Summary
Background
More than 50 000 people participated in the rescue and recovery work that followed the Sept 11, 2001 (9/11) attacks on the World Trade Center (WTC). Multiple health problems in these workers were reported in the early years after the disaster. We report incidence and prevalence rates of physical and mental health disorders during the 9 years since the attacks, examine their associations with occupational exposures, and quantify physical and mental health comorbidities.
Methods
In this longitudinal study of a large cohort of WTC rescue and recovery workers, we gathered data from 27 449 participants in the WTC Screening, Monitoring, and Treatment Program. The study population included police officers, firefighters, construction workers, and municipal workers. We used the Kaplan-Meier procedure to estimate cumulative and annual incidence of physical disorders (asthma, sinusitis, and gastro-oesophageal reflux disease), mental health disorders (depression, post-traumatic stress disorder [PTSD], and panic disorder), and spirometric abnormalities. Incidence rates were assessed also by level of exposure (days worked at the WTC site and exposure to the dust cloud).
Findings
9-year cumulative incidence of asthma was 27·6% (number at risk: 7027), sinusitis 42·3% (5870), and gastro-oesophageal reflux disease 39·3% (5650). In police officers, cumulative incidence of depression was 7·0% (number at risk: 3648), PTSD 9·3% (3761), and panic disorder 8·4% (3780). In other rescue and recovery workers, cumulative incidence of depression was 27·5% (number at risk: 4200), PTSD 31·9% (4342), and panic disorder 21·2% (4953). 9-year cumulative incidence for spirometric abnormalities was 41·8% (number at risk: 5769); three-quarters of these abnormalities were low forced vital capacity. Incidence of most disorders was highest in workers with greatest WTC exposure. Extensive comorbidity was reported within and between physical and mental health disorders.
Interpretation
9 years after the 9/11 WTC attacks, rescue and recovery workers continue to have a substantial burden of physical and mental health problems. These findings emphasise the need for continued monitoring and treatment of the WTC rescue and recovery population.
Funding
Centers for Disease Control and Prevention and National Institute for Occupational Safety and Health.
Introduction
More than 50 000 people worked on the rescue and recovery effort that followed the terrorist attack on the World Trade Center (WTC) on Sept 11, 2001 (9/11).1 This population was highly diverse; it included first responders such as firefighters, police officers, and paramedics, but also included operating engineers, iron workers, railway tunnel workers, telecommunications workers, sanitation workers, medical examiner staff, and volunteers, many of whom had no training in response to civil disasters.2 These individuals were involved in rescue-and-recovery operations and clean-up of debris and restoration of essential services. They worked at Ground Zero, the WTC site, and also at barge-loading piers, vehicle cleaning stations, the landfill destinations for debris, and the medical examiner’s office.
WTC rescue and recovery workers were exposed to a complex mix of airborne toxins.3 Burning jet fuel from the hijacked airliners released a dense plume of black smoke containing benzene, other volatile organics, metals, and polycyclic aromatic hydrocarbons. The collapse of the towers pulverised building materials and created a dense cloud of dust that contained particulates, glass fibres, asbestos, lead, hydrochloric acid, polychlorinated biphenyls, organochlorine pesticides, and polychlorinated dioxins and furans.4 These workers were also exposed to psychological stressors: long work shifts, fear for personal safety, and exposure to body parts.2
Several studies have described the health problems that developed in rescue and recovery workers in the first months and years after 9/11. These problems included sinusitis, new-onset cough, wheeze, gastro-oesophageal reflux disease, depression, post-traumatic stress disorder (PTSD), panic disorder, and other pulmonary illnesses.2, 5-10
Despite this abundance of information on short-term and mid-term physical and mental health disorders in WTC rescue and recovery workers,6,10,11 additional data on the long-term trajectories of these disorders are unknown. We aimed to assess the cumulative incidence and current prevelance of physical and mental health disorders over the 9 years since the WTC attacks, examine their associations with occupational exposures, and quantify comorbidities within and between physical and mental health problems. Such information is needed to guide the care of WTC rescue and recovery workers and to plan responses to future disasters.
Methods
Study population
In this longitudinal cohort, the study population consisted of 27 449 WTC rescue and recovery workers who participated in the WTC Screening, Monitoring, and Treatment Program. Workers included in this analysis (ie, those who worked in protective services or military, construction, electrical or telecommunication repair, transportation or material moving, other occupations, or were unemployed or retired) were enrolled between July 16, 2002, and Sept 11, 2010. Eligible WTC responders were those who had worked or volunteered in lower Manhattan, or the Staten Island landfill or barge-loading piers for 4 h or more from 9/11 to Sept 14, 2001, 24 h or more during September, 2001, or 80 h or more from September, 2001, to December, 2001. Members of the Office of the Chief Medical Examiner who processed human remains were also eligible, as were workers from the Port Authority Trans Hudson Corporation who were engaged in cleaning tunnels for 24 h or more from 9/11 to July 1, 2002 (additional details of the programme have been described previously).12 Members of the Fire Department of the City of New York (FDNY) were assessed by a parallel programme13 and thus, not represented in our cohort. Similarly, the New York City Department of Health established a registry with interview data gathered from rescue and recovery workers and lower Manhattan residents, schoolchildren, building occupants, and passers-by; these data are not included in our study.14 Although New York City firefighters and local residents are not represented in our cohort, the WTC Screening, Monitoring, and Treatment Program is unique in that it contains interview and physical examination data for a large and diverse group of non-firefighter rescue and recovery workers.
Procedures
Recruitment into our cohort was done by extensive outreach and publicity in partnership with organised labour, community, and volunteer organisations, legislative and governmental agencies, and public media outlets. Participation was voluntary and involved a comprehensive baseline examination, including medical, mental health, and exposure-assessment questionnaires, and a standardised physical examination plus spirometry. Follow-up assessments were offered every 12 to 18 months.
Presence of asthma, sinusitis, and gastro-oesophageal reflux disease was established by rescue and recovery workers’ self-report of physician diagnosis. Workers also reported the date of diagnosis and, for pre-existing disorders, whether these disorders had recurred after 9/11. Mental health screening was undertaken with standardised methods to assess for symptoms of depression (patient health questionnaire [PHQ]), PTSD (PTSD symptom checklist-specific version, which includes questions about symptoms in reference to the 9/11 attacks) and panic disorder (PHQ).15,16 Rescue and recovery workers were classified as having symptoms consistent with depression, PTSD, or panic disorder with validated algorithms.15-17
To assess lung function, rescue and recovery workers underwent spirometric examination at each visit done at different sites by uniformly trained technicians and with standard techniques.18 Spirometric results were compared with reference values dependent on age, sex, race and ethnic origin, and interpreted with established guide-lines.19 Pulmonary obstruction was defined as forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) below the lower limit of normal. Spirometry with FVC lower than the lower limit of normal but FEV1/FVC at the lower limit of normal or higher was categorised as low FVC. Rescue and recovery workers with pulmonary obstruction and low FVC were classified as having mixed airway disease.
Four exposure groups were created: very high, high, intermediate, and low. Group assignment of rescue workers was based on the total time spent working at the WTC site, exposure to the cloud of debris from the collapse of the WTC buildings, and work on the pile of debris. The very high exposure group consisted of those who worked more than 90 days, were exposed to the dust cloud, and worked at least some time on the pile. The high group was comprised of rescue workers who were exposed to the dust cloud but either worked less than 90 days or did not work on the pile. The intermediate group was comprised of workers not exposed to the dust cloud and who either worked between 40 days and 90 days or did not work on the pile. The lowest exposure group included those who worked less than 40 days, were not exposed to dust from the collapse, and did not work in the debris pile.
Statistical analysis
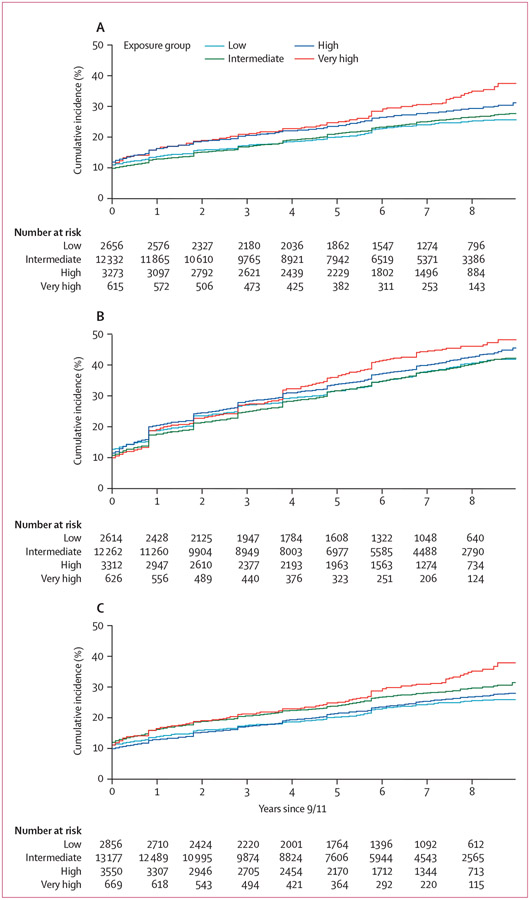
We used Kaplan-Meier estimates to calculate the cumulative incidence and number of individuals at risk for asthma, sinusitis, and gastro-oesophageal reflux disease. On the basis of the Kaplan-Meier curves, we estimated time from 9/11 to the first date that the responder reported a physician diagnosis of each disorder. Results were censored at the date of the last follow-up visit before Sept 11, 2010. Cumulative incidence of these disorders before 9/11 is shown at the intercept of the cumulative incidence curve (figure 1).
Figure 1: Cumulative Incidence of physical disorders in the World Trade Center Screening, Monitoring, and Treatment Program study population.
Cumulative incidence of asthma (A). Cumulative incidence of sinusitis was similar in the intermediate and low exposure groups (B). Incidence of gastro-oesophageal reflux disease incidence was increased only in the very-high-exposure group compared with other groups (C). 9/11=September 11, 2001.
PHQ and PTSD-symptom-checklist scores were not available before the rescue and recovery workers’ first visit to the programme. Workers were interval-censored between the visit date of their first positive screening for a particular mental health disorder and their previous visit; those who screened positive at the first visit were left-censored. Cumulative incidence was calculated with an algorithm for interval censored data.20 Previous research has shown a lower prevalence of mental health disorders in police officers than in other rescue and recovery workers.21,22 Thus, the cumulative incidence of these disorders was assessed separately for New York City police officers versus other workers. We also used methods for interval-censored data to asses the incidence of spirometric abnormalities. Rescue and recovery workers were categorised as having normal or abnormal (obstructive, low FVC, or mixed patterns) spirometric findings. This grouping is consistent with data that showed that most rescue and recovery workers with low FVC had obstructive lung disease.23 To assess the annual risk of developing each disorder, we estimated conditional incidence rates (ie, the risk of developing a disorder in a specific year) by dividing the increment in the cumulative incidence during each year of follow-up by the cumulative incidence rate at the start of the year.
The prevalence of active asthma, sinusitis, and gastro-oesophageal reflux disease 9 years after exposure was calculated as the ratio of the number of rescue workers who reported being under physician care, taking drugs, or having had an acute episode of a specific disorder during the month before the follow-up visit, to the number of rescue workers examined during that year. The proportion of rescue and recovery workers who had symptoms consistent with depression, PTSD, panic disorder, or abnormal spirometry during the 9th year of the programme was also calculated.
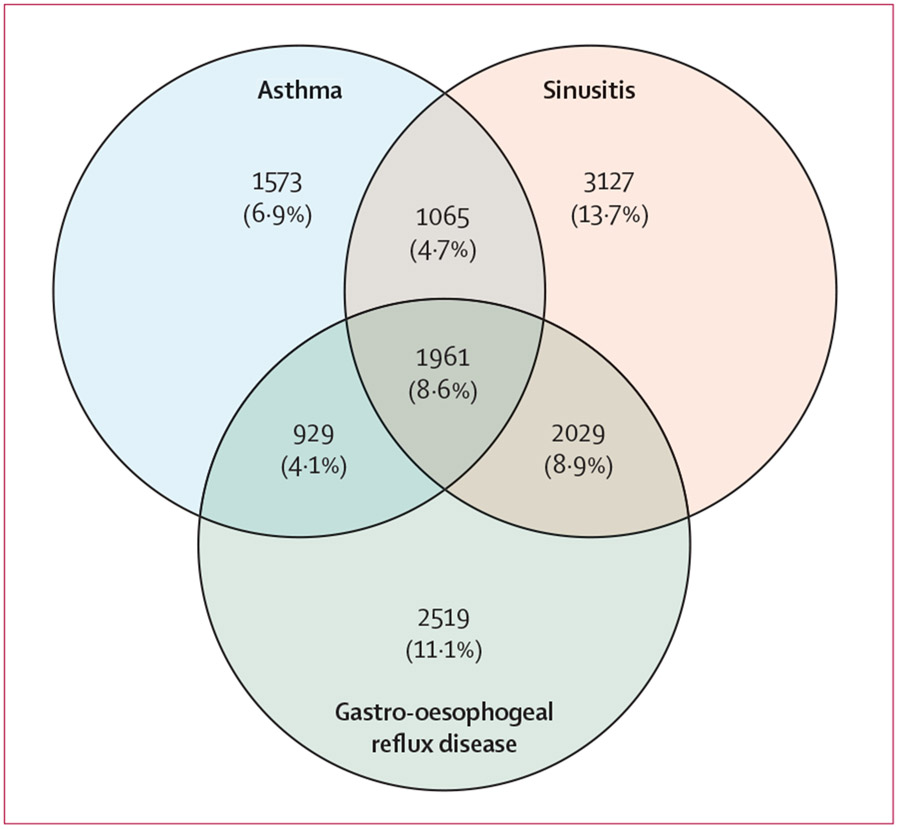
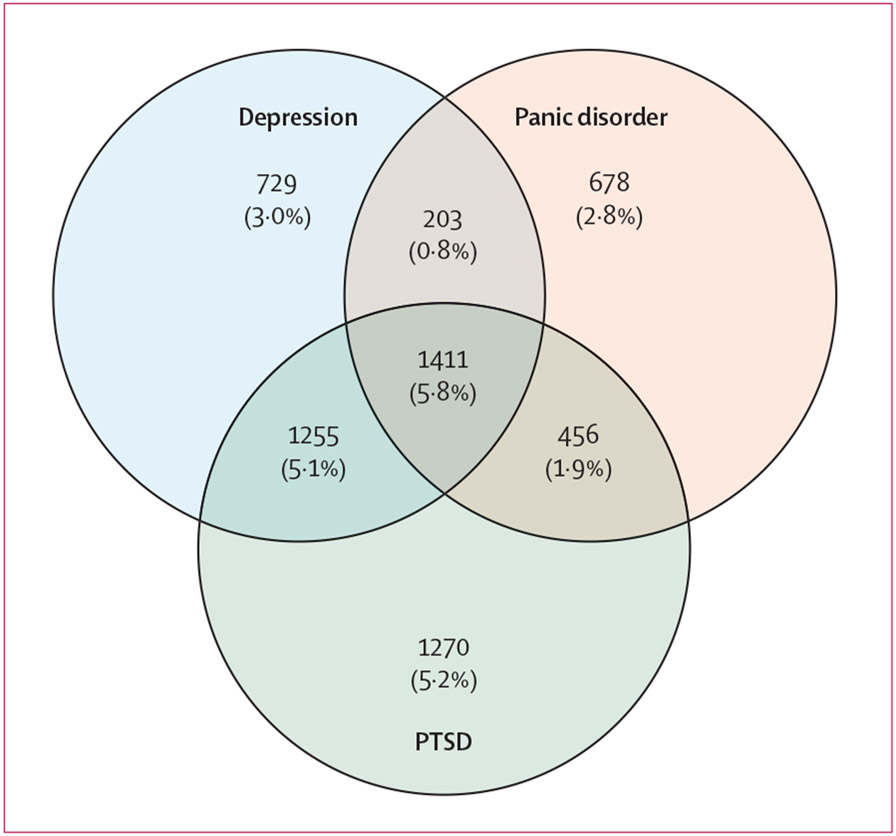
To assess associations of health disorders with exposures after 9/11, we examined the cumulative incidence of each physical and mental health diagnosis and spirometric abnormality by exposure group. To assess the extent to which WTC rescue and recovery workers suffered from multiple physical or mental health problems, we constructed Venn diagrams. Analyses were done with SAS (version 9.1). The study was approved by the Institutional Review Board of Mount Sinai School of Medicine and all participants provided signed consent to use their data.
Role of the funding source
The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication
Results
Most rescue and recovery workers in our cohort were male, white, and had a median age of 38 years on 9/11 (table 1). The most common occupations were protective service or military and construction (table 1). Over a tenth of rescue workers were in the low WTC exposure category, about two-thirds were intermediate category, about a fifth were in the high category, and only a few were in the very high category (table 1). The overall distribution of baseline characteristics was relatively similar across the four exposure groups; except that males and protective service or military personnel were over-represented in the very high exposure category.
Table 1:
Baseline demographic characteristics of the World Trade Center Screening, Monitoring, and Treatment Program study population
| Participants (N=27 449) |
|
|---|---|
| Median age (years)* | 38 (33–44) |
| Sex | |
| Male | 23 468 (86%) |
| Race | |
| White | 15 657 (57%) |
| Black | 2963 (11%) |
| Asian | 373 (1%) |
| Other | 755 (3%) |
| Unknown | 7701 (28%) |
| Hispanic† | 6475 (31%) |
| Smoking‡ | |
| Current | 4054 (15%) |
| Former | 6315 (24%) |
| Never | 15 897 (61%) |
| Occupation§ | |
| Protective services or military | 12 273 (48%) |
| Construction | 5956 (23%) |
| Electrical or telecommunication repair workers | 1794 (7%) |
| Transportation or material movers | 1128 (4%) |
| Other occupations | 4025 (16%) |
| Unemployed or retired | 477 (2%) |
| Union member | 22 558 (83%) |
| Working status at the site¶ | |
| Worker | 21 287 (81%) |
| Volunteer | 2768 (11%) |
| Worked and volunteer | 2127 (8%) |
| WTC exposure category∥ | |
| Low | 3235 (14%) |
| Intermediate | 14 769 (65%) |
| High | 4019 (18%) |
| Very high | 749 (3%) |
| Directly exposed to the dust cloud from collapse | 5059 (21%) |
| Started working on 9/11 | 12 041 (44%) |
| Year of enrolment into the programme¶ | |
| ≤2004 | 11 296 (41%) |
| 2005–07 | 9509 (35%) |
| ≥2008 | 6643 (24%) |
Data are number (%) or median (IQR). 9/11=Sept 11, 2001. WTC=World Trade Center.
Age on 9/11.
Data missing for 6206 rescue and recovery workers who did not answer the question about ethnic origin.
Data missing for 1183 rescue and recovery workers.
Data missing for 1796 rescue and recovery workers.
Data missing for 1267 rescue and recovery workers.
Data missing for 4677 rescue and recovery workers.
Rates of rescue and recovery worker follow-up were 71% (17 224) for the first visit, 61% (9681) for the second, and 55% (4410) for the third. Cumulative incidence of asthma increased from 10·5% (number at risk: 24 985) at baseline to 13·7% (22 360) at year 1, 21·1% (16 897) at year 5, and 27·6% (7027) at year 9 (figure 1 and table 2). Annual incidence was highest during the 1st year after 9/11 and then remained stable in subsequent years at about 2% (table 3). Cumulative incidence of sinusitis increased from 10·7% (number at risk: 25 041) before 9/11 to 18·0% (22 357) at year 1, 31·2% (15 204) at year 5, and 42·3% (5870) at year 9. (table 2). Highest incidence of sinusitis occurred during the first year after WTC exposure, and thereafter, was about 4% (table 3). For gastro-oesophageal reflux disease, cumulative incidence was 5·8% (number at risk: 25 539) at baseline and cumulatively increased to 10·7% (24 055) at year 1, 25·4% (16 828) at year 5, and 39·3% (5650) at year 9 (table 2). Annual incidence ranged from 4–6% in all follow-up years. At year 9, prevalence of active asthma was 18·1% (1893), of sinusitis was 20·0% (2042), and of gastro-oesophageal reflux disease was 32·6% (3195).
Table 2:
Cumulative incidence before and after 9/11 of physical disorders, mental health symptoms, and spirometric abnormalities in the World Trade Center Screening, Monitoring, and Treatment Program study population
| Pre-exposure | Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 | Year 9 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Physical health | ||||||||||
| Asthma | 10·5% (24 985) | 13·7% (22 360) | 15·8% (21 496) | 17·5% (19 505) | 19·3% (18 227) | 21·1% (16 897) | 23·4% (15 317) | 25·0% (12 809) | 26·4% (10 744) | 27·6% (7027) |
| Sinusitis | 10·7% (25 041) | 18·0% (22 357) | 21·8% (20 476) | 25·2% (18 238) | 28·3% (16 709) | 31·2% (15 204) | 34·4% (13 537) | 37·3% (11 100) | 39·8% (9109) | 42·3% (5870) |
| Gastro-oesophageal reflux disease | 5·8% (25 539) | 10·7% (24 055) | 14·4% (22 741) | 17·9% (20 343) | 21·5% (18 603) | 25·4% (16 828) | 29·9% (14 796) | 33·6% (11 896) | 37·1% (9423) | 39·3% (5650) |
| Mental health symptoms | ||||||||||
| New York City police | ||||||||||
| Depression | ·· | 1·7% (9573) | 2·0% (9467) | 2·3% (8734) | 3·7% (8026) | 3·7% (7510) | 4·2% (6999) | 4·2% (6097) | 6·2% (5420) | 7·0% (3648) |
| PTSD | ·· | 2·5% (9866) | 2·5% (9679) | 4·0% (9124) | 4·6% (8624) | 5·7% (8155) | 6·3% (7597) | 7·4% (6537) | 8·4% (5601) | 9·3% (3761) |
| Panic disorder | ·· | 2·3% (9820) | 2·6% (9691) | 3·1% (8928) | 4·4% (8186) | 4·4% (7659) | 5·6% (7158) | 5·7% (6271) | 7·0% (5591) | 8·4% (3780) |
| Other rescue and recovery workers* | ||||||||||
| Depression | ·· | 10·8% (15 062) | 12·7% (14 105) | 15·3% (11 620) | 17·0% (9855) | 17·4% (8847) | 19·0% (8205) | 22·3% (7138) | 24·6% (6229) | 27·5% (4200) |
| PTSD | ·· | 12·8% (16 054) | 13·5% (14 641) | 17·1% (12 306) | 19·8% (10 762) | 22·6% (9785) | 24·2% (8956) | 27·2% (7682) | 29·7% (6473) | 31·9% (4342) |
| Panic disorder | ·· | 5·0% (15 995) | 5·7% (15 302) | 8·1% (12 880) | 12·8% (10 964) | 12·8% (10 083) | 13·7% (9446) | 14·2% (8302) | 18·5% (7349) | 21·2% (4953) |
| Abnormal spirometry | ·· | 23·7% (24 566) | 24·9% (22 174) | 27·1% (19 105) | 28·5% (16 542) | 29·1% (14 378) | 32·4% (12 700) | 34·9% (10 883) | 37·9% (8949) | 41·8% (5769) |
Data are % (number at risk). Number of individuals at risk is estimated from cumulative incidence curves. PTSD=post-traumatic stress disorder.
All workers except New York City police officers.
Table 3:
Annual conditional incidence after 9/11 of physical disorders, mental health symptoms, and spirometric abnormalities in the World Trade Center Screening, Monitoring, and Treatment Program study population
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 | Year 9 | |
|---|---|---|---|---|---|---|---|---|---|
| Physical health | |||||||||
| Asthma | 3·4% (22 360) | 2·5% (21 496) | 2·0% (19 505) | 2·2% (18 227) | 2·2% (16 897) | 2·9% (15 317) | 2·1% (12 809) | 1·8% (10 744) | 1·8% (7027) |
| Sinusitis | 8·0% (22 357) | 4·7% (20 476) | 4·2% (18 238) | 4·2% (16 709) | 4·0% (15 204) | 4·6% (13 537) | 4·4% (11 100) | 4·0% (9109) | 4·3% (5870) |
| Gastro-oesophageal reflux disease | 5·0% (24 055) | 4·3% (22 741) | 4·0% (20 343) | 4·4% (18 603) | 4·9% (16 828) | 6·0% (14 796) | 5·3% (11 896) | 5·0% (9423) | 4·1% (5650) |
| Mental health symptoms | |||||||||
| New York City police | |||||||||
| Depression | ··* | 0·3% (9467) | 0·3% (8734) | 1·4% (8026) | 0·0% (7510) | 0·5% (6999) | 0·0% (6097) | 2·0% (5420) | 0·9% (3648) |
| PTSD | ·· | 0·1% (9679) | 0·0% (9124) | 1·8% (8624) | 0·8% (8155) | 1·3% (7597) | 0·4% (6537) | 1·8% (5601) | 1·0% (3761) |
| Panic disorder | ·· | 0·2% (9691) | 0·4% (8928) | 1·5% (8186) | 0·0% (7659) | 0·7% (7158) | 0·5% (6271) | 1·3% (5591) | 1·7% (3780) |
| Other rescue and recovery workers | |||||||||
| Depression | ·· | 3·6% (14 105) | 2·9% (11 620) | 2·0% (9855) | 0·4% (8847) | 1·9% (8205) | 4·2% (7138) | 2·9% (6229) | 3·9% (4200) |
| PTSD | ·· | 0·3% (14 641) | 3·5% (12 306) | 4·4% (10 762) | 3·3% (9785) | 2·3% (8956) | 4·0% (7682) | 2·8% (6473) | 3·7% (4342) |
| Panic disorder | ·· | 1·3% (15 302) | 1·4% (12 880) | 3·9% (10 964) | 2·3% (10 083) | 0·9% (9446) | 0·6% (8302) | 4·9% (7349) | 2·9% (4953) |
| Abnormal spirometry | ·· | 1·6% (22 174) | 1·0% (19 105) | 3·9% (16 542) | 0·8% (14 378) | 2·5% (12 700) | 5·8% (10 883) | 4·7% (8949) | 6·2% (5769) |
Data are % (number at risk). Number of individuals at risk estimated from cumulative incidence curves. PTSD=post-traumatic stress disorder.
No rate was estimated for year 1 because no data on mental health symptoms was available before 9/11. 9/11=Sept 11, 2001.
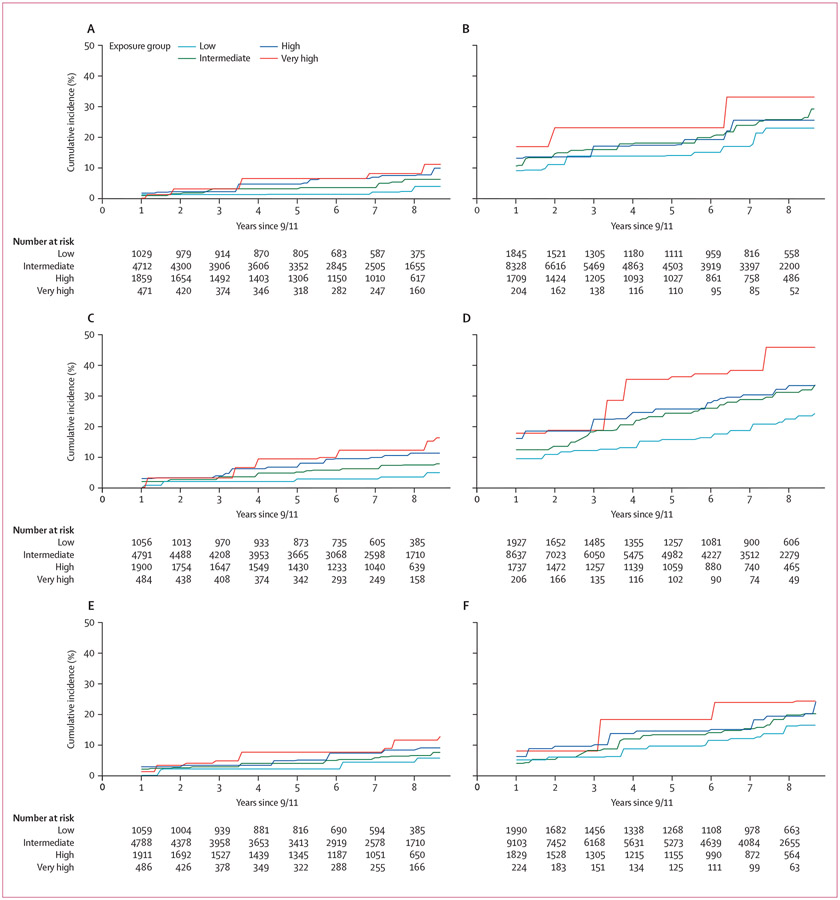
Overall, 272 (1%) of rescue and recovery workers reported a history of physician diagnosed PTSD before 9/11 and 696 (3%) reported a previous diagnosis of depression. Cumulative incidence of PTSD, depression, and panic disorder was substantially lower in New York City police officers than in other rescue and recovery workers (table 2). PTSD was the mental health disorder with the highest cumulative incidence in both groups at all time intervals (table 2). Among police officers, annual incidence of PTSD peaked in the 4th year after 9/11 and then stabilised at about 1–2% per year (table 3). The annual incidence of PTSD for other rescue workers also peaked in the 4th year of follow-up and remained at about 3–4% in subsequent years (table 3).
Cumulative incidence of depression in New York City police officers was 1·7% (number at risk: 9573) at year 1, 3·7% (7510) at year 5, and 7·0% (3648) at year 9; in other rescue and recovery workers cumulative incidence was 10·8% (15 062) at year 1, 17·4% (8847) at year 5, and 27·5% (4200) at year 9 (table 2). Cumulative incidence of panic disorder in police officers was 2·3% (number at risk: 9820) at year 1 and increased to 4·4% (7659) at year 5 and 8·4% (3780) at year 9. For other rescue and recovery workers, cumulative incidence rates of panic disorder were 5·0% (number at risk: 15 995) at year 1, 12·8% (10 083) at year 5, and 21·2% (4953) at year 9 (table 2). At year 9, prevalence of depression in police officers was 4·5% (171), PTSD 5·0% (198), and panic disorder 4·8% (191); in other rescue workers, prevalence of depression was 17·9% (953), PTSD 19·2% (1141), and panic disorder 12·3% (727).
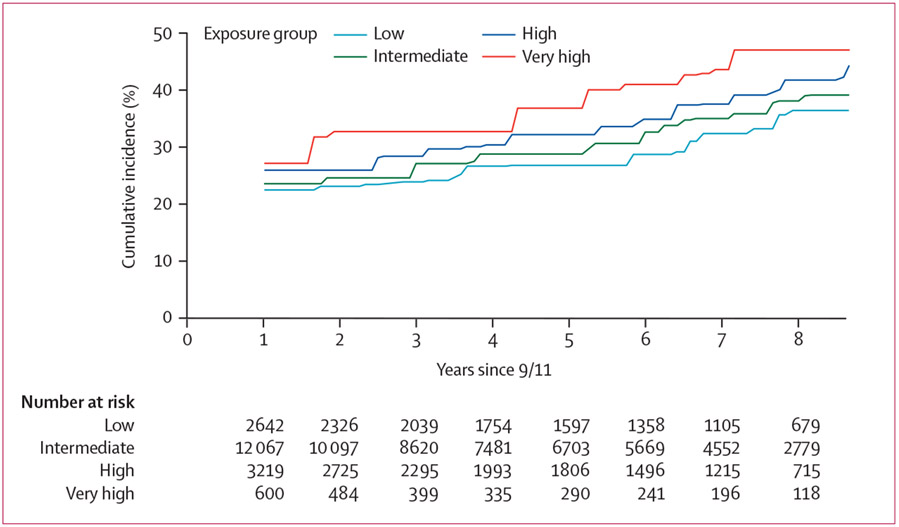
Cumulative incidence rates of abnormal spirometry were 23·7% (number at risk: 24 566) at year 1, 29·1% (14 378) at year 5, and 41·8% (5769) at year 9 (table 2). Annual incidence of new abnormalities in lung function was about 1–2% in the initial years after exposure and then increased to 5–6% in the latter years of follow-up. At year 9, prevalence of obstructive pulmonary disease in rescue and recovery workers was 4·4% (399), low FVC 21·8% (1992), and mixed abnormalities 2·1% (188).
In analyses of exposure-stratified cumulative incidence rates, we noted that risk of asthma, sinusitis, and gastro-oesophageal reflux disease was greatest in workers with the highest levels of exposure (figure 1A-C). Overall, we reported similar findings for mental health disorders (figure 2A-F) and spirometric abnormalities (figure 3).
Figure 2: Cumulative incidence of mental health disorders in New York City police officers and other rescue and recovery workers in the World Trade Center Screening, Monitoring, and Treatment Program study population.
Symptoms of depression in police officers were similar in the very-high and high-exposure categories (A). Symptoms of depression in other rescue and recovery workers were similar in the high and intermediate exposure categories (B). Symptoms of post-traumatic stress disorder (PTSD) were more common in police officers with higher exposure (C). Higher levels of exposure were associated with increased rates of PTSD symptoms in other responders (D). Symptoms of panic disorders were more common in police officers with higher levels of exposure (E). High exposure levels were associated with increased rates of panic-disorder symptoms in other rescue and recovery workers (F). 9/11=September 11, 2001.
Figure 3: Cumulative incidence of abnormal spirometry in the World Trade Center Screening, Monitoring, and Treatment Program study population.
9/11=September 11, 2001.
We identified extensive comorbidities associated with physical and mental health disorders. Overall, nearly a tenth of rescue and recovery workers reported physician diagnosis of three disorders: asthma, sinusitis, and gastro-oesophageal reflux disease (figure 4). About 18% of rescue and recovery workers reported diagnoses of two disorders (figure 4). The proportion of rescue and recovery workers with symptoms consistent with PTSD, depression, and panic disorder are shown in figure 5. The proportion of those with symptoms of both depression and PTSD were also reported (figure 5). Substantial comorbidity across physical and mental health disorders was also reported: 1459 (48·3%) rescue and recovery workers with asthma, 2006 (38·2%) with sinusitis, and 2348 (42·7%) with gastro-oesophageal reflux disease reported at least one mental health disorder. Similarly, 2806 (69·6%) with PTSD, 2153 (70·4%) with depression, and 1129 (72·4%) with panic disorder reported a physician diagnosis of at least one physical disorder.
Figure 4: Physical comorbidities in the World Trade Center Screening, Monitoring, and Treatment Program study population.
The Venn diagram shows the extent of comorbidity in World Trade Center rescue and recovery workers who reported ever having asthma, sinusitis, or gastro-oesophageal reflux disease.
Figure 5: Mental health comorbidities in the World Trade Center Screening, Monitoring, and Treatment Program study population.
High number of rescue and recovery workers had symptoms consistent with several of the mental health disorders assessed during the 9 year follow-up. PTSD= post-traumatic stress disorder.
Discussion
We reported that about 10–30% of rescue and recovery workers still had persistent medical disorders 9 years after the WTC attacks. More than a fifth had multiple physical and mental health problems. Most health disorders were more common in rescue and recovery workers with highest levels of exposure to dust and smoke than in those with lower levels of exposure (panel).
Our finding of upper and lower airway injury in WTC rescue and recovery workers is consistent with data from studies that have shown high rates of respiratory disease and declines in pulmonary function after exposure to WTC dust.6,10,24 A study of New York City firefighters who responded to WTC attack showed a striking decline in FEV1 in the 12-month period after 9/11.10 Airway obstruction with air trapping seemed to be the main physiological mechanism underlying this reduction in lung function.23 Similarly, data from the WTC registry, which tracks diagnoses in rescue and recovery workers and residents of lower Manhattan, showed high rates of new onset asthma after the attacks.6 We noted that annual incidence of abnormal spirometry in rescue and recovery workers was higher in the later years of follow-up than in earlier years. A possible explanation for this unanticipated finding is that some workers who had early subclinical loss of lung function after 9/11 crossed the threshold of abnormality only several years later as the result of further pathological or age-related decline in lung function. However, other factors, including temporal biases in the study population, cannot be excluded.
Inhalation of toxic, highly alkaline dust (pH 10–11) is the probable cause of upper and lower respiratory injury in rescue and recovery workers. The dust generated by the collapse of the WTC towers and the diesel exhaust fumes produced by rescue and recovery machinery might have caused inflammation of responders’ airways, which could have led to irritant-induced rhinosinusitis, pharyngitis, and asthma. Previous studies in occupational settings have shown that comparable levels of exposure to airborne pollutants are associated with reactive airway disease.25,26 Furthermore, animal studies have shown that exposure of the respiratory tract to high levels of fine particulate matter obtained from the WTC site has been associated with development of pulmonary inflammation and airway hyper-responsiveness.27 Collectively, these findings underscore the importance of providing rescue workers with access to respiratory protection and enforcing its use while responding to disasters.
Previous studies have shown that New York City police officers were at lower risk than some responders for developing mental health disorders after the WTC attacks.21,22 Possible reasons for these findings include training, previous experience in dealing with similar stressors, self-selection of individuals with high resilience during recruitment into the workforce, and possible under-reporting of psychological symptoms because of perceived job-related repercussions. We report here that PTSD and depression are the most common mental health disorders in police officers and other individuals involved with the WTC rescue and recovery efforts, a finding consistent with research showing that most WTC rescue and recovery workers with depression had comorbid PTSD.28
We established that rates of panic disorder remained raised up to 9 years after 9/11. These findings could have been due, in part, to anxiety symptoms that existed before WTC exposure or because some patients with generalised anxiety disorder could have been included by use of our screening method. These mental health problems occurred most commonly in rescue and recovery workers exposed to the dust cloud, which is consistent with previous findings of post-disaster psychopathological research.6,21,29-31
We assessed overall rates of mental health disorders in rescue and recovery workers without undertaking further analyses to stratify the sample by established risk factors such as age, sex, race or ethnic origin. Thus, our overall results might underestimate or overestimate the actual rates of mental health disorders in specific subgroups of workers. Similarly, data for ethnic origin were missing for some responders (table 1). Previous studies, for example, have shown that Hispanic WTC rescue and recovery workers have a high risk for PTSD. Consequently, the rate of PTSD seen in our study could have been underestimated, if a substantial proportion of workers with missing data for ethnic origin were Hispanics.
We do not know exactly how representative our study cohort is of the entire population of WTC first responders, because participation in our programme was voluntary. This potential shortcoming is compounded by the fact that comprehensive records of participation in the WTC rescue and recovery effort were not maintained. Therefore, neither the total number of rescue and recovery workers nor the proportion of them participating in our programme is known.
Estimates of the size of the WTC rescue and recovery worker population have varied. Calculations that need a minimal worker involvement and time undertaking rescue and recovery work suggest that the true number of workers is more than 50 000.1 The number of WTC workers enrolled in our programme and in the parallel programme done by the FDNY is more than 40 000.1 Hence, these two programmes combined are assessing a substantial proportion of the rescue and recovery workers. As a result of the staggered and voluntary enrolment of individuals into our programme, we do not have information from each responder at every follow-up time. However, we used robust statistical methods to estimate unbiased rates of physical and mental health disorders in the absence of complete data and to provide information on the number of rescue and recovery workers at risk at each year after 9/11. Nonetheless, self-selection of workers into our programme on the basis of WTC exposure, perceived risk, or presence of physical or mental health disorders could have occurred, which might reduce the generalisability of our findings to all WTC rescue and recovery workers.
Recruitment into our programme was staggered with some rescue and recovery workers joining in the last 3 years of the study. Although the sociodemographic characteristics of early and recent enrollees was relatively similar, we cannot exclude the possibility of recall bias or self-selection of workers at increased risk for physical or mental health disorders in late enrolees. Incidence and prevalence of most physical disorders were similar in our cohort and the FDNY cohort, which suggests that workers with medical problems have not enrolled in disproportionate numbers in our programme. By contrast with our cohort, participation in the FDNY programme was mandatory for all active duty New York City firefighters and paramedics. Therefore, the possibility of selection bias in the FDNY cohort is minimal.
We did not use an external control population to compare the rates of physical and mental health disorders in WTC rescue and recovery workers. Identification of an appropriate control group was difficult because of the unique nature of the population of workers and the possibility of a healthy worker effect in the study cohort (ie, workers commonly having lower rates of disease than the general population because severely ill and disabled individuals are less likely to be employed).32
We established the presence of physical disorders with self-reported information. However, objective lung function data were available from spirometry and we used validated methods to assess the presence of mental health disorders. Thus, incidence rates and prevalence of these disorders should be minimally affected by reporting bias.
We categorised each worker’s level of exposure solely on the basis of three factors: exposure to the dust cloud, total time spent working at the WTC site, and work on the debris pile. These exposures have been consistently associated with risk of illnesses in WTC rescue and recovery workers and we identified positive dose–response relations in our analyses similar to those reported in other studies.2,6 We did not, however, assess the extent to which other exposure factors, such as use of respiratory protection, personal hygiene measures, or exposure to body parts, might have influenced the observed risk of physical or mental health disorders.
Our findings show a substantial burden of persistent physical and mental disorders in rescue and recovery workers who rushed to the site of the WTC and laboured there for weeks and months 10 years ago. Many of these individuals now suffer from multiple health problems. The findings of this study emphasise the need for continued monitoring and treatment of the rescue and recovery worker population and underscore the importance of providing adequate health monitoring and treatment for these individuals. Planning for future disasters should anticipate the probability of persistent physical and mental illness in rescue and recovery workers.
Panel: Research in context.
Systematic review
We searched Medline from September, 2006, to May, 2011, without language restrictions, for original studies and reviews assessing long-term illnesses in WTC rescue and recovery workers and volunteers. We used the search terms: “illnesses”, “September 11”, and “World Trade Center attacks”. We identified five original studies and one review that summarised some of the illnesses reported by WTC rescue and recovery workers and volunteers at 5–7 years after 9/11.
Interpretation
The high prevalence of physical and mental health disorders in WTC rescue and recovery workers 9 years after the WTC disaster underscores the importance of continual provision of adequate health monitoring and treatment for these individuals. These data suggest that the clinical management of the health consequences of WTC exposures will require coordinated physical and mental health care. Planning for future disasters should anticipate the probability of persistent physical and mental illness in rescue and recovery workers.
WTC=World Trade Center. 9/11=September 11, 2001.
Acknowledgments
We thank the staff of the World Trade Center (WTC) Worker and Volunteer Medical Screening, Medical Monitoring, and Treatment programmes; the labour, community, and volunteer organisation stake-holders; and the WTC rescue and recovery workers, who gave of themselves so readily in response to the WTC attacks and to whom the WTC programmes are dedicated. This work was supported by the Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (contract 200-2002-0038 and grant 5U1O 0H008232), the American Red Cross Liberty Fund, The September 11th Recovery Program, The Bear Stearns Charitable Foundation, The September 11th Fund, The Robin Hood Foundation Relief Fund, and many others. The contents of this report are solely the responsibility of the authors and do not necessarily represent the official views of Centers for Disease Control or the National Institute for Occupational Safety and Health.
Footnotes
Conflicts of interest
JPW is a member of the research board of EHE International. All other authors declare that they have no conflicts of interest.
Contributor Information
Juan P Wisnivesky, Division of General Internal Medicine, Mount Sinai School of Medicine, New York, NY, USA; Division of Pulmonary and Critical Care Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Susan L Teitelbaum, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Andrew C Todd, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Paolo Boffetta, Institute for Translational Epidemiology, Mount Sinai School of Medicine, New York, NY, USA.
Michael Crane, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Laura Crowley, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Rafael E de la Hoz, Division of General Internal Medicine, Mount Sinai School of Medicine, New York, NY, USA; Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Cornelia Dellenbaugh, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Denise Harrison, Department of Medicine, Bellevue Hospital Center/New York University School of Medicine, New York, NY, USA.
Robin Herbert, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Hyun Kim, Department of Population Health, Hofstra North Shore-LIJ School of Medicine, Great Neck, NY, USA.
Yunho Jeon, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Julia Kaplan, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Craig Katz, Department of Psychiatry, Mount Sinai School of Medicine, New York, NY, USA.
Stephen Levin, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Ben Luft, Department of Medicine, State University of New York at Stony Brook, Port Jefferson, NY, USA.
Steven Markowitz, Queens College, City University of New York, Flushing, NY, USA.
Jacqueline M Moline, Department of Population Health, Hofstra North Shore-LIJ School of Medicine, Great Neck, NY, USA.
Fatih Ozbay, Department of Psychiatry, Mount Sinai School of Medicine, New York, NY, USA.
Robert H Pietrzak, Department of Psychiatry, Yale University School of Medicine and National Center for Post-traumatic Stress Disorder, Veterans Administration Connecticut Healthcare System, West Haven, CT, USA.
Moshe Shapiro, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Vansh Sharma, Department of Psychiatry, Mount Sinai School of Medicine, New York, NY, USA.
Gwen Skloot, Pulmonary and Critical Care Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Steven Southwick, Department of Psychiatry, Yale University School of Medicine and National Center for Post-traumatic Stress Disorder, Veterans Administration Connecticut Healthcare System, West Haven, CT, USA.
Lori A Stevenson, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Iris Udasin, University of Medicine and Dentistry of New Jersey, Piscataway, NJ, USA.
Sylvan Wallenstein, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
Philip J Landrigan, Department of Preventive Medicine, Mount Sinai School of Medicine, New York, NY, USA.
References
- 1.Savitz DA, Oxman RT, Metzger KB, et al. Epidemiologic research on man-made disasters: strategies and implications of cohort definition for World Trade Center worker and volunteer surveillance program. Mt Sinai J Med 2008; 75: 77–87. [DOI] [PubMed] [Google Scholar]
- 2.Herbert R, Moline J, Skloot G, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect 2006; 114: 1853–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landrigan PJ, Lioy PJ, Thurston G, et al. Health and environmental consequences of the world trade center disaster. Environ Health Perspect 2004; 112: 731–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lioy PJ, Weisel CP, Millette JR, et al. Characterization of the dust/smoke aerosol that settled east of the World Trade Center (WTC) in lower Manhattan after the collapse of the WTC 11 September 2001. Environ Health Perspect 2002; 110: 703–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Prezant DJ, Weiden M, Banauch GI, et al. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med 2002; 347: 806–15. [DOI] [PubMed] [Google Scholar]
- 6.Brackbill RM, Hadler JL, DiGrande L, et al. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA 2009; 302: 502–116. [DOI] [PubMed] [Google Scholar]
- 7.Safirstein BH, Klukowicz A, Miller R, Teirstein A. Granulomatous pneumonitis following exposure to the World Trade Center collapse. Chest 2003; 123: 301–04. [DOI] [PubMed] [Google Scholar]
- 8.Mann JM, Sha K, Kline G, Breuer FU, Miller A. World Trade Center dyspnea: bronchiolitis obliterans with functional improvement: a case report. Am J Ind Med 2005; 48: 225–29. [DOI] [PubMed] [Google Scholar]
- 9.Crowley LE, Herbert R, Moline JM, et al. “Sarcoid like” granulomatous pulmonary disease in World Trade Center disaster responders. Am J Ind Med 2011; 54: 175–84. [DOI] [PubMed] [Google Scholar]
- 10.Aldrich TK, Gustave J, Hall CB, et al. Lung function in rescue workers at the World Trade Center after 7 years. N Engl J Med 2010; 362: 1263–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mauer MP, Cummings KR, Hoen R. Long-term respiratory symptoms in World Trade Center responders. Occup Med (Lond) 2010; 60: 145–51. [DOI] [PubMed] [Google Scholar]
- 12.Moline JM, Herbert R, Levin S, et al. WTC medical monitoring and treatment program: comprehensive health care response in aftermath of disaster. Mt Sinai J Med 2008; 75: 67–75. [DOI] [PubMed] [Google Scholar]
- 13.Feldman DM, Baron SL, Bernard BP, et al. Symptoms, respirator use, and pulmonary function changes among New York City firefighters responding to the World Trade Center disaster. Chest 2004; 125: 1256–64. [DOI] [PubMed] [Google Scholar]
- 14.Murphy J, Brackbil RM, Thalji L, Dolan M, Pulliam P, Walker DJ. Measuring and maximizing coverage in the World Trade Center Health Registry. Stat Med 2007; 26: 1688–701. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999; 282: 1737–44. [DOI] [PubMed] [Google Scholar]
- 16.Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Annual Convention of the International Society for Traumatic Stress Studies. San Antonio, TX, USA; Oct 24–27, 1993. [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–38. [DOI] [PubMed] [Google Scholar]
- 19.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005; 26: 948–68. [DOI] [PubMed] [Google Scholar]
- 20.Zhan J A Hybrid Algorithm for Computation of the Nonparametric Maximum Likelihood Estimator From Censored Data. JASA 1997; 92: 945–59. [Google Scholar]
- 21.Perrin MA, DiGrande L, Wheeler K, Thorpe L, Farfel M, Brackbil R. Differences in PTSD prevalence and associated risk factors among World Trade Center disaster rescue and recovery workers. Am J Psychiatry 2007; 164: 1385–94. [DOI] [PubMed] [Google Scholar]
- 22.Renck B, Weisaeth L, Skarbo S. Stress reactions in police officers after a disaster rescue operation. Nord J Psychiatry 2002; 56: 7–14. [DOI] [PubMed] [Google Scholar]
- 23.Weiden MD, Ferrier N, Nolan A, et al. Obstructive airways disease with air trapping among firefighters exposed to World Trade Center dust. Chest 2010; 137: 566–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Udasin I, Schechter C, Crowley L, et al. Respiratory symptoms were associated with lower spirometry results during the first examination of WTC responders. J Occup Environ Med 2011; 53: 49–54. [DOI] [PubMed] [Google Scholar]
- 25.Brooks SM, Weiss MA, Bernstein IL. Reactive airways dysfunction syndrome (RADS). Persistent asthma syndrome after high level irritant exposures. Chest 1985; 88: 376–84. [DOI] [PubMed] [Google Scholar]
- 26.Lombardo LJ, Balmes JR. Occupational asthma: a review. Environ Health Perspect 2000; 108 (suppl 4): 697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gavett SH, Haykal-Coates N, Highfill JW, et al. World Trade Center fine particulate matter causes respiratory tract hyperresponsiveness in mice. Environ Health Perspect 2003; 111: 981–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stellman JM, Smith RP, Katz CL, et al. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect 2008; 116: 1248–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. Am J Epidemiol 2011; 173: 271–81. [DOI] [PubMed] [Google Scholar]
- 30.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004; 351: 13–22. [DOI] [PubMed] [Google Scholar]
- 31.Tapp LC, Baron S, Bernard B, Driscoll R, Mueller C, Wallingford K. Physical and mental health symptoms among NYC transit workers seven and one-half months after the WTC attacks. Am J Ind Med 2005; 47: 475–83. [DOI] [PubMed] [Google Scholar]
- 32.Choi BC. Definition, sources, magnitude, effect modifiers, and strategies of reduction of the healthy worker effect. J Occup Med 1992; 34: 979–88. [PubMed] [Google Scholar]