Abstract
Background
By July 2021, Canada had received enough COVID-19 vaccines to fully vaccinate every eligible Canadian. However, despite the availability of vaccines, some eligible individuals remain unvaccinated. Differences in vaccination uptake can be driven by health inequalities which have been exacerbated and amplified by the pandemic. This study aims to assess inequalities in COVID-19 vaccination uptake and intent in adults 18 years or older across Canada by identifying sociodemographic factors associated with non-vaccination and low vaccination intent using data drawn from the June to August 2021 Canadian Community Health Survey (CCHS).
Methods
The CCHS is an annual cross-sectional and nationally representative survey conducted by Statistics Canada, which collects health-related information. Since September 2020, questions about the COVID-19 pandemic are asked. Adjusted logistic regression models were fitted to examine associations between vaccination uptake or intent and sociodemographic and health related variables. Region, age, gender, level of education, Indigenous status, visible minority status, perceived health status, and having a regular healthcare provider were considered as predictors, among other factors.
Results
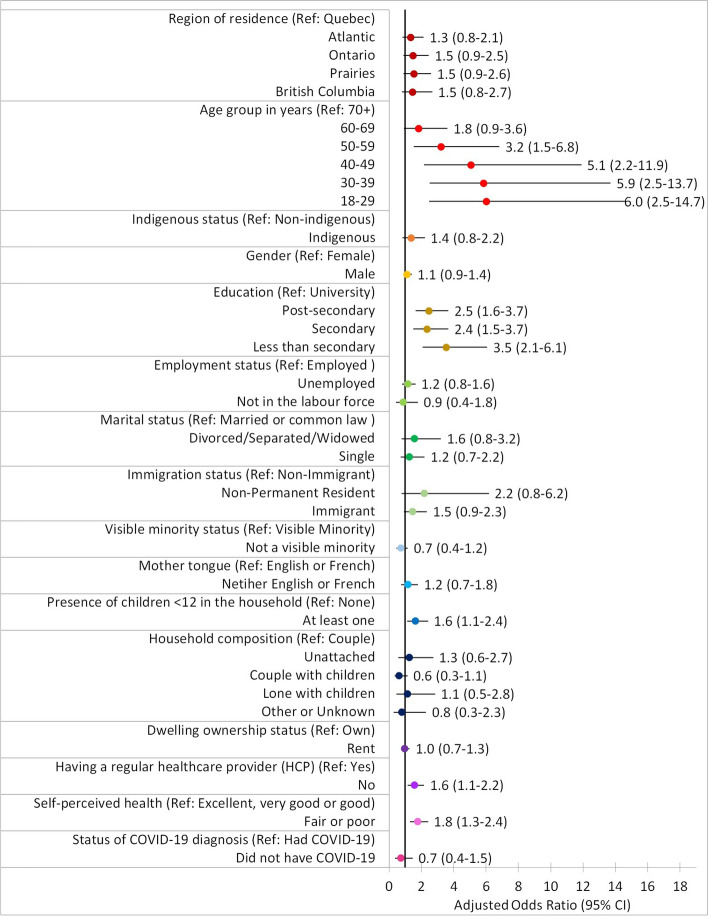
The analysis included 9,509 respondents. The proportion of unvaccinated was 11%. Non-vaccination was associated with less than university education (aOR up to 3.5, 95% CI 2.1–6.1), living with children under 12 years old (aOR 1.6, 95% CI 1.1–2.4), not having a regular healthcare provider (aOR 1.6, 95% CI 1.1–2.2), and poor self-perceived health (aOR 1.8, 95% CI 1.3–2.4).
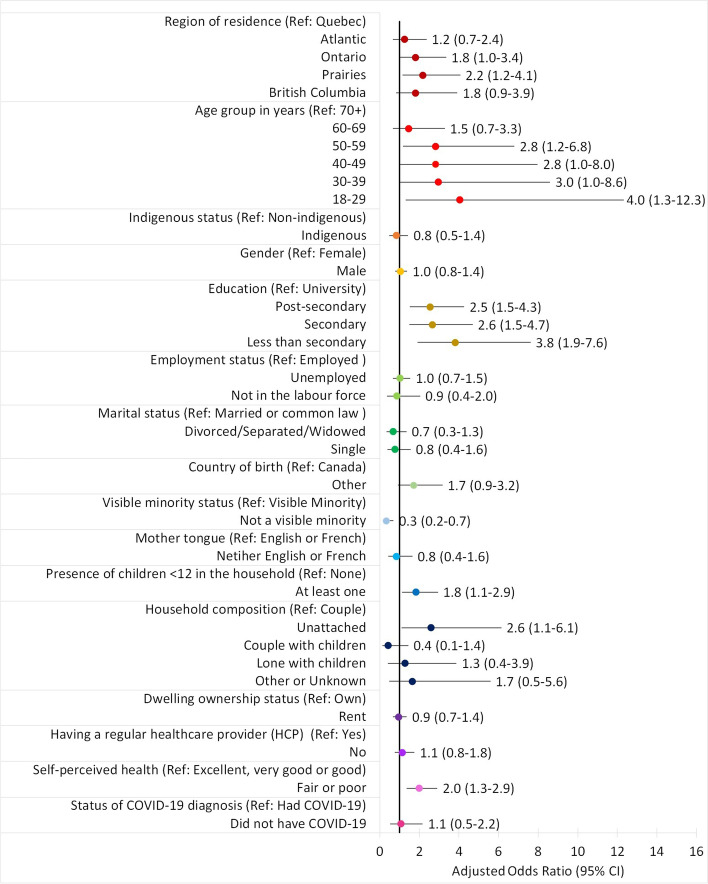
Only 5% of the population had low intention to get vaccinated. Being unlikely to get vaccinated was associated with the Prairies region (aOR 2.2, 95% CI 1.2–4.1), younger age groups (aOR up to 4.0, 95% CI 1.3–12.3), less than university education (aOR up to 3.8, 95% CI 1.9–7.6), not being part of a visible minority group (aOR 3.0, 95% CI 1.4–6.4), living with children under 12 years old (aOR 1.8, 95% CI 1.1–2.9), unattached individuals (aOR 2.6, 95% CI 1.1–6.1), and poor self-perceived health (aOR 2.0, 95% CI 1.3–2.9).
Conclusions
Disparities were observed in vaccination uptake and intent among various sociodemographic groups. Awareness of inequalities in COVID-19 vaccination uptake and intent is needed to determine the vaccination barriers to address in vaccination promotion strategies.
Keywords: COVID-19, Vaccine, Vaccination Coverage, Intention, Health equity, Canada
Background
Canada initiated its COVID-19 vaccination campaign on December 14, 2020 to first administer doses to priority groups (i.e. those at high risk of severe illness and death from COVID-19 and those who are most likely to be exposed to the virus: residents and staff of congregate living settings, frontline healthcare workers, adults in Indigenous communities, adults of advanced age) and then followed with broader availability to the public throughout 2021. Vaccine prioritization varied by province, but was predominantly based on age, starting with the elderly and then decreasing in 5- or 10-year age bands. In the ten Canadian provinces, all adults 18 years or older became eligible to receive their first dose between May 10 and May 27, 2021. By the end of July, enough vaccine doses had been acquired to fully vaccinate every eligible person in Canada [1].
Health inequities, which have been exacerbated and amplified by the pandemic, are among the diverse forms of barriers as they affect the accessibility, acceptance and uptake of COVID-19 vaccines in equity-seeking groups [2, 3]. Health inequalities represent any measurable difference in health across individuals or socially relevant subpopulations [4]. When these differences are preventable, unjust or unnecessary, they are considered health inequities [4]. By measuring health inequalities, we can develop a better understanding of how to prevent them from persisting unfairly and further contributing to health inequities [4].
Health inequalities related to vaccination intent were observed in different groups in Canada. Indeed, younger age, lower education or income, identifying as non-white or Indigenous, being born outside of Canada and living in a household of at least five members were negatively associated with the intent to get vaccinated [5–7]. In the COVID-19 Vaccination Coverage Survey, males, and individuals with lower education or household income had higher odds of not intending to get vaccinated [8].
While the literature on vaccination intent provides insight on how sociodemographic factors influences health inequalities in vaccination uptake, few articles have yet to be published on disparities in vaccination uptake in Canada. Of the few studies available, most came from the US and the UK where findings indicated that vaccination coverage differ across gender, socioeconomic status, visible minority status and area of residency [9–11]. Despite having positive intentions to vaccinate, health inequalities in vaccination uptake can also occur in some groups or individuals due to systemic barriers in access [2].
As the pandemic continues to unfold, it is critical to ensure equitable distribution and uptake of COVID-19 vaccines in order to reduce morbidity and mortality. Understanding how socioeconomic inequalities have been impacting the current COVID-19 vaccination campaign in Canada is crucial to help public health authorities improve vaccine acceptance in order to limit hospitalizations and deaths, especially given the disproportionate health and economic impact COVID-19 has on marginalized groups [12]. In that regard, the annual Canadian Community Health Survey (CCHS), which collects health-related data, was leveraged by adding a COVID-19 module asking questions on vaccination uptake and intent. Using CCHS data, the purpose of this study was to assess inequalities in COVID-19 vaccination uptake and intent at the national level by identifying sociodemographic factors associated with non-vaccination and low vaccination intent.
Methods
Data source and study sample
The data used in this study were drawn from the 2021 collection cycle of the Canadian Community Health Survey. The CCHS is an annual cross-sectional and nationally representative survey conducted by Statistics Canada. Briefly, the survey collects information on health status, health care utilization and health determinants for Canadians 12 years or older residing in the 10 provinces and 3 territories, excluding full-time members of the Canadian Forces, children in foster care, those who live in institutions, those who live on reserve, as well as those living in Nunavik and Terres-Cries-de-la-Baie-James. The survey sample was selected using a multistage stratified cluster design. Due to the complex survey design, survey weights were given to each respondent and were calibrated by province, age group, and sex to ensure that the sample data is representative of the Canadian population. More details on the survey design and sampling method are available in a previously published report [13]. In September 2020, questions about experiences related to the pandemic along with a question on COVID-19 vaccination intent were introduced, followed by a question on COVID-19 vaccination uptake in March 2021.
The CCHS has multiple non-overlapping collection periods throughout the year and this study is based on the collection period for the months of June to August 2021. For this specific period, data was collected between June 1st and September 5th exclusively using computer-assisted telephone interviewing (CATI). The data file used for the current study included only respondents living in the provinces for a total of n = 10,093 participants. Since adolescents 12 to 17 years old were only offered appointments for COVID-19 vaccines towards the end of May in most provinces and would not have had sufficient time to get vaccinated prior to the start of the data collection period, they were excluded from this study resulting in a final sample of n = 9,509. The response rate for the population of study, Canadians aged 18 and older living in the provinces, was 22.6%.
Measures
Respondents were asked to provide information on sociodemographic and health-related characteristics, as well as experiences during the COVID-19 pandemic.
Vaccination status
Participants were asked the following question: “Have you been vaccinated against COVID-19?” to which they could respond with “Yes, received at least one dose” or “No”. The responses from this question were used to represent vaccination status as one of two binary outcome variables.
Vaccination intent
For those who responded “No” to the previous question, a follow-up question was asked: “How likely is it that you would get a COVID-19 vaccine? Would you say…?” to which respondents answered using a 4-point Likert scale: ‘Very likely’, ‘Somewhat likely’, ‘Somewhat unlikely’, and ‘Very unlikely’. Responses were then regrouped to derive the second binary outcome variable, vaccination intent. Respondents who said they were vaccinated with at least one dose and those who were not vaccinated but who reported being very or somewhat likely to get a vaccine were recoded as being “vaccinated or likely to get vaccinated”. Those who reported being very or somewhat unlikely to get a vaccine were recoded as being “unlikely to get vaccinated”.
Sociodemographic factors
The CCHS collects information on several sociodemographic factors. For this study, predictors of interest were selected a priori based on factors previously demonstrated to be related to the modeled outcome according to literature and/or factors considered by the authors to conceptually have a potential association. Region of residence, age group, gender, level of education, Indigenous status, employment status, marital status, immigration status or country of birth, visible minority status, presence of children under 12 years old in the household, mother tongue, household composition, and dwelling ownership status were included as predictors. Data from Newfoundland and Labrador, Prince-Edward-Island, New Brunswick, and Nova Scotia were combined into the Atlantic Region; the three Prairie provinces (Manitoba, Saskatchewan, and Alberta) were also regrouped given the smaller sample sizes in these provinces. Moreover, due to a small number of observations under “other” gender identities, this group was excluded and gender was regarded as a binary variable (males and females). For similar reasons, the Indigenous status variable was regrouped into two categories, Indigenous and non-Indigenous, and the visible minority status variable was reported as either not a visible minority or part of a visible minority. It was not possible to obtain information on household income. Instead, education, dwelling ownership status, and household composition were used as proxy variables for socioeconomic status (SES). The former two indicators have also been used as valid SES measures in other studies [14]. Household composition is also used as a proxy for SES since it has been found that poverty rates change based on the type of household composition [15].
Health-related factors
Many health-related questions were included in the CCHS. For this study, we focused on questions regarding status of COVID-19 diagnosis, perceived health status, and having a regular healthcare provider as additional predictor variables.
Control variables
Region of residence, age group, and Indigenous status were used to adjust for differences in vaccination rollout plans and vaccination eligibility across the provinces. Therefore, any association observed between vaccination status and control variables should be interpreted with caution as differences in provincial vaccine eligibility could confound them.
Statistical analysis
All analyses were conducted using SAS software version 9.4 of the SAS System for Windows.1 Descriptive statistics (frequencies and percentages) were computed to examine the distribution of vaccination status, vaccination intent, as well as sociodemographic factors in the population. To compare vaccination status among sociodemographic groups, the proportion of unvaccinated individuals was broken down by sociodemographic factors. Likewise, the proportion of those unlikely to get vaccinated by sociodemographic factor was also calculated to compare vaccination intent among different groups. The confidence interval of these proportions were then adjusted using the Wilson interval to account for the normal approximation of the binomial distribution [16]. For the final analysis, unadjusted (simple) and adjusted (multiple) logistic regression models were employed to examine associations between the response (vaccination status or intent) and predictor (sociodemographic and health-related) variables. The unadjusted models ran each of the predictor variables against each of the two outcomes, whereas the adjusted models included all predictor variables in the model.
To identify the sociodemographic determinants of non-vaccination and low vaccination intent, we examined the odds ratios (OR) generated by the logistic regression models. Specifically for vaccination status, we tested differences in the odds of being unvaccinated versus having at least one dose among sociodemographic groups. Similarly, for intent, we tested differences in the odds of being unlikely to get vaccinated versus being already vaccinated or likely to get vaccinated. A Tukey–Kramer adjustment was applied to the confidence intervals associated with the odds ratios to account for multiple comparisons.
Sampling weights were used to obtain accurate and representative estimates for the proportions and odds ratios, and their corresponding estimated variances were calculated using 1,000 bootstrap weights. All estimates were computed using a significance level of alpha = 0.05.
Results
A total of 9,509 adult respondents from the 10 provinces were included in the analyses. Table 1 describes the sociodemographic distribution of the study sample. Of the five regions, British Columbia had the least number of respondents (9.1%) while Ontario had the most (30.6%). For gender, 55.7% of the sample were female, 44.1% were male and 0.2% had other or unknown gender identity. Sample proportions increased with increasing age groups from 8.1% in the 18–29 age group to 29.4% in the 70 and over. Almost two thirds of the sample had at least a post-secondary education (63.7%) and more than half (55.9%) were either married or living common-law. Lastly, 4.6% reported being Indigenous (i.e. identifying with at least one of the three Indigenous groups: First Nations, Métis, or Inuit) and 10.0% identified as being part of a visible minority group.
Table 1.
Characteristics of survey respondents
| Variables | Unweighted | Weighted | |
|---|---|---|---|
| Frequency (n) | Percent (%) | Percent (%) | |
| Region of Residence | |||
| Atlantic | 1893 | 19.9 | 6.6 |
| Quebec | 1540 | 16.2 | 22.7 |
| Ontario | 2906 | 30.6 | 39.4 |
| Prairies | 2309 | 24.3 | 17.4 |
| British Columbia | 861 | 9.1 | 13.9 |
| Gender | |||
| Female | 5295 | 55.7 | 50.7 |
| Male | 4197 | 44.1 | 49.3 |
| Other or Unknown | 17 | 0.2 | - |
| Age Group | |||
| 18–29 | 769 | 8.1 | 18.2 |
| 30–39 | 1210 | 12.7 | 17.6 |
| 40–49 | 1150 | 12.1 | 16.7 |
| 50–59 | 1346 | 14.2 | 15.3 |
| 60–69 | 2242 | 23.6 | 17.1 |
| 70 + | 2792 | 29.4 | 15.2 |
| Level of Education | |||
| Less than secondary | 1263 | 13.3 | 9 |
| Secondary | 2129 | 22.4 | 22.1 |
| Post-secondary | 3144 | 33.1 | 31.4 |
| University | 2913 | 30.6 | 37.5 |
| Unknown | 60 | 0.6 | - |
| Marital Status | |||
| Married/Common law | 5317 | 55.9 | 61.7 |
| Divorced/Separated/Widowed | 2236 | 23.5 | 12.1 |
| Single | 1945 | 20.5 | 26.2 |
| Unknown | 11 | 0.1 | - |
| Indigenous Identitya | |||
| Indigenous | 433 | 4.6 | 3.2 |
| Non-indigenous | 8966 | 94.3 | 96.8 |
| Unknown | 110 | 1.2 | - |
| Indigenous Identity | |||
| First Nation | 196 | 2.1 | 1.4 |
| Metis | 209 | 2.2 | 1.7 |
| Inuit | F | F | F |
| Multiple | F | F | F |
| Non-indigenous | 8966 | 94.3 | 96.9 |
| Unknown | 119 | 1.3 | - |
| Visible Minority Status | |||
| Visible minority | 951 | 10 | 22.5 |
| Not a visible minority | 8426 | 88.6 | 77.5 |
| Unknown | 132 | 1.4 | - |
| Immigration Status | |||
| Non-Immigrant | 7827 | 82.3 | 73.5 |
| Immigrant | 1465 | 15.4 | 24.3 |
| Non-permanent resident | 117 | 1.2 | 2.3 |
| Unknown | 100 | 1.1 | - |
| Country of Birth | |||
| Canada | 7827 | 82.3 | 73.2 |
| Other | 1596 | 16.8 | 26.8 |
| Unknown | 86 | 0.9 | - |
| COVID-19 Status | |||
| Had COVID-19 | 181 | 1.9 | 3.6 |
| Did not have COVID-19 | 9050 | 95.2 | 96.4 |
| Unknown | 278 | 2.9 | - |
| Household Composition | |||
| Unattached | 3176 | 33.4 | 16 |
| Couple | 3286 | 34.6 | 29.1 |
| Couple with children | 2100 | 22.1 | 41.5 |
| Lone with children | 679 | 7.1 | 8.2 |
| Other or Unknown | 268 | 2.8 | 5.2 |
| Employment Status | |||
| Employed | 4497 | 47.3 | 62.4 |
| Unemployed | 3483 | 36.6 | 29.5 |
| Not in the labour force | 1486 | 15.6 | 8.1 |
| Unknown | 43 | 0.5 | - |
| Having a Regular Healthcare Provider | |||
| Yes | 8360 | 88 | 85.3 |
| No | 1129 | 11.9 | 14.7 |
| Unknown | 13 | 0.1 | - |
| Self-Perceived Health | |||
| Excellent, very good or good | 8072 | 84.9 | 88.5 |
| Fair or poor | 1426 | 15 | 11.5 |
| Unknown | 11 | 0.1 | - |
| Children under 12 in the household | |||
| None | 8159 | 85.8 | 79.8 |
| 1 or more | 1350 | 14.2 | 20.2 |
| Mother Tongue | |||
| English or French | 8394 | 88.2 | 81.9 |
| Neither English or French | 1018 | 10.7 | 18.1 |
| Unknown | 97 | 1 | - |
| Dwelling Ownership Status | |||
| Rent | 1991 | 20.9 | 22.7 |
| Own | 7431 | 78.1 | 77.3 |
| Unknown | 87 | 0.9 | - |
| Vaccination Status | |||
| At least one dose | 8151 | 85.7 | 88.7 |
| Unvaccinated | 1072 | 11.3 | 11.3 |
| Unknown | 286 | 3 | - |
| Vaccination Intent | |||
| Likely | 494 | 5.2 | 6 |
| Unlikely | 553 | 5.8 | 5 |
| Already vaccinated | 8151 | 85.7 | 89 |
| Unknown | 311 | 3.3 | - |
a Indigenous group includes First Nations, Metis, and/or Inuit
F Suppressed due to data quality concerns and/or confidentiality reasons
Vaccination
According to this nationally representative sample, COVID-19 vaccination coverage in the ten Canadian provinces from June to September 2021 was 89% (Table 2). Overall, the proportion of unvaccinated did not differ by region. Differences across genders, visible minority status, mother tongue, and history of COVID-19 diagnosis were also not detected although vaccination rates improved with increasing age.
Table 2.
Associations between sociodemographic factors and vaccination status: Odds of being unvaccinated vs. vaccinated
| Predictors | Sample Sizea | % Not vaccinated | Simple Logistic Regression | Multiple Logistic Regressionb | ||
|---|---|---|---|---|---|---|
| n | % (95% CIc) | OR (95% CId) | P-value | aOR (95% CId) | P-value | |
| Overall | 9223 | 11 (10–13) | ||||
| Region of Residencee | ||||||
| Atlantic | 1812 | 10 (9–13) | 1.1 (0.7–1.6) | 0.996 | 1.3 (0.8–2.1) | 0.493 |
| Quebec | 1513 | 10 (8–12) | Reference | Reference | ||
| Ontario | 2808 | 12 (10–14) | 1.2 (0.8–1.9) | 0.81 | 1.5 (0.9–2.5) | 0.227 |
| Prairies | 2253 | 13 (11–15) | 1.3 (0.8–2.1) | 0.412 | 1.5 (0.9–2.6) | 0.179 |
| British Columbia | 837 | 11 (8–14) | 1.1 (0.6–1.9) | 0.989 | 1.5 (0.8–2.7) | 0.446 |
| Age Groupe | ||||||
| 18–29 | 752 | 17 (13–21) | 4.4 (2.6–7.4) | < 0.001 | 6.0 (2.5–14.7) | < 0.001 |
| 30–39 | 1183 | 15 (12–18) | 3.8 (2.3–6.3) | < 0.001 | 5.9 (2.5–13.7) | < 0.001 |
| 40–49 | 1139 | 13 (11–17) | 3.5 (2.1–5.7) | < 0.001 | 5.1 (2.2–11.9) | < 0.001 |
| 50–59 | 1331 | 9 (8–12) | 2.3 (1.4–3.8) | < 0.001 | 3.2 (1.5–6.8) | < 0.001 |
| 60–69 | 2193 | 7 (6–9) | 1.8 (1.1–2.9) | 0.018 | 1.8 (0.9–3.6) | 0.114 |
| 70 + | 2625 | 4 (3–6) | Reference | Reference | ||
| Indigenous Identitye | ||||||
| Indigenous | 419 | 19 (13–26)E | 1.9 (1.2–2.9) | 0.004 | 1.4 (0.8–2.2) | 0.214 |
| Non-Indigenous | 8697 | 11 (10–12) | Reference | Reference | ||
| Gender | ||||||
| Male | 4009 | 11 (9–12) | 1.2 (0.9–1.4) | 0.185 | 1.1 (0.9–1.4) | 0.36 |
| Female | 5199 | 12 (10–14) | Reference | Reference | ||
| Level of Education | ||||||
| Less than secondary | 1181 | 16 (12–20) | 2.5 (1.5–4.0) | < 0.001 | 3.5 (2.1–6.1) | < 0.001 |
| Secondary | 2063 | 13 (11–16) | 2.0 (1.4–3.1) | < 0.001 | 2.4 (1.5–3.7) | < 0.001 |
| Post-secondary | 3070 | 14 (12–16) | 2.1 (1.4–3.0) | < 0.001 | 2.5 (1.6–3.7) | < 0.001 |
| University | 2856 | 7 (6–9) | Reference | Reference | ||
| Employment Status | ||||||
| Employed | 4443 | 12 (10–14) | Reference | Reference | ||
| Unemployed | 3371 | 11 (10–13) | 1.0 (0.7–1.3) | 0.901 | 1.2 (0.8–1.6) | 0.618 |
| Not in the labour force | 1367 | 4 (3–6)E | 0.3 (0.2–0.5) | < 0.001 | 0.9 (0.4–1.8) | 0.892 |
| Marital Status | ||||||
| Divorced/Separated/Widowed | 2189 | 13 (11–16) | 1.5 (1.1–2.2) | 0.011 | 1.6 (0.8–3.2) | 0.297 |
| Single | 1901 | 16 (13–19) | 1.8 (1.4–2.5) | < 0.001 | 1.2 (0.7–2.2) | 0.634 |
| Married/Common law | 5122 | 9 (8–10) | Reference | Reference | ||
| Immigration Status | ||||||
| Non-Immigrant | 7604 | 11 (10–12) | Reference | Reference | ||
| Non-Permanent Resident | 112 | 27 (16–41)E | 3.1 (1.3–7.5) | 0.009 | 2.2 (0.8–6.2) | 0.182 |
| Immigrant | 1411 | 11 (9–14) | 1.1 (0.8–1.5) | 0.806 | 1.5 (0.9–2.3) | 0.147 |
| Visible Minority Status | ||||||
| Not a visible minority | 8170 | 11 (10–12) | Reference | Reference | ||
| Visible minority | 923 | 12 (9–15) | 1.1 (0.8–1.5) | 0.45 | 0.7 (0.4–1.2) | 0.178 |
| Mother Tongue | ||||||
| English or French | 8160 | 11 (10–12) | Reference | Reference | ||
| Neither English or French | 968 | 13 (10–17) | 0.9 (0.5–1.5) | 0.45 | 1.2 (0.7–1.8) | 0.512 |
| Children under 12 in the household | ||||||
| 1 or more | 1323 | 15 (12–17) | 1.5 (1.2–1.8) | 0.001 | 1.6 (1.1–2.4) | 0.013 |
| None | 7900 | 10 (9–12) | Reference | Reference | ||
| Household Composition | ||||||
| Unattached | 3147 | 13 (11–16) | 1.8 (1.2–2.7) | 0.001 | 1.3 (0.6–2.7) | 0.927 |
| Couple with children | 2052 | 11 (9–13) | 1.4 (0.9–2.1) | 0.14 | 0.6 (0.3–1.1) | 0.207 |
| Lone with children | 644 | 20 (15–25) | 2.9 (1.7–4.8) | < 0.001 | 1.1 (0.5–2.8) | 0.996 |
| Couple | 3119 | 8 (6–10) | Reference | Reference | ||
| Other, Unknown | 261 | 14 (9–22)E | 1.3 (0.9–1.7) | 0.135 | 0.8 (0.3–2.3) | 0.974 |
| Dwelling Ownership Status | ||||||
| Rent | 1949 | 15 (13–18) | 1.7 (1.3–2.1) | < 0.001 | 1.0 (0.7–1.3) | 0.829 |
| Own | 7190 | 10 (9–11) | Reference | Reference | ||
| Having a Regular Healthcare Provider | ||||||
| No | 1105 | 18 (14–22) | 1.9 (1.4–2.5) | < 0.001 | 1.6 (1.1–2.2) | 0.006 |
| Yes | 8098 | 10 (9–11) | Reference | Reference | ||
| Self-Perceived Health | ||||||
| Fair or poor | 1310 | 16 (13–20) | 1.6 (1.2–2.1) | 0.001 | 1.8 (1.3–2.4) | < 0.001 |
| Excellent, very good or good | 7903 | 11 (10–12) | Reference | Reference | ||
| COVID-19 Status | ||||||
| Did not have COVID-19 | 9029 | 11 (10–12) | 0.7 (0.4–1.4) | 0.342 | 0.7 (0.4–1.5) | 0.37 |
| Had COVID-19 | 181 | 14 (8–24)E | Reference | Reference | ||
Bold values indicate significant odds ratios after adjustment at the 5% level
a Sample sizes for proportions and simple logistic regression models do not always add up to the total n = 9,509 due to missing values in predictor and outcome variables
b Sample size for the multiple logistic regression is n = 8,908
c Wilson score interval for binomial proportions
d 95% confidence intervals for odds ratios (OR) were adjusted using the Tukey–Kramer method for multiple comparisons
e Covariates to control for provincial differences in vaccination rollout plans and vaccination eligibility
E Estimate is of marginal quality, use with caution
After adjusting for covariates, vaccination status was associated with level of education, presence of children under 12 years old in the household, having a regular healthcare provider, and self-perceived health (Table 2 and Fig. 1). Adults with education below university were more likely to be unvaccinated than university graduates, with adjusted odds ratios (aOR) ranging from 2.4 (95% CI 1.5–3.7) to 3.5 (95% CI 2.1–6.1). Those living with at least one child under 12 years old were also more likely to be unvaccinated than those living without children (aOR 1.6, 95% CI 1.1–2.4). The risk of being unvaccinated was also higher in those without a regular healthcare provider compared to those who had one (aOR 1.6, 95% CI 1.1–2.2) and in those who perceived their health as fair or poor compared to those who perceived it as excellent, very good or good (aOR 1.8, 95% CI 1.3–2.4). As expected, due to the vaccine rollout by descending age group, vaccination decreased significantly with decreasing age.
Fig. 1.
Adjusted odds ratios: Being unvaccinated versus vaccinated by sociodemographic and health factors
Intent to get vaccinated
Only 5% of the population did not intend to get vaccinated (Table 3). The proportion of those unlikely to get vaccinated were slightly higher in the Prairies compared to the other regions. Vaccination intent did not differ across Indigenous identity, gender, employment status, marital status, country of birth, mother tongue, dwelling ownership status, having a regular healthcare provider, or status of COVID-19 diagnosis. Based on the adjusted model, vaccination intent was associated with region of residence, age, level of education, visible minority status, presence of children under 12 years old in the household, household composition, and self-perceived health (Table 3 and Fig. 2). The risk of being unlikely to get vaccinated was greater in the Prairies compared to the risk in the province of Quebec (aOR 2.2, 95% CI 1.2–4.1). Additional comparisons among the regions also showed that risks were greater in the Prairies than in the Atlantic region. Greater risks were also observed in those less than 40 years old and between 50 to 59 compared to those 70 and over (aOR between 2.8, 95% CI 1.2–6.8 and 4.0, 95% CI 1.3–12.3). The intent not to get vaccinated was more frequent in individuals with no university degree than in university graduates (aOR between 2.5, 95% CI 1.5–4.3 and 3.8, 95% CI 1.9–7.6). The intent not to get vaccinated was also more frequent in those living with at least one child under 12 years old than in those with no children (aOR 1.8, 95% CI 1.1–2.9), more frequent in unattached individuals than in those living in a couple (aOR 2.6, 95% CI 1.1–6.1), and more frequent in those who perceived their health as fair or poor than in those perceiving it as excellent, very good or good (aOR 2.0, 95% CI 1.3–2.9). However, decreased risks (aOR 0.3, 95% CI 0.2–0.7) of being unlikely to get vaccinated were observed in those who are part of a visible minority group compared to those who are not a visible minority.
Table 3.
Sociodemographic indicators of intent: Odds of being unlikely to get vaccinated vs. likely or vaccinated
| Sample Sizea | Unlikely to get vaccinated | Simple Logistic Regression | Multiple Logistic Regressionb | |||
|---|---|---|---|---|---|---|
| Predictors | n | % (95% CIc) | OR (95% CId) | P-value | aOR (95% CId) | P-value |
| Overall | 9198 | 5 (4–6) | ||||
| Region of Residencee | ||||||
| Atlantic | 1804 | 4 (3–6) | 1.1 (0.6–2.0) | 0.988 | 1.2 (0.7–2.4) | 0.885 |
| Quebec | 1511 | 4 (3–5)E | Reference | Reference | ||
| Ontario | 2796 | 5 (4–7) | 1.3 (0.7–2.4) | 0.686 | 1.8 (1.0–3.4) | 0.083 |
| Prairies | 2251 | 7 (5–8) | 1.8 (1.0–3.2) | 0.064 | 2.2 (1.2–4.1) | 0.007 |
| British Columbia | 836 | 5 (3–7)E | 1.2 (0.6–2.6) | 0.964 | 1.8 (0.9–3.9) | 0.239 |
| Age Groupe | ||||||
| 18–29 | 749 | 6 (4–8)E | 1.9 (0.9–3.9) | 0.122 | 4.0 (1.3–12.3) | 0.005 |
| 30–39 | 1178 | 6 (4–8)E | 1.9 (1.0–3.6) | 0.054 | 3.0 (1.0–8.6) | 0.043 |
| 40–49 | 1131 | 6 (4–8)E | 1.9 (1.0–3.6) | 0.061 | 2.8 (1.0–8.0) | 0.052 |
| 50–59 | 1326 | 6 (4–7) | 1.9 (1.0–3.4) | 0.036 | 2.8 (1.2–6.8) | 0.011 |
| 60–69 | 2192 | 4 (3–6) | 1.4 (0.8–2.6) | 0.512 | 1.5 (0.7–3.3) | 0.763 |
| 70 + | 2622 | 3 (2–4) | Reference | Reference | ||
| Indigenous Identitye | ||||||
| Indigenous | 418 | 7 (4–11)E | 1.5 (0.9–2.4) | 0.115 | 0.8 (0.5–1.4) | 0.497 |
| Non-indigenous | 8674 | 5 (4–6) | Reference | Reference | ||
| Gender | ||||||
| Male | 3996 | 5 (4–6) | 1.1 (0.8–1.5) | 0.456 | 1.0 (0.8–1.4) | 0.79 |
| Female | 5187 | 5 (4–6) | Reference | Reference | ||
| Level of Education | ||||||
| Less than secondary | 1177 | 8 (6–11)E | 3.3 (1.8–6.0) | < 0.001 | 3.8 (1.9–7.6) | < 0.001 |
| Secondary | 2055 | 6 (5–8) | 2.5 (1.5–4.4) | < 0.001 | 2.6 (1.5–4.7) | < 0.001 |
| Post-secondary | 3064 | 6 (5–8) | 2.6 (1.6–4.2) | < 0.001 | 2.5 (1.5–4.3) | < 0.001 |
| University | 2849 | 3 (2–3)E | Reference | Reference | ||
| Employment Status | ||||||
| Employed | 4427 | 5 (4–6) | Reference | Reference | ||
| Unemployed | 3363 | 5 (4–6) | 1.0 (0.7–1.4) | 0.944 | 1.0 (0.7–1.5) | 0.999 |
| Not in the labour force | 1367 | 3 (2–5)E | 0.6 (0.4–1.0) | 0.063 | 0.9 (0.4–2.0) | 0.913 |
| Marital Status | ||||||
| Divorced/Separated/Widowed | 2185 | 6 (5–8) | 1.5 (1.0–2.2) | 0.065 | 0.7 (0.3–1.3) | 0.38 |
| Single | 1887 | 6 (4–8)E | 1.4 (0.9–2.1) | 0.132 | 0.8 (0.4–1.6) | 0.664 |
| Married/Common law | 5115 | 4 (4–5) | Reference | Reference | ||
| Country of Birth | ||||||
| Canada | 7586 | 5 (5–6) | Reference | Reference | ||
| Other | 1529 | 4 (3–6)E | 0.8 (0.5–1.1) | 0.131 | 1.7 (0.9–3.2) | 0.09 |
| Visible Minority Status | ||||||
| Not a visible minority | 8151 | 6 (5–6) | Reference | Reference | ||
| Visible minority | 920 | 3 (2–4)E | 0.5 (0.3–0.8) | 0.003 | 0.3 (0.2–0.7) | 0.004 |
| Mother Tongue | ||||||
| English or French | 8142 | 5 (4–6) | Reference | Reference | ||
| Neither English or French | 961 | 3 (2–5)E | 0.6 (0.4–1.0) | 0.055 | 0.8 (0.4–1.6) | 0.593 |
| Children under 12 in the household | ||||||
| 1 or more | 1319 | 6 (5–8) | 1.2 (0.9–1.8) | 0.161 | 1.8 (1.1–2.9) | 0.016 |
| None | 7879 | 5 (4–6) | Reference | Reference | ||
| Household Composition | ||||||
| Unattached | 3134 | 7 (6–9) | 2.1 (1.3–3.3) | < 0.001 | 2.6 (1.1–6.1) | 0.022 |
| Couple | 3116 | 4 (3–5) | Reference | Reference | ||
| Couple with children | 2047 | 4 (3–6) | 1.2 (0.7–2.0) | 0.909 | 0.4 (0.1–1.4) | 0.313 |
| Lone with children | 640 | 6 (4–10)E | 1.8 (0.9–3.5) | 0.132 | 1.3 (0.4–3.9) | 0.977 |
| Other or Unknown | 261 | 7 (4–13)E | 2.0 (0.7–5.5) | 0.312 | 1.7 (0.5–5.6) | 0.796 |
| Dwelling Ownership Status | ||||||
| Rent | 1935 | 6 (5–8) | 1.3 (1.0–1.8) | 0.095 | 0.9 (0.7–1.4) | 0.763 |
| Own | 7179 | 5 (4–5) | Reference | Reference | ||
| Having a Regular Healthcare Provider | ||||||
| No | 1101 | 6 (4–8)E | 1.2 (0.8–1.7) | 0.291 | 1.1 (0.8–1.8) | 0.529 |
| Yes | 8077 | 5 (4–6) | Reference | Reference | ||
| Self-Perceived Health | ||||||
| Fair or poor | 1305 | 9 (6–12)E | 2.0 (1.4–2.9) | < 0.001 | 2.0 (1.3–2.9) | < 0.001 |
| Excellent, very good or good | 7884 | 5 (4–5) | Reference | Reference | ||
| COVID-19 Status | ||||||
| Did not have COVID-19 | 9004 | 5 (4–6) | 1.2 (0.6–2.4) | 0.52 | 1.1 (0.5–2.2) | 0.865 |
| Had COVID-19 | 181 | F | Reference | Reference | ||
Bold values indicate significant odds ratios after adjustment at the 5% level
a Sample sizes for proportions and simple logistic regression models do not always add up to the total n = 9,509 due to missing values in predictor and outcome variables
b Sample size for the multiple logistic regression is n = 8,905
c Wilson score interval for binomial proportions
d 95% confidence intervals for odds ratios (OR) were adjusted using the Tukey–Kramer method for multiple comparisons
e Covariates to control for provincial differences in vaccination rollout plans and vaccination eligibility
E Estimate is of marginal quality, use with caution
F Estimate is suppressed due to data quality concerns
Fig. 2.
Adjusted odds ratios: Unlikely to get vaccinated versus likely or vaccinated by sociodemographic factors
Discussion
COVID-19 vaccination
In this study, vaccination coverage among Canadian adults was high, with 89% having received at least one dose of a COVID-19 vaccine. Only 11% of the population were unvaccinated. This coverage is somewhat higher than what was reported by the Canadian COVID-19 vaccination coverage surveillance system where by beginning of September 2021, 84% of those 18 and older received at least one dose, which may be explained by differences between the CCHS respondents and the general population [17]. Among all the sociodemographic factors included in the vaccination status model, age, level of education, presence of children under 12 years old in the household, having a healthcare provider and self-perceived health were identified as significant determinants of COVID-19 vaccine uptake.
The proportion of unvaccinated individuals decreased with increasing age ranging from 17% in 18–29 years old to 4% in those aged 70 years or over. This can be partially explained by the vaccination rollout, as the elderly population was eligible to get vaccinated earlier in the campaign [18]. Analogously, some studies highlighted that risk perceptions toward COVID-19 differ by age [19, 20]. Given that the severity and mortality of COVID-19 increases with age [21], older adults might feel more at risk, thus more motivated to be vaccinated. In fact, increased risk perceptions of COVID-19 have also been shown to be a strong predictor of COVID-19 vaccine acceptance [22].
In this study, only one of the three proxy variables for SES, namely education, was significantly associated with vaccination status. Individuals with less than university education had a higher risk of being unvaccinated than university graduates. Similarly, a recent study in the US looked at patterns in COVID-19 vaccination coverage among adults and reported that vaccination uptake was lower among adults with low educational attainment, which is consistent with our results [23]. Education is proven to be associated with greater engagement in pro-health behaviors which could be seen as a factor in favor of vaccination [24].
According to the CCHS results, individuals who lived with at least one child under 12 years old had a higher risk of being unvaccinated. One might postulate that this association is driven by age since individuals living with young children are, for the vast majority, younger adults. However, it should be noted that this association is still significant when adjusted for age groups. A study in the US found similar results where the presence of children was negatively associated with COVID-19 vaccination [23]. As postulated by Bell et al., this may be related to access barriers to vaccination; parents of younger children may face obstacles to schedule and attend vaccination appointments due to competing priorities [25].
The risk of being unvaccinated was also significantly higher in those who had fair or poor self-perceived health compared to those with excellent, very good or good self-perceived health (aOR 1.8). This could be explained by the fact that individuals with poor health had less intent to get vaccinated, and therefore the coverage was lower. A study in the U.S found that those with underlying medical conditions and BMI > 40 were not more willing to get vaccinated than those without these risk factors [26]. This could be associated with different perceptions on vaccine safety, side effects and effectiveness among those with poor health. One study demonstrated that people cared more about the vaccine’s health risk than its effectiveness [27]. Therefore, those with poor health may be more concerned with health risks associated with getting vaccinated than being immunized against COVID-19. On top of that, reduced COVID-19 mortality risk following immunization may in part explain the current finding as it suggests substantial “healthy vaccinee effects” which refers to a situation when vaccinated individuals tend to be healthier than unvaccinated individuals [28]. This pattern is the opposite of what was observed for influenza vaccination in Canada in previous cycles of the same survey (CCHS) where excellent self-perceived health was associated with non-vaccination among adults aged 18 to 64 years with a chronic medical condition and in adults aged 65 years and older [29].
Finally, having a regular healthcare provider was positively associated with COVID-19 vaccine uptake. It is conceivable that individuals with a regular healthcare provider may have easier access to health-related resources and may be more willing to get vaccinated in order to protect themselves from the disease. Additionally, multiple studies have demonstrated that those who are hesitant to get a COVID-19 vaccine are concerned about the safety of the vaccines and the risks and side effects attached to it [22, 30–33]. Considering healthcare providers as being one of the trusted sources of information on vaccination, they may help to soothe the fear and concerns over COVID-19 vaccines, reassure their patients on the safety and effectiveness of the vaccines, and promote vaccination during consultations, which can therefore improve vaccine uptake [8, 34].
COVID-19 vaccination intent
The proportion of the population who did not intend to get vaccinated against COVID-19 was as low as 5%. When adjusting for all other predictor variables, lower vaccination intent was significantly associated with region, younger age, lower educational attainment, not being part of a visible minority group, presence of children under 12 years in the household, unattached individuals and poor self-perceived health.
Vaccination intent differed between the Canadians provinces. Individuals living in the Prairies had higher risks of not intending to get vaccinated compared to other provinces. In the same vein, another Canadian study also found that these three provinces had higher proportions of individuals who did not intend to get vaccinated [7]. However, once adjusted for other sociodemographic factors, these differences were not significant despite individuals from Alberta having higher predicted probability of not intending to get vaccinated [7].
Adults younger than 40 years old and between 50 to 59 had lower COVID-19 vaccination intent than those aged 70 or over. Other Canadians studies had similar results where individuals below 60 years of age demonstrated lower intent to get vaccinated [5, 7]. A systematic review of 45 studies conducted in various countries hypothesized that older individuals have a greater sense of responsibility and accountability for themselves and their surroundings compared to the younger population which may also explain why older individuals were more likely to be vaccinated [35].
Following the pattern of vaccination status, the intent not to get vaccinated was more frequent in individuals with no university degree than in those who held such a degree. This is in agreement with another Canadian study that reported having a university education level as one of the strongest predictors of COVID-19 vaccine intention [22]. Education level plays an important role in vaccination acceptance as it highly correlates with belief in COVID-19 vaccine safety [36]. According to Kricorian et al., individuals who believed COVID-19 vaccines to be unsafe were likely to have difficulty understanding scientific information, higher mistrust in scientific research, and not to follow scientific recommendations. This could contribute to the lower intent of receiving the vaccine.
Moreover, visible minorities overall were found to be more eager to get vaccinated than the rest of the population. A major caveat to this finding was that it applies to visible minorities as a whole, as the number of participants from these groups in this study was not sufficient to analyse them separately. Supporting evidence from a US study indicates that some visible minority groups such as Asians and Hispanics are less likely to have vaccine hesitancy than Whites across all hesitancy measures [37]. Nevertheless, according to other studies in other countries, higher vaccine hesitancy was observed in most minority ethnic groups compared to the White British or Irish group; and identifying as Black or African American was associated with lower vaccination likelihood as opposed to identifying as White [38, 39]. The association between visible minority status and vaccination intent observed in the current study may in part be explained by the multi-ethnic characteristic of the Canadian healthcare workers. In Canada, visible minorities account for approximately one third of nurse aides, orderlies and patient service associates, with higher proportions of Black, Filipino and South Asian workers in these occupations [40]. In addition to having been prioritized for vaccination, being at increased risk of COVID-19 infection and transmission may contribute to healthcare workers increased willingness to get vaccinated. Further exploration is essential to better understand the association between the various visible minority groups and COVID-19 vaccination intent.
Presence of children under 12 years old in the household was negatively associated with COVID-19 vaccination intent (aOR 1.8). A Canadian study on predictors of vaccine hesitancy for COVID-19 public health messaging implications revealed that having more than three children in the family is a strong determinant of immunization noncompliance [41]. This finding is also consistent with other research where presence of children in the household increased the odds of vaccine hesitancy [37, 42]. It could seem counterintuitive given that having multiple children ought to encourage parents to vaccinate in order to prevent cross-infection within the household. Nonetheless, relations between family size and vaccination intent may be explained through other socioeconomic factors.
Additionally, unattached individuals had lower COVID-19 vaccination intent than coupled individuals. A US nationwide study on predictors of intention to vaccinate against COVID-19 also demonstrated that having a spouse or partner was associated with higher anticipated likelihood of vaccination [43]. Unattached individuals might not have as much collective family responsibilities as married individuals and those with children, which could explain their lower vaccination intent [35].
Lastly, the current study showed that individuals with fair or poor self-perceived health had lower intention to vaccinate against COVID-19 than those with excellent, very good, good self-perceived health. This is in agreement with a study on COVID-19 vaccine hesitancy associated factors in Saskatchewan where individuals with very good or excellent health status were more likely to vaccinate than those with poor of fair health status [6]. However, more research is warranted to examine the association between self-perceived health and COVID-19 vaccination intent, especially since many perceived that aspects of their overall health had deteriorated during the pandemic [44].
In the present study, some sociodemographic factors such as gender, immigration status, Indigenous identity, and employment status were not significantly associated with COVID-19 vaccination uptake or intent. However, previous studies conducted in Canada showed that being a male was positively associated with vaccination intent [22, 45]. Although no difference in uptake for Indigenous status was observed in the adjusted model, Indigenous groups might still differ from non-Indigenous. It should be noted that statistical non-significance is not proof of absence of an association. Sometimes, the non-significant result is due to lack of power rather than lack of effect; the sample size of Indigenous respondents might be too small to provide sufficient power to detect an association. This can also be true for small groups of other variables such as immigration status or COVID-19 status. Other Canadian studies with various sample sizes of Indigenous respondents and somewhat different target populations found that Indigenous groups and individuals born outside of Canada had lower odds of getting vaccinated [5–7].
Given the paucity of studies assessing inequalities in COVID-19 vaccination uptake and intent, further work is needed for a deeper understanding of the contributing factors in the Canadian context.
Factors other than sociodemographic can also play a role in vaccination uptake and intent. Health inequities, vaccine hesitancy as well as knowledge, attitudes and beliefs (KABs) are among the multitude of factors that can have an impact. Although some KABs have been associated with sociodemographic characteristics, including only sociodemographic variables in the models might not provide a comprehensive picture. Unfortunately, information on KABs was not collected in the CCHS. Nonetheless, the assessment of sociodemographic factors can inform interventions by identifying target groups. Some people do not intend to get vaccinated due to concerns about the safety and effectiveness of the vaccine [22]. The novelty of COVID-19 vaccines could also play a role in Canadians’ intent to get vaccinated, as well as their lack of knowledge about vaccination [22, 45].
Strengths and limitations
As with any large scale survey, the CCHS has several strengths and limitations that must be carefully considered when interpreting the results. A major strength of the survey was the sufficiently large sample size to allow for analysis by several sociodemographic and health-related factors. Additionally, given the complex survey design and the use of survey weights, the findings are nationally representative and allows us to make inferences to the Canadian population. This study can also be a catalyst to potential additional works to examine hypotheses on changes of vaccination status and intent over time, on intent at the provincial level, and on the impact of additional sociodemographic indicators such as household income and rural/urban living area. Most importantly, this study is one of few that examine vaccination status and intent at the national level in Canada, contributing to the growing body of research on COVID-19 vaccine acceptance or hesitancy.
Some study limitations need to be acknowledged. The CCHS shares the usual limitations of surveys based on self-reporting which may be subject to recall bias given that the data was collected more than 7 months after the beginning of COVID-19 vaccination. However, recall bias is less likely to occur in the present study due to high media coverage surrounding the COVID-19 vaccination campaign and the proof of vaccination credentials issued by many jurisdictions across Canada. There are also some limitations to collecting data only through telephone interviews [46]. As a result of the COVID-19 pandemic, no computer-assisted personal interviewing (CAPI) was conducted in 2021; only CATI was used to collect data. Consequently, CATI is limited by the fact that participants have the possibility to not answer the phone whereas they are a lot less comfortable refusing an interview when they are facing the interviewer in person often resulting in lower response rates for CATI compared to CAPI. Indeed, the CCHS response rates significantly decreased in 2021. As was done for previous CCHS cycles, survey weights were adjusted to minimize any potential bias that could arise from survey non-response; non-response adjustments and calibration using available auxiliary information were applied. Despite these rigorous adjustments and validations, the higher non-response rate increases the risk of a remaining bias and increases the magnitude with which such a bias could impact estimates produced using the survey data. Moreover, selection bias cannot be ruled out since individuals with greater interest in the topic could be more likely to respond to the survey. In addition, as with all surveys, the social desirability bias needs to be considered.
In addition, the small number of observations among visible minority groups prohibited a more detailed breakdown of the visible minority status variable by individual visible minority group. This may explain why our finding on visible minority is inconsistent with other studies conducted in Canada or elsewhere. As with many other Statistics Canada surveys, the CCHS excluded First Nations on-reserve communities. Moreover, for the Indigenous status variable, the small number of observations did not allow a further analysis broken down by First Nation, Métis and Inuit. Future research should strive to include a sufficient number of visible minority and Indigenous participants to allow more detailed analyses of intent to get vaccinated and vaccination coverage in these populations. Continued collection would allow for data pooling to increase the sample size and further explore sub-populations.
Conclusion
Overall, a vast majority of the Canadian population was either vaccinated with at least one dose or likely to receive a COVID-19 vaccine. In this study, after adjustment for covariates, lower vaccination uptake was associated with younger age, lower educational attainment, presence of children in the household, not having a regular health care provider, and fair or poor self-perceived health. Furthermore, lower COVID-19 vaccination intent was associated with residing in the Prairies region, younger age, lower level of education, presence of young children in the household, fair or poor self-perceived health, not being part of a visible minority group and unattached individuals. Ongoing monitoring of inequalities in COVID-19 vaccination uptake and intent is needed to precisely identify vaccination barriers among partially vaccinated and unvaccinated populations. Addressing these barriers with better targeted interventions and promotion strategies is the key to achieve higher coverage rates and to protect all Canadians against the disease.
Acknowledgements
We are grateful to all the participants and to the outstanding collaborators from Statistics Canada; Haileigh McDonald, José Gaudet, Linda Lefebvre, and Matthew Olsheskie.
Abbreviations
- aOR
Adjusted odds ratio
- CATI
Computer-assisted telephone interviewing
- CCHS
Canadian Community Health Survey
- CI
Confidence interval
- COVID-19
Coronavirus disease of 2019
- HCP
Healthcare provider
- KABs
Knowledge, attitudes and beliefs
- OR
Odds ratio
- Ref
Reference
- SAS
Statistical Analysis System
- SES
Socioeconomic status
- US
United States
Authors’ contributions
All the authors contributed to the paper. The opinions expressed are those of the authors and do not necessarily reflect the views of the Public Health Agency of Canada or Statistics Canada. Study design and questionnaire development were performed by the Canadian Community Health Survey (CCHS) team at Statistics Canada. Data collection was performed by Statistics Canada. Data analysis was performed by Mireille Guay, Ruoke Chen, Aubrey Maquiling, Audrey Racine, Donalyne-Joy Baysac, and Valérie Lavergne. Results interpretation and insights for the discussion were provided by Ève Dubé, Shannon MacDonald, Nicolas Gilbert, MG, RC, AM, VL, DJB and AR. The first draft of the manuscript was written by MG, AM, RC, AR, VL and DJB, with co-authors providing comments and feedback on versions of the manuscript. All the authors read and approved the final manuscript.
Funding
No funding was received for the design of the study and collection, analysis and interpretation of data and in writing the manuscript.
Availability of data and materials
The dataset analyzed during the current study is available in the Statistics Canada Research Data Centres, https://www.statcan.gc.ca/en/microdata/data-centres.
Declarations
Ethics approval and consent to participate
All experiments and methods were carried out in accordance with relevant guidelines and regulations. The survey was carried out in compliance with the Statistics Act and other applicable laws and regulations. The Statistics Act prohibits Statistics Canada and any individual accessing Statistics Canada data from releasing any information it collects that could identify any person, business, or organization, unless consent has been given by the respondent or as permitted by the Act. Various confidentiality rules are applied to all data that are released or published to prevent the identification of survey participants or the publication or disclosure of any other information deemed confidential. If necessary, data are suppressed to prevent direct or residual disclosure of identifiable data.
All questionnaires used by Statistics Canada, including the CCHS questionnaire, have to be qualitatively tested and approved by Statistics Canada’s Questionnaire Design and Research Center. This process asks a set of representative participants to assess the content of the questionnaire, for overall understanding and appropriateness. All experimental protocols were approved by Statistics Canada’s Office of Privacy Management and Information Coordination and its Data Ethics Secretariat, which apply many of the same criteria as an IRB when reviewing requests for datasets. In addition, the Health Canada and Public Health Agency of Canada Research Ethics Board was consulted as they would be the IRB of record for this study. We were informed that this study is exempt from REB review pursuant to Article 2.2 of the Tri-Council Policy Statement on Ethical Conduct for Research Involving Humans (https://ethics.gc.ca/eng/policy-politique_tcps2-eptc2_2018.html). Statistics Canada’s CCHS data are considered information that is publicly available through a mechanism set out by legislation or regulation that is protected by law and therefore their use for research purposes does not require REB review, as long as there is no linkage to other datasets.
Informed consent was implied if respondents continued to respond to the telephone survey after the interviewer stated: “Your participation in this survey is voluntary and your responses will be kept confidential”. Informed consent was obtained from parents or legal guardians of minors 12 to 14 years of age.
Consent for publication
Not applicable.
Competing interests
The author(s) declare(s) that there is no conflict of interest.
Footnotes
Copyright © 2017 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Government of Canada . Canada reaches major vaccine campaign milestone. Moncton: Government of Canada; 2021. [Google Scholar]
- 2.Ismail SJ, Tunis MC, Zhao L, Quach C. Navigating inequities: a roadmap out of the pandemic. BMJ Glob Health. 2021;6(1):e004087. doi: 10.1136/bmjgh-2020-004087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iveniuk J, Leon S. An uneven recovery: Measuring COVID-19 vaccine equity in Ontario. Toronto (ON): Wellesley Institute; 2021. [Google Scholar]
- 4.Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob health action. 2015;8:27106. doi: 10.3402/gha.v8.27106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogilvie GS, Gordon S, Smith LW, Albert A, Racey CS, Booth A, et al. Intention to receive a COVID-19 vaccine: results from a population-based survey in Canada. BMC Public Health. 2021;21(1):1017. doi: 10.1186/s12889-021-11098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muhajarine N, Adeyinka DA, McCutcheon J, Green KL, Fahlman M, Kallio N. COVID-19 vaccine hesitancy and refusal and associated factors in an adult population in Saskatchewan, Canada: Evidence from predictive modelling. PLoS One. 2021;16(11):e0259513. doi: 10.1371/journal.pone.0259513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tang X, Gelband H, Nagelkerke N, Bogoch I, Brown P, Morawski E, et al. COVID-19 vaccination intention during early vaccine rollout in Canada: a nationwide online survey. Lancet Reg Health Am. 2021;2:100055. doi: 10.1016/j.lana.2021.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Public Health Agency of Canada . COVID-19 Vaccination Coverage Survey (CVCS) Ottawa (ON): Government of Canada; 2021. [Google Scholar]
- 9.Crane MA, Faden RR, Romley JA. Disparities in county COVID-19 vaccination rates linked to disadvantage and hesitancy. Health Aff. 2021;40(11):1792–1796. doi: 10.1377/hlthaff.2021.01092. [DOI] [PubMed] [Google Scholar]
- 10.Nafilyan V, Dolby T, Razieh C, Gaughan C, Morgan J, Ayoubkhani D, et al. Sociodemographic inequality in COVID-19 vaccination coverage amongst elderly adults in England: a national linked data study. BMJ Open. 2021;11(7):e053402. doi: 10.1136/bmjopen-2021-053402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perry M, Akbari A, Cottrell S, Gravenor MB, Roberts R, Lyons RA, et al. Inequalities in coverage of COVID-19 vaccination: a population register based cross-sectional study in Wales. UK Vaccine. 2021;39(42):6256–6261. doi: 10.1016/j.vaccine.2021.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.MacDonald NCJ, Dubé E, Graham J, Greenwood M, Harmon S, McElhaney J, McMurty CM, Middleton A, Steenbeek A, Taddio A. Royal society of Canada COVID-19 report: enhancing COVID-19 vaccine acceptance in Canada. FACETS. 2021;6:1184–1246. doi: 10.1139/facets-2021-0037. [DOI] [Google Scholar]
- 13.Statistics Canada . Canadian Community Health Survey - Annual component(CCHS) - 2021. Ottawa (ON): Gouvernment of Canada; 2021. [Google Scholar]
- 14.Coffee N, Lockwood T, Hugo G, Paquet C, Howard N. Relative residential property value as a socio-economic status indicator for health research. Int J Health Geogr. 2013;12:22. doi: 10.1186/1476-072X-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snyder AR, McLaughlin DK, Findeis J. Household composition and poverty among female-headed households with children: differences by race and residence. Rural Sociol. 2006;71(4):597–624. doi: 10.1526/003601106781262007. [DOI] [Google Scholar]
- 16.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;158:22. doi: 10.2307/2276774. [DOI] [Google Scholar]
- 17.Public Health Agency of Canada . Canadian COVID-19 vaccination coverage report. Ottawa (ON): Government of Canada; 2021. [Google Scholar]
- 18.National Advisory Committee on Immunization . Recommendations on the use of COVID-19 vaccines. Ottawa (ON): Public Health Agency of Canada; 2021. [Google Scholar]
- 19.Bruine de Bruin W. Age Differences in COVID-19 Risk Perceptions and Mental Health: Evidence From a National U.S. Survey Conducted in March 2020. J Gerontol B Psychol Sci Soc Sci. 2021;76(2):e24–e9. doi: 10.1093/geronb/gbaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosi A, Van Vugt F, Lecce S, Ceccato I, Vallarino M, Rapisarda F, et al. Risk perception in a real-world situation (COVID-19): how it changes from 18 to 87 years old. Front Psychol. 2021;12:646558. doi: 10.3389/fpsyg.2021.646558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wingert A, Pillay J, Gates M, Guitard S, Rahman S, Beck A, et al. Risk factors for severity of COVID-19: a rapid review to inform vaccine prioritisation in Canada. BMJ Open. 2021;11(5):e044684. doi: 10.1136/bmjopen-2020-044684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dubé E, Dionne M, Pelletier C, Hamel D, Gadio S. COVID-19 vaccination attitudes and intention among Quebecers during the first and second waves of the pandemic: findings from repeated cross-sectional surveys. Hum Vaccin Immunother. 2021:1–11. 10.1080/21645515.2021.1947096. [DOI] [PMC free article] [PubMed]
- 23.Barry V, Dasgupta S, Weller DL, Kriss JL, Cadwell BL, Rose C, Pingali C, Musial T, Sharpe JD, Flores SA, Greenlund KJ, Patel A, Stewart A, Qualters JR, Harris L, Barbour KE, Black CL. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity - United States, December 14, 2020-may 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(22):818–824. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Syan SK, Gohari MR, Levitt EE, Belisario K, Gillard J, DeJesus J, et al. COVID-19 vaccine perceptions and differences by sex, age, and education in 1,367 community adults in Ontario. Front Public Health. 2021;9. 10.3389/fpubh.2021.719665. [DOI] [PMC free article] [PubMed]
- 25.Bell CA, Simmonds KA, MacDonald SE. Exploring the heterogeneity among partially vaccinated children in a population-based cohort. Vaccine. 2015;33(36):4572–4578. doi: 10.1016/j.vaccine.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 26.Kelly BJ, Southwell BG, McCormack LA, Bann CM, MacDonald PDM, Frasier AM, et al. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect Dis. 2021;21(1):338. doi: 10.1186/s12879-021-06023-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cerda AA, García LY. Hesitation and refusal factors in individuals’ decision-making processes regarding a Coronavirus Disease 2019 vaccination. Front Public Health. 2021;9:626852. doi: 10.3389/fpubh.2021.626852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu S, Huang R, Sy L, Glenn S, Ryan D, Morrissette K, et al. COVID-19 vaccination and Non-COVID-19 mortality risk - seven integrated health care organizations, United States, December 14, 2020-July 31, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1520–1524. doi: 10.15585/mmwr.mm7043e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Roy M, Sherrard L, Dubé E, Gilbert NL. Determinants of non-vaccination against seasonal influenza. Health Rep. 2018;29(10):12–22. [PubMed] [Google Scholar]
- 30.Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021 doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen KH, Srivastav A, Razzaghi H, Williams W, Lindley MC, Jorgensen C, et al. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination - United States, September and December 2020. Am J Transplant. 2021;21(4):1650–1656. doi: 10.1111/ajt.16560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verger P, Scronias D, Dauby N, Adedzi KA, Gobert C, Bergeat M, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill. 2021;26(3). 10.2807/1560-7917.ES.2021.26.3.2002047. [DOI] [PMC free article] [PubMed]
- 33.Frank K, Arim R. Canadians’ willingness to get a COVID-19 vaccine when one becomes available: What role does trust play? Ottawa (ON): Statistics Canada; 2020. [Google Scholar]
- 34.Public Health Agency of Canada . Seasonal influenza vaccination coverage in Canada, 2019–2020. Ottawa (ON): Government of Canada; 2020. [Google Scholar]
- 35.Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “Vaccination Refusal could prolong the war of this pandemic” - a systematic review. Risk Manag Healthc Policy. 2021;14:2609–2623. doi: 10.2147/RMHP.S311074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kricorian K, Civen R, Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccines Immunother. 2022;18(1):1950504. doi: 10.1080/21645515.2021.1950504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu R, Li GM. Hesitancy in the time of coronavirus: Temporal, spatial, and sociodemographic variations in COVID-19 vaccine hesitancy. SSM Popul Health. 2021;15:100896. doi: 10.1016/j.ssmph.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agley J, Xiao Y, Thompson EE, Golzarri-Arroyo L. Factors associated with reported likelihood to get vaccinated for COVID-19 in a nationally representative US survey. Public Health. 2021;196:91–94. doi: 10.1016/j.puhe.2021.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson E, Edjoc R, Atchessi N, Striha M, Gabrani-Juma I, Dawson T. COVID-19: a case for the collection of race data in Canada and abroad. Can Commun Dis Rep. 2021;47(7–8):300–304. doi: 10.14745/ccdr.v47i78a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hudson A, Montelpare WJ. Predictors of vaccine hesitancy: implications for COVID-19 public health messaging. Int J Environ Res. 2021;18(15):8054. doi: 10.3390/ijerph18158054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruiz JB, Bell RA. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leigh PJ, Fiest K, Brundin-Mather RA-O, Plotnikoff K, Soo A, Sypes EE, et al. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: Self-reported beliefs, knowledge, and behaviors. PloS One. 2020;15(10):e0241259. doi: 10.1371/journal.pone.0241259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dzieciolowska S, Hamel D, Gadio S, Dionne M, Gagnon D, Robitaille L, et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. Am J Infect Control. 2021;49(9):1152–1157. doi: 10.1016/j.ajic.2021.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi BCK. Computer assisted telephone interviewing (CATI) for health surveys in public health surveillance: methodological issues and challenges ahead. Chronic Dis Can. 2004;25(2):21–27. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analyzed during the current study is available in the Statistics Canada Research Data Centres, https://www.statcan.gc.ca/en/microdata/data-centres.