courses have been shown to improve health professions students’ clinical education outcomes, ethics, and humanity, as well as to encourage them to reflect on and process the concepts of death and illness that they will undoubtedly encounter in practice [8–13]. Working in small groups in the cadaver laboratory has also been shown to have benefits for the formation of professional identities, including the practice of behavior and attitudes required of medical and health professionals [13, 14]. In addition to the initiation of introspection on ethics, empathy, and humanistic values observed in medical students [15–19], some have reported that dissection-based anatomy teaching can promote respect and compassion [20]. Furthermore, dissection-based laboratory environments help students to develop coping mechanisms for encounters with and around the topic of death [21]. These are all crucial elements of the hidden anatomy curriculum that prepare students for a future of patient interactions in clinical practice.
The associations between participation in cadaveric dissection, strong emotions, and reflection on the topic of death among students have been reported extensively in the education literature [13, 22–26]. It is generally agreed upon that reflective practices are important, particularly for young health professions students as they begin life-long careers as medical and allied healthcare practitioners [27]. However, while knowledge-based assessments can be easily administered via remote examination [28], evaluation of non-traditional discipline-independent skills that are commonly conveyed via cadaveric dissection (e.g., empathy, compassion, reflection on the topic of death) are difficult to assess and often overlooked. Furthermore, because human anatomy education is traditionally an in-person discipline, published research on how different anatomy teaching formats initiate students’ reflections on ethics and other topics, including reflection on death, are mostly based on traditional approaches that include exposure to a full-body human cadaver or cadaveric specimens [6, 13, 15, 16, 21, 29–31]. There is a paucity of research on whether non-traditional or modified anatomy curricula can elicit similar outcomes as traditional cadaver-based settings, especially during the persistent COVID-19 pandemic [32, 33].
This research team recently observed the impact that the format of anatomy teaching can have on how anatomy course participation can initiate students’ reflections on the topic of death [34]. Through identifying different themes of reflection and categorizing them based on the students’ enrollment in either dissection, prosection, hybrid, or non-dissection-based course formats, the authors observed that preclinical students’ exposure to a deceased person, as a whole human body or in part, may have encouraged them to reflect more on death and dying than their peers in less cadaver-focused curricula. Courses that did not expose students to any cadaveric specimens did not appear to initiate reflection on the topic of death at all [34]. This initial observational study did not include a quantitative portion and was conducted prior to the COVID-19 pandemic, with only a limited number of participants. However, the findings indicated that the presence of a cadaver in the learning activities seemed important for students to initiate reflective thinking [34].
Based on the above observations, the authors formulated a study to investigate whether anatomy course formats (e.g., dissection, prosection, or remote instruction) had disparate impacts on the initiation of reflection on the topic of death among health professions students. The objective of the current study was to elicit additional qualitative data and provide quantitative data to support the previous findings in anatomy courses during the COVID-19 pandemic in 2020 [34]. It was hypothesized that the anatomy course formats that included exposure to whole-body human cadavers and/or prosected cadaveric specimens would be more likely to initiate students’ reflections on the topic of death.
This report provides details of the changes made to anatomy course formats at 13 institutions from various countries during the 2020 COVID-19 pandemic. The changes are described and associated with their impact on students’ reflections on death. Analysis of the student feedback obtained in this study will help to elucidate the impact of cadaver exposure on the hidden anatomy curriculum. This type of insight may influence how educators choose to teach anatomy in the future and/or initiate a discussion on how different modalities can be leveraged to encourage reflection on the topic of death when it is not possible to teach using cadaveric specimens. Regardless of the findings, discussions on how best to promote the development of non-traditional discipline-independent skills that are typically learned during in-person dissection-based anatomy courses are needed if traditional laboratory formats are omitted in the future.
Material and Methods
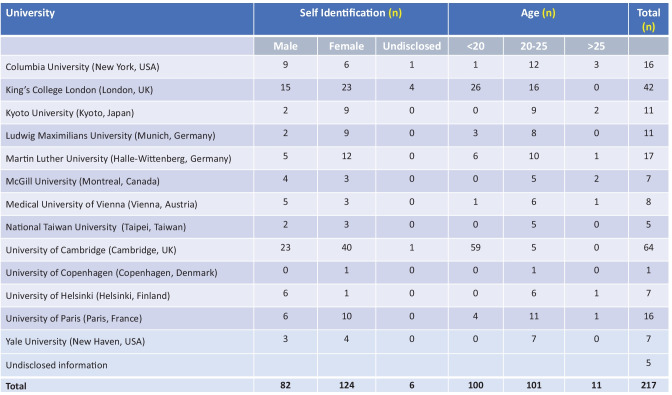
In the fall semester of 2020, 217 medical, dental, premedical undergraduate, and health sciences students from 13 international universities met to discuss differences in their anatomy courses in small online focus groups on Zoom (Zoom Video Communications, Inc., San Jose, CA), as part of the “International Collaboration and Exchange Program (ICEP) – Preparing Global Leaders for Healthcare” [35, 36]. The ICEP program facilitates online networking and travel exchanges (when international travel restrictions permit) between students enrolled in anatomy courses at pre-medical, medical, and dental levels around the globe. The goal of the program is to convey skills to future global healthcare leaders so that they can solve healthcare issues in a globally collaborative manner. Details of the participating students’ demographic information are listed in Table 1.
Table 1.
Student demographics. At the time of the survey, the students were at different stages within their respective anatomy courses
Descriptions of the formats of anatomy education delivery at the 13 universities were collected as part of a student survey in Qualtrics XM (Qualtrics International, Inc., Seattle, WA) and confirmed via faculty questionnaires. The faculty questionnaires to determine changes made to anatomy course formats in response to the COVID-19 pandemic were collected via Google Forms (Alphabet, Inc., Mountain View, CA).
For the quantitative comparison, a multiple-choice question was administered to determine whether or not students felt that the anatomy course initiated their reflection on the topic of death. The question “Did/does your anatomy course initiate your thinking about life’s passing?” was adapted from previous work where students were asked “How did your anatomy course initiate your thinking on life’s passing?” [34].
Previous work has shown that this question was capable of eliciting thoughtful responses from students, which were analyzed through inductive thematic analysis to describe the prominent themes [34]. This previous work, which employed an inductive and deductive coding analysis, generated themes that included appreciation, avoidance, benefits, dichotomy, dignity, fragility of life, spirituality, and salience of death along with unchanged thought on the topic of death [34]. Based on those results, the current study aimed to address whether or not the type of exposure (i.e., dissection, prosection, and hybrid) to human cadavers or anatomical specimens had any impact on the themes represented in students’ reflections on the topic of death. Because it was expected that self-reporting would likely include several common thematic categories, students were given a list of such themes and asked to select which ones were most associated with their own reflections on death. These themes were adapted from previous observations on students’ initiation of reflection on death [34]. The questions included the following:
“Did/does your Anatomy course initiate your thinking on life’s passing?”
“The anatomy course initiated my thoughts on … Fragility of Life/Shortness of Life, Sanctity of Passing, Dignity of Life, Beauty of Life, Religion and Life, Dichotomy between Body and Soul, Mixed feelings on Death”
Given that the themes were already identified in previous work, a repeat of this qualitative analysis was not included in the present study [34]. All data were collected using multiple-choice questions administered on the Qualtrics XM© survey platform.
The analyses involved two components. The first was a comparison of students’ responses based on their self-reported anatomy education format (Group 1, comprehensive dissection; Group 2, hybrid dissection plus prosection; and Group 3, no dissection at all). Because students were at different stages within their anatomy courses at the time of the survey, with some students having already completed a year of anatomy education with body donors prior to COVID, a second portion of the analysis grouped the responses into students who had already been exposed to human bodies or remains and those who had not, prior to COVID.
Statistical analyses were performed using the Chi-squared test in Microsoft Excel© with an alpha value set at 0.05. These were used to detect any group differences in initiation of reflection on death between students who were exposed to cadaveric materials and those who were not. Additionally, the Chi-squared test of independence was used to compare the identification of themes related to the topic of death between these groups.
Ethical approval for this study was obtained at Columbia University (IRB—AAAS0074), McGill University (IRB Study No. A07-E54-17B), and the National Taiwan University (IRB—202001069 W).
Results
Anatomy Course Formats at Different Universities During the COVID-19 Pandemic
Table 2 depicts the differences in course formats at the participating universities before the onset of the COVID-19 pandemic and during the fall, 2020. Anatomy laboratory delivery formats included full dissection, hybrid (virtual, dissection-, and prosection-based), prosection only, and no laboratory exposure at all during the pandemic.
Table 2.
Anatomy course formats pre-COVID-19 and during the COVID-19 pandemic at 12 universities. Two schools did not change their anatomy course formats during the pandemic (National Taiwan University and University of Paris). Information from one university was not available. In fall 2020, some schools offered virtual prosections only and some offered in person prosections
| University | Pre-COVID | COVID Fall 2020 | ||||||
|---|---|---|---|---|---|---|---|---|
| Hands-on dissection? | Prosection? | Hands-on dissection? | Prosection? | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | |
|
Columbia University (New York, USA) |
54 h | - | - | - | - | (Fully virtual; 3D Atlas or Imaging only) | - | - |
|
King’s College London (London, UK) |
30 h | - | 90 h | - | - |
90 h (Virtual prosection with open learning sessions) |
- | |
|
Kyoto University (Kyoto, Japan) |
56 h | - | - | - | - | (Fully virtual; 3D Atlas or Imaging only) | - | - |
|
Ludwig Maximilian University (Munich, Germany) |
90 h | - | - | - |
90 h (Smaller groups) |
- | - | - |
|
Martin Luther University (Halle-Wittenberg, Germany) |
78 h | - | 4 h | - |
54 h (Reduced hours) |
- | 4 h | - |
|
McGill University (Montreal, Canada) |
20 h | - | - | - | 2 h | - | Virtual prosection | - |
|
Medical University of Vienna (Vienna, Austria) |
27 h | - | - | - | 100 h | - |
10 h (Virtual prosection) |
- |
| National Taiwan University (Taipei, Taiwan) | 150 h | - | - | - | 150 h | - | - | - |
| University of Cambridge (Cambridge, UK) | 104 h | - | 20 h | - |
84 h (Reduced hours) |
- | 64 h | - |
| University of Copenhagen (Copenhagen, Denmark) | 24 h | - | 58 h | - | 6 h | - | 58 h | - |
|
University of Helsinki (Helsinki, Finland) |
12 h | - | 6 h | - | - | - | 6 h | - |
|
University of Paris (Paris, France) |
(Fully virtual; 3D Atlas or imaging only) | |||||||
Comparisons between pre- and post-COVID-19 formats demonstrated that at least seven schools added a virtual component and/or reduced the course contact time with human cadavers during the pandemic. Columbia University did not offer students any exposure to human specimens at the time of the survey, but subsequently did. The University of Paris did not offer hands-on dissection before or during COVID-19. King’s College London taught a virtual prosection class during the pandemic. One school’s anatomy course was not affected by COVID-19 (National Taiwan University), where teaching continued in an unchanged format (full dissection without prosections).
Initiation of Reflection on the Topic of Death
In total, 217 students across 13 universities completed the survey. Out of that, 105 students indicated that they had dissected (Group 1), 21 had a hybrid dissection- and prosection-based course (Group 2), and 80 noted that they had no dissection-based experience (Group 3) at the time of the survey (Table 3). At the time of the survey, a total of 149 students responded that they had exposure to human cadavers or anatomical specimens (Group A), and 52 indicated that they did not (Group B; Table 4). Note, however, that not all students responded to this question. In addition, 11 participants (health professions students) had no anatomy course at all and therefore were excluded from further analyses. Response rate after accounting for the excluded control group was high; 201 students out of 206 responded to the exposure question.
Table 3.
Comparison between different groups based on anatomy format. There was a significant difference between student responses in the dissection course and students with no dissection course, regarding the initiation of the reflection on death (P = 0.023)
| Group 1 Dissection course |
Group 2 Hybrid dissection-prosection course |
Group 3 No dissection course |
No anatomy course | Total | |
|---|---|---|---|---|---|
| Reflection on death initiation | 79 (75%) | 15 (71%) | 45 (56%) | 1 (10%) | |
| No reflection on death initiation | 26 (25%) | 6 (29%) | 35 (44%) | 10 (90%) | |
| Total | 105 | 21 | 80 | 11 | 217 |
Table 4.
Comparison between groups based on their exposure to a cadaveric specimen in the anatomy course at the time of the survey. Some students did not respond to this question (n = 201 responded). When comparing responses from students who had exposure to a cadaveric specimen versus students without exposure there was a significant difference between the two groups (P = 0.0001). More students in the exposure group felt that the anatomy course led them to reflect on the topic of death
|
Group A Exposure to cadaveric specimen |
Group B No exposure to cadaveric specimen |
Total | |
|---|---|---|---|
| Reflection on death initiation | 113 (76%) | 24 (46%) | |
| No reflection on death initiation | 36 (24%) | 28 (54%) | |
| Total | 149 | 52 | 201 |
There was a discrepancy caused by students indicating that they had a dissection-based course despite not having had any actual exposure to human cadavers or anatomical specimens. This difference stemmed from the fact that the survey was taken at too early a time point in the anatomy course for some students. While their schools may have offered dissection later in the curriculum, they had not yet had any physical contact with human cadavers at the time of the survey. Therefore, the main analysis was based on students’ responses indicating if they had exposure or not at the time of the survey and the two groups (exposure to human cadavers and no exposure to human cadavers) were compared (Table 4).
Significantly more students who had exposure to human cadavers or anatomical specimens reported that the course did initiate thoughts about life’s passing, compared to students who did not have this exposure (P < 0.05; Table 3). Of note, there were a number of students who did not think that the anatomy course inspired them to think about the topic of death, despite being exposed to a human cadaver or anatomical specimens (n = 9). Furthermore, a high number of students did not have any exposure to human cadavers, yet they felt that the anatomy course did initiate reflection on this topic (n = 24; Group B; Table 4).
Two Chi-squared tests of independence were performed. The first was to assess the relationship between anatomy course format and themes on death and life shared by the students in the post-course reflections; the second was to assess the relationship between the students’ exposure to cadaveric specimen and the same themes on death and life. There was a significant relationship between course format and reflection themes (X2(21, 667) = [32.49], P = [0.10]). There was also a significant relationship between exposure to cadaveric specimen and reflection themes (X2(14, 654) = [75.03], P = [0.05]).
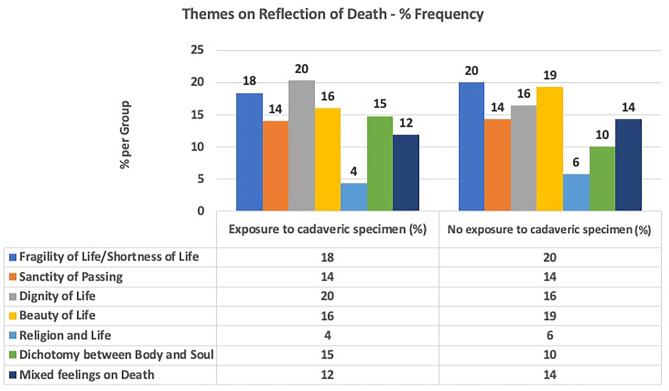
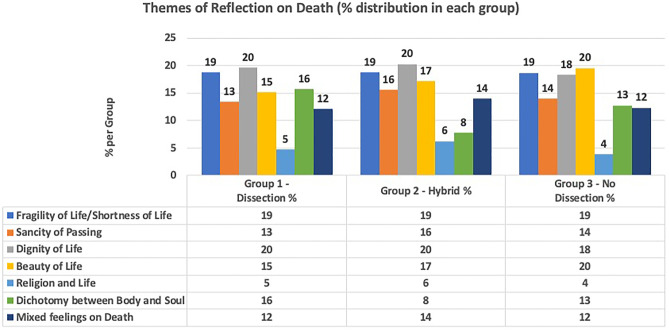
Themes About Reflection on Death
When students were asked to identify which of the suggested themes were most associated with their own reflections on the topic of death, Dignity of Life, Fragility of Life, and Dichotomy of Body and Soul were the prevalent themes that students identified with. A statistical comparison to determine whether the distribution of different themes was dependent on exposure to human cadavers revealed no significant differences between the two groups (exposure versus no exposure to a cadaveric specimen), indicating that the overall thematic content (representative of the depth of the reflections) from each group was not dissimilar (Fig. 1). However, a significance of P < 0.1 was observed between the groups.
Fig. 1.
Comparison of themes of students who had exposure to cadaveric specimens and students who did not have exposure
When comparing dissection-based courses to hybrid courses within the group that did have exposure to cadaveric material, no statistically significant differences in themes was observed (Fig. 2).
Fig. 2.
Comparison of groups of students who dissected or had a hybrid course or no hands-on dissection course
Discussion
The current study emphasizes the importance of anatomy dissection courses for promoting beneficial outcomes of the hidden curriculum, and it offers quantitative support to previous observations that dissection-based anatomy courses and exposure to human anatomical specimens can help students to initiate reflection on the topic of death [34]. This follow-up study shows that courses that do not offer exposure to human remains via dissection- or prosection-based components have a lesser likelihood of supporting students in their reflection on this topic and their subsequent development of non-traditional discipline-independent skills. Overall, these findings may have implications for the future of anatomy courses as the COVID-19 pandemic restrictions begin to be lifted in many countries.
Anatomy Courses and the COVID-19 Pandemic
During the pandemic, many anatomy courses had to temporarily discontinue in-person dissections for the first time. Prior to the above, some institutions had already successfully implemented anatomy courses that omitted full hands-on cadaveric dissections, citing resource constraints such as budget reductions, or the lack of expert faculty members [37]. Virtual 3D imaging technology has significantly improved and is becoming more readily available and utilized. Although there is still limited data available and the debate about the overall impact these technologies have on students’ learning persists [4, 38–53], the recent forced reductions of comprehensive dissection-based anatomy courses may encourage educators to include virtual 3D imaging technology in order to supplement their laboratory components. If virtual and 3D teaching are well received and result in comparable examination outcomes during this period, some institutions may consciously decide to reduce or omit cadaveric dissection altogether to save resources in the future [54]. Furthermore, an increasing shortage of expert faculty in anatomy education with skills in dissection may lead to decisions to not reintroduce dissection courses after the pandemic. Therefore, full hands-on cadaveric dissection risks becoming a relic of the past, which would reduce students’ exposure to experiences that encourage reflection on the topic of death that is beneficial for their future as healthcare professionals. When comparing the formats of anatomy teaching between the different schools in the present study, only one out of 13 schools did not offer any exposure to a cadaver even prior to the pandemic. A follow-up study is needed to explore how many of the schools that changed their teaching formats during the height of the pandemic reverted back to their original formats of teaching with hands-on cadaveric dissection and whether some schools instead modified their courses to have shorter dissection times or complete omission of dissection and/or cadaveric exposure.
Hidden Curriculum
Studies have shown that the hidden curriculum associated with anatomy courses is very extensive and goes well beyond the boundaries of the overt teaching of anatomical facts and concepts [6, 13, 14]. The non-traditional discipline-independent skills encouraged by the initiation of reflection about the topic of death such as, empathy, compassion, and ethics are important learning objectives that anatomy courses can provide [17–20, 23–25]. These skills are often not specifically taught or addressed in other subjects in medical or dental school, particularly in the early preclinical years. These often-called “soft” skills are typically not evaluated or assessed; however, students are expected to have obtained these competencies by the time they enter their clinical years or at least before they graduate. The authors are concerned that the generation of health professions students who have been taught mostly online may lack an early transformational encounter with death and therefore miss out on an important developmental opportunity.
Traditionally, medical schools build upon the skills that students obtain in their preclinical years as they progress through to their degrees. The long-term impact of deficiencies in these skills may not become evident until years into the future—perhaps not even until students enter their clinical years or after graduation. Therefore, the authors suggest that if cadaveric dissection was omitted during the pandemic, curricular enrichment to include teaching and reflection on the topic of death outside of the anatomy course is needed. Supplementing students’ learning with other activities that can enhance empathy, compassion, and ethics in the years after the pandemic is vital—potentially via courses in the overt medical curriculum. This study indicates that without exposure to human cadavers or anatomical specimens, there is a lesser likelihood that students will think about the subject of death. While empathy, compassion, and teamwork may be incorporated into other subject matters, the very sensitive topic of death may be difficult to initiate without the exposure to a deceased human being. The authors suggest that exposure to other experiences (e.g., a visit to a hospital morgue, an internship in a pathology autopsy department, or work experience in a funeral home) in combination with reflective writing exercises may be a way to incorporate this topic into the curriculum if anatomy dissection is omitted. While elements of autopsy approaches have occasionally been offered in the past, the focus was often on the autopsy experience, and the reflection on death within this experience is currently not part of a standard curriculum [55–60]. Further research is needed before alternative experiences are instituted.
Initiation of the Reflection on the Topic of Death
The first encounter with death is challenging for young students [23, 61]. Although previous studies have shown that many students have had experience or encounters with death prior to the start of the anatomy course [24, 62], it has become less and less likely in this modern era that a young person in their late teenage years or early 20 s has encountered death. Improved medical care, times of peace, and rare epidemics make it more likely that today’s students’ grandparents are still alive, and any previous experiences that they may have had with death were most likely due to unusual or tragic circumstances. However, the recent pandemic may have changed young peoples’ experiences with death, and it will be important to follow up with student populations in the global health professions to determine if the pandemic has initiated reflection on the topic of life and death. Nevertheless, for many students, the cadaver laboratory and dissection-based anatomy courses will remain their first contact with death and an environment in which they have the opportunity to intensely reflect on this topic [62].
Despite having had exposure to human cadavers, there were some students who did not think that the anatomy course inspired them to consider the topic of death. This may have been due to a variety of reasons such as young age, cultural avoidance of the topic of death, a perceived professional expectation to hide emotions, detachment as a coping mechanism, a regard of the cadaver as a patient/mentor/teacher and not as a deceased person, and other factors [63–65]. This finding confirms observations from a study prior to the COVID-19 pandemic that some students may avoid this topic despite having access to a full-body human cadaveric dissection-based course [34]. Thus, further investigation is needed regarding how to persuade these future medical and health professionals to reflect on and discuss the sensitive topic of death.
In contrast, there were students who did not have any exposure to human cadavers or anatomical specimens, yet they felt that the anatomy course still helped them to initiate reflections on this topic. An explanation for this finding is that by thinking of the human body donors or being exposed to photos of anatomy laboratories online, some students will reflect on this topic due to the historical association of the anatomy course with cadavers and death. If anatomy is increasingly taught without any human cadavers or human remains, this historical association will fade among the following several generations of students. Thus, preventive measures (e.g., inclusion of the history of anatomy teaching and body donation in anatomy courses) should be considered now.
Themes About Reflection on Death
It was interesting to observe that the depth and themes of the reflections were similar in all students that reflected on this topic. However, it appears that once the students initiated their reflection on the topic of death, there was no significant difference in the types of themes that they focused on. Nevertheless, there may have been slight differences in the individual context and depth of their reflections as shown in our analysis. Dignity of Life and Sanctity of Passing were important topics the dissecting students felt that the anatomy experience led them to think about. Introducing a young person to value life and to think about death can be essential on their path to maturing in their career as a healthcare professional. This thought process of realizing the “gray zone” between the physical body and the soul of a person may trigger thinking in students that can help them to mature and look beyond a patient’s physical ailments towards a holistic approach in medicine [66–70]. Such reflection is difficult to initiate without some exposure to, or experience with death.
Of further note is the framework of the international exchange program, which included small group peer discussions about the respective anatomy courses at schools in different countries. These discussions often shifted into a conversation about body donation (anecdotal observation) and may have influenced students who would have otherwise not reflected on the topic of death. Thus, more students indicated they reflected on this topic (especially, those who did not have exposure to human cadavers) and may have felt that the course initiated their reflections on the topic of death. However, without the prior peer discussion, this may not have been the case.
As restrictions on anatomy courses continue to encroach on teaching time and resources [71, 72], the authors feel that a network of international collaborations among anatomy and medical educators, such as the ICEP, can help with teaching anatomy in the twenty-first century, particularly, regarding “soft” skills development and other areas of the hidden curriculum.
Limitations
A major limitation of the study is the setting of the project and its timing in the virtual international program. Because there was no timeline given with regard to submitting the survey, some students began discussing this topic in small groups prior to submission of the survey. Therefore, a small number of students who did not dissect may have been influenced by their interactions with their peers. A follow-up study that excludes students who have had prior discussions about this topic is needed.
Furthermore, because many of the participating schools resorted to virtual teaching during the pandemic, it will be important to study if actual physical exposure (e.g., being in the same room, touching, and dissection experience), versus online visual exposure, to human bodies and remains has an impact on the students’ experiences.
Conclusion
Anatomy dissection courses are important for the initiation of students’ reflections on the topic of death. This study suggests that eliminating the opportunity for students to interact with human cadavers during COVID-19 resulted in insufficient reflection on this topic by preclinical students. While there are alternative ways to introduce the topic of death to students, the experience with human remains in the anatomy course cannot easily be reproduced for many reasons. Further research is needed before such alternatives should be considered or instituted.
Acknowledgements
The authors thank Michael Fortgang, MD, for helpful review of the manuscript, the students enrolled in the “International Collaboration and Exchange Program (ICEP) – Preparing Global Leaders for Healthcare” (https://www.internationalcollaborationexchange.org) for their participation in this research, and the collaborators at the international universities and the members of the advisory board of ICEP for their advice about the program (Drs. Leo Buhler, Mark Hardy, and Snehal Patel).
Declarations
Ethics Approval
Ethical approval was obtained at Columbia University (IRB—AAAS0074), McGill University (IRB Study No. A07-E54-17B), and the National Taiwan University (IRB—202001069 W).
Consent to Participate
Obtained as part of student questionnaires per IRB.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harmon DJ, Attardi SM, Barremkala M, Bentley DC, Brown KM, Dennis JF, et al. An analysis of anatomy education before and during COVID-19: May-August 2020. Anat Sci Educ. 2021 doi: 10.1002/ase.2051. [DOI] [PubMed] [Google Scholar]
- 2.Pather N, Blyth P, Chapman JA, Dayal MR, Flack N, Fogg QA, et al. Forced disruption of anatomy education in Australia and New Zealand: an acute response to the COVID-19 pandemic. Anat Sci Educ. 2020;13(3):284–300. doi: 10.1002/ase.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iwanaga J, Loukas M, Dumont AS, Tubbs RS. A review of anatomy education during and after the COVID-19 pandemic: revisiting traditional and modern methods to achieve future innovation. Clin Anat. 2021;34(1):108–114. doi: 10.1002/ca.23655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoo H, Kim D, Lee YM, Rhyu IJ. Adaptations in anatomy education during COVID-19. J Korean Med Sci. 2021;36(1):e13. doi: 10.3346/jkms.2021.36.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bond G, Franchi T. Resuming cadaver dissection during a pandemic. Med Educ Online. 2021;26(1):1842661. doi: 10.1080/10872981.2020.1842661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cocks M. The hidden curriculum. CMAJ. 2014;186(2):152. doi: 10.1503/cmaj.131455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghosh SK. Cadaveric dissection as an educational tool for anatomical sciences in the 21st century. Anat Sci Educ. 2017;10(3):286–299. doi: 10.1002/ase.1649. [DOI] [PubMed] [Google Scholar]
- 8.Arráez-Aybar LA, Casado-Morales MI, Castaño-Collado G. Anxiety and dissection of the human cadaver: an unsolvable relationship? Anat Rec. 2004;279. 10.1002/ar.b.20022. [DOI] [PubMed]
- 9.Moxham BJ, Plaisant O, Lignier B, Morgan S. Attitudes and responses of medical students and professional anatomists to dissecting different regions of the body. Clin Anat. 2019;32(2):253–267. doi: 10.1002/ca.23294. [DOI] [PubMed] [Google Scholar]
- 10.Dyer GS, Thorndike ME. Quidne mortui vivos docent? The evolving purpose of human dissection in medical education. Acad Med. 2000;75(10):969–979. doi: 10.1097/00001888-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Aziz MA, McKenzie JC, Wilson JS, Cowie RJ, Ayeni SA, Dunn BK. The human cadaver in the age of biomedical informatics. Anat Rec. 2002;269(1):20–32. doi: 10.1002/ar.10046. [DOI] [PubMed] [Google Scholar]
- 12.Rizzolo LJ. Human dissection: an approach to interweaving the traditional and humanistic goals of medical education. Anat Rec. 2002;269(6):242–248. doi: 10.1002/ar.10188. [DOI] [PubMed] [Google Scholar]
- 13.Kassam C, Duschinsky R, Brassett C, Barclay S. ‘Knowing everything and yet nothing about her’: medical students’ reflections on their experience of the dissection room. Med Humanit. 2020;46(4):403–410. doi: 10.1136/medhum-2019-011708. [DOI] [PubMed] [Google Scholar]
- 14.Kumar Ghosh S, Kumar A. Building professionalism in human dissection room as a component of hidden curriculum delivery: a systematic review of good practices. Anat Sci Educ. 2019;12(2):210–221. doi: 10.1002/ase.1836. [DOI] [PubMed] [Google Scholar]
- 15.Stephens GC, Rees CE, Lazarus MD. How does donor dissection influence medical students’ perceptions of ethics? A cross-sectional and longitudinal qualitative study. Anat Sci Educ. 2019;12(4):332–348. doi: 10.1002/ase.1877. [DOI] [PubMed] [Google Scholar]
- 16.Jones TW. Creating a longitudinal environment of awareness: teaching professionalism outside the anatomy laboratory. Acad Med. 2013;88(3):304–308. doi: 10.1097/ACM.0b013e318280f075. [DOI] [PubMed] [Google Scholar]
- 17.Guo K, Luo T, Zhou LH, Xu D, Zhong G, Wang H, et al. Cultivation of humanistic values in medical education through anatomy pedagogy and gratitude ceremony for body donors. BMC Med Educ. 2020;20(1):440. doi: 10.1186/s12909-020-02292-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hildebrandt S. Thoughts on practical core elements of an ethical anatomical education. Clin Anat. 2016;29(1):37–45. doi: 10.1002/ca.22645. [DOI] [PubMed] [Google Scholar]
- 19.Kaye A, Miranda M, Jones T. The donor letter project: learning professionalism and fostering empathy in an anatomy curriculum. J Med Humanit. 2019;40(4):607–612. doi: 10.1007/s10912-019-09573-x. [DOI] [PubMed] [Google Scholar]
- 20.Weeks SE, Harris EE, Kinzey WG. Human gross anatomy: a crucial time to encourage respect and compassion in students. Clin Anat. 1995;8(1):69–79. doi: 10.1002/ca.980080113. [DOI] [PubMed] [Google Scholar]
- 21.Dueñas AN, Kirkness K, Finn GM. Uncovering hidden curricula: use of dark humor in anatomy labs and its implications for basic sciences education. Med Sci Educ. 2020;30(1):345–354. doi: 10.1007/s40670-019-00912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hildebrandt S. What is happening in our anatomical dissection rooms? Clin Anat. 2014;27(6):833–834. doi: 10.1002/ca.22396. [DOI] [PubMed] [Google Scholar]
- 23.Marks SC, Jr, Bertman SL, Penney JC. Human anatomy: a foundation for education about death and dying in medicine. Clin Anat. 1997;10(2):118–122. doi: 10.1002/(sici)1098-2353(1997)10:2<118::Aid-ca8>3.0.Co;2-r. [DOI] [PubMed] [Google Scholar]
- 24.Horne DJ, Tiller JW, Eizenberg N, Tashevska M, Biddle N. Reactions of first-year medical students to their initial encounter with a cadaver in the dissecting room. Acad Med. 1990;65(10):645–646. doi: 10.1097/00001888-199010000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Criado-Álvarez JJ, González González J, Romo Barrientos C, Ubeda-Bañon I, Saiz-Sanchez D, Flores-Cuadrado A, et al. Learning from human cadaveric prosections: examining anxiety in speech therapy students. Anat Sci Educ. 2017;10(5):487–494. doi: 10.1002/ase.1699. [DOI] [PubMed] [Google Scholar]
- 26.Romo Barrientos C, Jose Criado-Alvarez J, Gonzalez-Gonzalez J, Ubeda-Banon I, Saiz-Sanchez D, Flores-Cuadrado A, et al. Anxiety among medical students when faced with the practice of anatomical dissection. Anat Sci Educ. 2019;12(3):300–309. doi: 10.1002/ase.1835. [DOI] [PubMed] [Google Scholar]
- 27.Prayson RA, Dannefer EF. Fostering self-reflection on the anatomy laboratory: Dealing with death and the taboo. Anat Sci Educ. 2014;7(5):417–418. doi: 10.1002/ase.1437. [DOI] [PubMed] [Google Scholar]
- 28.Franchi T. The impact of the Covid-19 pandemic on current anatomy education and future careers: a student’s perspective. Anat Sci Educ. 2020;13(3):312–315. doi: 10.1002/ase.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finn GM, Danquah A, Matthan J. Colonization, cadavers, and color: Considering decolonization of anatomy curricula. Anat Rec (Hoboken) 2022;305(4):938–951. doi: 10.1002/ar.24855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Whelan A, Leddy JJ, Mindra S, Matthew Hughes JD, El-Bialy S, Ramnanan CJ. Student perceptions of independent versus facilitated small group learning approaches to compressed medical anatomy education. Anat Sci Educ. 2016;9(1):40–51. doi: 10.1002/ase.1544. [DOI] [PubMed] [Google Scholar]
- 31.Wilson AB, Lazarus MD. Closing a window - opening a door: a response to the letter to the editor. Clin Anat. 2018;31(8):1207–1209. doi: 10.1002/ca.23226. [DOI] [PubMed] [Google Scholar]
- 32.Bentley BS, Hill RV. Objective and subjective assessment of reciprocal peer teaching in medical gross anatomy laboratory. Anat Sci Educ. 2009;2(4):143–149. doi: 10.1002/ase.96. [DOI] [PubMed] [Google Scholar]
- 33.Karunakaran I, Thirumalaikolundusubramanian P, Nalinakumari SD. A preliminary survey of professionalism teaching practices in anatomy education among Indian Medical Colleges. Anat Sci Educ. 2017;10(5):433–443. doi: 10.1002/ase.1679. [DOI] [PubMed] [Google Scholar]
- 34.Wu A, Yu ACX, Chang CS, Goel R, Sagoo MG, Sakurai T, et al. Initiating students’ reflections on life’s passing in the anatomy course - an international observation at 14 universities. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2021:151741. 10.1016/j.aanat.2021.151741. [DOI] [PubMed]
- 35.Wu A, Noël GPJC, Wingate R, Kielstein H, Sakurai T, Viranta-Kovanen S, Chien C-L, Traxler H, Waschke J, Vielmuth F, Sagoo MG, Kitahra S, Kato Y, Keay KA, Olsen J, Bernd P. An international partnership of 12 anatomy departments – improving global health through internationalization of medical education. Ann Glob Health. 2020;86(1):27. doi: 10.5334/aogh.2665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu A. International collaboration and exchange program - preparing global leaders for healthcare. https://www.internationalcollaborationexchange.org. Accessed 2021.
- 37.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: a review for its modernization. Anat Sci Educ. 2010;3(2):83–93. doi: 10.1002/ase.139. [DOI] [PubMed] [Google Scholar]
- 38.Abdulcadir J, Dewaele R, Firmenich N, Remuinan J, Petignat P, Botsikas D, et al. In vivo imaging-based 3-dimensional pelvic prototype models to improve education regarding sexual anatomy and physiology. J Sex Med. 2020;17(9):1590–1602. doi: 10.1016/j.jsxm.2020.05.025. [DOI] [PubMed] [Google Scholar]
- 39.Alharbi Y, Al-Mansour M, Al-Saffar R, Garman A, Alraddadi A. Three-dimensional virtual reality as an innovative teaching and learning tool for human anatomy courses in medical education: a mixed methods study. Cureus. 2020;12(2):e7085. doi: 10.7759/cureus.7085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li QY, Zhang Q, Yan C, He Y, Phillip M, Li F, et al. Evaluating phone camera and cloud service-based 3D imaging and printing of human bones for anatomical education. BMJ Open. 2020;10(2):e034900. doi: 10.1136/bmjopen-2019-034900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyer ER, Cui D. Anatomy visualizations using stereopsis: assessment and implication of stereoscopic virtual models in anatomical education. Adv Exp Med Biol. 2020;1235:117–130. doi: 10.1007/978-3-030-37639-0_7. [DOI] [PubMed] [Google Scholar]
- 42.Murgitroyd E, Madurska M, Gonzalez J, Watson A. 3D digital anatomy modelling - practical or pretty? The surgeon : J Royal Coll Surg Edinburgh and Ireland. 2015;13(3):177–180. doi: 10.1016/j.surge.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 43.Wada Y, Nishi M, Yoshikawa K, Higashijima J, Miyatani T, Tokunaga T, et al. Usefulness of virtual three-dimensional image analysis in inguinal hernia as an educational tool. Surg Endosc. 2020;34(5):1923–1928. doi: 10.1007/s00464-019-06964-y. [DOI] [PubMed] [Google Scholar]
- 44.Boscolo-Berto R, Tortorella C, Porzionato A, Stecco C, Picardi EEE, Macchi V, et al. The additional role of virtual to traditional dissection in teaching anatomy: a randomised controlled trial. Surg Radiol Anat : SRA. 2021;43(4):469–479. doi: 10.1007/s00276-020-02551-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cai B, Rajendran K, Bay BH, Lee J, Yen CC. The effects of a functional three-dimensional (3d) printed knee joint simulator in improving anatomical spatial knowledge. Anat Sci Educ. 2019;12(6):610–618. doi: 10.1002/ase.1847. [DOI] [PubMed] [Google Scholar]
- 46.Dhulipalla R, Marella Y, Katuri KK, Nagamani P, Talada K, Kakarlapudi A. Effect of 3D animation videos over 2D video projections in periodontal health education among dental students. J Int Soc Prev Community Dent. 2015;5(6):499–505. doi: 10.4103/2231-0762.170526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hu A, Wilson T, Ladak H, Haase P, Doyle P, Fung K. Evaluation of a three-dimensional educational computer model of the larynx: voicing a new direction. Journal of otolaryngology - head & neck surgery = Le Journal d'oto-rhino-laryngologie et de chirurgie cervico-faciale. 2010;39(3):315–22. [PubMed]
- 48.Hu KC, Salcedo D, Kang YN, Lin CW, Hsu CW, Cheng CY, et al. Impact of virtual reality anatomy training on ultrasound competency development: a randomized controlled trial. PLoS ONE. 2020;15(11):e0242731. doi: 10.1371/journal.pone.0242731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitrousias V, Varitimidis SE, Hantes ME, Malizos KN, Arvanitis DL, Zibis AH. Anatomy learning from prosected cadaveric specimens versus three-dimensional software: a comparative study of upper limb anatomy. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2018;218:156–64. 10.1016/j.aanat.2018.02.015. [DOI] [PubMed]
- 50.Peterson DC, Mlynarczyk GS. Analysis of traditional versus three-dimensional augmented curriculum on anatomical learning outcome measures. Anat Sci Educ. 2016;9(6):529–536. doi: 10.1002/ase.1612. [DOI] [PubMed] [Google Scholar]
- 51.Van Nuland SE, Rogers KA. The anatomy of E-learning tools: does software usability influence learning outcomes? Anat Sci Educ. 2016;9(4):378–390. doi: 10.1002/ase.1589. [DOI] [PubMed] [Google Scholar]
- 52.Vuchkova J, Maybury TS, Farah CS. Testing the educational potential of 3D visualization software in oral radiographic interpretation. J Dent Educ. 2011;75(11):1417–1425. doi: 10.1002/j.0022-0337.2011.75.11.tb05198.x. [DOI] [PubMed] [Google Scholar]
- 53.Yin MS, Haddawy P, Suebnukarn S, Rhienmora P. Automated outcome scoring in a virtual reality simulator for endodontic surgery. Comput Methods Programs Biomed. 2018;153:53–59. doi: 10.1016/j.cmpb.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 54.Melissa A. Carroll P, MS, Darren S. Hoffmann P, James L. Karnes P, PT, Sheryl L. Sanders P. Gross anatomy during the pandemic - cadaver dissection is essential as a learning tool. In: Anatomy AAf, editor.2020.
- 55.Chen JY, Chan GS, Tsang JP, Tsang GK. The hospital mortuary: learning about death… and life. Med Educ. 2016;50(11):1145–1146. doi: 10.1111/medu.13201. [DOI] [PubMed] [Google Scholar]
- 56.Bamber AR, Quince TA. The value of postmortem experience in undergraduate medical education: current perspectives. Adv Med Educ Pract. 2015;6:159–170. doi: 10.2147/amep.S46669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bamber AR, Quince TA, Barclay SI, Clark JD, Siklos PW, Wood DF. Medical student attitudes to the autopsy and its utility in medical education: a brief qualitative study at one UK medical school. Anat Sci Educ. 2014;7(2):87–96. doi: 10.1002/ase.1384. [DOI] [PubMed] [Google Scholar]
- 58.Conran P, Nowacek G, Adams T, Smith L. Medical students’ attitudes toward the autopsy. Acad Med. 1996;71(6):681–683. doi: 10.1097/00001888-199606000-00026. [DOI] [PubMed] [Google Scholar]
- 59.Kemp WL, Koponen M, Sens MA. Forensic autopsy experience and core entrustable professional activities: a structured introduction to autopsy pathology for preclinical student. Acad Pathol. 2019;6:2374289519831930. doi: 10.1177/2374289519831930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Talmon G. The use of autopsy in preclinical medical education: a survey of pathology educators. Arch Pathol Lab Med. 2010;134(7):1047–1053. doi: 10.5858/2009-0333-oa.1. [DOI] [PubMed] [Google Scholar]
- 61.Robbins BD, Tomaka A, Innus C, Patterson J, Styn G. Lessons from the dead: the experiences of undergraduates working with cadavers. Omega (Westport) 2008;58(3):177–192. doi: 10.2190/om.58.3.b. [DOI] [PubMed] [Google Scholar]
- 62.Alt-Epping B, Lohse C, Viebahn C, Steinbuchel N, Benze G, Nauck F. On death and dying - an exploratory and evaluative study of a reflective, interdisciplinary course element in undergraduate anatomy teaching. BMC Med Educ. 2014;14:15. doi: 10.1186/1472-6920-14-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dickinson GE, Lancaster CJ, Winfield IC, Reece EF, Colthorpe CA. Detached concern and death anxiety of first-year medical students: before and after the gross anatomy course. Clin Anat. 1997;10(3):201–207. doi: 10.1002/(sici)1098-2353(1997)10:3<201::Aid-ca5>3.0.Co;2-w. [DOI] [PubMed] [Google Scholar]
- 64.Tseng WT, Lin YP. “Detached concern” of medical students in a cadaver dissection course: a phenomenological study. Anat Sci Educ. 2016;9(3):265–271. doi: 10.1002/ase.1579. [DOI] [PubMed] [Google Scholar]
- 65.Chiou RJ, Tsai PF, Han DY. Effects of a “silent mentor” initiation ceremony and dissection on medical students' humanity and learning. BMC Res Notes. 2017;10(1):483. doi: 10.1186/s13104-017-2809-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dolan B. Soul searching: a brief history of the mind/body debate in the neurosciences. Neurosurg Focus. 2007;23(1):E2. doi: 10.3171/foc.2007.23.1.2. [DOI] [PubMed] [Google Scholar]
- 67.Hasselkus BR. Keeping body and soul together. The American journal of occupational therapy : official publication of the American Occupational Therapy Association. 2002;56(4):367–368. doi: 10.5014/ajot.56.4.367. [DOI] [PubMed] [Google Scholar]
- 68.Santoro G, Wood MD, Merlo L, Anastasi GP, Tomasello F, Germanò A. The anatomic location of the soul from the heart, through the brain, to the whole body, and beyond: a journey through Western history, science, and philosophy. Neurosurgery. 2009;65(4):633–43; discussion 43. 10.1227/01.Neu.0000349750.22332.6a. [DOI] [PubMed]
- 69.Wragge-Morley A. Imagining the soul: Thomas Willis (1621–1675) on the anatomy of the brain and nerves. Prog Brain Res. 2018;243:55–73. doi: 10.1016/bs.pbr.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 70.Lanoix JP, Toussaint L. Holistic medicine must mean whole: how to deal with spirituality. Adv Mind Body Med. 2021;35(1):9–15. [PubMed] [Google Scholar]
- 71.Drake RL, McBride JM, Pawlina W. An update on the status of anatomical sciences education in United States medical schools. Anat Sci Educ. 2014;7(4):321–325. doi: 10.1002/ase.1468. [DOI] [PubMed] [Google Scholar]
- 72.Drake RL, McBride JM, Lachman N, Pawlina W. Medical education in the anatomical sciences: the winds of change continue to blow. Anat Sci Educ. 2009;2(6):253–259. doi: 10.1002/ase.117. [DOI] [PubMed] [Google Scholar]