Abstract
Patient: Female, 41-year-old
Final Diagnosis: Metastatic breast cancer
Symptoms: Low back pain
Medication:—
Clinical Procedure: —
Specialty: Oncology • Rehabilitation • Traditional Medicine
Objective:
Unusual clinical course
Background:
Breast cancer is the most common cancer in women and the most common cause of spinal metastasis, and it may recur months to years after treatment.
Case Report:
A 41-year-old woman, recovered from breast cancer, presented to a chiropractor with acute-on-chronic 3-week history of low back pain radiating to the right leg. She had seen 2 providers previously; lumbar spondylosis had been diagnosed via radiography. Given her recent symptom progression and cancer history, the chiropractor ordered lumbar magnetic resonance imaging, revealing L5 vertebral marrow replacement, suggestive of metastasis. The chiropractor referred her to an oncologist. While awaiting biopsy and oncologic treatments, the oncologist cleared the patient to receive gentle spinal traction and soft tissue manipulation, which alleviated her back pain. The patient continued radiation and chemotherapy, with low back pain remaining improved over 18 months. A literature review identified 7 previous cases of women presenting to a chiropractor with breast cancer metastasis. Including the current case, most had spinal pain and vertebral metastasis (75%) and history of breast cancer (88%) diagnosed a mean 5±3 years prior.
Conclusions:
This case illustrates a woman with low back pain due to recurrent metastatic breast cancer, identified by a chiropractor, and the utility of a multidisciplinary approach to pain relief during oncologic care. Our literature review suggests that although uncommon, such patients can present to chiropractors with spinal pain from vertebral metastasis and have a known history of breast cancer. Conservative therapies should be used cautiously and under oncologic supervision in such cases.
Keywords: Breast Neoplasms, Chiropractic, Low Back Pain, Neoplasm Metastasis
Background
Breast cancer is the most common cancer in women [1]. It is also the most common cause of spinal metastasis, which most often affects the lumbar spine when it occurs [2,3]. About 18% of women with a history of breast cancer experience at least 1 recurrence of cancer, at a median of 7 years after initial diagnosis [4]. However, the timing of recurrence is highly variable and can range from months to years after treatment [4,5]. Accordingly, clinicians must be aware of the possibility of recurrent breast cancer as a cause of low back pain.
In Hong Kong, the site of the present study, the mean age of diagnosis of breast cancer is 53 years [6]. Breast cancer is less common in Hong Kong than in other westernized countries, with an age-standardized incidence rate of 59 cases per 100 000, compared with the United States, which has a rate of 95 per 100 000 [6]. However, the incidence of breast cancer has been projected to increase in Hong Kong [7]. In general, many of the risk factors for breast cancer identified in Asian countries, such as smoking and obesity, are consistent with risk factors identified in other areas of the world [6].
Clinicians must have a high index of suspicion regarding any new-onset pain among patients with a history of breast cancer [8,9]. A history of cancer is more predictive of current malignancy in patients with low back pain than any other patient-reported symptom (positive likelihood ratio of 7.3) [10,11]. Further, one study found that certain new-onset symptoms were associated with recurrence of cancer in general, such as low back pain (odds ratio of 4.2), flank pain, vomiting, edema, and chest pain [9].
Chiropractors are health care providers that treat neuromusculoskeletal disorders, the most common of which is low back pain [12]. Accordingly, these providers rarely encounter patients with undiagnosed malignancy [13,14]. Although such encounters occur about once every 8 years in practice [13], malignancy is important to identify given the potential morbidity when it is undiagnosed and untreated. This case highlights the role of the chiropractor in identifying recurrent metastatic breast cancer and communicating clinical findings to the oncology team.
Case Report
Patient Information
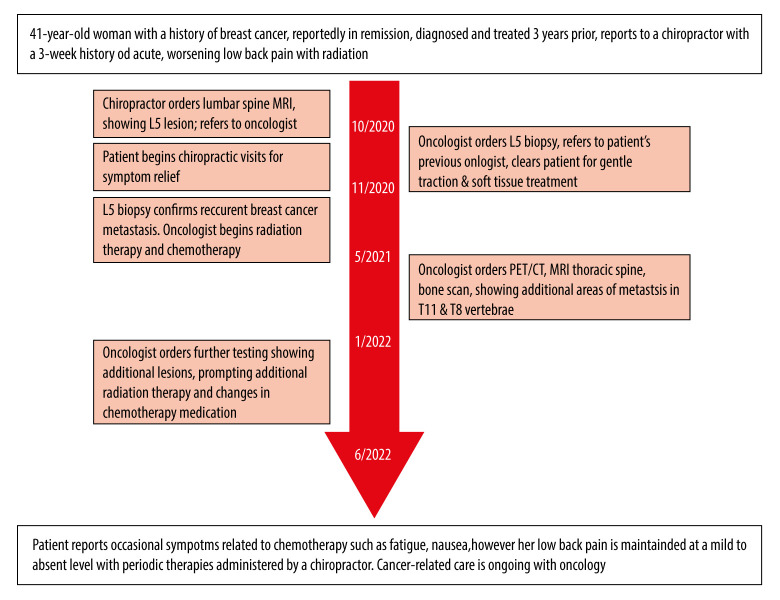
A 41-year-old woman presented to a chiropractor with a 3-week history of sudden-onset constant low back pain with associated intermittent right lower extremity pain, rated 6 out of 10 in severity on the numeric pain rating scale (Figure 1). Her symptoms were exacerbated when lifting or holding heavy objects, especially when squatting down to lift. Her World Health Organization Quality-of-Life Scale score was 72%. She denied any pain waking her at night, unintentional weight loss, fever, chills, fatigue, and bladder or bowel disturbances. She endorsed a history of breast cancer but denied having trauma or other illnesses. The patient was very active, and had engaged in hiking, swimming, and Tai Chi for several years. She had 2 children, was a nonsmoker, and had no family history of cancer.
Figure 1.
Timeline of care. MRI – magnetic resonance imaging; PET/CT – positron emission tomography computed tomography.
The patient’s breast cancer had been diagnosed 3 years prior at age 35, and was treated with a modified radical mastectomy with reconstruction using a transverse rectus abdominus flap procedure and 4 cycles of adjuvant dose-dense chemo-therapy using adriamycin and cyclophosphamide, followed by 4 cycles of paclitaxel and trastuzumab. At the time, she tested negative for HER2 and breast cancer type 1 susceptibility proteins, and her Ki-67 marker was low (<15%). The patient had received a clinical diagnosis of a breast cancer tumor between 2 and 5 cm and metastasis in 1 to 3 axillary lymph nodes, with no identified distant metastasis, yielding a classification of malignant tumors for tumors, nodes, and metastases (TNM) of cT2N1M0. She had undergone routine follow-ups for breast cancer after treatment every 6 months, which included mammography, chest radiographs, and blood and urine testing, and was reportedly declared to be in remission from breast cancer for over 6 months prior to presentation to the chiropractor. At the time of her presentation to the chiropractor, she was no longer being prescribed chemotherapy medications and had not undergone any recent advanced imaging.
The patient first had intermittent episodes of localized, mild low back pain 16 months prior. The patient accordingly visited her primary care provider as well as a sports medicine provider for evaluation at that time. The sports medicine provider performed radiography, the report of which noted a mild levo-convex thoracolumbar curvature and degenerative changes of the lumbar spine; however, there was no mention of possible metastasis. The provider diagnosed degenerative spondylosis and referred the patient for physical therapy.
The patient’s symptoms progressed acutely over the 3 weeks preceding her initial chiropractic visit and were now accompanied by radiating pain down to the right leg, including the calf, shin, and foot, with mild tingling diffusely in the foot. Over-the-counter nonsteroidal anti-inflammatory drugs did not provide any relief. Given these worsening symptoms, she sought a chiropractor for another opinion.
Clinical Findings
Upon examination by the chiropractor, the patient appeared physically fit. Her active thoracolumbar range of motion was normal and painless. However, passive lumbar extension and right lateral lumbar flexion exacerbated her low back pain. Spinal palpation revealed tenderness and stiffness at the L4/5 and L5/S1 segments. Muscle palpation revealed hypertonicity of the quadratus lumborum and lumbar paraspinal muscles bilaterally. A neurological examination was normal, including lower extremity muscle stretch reflexes, sensation, and muscle strength testing. The right straight leg raise was restricted, which provoked a tightness sensation in the right hamstring.
The chiropractor initially suspected lumbar disc displacement as the working diagnosis. However, given the patient’s history of cancer and acute-onset pain without trauma, which had progressed despite conservative care, the chiropractor ordered lumbar spine magnetic resonance imaging (MRI) to evaluate for potential metastasis, which was performed the same day in the facility’s imaging center.
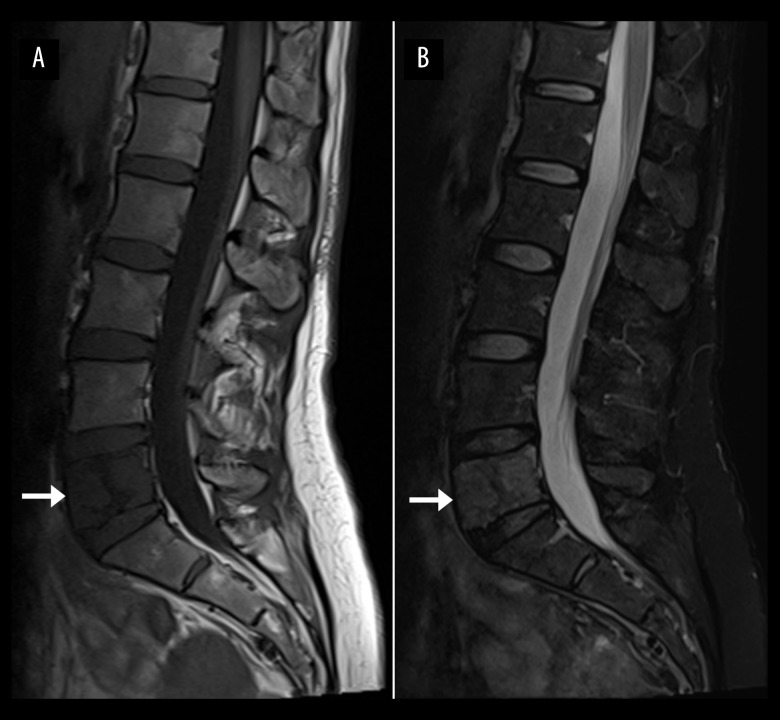
The lumbar spine MRI revealed bone marrow replacement at the L5 vertebral body extending into the right L5 pedicle, suggestive of metastasis (Figure 2). In addition, mild disc bulges at L4/5 and L5/S1 were noted, each 2 mm in anteroposterior dimension from the disc margin, with no central or neuroforaminal stenosis present. There was no evidence of pathological fracture. Given the potential metastasis, the chiropractor referred the patient to an oncologist employed within the same healthcare organization and consulted with this specialist regarding the patient.
Figure 2.
Lumbar spine magnetic resonance imaging. T1-weighted (A) and fat-suppressed T2-weighted (B) mid-sagittal views, showing marrow replacement of the entire L5 vertebral body, indicated by an abnormal heterogenous T1-weighted hypointense, T2-weighted hyperintense marrow signal change (arrows). The marrow change also extends into the right L5 pedicle (not shown).
The oncologist concluded that the L5 lesion likely represented recurrent metastasis from the patient’s previous breast cancer and scheduled a follow-up visit with the patient. The oncolo-gist informed the patient that she may have a metastatic lesion in her lower back and suggested prescription pain medications until further testing and treatment could be carried out. In addition, the patient was scheduled for a biopsy of the L5 lesion and was referred to her previous oncology team with whom she scheduled an appointment the following month.
The patient preferred to avoid taking pain medications. Given her predilection toward conservative care and a delay in obtaining follow-up oncology testing and treatment, the oncologist approved of a treatment regimen in the interim. This consisted of low force mechanical spinal traction and soft tissue manipulation, as means of providing the patient relief in a gentle manner. Traction was chosen to help gently unload the patient’s lumbar spine, placing her in a position of relief, considering her symptoms were exacerbated by increased spinal loading while upright. Accordingly, the conservative care was administered after providing informed consent of the available options and was arrived at through shared decision-making of the patient, chiropractor, and an oncologist.
The chiropractic treatments began the first full week after the patient’s initial presentation. She received intermittent motorized lumbar traction (MID spine decompression device, WIZ Medical, Korea) daily for 6 consecutive days with sessions lasting 20 min (Figure 3). The patient was positioned supine, the ratio of hold to rest time was 2: 1, and traction force was set to a quarter of the patient’s body weight (ie, 25% of 50 kg, or 13 kg). Typically, a traction force of 30% to 60% of body weight is used for low back pain [15]. However, given the circumstances of the patient’s likely metastasis, a value below the lowest typical threshold was used as a safety precaution. The patient reported relief in the traction position, and this therapy was supervised by the treating chiropractic clinician.
Figure 3.

Demonstration of mechanical traction (MID spine decompression device, WIZ Medical, Korea).
The chiropractor also administered instrument-assisted soft tissue manipulation, also called scraping therapy or gua sha (Strig, massage device, Korea) to help reduce the patient’s low back pain and muscle hypertonicity (Figure 4). After the first week of treatment, the patient reported her pain severity had reduced to a 2 out of 10. Subsequent chiropractic treatment sessions were reduced in frequency as the patient’s low back pain improved, to 3 visits per week for 3 weeks, then 1 visit per week for 6 months. The patient was encouraged to stay active with swimming, hiking, and Tai Chi to tolerance yet to avoid heavy lifting and spinal loading.
Figure 4.

Administration of instrument-assisted soft tissue manipulation. The practitioner applies a thin layer of emollient/lotion to the patient’s skin then gently strokes the massage tool (Strig, Korea) across the skin surface (arrows).
Exactly 2 weeks after initial presentation, the oncologist conducted a computed tomography (CT)-guided core biopsy of the L5 vertebral lesion (Figure 5). Histopathological testing identified malignant cells, consistent with a diagnosis of metastatic adenocarcinoma/ductal carcinoma, which confirmed a recurrence of the patient’s breast cancer. The oncologist preferred that the patient’s original oncology team treat the patient because they were more familiar with her course of care over the past 3 years and relayed these results to the outside hospital where she was treated previously.
Figure 5.
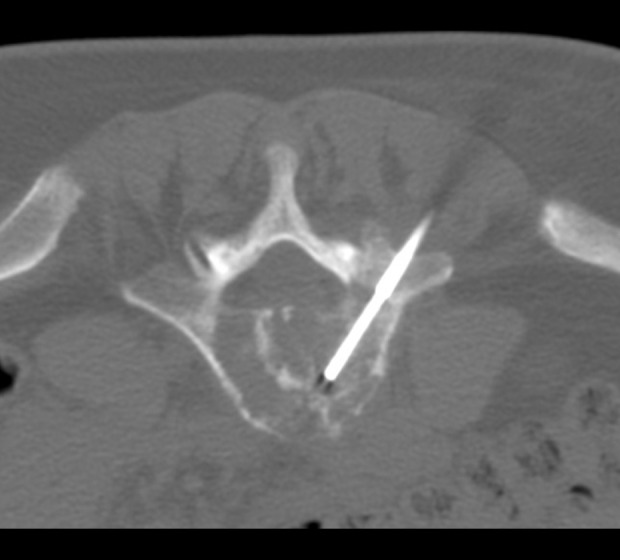
Intra-procedural axial section of the computed tomography-guided biopsy of the L5 vertebra.
Further testing of the biopsy indicated the tumor was estrogen receptor positive, with an Allred score of 7 of a maximum 8 and H-score of 170 of a maximum 300. Testing for the progesterone receptor was negative. Expression of c-erbB2 oncoprotein was equivocal, with weak membranous staining for the c-erbB2 oncoprotein in more than 10% of the tumor cells (score 2/3). About 6% of the tumor cell nuclei expressed the proliferation marker Ki-67, indicating a low proliferative activity.
At 18 days after the patient’s initial presentation, she visited her previous oncologist, who performed a bone scan that revealed no additional sites of metastasis. Radiation therapy was initiated at an absorbed dose of 4 Gray over 5 consecutive days and was directed to the region spanning the vertebral segments T12 to S1. This was followed by the administration of letrozole and ribociclib.
At 5 months after initial presentation, the oncologist ordered an F18-fluorodeoxyglucose positron emission tomography CT (F18-FDG PET/CT) scan which revealed increased metabolic activity in the T11 vertebra, suggestive of an additional site of metastasis, as well as heightened activity in the previously identified L5 vertebra. The oncologist then ordered an MRI of the thoracic spine, which again showed the lesion in T11 and identified a new area of concern in the T8 vertebral body, measuring 0.57×0.49×0.53 cm, suggestive of an early meta-static lesion. This was followed up by a bone scan, which revealed no additional sites of metastasis.
At 7 months after initial presentation, the patient’s low back pain and radiating leg pain were almost completely resolved. Her low back pain was mild and occasional at this point, but when it occurred it was quickly resolved after soft tissue manipulation and traction. She also occasionally had transient myalgia, fatigue, nausea, and vomiting, likely related to the chemotherapy treatments. She remained under chiropractic care once per month for the next 12 months, which included ongoing soft tissue manipulation and mechanical traction. The chiropractor also introduced rehabilitative exercises including cat-cow, bird-dog, and gluteal bridge exercises (Figure 6).
Figure 6.

Demonstration of gluteal bridge exercise. The patient begins supine with the back flat against the table, then raises the back and hips to the elevated position shown.
At 14 months after initial patient presentation, the oncologist ordered a brain MRI, which was unremarkable. The oncologist also ordered another F18-FDG PET/CT scan, which revealed a new lesion in the liver, consistent with metastasis. The activity, measured by the standardized uptake values, of the L5 and T11 vertebral lesions had reduced; however, there were new skeletal lesions in the left femur, right 1st rib, and right inferior pubic ramus and continued activity at the T8 vertebra. Given these new lesions, the oncologist changed the chemotherapy regimen to exemestane and everolimus. Despite the presence of new skeletal lesions, the patient did not develop any new symptoms or bone pain in the femur, ribcage, pelvis, or mid-back.
At 18 months after patient presentation, a follow-up with an MRI of the upper abdomen showed no evidence of liver metastasis, while the T8, T11, and L5 lesions were re-demonstrated. A repeat bone scan revealed a new lesion in the left 9th and right 6th ribs, while the L5 and femoral lesions were considered stable. The patient was accordingly treated with further radiation therapy.
At 20 months after presentation, the patient remained under the care of her oncologist and continued undergoing additional testing and treatments. Throughout the course of care and follow-up, the patient remained active with a modified exercise program and continues hiking, swimming, and doing Tai Chi in addition to the exercises shown to her by the chiropractor. The patient provided written consent for publication of this case report and any accompanying images. This case report was prepared according to the Case Report Guidelines (CARE) and checklist [16].
Discussion
This case illustrates a young, otherwise healthy woman with acute progressive low back pain that was ultimately diagnosed as recurrent metastatic breast cancer via the aid of a chiropractor. Because the patient had prior episodes of mild low back pain, it is possible that she had a site of metastasis in the L5 vertebra for months that was previously undetected by radiography. However, radiographs are a poor screening tool for cancer, as 50% of bone mineral must be lost before a metastatic lesion can be identified [17]. Upon presenting to the chiropractor, the patient demonstrated various red flags in addition to her history of cancer, such as a change in the character of her pain and increasing pain that was unresponsive to pain medications [18], which further justified the use of lumbar MRI that ultimately revealed the relevant pathology in her low back.
The patient’s low back pain was likely related to her L5 metastatic lesion. Although she had 2 lumbar disc bulges, these were relatively small and there was no neuroforaminal or central canal stenosis [19]. Sclerotomal pain referral from the L5 lesion could have accounted for her symptoms, as this has been suggested as a mechanism for pseudo-radicular lower extremity pain occurring in patients with vertebral metastasis [20].
The treatment for low back pain in the current case differs from other options that have been reported in the literature, such as NSAIDs, opioids [21], and steroids [22]. Because the patient preferred to avoid pain medications, an alternative conservative option was offered. We suggest that the patient’s rapid improvement in pain was due to the combination of spinal traction and soft tissue manipulation, considering that she obtained this relief prior to initiating chemotherapy and radiation therapy. We believe the relief afforded by gentle traction was related to unloading her upper body weight from the L5 spinal lesion, which appeared sensitive to increased loading. Further, the instrument-assisted soft tissue manipulation may suppress nociceptive signals (ie, pain) [23], which could have inhibited sclerotomal pain arising from the L5 lesion.
According to a search of PubMed, Google Scholar, the Index to Chiropractic Literature, and recent review papers [24–26] on June 19, 2022, we identified 7 previously published cases of patients that presented to a chiropractor with previously undiagnosed breast cancer metastasis [27–33]. In addition to the current case (total 8 cases), the mean patient age was 54±17 years, with all patients being women and 6 of 8 (75%) presenting with spinal pain (Table 1).
Table 1.
Patients with undiagnosed breast cancer metastasis presenting to a chiropractor.
| Author | Year | Patient age (years) | Symptoms | Breast cancer history | Initial means of diagnosis | Region(s) of skeletal metastasis* |
|---|---|---|---|---|---|---|
| Boysen | 2016 | 44 | LBP with radiation to hip | Yes. In remission for 3 years. Further details unclear | MRI (region unclear) | Acetabulum |
| Conley | 1983 | 54 | Shoulder & arm pain | Yes. Mastectomy 5 years prior | Thoracic & lumbar radiographs | Ilium, thoracic spine, hip |
| Current case | 2022 | 41 | LBP and leg pain | Yes, 3 years prior. Had mastectomy, chemotherapy, radiation. Remission >6 months | Lumbar MRI | L5 |
| Grilliot | 1983 | 76 | Mid-thoracic pain | Yes, 7 years prior. Had mastectomy | Chest and thoracic radiographs | T9, T10 |
| Grod | 1994 | 46 | LBP with radiation to leg | Yes, 2 years prior. Had mastectomy, normal bone scans | Lumbar radiographs | L2 |
| Kahn | 2017 | 27 | LBP, lack of response to care | No | Lumbar MRI | L1, L2 |
| Kanga | 2015 | 65 | Cervical, mid-thoracic, and LBP, pressure in head | Yes, 4 years prior. Treated with chemotherapy, recent negative whole-body CT | PCP referral & subsequent brain MRI, CT thorax | T9, L1 |
| Osterhouse | 2004 | 80 | Lower extremity pain, fatigue, anorexia | Yes, 12 years ago. Reportedly in remission. Further details unclear | Cancer antigen 27–29, ankle radiographs | Ankle |
Region of skeletal metastasis upon presentation to the chiropractor. CT – computed tomography; F – Female; LBP – low back pain; MRI – magnetic resonance imaging; M – male; NR – not reported; PCP – primary care provider.
All patients (8/8, 100%) had skeletal metastasis, which involved the thoracolumbar spine in 6 of 8 (75%) patients. Seven of 8 patients (88%) had a history of breast cancer, which was diagnosed a mean 5±3 years previously. Imaging was used to aid in identification of the potential metastasis in each case, whether performed by the chiropractor or after referral. The clinical features of the present case match the typical pattern identified in the literature with respect to the presence of spine pain, vertebral metastasis, and a history of breast cancer within the past few years.
When a patient with a history of cancer presents with new low back pain, clinicians should consider ordering lumbar MRI rather than CT or radiography [34]. Further, MRI without and with contrast can be optimal; however, this requires consideration of potential kidney disease or other adverse exceptions for the use of contrast [34]. In the setting of the present case (Hong Kong) and in the United States, chiropractors are able to order MRI [35,36]. In regions where the scope of practice does not permit this, chiropractors could alternatively refer patients suspected of metastasis to a medical physician.
Recent studies have examined the utility of rehabilitation programs including exercise and manual therapies for patients with breast cancer; however, these have focused mostly on treatment of shoulder and upper extremity complaints following mastectomy [37,38]. Conversely, less is known about multidisciplinary care for back pain in those with recurrent breast cancer metastasis affecting the spine. Given this lack of research, conservative care was administered with caution in the present case.
Although spinal metastasis has been listed as a contraindication to spinal traction [39], we are unaware of any evidence that this therapy is dangerous or associated with adverse outcomes. Manual traction has previously been reported in a case of spinal metastasis with no apparent adverse effects [40]. In fact, partial body weight pull ups, which can have a comparable effect on the spine as low-force traction as used in the present case, are a recommended rehabilitation exercise for those with spine metastasis, as they involve a low spinal load [41].
In general, patients with spinal metastasis should avoid exercises that increase spinal load [42]. Although evidence is limited regarding the optimal exercise regimen [42], a recent study found that certain spine stabilization exercises, similar to those provided in the present study, can be safe and do not increase the risk of pathological spinal fracture [43]. Research regarding instrument-assisted soft tissue manipulation in those with spinal neoplasm is also limited [44]. However, one study which included patients with spine metastasis found that massage therapy, a similar technique, could be safely administered and also led to significant reductions in pain [45].
Despite the apparent success and safety of gentle mechanical traction, soft tissue manipulation, and exercises in this case, there is overall limited evidence that these therapies safely reduce pain in patients with spinal metastasis. Further studies should examine the effectiveness and safety of these therapies as add-ons to chemotherapy in such patients. Currently, these therapies cannot be broadly recommended, and practitioners interested in administering these modalities should discuss their safety and utility with the patient’s oncologist on a case-by-case basis.
Limitations
As a single case report, these results are not generalizable. First, the patient was generally in good health aside from the breast cancer, being young and physically fit. These factors could have also contributed to a better improvement with therapies. Second, while she initially responded positively to conservative therapies, her long-term relief from low back pain could be attributed to effects of the radiation therapy or chemotherapy. Third, several tests were unavailable from the oncologist at the outside hospital. Apart from imaging reports, prior and follow-up advanced imaging were often unavailable from the patient’s outside hospital.
Conclusions
This case presents a woman with low back pain and a history of breast cancer who was diagnosed as having recurrent breast metastasis via the aid of a chiropractor. In addition, her low back pain responded positively to a regimen of gentle traction and manual therapy while she awaited further oncologic testing and treatment. The present case and literature review suggest that chiropractors rarely encounter patients with recurrent breast metastasis months to years after their initial diagnosis, and that these patients typically present with spinal pain caused by vertebral metastasis. Chiropractors should refer any patient with suspected metastasis to an oncologist for care. There is limited evidence to guide conservative or manual therapies for pain in these patients, and any such treatments must be considered carefully through a team approach on a case-by-case basis.
Acknowledgments
We thank Sheryl Walters, MLS, for her assistance in obtaining chiropractic case reports for our literature review.
Footnotes
Department and Institution Where Work Was Done
New York Chiropractic and Physiotherapy Centre, EC Healthcare, Kowloon, Hong Kong.
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.Momenimovahed Z, Salehiniya H. Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer (Dove Med Press) 2019;11:151–64. doi: 10.2147/BCTT.S176070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maccauro G, Spinelli MS, Mauro S, et al. Physiopathology of spine metastasis. Int J Surg Oncol. 2011;2011:107969. doi: 10.1155/2011/107969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaberg J, Gainor BJ. A profile of metastatic carcinoma of the spine. Spine. 1985;10:19–20. doi: 10.1097/00007632-198501000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Lafourcade A, His M, Baglietto L, Boutron-Ruault M-C, et al. Factors associated with breast cancer recurrences or mortality and dynamic prediction of death using history of cancer recurrences: The French E3N cohort. BMC Cancer. 2018;18:171. doi: 10.1186/s12885-018-4076-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riggio AI, Varley KE, Welm AL. The lingering mysteries of metastatic recurrence in breast cancer. Br J Cancer. 2021;124:13–26. doi: 10.1038/s41416-020-01161-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Youn HJ, Han W. A review of the epidemiology of breast cancer in asia: focus on risk factors. Asian Pac J Cancer Prev. 2020;21(4):867–80. doi: 10.31557/APJCP.2020.21.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong IOL, Schooling CM, Cowling BJ, Leung GM. Breast cancer incidence and mortality in a transitioning Chinese population: Current and future trends. Br J Cancer. 2015;112:167–70. doi: 10.1038/bjc.2014.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carty NJ, Foggitt A, Hamilton CR, et al. Patterns of clinical metastasis in breast cancer: An analysis of 100 patients. Eur J Surg Oncol. 1995;21:607–8. doi: 10.1016/s0748-7983(95)95176-8. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton W, Barrett J, Stapley S, Sharp D, Rose P. Clinical features of metastatic cancer in primary care: A case-control study using medical records. Br J Gen Pract. 2015;65:e516–22. doi: 10.3399/bjgp15X686077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maselli F, Palladino M, Barbari V, et al. The diagnostic value of Red Flags in thoracolumbar pain: A systematic review. Disabil Rehabil. 2022;44(8):1190–206. doi: 10.1080/09638288.2020.1804626. [DOI] [PubMed] [Google Scholar]
- 11.Premkumar A, Godfrey W, Gottschalk MB, Boden SD. Red flags for low back pain are not always really red: a prospective evaluation of the clinical utility of commonly used screening questions for low back pain. J Bone Joint Surg Am. 2018;100(5):368–74. doi: 10.2106/JBJS.17.00134. [DOI] [PubMed] [Google Scholar]
- 12.Beliveau PJH, Wong JJ, Sutton DA, et al. The chiropractic profession: A scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropr Man Ther. 2017;25:35. doi: 10.1186/s12998-017-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daniel DM, Ndetan H, Rupert RL, Martinez D. Self-reported recognition of undiagnosed life threatening conditions in chiropractic practice: A random survey. Chiropr Man Ther. 2012;20:1–6. doi: 10.1186/2045-709X-20-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Himelfarb I, Hyland J, Ouzts N, et al. National Board of Chiropractic Examiners: Practice analysis of chiropractic 2020 [Internet] Greeley, CO: NBCE; 2020. Available from: https://www.nbce.org/practice-analysis-of-chiropractic-2020/ [cited 2020 Nov 7] [Google Scholar]
- 15.Meszaros TF, Olson R, Kulig K, et al. Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain. J Orthop Sports Phys Ther. 2000;30:595–601. doi: 10.2519/jospt.2000.30.10.595. [DOI] [PubMed] [Google Scholar]
- 16.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: Consensus-based clinical case reporting guideline development. J Med Case Rep. 2013;7:223. doi: 10.1186/1752-1947-7-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah LM, Salzman KL. Imaging of spinal metastatic disease. Int J Surg Oncol. 20112011 doi: 10.1155/2011/769753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zheng A, Rocos B. Metastatic spinal disease: current concepts. Bone Joint 360. 2022;11:769753. [Google Scholar]
- 19.Suri P, Boyko EJ, Goldberg J, et al. Longitudinal associations between incident lumbar spine MRI findings and chronic low back pain or radicular symptoms: Retrospective analysis of data from the longitudinal assessment of imaging and disability of the back (LAIDBACK) BMC Musculoskelet Disord. 2014;15:1. doi: 10.1186/1471-2474-15-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caraceni A, Zecca E, Formaglio F, Ricchini F. Bone metastases from prostate cancer: From symptom control to pain palliation Bone Metastases from Prostate Cancer. Springer; 2017. pp. 251–70. [Google Scholar]
- 21.Hara S. Opioids for metastatic bone pain. Oncology. 2008;74:52–54. doi: 10.1159/000143219. [DOI] [PubMed] [Google Scholar]
- 22.Yousef AAA, El-mashad NM. Pre-emptive value of methylprednisolone intravenous infusion in patients with vertebral metastases. A double-blind randomized study. J Pain Symptom Manage. 2014;48:762–69. doi: 10.1016/j.jpainsymman.2013.12.232. [DOI] [PubMed] [Google Scholar]
- 23.Chu ECP, Wong AYL, Sim P, Krüger F. Exploring scraping therapy: Contemporary views on an ancient healing – a review. J Family Med Prim Care. 2021;10:2757. doi: 10.4103/jfmpc.jfmpc_360_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alcantara J, Alcantara JD, Alcantara J. The chiropractic care of patients with cancer: A systematic review of the literature. Integr Cancer Ther. 2012;11:304–12. doi: 10.1177/1534735411403309. [DOI] [PubMed] [Google Scholar]
- 25.Laoudikou MT, McCarthy PW. Patients with cancer. Is there a role for chiropractic? J Can Chiropr Assoc. 2020;64:32. [PMC free article] [PubMed] [Google Scholar]
- 26.Trager RJ, Dusek JA. Chiropractic case reports: A review and bibliometric analysis. Chiropr Man Therap. 2021;29:17. doi: 10.1186/s12998-021-00374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conley R, Longnecker R. Metastatic carcinoma. ACA J Chiropr. 1983;20:71–74. [Google Scholar]
- 28.Grilliot J, Danz J. Metastatic carcinoma. ACA J Chiropr. 1983;20:71–72. [Google Scholar]
- 29.Boysen J. Occult breast cancer metastasis masked by musculoskeletal pain in the hip: A case report. J Chiropr Educ [Internet] 2016. p. 70. Available from: [cited 2022 Jun 19] [DOI]
- 30.Grod JP, Crowther ER. Metastatic bone disease secondary to breast cancer: An all too common cause of low back pain. J Can Chiropr Assoc. 1994;38:139–45. [Google Scholar]
- 31.Kahn EA. A Young Female Athlete With Acute Low Back Pain Caused by Stage IV Breast Cancer. J Chiropr Med. 2017;16:230. doi: 10.1016/j.jcm.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanga I, Steiman I. Chiropractic management of a patient with breast cancer metastases to the brain and spine: A case report. J Can Chiropr Assoc. 2015;59:269. [PMC free article] [PubMed] [Google Scholar]
- 33.Osterhouse MD, Guebert GM. Bilateral acrometastasis secondary to breast cancer. J Manipulative Physiol Ther. 2004;27:275–79. doi: 10.1016/j.jmpt.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 34.Davis PC, Wippold II FJ, Brunberg JA, et al. ACR Appropriateness Criteria® on low back pain. J Am Coll Radiol. 2009;6:401–7. doi: 10.1016/j.jacr.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 35.Chang M. The chiropractic scope of practice in the United States: A cross-sectional survey. J Manipulative Physiol Ther. 2014;37:363–76. doi: 10.1016/j.jmpt.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 36.Leung KY, Chu E. Hong Kong chiropractic survey: Analysis of data. Asia- Pac J Chiropr. 2021:2. [Google Scholar]
- 37.Paolucci T, Bernetti A, Bai AV, et al. Two different rehabilitative protocols in comparison. Eur J Phys Rehabil Med. 2020;57:137–47. doi: 10.23736/S1973-9087.20.06138-9. [DOI] [PubMed] [Google Scholar]
- 38.Paolucci T, Bernetti A, Bai AV, et al. The sequelae of mastectomy and quadrantectomy with respect to the reaching movement in breast cancer survivors: Evidence for an integrated rehabilitation protocol during oncological care. Support Care Cancer. 2021;29:899–908. doi: 10.1007/s00520-020-05567-x. [DOI] [PubMed] [Google Scholar]
- 39.Pellecchia GL. Lumbar traction: A review of the literature. J Orthop Sports Phys Ther. 1994;20(5):262–67. doi: 10.2519/jospt.1994.20.5.262. [DOI] [PubMed] [Google Scholar]
- 40.Mabry LM, Ross MD, Tonarelli JM. Metastatic cancer mimicking mechanical low back pain: A case report. J Man Manip Ther. 2014;22:162–69. doi: 10.1179/2042618613Y.0000000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Molinares DM, Huang LY. Rehabilitation principles in bone metastasis. Oper Tech Orthop. 2021;31:100900. [Google Scholar]
- 42.Guo Y, Ngo-Huang AT, Fu JB. Perspectives on spinal precautions in patients who have cancer and spinal metastasis. Phys Ther. 2020;100:554–63. doi: 10.1093/ptj/pzz178. [DOI] [PubMed] [Google Scholar]
- 43.Sprave T, Rosenberger F, Verma V, et al. Paravertebral muscle training in patients with unstable spinal metastases receiving palliative radiotherapy: An exploratory randomized feasibility trial. Cancers (Basel) 2019;11(11):1771. doi: 10.3390/cancers11111771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chu EC-P, Trager RJ, Chen ATC. Conservative management of low back pain related to an unresectable aggressive sacral hemangioma: A case report. Am J Case Rep. 2022;23:e936984. doi: 10.12659/AJCR.936984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jane S-W, Wilkie DJ, Gallucci BB, et al. Effects of a full-body massage on pain intensity, anxiety, and physiological relaxation in taiwanese patients with metastatic bone pain: A pilot study. J Pain Symptom Manage. 2009;37:754–63. doi: 10.1016/j.jpainsymman.2008.04.021. [DOI] [PubMed] [Google Scholar]