Abstract
Wound healing is a recovering process of damaged tissues by replacing dysfunctional injured cellular structures. Natural compounds for wound treatment have been widely used for centuries. Numerous published works provided reviews of natural compounds for wound healing applications, which separated the approaches based on different categories such as characteristics, bioactivities, and modes of action. However, current studies provide reviews of natural compounds that originated from only plants or animals. In this work, we provide a comprehensive review of natural compounds sourced from both plants and animals that target the different bioactivities of healing to promote wound resolution. The compounds were classified into four main groups (i.e., anti-inflammation, anti-oxidant, anti-bacterial, and collagen promotion), mostly studied in current literature from 1992 to 2022. Those compounds are listed in tables for readers to search for their origin, bioactivity, and targeting phases in wound healing. We also reviewed the trend in using natural compounds for wound healing.
Keywords: wound healing, natural compounds, bioactivity, anti-inflammation, anti-oxidant, anti-bacterial, collagen promotion, targeting phase
1. Introduction
Wounds occur as a result of accidental or surgical trauma and from a variety of medical conditions. This wound often causes pain, inflammation, and loss of function, which affects a patient’s life and financial costs [1]. Wounds are classified as acute wounds or chronic wounds. Wound healing is a complex process of replacing damaged and dysfunctional cellular structures and tissue layers [2]. Acute wounds go through stages of healing, and signs of healing are well-defined within four weeks. Chronic wounds do not undergo normal progression through the healing phases, and healing is not apparent within four weeks. It can be said that the wound healing process depends on factors at the wound site, systemic mediators, type of injury, or any underlying disease [3]. Wound treatment is mainly performed by strategies such as physical closure of the wound margin, sutures, and dressings. When the wound is inaccessible, leave the wound open and let the damaged area clear itself and fill with connective tissue, and the healing process occurs sequentially through phases.
Natural compounds have been used for thousands of years to treat wounds. Natural compounds are found in many plants and animals, which are an abundantly available source for wound treatment. They have proven effective in healing through Chinese and Indian traditional medicines. Due to a vast number of natural compounds, reviews of those compounds would benefit readers and researchers in systematically finding interesting compounds and developing new products for wound healing treatment. Previously, many review papers discussed natural compounds for wound healing treatment [1,4,5,6,7,8,9,10,11,12]. For example, Ryall and colleagues discussed current advancements in skin delivery of natural bioactive compounds for wound management (e.g., turmeric, green tea, honey, garlic, aloe vera, etc.) [4]. Vitale et al. focused on medicinal plants’ phytochemistry and biological activity in wound healing [5]. Ataide and colleagues discussed the activities of pro-wound healing compounds and their mode of action [7]. Dumitru et al. discussed bee products for wound healing treatment [13]. Fana et al. reviewed natural wound healing compounds in traditional Iranian medicine [11]. Those reviews provided many natural compounds for wound healing treatment. However, they only gave tables or lists of natural compounds regarding categories, bioactivities, and mode of action. Those reviews lack discussion on which phase of wound healing natural compounds are affected. Readers might find difficulty when they want to search for information on interesting compounds (wound healing phase, category, chemical formula, mechanism, etc.).
Herein, we give a review of natural compounds (from both plants and animals) that play important roles in wound healing, also their healing mechanisms and limitations in use. We classified those compounds based on targeting bioactivities for wound healing. We also summarized the current trends in using natural compounds. We provided data tables for readers to search natural compounds regarding their origin, bioactivity, and targeting phases in wound healing.
2. The Process of Wound Healing
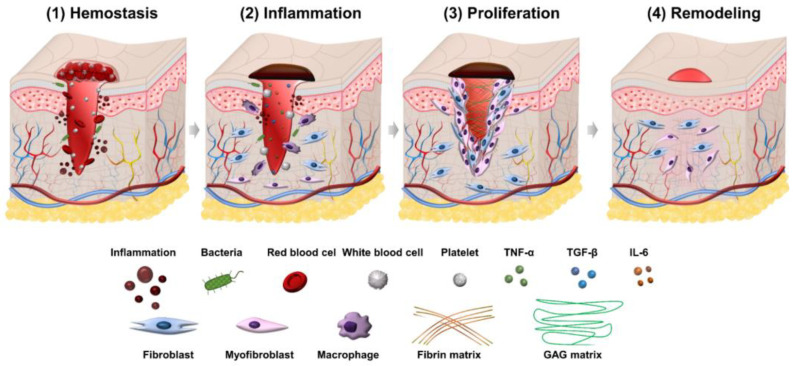
Wound healing is a process consisting of four phases: hemostasis, inflammation, proliferation, and remodeling. Illustration of the wound healing process is shown in Figure 1.
Figure 1.
Illustration of four phases in the wound healing process.
2.1. Hemostasis Phase
Wound healing first begins with hemostasis. The lymphatic vessels are injured in this phase, and blood flows out to remove microorganisms and antigens [14]. The body will activate different clotting cascades and thrombocytes to agglomerate by exposed collagen. At the same time, platelets activate vasoconstriction to reduce blood loss and fill tissue gaps in injured vessels with blood clots containing cytokines and growth factors [15]. The clot contains the molecules fibrin, fibronectin, vitronectin, and thrombospondin, which form a temporary matrix as a scaffolding structure for the migration of leukocytes, keratinocytes, fibroblasts, and endothelial cells, and it is a reservoir of growth factors that stabilize blood clots and avoid bleeding.
2.2. Inflammation Phase
The second phase of wound healing is inflammation which focuses on cleaning the wound and preparing for new tissue formation in the wound. This stage has the appearance of neutrophils and lasts about 2–5 days from when the wound becomes infected. Neutrophils can phagocytize and secrete proteases (elastase, cathepsin G, proteinase 3) that help destroy bacteria in the wound and deco remove debris. Neutrophils also release mediators (TNF-α, IL-1 and IL-6) to amplify the inflammatory response, stimulating VEGF and IL-8 to respond to repair during wound healing [16]. The macrophage process then supports the ongoing process by phagocytosis of the debris and secretion of growth factors, chemokines, and cytokines [17]. Macrophages promote and address inflammation, eliminate apoptotic, and support cell proliferation and tissue recovery after injury [18]. In the inflammatory phase, there are often symptoms of edema, erythema and pain.
2.3. Proliferation Phase
The proliferation phase is the most important phase of the wound healing process and lasts from 6 to 21 days. During the proliferation phase of wound healing, the wound is healed with fresh collagen and extracellular matrix tissue. After that, the wound shrinks as new tissues develop. A new network of blood vessels must be created for granulation tissues to remain healthy and receive an adequate supply of nutrients and oxygen. The modulation of fibroblasts toward myofibroblasts promotes the formation of granulation tissue. The myofibroblasts are characterized by the capacity to produce force and synthesize extracellular matrix components that allow the contraction of granulation tissue [19]. By gripping the wound boundaries and pulling them together, myofibroblasts use a technique akin to that of smooth muscle cells to close the wound. In the initial stages of wound healing, granulation tissue appears pink or red and has an uneven texture. Furthermore, healthy granulation tissue is clot-resistant [20,21]. Dark granulation tissue may be brought on by an infection, ischemia, or insufficient perfusion. Near the conclusion of the proliferation phase, epithelial cells resurface the wound. Keeping wounds moist accelerates epithelialization. Epithelialization occurs when occlusive or semi-occlusive dressings are applied within 48 h after the injury. This is because adequate tissue humidity is maintained. One accomplishment of the proliferation phase is replacing the temporary fibrin matrix with a new matrix made of collagen fibers, proteoglycans, and fibronectin to restore the structure and function of tissues. Another crucial stage of healing is angiogenesis, or the ingrowth of new capillaries to replace previously damaged vessels and restore circulation. The creation of granulation tissue and epithelialization are other important phenomena in this healing period. In the proliferation phase of healing, fibroblasts are the most important cells [22,23]. For fibroblasts to migrate in the extracellular matrix, they must first recognize and interact with particular matrix components. Fibroblasts in the normal dermis are usually dormant and sparsely scattered, but they are active and plentiful in the provisional matrix wound site and granulation tissue [24,25]. Their migration and aggregation in the wound site necessitate morphological changes and the production and secretion of proteases to clear a passage from the ECM into the wound site. The chemotactic growth factors, cytokines, and chemokines concentration gradient, as well as the alignment of the fibrils in the ECM and provisional matrix, control the direction of fibroblast migration. Rather than crossing these fibrils, fibroblasts prefer to move along them [26,27]. To help them move through the matrix, fibroblasts produce proteolytic enzymes on a local level. Collagenase (MMP-1), gelatinases (MMP-2 and MMP-9) that destroy gelatin substrates, and stromelysin (MMP-3), which has various protein substrates in the ECM, are three kinds of MMPs released by fibroblasts [28,29]. After migrating into the matrix, fibroblasts change shape, settle down, and begin to proliferate and generate granulation tissue components such as collagen, elastin, and proteoglycans. Fibroblasts connect to the provisional fibrin matrix cables and begin producing collagen [19,30]. Type III collagen, like other extracellular matrix proteins and proteoglycans, is generated in high amounts at first [31]. Collagen mRNA is connected to polyribosomes on the endoplasmic reticulum, where new collagen chains are formed after transcription and processing. A crucial stage in this process involves proline and lysine residue hydroxylation.
2.4. Remodeling Phase
Closure of acute and chronic wounds is regarded as the wound healing endpoint in most clinical settings, yet wounds can continue to undergo remodeling or tissue maturation for months or even years [32,33]. This final stage of wound healing decides whether scarring will occur and whether the wound will reoccur. Regression of the neo vasculature, a periodic deposition to the ECM, and subsequent reconstruction of granulation tissue to scar tissue are all part of the remodeling phase [26]. Collagen III makes up the majority of granulation tissue, which is gradually replaced by the stronger collagen I as the wound heals. This occurs due to simultaneous collagen I production and collagen III lysis, followed by ECM remodeling [34]. In the remodeling phase, scar tissues are created, and it might take several months or years to complete, depending on the severity and location of the wound, and used therapeutic procedures. During this time, the new tissue gradually gets stronger and more flexible. Elasticity and tensile strength of the skin are both getting stronger because of collagen synthesis. After re-epithelialization, macrophages regain their phagocytic phenotype. Excessed cells and matrix no longer required for wound healing are phagocytosed by Mreg or M2c-like macrophages [24].
3. Classification of Natural Compounds for Wound Healing by Their Properties
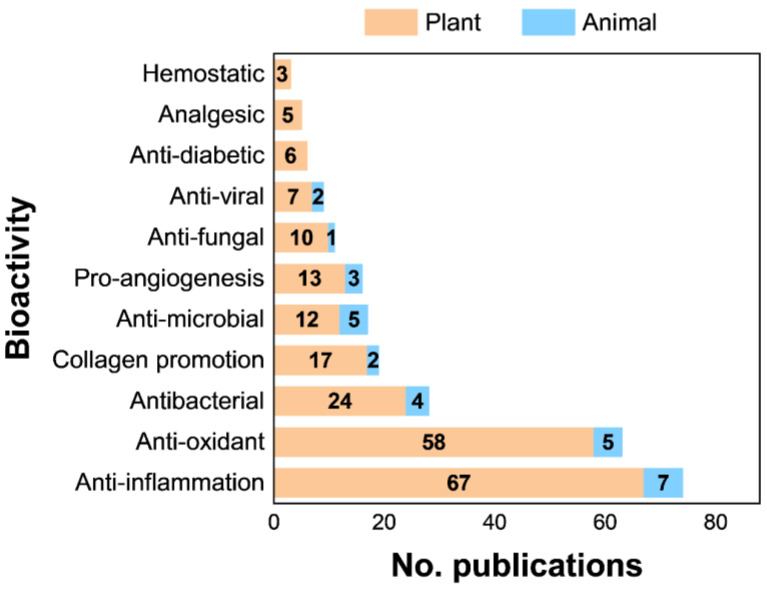
From the literature search, we collected a list of 137 research articles [30,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170] relating natural compounds for wound healing. We classified them into groups regarding their bioactivities (i.e., anti-inflammation, anti-oxidant, antibacterial, collagen promotion, etc.) (Figure 2). The origin of those compounds (i.e., plant and animal) was also considered. Among bioactivities, anti-inflammation, anti-oxidant, anti-bacterial, and collagen promotion are studied the most. Therefore, in this study, we focused our discussion on natural compounds regarding these bioactivities. A data table containing a list of those literature and the compounds were provided in the Supplementary Materials.
Figure 2.
Summary of collected literature based on bioactivities of natural compounds used in wound healing.
3.1. Natural Compounds with Anti-Inflammation Properties
The inflammatory response is an important process in wound healing. Inflammation and anti-inflammation affect the process of hemostasis, removal of harmful microorganisms, damaged tissues, and wound cleaning [171]. However, if the inflammation phase is prolonged, it will lead to a pathological condition and affect the wound healing process [172,173]. To solve this problem, compounds with an anti-inflammation activity that impact the wound healing process are a therapeutic target. A list of compounds reading anti-inflammation is shown in Table 1.
Table 1.
Compounds with anti-inflammation.
| Compound | Origin | Using Part | Other Bioactivities | Targeting Phase | ExperimentalModel | Type of Wound | Ref. |
|---|---|---|---|---|---|---|---|
| Asiatic acid | Plant (Centella asiatica) |
Leaves | Anti-microbial Anti-oxidant Pro-collagen |
Inflammation Proliferation Remodeling |
Human | Diabetic Burn | [174] |
| Pinocembrin | Plant | N/A | N/A | Inflammation | HaCaT cell | N/A | [113] |
| Ursolic acid | Plant (Hedyotis herbacea) |
N/A | Anti-microbial | Inflammation | Rat | Incision Excision | [175] |
| Myricetin | Plant (Tecomaria capensis v. aurea) |
N/A | Anti-oxidant Anti-allergic Analgesic |
Inflammation | Rat | Excision | [47] |
| Myricetin | Plant | N/A | Anti-oxidant | N/A | In vitro | N/A | [59] |
| Apigenin | Plant | Fruits Beans Tea leaves |
Anti-oxidant Pro-angiogenic |
Inflammation Proliferation |
Rat | Random skin flaps | [109] |
| Lupeol | Plant (Bowdichia virgilioides Kunth) |
Stem bark | Anti-oxidant | Inflammation Proliferation Remodeling |
Rat | Excision | [58] |
| Lupeol | Plant (Bowdichia virgilioides Kunth) |
Stem bark | Anti-oxidant | Inflammation Proliferation |
Rat | Excision | [176] |
| Steroidal glycoside | Plant | N/A | Dermal fibroblast migration activity | Inflammation Proliferation Remodeling |
Human dermal fibroblast cells | Human wound | [56] |
| Verbascoside | Plant (Plantago subulata) |
Aerial parts | Anti-oxidant Anti-fugal Anti-bacterial Anti-viral |
Inflammation Proliferation |
L929 fibroblasts RAW 264.7 cells |
N/A | [62] |
| Verbascoside | Plant (Plantago australis) |
Leaves | Anti-oxidant Healing |
Inflammation Proliferation |
HaCaT cells Rat |
Excision | [177] |
| Hesperetin | Plant | Citrus species | Anti-microbial Anti-oxidant |
Inflammation Proliferation Remodeling |
Rat | Excision diabetic foot ulcer |
[102] |
| Hesperetin | Plant | Citrus species | Anti-oxidant Pro-collagen |
Inflammation | Rat | Diabetic foot ulcer | [154] |
| Carophylolide | Plant (Calophyllum inophyllum Linn) |
Seed | Anti-microbial Anti-coagulant |
Inflammation | Mice | Incision | [55] |
| Artocarpin | Plant (A.communis.) |
Heartwood | Anti-oxidative, Anti-microbial |
Inflammation Proliferation |
Mice HUVECs cells |
Excision | [50] |
| Bilirubin | Mammals | Product of heme catabolism | Anti-oxidant | Inflammation Proliferation Remodeling |
Rat | Excision | [138] |
3.1.1. Myricetin
Myricetin (Myr) is a flavonoid that has been reported for wound healing [47,59]. Myricetin is present in many fruits and has many biochemical properties such as antioxidant, anti-allergic, anti-inflammation, and immunomodulatory function [178,179,180,181]. Elshamy et al. isolated myricetin from Tecomaria capensis v. aurea and examined its wound healing ability in albino rats [47]. Myr affects inflammatory cytokines such as tumor necrosis factor-α (TNF-α), cluster of differentiation 68 (CD68), as well as interleukin-1β (IL-1β). Myr also showed increased expression of serum proinflammatory cytokines (e.g., IL-1β and TNF-α) and decreased expression of macrophage CD68. The above findings suggest that Myr could be used therapeutically in wound healing by enhancing inflammatory cytokines and systemic reorganization. Other than that, Sklenarova et al. investigated Myr’s ability to heal wounds [59]. This study showed the inhibition of proinflammatory cytokines production (e.g., IL-6 and IL-8) in skin cells by Myr.
However, myricetin is very poorly soluble in water [182]. This affects its bioavailability [183]. This limitation needs to solve by combining Myr with other compounds or biomaterial to improve the water solubility of Myr.
3.1.2. Calophyllolide (CP)
Calophyllolide (CP) is isolated from Calophyllum inophyllum Linn and has been reported with anti-inflammatory, anti-microbial, and anti-coagulant activities [184,185,186]. Nguyen et al. studied the long-lasting anti-inflammatory effects of CP in the healing process [55]. They showed that CP treatment suppresses prolonged inflammation by downregulating IL-1β, IL-6, TNF-α, and upregulating IL-10. Moreover, CP inhibits MPO activity and increases M2 macrophage bias through upregulating M2-associated gene expression, leading to benefits in wound healing.
3.1.3. Steroidal Glycoside
Steroidal glycoside is extracted from Lilium longiflorum Thunb. Di et al. confirmed that wound treatment with steroidal glycosides would upregulate early inflammatory genes such as IL2, IL4, IL10, CD40LG, IFNG, and CXCL11, remodeling genes like CTSG, F13A1, FGA, MMP and PLG) [56]. Concurrently, wound treatment with steroidal glycosides also displayed a selective downregulation of genes regarding inflammation (CXCL2 and CCL7) and regeneration (MMP7 and PLAT) [56]. The above findings suggest an impact of wound treatment with steroidal glycosides on wound healing, leading to early termination of the inflammatory response and shortening the early stages of tissue regeneration.
3.1.4. Verbascoside (Acteoside)
Verbascoside is a phenolic compound with various bio-properties such as anti-inflammation, antioxidant, and healing [187,188,189]. Nathalia et al. isolated verbascoside from Plantago australis and examined its wound healing and anti-inflammatory activity [177]. This study has confirmed that verbascoside significantly reduced inflammatory cytokines (TNFα, INFγ, IL-6, MCP-1 and IL-12p70). In another study, Yasin et al. extracted verbascoside from Plantago subulata and evaluated its biological activity [62]. The in vitro test with RAW264.7 cell showed that when the cell was treated with verbascoside, the level of NO, PGE2, and TNF-α cytokines decreased. Another part of the study also confirmed that verbascoside from Plantago subulata has wound healing activities. The above studies suggested verbascoside has wound healing activities and may have related to anti-inflammation.
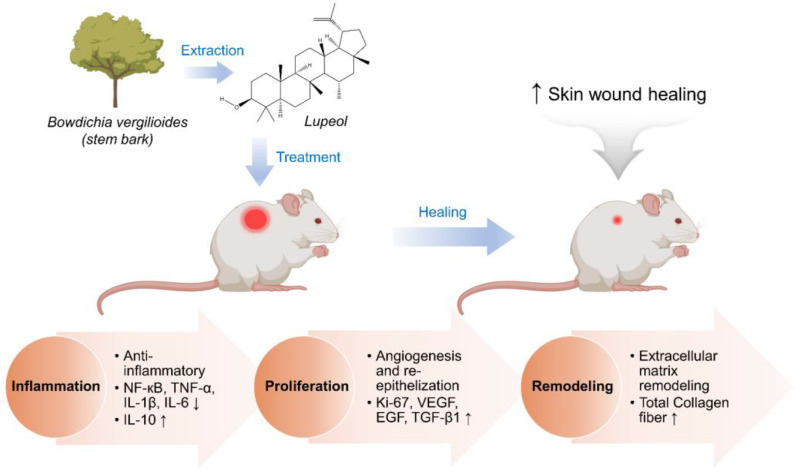
3.1.5. Lupeol
Lupeol is a bioactive compound mainly found in Bowdichia virgilioides and fruit such as mango, soybean, and olive [58]. Researchers reported that Lupeol had antioxidant, antiinflammation, and antidiabetic activity [190,191,192]. To evaluate the wound healing ability of lupeol, Fernando et al. conducted experiments on rats and showed interesting results [176]. The results showed that lupeol effectively reduced inflammatory cytokines (e.g., NF-κB and IL-6) while increasing IL-10. Moreover, Lupeol also has effects on angiogenesis and cell proliferation by decreased expression of Vegf-A and increased expression of Hif-1α. There are markers for the angiogenic process and proliferation of wound healing. Another study was also done by Fernando et al., once again further identifying the wound healing activities of lupeol in the cream form [58]. The results showed that wound treatment with lupeol cream affects proinflammatory cytokines, such as reducing the expression of TNF-α, IL-1β and IL-6 and increasing the expression of IL-10 (Figure 3). In addition, lupeol treatment was also shown to improve vascular endothelial growth factor (VEGF) and epidermal growth factor (EGF) and increase gene expression of transforming growth factor beta-1 (TGF-β1) after 7 days. These are the factors that involve the proliferative phase in wound healing. Lupeol accelerates remodeling by increasing collagen fiber synthesis. These are studies that demonstrate the wound healing capacity of lupeol.
Figure 3.
The effect of lupeol cream on wound healing. Up and down arrows mean increasing and decreasing of concentration, respectively. Reproduced with permission from Beserra et al., “From Inflammation to Cutaneous Repair: Topical Applica-tion of Lupeol Improves Skin Wound Healing in Rats by Modulating the Cytokine Levels, NF-κB, Ki-67, Growth Factor Expression, and Distribution of Collagen Fibers”; published by MDPI, 2020 [58].
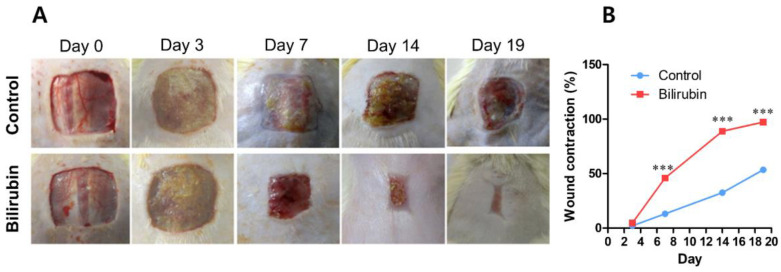
3.1.6. Bilirubin
Bilirubin is a red-orange compound that is the end product of heme catabolism in mammals and also plays an important role in protecting cellular [193]. By speculating that Bilirubin might benefit wound healing, Azad et al. evaluated the wound healing process in rat skin when treated with bilirubin [54]. When the wound was treated with Bilirubin, pro-inflammatory factors (e.g., ICAM-1 and TNF-α) decreased, and interleukin-10 (IL-10) expression was increased. Wound contraction, hydroxyproline, and glucosamine levels were also increased in treated rats. In addition, Mahendra et al. also studied the effect of Bilirubin on growth factors, cytokines, and angiogenesis during wound healing in diabetic rats [138]. This study showed that pro-inflammatory cytokines such as TNF-α, MMP-9, and IL-1β decreased mRNA expression while increasing IL-10 expression. Gene expression of anti-oxidative, angiogenic agents (e.g., VEGF, HIF-1α, SDF-1α, TGF-β) was also upregulated in Bilirubin-treated rats. Wound closure, collagen deposition, and blood vessel formation in treated rats were also higher than in the control group (Figure 4). These results partly confirmed the role of Bilirubin in regulating pro-inflammatory and angiogenic factors in the wound healing process.
Figure 4.
(A) Representative images of the wound treated with Bilirubin and (B) wound contraction after 19 days. Three asterisks (***) indicates p-value < 0.001. Reproduced with permission from Ram et al., “Bilirubin modulated cytokines, growth factors and angiogenesis to improve cutaneous wound healing process in diabetic rats”, published by Elsevier, 2016 [138].
3.1.7. Pinocembrin
Pinocembrin (5,7-dihydroxyflavonone) is one of the flavonoid compounds found in propolis, honey, and plants of the Piperaceae family [194]. The compound showed various potential bioactivities for healing treatment (e.g., anti-bacteria, anti-inflammation, anti-fibrosis, anti-oxidation) [194]. For example, Drewes and colleagues showed that pinocembrin had notable antibacterial activity toward Staphylococcus aureus (minimum inhibitory concentration of 6.3 μg/mL) and Pseudomonas aeruginosa (minimum inhibitory concentration of 45–63 μg/mL) [195]. Pinocembrin also showed anti-inflammatory activity against sheep red blood cell-induced delayed-type hypersensitivity reaction [196]. Pinocembrin is currently in traditional Chinese medicine for wound healing [103]. Li and colleagues investigated the effects of pinocembrin on skin fibrosis by in vitro and in vivo approaches [103]. The study showed that pinocembrin could significantly reduce bleomycin-induced skin fibrosis and fibrosis-related protein expression of keloid tissues in xenograft mice. They also confirmed the mechanism of anti-fibrotic activity of pinocembrin that pinocembrin suppressed TGF-β1/Smad signaling and attenuated TGF-β1-induced activation of skin fibroblasts.
3.2. Natural Compounds with Anti-Oxidant Properties
Antioxidants are one of the therapeutic targets to improve wound healing mechanisms, especially free radicals and oxidative reactions. They are known as an important factor in the regulation of the healing process [54,197,198]. A high concentration of oxidants in the wound inadvertently harms the wound and some enzymatic reactions during the healing process [199]. Because of that, the presence of antioxidants is a necessity in the wound healing process. A list of compounds reading antioxidant is shown in Table 2.
Table 2.
Compounds with anti-oxidant.
| Compound | Origin | Using Part | Other Bioactivities | Target Phase | Experimental Model | Type of Wound | Ref. |
|---|---|---|---|---|---|---|---|
| Quercetin | Plant (Oxytropis falcata Bunge) |
Fruits | Anti-inflammatory Anti-infection |
Inflammation Proliferation Remodeling |
Mice | Excision | [63] |
| Resveratrol | Plant | N/A | Anti-inflammatory Anti-bacterial |
Inflammation Proliferation |
HUVE cells Rat |
Burn injury | [149] |
| Catechin | Plant (Green tea) |
N/A | Anti-bacterial Anti-inflammatory Pro-angiogenic |
Inflammation | Mice | Chronic diabetic wound | [65] |
| Catechin | N/A | N/A | N/A | N/A | Mouse NIH/3T3 fibroblast cell | N/A | [200] |
| Luteolin | Plant | N/A | Anti-inflammatory Anti-allergenic |
Inflammation Proliferation |
Rat | Excision | [42] |
| Syringic acid | Plant | Fruits | Anti-inflammatory Anti-microbial Anti-adipogenic |
Inflammation Proliferation Remodeling |
Rat | Incision diabetic wound | [133] |
| Metformin | N/A | N/A | Anti-hypoglycemic | Inflammation Proliferation |
Mice | Diabetic wounds | [87] |
| Naringenin | Plant | Citrus fruits | Anti-inflammatory | Proliferation Inflammation |
Rat | Thermally-induced skin damage | [201] |
| Galic acid | Plant | Fruits Leaves Flower |
Anti-inflammatory Analgesic |
Inflammation Proliferation |
HaCaT MEF HF21 cells |
Hyperglucidic conditions | [61] |
| Ferulic acid | Plant (vegetables, cereals, coffee) |
Seed Fruits |
Anti-inflammatory Antimicrobial |
Inflammation Proliferation |
Rat | Excision diabetic wounds | [84] |
| Curcumin | Plant | Turmeric | Anti-inflammatory | Inflammation Proliferation |
Rat | Excision | [82] |
| Curcumin | Plant (Curcuma longa) |
Turmeric | Anti-inflammatory Anti-infective |
Inflammation | Rat | Excision | [57] |
| Curcumin | Plant | Turmeric | Anti-inflammatory | Inflammation | Human keratinocytes and fibroblasts | H2O2 condition | [60] |
| Curcumin | Plant (Curcuma longa) |
Turmeric | N/A | Inflammation | Human keratinocytes | Hypoxanthine/xanthine oxidase injury | [202] |
3.2.1. Curcumin
Curcumin is mainly extracted from turmeric (Curcuma longa L.) and has shown several bioactive properties such as anti-inflammatory, antioxidant, and anti-coagulant [203,204]. Several studies demonstrated curcumin’s wound healing effects as an antioxidant [57,60,82,202]. Phan et al. confirmed that curcumin protects human dermal fibroblasts and epidermal when exposed to hydrogen peroxide and superoxide radicals [60]. Gadekar et al. evaluated the protective potential of curcumin against keratinocytes and fibroblasts in H2O2-induced injury [82]. Through the antioxidant activity, Bonte et al. also demonstrated that curcumin protects human keratinocytes from xanthine oxidase damage [202]. Mohanty et al. reported the ability of curcumin to reduce ROS and lipid peroxidation, thereby reducing the activation of antioxidant enzymes after wound treatment in rats [57]. The above studies show the impact of Curcumin in the role of an antioxidant in wound healing and its potential in developing methods of using Curcumin in treating wounds.
Despite its excellent biological effects, curcumin has limitations in its therapeutic use because it is virtually insoluble in water leading to instability and poor bioavailability [205].
3.2.2. Quercetin
Quercetin is known as a flavonoid found in many vegetables, fruits, and seeds such as citrus, onion, tea, spices, etc. It is also a famous strong antioxidant and anti-inflammation activities compound [206]. Kant et al. showed that quercetin (0.3%) helps the wound heal the fastest and significantly improves oxidative stress, regulates cytokines and growth factors, and promotes fibroblast proliferation, formation of vessels, and collagen deposition [64]. Mi et al. presented an intensive study evaluating the wound healing effects of Quercetin, which is extracted from Oxytropis falcata Bunge, a traditional Chinese legume distributed in Tibet [63]. This study showed that quercetin-treated wounds had an increase in collagen fiber content and a significant decrease in inflammatory factors (TNF-α, IL-1β and IL-6). In addition, glutathione (GSH) is an antioxidant and an important redox regulator controlling the inflammatory process [207]. Mi et al. also showed that quercetin treatment improved GSH levels suggesting quercetin has a potent antioxidant capacity in skin wounds. In brief, quercetin exhibits an effective wound-healing effect on the skin by enhancing fibroblast migration and proliferation, and inhibiting inflammation through antioxidant activities.
Like most flavonoids, quercetin is poorly soluble in water [208]. This physical limitation affects the application of quercetin in wound treatment. Therefore, further studies on the combination of quercetin are needed to increase its applicability in the future.
3.2.3. Catechin
Catechin is a flavonoid with good antioxidant activity; it plays a beneficial role in physiological activity [160,209]. Baek et al. prepared a PCL/(+)-catechin/gelatin film and evaluated its applicability for wound treatment [200]. The results show that PCL/(+)-catechin/gelatin film prevents harmful factors from the outside, and reduces oxidative stress at the wound effectively to help the wound heal. Zhao et al. confirmed that the EGCG-3-acrylamido phenyl boronic acid-acrylamide (EACPA) hydrogel has antioxidant, antibacterial, antiinflammatory, and proangiogenic effects, and modulates macrophage polarity to accelerate wound healing, also facilitates easy dressing change [65]. This study clearly shows the effect of the antioxidant EACPA on wound healing through the down-regulation of the majority of intracellular ROS in Rosup-stimulated L929 fibroblasts.
Despite having such outstanding activities, catechins are less stable in water. To overcome this problem, several studies were carried out using reducing agents and the formation of micro- and nanoparticles [66,210].
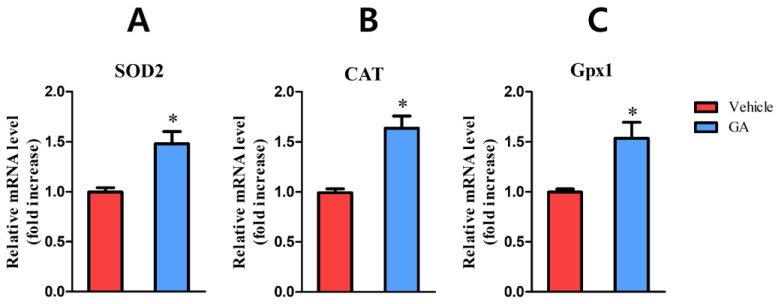
3.2.4. Galic Acid (GA)
Galic acid (GA) is present in almost every plant. It is found in many different parts of plants, such as fruits, leaves, and stems, with powerful properties such as antioxidant, antiinflammation, anticancer, and neuroprotective [211,212,213]. Yang et al. conducted research to evaluate the effects of GA on wound healing in normal and hyperglucidic conditions [61]. This study indicated that GA could protect skin cells from oxidative stress induced by H2O2 and ROS-induced cytotoxicity. Additionally, GA could upregulate the expression of antioxidant genes such as catalase (CAT), superoxide dismutase 2 (SOD2) and glutathione peroxidase 1 (Gpx1) (Figure 5). Furthermore, GA also accelerates keratinocyte migration during wound healing and activates wound healing factors such as c-Jun N-terminal kinases (JNK), focal adhesion kinases (FAK), and extracellular signal-regulated kinases (Erk). Therefore, this study indicated that GA is a promising antioxidant for wound treatment. However, GA is only soluble in organic solvents, which limits its topical applications on the skin.
Figure 5.
Gallic acid regulates the expression of anti-oxidant genes. (A): SOD2, (B): CAT, (C): Gpx1. Asterisk (*) indicates p-value < 0.05. Reproduced with permission from Yang et al., “Gallic Acid Promotes Wound Healing in Normal and Hyperglucidic Conditions”, published by MDPI, 2016 [61].
3.2.5. Resveratrol (RSV)
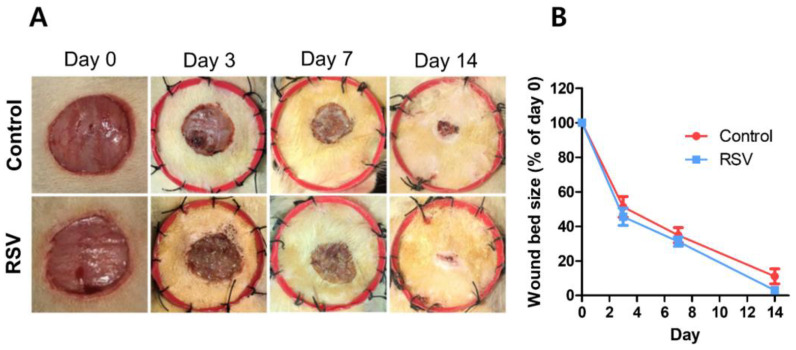
Resveratrol is found in more than 70 different plant species and is known for its outstanding medicinal properties such as antioxidant, anticancer, anti-inflammatory, and antibacterial properties [214,215,216,217]. Zhou et al. examined the wound healing ability of resveratrol through the cell and in vivo experiments [149]. Resveratrol protects from H2O2-induced injury, effectively decreases H2O2-induced injured cell migration, and effectively suppresses intracellular ROS production by H2O2 in HUVECs. In vivo tests also confirmed that resveratrol speeds up wound healing, improves skin structure, and reduces inflammation (Figure 6). These effects may be due to resveratrol upregulating Mn-SOD, thereby reducing oxidative damage. On the other hand, Bilgic et al. evaluated the wound healing ability of resveratrol in Wistar albino rats [218]. They showed that the resveratrol-treated wound had a higher neovascularization level than the untreated control group. Furthermore, levels of glutathione peroxidases, enzymes that remove reactive oxygen and nitrogen species from the body, were higher in the resveratrol treatment group. These results suggested that resveratrol affected wound healing through its antioxidant effects.
Figure 6.
Effect of resveratrol on wound healing. (A): Representative images of wound bed size from two groups. (B): Quantitation of wound bed sizes. Reproduced with permission from Zhou et al., “Resveratrol accelerates wound healing by attenuating oxidative stress-induced impairment of cell proliferation and migration”, published by Elsevier, 2021 [149].
3.2.6. Naringenin
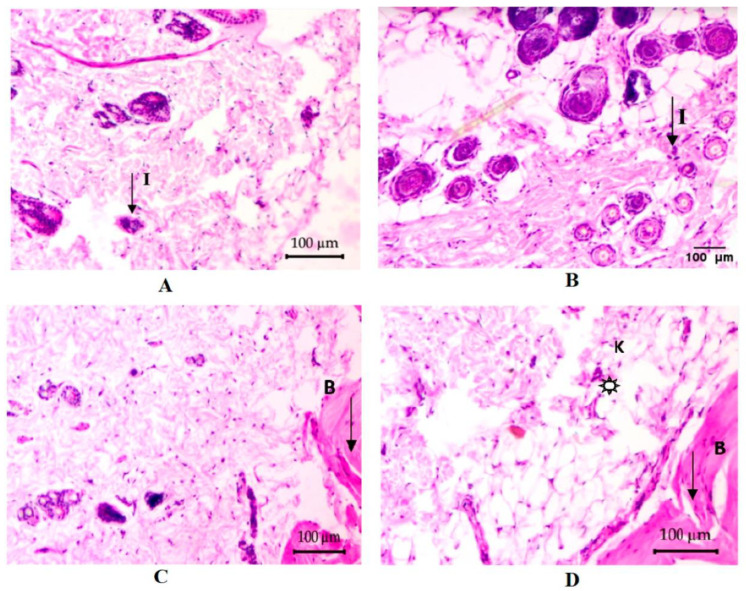
Naringenin is known as a polyphenol, mainly found in citrus fruits, with outstanding biological properties such as anti-inflammatory, antioxidant, cholesterol-lowering, and anticancer [219,220]. Al-Roujayee et al. evaluated the effect of naringenin in rats for inflammatory responses and oxidative stress caused by thermal burn-induced [201]. The results showed that when the burn was treated with naringenin, the activities of glutathione-S-transferase (GST), superoxide dismutase (SOD), catalase, glutathione peroxidase (GPx), and catalase increased. Thiobarbituric acid reactive substances (TBARS) and glutathione (GSH) levels were also restored on day 7 of treatment. In addition, naringenin was also used to combine with other compounds (e.g., chitosan) to improve wound healing capacity. Akrawi and colleagues showed that a nanoemulsion product containing both naringenin and chitosan significantly increased wound contraction in Wistar rats after 14 days of treatment, and naringenin stimulated antiinflammatory and antioxidant effects (Figure 7) [72]. These results suggest the potential for the treatment of burn wounds of naringenin base on antioxidant activities.
Figure 7.
Representative photomicrographs of the rat skin tissues in the control, drug-free chitosan-coated naringenin and chitosan-coated naringenin (CNNE) treated groups of abrasion model in albino Wistar rats. (A) Wound area before the treatment at day 0, (B) control group at day 14, (C) drug-free chitosan-coated naringenin formulation treated group at day 14, and (D) CNNE treated group at day 14. (I: inflammatory cells; B: blood vessels; K: keratinization; Star icon: granulated tissue). Reproduced with permission from Akrawi et al., “Development and Optimization of Naringenin-Loaded Chitosan-Coated Nanoemulsion for Topical Therapy in Wound Healing”, published by MDPI, 2020 [72].
3.3. Natural Compounds with Antibacterial Properties
The antibacterial activity of a compound could be ascribed by two mechanisms: inhibition of synthesis of vital components of bacteria or suppression of antibacterial resistance [221]. Natural compounds with antibacterial properties might target mostly the inflammation phase of wound healing (Table 3).
Table 3.
Compounds with anti-bacterial.
| Compound | Origin | Using Part | Other Bioactivities | Target Phase | Experimental Model | Type of Wound | Ref. |
|---|---|---|---|---|---|---|---|
| Chitosan | Animal (Crab) |
Shells | Anti-microbial Anti-inflammation |
Inflammation | Diabetic db/db mice | Excision wound | [222] |
| Pinocembrin | Animal (Bee) |
PropolisHoney | Anti-oxidation Anti-inflammatory Anti-apoptosis |
Proliferation | Human Keloid fibroblast Mice |
keloid xenograft | [103] |
| Lupeol | Plant (Bowdichia virgilioides Kunth) |
Stem bark | Anti-oxidant Antidiabetic |
Inflammation Proliferation Remodeling |
Rat | Excision | [58] |
| Hydrogen peroxide | Animal (Bee) |
Honey | N/A | Inflammation | HaCaT cells | N/A | [223] |
| Methylglyoxal | Animal (Bee) |
Honey (Manuka) | N/A | N/A | N/A | N/A | [52] |
| Tannins | Plant (E. phaseoloides (L.) Merr) |
N/A | Anti-oxidant Anti-inflammatory |
Inflammation Proliferation Remodeling |
Rat | Excision | [105] |
| Arnebin-1 | Plant (Arnebianobilis) |
Root | Anti-fungal | Proliferation | Rat | Excision | [147] |
| Hydroalcoholic extract | Plant (Caseariasylvestris Sw.) |
Leaves | Anti-inflammatory Antiseptic |
Proliferation | Rodent | Scald burns | [83] |
| Dichloromethane andhexanoic fractions | Plant (Calendula officinalis L.) |
Flower | Anti-inflammatory Anti-septic |
Inflammation Proliferation | Rat | Excision | [129] |
| Lawsone | Plant (Lawsonia Alba Lam.) |
Leaves | Anti-fungal Anti-parasitic Anti-viral |
N/A | Rat | Excision Incision |
[111] |
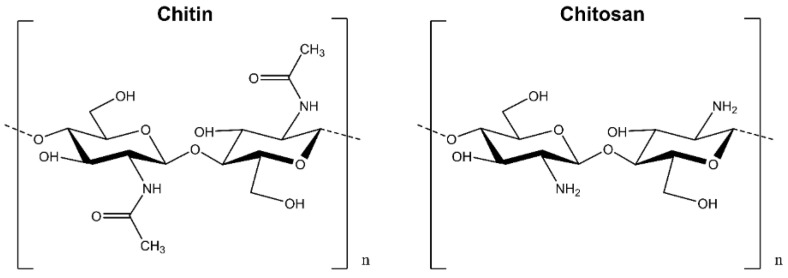
3.3.1. Chitosan and Chitin
The first use of chitosan and chitin (Figure 8) as wound healing accelerators dates back to the research of Prudden et al. [224]. Chitin (poly-N-acetyl-d-glucosamine-(1–4)-poly-N-acetyl-d-glucosamine) is one of the most prevalent polysaccharides with the largest source from the exoskeleton of marine crustaceans, shrimp, crabs, insects, fungi, and yeasts after cellulose [225]. Chitosan is a copolymer of glucosamine and N-acetylglucosamine units connected by 1–4 glucosidic linkages and is the most important chitin derivative.
Figure 8.
Chemical structure of Chitin and Chitosan.
The secret to the antibacterial capabilities of chitosan is that positively regulating substances make it more susceptible to interacting with negatively charged molecules in bacterial membranes, such as anionic polysaccharides, proteins, and nucleic acids [226,227]. Chitosan has significant advantages in wound treatment due to its biocompatibility, biodegradability, nontoxicity, adsorption properties, and hemostatic qualities [228,229,230]. However, chitosan is insoluble in neutral and alkaline aqueous solutions with pH values greater than 6.5, severely restricting its use [231]. Therefore, chitosan has been integrated into several formulations employing nanoparticles, hydrogel, micelles, hyaluronic/oleic acid-loaded, and glucosylation of the hydrophobic molecule in pre-clinical investigations to improve its bioavailability [53,232,233,234,235].
3.3.2. Honey Bee
Bee products are also natural antibacterial sources widely used in wound healing. Honey from bees has been applied to wound treatment for thousands of years, with the first written recorded between 2600 and 2200 BCE in an ancient Egyptian trauma manual [51,236]. Honey is a concentrated aqueous solution of inverted sugars that contains 40% fructose, 40% glucose, 20% water, enzymes, vitamins and minerals, with a pH of 3.6 [237,238]. Most conventional honey produces hydrogen peroxide by the endogenous enzyme glucoseoxidase, which is responsible for its antibacterial activity. When hydrogen peroxide decomposes, it produces highly reactive free radicals, which react with the bacteria and decimate them [238]. However, several other “non-peroxide” kinds of honey (Ex. Manuka, jelly bush) own antibacterial properties because of the low pH medium and supersaturated sugar level [239]. Especially, Atrott and Henle suggested that Manuka honey has significant levels of methylglyoxal, a unique antibacterial component solely responsible for the special antibacterial effect [52].
3.3.3. Propolis
Propolis was used by ancient Egyptians, Romans, and Persians. Propolis could be obtained from honey bees, tree buds, and other botanical sources (e.g., poplar, willow, elm, alder, birch, beech, etc.) [240,241,242]. Propolis consists of more than 300 chemical compounds such as polyphenols, phenolic aldehydes, amino acids, steroids, etc. [243,244,245]. The most important components in propolis are flavonoids, phenylpropanoids, cinnamic acids and their esters, and glycerides [246,247]. The antibacterial properties of propolis against Gram-positive bacteria also appear mostly due to flavonoids, esters, and aromatic acids found in the resin [246].
3.3.4. Tannins
Along with animal products that have antibacterial activity, many medical plants used in wound healing also show potent antibacterial properties such as tannins. Su et al. reported that tannins extracted from Entada phaseoloides (L.) Merr. exhibited the antibacterial property by suppressing protein synthesis, modification of nucleic acid metabolism, prevention of alteration of cell wall formation, modification of cell membrane function, and inhibition of bacterial growth [105].
3.3.5. Allicin
Allicin, the chemical responsible for the strong odor of garlic, is the active ingredient that has been proved in numerous trials to enhance wound healing [127,248,249,250]. Apart from antioxidant activity, allicin also shows an antibacterial effect, and its mode of action has already been researched. The sulfhydryl alteration of bacterial proteins was found to be the mechanism by which allicin manifests its antibacterial activity toward Staphylococcus aureus [248,251].
3.3.6. Terpene Esters
Terpene esters could be extracted from bee propolis [252]. Terpene esters demonstrated antibacterial activity toward Staphylococcus aureus, as shown in the study of Trusheva and colleagues [252]. The mechanism of the antibacterial activity of terpene esters has not been fully elucidated.
3.4. Natural Compounds with Collagen Promotion Properties
Collagen is the protein that is most prevalent in the body. Collagen function in wound healing is to draw fibroblasts and promote the deposition of fresh collagen in the wound bed. The use of collagen dressing technology aids in promoting the formation of new tissues while promoting angiogenesis, autolytic debridement, and re-epithelialization. Hence, the compounds capable of promoting collagen synthesis in the healing process play an important role. A list of compounds with collagen promotion is shown in Table 4.
Table 4.
Compounds with collagen promotion.
| Compound | Origin | Using Part | Other Bioactivities | Target Phase | Experimental Model | Type of Wound | Ref. |
|---|---|---|---|---|---|---|---|
| Honey | Animal (Bee) |
Honey | Anti-bacterial | Proliferation | Rat | Excision | [253] |
| Calendula officinalis extract | Plant (Calendula officinalis) |
Flower | Anti-bacterial | Proliferation | Rat | Excision | [98] |
| Saponins | Plant (Panax Notoginseng) |
Root Rhizome |
Anti-inflammation Anti-oxidant Anti-apoptosis Anti-coagulation |
Remodeling | Hypertrophic scar fibroblast | N/A | [165] |
| Cryptotanshinone | Plant (Salvia miltiorrhiza Bge.) |
N/A | Anti-inflammatory Anti-oxidative Anti-bacterial |
Remodeling | Diabetic mice | Excision | [49] |
| Bexarotene, Taspine, and 2-hydroxy-1-naphthaldehyde Isonicotinoylhydrazone |
Plant (Daemonorops draco) |
N/A | Anti-bacterial Anti-inflammation |
Inflammation Proliferation |
THP-1, HaCaT, NIH-3T3 cells | N/A | [35] |
| Sesamol | Plant | Sesame oil | Anti-inflammatory Anti-oxidant |
Inflammation Proliferation |
Rat | Diabetic foot ulcer | [86] |
| Astragaloside IV | Plant (Astragali Radix) |
N/A | Anti-inflammatory Anti-oxidative |
Inflammation Proliferation |
Mice | Excision | [108] |
| Polysaccharide APS2-1 | Plant (Astragalus membranaceus) |
Roots | Anti-inflammatory | Inflammation Proliferation |
Mice | Excision | [163] |
| Aloe vera gel | Plant (Aloe vera) |
Leaves | Anti-inflammatory Anti-bacterial Anti-viral Anti-fugal |
Proliferation | Mouse embryonic fibroblasts | N/A | [254] |
| Asiaticoside | Plant (Centella asiatica) |
Aerial parts | Anti-oxidant | Proliferation | Rabbit | Incision | [135] |
| Gallic acid and quercetin | Plant (Glycyrrhiza glabra L.) |
Roots | Anti-inflammatory Anti-bacterial Anti-microbial Antioxidant |
Inflammation Proliferation |
Pig | Excision | [88] |
| Asiatic acid | Plant (Centella asiatica) |
Aerial parts | Anti-oxidative | Proliferation | Rat | Wound burn | [141] |
| β-Glucans | Fungi | N/A | Anti-biotic | Proliferation | Human dermal fibroblasts |
N/A | [255] |
| Alkaloids | Plant (Evolvulus alsinoides) |
Aerial parts | Anti-bacterial Anti-fugal Anti-oxidant |
Proliferation | Rat | Incision | [256] |
| Asiaticoside and madecassoside | Plant (Centella asiatica) |
N/A | Anti-oxidant | Proliferation | Rat | Burn injury | [89] |
| Triterpenes | Plant (Buddleia scordioides) |
Leaves | N/A | Proliferation | Diabetic rat | Incision Excision |
[257] |
| Deoxyelephantopin | Plant (Elephantopus scaber) |
Leaves | Anti-inflammatory | Inflammation Proliferation |
Rat | Incision | [139] |
3.4.1. Saponins
Saponins are glycoside compounds widely found in the plant kingdom. Saponins include various groups and are categorized according to their structure [258]. For instance, Wang et al. reported four novel steroidal saponins, together with two known compounds (i.e., bletilnoside A and 3-O-β-d-glucopyranosyl-3-epi-neoruscogenin), were extracted from Bletilla striata which is a popular traditional Chinese herb [153]. Numerous biological processes, including hemolysis [259], antibacterial [260,261], antiviral [262], antioxidative [263], antiinflammatory activities [264,265], and collagen promotion [44] can be enhanced by saponin treatment. Yu et al. explored the function of Panax notoginseng saponins (PNS) in encouraging anterior cruciate ligament (ACL) fibroblast migration, proliferation, and expression of fibronectin, collagen I, and collagen III to the healing of an ACL injury. PNS may play an essential role via phosphorylating PI3K, AKT, and ERK [44].
3.4.2. Cryptotanshinone
Cryptotanshinone extracted from Salvia miltiorrhiza Bge is a natural accelerated procollagen compound in the wound healing process. Improved angiogenesis and collagen deposition can result from the activity of cryptotanshinone, which reduce leukocyte infiltration, enhance eNOS phosphorylation, boost VEGF and Ang-1 protein production, suppress MMP2 and MMP9 protein expression, and increase fibroblast translation [49].
3.4.3. Artocarpin
There have been claims that the prenylated flavonoid artocarpin, isolated from the plant Artocarpus communis, has anti-inflammatory and anticancer activities [266,267,268,269,270]. Yeh et al. demonstrated that by stimulating the JNK and P38 pathways, Artocarpin boosted collagen formation, proliferation, and migration of human fibroblasts. Artocarpin also enhanced the proliferation of human endothelial cells through the Akt and P38 pathways and human keratinocytes through the ERK and P38 pathways [50].
3.4.4. β-Glucans
β-glucans are glucose polymers, and they can be found in yeast, grains, and fungi. These substances are classified as biological response modifiers [271]. Many studies have demonstrated that particulate and soluble β-glucans improved immune functions with anti-infective, anticancer, and immunomodulatory effects [272,273,274]. β-glucans improve wound healing by enhancing the infiltration of macrophages, which drives tissue granulation, collagen deposition, and re-epithelialization. With excellent stability and resistance to wound proteases, β-glucan-based wound dressings constitute an ideal wound healing agent [275].
3.4.5. Amino Acids and Peptides
Besides the traditional medicinal plants, the sources of natural procollagen compounds containing amino acids and peptides for wound healing also from animals (e.g., bees, mollusks, snail, fish, etc.) are widely reported. For fibroblasts, which need an acidic environment to perform tasks like migrating and organizing collagen, the low pH of honey may help establish and maintain ideal circumstances [276]. Badiu et al. indicated that amino acids from Rapana venosa and Mytilus galloprovincialis enhance dermal and epidermal neoformation to hasten skin wound healing [70]. Indeed, the mechanism insight of these amino acids’ enhancing wound healing effects was proposed to be closely related to differential regulation of macrophage arginine metabolism, in which TGF-β1 may play an essential coregulatory role [277]. In addition, the bioactive peptide extracted from terrestrial snail Cryptozona bistrialis stimulates in vitro migration of NIH/3T3 mouse fibroblast cells. In vivo tests on healthy and diabetic-induced Wistar albino rats also showed that the Crypto-zona bistrialis-peptide was efficient in boosting wound healing [71]. The increased wound contraction is believed to be due to the significant increase in collagen content through the enhanced migration of fibroblasts and epithelial cells to the wound site. However, the extract compounds from animal sources had not shown the exact chemical formula.
4. Current Trending Use of Natural Compounds in Wound Healing
The market size for advanced wound care technologies is estimated to be $22 billion by 2030, which will focus on new wound care technologies such as bacterial burden management and biological therapies [278].
The basic understanding of natural compounds and their treatment limitations have been gradually overcome, creating medical products with outstanding features in wound treatment. Currently, the research into medical materials using natural compounds such as gels and films also shows the effectiveness and potential in the future.
Composite dressing shave replaced traditional dressings by combining wound healing drugs such as natural products (chitosan and diazo resin [68]) and growth factors (collagen sponge [73]) to protect the wound from infection and exchange oxygen with the wound [71]. Electrospun nanofiber mats are also a strategy for wound healing. Curcumin has been complexed with nanofiber mats to avoid its limitation (i.e., water insolubility); combining it with an oil layer can increase the bioavailability of curcumin while keeping the wound moist [116].
A hydrogel is also a new approach to biomaterials for wound healing. Hydrogels deliver curcumin, chitosan, and this natural compound released into the wounds. The formulation of this hydrogel not only provides natural healing properties and forms a moist middle layer for the wound. Hydrogels have become a popular new drug/material and a new research area that improves traditional natural compounds in wound treatment [279].
Microneedles are loaded with natural compounds and can penetrate through the dermis layer of the skin. Some studies have reported the superior wound healing ability of microneedles containing manuka honey and green tea extract compared with conventional skin creams [36,67].
Research directions and application of natural compounds to new technology have contributed to speeding up the healing process, solving the limitations of natural compounds, and improving their effectiveness.
5. Conclusions
Wound healing is a complex biological process of recovering devitalized cellular structures with four overlapping phases involving hemostasis, inflammation, proliferation, and remodeling. Effective therapies for wound healing using natural products are highly beneficial for patients due to their easy accessibility and low cost. This work proposed a comprehensive review of natural products for wound healing based on bioactivities from plants and animals, providing an overall picture of the chemical origin of natural products to biological wound healing mechanisms. The main four primary bioactivities of natural products, including anti-inflammation, anti-oxidant, antibacterial, and collagen promotion, are utilized to classify and investigate the targeting phases. Data tables containing detail of origin, bioactivity, targeting phase, experimental model, and type of wound were also provided for readers.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms23179573/s1.
Author Contributions
Conceptualization, S.-Y.N. and C.-Y.H.; writing—original draft preparation, L.T.V.A., P.T.N., X.-T.T., N.N.G. and N.-V.L.; writing—review and editing, N.-V.L., P.N.C., S.-Y.N. and C.-Y.H.; supervision, P.N.C., S.-Y.N. and C.-Y.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Institute of Information and Communications Technology Planning and Evaluation (IITP) grant funded by the Korean government (MSIT) (No. 2020-0-00990, Platform Development and Proof of High Trust and Low Latency Processing for Heterogeneous Atypical Large Scaled Data in 5G-IoT Environment) and by the Technology Innovation Program (Nanomaterials based flexible and stretchable sensor system for multimodal monitoring and diagnosis of Sarcopenia, 20015793) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agyare C., Akindele A.J., Steenkamp V. Natural Products and/or Isolated Compounds on Wound Healing. Evid.-Based Complement. Altern. Med. 2019;2019:4594965. doi: 10.1155/2019/4594965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorg H., Tilkorn D.J., Hager S., Hauser J., Mirastschijski U. Skin Wound Healing: An Update on the Current Knowledge and Concepts. Eur. Surg. Res. 2017;58:81–94. doi: 10.1159/000454919. [DOI] [PubMed] [Google Scholar]
- 3.Schreml S., Szeimies R.-M., Prantl L., Landthaler M., Babilas P. Wound Healing in the 21st Century. J. Am. Acad. Dermatol. 2010;63:866–881. doi: 10.1016/j.jaad.2009.10.048. [DOI] [PubMed] [Google Scholar]
- 4.Ryall C., Duarah S., Chen S., Yu H., Wen J. Advancements in Skin Delivery of Natural Bioactive Products for Wound Management: A Brief Review of Two Decades. Pharmaceutics. 2022;14:1072. doi: 10.3390/pharmaceutics14051072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vitale S., Colanero S., Placidi M., Di Emidio G., Tatone C., Amicarelli F., D’Alessandro A.M. Phytochemistry and Biological Activity of Medicinal Plants in Wound Healing: An Overview of Current Research. Molecules. 2022;27:3566. doi: 10.3390/molecules27113566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ibrahim N., Wong S., Mohamed I., Mohamed N., Chin K.-Y., Ima-Nirwana S., Shuid A. Wound Healing Properties of Selected Natural Products. Int. J. Environ. Res. Public Health. 2018;15:2360. doi: 10.3390/ijerph15112360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Artem Ataide J., Caramori Cefali L., Machado Croisfelt F., Arruda Martins Shimojo A., Oliveira-Nascimento L., Gava Mazzola P. Natural Actives for Wound Healing: A Review. Phyther. Res. 2018;32:1664–1674. doi: 10.1002/ptr.6102. [DOI] [PubMed] [Google Scholar]
- 8.Pasupuleti V.R., Sammugam L., Ramesh N., Gan S.H. Honey, Propolis, and Royal Jelly: A Comprehensive Review of Their Biological Actions and Health Benefits. Oxid. Med. Cell. Longev. 2017;2017:1259510. doi: 10.1155/2017/1259510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Viuda-Martos M., Ruiz-Navajas Y., Fernández-López J., Pérez-Álvarez J.A.A. Functional Properties of Honey, Propolis, and Royal Jelly. J. Food Sci. 2008;73:117–124. doi: 10.1111/j.1750-3841.2008.00966.x. [DOI] [PubMed] [Google Scholar]
- 10.Radha M.H., Laxmipriya N.P. Evaluation of Biological Properties and Clinical Effectiveness of Aloe Vera: A Systematic Review. J. Tradit. Complement. Med. 2015;5:21–26. doi: 10.1016/j.jtcme.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fana S.E., Ahmadpour F., Rasouli H.R., Tehrani S.S., Maniati M. The Effects of Natural Compounds on Wound Healing in Iranian Traditional Medicine: A Comprehensive Review. Complement. Ther. Clin. Pract. 2021;42:101275. doi: 10.1016/j.ctcp.2020.101275. [DOI] [PubMed] [Google Scholar]
- 12.Hajialyani M., Tewari D., Sobarzo-Sánchez E., Nabavi S.M., Farzaei M.H., Abdollahi M. Natural Product-Based Nanomedicines for Wound Healing Purposes: Therapeutic Targets and Drug Delivery Systems. Int. J. Nanomed. 2018;13:5023–5043. doi: 10.2147/IJN.S174072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumitru C.D., Neacsu I.A., Grumezescu A.M., Andronescu E. Bee-Derived Products: Chemical Composition and Applications in Skin Tissue Engineering. Pharmaceutics. 2022;14:750. doi: 10.3390/pharmaceutics14040750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strodtbeck F. Physiology of Wound Healing. Newborn Infant Nurs. Rev. 2001;1:43–52. doi: 10.1053/nbin.2001.23176. [DOI] [Google Scholar]
- 15.Martin P. Wound Healing--Aiming for Perfect Skin Regeneration. Science. 1997;276:75–81. doi: 10.1126/science.276.5309.75. [DOI] [PubMed] [Google Scholar]
- 16.Eming S.A., Krieg T., Davidson J.M. Inflammation in Wound Repair: Molecular and Cellular Mechanisms. J. Investig. Dermatol. 2007;127:514–525. doi: 10.1038/sj.jid.5700701. [DOI] [PubMed] [Google Scholar]
- 17.Tziotzios C., Profyris C., Sterling J. Cutaneous Scarring: Pathophysiology, Molecular Mechanisms, and Scar Reduction Therapeutics. J. Am. Acad. Dermatol. 2012;66:13–24. doi: 10.1016/j.jaad.2011.08.035. [DOI] [PubMed] [Google Scholar]
- 18.Koh T.J., DiPietro L.A. Inflammation and Wound Healing: The Role of the Macrophage. Expert Rev. Mol. Med. 2011;13:e23. doi: 10.1017/S1462399411001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Desmouliere A., Darby I.A., Laverdet B., Bonté F. Fibroblasts and Myofibroblasts in Wound Healing. Clin. Cosmet. Investig. Dermatol. 2014;7:301. doi: 10.2147/CCID.S50046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grey J.E., Enoch S., Harding K.G. Wound Assessment. BMJ. 2006;332:285–288. doi: 10.1136/bmj.332.7536.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krzyszczyk P., Schloss R., Palmer A., Berthiaume F. The Role of Macrophages in Acute and Chronic Wound Healing and Interventions to Promote Pro-Wound Healing Phenotypes. Front. Physiol. 2018;9:419. doi: 10.3389/fphys.2018.00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson K.E., Wilgus T.A. Vascular Endothelial Growth Factor and Angiogenesis in the Regulation of Cutaneous Wound Repair. Adv. Wound Care. 2014;3:647–661. doi: 10.1089/wound.2013.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miricescu D., Badoiu S.C., Stanescu-Spinu I.-I., Totan A.R., Stefani C., Greabu M. Growth Factors, Reactive Oxygen Species, and Metformin—Promoters of the Wound Healing Process in Burns? Int. J. Mol. Sci. 2021;22:9512. doi: 10.3390/ijms22179512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodrigues M., Kosaric N., Bonham C.A., Gurtner G.C. Wound Healing: A Cellular Perspective. Physiol. Rev. 2019;99:665–706. doi: 10.1152/physrev.00067.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moretti L., Stalfort J., Barker T.H., Abebayehu D. The Interplay of Fibroblasts, the Extracellular Matrix, and Inflammation in Scar Formation. J. Biol. Chem. 2022;298:101530. doi: 10.1016/j.jbc.2021.101530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xue M., Jackson C.J. Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring. Adv. Wound Care. 2015;4:119–136. doi: 10.1089/wound.2013.0485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen H., Li G., Liu Y., Ji S., Li Y., Xiang J., Zhou L., Gao H., Zhang W., Sun X., et al. Pleiotropic Roles of CXCR4 in Wound Repair and Regeneration. Front. Immunol. 2021;12:668758. doi: 10.3389/fimmu.2021.668758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pittayapruek P., Meephansan J., Prapapan O., Komine M., Ohtsuki M. Role of Matrix Metalloproteinases in Photoaging and Photocarcinogenesis. Int. J. Mol. Sci. 2016;17:868. doi: 10.3390/ijms17060868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levin M., Udi Y., Solomonov I., Sagi I. Next Generation Matrix Metalloproteinase Inhibitors—Novel Strategies Bring New Prospects. Biochim. Biophys. Acta Mol. Cell Res. 2017;1864:1927–1939. doi: 10.1016/j.bbamcr.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 30.Rajkumar V.S., Shiwen X., Bostrom M., Leoni P., Muddle J., Ivarsson M., Gerdin B., Denton C.P., Bou-Gharios G., Black C.M., et al. Platelet-Derived Growth Factor-β Receptor Activation Is Essential for Fibroblast and Pericyte Recruitment during Cutaneous Wound Healing. Am. J. Pathol. 2006;169:2254–2265. doi: 10.2353/ajpath.2006.060196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang C., Brisson B.K., Terajima M., Li Q., Hoxha K., Han B., Goldberg A.M., Sherry Liu X., Marcolongo M.S., Enomoto-Iwamoto M., et al. Type III Collagen Is a Key Regulator of the Collagen Fibrillar Structure and Biomechanics of Articular Cartilage and Meniscus. Matrix Biol. 2020;85–86:47–67. doi: 10.1016/j.matbio.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zou M.-L., Teng Y.-Y., Wu J.-J., Liu S.-Y., Tang X.-Y., Jia Y., Chen Z.-H., Zhang K.-W., Sun Z.-L., Li X., et al. Fibroblasts: Heterogeneous Cells With Potential in Regenerative Therapy for Scarless Wound Healing. Front. Cell Dev. Biol. 2021;9:713605. doi: 10.3389/fcell.2021.713605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eriksson E., Liu P.Y., Schultz G.S., Martins-Green M.M., Tanaka R., Weir D., Gould L.J., Armstrong D.G., Gibbons G.W., Wolcott R., et al. Chronic Wounds: Treatment Consensus. Wound Repair Regen. 2022;30:156–171. doi: 10.1111/wrr.12994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Czubryt M.P. Common Threads in Cardiac Fibrosis, Infarct Scar Formation, and Wound Healing. Fibrogenesis Tissue Repair. 2012;5:19. doi: 10.1186/1755-1536-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ticona L.A., Sánchez Á.R., Sánchez-Corral J.S., Moreno P.I., Domenech M.O. Anti-Inflammatory, pro-Proliferative and Antimicrobial Potential of the Compounds Isolated from Daemonorops Draco (Willd.) Blume. J. Ethnopharmacol. 2021;268:113668. doi: 10.1016/j.jep.2020.113668. [DOI] [PubMed] [Google Scholar]
- 36.Park S.Y., Lee H.U., Lee Y.-C.C., Kim G.H., Park E.C., Han S.H., Lee J.J.G., Choi S., Heo N.S., Kim D.L., et al. Wound Healing Potential of Antibacterial Microneedles Loaded with Green Tea Extracts. Mater. Sci. Eng. C. 2014;42:757–762. doi: 10.1016/j.msec.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 37.Badiu D.L., Balu A.M., Barbes L., Luque R., Nita R., Radu M., Tanase E., Rosoiu N. Physico-Chemical Characterisation of Lipids from Mytilus Galloprovincialis (L.) and Rapana Venosa and Their Healing Properties on Skin Burns. Lipids. 2008;43:829–841. doi: 10.1007/s11745-008-3205-2. [DOI] [PubMed] [Google Scholar]
- 38.Benedek B., Rothwangl-Wiltschnigg K., Rozema E., Gjoncaj N., Reznicek G., Jurenitsch J., Kopp B., Glasl S. Yarrow (Achillea Millefolium L. s.l.): Pharmaceutical Quality of Commercial Samples. Pharmazie. 2008;63:23–26. [PubMed] [Google Scholar]
- 39.Bonte F., Dumas M., Chaudagne C., Meybeck A. Influence of Asiatic Acid, Madecassic Acid, and Asiaticoside on Human Collagen I Synthesis. Planta Med. 1994;60:133–135. doi: 10.1055/s-2006-959434. [DOI] [PubMed] [Google Scholar]
- 40.Carvalho F.A., Uchina H.S., Borges F.A., Oyafuso M.H., Herculano R.D., Gremião M.P.D., Santos A.G. Natural Membranes of Hevea Brasiliensis Latex as Delivery System for Casearia Sylvestris Leaf Components. Rev. Bras. Farmacogn. 2018;28:102–110. doi: 10.1016/j.bjp.2017.10.007. [DOI] [Google Scholar]
- 41.Chen W.C., Liou S.S., Tzeng T.F., Lee S.L., Liu I.M. Effect of Topical Application of Chlorogenic Acid on Excision Wound Healing in Rats. Planta Med. 2013;79:616–621. doi: 10.1055/s-0032-1328364. [DOI] [PubMed] [Google Scholar]
- 42.Chen L.Y., Cheng H.L., Kuan Y.H., Liang T.J., Chao Y.Y., Lin H.C. Therapeutic Potential of Luteolin on Impaired Wound Healing in Streptozotocin-Induced Rats. Biomedicines. 2021;9:761. doi: 10.3390/biomedicines9070761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cho S., Lee S., Lee M.J., Lee D.H., Won C.H., Kim S.M., Chung J.H. Dietary Aloe Vera Supplementation Improves Facial Wrinkles and Elasticity and It Increases the Type i Procollagen Gene Expression in Human Skin in Vivo. Ann. Dermatol. 2009;21:6–11. doi: 10.5021/ad.2009.21.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yu L., Xie J., Xin N., Wang Z. Panax Notoginseng Saponins Promote Wound Repair of Anterior Cruciate Ligament through Phosphorylation of PI3K, AKT and ERK. Int. J. Clin. Exp. Pathol. 2015;8:441–449. [PMC free article] [PubMed] [Google Scholar]
- 45.Alemzadeh E., Oryan A. Effectiveness of a Crocus Sativus Extract on Burn Wounds in Rats. Planta Med. 2018;84:1191–1200. doi: 10.1055/a-0631-3620. [DOI] [PubMed] [Google Scholar]
- 46.Almasian A., Najafi F., Eftekhari M., Ardekani M.R.S., Sharifzadeh M., Khanavi M. Polyurethane/Carboxymethylcellulose Nanofibers Containing Malva Sylvestris Extract for Healing Diabetic Wounds: Preparation, Characterization, in Vitro and in Vivo Studies. Mater. Sci. Eng. C. 2020;114:111039. doi: 10.1016/j.msec.2020.111039. [DOI] [PubMed] [Google Scholar]
- 47.Elshamy A.I., Ammar N.M., Hassan H.A., El-Kashak W.A., Al-Rejaie S.S., Abd-ElGawad A.M., Farrag A.-R.R.H. Topical Wound Healing Activity of Myricetin Isolated from Tecomaria Capensis v. Aurea. Molecules. 2020;25:4870. doi: 10.3390/molecules25214870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ambiga S., Narayanan R., Gowri D., Sukumar D., Madhavan S. Evaluation of wound healing activity of flavonoids from ipomoea carnea Jacq. Anc. Sci. Life. 2007;26:45–51. [PMC free article] [PubMed] [Google Scholar]
- 49.Song M., Chen L., Zhang L., Li C., Coffie J.W., Fang Z., Zhang L., Wang S., Gao X., Wang H. Cryptotanshinone Enhances Wound Healing in Type 2 Diabetes with Modulatory Effects on Inflammation, Angiogenesis and Extracellular Matrix Remodelling. Pharm. Biol. 2020;58:845–853. doi: 10.1080/13880209.2020.1803369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yeh C.-J., Chen C.-C., Leu Y.-L., Lin M.-W., Chiu M.-M., Wang S.-H. The Effects of Artocarpin on Wound Healing: In Vitro and in Vivo Studies. Sci. Rep. 2017;7:15599. doi: 10.1038/s41598-017-15876-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Majtan J. Methylglyoxal—A Potential Risk Factor of Manuka Honey in Healing of Diabetic Ulcers. Evid.-Based Complement. Altern. Med. 2011;2011:295494. doi: 10.1093/ecam/neq013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Atrott J., Henle T. Methylglyoxal in Manuka Honey—Correlation with Antibacterial Properties. Czech J. Food Sci. 2009;27:S163–S165. doi: 10.17221/911-CJFS. [DOI] [Google Scholar]
- 53.Wang X., Xu P., Yao Z., Fang Q., Feng L., Guo R., Cheng B. Preparation of Antimicrobial Hyaluronic Acid/Quaternized Chitosan Hydrogels for the Promotion of Seawater-Immersion Wound Healing. Front. Bioeng. Biotechnol. 2019;7:360. doi: 10.3389/fbioe.2019.00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kant V., Jangir B.L., Nigam A., Kumar V., Sharma S. Dose Regulated Cutaneous Wound Healing Potential of Quercetin in Male Rats. Wound Med. 2017;19:82–87. doi: 10.1016/j.wndm.2017.10.004. [DOI] [Google Scholar]
- 55.Nguyen V.-L., Truong C.-T., Nguyen B.C.Q., Van Vo T.-N., Dao T.-T., Nguyen V.-D., Trinh D.-T.T., Huynh H.K., Bui C.-B. Anti-Inflammatory and Wound Healing Activities of Calophyllolide Isolated from Calophyllum Inophyllum Linn. PLoS ONE. 2017;12:e0185674. doi: 10.1371/journal.pone.0185674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Di R., Murray A.F., Xiong J., Esposito D., Komarnytsky S., Gianfagna T.J., Munafo J.P. Lily Steroidal Glycoalkaloid Promotes Early Inflammatory Resolution in Wounded Human Fibroblasts. J. Ethnopharmacol. 2020;258:112766. doi: 10.1016/j.jep.2020.112766. [DOI] [PubMed] [Google Scholar]
- 57.Mohanty C., Das M., Sahoo S.K. Sustained Wound Healing Activity of Curcumin Loaded Oleic Acid Based Polymeric Bandage in a Rat Model. Mol. Pharm. 2012;9:2801–2811. doi: 10.1021/mp300075u. [DOI] [PubMed] [Google Scholar]
- 58.Beserra F.P., Gushiken L.F.S., Vieira A.J., Bérgamo D.A., Bérgamo P.L., de Souza M.O., Hussni C.A., Takahira R.K., Nóbrega R.H., Martinez E.R.M., et al. From Inflammation to Cutaneous Repair: Topical Application of Lupeol Improves Skin Wound Healing in Rats by Modulating the Cytokine Levels, NF-ΚB, Ki-67, Growth Factor Expression, and Distribution of Collagen Fibers. Int. J. Mol. Sci. 2020;21:4952. doi: 10.3390/ijms21144952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sklenářová R., Svrčková M., Hodek P., Ulrichová J., Franková J. Effect of the Natural Flavonoids Myricetin and Dihydromyricetin on the Wound Healing Process in Vitro. J. Appl. Biomed. 2021;19:149–158. doi: 10.32725/jab.2021.017. [DOI] [PubMed] [Google Scholar]
- 60.Phan T.-T., See P., Lee S.-T., Chan S.-Y. Protective Effects of Curcumin against Oxidative Damage on Skin Cells In Vitro: Its Implication for Wound Healing. J. Trauma Inj. Infect. Crit. Care. 2001;51:927–931. doi: 10.1097/00005373-200111000-00017. [DOI] [PubMed] [Google Scholar]
- 61.Yang D., Moh S., Son D., You S., Kinyua A., Ko C., Song M., Yeo J., Choi Y.-H., Kim K. Gallic Acid Promotes Wound Healing in Normal and Hyperglucidic Conditions. Molecules. 2016;21:899. doi: 10.3390/molecules21070899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Genc Y., Harput U.S., Saracoglu I. Active Compounds Isolated from Plantago Subulata L. via Wound Healing and Antiinflammatory Activity Guided Studies. J. Ethnopharmacol. 2019;241:112030. doi: 10.1016/j.jep.2019.112030. [DOI] [PubMed] [Google Scholar]
- 63.Mi Y., Zhong L., Lu S., Hu P., Pan Y., Ma X., Yan B., Wei Z., Yang G. Quercetin Promotes Cutaneous Wound Healing in Mice through Wnt/β-Catenin Signaling Pathway. J. Ethnopharmacol. 2022;290:115066. doi: 10.1016/j.jep.2022.115066. [DOI] [PubMed] [Google Scholar]
- 64.Kant V., Jangir B.L., Kumar V., Nigam A., Sharma V. Quercetin Accelerated Cutaneous Wound Healing in Rats by Modulation of Different Cytokines and Growth Factors. Growth Factors. 2020;38:105–119. doi: 10.1080/08977194.2020.1822830. [DOI] [PubMed] [Google Scholar]
- 65.Zhao X., Pei D., Yang Y., Xu K., Yu J., Zhang Y., Zhang Q., He G., Zhang Y., Li A., et al. Green Tea Derivative Driven Smart Hydrogels with Desired Functions for Chronic Diabetic Wound Treatment. Adv. Funct. Mater. 2021;31:2009442. doi: 10.1002/adfm.202009442. [DOI] [Google Scholar]
- 66.Dube A., Ng K., Nicolazzo J.A., Larson I. Effective Use of Reducing Agents and Nanoparticle Encapsulation in Stabilizing Catechins in Alkaline Solution. Food Chem. 2010;122:662–667. doi: 10.1016/j.foodchem.2010.03.027. [DOI] [Google Scholar]
- 67.Frydman G.H., Olaleye D., Annamalai D., Layne K., Yang I., Kaafarani H.M.A., Fox J.G. Manuka Honey Microneedles for Enhanced Wound Healing and the Prevention and/or Treatment of Methicillin-Resistant Staphylococcus Aureus (MRSA) Surgical Site Infection. Sci. Rep. 2020;10:13229. doi: 10.1038/s41598-020-70186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gao L., Zhang H., Yu B., Li W., Gao F., Zhang K., Zhang H., Shen Y., Cong H. Chitosan Composite Hydrogels Cross-linked by Multifunctional Diazo Resin as Antibacterial Dressings for Improved Wound Healing. J. Biomed. Mater. Res. Part A. 2020;108:1890–1898. doi: 10.1002/jbm.a.36952. [DOI] [PubMed] [Google Scholar]
- 69.Dinda M., Mazumdar S., Das S., Ganguly D., Dasgupta U.B., Dutta A., Jana K., Karmakar P. The Water Fraction of Calendula officinalis Hydroethanol Extract Stimulates In Vitro and In Vivo Proliferation of Dermal Fibroblasts in Wound Healing. Phyther. Res. 2016;1707:1696–1707. doi: 10.1002/ptr.5678. [DOI] [PubMed] [Google Scholar]
- 70.Badiu D.L., Luque R., Dumitrescu E., Craciun A., Dinca D. Amino Acids from Mytilus Galloprovincialis (L.) and Rapana Venosa Molluscs Accelerate Skin Wounds Healing via Enhancement of Dermal and Epidermal Neoformation. Protein. J. 2010;29:81–92. doi: 10.1007/s10930-009-9225-9. [DOI] [PubMed] [Google Scholar]
- 71.Ulagesan S., Sankaranarayanan K., Kuppusamy A. Functional Characterisation of Bioactive Peptide Derived from Terrestrial Snail Cryptozona Bistrialis and Its Wound-Healing Property in Normal and Diabetic-Induced Wistar Albino Rats. Int. Wound J. 2018;15:350–362. doi: 10.1111/iwj.12872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Akrawi S.H., Gorain B., Nair A.B., Choudhury H., Pandey M., Shah J.N., Venugopala K.N. Development and Optimization of Naringenin-Loaded Chitosan-Coated Nanoemulsion for Topical Therapy in Wound Healing. Pharmaceutics. 2020;12:893. doi: 10.3390/pharmaceutics12090893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yao C., Yao P., Wu H., Zha Z. Acceleration of Wound Healing in Traumatic Ulcers by Absorbable Collagen Sponge Containing Recombinant Basic Fibroblast Growth Factor. Biomed. Mater. 2006;1:33–37. doi: 10.1088/1748-6041/1/1/005. [DOI] [PubMed] [Google Scholar]
- 74.Başer K.H., Demirci B., Demirci F., Koçak S., Akıncı Ç., Malyer H., Güleryüz G. Composition and Antimicrobial Activity of the Essential Oil of Achillea Multifida. Planta Med. 2002;68:941–943. doi: 10.1055/s-2002-34923. [DOI] [PubMed] [Google Scholar]
- 75.Güzel S., Özay Y., Kumaş M., Uzun C., Özkorkmaz E.G., Yıldırım Z., Ülger M., Güler G., Çelik A., Çamlıca Y., et al. Wound healing properties, antimicrobial and antioxidant activities of Salvia kronenburgii and Salvia euphratica var. euphratica on excision and incision wound models in diabetic rats. Biomed. Pharmacother. 2019;111:1260–1276. doi: 10.1016/j.biopha.2019.01.038. [DOI] [PubMed] [Google Scholar]
- 76.Tadić V., Arsić I., Zvezdanović J., Zugić A., Cvetković D., Pavkov S. The Estimation of the Traditionally Used Yarrow (Achillea Millefolium L. Asteraceae) Oil Extracts with Anti-Inflamatory Potential in Topical Application. J. Ethnopharmacol. 2017;199:138–148. doi: 10.1016/j.jep.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 77.Dorjsembe B., Lee H.J., Kim M., Dulamjav B., Jigjid T., Nho C.W. Achillea Asiatica Extract and Its Active Compounds Induce Cutaneous Wound Healing. J. Ethnopharmacol. 2017;206:306–314. doi: 10.1016/j.jep.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 78.Farahpour M.R., Pirkhezr E., Ashrafian A., Sonboli A. Accelerated Healing by Topical Administration of Salvia Officinalis Essential Oil on Pseudomonas Aeruginosa and Staphylococcus Aureus Infected Wound Model. Biomed. Pharmacother. 2020;128:110120. doi: 10.1016/j.biopha.2020.110120. [DOI] [PubMed] [Google Scholar]
- 79.Fetse J., Kyekyeku J., Dueve E., Mensah K. Wound Healing Activity of Total Alkaloidal Extract of the Root Bark of Alstonia Boonei (Apocynacea) Br. J. Pharm. Res. 2014;4:2642–2652. doi: 10.9734/BJPR/2014/13952. [DOI] [Google Scholar]
- 80.Fronza M., Heinzmann B., Hamburger M., Laufer S., Merfort I. Determination of the Wound Healing Effect of Calendula Extracts Using the Scratch Assay with 3T3 Fibroblasts. J. Ethnopharmacol. 2009;126:463–467. doi: 10.1016/j.jep.2009.09.014. [DOI] [PubMed] [Google Scholar]
- 81.Fu J., Huang J., Lin M., Xie T., You T. Quercetin Promotes Diabetic Wound Healing via Switching Macrophages From M1 to M2 Polarization. J. Surg. Res. 2020;246:213–223. doi: 10.1016/j.jss.2019.09.011. [DOI] [PubMed] [Google Scholar]
- 82.Gadekar R., Saurabh M.K., Thakur G.S., Saurabh A. Study of Formulation, Characterisation and Wound Healing Potential of Transdermal Patches of Curcumin. Asian J. Pharm. Clin. Res. 2012;5:225–230. [Google Scholar]
- 83.De Campos E.P., Trombini L.N., Rodrigues R., Portella D.L., Werner A.C., Ferraz M.C., De Oliveira R.V.M.H., Cogo J.C., Oshima-Franco Y., Aranha N., et al. Healing Activity of Casearia Sylvestris Sw. in Second-Degree Scald Burns in Rodents. BMC Res. Notes. 2015;8:1–8. doi: 10.1186/s13104-015-1251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ghaisas M.M., Kshirsagar S.B., Sahane R.S. Evaluation of Wound Healing Activity of Ferulic Acid in Diabetic Rats. Int. Wound J. 2014;11:523–532. doi: 10.1111/j.1742-481X.2012.01119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ghanadian M., Soltani R., Homayouni A., Khorvash F., Jouabadi S.M., Abdollahzadeh M. The Effect of Plantago Major Hydroalcoholic Extract on the Healing of Diabetic Foot and Pressure Ulcers: A Randomized Open-Label Controlled Clinical Trial. Int. J. Low. Extrem. Wounds. 2022 doi: 10.1177/15347346211070723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gourishetti K., Keni R., Nayak P.G., Jitta S.R., Bhaskaran N.A., Kumar L., Kumar N., Krishnadas N., Shenoy R.R. Sesamol-Loaded Plga Nanosuspension for Accelerating Wound Healing in Diabetic Foot Ulcer in Rats. Int. J. Nanomedicine. 2020;15:9265–9282. doi: 10.2147/IJN.S268941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Han X., Tao Y., Deng Y., Yu J., Sun Y., Jiang G. Metformin Accelerates Wound Healing in Type 2 Diabetic Db/Db Mice. Mol. Med. Rep. 2017;16:8691–8698. doi: 10.3892/mmr.2017.7707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hanafi N., Talebpour Amiri F., Shahani S., Enayatifard R., Ghasemi M., Karimpour A.A. Licorice Cream Promotes Full-Thickness Wound Healing in Guinea Pigs. Marmara Pharm. J. 2018;22:411–421. doi: 10.12991/jrp.2018.81. [DOI] [Google Scholar]
- 89.Hou Q., Li M., Lu Y.H., Liu D.H., Li C.C. Burn Wound Healing Properties of Asiaticoside and Madecassoside. Exp. Ther. Med. 2016;12:1269–1274. doi: 10.3892/etm.2016.3459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hsiao C.Y., Hung C.Y., Tsai T.H., Chak K.F. A Study of the Wound Healing Mechanism of a Traditional Chinese Medicine, Angelica Sinensis, Using a Proteomic Approach. Evid.-Based Complement. Altern. Med. 2012;2012:467531. doi: 10.1155/2012/467531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hu W., Wang A.M., Wu S.Y., Zhang B., Liu S., Gou Y.B., Wang J.M. Debriding Effect of Bromelain on Firearm Wounds in Pigs. J. Trauma. Inj. Infect. Crit. Care. 2011;71:966–972. doi: 10.1097/TA.0b013e3182028929. [DOI] [PubMed] [Google Scholar]
- 92.Kandhare A.D., Alam J., Patil M.V.K., Sinha A., Bodhankar S.L. Wound Healing Potential of Naringin Ointment Formulation via Regulating the Expression of Inflammatory, Apoptotic and Growth Mediators in Experimental Rats. Pharm. Biol. 2016;54:419–432. doi: 10.3109/13880209.2015.1038755. [DOI] [PubMed] [Google Scholar]
- 93.Kang C.W., Han Y.E., Kim J., Oh J.H., Cho Y.H., Lee E.J. 4-Hydroxybenzaldehyde Accelerates Acute Wound Healing through Activation of Focal Adhesion Signalling in Keratinocytes. Sci. Rep. 2017;7:14192. doi: 10.1038/s41598-017-14368-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dinda M., Dasgupta U., Singh N., Bhattacharyya D., Karmakar P. PI3K-Mediated Proliferation of Fibroblasts by Calendula officinalis Tincture: Implication in Wound Healing. Phyther. Res. 2015;29:607–616. doi: 10.1002/ptr.5293. [DOI] [PubMed] [Google Scholar]
- 95.Karakaş F.P., Karakaş A., Boran Ç., Türker A.U., Yalçin F.N., Bilensoy E. The Evaluation of Topical Administration of Bellis Perennis Fraction on Circular Excision Wound Healing in Wistar Albino Rats. Pharm. Biol. 2012;50:1031–1037. doi: 10.3109/13880209.2012.656200. [DOI] [PubMed] [Google Scholar]
- 96.Karatas O., Gevrek F. Gallic Acid Liposome and Powder Gels Improved Wound Healing in Wistar Rats. Ann. Med. Res. 2019;26:2720. doi: 10.5455/annalsmedres.2019.05.301. [DOI] [Google Scholar]
- 97.Karimzadeh S., Farahpour M.R. Topical Application of Salvia Officinalis Hydroethanolic Leaf Extract Improves Wound Healing Process. Indian J. Exp. Biol. 2017;55:98–106. [PubMed] [Google Scholar]
- 98.Kharat Z., Amiri Goushki M., Sarvian N., Asad S., Dehghan M.M., Kabiri M. Chitosan/PEO Nanofibers Containing Calendula officinalis Extract: Preparation, Characterization, in Vitro and in Vivo Evaluation for Wound Healing Applications. Int. J. Pharm. 2021;609:121132. doi: 10.1016/j.ijpharm.2021.121132. [DOI] [PubMed] [Google Scholar]
- 99.Khorasani G., Hosseinimehr S.J., Zamani P., Ghasemi M., Ahmadi A. The Effect of Saffron (Crocus Sativus) Extract for Healing of Second-Degree Burn Wounds in Rats. Keio J. Med. 2008;57:190–195. doi: 10.2302/kjm.57.190. [DOI] [PubMed] [Google Scholar]
- 100.Kumar S., Ghosh D., Biswas T.K., Dutta U., Das P., Kundu S. Spermatheca Gland Extract of Snail (Telescopium Telescopium) Has Wound Healing Potential: An Experimental Study in Rabbits. Int. J. Low. Extrem. Wounds. 2008;7:204–209. doi: 10.1177/1534734608326916. [DOI] [PubMed] [Google Scholar]
- 101.Labib R.M., Ayoub I.M., Michel H.E., Mehanny M., Kamil V., Hany M., Magdy M., Moataz A., Maged B., Mohamed A. Appraisal on the Wound Healing Potential of Melaleuca Alternifolia and Rosmarinus officinalis L. Essential Oil-Loaded Chitosan Topical Preparations. PLoS ONE. 2019;14:e0219561. doi: 10.1371/journal.pone.0219561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li W., Kandhare A.D., Mukherjee A.A., Bodhankar S.L. Hesperidin, a Plant Flavonoid Accelerated the Cutaneous Wound Healing in Streptozotocin-Induced Diabetic Rats: Role of TGF-B/SMADS and ANG-1/TIE-2 Signaling Pathways. EXCLI J. 2018;17:399–419. doi: 10.17179/excli2018-1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li X., Zhai Y., Xi B., Ma W., Zhang J., Ma X., Miao Y., Zhao Y., Ning W., Zhou H., et al. Pinocembrin Ameliorates Skin Fibrosis via Inhibiting Tgf-β1 Signaling Pathway. Biomolecules. 2021;11:1240. doi: 10.3390/biom11081240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liu Y.Y., Wu J.Q., Fan R.Y., He Z.H., Li C.Y., He M.F. Isoliquiritin Promote Angiogenesis by Recruiting Macrophages to Improve the Healing of Zebrafish Wounds. Fish Shellfish Immunol. 2020;100:238–245. doi: 10.1016/j.fsi.2020.02.071. [DOI] [PubMed] [Google Scholar]
- 105.Su X., Liu X., Wang S., Li B., Pan T., Liu D., Wang F., Diao Y., Li K. Wound-Healing Promoting Effect of Total Tannins from Entada phaseoloides (L.) Merr. in Rats. Burns. 2017;43:830–838. doi: 10.1016/j.burns.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 106.Lodhi S., Singhai A.K. Wound Healing Effect of Flavonoid Rich Fraction and Luteolin Isolated from Martynia Annua Linn. on Streptozotocin Induced Diabetic Rats. Asian Pac. J. Trop. Med. 2013;6:253–259. doi: 10.1016/S1995-7645(13)60053-X. [DOI] [PubMed] [Google Scholar]
- 107.Luo Y., Diao H., Xia S., Dong L., Chen J., Zhang J. A Physiologically Active Polysaccharide Hydrogel Promotes Wound Healing. J. Biomed. Mater. Res. Part A. 2010;94:193–204. doi: 10.1002/jbm.a.32711. [DOI] [PubMed] [Google Scholar]
- 108.Luo X., Huang P., Yuan B., Liu T., Lan F., Lu X., Dai L., Liu Y., Yin H. Astragaloside IV Enhances Diabetic Wound Healing Involving Upregulation of Alternatively Activated Macrophages. Int. Immunopharmacol. 2016;35:22–28. doi: 10.1016/j.intimp.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 109.Ma X., Lin Y., Liu Y., Li W., He J., Fang M., Lin D. Effects of Apigenin Treatment on Random Skin Flap Survival in Rats. Front. Pharmacol. 2021;12:625733. doi: 10.3389/fphar.2021.625733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Manconi M., Manca M.L., Caddeo C., Cencetti C., di Meo C., Zoratto N., Nacher A., Fadda A.M., Matricardi P. Preparation of Gellan-Cholesterol Nanohydrogels Embedding Baicalin and Evaluation of Their Wound Healing Activity. Eur. J. Pharm. Biopharm. 2018;127:244–249. doi: 10.1016/j.ejpb.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 111.Mandawgade S.D., Patil K.S. Wound Healing Potential of Some Active Principles of Lawsonia Alba Lam. Leaves. Indian J. Pharm. Sci. 2003;65:390–394. [Google Scholar]
- 112.Marquele-Oliveira F., da Silva Barud H., Torres E.C., Machado R.T.A., Caetano G.F., Leite M.N., Frade M.A.C., Ribeiro S.J.L., Berretta A.A. Development, Characterization and Pre-Clinical Trials of an Innovative Wound Healing Dressing Based on Propolis (EPP-AF®)-Containing Self-Microemulsifying Formulation Incorporated in Biocellulose Membranes. Int. J. Biol. Macromol. 2019;136:570–578. doi: 10.1016/j.ijbiomac.2019.05.135. [DOI] [PubMed] [Google Scholar]
- 113.Mazzotta S., Governa P., Borgonetti V., Marcolongo P., Nanni C., Gamberucci A., Manetti F., Pessina F., Carullo G., Brizzi A., et al. Pinocembrin and Its Linolenoyl Ester Derivative Induce Wound Healing Activity in HaCaT Cell Line Potentially Involving a GPR120/FFA4 Mediated Pathway. Bioorg. Chem. 2021;108:104657. doi: 10.1016/j.bioorg.2021.104657. [DOI] [PubMed] [Google Scholar]
- 114.Mellin T.N., Cashen D.E., Ronan J., Murphy B.S., DiSalvo J., Thomas K.A. Acidic Fibroblast Growth Factor Accelerates Dermal Wound Healing in Diabetic Mice. J. Investig. Dermatol. 1995;104:850–855. doi: 10.1111/1523-1747.ep12607026. [DOI] [PubMed] [Google Scholar]
- 115.Mittraphab Y., Nagata M., Matsumoto M., Shimizu K. Antioxidant and Protective Effect of Acetone Extract of Entada phaseoloides Leaves on UVB-Irradiated Human Epidermal Keratinocytes (HaCaT Cells) by Inhibiting COX-2, INOS, and Caspase-3 Activation. Nat. Prod. Commun. 2022;17:1934578X221078627. doi: 10.1177/1934578X221078627. [DOI] [Google Scholar]
- 116.García-Salinas S., Evangelopoulos M., Gámez-Herrera E., Arruebo M., Irusta S., Taraballi F., Mendoza G., Tasciotti E. Electrospun Anti-Inflammatory Patch Loaded with Essential Oils for Wound Healing. Int. J. Pharm. 2020;577:119067. doi: 10.1016/j.ijpharm.2020.119067. [DOI] [PubMed] [Google Scholar]
- 117.Mo J., Panichayupakaranant P., Kaewnopparat N., Nitiruangjaras A., Reanmongkol W. Wound Healing Activities of Standardized Pomegranate Rind Extract and Its Major Antioxidant Ellagic Acid in Rat Dermal Wounds. J. Nat. Med. 2014;68:377–386. doi: 10.1007/s11418-013-0813-9. [DOI] [PubMed] [Google Scholar]
- 118.Mochizuki S., Takano M., Sugano N., Ohtsu M., Tsunoda K., Koshi R., Yoshinuma N. The Effect of B Vitamin Supplementation on Wound Healing in Type 2 Diabetic Mice. J. Clin. Biochem. Nutr. 2016;58:64–68. doi: 10.3164/jcbn.14-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mohammed B.M., Fisher B.J., Kraskauskas D., Ward S., Wayne J.S., Brophy D.F., Fowler A.A., Yager D.R., Natarajan R. Vitamin C Promotes Wound Healing through Novel Pleiotropic Mechanisms. Int. Wound J. 2016;13:572–584. doi: 10.1111/iwj.12484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Moura-Letts G., Villegas L.F., Marçalo A., Vaisberg A.J., Hammond G.B. In Vivo Wound-Healing Activity of Oleanolic Acid Derived from the Acid Hydrolysis of Anredera Diffusa. J. Nat. Prod. 2006;69:978–979. doi: 10.1021/np0601152. [DOI] [PubMed] [Google Scholar]
- 121.Nair A.V., Raman M., Doble M. Cyclic β-(1→3) (1→6) Glucan/Carrageenan Hydrogels for Wound Healing Applications. RSC Adv. 2016;6:98545–98553. doi: 10.1039/C6RA23386D. [DOI] [Google Scholar]
- 122.Do Nascimento J.E.T., Rodrigues A.L.M., De Lisboa D.S., Liberato H.R., Falcão M.J.C., Da Silva C.R., Nobre Júnior H.V., Braz Filho R., De Paula Junior V.F., Alves D.R., et al. Chemical Composition and Antifungal in Vitro and in Silico, Antioxidant, and Anticholinesterase Activities of Extracts and Constituents of Ouratea Fieldingiana (DC.) Baill. Evid.-Based Complement. Altern. Med. 2018;2018:1748487. doi: 10.1155/2018/1748487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nasiri E., Hosseinimehr S.J., Azadbakht M., Akbari J., Enayati-Fard R., Azizi S. Effect of Malva Sylvestris Cream on Burn Injury and Wounds in Rats. Avicenna J. Phytomedicine. 2015;5:341–354. [PMC free article] [PubMed] [Google Scholar]
- 124.Nicolaus C., Junghanns S., Hartmann A., Murillo R., Ganzera M., Merfort I. In Vitro Studies to Evaluate the Wound Healing Properties of Calendula officinalis Extracts. J. Ethnopharmacol. 2017;196:94–103. doi: 10.1016/j.jep.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 125.Nikita G., Vivek P., Chhaya G. Wound-Healing Activity of an Oligomer of Alkannin/Shikonin, Isolated from Root Bark of Onosma Echioides. Nat. Prod. Res. 2015;29:1584–1588. doi: 10.1080/14786419.2014.986126. [DOI] [PubMed] [Google Scholar]
- 126.Oloumi M.M., Derakhshanfar A., Nikpoor A. Healing Potential of Liquorice Root Extract on Dermal Wounds in Rats. J. Vetinary Res. 2007;62:147–154. [Google Scholar]
- 127.Novianty R.A., Chrismawaty B.E., Subagyo G. Effect of Allicin for Re-Epithelialization During Healing in Oral Ulcer Model. Indones. J. Dent. Res. 2015;1:87. doi: 10.22146/theindjdentres.9990. [DOI] [Google Scholar]
- 128.Ozdemir O., Ozkan K., Hatipoglu F., Uyaroglu A., Arican M. Effect of Asiaticoside, Collagenase, and Alpha-Chymotrypsin on Wound Healing in Rabbits. Wounds. 2016;28:279–286. [PubMed] [Google Scholar]
- 129.Parente L.M.L., Lino Júnior R.D.S., Tresvenzol L.M.F., Vinaud M.C., De Paula J.R., Paulo N.M. Wound Healing and Anti-Inflammatory Effect in Animal Models of Calendula officinalis L. Growing in Brazil. Evid.-Based Complement. Altern. Med. 2012;2012:375671. doi: 10.1155/2012/375671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pirbalouti A.G., Shahrzad A., Abed K., Hamedi B. Wound Healing Activity of Malva Sylvestris and Punica Granatum in Alloxan-Induced Diabetic Rats. Acta Pol. Pharm. Drug Res. 2010;67:511–516. [PubMed] [Google Scholar]
- 131.Primarizky H., Yuniarti W.M., Lukiswanto B.S. Ellagic Acid Activity in Healing Process of Incision Wound on Male Albino Rats (Rattus Norvegicus) KnE Life Sci. 2017;3:224. doi: 10.18502/kls.v3i6.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Rashed A.N., Afifi F.U., Disi A.M. Simple Evaluation of the Wound Healing Activity of a Crude Extract of Portulaca Oleracea L. (Growing in Jordan) in Mus Musculus JVI-1. J. Ethnopharmacol. 2003;88:131–136. doi: 10.1016/S0378-8741(03)00194-6. [DOI] [PubMed] [Google Scholar]
- 133.Ren J., Yang M., Xu F., Chen J., Ma S. Acceleration of Wound Healing Activity with Syringic Acid in Streptozotocin Induced Diabetic Rats. Life Sci. 2019;233:116728. doi: 10.1016/j.lfs.2019.116728. [DOI] [PubMed] [Google Scholar]
- 134.Scrima M., Melito C., Merola F., Iorio A., Vito N., Giori A.M., Ferravante A. Evaluation of Wound Healing Activity of Salvia Haenkei Hydroalcoholic Aerial Part Extract on in Vitro and in Vivo Experimental Models. Clin. Cosmet. Investig. Dermatol. 2020;13:627–637. doi: 10.2147/CCID.S224418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sh Ahmed A., Taher M., Mandal U.K., Jaffri J.M., Susanti D., Mahmood S., Zakaria Z.A. Pharmacological Properties of Centella Asiatica Hydrogel in Accelerating Wound Healing in Rabbits. BMC Complement. Altern. Med. 2019;19:1–7. doi: 10.1186/s12906-019-2625-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Shafeie N., Naini A.T., Jahromi H.K. Comparison of Different Concentrations of Calendula officinalis Gel on Cutaneous Wound Healing. Biomed. Pharmacol. J. 2015;8:979–992. doi: 10.13005/bpj/850. [DOI] [Google Scholar]
- 137.Shukla A., Rasik A.M., Patnaik G.K. Depletion of Reduced Glutathione, Ascorbic Acid, Vitamin E and Antioxidant Defence Enzymes in a Healing Cutaneous Wound. Free Radic. Res. 1997;26:93–101. doi: 10.3109/10715769709097788. [DOI] [PubMed] [Google Scholar]
- 138.Ram M., Singh V., Kumawat S., Kant V., Tandan S.K., Kumar D. Bilirubin Modulated Cytokines, Growth Factors and Angiogenesis to Improve Cutaneous Wound Healing Process in Diabetic Rats. Int. Immunopharmacol. 2016;30:137–149. doi: 10.1016/j.intimp.2015.11.037. [DOI] [PubMed] [Google Scholar]
- 139.Singh S.D.J., Krishna V., Mankani K.L., Manjunatha B.K., Vidya S.M., Manohara Y.N. Wound Healing Activity of the Leaf Extracts and Deoxyelephantopin Isolated from Elephantopus Scaber Linn. Indian J. Pharmacol. 2005;37:238–242. [Google Scholar]
- 140.Siriwattanasatorn M., Itharat A., Thongdeeying P., Ooraikul B. In Vitro Wound Healing Activities of Three Most Commonly Used Thai Medicinal Plants and Their Three Markers. Evid.-Based Complement. Altern. Med. 2020;2020:6795383. doi: 10.1155/2020/6795383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Somboonwong J., Kankaisre M., Tantisira B., Tantisira M.H. Wound Healing Activities of Different Extracts of Centella Asiatica in Incision and Burn Wound Models: An Experimental Animal Study. BMC Complement. Altern. Med. 2012;12:103. doi: 10.1186/1472-6882-12-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sui H., Wang F., Weng Z., Song H., Fang Y., Tang X., Shen X. A Wheat Germ-Derived Peptide YDWPGGRN Facilitates Skin Wound-Healing Processes. Biochem. Biophys. Res. Commun. 2020;524:943–950. doi: 10.1016/j.bbrc.2020.01.162. [DOI] [PubMed] [Google Scholar]
- 143.Süntar I., Küpeli Akkol E., Keles H., Yesilada E., Sarker S.D. Exploration of the Wound Healing Potential of Helichrysum Graveolens (Bieb.) Sweet: Isolation of Apigenin as an Active Component. J. Ethnopharmacol. 2013;149:103–110. doi: 10.1016/j.jep.2013.06.006. [DOI] [PubMed] [Google Scholar]
- 144.Tai A., Sawano T., Yazama F., Ito H. Evaluation of Antioxidant Activity of Vanillin by Using Multiple Antioxidant Assays. Biochim. Biophys. Acta Gen. Subj. 2011;1810:170–177. doi: 10.1016/j.bbagen.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 145.Tang T., Yin L., Yang J., Shan G. Emodin, an Anthraquinone Derivative from Rheum Officinale Baill, Enhances Cutaneous Wound Healing in Rats. Eur. J. Pharmacol. 2007;567:177–185. doi: 10.1016/j.ejphar.2007.02.033. [DOI] [PubMed] [Google Scholar]
- 146.Thaloor D., Miller K.J., Gephart J., Mitchell P.O., Pavlath G.K. Systemic Administration of the NF-ΚB Inhibitor Curcumin Stimulates Muscle Regeneration after Traumatic Injury. Am. J. Physiol. Cell Physiol. 1999;277:C320–C329. doi: 10.1152/ajpcell.1999.277.2.C320. [DOI] [PubMed] [Google Scholar]
- 147.Thangapazham R.L., Sharad S., Maheshwari R.K. Phytochemicals in Wound Healing. Adv. Wound Care. 2016;5:230–241. doi: 10.1089/wound.2013.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Tsoutsos D., Kakagia D., Tamparopoulos K. The Efficacy of Helix Aspersa Müller Extract in the Healing of Partial Thickness Burns: A Novel Treatment for Open Burn Management Protocols. J. Dermatolog. Treat. 2009;20:219–222. doi: 10.1080/09546630802582037. [DOI] [PubMed] [Google Scholar]
- 149.Zhou X., Ruan Q., Ye Z., Chu Z., Xi M., Li M., Hu W., Guo X., Yao P., Xie W. Resveratrol Accelerates Wound Healing by Attenuating Oxidative Stress-Induced Impairment of Cell Proliferation and Migration. Burns. 2021;47:133–139. doi: 10.1016/j.burns.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 150.Umasankar K., Nambikkairaj B., Manley Backyavathy D. Effect of Topical Treatment of Rosmarinus officinalis Essential Oil on Wound Healing in Streptozotocin Induced Diabetic Rats. Nat. Environ. Pollut. Technol. 2012;11:607–611. [Google Scholar]
- 151.Vidya S.M., Krishna V., Manjunatha B.K., Bharath B.R., Rajesh K.P., Manjunatha H., Mankani K.L. Wound Healing Phytoconstituents from Seed Kernel of Entada Pursaetha DC. and Their Molecular Docking Studies with Glycogen Synthase Kinase 3-β. Med. Chem. Res. 2012;21:3195–3203. doi: 10.1007/s00044-011-9860-5. [DOI] [Google Scholar]
- 152.Wahedi H.M., Park Y.U., Moon E.Y., Kim S.Y. Juglone Ameliorates Skin Wound Healing by Promoting Skin Cell Migration through Rac1/Cdc42/PAK Pathway. Wound Repair Regen. 2016;24:786–794. doi: 10.1111/wrr.12452. [DOI] [PubMed] [Google Scholar]
- 153.Wang W., Meng H. Cytotoxic, Anti-Inflammatory and Hemostatic Spirostane-Steroidal Saponins from the Ethanol Extract of the Roots of Bletilla Striata. Fitoterapia. 2015;101:12–18. doi: 10.1016/j.fitote.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 154.Wang L., He T., Fu A., Mao Z., Yi L., Tang S., Yang J. Hesperidin Enhances Angiogenesis via Modulating Expression of Growth and Inflammatory Factor in Diabetic Foot Ulcer in Rats. Eur. J. Inflamm. 2018;16:2058739218775255. doi: 10.1177/2058739218775255. [DOI] [Google Scholar]
- 155.Yang W.T., Ke C.Y., Wu W.T., Tseng Y.H., Lee R.P. Antimicrobial and Anti-Inflammatory Potential of Angelica Dahurica and Rheum Officinale Extract Accelerates Wound Healing in Staphylococcus Aureus-Infected Wounds. Sci. Rep. 2020;10:5596. doi: 10.1038/s41598-020-62581-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Yen J.H., Chio W.T., Chuang C.J., Yang H.L., Huang S.T. Improved Wound Healing by Naringin Associated with MMP and the VEGF Pathway. Molecules. 2022;27:1695. doi: 10.3390/molecules27051695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yu M.H., Choi J.H., Chae I.G., Im H.G., Yang S.A., More K., Lee I.S., Lee J. Suppression of LPS-Induced Inflammatory Activities by Rosmarinus officinalis L. Food Chem. 2013;136:1047–1054. doi: 10.1016/j.foodchem.2012.08.085. [DOI] [PubMed] [Google Scholar]
- 158.Zangeneh A., Pooyanmehr M., Zangeneh M.M., Moradi R., Rasad R., Kazemi N. Therapeutic Effects of Glycyrrhiza Glabra Aqueous Extract Ointment on Cutaneous Wound Healing in Sprague Dawley Male Rats. Comp. Clin. Path. 2019;28:1507–1514. doi: 10.1007/s00580-019-03007-9. [DOI] [Google Scholar]
- 159.Zeka K., Ruparelia K.C., Sansone C., Macchiarelli G., Continenza M.A., Arroo R.R.J. New Hydrogels Enriched with Antioxidants from Saffron Crocus Can Find Applications in Wound Treatment and/or Beautification. Skin Pharmacol. Physiol. 2018;31:95–98. doi: 10.1159/000486135. [DOI] [PubMed] [Google Scholar]
- 160.Orhan I.E., Akkol E.K., Suntar I., Yesilada E. Assessment of Anticholinesterase and Antioxidant Properties of the Extracts and (+)-Catechin Obtained from Arceuthobium oxycedri (D.C.) M. Bieb (Dwarf Mistletoe) South African J. Bot. 2019;120:309–312. doi: 10.1016/j.sajb.2018.09.023. [DOI] [Google Scholar]
- 161.Zeng Z., Zhu B.H. Arnebin-1 Promotes the Angiogenesis of Human Umbilical Vein Endothelial Cells and Accelerates the Wound Healing Process in Diabetic Rats. J. Ethnopharmacol. 2014;154:653–662. doi: 10.1016/j.jep.2014.04.038. [DOI] [PubMed] [Google Scholar]
- 162.Zeng Z., Huang W.D., Gao Q., Su M.L., Yang Y.F., Liu Z.C., Zhu B.H. Arnebin-1 Promotes Angiogenesis by Inducing ENOS, VEGF and HIF-1α Expression through the PI3K-Dependent Pathway. Int. J. Mol. Med. 2015;36:685–697. doi: 10.3892/ijmm.2015.2292. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 163.Zhao B., Zhang X., Han W., Cheng J., Qin Y. Wound Healing Effect of an Astragalus Membranaceus Polysaccharide and Its Mechanism. Mol. Med. Rep. 2017;15:4077–4083. doi: 10.3892/mmr.2017.6488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zhao Y., Wang Q., Yan S., Zhou J., Huang L., Zhu H., Ye F., Zhang Y., Chen L., Chen L., et al. Bletilla Striata Polysaccharide Promotes Diabetic Wound Healing Through Inhibition of the NLRP3 Inflammasome. Front. Pharmacol. 2021;12:659215. doi: 10.3389/fphar.2021.659215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhi Y., Wang H., Huang B., Yan G., Yan L.Z., Zhang W., Zhang J. Panax Notoginseng Saponins Suppresses TRPM7 via the PI3K/AKT Pathway to Inhibit Hypertrophic Scar Formation in Vitro. Burns. 2021;47:894–905. doi: 10.1016/j.burns.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 166.Zhou G., Ruhan A., Ge H., Wang L., Liu M., Wang B., Su H., Yan M., Xi Y., Fan Y. Research on a Novel Poly (Vinyl Alcohol)/Lysine/Vanillin Wound Dressing: Biocompatibility, Bioactivity and Antimicrobial Activity. Burns. 2014;40:1668–1678. doi: 10.1016/j.burns.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 167.Abu-Al-Basal M.A. Healing Potential of Rosmarinus officinalis L. on Full-Thickness Excision Cutaneous Wounds in Alloxan-Induced-Diabetic BALB/c Mice. J. Ethnopharmacol. 2010;131:443–450. doi: 10.1016/j.jep.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 168.Afshar M., Ravarian B., Zardast M., Moallem S.A., Fard M.H., Valavi M. Evaluation of Cutaneous Wound Healing Activity of Malva Sylvestris Aqueous Extract in BALB/c Mice. Iran. J. Basic Med. Sci. 2015;18:616–622. [PMC free article] [PubMed] [Google Scholar]
- 169.Deng Z.H., Yin J., Luo W., Kotian R.N., Gao S., Yi Z.Q., Xiao W.F., Li W.P., Li Y.S. The Effect of Earthworm Extract on Promoting Skin Wound Healing. Biosci. Rep. 2018;38:1–11. doi: 10.1042/BSR20171366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Diao H., Li X., Chen J., Luo Y., Chen X., Dong L., Wang C., Zhang C., Zhang J. Bletilla Striata Polysaccharide Stimulates Inducible Nitric Oxide Synthase and Proinflammatory Cytokine Expression in Macrophages. J. Biosci. Bioeng. 2008;105:85–89. doi: 10.1263/jbb.105.85. [DOI] [PubMed] [Google Scholar]
- 171.Reinke J.M., Sorg H. Wound Repair and Regeneration. Eur. Surg. Res. 2012;49:35–43. doi: 10.1159/000339613. [DOI] [PubMed] [Google Scholar]
- 172.Landén N.X., Li D., Ståhle M. Transition from Inflammation to Proliferation: A Critical Step during Wound Healing. Cell. Mol. Life Sci. 2016;73:3861–3885. doi: 10.1007/s00018-016-2268-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Cañedo-Dorantes L., Cañedo-Ayala M. Skin Acute Wound Healing: A Comprehensive Review. Int. J. Inflam. 2019;2019:3706315. doi: 10.1155/2019/3706315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Arribas-López E., Zand N., Ojo O., Snowden M.J., Kochhar T. A Systematic Review of the Effect of Centella Asiatica on Wound Healing. Int. J. Environ. Res. Public Health. 2022;19:3266. doi: 10.3390/ijerph19063266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Babu K.A., Sivakrishnan S., Jasemine S. Evaluation of in Vivo Wound Healing Activity of Ursolic Acid Rich Chloroform Extract of Hedyotis Herbacea Linn Ointment. J. Pharm. Res. Int. 2021;33:246–255. doi: 10.9734/jpri/2021/v33i39A32167. [DOI] [Google Scholar]
- 176.Beserra F.P., Vieira A.J., Gushiken L.F.S., de Souza E.O., Hussni M.F., Hussni C.A., Nóbrega R.H., Martinez E.R.M., Jackson C.J., de Azevedo Maia G.L., et al. Lupeol, a Dietary Triterpene, Enhances Wound Healing in Streptozotocin-Induced Hyperglycemic Rats with Modulatory Effects on Inflammation, Oxidative Stress, and Angiogenesis. Oxid. Med. Cell. Longev. 2019;2019:3182627. doi: 10.1155/2019/3182627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.de Moura Sperotto N.D., Steffens L., Veríssimo R.M., Henn J.G., Péres V.F., Vianna P., Chies J.A.B., Roehe A., Saffi J., Moura D.J. Wound Healing and Anti-Inflammatory Activities Induced by a Plantago Australis Hydroethanolic Extract Standardized in Verbascoside. J. Ethnopharmacol. 2018;225:178–188. doi: 10.1016/j.jep.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 178.Wang T., Li Q., Bi K. Bioactive Flavonoids in Medicinal Plants: Structure, Activity and Biological Fate. Asian J. Pharm. Sci. 2018;13:12–23. doi: 10.1016/j.ajps.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Wang S.-J., Tong Y., Lu S., Yang R., Liao X., Xu Y.-F., Li X. Anti-Inflammatory Activity of Myricetin Isolated from Myrica Rubra Sieb. et Zucc. Leaves. Planta Med. 2010;76:1492–1496. doi: 10.1055/s-0030-1249780. [DOI] [PubMed] [Google Scholar]
- 180.Rehman M.U., Rather I.A. Myricetin Abrogates Cisplatin-Induced Oxidative Stress, Inflammatory Response, and Goblet Cell Disintegration in Colon of Wistar Rats. Plants. 2019;9:28. doi: 10.3390/plants9010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Semwal D.K., Semwal R.B., Combrinck S., Viljoen A. Myricetin: A Dietary Molecule with Diverse Biological Activities. Nutrients. 2016;8:90. doi: 10.3390/nu8020090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hong C., Xie Y., Yao Y., Li G., Yuan X., Shen H. A Novel Strategy for Pharmaceutical Cocrystal Generation without Knowledge of Stoichiometric Ratio: Myricetin Cocrystals and a Ternary Phase Diagram. Pharm. Res. 2015;32:47–60. doi: 10.1007/s11095-014-1443-y. [DOI] [PubMed] [Google Scholar]
- 183.Dang Y., Lin G., Xie Y., Duan J., Ma P., Li G., Ji G. Quantitative Determination of Myricetin in Rat Plasma by Ultra Performance Liquid Chromatography Tandem Mass Spectrometry and Its Absolute Bioavailability. Drug Res. (Stuttg). 2013;64:516–522. doi: 10.1055/s-0033-1363220. [DOI] [PubMed] [Google Scholar]
- 184.Bhalla T.N., Saxena R.C., Nigam S.K., Misra G., Bhargava K.P. Calophyllolide—A New Non-Steroidal Anti-Inflammatory Agent. Indian J. Med. Res. 1980;72:762–765. [PubMed] [Google Scholar]
- 185.Yimdjo M.C., Azebaze A.G., Nkengfack A.E., Meyer A.M., Bodo B., Fomum Z.T. Antimicrobial and Cytotoxic Agents from Calophyllum Inophyllum. Phytochemistry. 2004;65:2789–2795. doi: 10.1016/j.phytochem.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 186.Arora R.B., Mathur C.N., Seth S.D.S. Calophyllolide, a Complex Coumarin Anticoagulant from Calophyllum Inophyllum Linn. J. Pharm. Pharmacol. 2011;14:534–535. doi: 10.1111/j.2042-7158.1962.tb11133.x. [DOI] [PubMed] [Google Scholar]
- 187.Schapoval E.E., Winter de Vargas M.R., Chaves C.G., Bridi R., Zuanazzi J.A., Henriques A.T. Antiinflammatory and Antinociceptive Activities of Extracts and Isolated Compounds from Stachytarpheta Cayennensis. J. Ethnopharmacol. 1998;60:53–59. doi: 10.1016/S0378-8741(97)00136-0. [DOI] [PubMed] [Google Scholar]
- 188.Lee K.-W., Kim H.J., Lee Y.S., Park H.-J., Choi J.-W., Ha J., Lee K.-T. Acteoside Inhibits Human Promyelocytic HL-60 Leukemia Cell Proliferation via Inducing Cell Cycle Arrest at G0/G1 Phase and Differentiation into Monocyte. Carcinogenesis. 2007;28:1928–1936. doi: 10.1093/carcin/bgm126. [DOI] [PubMed] [Google Scholar]
- 189.Hausmann M., Obermeier F., Paper D.H., Balan K., Dunger N., Menzel K., Falk W., Schoelmerich J., Herfarth H., Rogler G. In Vivo Treatment with the Herbal Phenylethanoid Acteoside Ameliorates Intestinal Inflammation in Dextran Sulphate Sodium-Induced Colitis. Clin. Exp. Immunol. 2007;148:373–381. doi: 10.1111/j.1365-2249.2007.03350.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Sudhahar V., Kumar S.A., Varalakshmi P. Role of Lupeol and Lupeol Linoleate on Lipemic–Oxidative Stress in Experimental Hypercholesterolemia. Life Sci. 2006;78:1329–1335. doi: 10.1016/j.lfs.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 191.Alqahtani A., Hamid K., Kam A., Wong K.H., Abdelhak Z., Razmovski-Naumovski V., Chan K., Li K.M., Groundwater P.W., Li G.Q. The Pentacyclic Triterpenoids in Herbal Medicines and Their Pharmacological Activities in Diabetes and Diabetic Complications. Curr. Med. Chem. 2013;20:908–931. [PubMed] [Google Scholar]
- 192.Badshah H., Ali T., Rehman S., Amin F., Ullah F., Kim T.H., Kim M.O. Protective Effect of Lupeol Against Lipopolysaccharide-Induced Neuroinflammation via the P38/c-Jun N-Terminal Kinase Pathway in the Adult Mouse Brain. J. Neuroimmune Pharmacol. 2016;11:48–60. doi: 10.1007/s11481-015-9623-z. [DOI] [PubMed] [Google Scholar]
- 193.Stocker R., Yamamoto Y., McDonagh A.F., Glazer A.N., Ames B.N. Bilirubin Is an Antioxidant of Possible Physiological Importance. Science. 1987;235:1043–1046. doi: 10.1126/science.3029864. [DOI] [PubMed] [Google Scholar]
- 194.Rasul A., Millimouno F.M., Ali Eltayb W., Ali M., Li J., Li X. Pinocembrin: A Novel Natural Compound with Versatile Pharmacological and Biological Activities. BioMed Res. Int. 2013;2013:379850. doi: 10.1155/2013/379850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Drewes S.E., van Vuuren S.F. Antimicrobial Acylphloroglucinols and Dibenzyloxy Flavonoids from Flowers of Helichrysum Gymnocomum. Phytochemistry. 2008;69:1745–1749. doi: 10.1016/j.phytochem.2008.02.022. [DOI] [PubMed] [Google Scholar]
- 196.Sala A., Recio M.C., Schinella G.R., Máñez S., Giner R.M., Cerdá-Nicolás M., Ríos J.L. Assessment of the Anti-Inflammatory Activity and Free Radical Scavenger Activity of Tiliroside. Eur. J. Pharmacol. 2003;461:53–61. doi: 10.1016/S0014-2999(02)02953-9. [DOI] [PubMed] [Google Scholar]
- 197.Amri B., Martino E., Vitulo F., Corana F., Kaâb L.B.-B., Rui M., Rossi D., Mori M., Rossi S., Collina S. Marrubium Vulgare L. Leave Extract: Phytochemical Composition, Antioxidant and Wound Healing Properties. Molecules. 2017;22:1851. doi: 10.3390/molecules22111851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Schwentker A., Vodovotz Y., Weller R., Billiar T.R. Nitric Oxide and Wound Repair: Role of Cytokines? Nitric Oxide. 2002;7:1–10. doi: 10.1016/S1089-8603(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 199.EDWARDS J. In Vitro Inhibition of Human Neutrophil Elastase by Oleic Acid Albumin Formulations from Derivatized Cotton Wound Dressings. Int. J. Pharm. 2004;284:1–12. doi: 10.1016/j.ijpharm.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 200.Baek S., Park H., Kim M., Lee D. Preparation of PCL/(+)-Catechin/Gelatin Film for Wound Healing Using Air-Jet Spinning. Appl. Surf. Sci. 2020;509:145033. doi: 10.1016/j.apsusc.2019.145033. [DOI] [Google Scholar]
- 201.Al-Roujayee A.S. Naringenin Improves the Healing Process of Thermally-Induced Skin Damage in Rats. J. Int. Med. Res. 2017;45:570–582. doi: 10.1177/0300060517692483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Bonté F., Noel-Hudson M.-S., Wepierre J., Meybeck A. Protective Effect of Curcuminoids on Epidermal Skin Cells under Free Oxygen Radical Stress. Planta Med. 1997;63:265–266. doi: 10.1055/s-2006-957669. [DOI] [PubMed] [Google Scholar]
- 203.Chainani-Wu N. Safety and Anti-Inflammatory Activity of Curcumin: A Component of Tumeric (Curcuma longa) J. Altern. Complement. Med. 2003;9:161–168. doi: 10.1089/107555303321223035. [DOI] [PubMed] [Google Scholar]
- 204.Joe B., Vijaykumar M., LOKESH B.R. Biological Properties of Curcumin-Cellular and Molecular Mechanisms of Action. Crit. Rev. Food Sci. Nutr. 2004;44:97–111. doi: 10.1080/10408690490424702. [DOI] [PubMed] [Google Scholar]
- 205.Anand P., Kunnumakkara A.B., Newman R.A., Aggarwal B.B. Bioavailability of Curcumin: Problems and Promises. Mol. Pharm. 2007;4:807–818. doi: 10.1021/mp700113r. [DOI] [PubMed] [Google Scholar]
- 206.Aceituno-Medina M., Mendoza S., Rodríguez B.A., Lagaron J.M., López-Rubio A. Improved Antioxidant Capacity of Quercetin and Ferulic Acid during In-Vitro Digestion through Encapsulation within Food-Grade Electrospun Fibers. J. Funct. Foods. 2015;12:332–341. doi: 10.1016/j.jff.2014.11.028. [DOI] [Google Scholar]
- 207.Bains R., Bains V. The Antioxidant Master Glutathione and Periodontal Health. Dent. Res. J. 2015;12:389. doi: 10.4103/1735-3327.166169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Gugler R., Leschik M., Dengler H.J. Disposition of Quercetin in Man after Single Oral and Intravenous Doses. Eur. J. Clin. Pharmacol. 1975;9:229–234. doi: 10.1007/BF00614022. [DOI] [PubMed] [Google Scholar]
- 209.Caro A.A., Davis A., Fobare S., Horan N., Ryan C., Schwab C. Antioxidant and Pro-Oxidant Mechanisms of (+) Catechin in Microsomal CYP2E1-Dependent Oxidative Stress. Toxicol. Vitr. 2019;54:1–9. doi: 10.1016/j.tiv.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Ye J.-H.H., Augustin M.A. Nano- and Micro-Particles for Delivery of Catechins: Physical and Biological Performance. Crit. Rev. Food Sci. Nutr. 2019;59:1563–1579. doi: 10.1080/10408398.2017.1422110. [DOI] [PubMed] [Google Scholar]
- 211.Ng T.B., He J.S., Niu S.M., Pi Z.F., Shao W., Liu F., Zhao L. A Gallic Acid Derivative and Polysaccharides with Antioxidative Activity from Rose (Rosa Rugosa ) Flowers. J. Pharm. Pharmacol. 2010;56:537–545. doi: 10.1211/0022357022944. [DOI] [PubMed] [Google Scholar]
- 212.Ma J., Luo X.-D., Protiva P., Yang H., Ma C., Basile M.J., Weinstein I.B., Kennelly E.J. Bioactive Novel Polyphenols from the Fruit of Manilkara Zapota (Sapodilla) J. Nat. Prod. 2003;66:983–986. doi: 10.1021/np020576x. [DOI] [PubMed] [Google Scholar]
- 213.Mansouri M.T., Soltani M., Naghizadeh B., Farbood Y., Mashak A., Sarkaki A. A Possible Mechanism for the Anxiolytic-like Effect of Gallic Acid in the Rat Elevated plus Maze. Pharmacol. Biochem. Behav. 2014;117:40–46. doi: 10.1016/j.pbb.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 214.Burns J., Yokota T., Ashihara H., Lean M.E.J., Crozier A. Plant Foods and Herbal Sources of Resveratrol. J. Agric. Food Chem. 2002;50:3337–3340. doi: 10.1021/jf0112973. [DOI] [PubMed] [Google Scholar]
- 215.Marques F.Z., Markus M.A., Morris B.J. Resveratrol: Cellular Actions of a Potent Natural Chemical That Confers a Diversity of Health Benefits. Int. J. Biochem. Cell Biol. 2009;41:2125–2128. doi: 10.1016/j.biocel.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 216.Malhotra A., Bath S., Elbarbry F. An Organ System Approach to Explore the Antioxidative, Anti-Inflammatory, and Cytoprotective Actions of Resveratrol. Oxid. Med. Cell. Longev. 2015;2015:803971. doi: 10.1155/2015/803971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Means J., Gerdes B., Koulen P. Distinct Mechanisms Underlying Resveratrol-Mediated Protection from Types of Cellular Stress in C6 Glioma Cells. Int. J. Mol. Sci. 2017;18:1521. doi: 10.3390/ijms18071521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bilgic T. Partial Effect of Resveratrol on Wound Healing: Study on Wistar Albino Rats. Eurasian J. Med. Investig. 2022;5:460–468. doi: 10.14744/ejmi.2021.97868. [DOI] [Google Scholar]
- 219.Gattuso G., Barreca D., Gargiulli C., Leuzzi U., Caristi C. Flavonoid Composition of Citrus Juices. Molecules. 2007;12:1641–1673. doi: 10.3390/12081641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Patel K., Singh G.K., Patel D.K. A Review on Pharmacological and Analytical Aspects of Naringenin. Chin. J. Integr. Med. 2018;24:551–560. doi: 10.1007/s11655-014-1960-x. [DOI] [PubMed] [Google Scholar]
- 221.Khameneh B., Iranshahy M., Soheili V., Fazly Bazzaz B.S. Review on Plant Antimicrobials: A Mechanistic Viewpoint. Antimicrob. Resist. Infect. Control. 2019;8:118. doi: 10.1186/s13756-019-0559-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yanagibayashi S., Kishimoto S., Ishihara M., Murakami K., Aoki H., Takikawa M., Fujita M., Sekido M., Kiyosawa T. Novel Hydrocolloid-Sheet as Wound Dressing to Stimulate Healing-Impaired Wound Healing in Diabetic Db/Db Mice. Biomed. Mater. Eng. 2012;22:301–310. doi: 10.3233/BME-2012-0720. [DOI] [PubMed] [Google Scholar]
- 223.Martinotti S., Laforenza U., Patrone M., Moccia F., Ranzato E. Honey-Mediated Wound Healing: H2O2 Entry through AQP3 Determines Extracellular Ca2+ Influx. Int. J. Mol. Sci. 2019;20:764. doi: 10.3390/ijms20030764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Ueno H., Mori T., Fujinaga T. Topical Formulations and Wound Healing Applications of Chitosan. Adv. Drug Deliv. Rev. 2001;52:105–115. doi: 10.1016/S0169-409X(01)00189-2. [DOI] [PubMed] [Google Scholar]
- 225.Rinaudo M. Chitin and Chitosan: Properties and Applications. Prog. Polym. Sci. 2006;31:603–632. doi: 10.1016/j.progpolymsci.2006.06.001. [DOI] [Google Scholar]
- 226.Bhattarai N., Gunn J., Zhang M. Chitosan-Based Hydrogels for Controlled, Localized Drug Delivery. Adv. Drug Deliv. Rev. 2010;62:83–99. doi: 10.1016/j.addr.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 227.Chung Y.-C., Chen C.-Y. Antibacterial Characteristics and Activity of Acid-Soluble Chitosan. Bioresour. Technol. 2008;99:2806–2814. doi: 10.1016/j.biortech.2007.06.044. [DOI] [PubMed] [Google Scholar]
- 228.Song E.-H., Shang J., Ratner D.M. Polymer Science: A Comprehensive Reference. Elsevier; Amsterdam, The Netherlands: 2012. Polysaccharides; pp. 137–155. [Google Scholar]
- 229.LogithKumar R., KeshavNarayan A., Dhivya S., Chawla A., Saravanan S., Selvamurugan N. A Review of Chitosan and Its Derivatives in Bone Tissue Engineering. Carbohydr. Polym. 2016;151:172–188. doi: 10.1016/j.carbpol.2016.05.049. [DOI] [PubMed] [Google Scholar]
- 230.Khoshfetrat A.B., Khanmohammadi M., Sakai S., Taya M. Enzymatically-Gellable Galactosylated Chitosan: Hydrogel Characteristics and Hepatic Cell Behavior. Int. J. Biol. Macromol. 2016;92:892–899. doi: 10.1016/j.ijbiomac.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 231.Mohamed R.R., Elella M.H.A.A., Sabaa M.W. Cytotoxicity and Metal Ions Removal Using Antibacterial Biodegradable Hydrogels Based on N-Quaternized Chitosan/Poly(Acrylic Acid) Int. J. Biol. Macromol. 2017;98:302–313. doi: 10.1016/j.ijbiomac.2017.01.107. [DOI] [PubMed] [Google Scholar]
- 232.Bagher Z., Ehterami A., Safdel M.H., Khastar H., Semiari H., Asefnejad A., Davachi S.M., Mirzaii M., Salehi M. Wound Healing with Alginate/Chitosan Hydrogel Containing Hesperidin in Rat Model. J. Drug Deliv. Sci. Technol. 2020;55:101379. doi: 10.1016/j.jddst.2019.101379. [DOI] [Google Scholar]
- 233.Verma J., Kanoujia J., Parashar P., Tripathi C.B., Saraf S.A. Wound Healing Applications of Sericin/Chitosan-Capped Silver Nanoparticles Incorporated Hydrogel. Drug Deliv. Transl. Res. 2017;7:77–88. doi: 10.1007/s13346-016-0322-y. [DOI] [PubMed] [Google Scholar]
- 234.Caetano G.F., Frade M.A.C., Andrade T.A.M., Leite M.N., Bueno C.Z., Moraes Â.M., Ribeiro-Paes J.T. Chitosan-Alginate Membranes Accelerate Wound Healing. J. Biomed. Mater. Res. Part B Appl. Biomater. 2015;103:1013–1022. doi: 10.1002/jbm.b.33277. [DOI] [PubMed] [Google Scholar]
- 235.Bonferoni M.C., Sandri G., Dellera E., Rossi S., Ferrari F., Mori M., Caramella C. Ionic Polymeric Micelles Based on Chitosan and Fatty Acids and Intended for Wound Healing. Comparison of Linoleic and Oleic Acid. Eur. J. Pharm. Biopharm. 2014;87:101–106. doi: 10.1016/j.ejpb.2013.12.018. [DOI] [PubMed] [Google Scholar]
- 236.Zubair R., Aziz N. As Smooth as Honey—The Historical Use of Honey as Topical Medication. JAMA Dermatology. 2015;151:1102. doi: 10.1001/jamadermatol.2015.1764. [DOI] [PubMed] [Google Scholar]
- 237.Kumar P., Kothari V., editors. Wound Healing Research. Springer; Singapore: 2021. [Google Scholar]
- 238.Christy E.M.-L., Clarke A.M., Ndip R.N. An Overview of Honey: Therapeutic Properties and Contribution in Nutrition and Human Health. African J. Microbiol. Res. 2011;5:844–852. [Google Scholar]
- 239.Mandal M.D., Mandal S. Honey: Its Medicinal Property and Antibacterial Activity. Asian Pac. J. Trop. Biomed. 2011;1:154–160. doi: 10.1016/S2221-1691(11)60016-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Bosio K., Avanzini C., D’avolio A., Ozino O., Savoia D. In Vitro Activity of Propolis against Streptococcus Pyogenes. Lett. Appl. Microbiol. 2000;31:174–177. doi: 10.1046/j.1365-2672.2000.00785.x. [DOI] [PubMed] [Google Scholar]
- 241.Kuropatnicki A.K., Szliszka E., Krol W. Historical Aspects of Propolis Research in Modern Times. Evid.-Based Complement. Altern. Med. 2013;2013:964149. doi: 10.1155/2013/964149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Afrouzan H., Tahghighi A., Zakeri S., Es-haghi A. Chemical Composition and Antimicrobial Activities of Iranian Propolis. Iran. Biomed. J. 2018;22:50–65. doi: 10.22034/ibj.22.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Huang S., Zhang C.-P., Wang K., Li G., Hu F.-L. Recent Advances in the Chemical Composition of Propolis. Molecules. 2014;19:19610–19632. doi: 10.3390/molecules191219610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Orhan H., Marol S., Hepşen İ.F., Şahin G. Effects of Some Probable Antioxidants on Selenite-Induced Cataract Formation and Oxidative Stress-Related Parameters in Rats. Toxicology. 1999;139:219–232. doi: 10.1016/S0300-483X(99)00128-6. [DOI] [PubMed] [Google Scholar]
- 245.Toreti V.C., Sato H.H., Pastore G.M., Park Y.K. Recent Progress of Propolis for Its Biological and Chemical Compositions and Its Botanical Origin. Evid.-Based Complement. Altern. Med. 2013;2013:697390. doi: 10.1155/2013/697390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Uzel A., Sorkun K.K., Önçaǧ Ö., Çoǧulu D., Gençay Ö., Salih B. Chemical Compositions and Antimicrobial Activities of Four Different Anatolian Propolis Samples. Microbiol. Res. 2005;160:189–195. doi: 10.1016/j.micres.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 247.Czyżewska U., Konończuk J., Teul J., Drągowski P., Pawlak-Morka R., Surażyński A., Miltyk W. Verification of Chemical Composition of Commercially Available Propolis Extracts by Gas Chromatography–Mass Spectrometry Analysis. J. Med. Food. 2015;18:584–591. doi: 10.1089/jmf.2014.0069. [DOI] [PubMed] [Google Scholar]
- 248.Fujisawa H., Watanabe K., SUMA K., Origuchi K., Matsufuji H., SEKI T., ARIGA T. Antibacterial Potential of Garlic-Derived Allicin and Its Cancellation by Sulfhydryl Compounds. Biosci. Biotechnol. Biochem. 2009;73:1948–1955. doi: 10.1271/bbb.90096. [DOI] [PubMed] [Google Scholar]
- 249.Leng B.-F., Qiu J.-Z., Dai X.-H., Dong J., Wang J.-F., Luo M.-J., Li H.-E., Niu X.-D., Zhang Y., Ai Y.-X., et al. Allicin Reduces the Production of α-Toxin by Staphylococcus Aureus. Molecules. 2011;16:7958–7968. doi: 10.3390/molecules16097958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Arzanlou M., Bohlooli S. Inhibition of Streptolysin O by Allicin—An Active Component of Garlic. J. Med. Microbiol. 2010;59:1044–1049. doi: 10.1099/jmm.0.019539-0. [DOI] [PubMed] [Google Scholar]
- 251.Alhashim M., Lombardo J. Mechanism of Action of Topical Garlic on Wound Healing. Dermatologic Surg. 2018;44:630–634. doi: 10.1097/DSS.0000000000001382. [DOI] [PubMed] [Google Scholar]
- 252.Trusheva B., Todorov I., Ninova M., Najdenski H., Daneshmand A., Bankova V. Antibacterial mono- and sesquiterpene esters of benzoic acids from Iranian propolis. Chem. Cent. J. 2010;4:8. doi: 10.1186/1752-153X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.SUGUNA L., CHANDRAKASAN G., JOSEPH K.T. Influence of Honey on Collagen Metabolism during Wound Healing in Rats. J. Clin. Biochem. Nutr. 1992;13:7–12. doi: 10.3164/jcbn.13.7. [DOI] [Google Scholar]
- 254.Hormozi M., Assaei R., Boroujeni M.B. The Effect of Aloe Vera on the Expression of Wound Healing Factors (TGFβ1 and BFGF) in Mouse Embryonic Fibroblast Cell: In Vitro Study. Biomed. Pharmacother. 2017;88:610–616. doi: 10.1016/j.biopha.2017.01.095. [DOI] [PubMed] [Google Scholar]
- 255.Seo G., Hyun C., Choi S., Kim Y.M., Cho M. The Wound Healing Effect of Four Types of Beta-Glucan. Appl. Biol. Chem. 2019;62:20. doi: 10.1186/s13765-019-0428-2. [DOI] [Google Scholar]
- 256.Mahibalan S., Stephen M., Nethran R.T., Khan R., Begum S. Dermal Wound Healing Potency of Single Alkaloid (Betaine) versus Standardized Crude Alkaloid Enriched-Ointment of Evolvulus Alsinoides. Pharm. Biol. 2016;54:2851–2856. doi: 10.1080/13880209.2016.1185636. [DOI] [PubMed] [Google Scholar]
- 257.Agra L.C., Ferro J.N.S., Barbosa F.T., Barreto E. Triterpenes with Healing Activity: A Systematic Review. J. Dermatolog. Treat. 2015;26:465–470. doi: 10.3109/09546634.2015.1021663. [DOI] [PubMed] [Google Scholar]
- 258.Güçlü-Üstündağ Ö., Mazza G., Guclu-Ustundag Ö., Mazza G. Saponins: Properties, Applications and Processing. Crit. Rev. Food Sci. Nutr. 2007;47:231–258. doi: 10.1080/10408390600698197. [DOI] [PubMed] [Google Scholar]
- 259.Baumann E., Stoya G., Völkner A., Richter W., Lemke C., Linss W. Hemolysis of Human Erythrocytes with Saponin Affects the Membrane Structure. Acta Histochem. 2000;102:21–35. doi: 10.1078/0065-1281-00534. [DOI] [PubMed] [Google Scholar]
- 260.Killeen G.F., Madigan C.A., Connolly C.R., Walsh G.A., Clark C., Hynes M.J., Timmins B.F., James P., Headon D.R., Power R.F. Antimicrobial Saponins of Yucca Schidigera and the Implications of Their in Vitro Properties for Their in Vivo Impact. J. Agric. Food Chem. 1998;46:3178–3186. doi: 10.1021/jf970928j. [DOI] [Google Scholar]
- 261.Konishi M., Hano Y., Takayama M., Nomura T., Hamzah A.S., Ahmad R.B., Jasmani H. Triterpenoid Saponins from Hedyotis Nudicaulis. Phytochemistry. 1998;48:525–528. doi: 10.1016/S0031-9422(98)00038-7. [DOI] [Google Scholar]
- 262.Simões C.M.O., Amoros M., Girre L. Mechanism of Antiviral Activity of Triterpenoid Saponins. Phyther. Res. 1999;13:323–328. doi: 10.1002/(SICI)1099-1573(199906)13:4<323::AID-PTR448>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 263.Yogeeswari P., Sriram D. Betulinic Acid and Its Derivatives: A Review on Their Biological Properties. Curr. Med. Chem. 2005;12:657–666. doi: 10.2174/0929867053202214. [DOI] [PubMed] [Google Scholar]
- 264.Just M., Recio M., Giner R., Cuéllar M., Máñez S., Bilia A., Ríos J.-L. Anti-Inflammatory Activity of Unusual Lupane Saponins from Bupleurum Fruticescens. Planta Med. 1998;64:404–407. doi: 10.1055/s-2006-957469. [DOI] [PubMed] [Google Scholar]
- 265.Navarro P., Giner R.M., Recio M.C., Máñez S., Cerdá-Nicolás M., Ríos J.-L. In Vivo Anti-Inflammatory Activity of Saponins from Bupleurum Rotundifolium. Life Sci. 2001;68:1199–1206. doi: 10.1016/S0024-3205(00)01019-5. [DOI] [PubMed] [Google Scholar]
- 266.Lee C.-W., Ko H.-H., Lin C.-C., Chai C.-Y., Chen W.-T., Yen F.-L. Artocarpin Attenuates Ultraviolet B-Induced Skin Damage in Hairless Mice by Antioxidant and Anti-Inflammatory Effect. Food Chem. Toxicol. 2013;60:123–129. doi: 10.1016/j.fct.2013.07.029. [DOI] [PubMed] [Google Scholar]
- 267.Han A.-R.R., Kang Y.-J.J., Windono T., Lee S.K., Seo E.-K.K. Prenylated Flavonoids from the Heartwood of Artocarpus Communis with Inhibitory Activity on Lipopolysaccharide-Induced Nitric Oxide Production. J. Nat. Prod. 2006;69:719–721. doi: 10.1021/np0600346. [DOI] [PubMed] [Google Scholar]
- 268.Yao X., Wu D., Dong N., Ouyang P., Pu J., Hu Q., Wang J., Lu W., Huang J. Moracin C, A Phenolic Compound Isolated from Artocarpus Heterophyllus, Suppresses Lipopolysaccharide-Activated Inflammatory Responses in Murine Raw264.7 Macrophages. Int. J. Mol. Sci. 2016;17:1199. doi: 10.3390/ijms17081199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Tzeng C.-W., Tzeng W.-S., Lin L.-T., Lee C.-W., Yen F.-L., Lin C.-C. Enhanced Autophagic Activity of Artocarpin in Human Hepatocellular Carcinoma Cells through Improving Its Solubility by a Nanoparticle System. Phytomedicine. 2016;23:528–540. doi: 10.1016/j.phymed.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 270.Arung E.T., Wicaksono B.D., Handoko Y.A., Kusuma I.W., Shimizu K., Yulia D., Sandra F. Cytotoxic Effect of Artocarpin on T47D Cells. J. Nat. Med. 2010;64:423–429. doi: 10.1007/s11418-010-0425-6. [DOI] [PubMed] [Google Scholar]
- 271.Bohn J.A., BeMiller J.N. (1→3)-β-d-Glucans as Biological Response Modifiers: A Review of Structure-Functional Activity Relationships. Carbohydr. Polym. 1995;28:3–14. doi: 10.1016/0144-8617(95)00076-3. [DOI] [Google Scholar]
- 272.Browder W., Williams D., Pretus H., Olivero G., Enrichens F., Mao P., Franchello A. Beneficial Effect of Enhanced Macrophage Function in the Trauma Patient. Ann. Surg. 1990;211:605–612. discussion 612–613. [PMC free article] [PubMed] [Google Scholar]
- 273.Sherwood E.R., Williams D.L., McNamee R.B., Jones E.L., Browder I.W., Di Luzio N.R. In Vitro Tumoricidal Activity of Resting and Glucan-Activated Kupffer Cells. J. Leukoc. Biol. 1987;42:69–75. doi: 10.1002/jlb.42.1.69. [DOI] [PubMed] [Google Scholar]
- 274.Pretus H.A., Ensley H.E., McNamee R.B., Jones E.L., Browder I.W., Williams D.L. Isolation, Physicochemical Characterization and Preclinical Efficacy Evaluation of Soluble Scleroglucan. J. Pharmacol. Exp. Ther. 1991;257:500–510. [PubMed] [Google Scholar]
- 275.Majtan J., Jesenak M. β-Glucans: Multi-Functional Modulator of Wound Healing. Molecules. 2018;23:806. doi: 10.3390/molecules23040806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Mellin T.N., Mennie R.J., Cashen D.E., Ronan J.J., Capparella J., James M.L., Disalvo J., Frank J., Linemeyer D., Gimenez-Gallego G., et al. Acidic Fibroblast Growth Factor Accelerates Dermal Wound Healing. J Investig. Dermatol. 1992;7:1–14. doi: 10.3109/08977199209023933. [DOI] [PubMed] [Google Scholar]
- 277.Shearer J.D., Richards J.R., Mills C.D., Caldwell M.D. Differential Regulation of Macrophage Arginine Metabolism: A Proposed Role in Wound Healing. Am. J. Physiol. Metab. 1997;272:E181–E190. doi: 10.1152/ajpendo.1997.272.2.E181. [DOI] [PubMed] [Google Scholar]
- 278.Tsao N. Advanced Wound Care Technologies 2020–2030. IDTechEx. 2022. [(accessed on 19 August 2022)]. Available online: https://www.idtechex.com/en/research-report/advanced-wound-care-technologies-2020-2030/682.
- 279.Buwalda S.J., Vermonden T., Hennink W.E. Hydrogels for Therapeutic Delivery: Current Developments and Future Directions. Biomacromolecules. 2017;18:316–330. doi: 10.1021/acs.biomac.6b01604. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.