Abstract
The use of telehealth technologies to provide clinical services to families of children with autism and other developmental disabilities is a rapidly growing area of research. In particular, remote training of caregivers via video conferencing appears to be a promising approach for disseminating behavior-analytic interventions (Neely, Rispoli, Gerow, Hong, Hagan-Burke, 2017; Tomlinson, Gore, & McGill, 2018). Although remote training offers a number of advantages, it brings a variety of challenges that are unique to this modality. The field would benefit from information on problems that practitioners may encounter when providing these services and how to train caregivers effectively. In this paper, we report on the experiences of 18 practitioners who provided caregiver training via telehealth from four different sites across a 4-year period. We describe a variety of technical and clinical issues that arose during service delivery, suggest strategies for preventing and remediating problems, and include case descriptions and data to illustrate our experiences. This information may help prepare practitioners to deliver telehealth services and guide further research in this area.
Keywords: autism, caregiver training, developmental disabilities, remote coaching, telehealth
Caregiver training is considered an integral component of effective treatments for individuals with autism and other developmental disabilities (Maglione, Gans, Das, Timbie, & Kasari, 2012; Schreibman, 2000). Practitioners provide this training as a supplement to professionally delivered therapy (e.g., Smith, Eikeseth, Klevstrand, & Lovaas, 1997) or as the sole method of intervention (e.g., Derby et al., 1997; for reviews, see Nevill, Lecavalier, & Stratis, 2018; Patterson, Smith, & Mirenda, 2012). Caregiver-mediated intervention helps ensure that treatment effects generalize across environments, offers a more cost-effective alternative to professionally delivered therapy, and enables families to access treatment services that are otherwise unavailable due to a shortage of qualified therapists.
Practitioners have commonly employed elements of behavioral skills training (BST), including modeling and practice with feedback, to train caregivers to implement a variety of behavioral interventions (Parsons, Rollyson, & Reid, 2012). However, a lack of adequate practitioners to provide this training, particularly in rural areas of the United States and in countries outside of the U.S., is a barrier to widespread dissemination of behavior-analytic interventions. To help fill this unmet need, an increasing amount of research has examined the utility of telehealth technologies to deliver caregiver-mediated services in the home and at school.
In the typical telehealth model, the practitioner uses video conferencing software to establish a live video and audio connection between the practitioner’s location (hereafter called the “host site”) and the caregiver’s location, often the home, via the internet (see Peterson, Piazza, Luczynski, & Fisher, 2017, for further description). During scheduled appointments, the practitioner implements components of traditional BST by describing the procedures and by delivering vocal prompts and feedback while observing the caregiver implement the procedures with the client within the camera’s view. This approach has been used to train parents, school personnel, and other professionals (e.g., speech therapists) to implement a variety of interventions (see Boisvert, Lang, Andrianopoulos, & Boscardin, 2010; Neely et al., 2017; Tomlinson et al., 2018; for reviews). Several studies also have compared the outcomes of remote versus in-person caregiver training services (e.g., Hay-Hansson & Eldevik, 2013; Lindgren et al., 2016; Reese, Slone, Soares, & Sprang, 2015; Xie et al., 2013). These findings generally suggest that remote training is a promising approach to caregiver-mediated intervention.
Providing caregiver-training services via telehealth has a number of advantages over in-person services. Telehealth increases caregivers’ access to qualified practitioners, eliminates the need for either the caregiver or practitioner to travel to appointments, and may offer a more cost-efficient way for caregivers to obtain important services (Lindgren et al., 2016). On the other hand, remote services can introduce a number of challenges for the practitioner. These challenges stem not only from the reliance on technology (e.g., need for good internet connection) but from the physical separation between the practitioner and caregiver.
Practitioners who desire to incorporate telehealth services into their practice would benefit from information about common challenges that arise when providing these services and guidelines for successful telehealth practice. Although remote and in-person training share some common challenges, those that are not unique to remote service delivery may be more likely to occur or may be more challenging to resolve when the practitioner is not physically present in the caregiver location. Several articles have described best practices for providing behavior analytic services via telehealth (e.g., Lee et al., 2015; Pollard, Karimi, & Ficcaglia, 2017; Rios, Kazemi, & Peterson, 2018; Romani & Schieltz, 2017). For example, Pollard et al. and Romani and Schieltz focused on ethical issues that may arise when working with families via telehealth (e.g., need for HIPAA-compliant video conferencing software; protections for clients who engage in risky behavior). Lee et al. focused on potential problems with technology that practitioners may encounter, such as delays in the audio transmission or blurry video feed, and provided suggestions for troubleshooting the issues.
As more practitioners begin to incorporate telehealth services into their practice, the field would benefit from further discussion of the challenges associated with remote caregiver training and potential solutions to these problems. This information may help practitioners adopt measures to prevent problems, prepare practitioners to resolve difficulties as they arise during service delivery, and guide further research in this emerging area. The purpose of this paper is to describe the experiences of practitioners at four separate host sites that offered caregiver training services to families via telehealth across a 4-year period. We share difficulties that they encountered and possible solutions for those issues, along with case descriptions and data to illustrate some of these experiences.
Method
Participants and Settings
We report on the experiences of 18 practitioners at four different sites who provided telehealth caregiver training services to 237 families between January 2015 and April 2019 for a total of 2,242 appointments. The host sites were located in Iowa, Texas, and Georgia. The practitioners had 1 to 20 years of experience training caregivers in behavior analytic procedures. At the start of the time period, they had 0 to 6 years of experience providing telehealth services to caregivers. Practitioners included five doctoral-level Board Certified Behavior Analysts (BCBAs) or licensed clinical psychologists with behavior-analytic training, two pre-doctoral students near the completion of their doctoral training in school or clinical psychology, and 11 BCBAs with master’s degrees. The practitioners conducted sessions in private offices, therapy rooms, home offices, and partitioned workstations. They used desktops or laptops computers, external or internal cameras and microphones, and HIPAA-compliant videoconferencing software, including Vidyo, V-see, Ring Central, and Zoom. Practitioners accessed the internet through either ethernet or wireless connections. All but one of the sites also video recorded all sessions.
The families resided in the same states as the host sites. All of the families responded to announcements (e.g., flyers posted in buildings and on websites; information disseminated to other providers) or phone contacts about the opportunity to receive caregiver training services at no cost as part of research projects. Nearly all of the caregivers who participated in the training were the mothers of the children. Participating children (hereafter referred to as “clients”) were between the ages of 1.7 years and 16 years. The majority of clients were diagnosed with autism, but they also included individuals diagnosed with intellectual disability, cerebral palsy, and Down syndrome. All of the clients engaged in one or more topographies of problem behavior, including aggression, disruption, self-injury, and noncompliance. At the client sites, telehealth sessions were conducted in one or more locations in the families’ homes, including living areas, bedrooms, and play rooms. The locations contained materials (instructional, communication, leisure) needed to conduct the sessions, along with the furniture and materials that were natural to that location (with some exceptions, as described further below). Families used a variety of equipment to conduct the telehealth sessions, including desktop computers, laptops, tablets, and smart phones, along with ancillary equipment (e.g., earbuds, external microphones, external webcams) in some cases. One of the host sites lent any necessary equipment (e.g., laptop, tablet, microphone) to clients who did not already possess it for the duration of their participation. The families downloaded the teleconferencing software for free and accessed it via links sent through private e-mail. Families used either ethernet or wireless internet connections.
Procedures
The majority of families received assessment and treatment services for the client’s problem behavior. Telehealth appointments with caregivers typically ranged from 45 min to 60 min each, with a frequency that ranged from once per month to twice per week, depending on the site and family. For most families, services continued until the family met the treatment goals or the family dropped out. Families who completed services received an average of 12 appointments (range, 1 – 34). After the initial intake appointment, the practitioner coached the caregiver to implement functional analyses ([FA] Iwata, Dorsey, Slifer, Bauman, & Richman, 1982/1994) or brief antecedent-based functional assessments (Call, Zangrillo, Delfs, & Findley, 2013) of targeted problem behavior using the procedures described by Wacker et al. (2013b). Treatment typically consisted of functional communication training. Practitioners trained the parent to conduct treatment using the procedures described by Wacker et al. (2013a). For most families, the goal was for the caregiver to implement the treatment with at least 90% accuracy when the practitioner delayed feedback until the end of the session and/or for problem behavior to decrease by at least 80% relative to levels in the relevant condition of the functional analysis. Multiple 5-min to 10-min assessment or treatment sessions typically occurred during each appointment. The practitioner and other trained observers used frequency, duration, or partial interval recording to collect data on individually-defined client responses, including problem behavior, communication, and compliance to instructions, either live or from video-recorded telehealth sessions. For the purpose of this paper, observers scored additional responses from video-recorded sessions (e.g., attempts to elope; reactive responses) related to specific challenges encountered (see further description below). Observers also collected data on caregiver responses related to the delivery of prescribed antecedents and consequences of client responses.
In preparation for this paper, the practitioners at each site met to generate a list of challenges that they had encountered and solutions that they had employed while providing telehealth services to families. A representative for each site then provided this information to the first author, who then combined and disseminated it to all of the sites. The practitioners had an opportunity to review the combined-site information, submit additional challenges and solutions, and provide relevant illustrative case data. Specifically, the first author asked the representatives to include all problems that they thought were worth mentioning, along with their attempts to solve them, regardless of whether they were successful. The first author also asked them to suggest other possible solutions to problems on the combined-site list even if they had not encountered those problems.
In the final step, the first author reviewed the information, omitted any redundancies, and arranged the information into the following six categories for organizational purposes: (a) technical issues, (b) challenges with remote viewing, (c) disruptions in the client’s environment, (d) other issues related to client behavior, (e) issues related to caregiver behavior, and (f) additional issues at the practitioner (host) site.
Results and Discussion
In the following sections, we describe common challenges and possible solutions within the specific categories described above, along with general guidelines for providing effective telehealth services. Table 1 provides a summary of these challenges and potential solutions.
Table 1.
Sample of Potential Challenges and Solutions When Providing Telehealth Services
| Challenges | Solutions |
|---|---|
| Technical Issues | |
| Caregiver does not have access to equipment | Establish lending library; locate nearby facility with equipment |
| Caregiver has connectivity issues | Upgrade modem/internet service; reduce number of devices |
| Caregiver has difficulty installing/using software | Provide task analyses; instruct caregiver via phone |
| Caregiver has hardware or software failures | Provide access to alternative hardware or software |
| Poor visibility due to room lighting | Close drapes, move away from window, change room lighting |
| Challenges with Remote Viewing | |
| Client not always in view | Modify camera position/session location, remove or rearrange furniture, install physical barriers, use multiple cameras |
| Client behavior difficult to see or hear | Arrange for caregiver to signal occurrences of target behaviors |
| Practitioner difficult to see or hear | Arrange for caregiver to wear Bluetooth headset, send text messages |
| Disruptions in Client’s Environment | |
| Items present in room disruptive to sessions | Instruct caregiver to remove superfluous items from room |
| Other family members interrupt sessions | Arrange sessions when other family members not at home |
| Other Issues Related to Client Behavior | |
| Client engages in dangerous behavior | Mail protective equipment to caregiver, train caregiver to block, prioritize treatments that minimize extinction bursts |
| Client reactive to practitioner’s image or voice | Disconnect audio and/or video feed |
| Issues Related to Caregiver Behavior | |
| Caregiver engages in emotional responding | Stop session, speak privately with caregiver |
| Caregiver behavior insensitive to vocal instructions | Arrange in-person appointments, model procedures on camera, review videotaped sessions with caregiver |
| Caregiver overly casual in dress or behavior | Clarify expectations at the outset of services |
| Issues at Host Site | |
| Practitioner shares office with others | Use headsets, speak softly, modify appointment schedule |
| Practitioner not specifically trained for telehealth | Obtain training and supervision from qualified practitioner |
Technical Issues
Advances in hardware, software, and internet speed have greatly improved the reliability and quality of connectivity for telehealth sessions (Peterson et al., 2017). Reviews of the literature on telehealth services suggest that technical issues have not prevented successful outcomes (Tomlinson et al., 2018). In our own analysis of connectivity issues for 564 appointments conducted with families in Texas, practitioners recorded the percentage of the total duration of each appointment (typically 60 min) that the practitioner completed due to the absence of connectivity problems. Just 5% of appointments lasted less than 73% of the scheduled duration due to connectivity issues, whereas 85% lasted at least 92% of the scheduled duration. This suggests that connectivity per se is not typically a barrier to effective telehealth services, although it may reduce the efficiency of services. Nonetheless, the use of technology introduces a variety of potential problems. In this section, we describe the technical challenges that we have encountered and provide suggestions for both preventing and remediating them to minimize the amount of lost clinical time.
First, a caregiver may not have access to hardware that authors frequently recommend in papers on telehealth services. Although a desktop computer or laptop with an external webcam and landline are ideal (Lee et al., 2015), we have found that any smart device with a built-in camera (e.g., phones, tablets) and internet access is adequate as long as it can support the necessary software (see also Rios et al., 2018, for a discussion of hardware). Such devices are now ubiquitous, but practitioners may still encounter families and caregivers who do not have access to this hardware. Practitioners might consider establishing a lending library to provide these individuals with temporary access to inexpensive hardware (e.g., tablets, iPods). These devices could be shipped to caregivers and then returned to the practitioner at the conclusion of clinical services. Occasionally, we have encountered problems with the family’s use of loaner equipment. For example, family members used the laptops for other purposes, resulting in the installation of irrelevant software, inappropriate downloads (e.g., pornographic pictures), and damage to the equipment (e.g., jammed DVD). Some families never returned the loaner equipment, with one family reporting that they had pawned the device. Thus, we recommend that practitioners establish a contract with caregivers regarding the care and use of loaned equipment (e.g., caregivers agree that the device will be exclusively dedicated to clinical sessions) and the terms of its return (e.g., caregivers agree to return the device to the practitioner within a certain amount of time following the termination of services). Alternatively, practitioners might identify a health-related clinic or center located near the caregiver with administrators who are willing to provide access to the necessary facilities, hardware, software, and internet connection.
Second, some caregivers may not have access to adequate internet speed (see Lee et al., 2015 for recommended upload, download, and latency to transmission speeds). In such cases, practitioners may resolve this issue by instructing caregivers to upgrade their modem or internet service, to reduce the number of devices that are accessing the internet simultaneously at their location, or to determine if certain rooms in their location have better internet access. For example, during an initial appointment with one family, the video frequently froze and the audio was of very poor quality at the host site, a problem that the caregiver also reported at the home location. An internet speed test at the family’s location and consultation with an information technology (IT) professional revealed that the family’s download speed, upload speed, and latency were slow but adequate. Further inquiry by the IT professional identified a potential problem: During the telehealth appointments, the mother was using a laptop connected via Wi-Fi for the sessions, the client and his brother were using separate Wi-Fi-connected tablets for entertainment, and the client’s father was using another Wi-Fi-connected laptop for work. The problem was immediately resolved when the family restricted the number of devices utilizing the Wi-Fi to just one laptop during the 60-min telehealth appointments. The client and his brother could still access all previously downloaded videos and games on their tablets, and the father accessed the internet on his laptop through an Ethernet connection if needed.
Although our experience indicates that connectivity per se is not a significant barrier to service provision, the practitioner may encounter a number of other barriers related to the use of technology-based service. For example, in a sample of 289 appointments with families in Iowa, we found that problems with technology disrupted an average of 25% of appointments (range, 5% – 55% per family) in some manner (i.e., resulted in cancelled or terminated appointments; included sessions that could not be scored for data collection purposes). Some caregivers may have difficulty using the software, particularly if they have limited experience with similar types of software. Practitioners encountering this issue might provide caregivers with a detailed task analysis for launching and navigating the application, along with associated screen shots. Practitioners also may find it beneficial to call caregivers on the phone to walk them through software installation or navigation. Selecting alternative software that is more user friendly may be helpful for caregivers who have continued problems. (See Lee et al., 2015; Peterson et al., 2017; Rios et al., 2018, for further discussion about available software). Practitioners should always first ensure that caregivers are correctly following instructions to launch and use the software. If so, continued software issues may occur if the caregivers’ browser is not compatible with the videoconferencing software. We recommend that practitioners instruct caregivers to update their browser or switch to a different browser to resolve software issues. In some cases, switching to a different device (e.g., using a smart phone instead of a laptop) will resolve software issues.
As noted previously, the video feed may sometimes become fuzzy or blurry due to connectivity issues. We have found that rebooting the video feed or asking the caregiver to tap the screen (when using a smartphone) may resolve this issue. Room lighting (e.g., proximity to a window with natural light) also may interfere with adequate visual clarity due to glare. In such cases, the practitioner may need to instruct the caregiver to move away from the window, close the drapes, or relocate to a room with different lighting. In the event of unresolved video interference, the practitioner should be prepared to provide more detailed spoken instructions to the caregiver and instruct the caregiver to describe what is happening in the session. In the event of unresolved audio failure, the practitioner should be prepared to use a telephone, e-mail, or messaging application (with appropriate privacy controls) to communicate with the caregiver.
Practitioners should devise other back-up plans that they can implement in the event of unresolved hardware or software failures during sessions. This will ensure that practitioners can continue services without interruption. One of our families lost a total of 9 weeks of potential services due to a combination of software upgrade difficulties and hardware issues with the caregiver’s iPad. Software may sometimes fail and cannot be recovered, or the practitioner may have limited time for troubleshooting. Back-up plans may involve arranging for caregivers to access alternative software or Internet browsers in the event of compatibility issues or asking caregivers to video record the sessions. Caregivers would then send the recordings to the practitioner for viewing and feedback. In the event of unresolved hardware issues, the practitioner might loan the caregiver a device, as described previously, so that appointments can continue while the hardware is out for repair.
Finally, we recommend that practitioners send separate videoconferencing links to families. Otherwise, the caregivers from two adjacent appointments could enter the conference room at the same time, breeching assurances of confidentiality.
Challenges with Remote Viewing
Observation of client and caregiver behavior is an essential component of effective telehealth services. However, beyond the technological issues described in the previous section, other problems may arise that make observation challenging to conduct remotely. These issues are less likely to occur during in-vivo services, so practitioners new to telehealth services may be unprepared to address or manage them during videoconferencing appointments. Besides room lighting, other aspects of the environment may create barriers to effective remote viewing. For example, it is critical for the client and caregiver to remain within the scope of the camera lens. In a sample of 289 appointments with families in Iowa, we found that an average of 31.5% of appointments included at least one session during which the practitioner could not view the client. This may occur if the size of the room or area is larger than the range of the camera lens, as the client or caregiver may easily move outside of the practitioner’s view. The practitioner may prevent or remedy this issue by considering the height and position of the camera. The caregiver may need to work with the practitioner to troubleshoot a variety of camera positions during the first appointment. Using shelves or tripods to raise the height of the camera may help expand the viewing range. If accessible, an external webcam that connects to the device via Bluetooth can make it easier to modify the position or height of the camera (see Lee et al., 2015; Peterson et al., 2017; Rios et al., 2018 for further discussion).
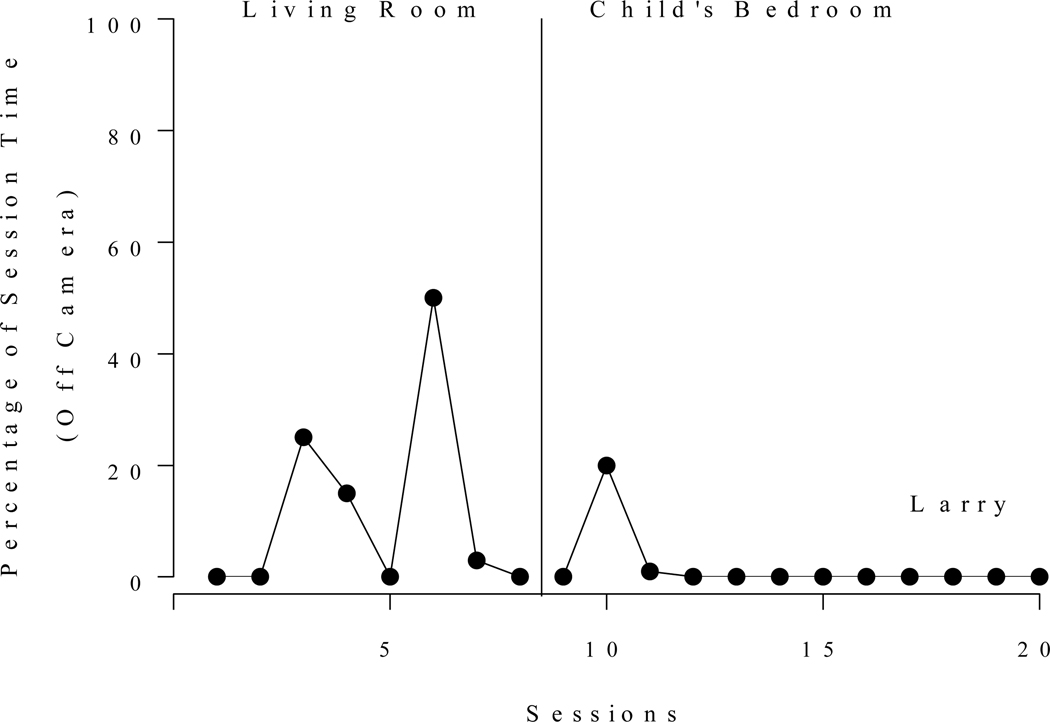
If none of these solutions remedy the problem, a potentially simpler solution is to identify a smaller room or area of the home for the sessions. For example, we moved the location of one family’s sessions from the living room to the client’s bedroom after the client, Larry, spent as much as 50% of the time off camera (defined as the client’s entire body out of the camera view for more than 1 s) during sessions in the living room (see left panel of Figure 1). The percentage of session time off camera decreased to zero in the new location (see right panel of Figure 1), with the exception of a single session during which Larry, a 6-year-old boy with ASD, positioned himself under a bed (see description of this problem below). Interobserver agreement collected on this measure for 35% of Larry’s sessions averaged 98.5% (range, 87% – 100%). Another solution is to use two cameras if a single camera is not adequate to keep the client and caregiver in view, particularly for those who move frequently around the room.
Figure 1.
Percentage of session time with Larry off-camera in the initial location (living room) and after re-locating sessions to the child’s bedroom.
Remote viewing also may be challenging if the client frequently elopes from the room or area during sessions. Practitioners might remedy this problem by having caregivers install child gates or arrange other accessible barriers (e.g., furniture) to block movement out of the area or by moving the location to a room with doors to prevent elopement. If these strategies do not prevent elopement, the practitioner might instruct the caregiver on appropriate ways to physically block elopement during sessions or arrange for the caregiver to place an additional camera outside of the area to capture the client’s behavior in a different location. If caregiver blocking or use of multiple stationary cameras are neither possible nor desirable, the practitioner might consider asking caregivers to carry or affix a smart device (e.g., phone, iPad, web-enabled body camera) to their bodies so that they can keep the client in view by following the client outside of the area. Other potential solutions may be evident by considering the possible function(s) of client elopement. For example, if elopement typically produces access to objects that are only available in an external location, the practitioner might ensure that the client can access those objects in the session room or area as long as this arrangement is compatible with the session goals.
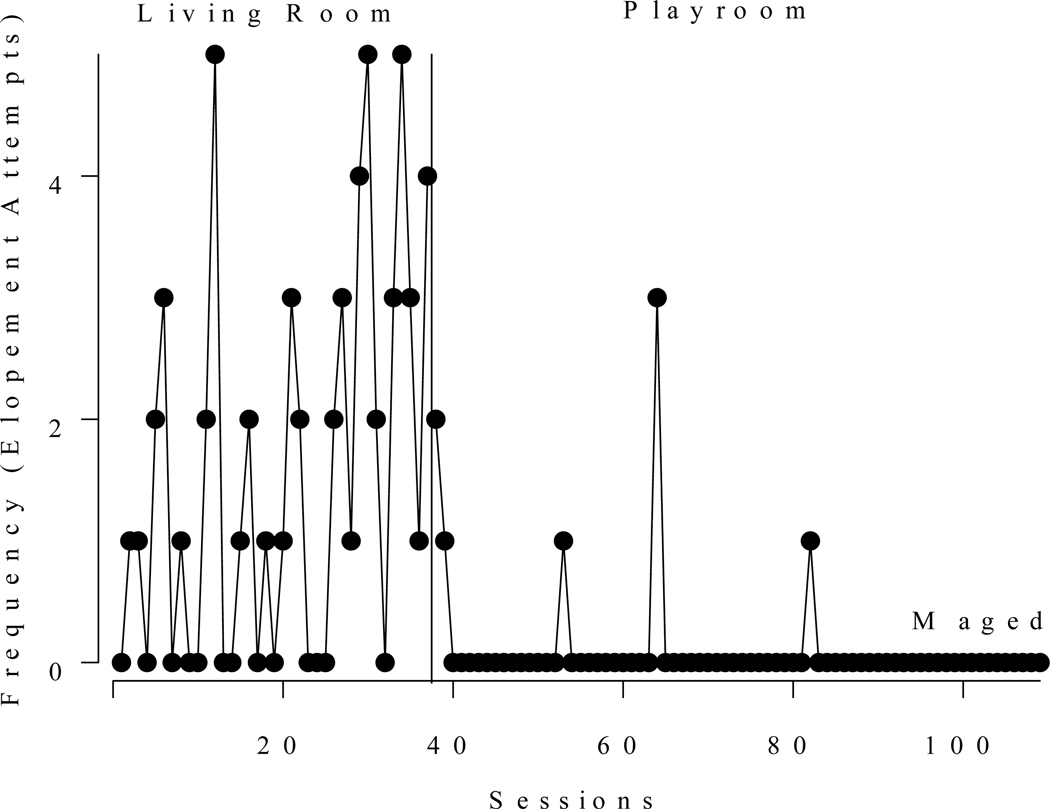
We evaluated several of these potential solutions while working with Maged, a 2-year, 8month old boy diagnosed with ASD, attention deficit/hyperactivity disorder, and developmental delay. Maged’s mother served as the primary trainee with assistance from Maged’s father when his work schedule allowed. Telehealth appointments initially occurred in the living area of the main floor, which seemed ideal because Maged was very active and the large open floor plan provided him with plenty of room to run. The practitioner instructed Maged’s family to position a laptop in one corner of the room to provide a wide view of the entire living area. Nonetheless, Maged began to run from the living area to rooms outside of the camera’s view and to hide behind furniture in the room when the parent initiated test sessions of an FA. Repositioning the laptop did not provide a complete view of all areas surrounding the large couches and recliner chairs in the room. Utilizing multiple cameras did not seem practical because he eloped to so many different areas of the home.
Thus, the practitioner instructed Maged’s mother to block attempts to elope from the living area and to move the laptop whenever Maged hid behind furniture so that he would be in the practitioner’s view. Maged’s father also assisted with blocking when he was available. However, blocking did not decrease Maged’s attempts to elope or to hide, and, more concerning, blocking often evoked Maged’s aggression towards his parents. Moving the laptop every time Maged hid behind furniture also became unmanageable due to the high frequency of this behavior. As shown in Figure 2, Maged attempted to elope (defined as passing through or attempting to pass through an entryway to an adjacent room, turning or pulling of the door handle in the playroom, and moving or attempting to move behind a piece of furniture) an average of 1.6 times per 5-min session during the FA and initial stages of treatment. Given these challenges, the practitioner and Maged’s parents decided to move the location of the sessions to a playroom, which was less than half the size of the living area and had a door that they could lock. Although this location created other challenges (discussed further below), Maged’s attempts to elope immediately decreased and rarely occurred across the remaining appointments, as shown in Figure 2. Interobserver agreement on elopement attempts, collected for 33% of sessions, averaged 94% (range, 80% – 100%).
Figure 2.
Frequency of Maged’s elopement attempts during sessions in the initial location (living room ) and after re-locating sessions to a playroom
Like Maged, clients who position themselves under or behind furniture also create problems for remote viewing. Practitioners should consider this potential barrier when helping caregivers select the most appropriate location for sessions. Possible solutions include removing or rearranging furniture to reduce the likelihood of obscured viewing, blocking the client’s access to certain areas of the room, installing physical barriers (e.g., child gates) in front of furniture, and placing objects next to or under furniture to block the client’s access to these spaces. If the caregiver is unable to block or retrieve the client (or it would be contraindicated to do so), the practitioner might pause the session when the client is not visible.
Even with appropriate positioning of the camera and an unobscured view, the practitioner may have difficulty observing or hearing certain aspects of client and caregiver behavior. When practitioners are physically present in the session location, they can modify their position to ensure that they detect less salient client responses (e.g., pinching the parent’s arm as a topography of aggression; requesting a toy with a low voice volume) or caregiver responses (e.g., providing pats on the back as a form of attention, speaking to the client with a low voice volume). When certain responses are difficult to see or hear during telehealth sessions despite good connectivity, the practitioner could arrange for the caregiver to signal the occurrence of selected targets (e.g., by raising the hand, holding up a card, speaking a code word). In some cases, positioning an additional camera close to the client also may help resolve some of these issues.
The ability of the caregiver to hear the practitioner’s instructions and feedback also is essential to effective telehealth services. Disruptive behavior of the client (e.g., yelling) may create a substantial challenge for the practitioner to communicate with the caregiver during critical moments of the session (e.g., when coaching the caregiver to respond appropriately to problem behavior). Potential solutions include having the caregiver wear a Bluetooth headset through which he or she can hear and speak to the practitioner, providing the caregiver with more explicit coaching or task analyses prior to beginning the session with the client, texting messages to the caregiver’s phone during sessions, and signaling the caregiver to pause interactions with the client so that the practitioner can provide instructions and feedback on fidelity.
For example, we encountered communication problems when moving the location of Maged’s sessions to the play room. Unlike the larger living area, the playroom had wood floors, less furniture and a high ceiling, all of which contributed to loud echoing. This made it more difficult for the practitioner and Maged’s parents to hear each other, particularly when Maged engaged in loud screaming and crying. Occasionally, Maged’s parents missed the practitioner’s directives, and the practitioner could not decipher questions and feedback provided by Maged’s parents. The practitioner became increasingly concerned when Maged’s parents could not hear his instructions when he described how to block Maged’s self-injury during sessions. To address this issue, the practitioner restructured the weekly appointments. The practitioner dedicated the first 5 min to 15 min and the final 15 min of the hourly appointments to answering parent questions, providing feedback on treatment fidelity, and describing procedural modifications and safety techniques (i.e., blocking and injury prevention). Although the practitioner devoted only about half of the hourly appointments to treatment sessions, the practitioner and Maged’s parents reported that the pre- and post-treatment discussion increased the efficiency of service delivery because it reduced the need for breaks during treatment time.
Disruptions in Client’s Environment
Other aspects of the client’s environment may interfere with effective telehealth services. Although some of these issues may arise when practitioners are physically present in the session location, they may be more difficult to resolve remotely. As such, we recommend that practitioners prepare in advance for some of these problems to ensure smoother sessions. When coaching caregivers to conduct assessments or treatment evaluations, it is often important to control the items that are present and available to clients in the session location. For example, the client’s uncontrolled access to preferred items could impact the outcomes of functional analyses, during which the caregiver is instructed to systematically withhold and deliver putative reinforcers for problem behavior. The presence or availability of alternative sources of reinforcement also could disrupt client performance when the practitioner is training caregivers to implement interventions. For example, the client may engage in responses that compete with the targeted skill (e.g., attempt to access or interact with preferred items) while the caregiver is learning to implement skill acquisition programs with the client.
Practitioners can avoid these problems by considering alternative areas or rooms for the sessions (e.g., the parent’s bedroom), at least temporarily, if the desired location (e.g., the family room) contains a lot of potentially distracting items. Practitioners also could instruct caregivers to remove superfluous items from the selected location prior to sessions or hide items where they will be out of the client’s reach (e.g., ask the caregiver to obtain a lidded toy box and place all items in this box prior to sessions). If none of these solutions is possible, practitioners could teach caregivers to block the client’s access to items or incorporate the items into sessions.
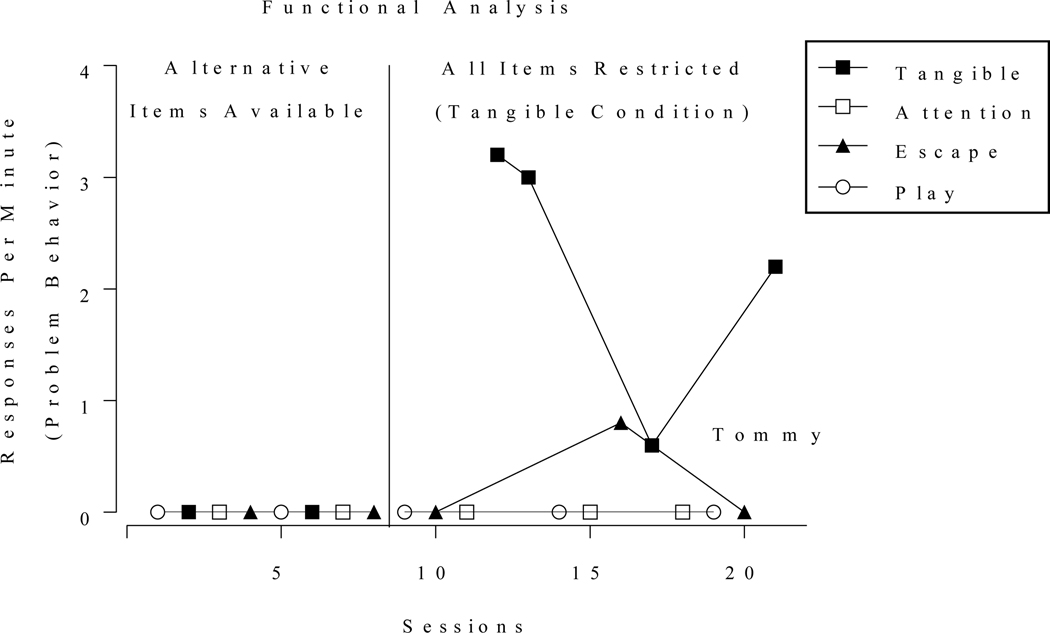
For example, during the tangible condition of the functional analysis, all potentially preferred items in the room (rather than the tangible(s) identified as targets for this condition) might be among those that the caregiver removes and then delivers contingent on problem behavior. We adopted this strategy while coaching a parent to conduct an FA with a 4-year-old boy, Tommy, referred for the assessment and treatment of aggression (hitting, biting, kicking, and head-butting), self-injury (hitting his head on hard surfaces), and inappropriate speech (making threats and cursing). The parent conducted sessions in his bedroom, which contained a variety of toys. The practitioner noticed that, during the tangible condition, the client interacted with toys other than those that the parent restricted as part of the planned contingencies for the session. To resolve this issue, the practitioner instructed the parent to remove any items that he picked up during the session while stating, “You can’t play with toys right now.” Contingent on problem behavior, the caregiver granted access to the restricted items, stating, “It’s Ok to play with toys now.” As shown in Figure 3, Tommy did not engage in any problem behavior during the FA prior to the modification, possibly because access to alternative tangible items abolished the reinforcing value of items the caregiver initially restricted. Interobserver agreement, collected for 37% of sessions, averaged 85.6% (range, 71% – 100%). Following the modification, problem behavior increased in the tangible condition while remaining low in the other conditions.
Figure 3.
Responses per minute of Tommy’s problem behavior during the inital sessions of the functional analysis and after items were restricted in the tangible condition of the functional analysis
The devices positioned for remote viewing or video conferencing also may constitute a source of disruption, particularly if the client commonly has access to smart devices (e.g., phones, iPads) that function as highly preferred items. The client may engage in responses that typically produce access to the item outside of sessions. For example, the client may repeatedly grab the device if in reach; if not in reach, the client may orient towards the device, repeatedly request it, or climb on furniture in an attempt to access it. Extinction-induced responding then may emerge when caregivers restrict access to devices that are necessary to conduct the telehealth sessions. One solution is to use two devices during sessions, one for the caregiver to use for the telehealth sessions and the other to use as a preferred item for the client. Another solution is to connect the laptop or smart device to an external webcam with an extended cord and place a cover over the device so that it is hidden from the client. The caregiver also could schedule time for the client to access the device outside of sessions to create an abolishing operation that reduces the reinforcing value of these devices or provide access to competing, highly preferred items during sessions.
Other types of disruptions might be more likely to occur when the professional is not physically present in the home. For example, the physical presence of the professional in the home typically may function as a discriminative stimulus for other family members to remain outside the session location or to refrain from interacting with the caregiver and client during appointments. As such, other members of the family may be more likely to interrupt sessions delivered via telehealth technologies. Such interruptions may divert the attention of the client or caregiver, potentially interfering with controlled evaluations (e.g., functional analyses) and reducing the amount of available training time if sessions must pause during this time. Such interferences might be particularly unavoidable if the family is living in a small home or apartment or if the caregiver is responsible for other family members. Possible solutions include asking the caregiver to schedule appointments when other family members will not be in the home, having another caregiver attend to other family members in a separate location of the home, and instructing the caregiver on the best methods for redirecting the client’ behavior if he or she attempts to interact with other family members.
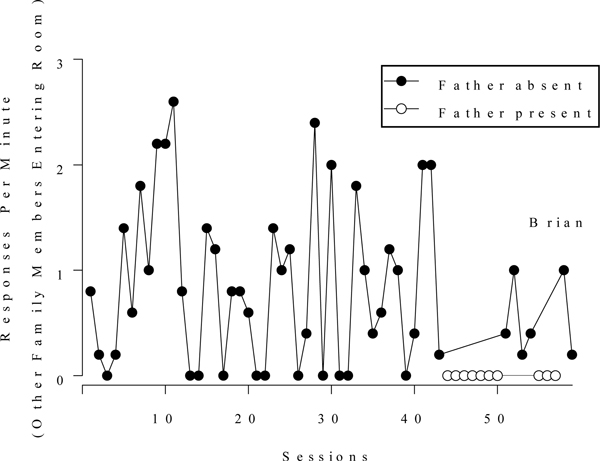
For example, we worked with the mother of a 2-year-old boy who engaged in aggression, disruption, and self-injury. They lived in a small apartment with the boy’s father and two older siblings. The other family members, particularly the siblings, frequently entered the session room. The mother would discontinue the sessions briefly to attend to the siblings. As shown in Figure 4 (closed symbols), family members entered the room more than 1 time per minute during many of the sessions, substantially slowing the progress of service delivery. To address this challenge, the practitioner made every effort to schedule appointments when the child’s father would be at home to attend to the siblings. No family members entered the room when the father was home (open symbols in Figure 4), indicating that he successfully prevented the interruptions. Interobserver agreement on family members entering the room, collected for 32% of sessions, averaged 83.7% (range, 68% – 100%). In some cases, however, a single caregiver must monitor multiple children. If so, the practitioner might instruct the caregiver to provide the children with access to high preference items outside of the session location and to schedule frequent breaks during the appointment.
Figure 4.
Responses per minute of family members entering the room during Brian’s sessions when his father was present versus absent in the home
The practitioner also should appraise elements of the environment in light of the client’s topographies of problem behavior. For example, if the client engages in property destruction during sessions, the practitioner could instruct the caregiver to remove breakable items from the room prior to the appointment, consider a different location, or teach the caregiver how to block the client’s attempts to destroy objects. The practitioner also should scan the area to identify and remove items that may place the client or caregiver at risk of injury if the client pushes or throws them during sessions.
Although various disruptions in the client’s environment can create challenges to the smooth delivery of assessment and treatment services, they are also a part of the natural environment where caregivers will be implementing the treatment. Practitioners should consider gradually re-introducing distractions (e.g., presence of other family members) into the sessions to help identify treatment modifications that may be necessary under more naturalistic conditions and to help promote maintenance and generalization of caregivers’ newly acquired skills. Indeed, the ability to incorporate an approach that would increase the ecological validity of caregiver training could be considered a benefit of telehealth services.
Other Issues Related to Client Behavior
Other aspects of the client’s behavior may complicate remote service provision. The practitioner will not be physically present to help prevent risk to the client or caregiver if the client’s problem behavior escalates during sessions. If severe behavior is possible, the practitioner might mail protective equipment to the caregiver prior to sessions, train the caregiver to block dangerous behavior safely, and recruit other family members to assist with sessions. The practitioner also might consider treatments that minimize extinction bursts (e.g., noncontingent reinforcement; demand fading; Hagopian, Crockett, Van Stone, DeLeon, & Bowman, 2000; Zarcone et al., 1993), or initially train the caregiver to implement the procedures in the absence of the client. For example, the practitioner could model the procedures on camera in role-play with a colleague or have the caregiver practice implementing the procedures in role-play with another family member. The practitioner also may encounter ethical issues if the client disrobes during sessions, particularly if the practitioner is recording the session. In such cases, the practitioner should be prepared to turn off the recording or instruct the caregiver to place the client in clothing that would be difficult to remove during sessions (e.g., singlets).
The practitioner’s image on the video screen or vocal instructions to the caregiver also may have a reactive effect on the client’s behavior. A variety of measures may help the practitioner avoid or reduce reactivity. Among the potential solutions, we recommend that the practitioner instruct the caregiver to use Bluetooth headphones, turn off the video feed at the host site (while maintaining the video feed at the caregiver site), speak to the caregiver in the client’s absence, avoid speaking directly to the client, communicate to the caregiver via text messages while muting the microphone, and have the caregiver conduct additional play sessions as a “warm up” at the start of services.
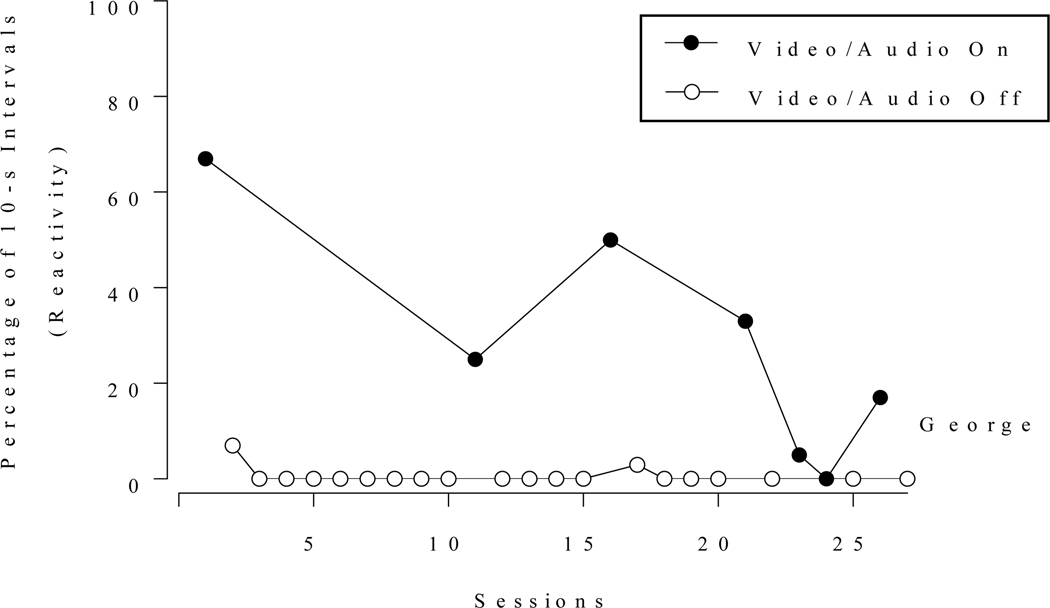
For example, George, a 7-year-old boy, engaged in a variety of apparent reactive behaviors during the first videoconferencing session. Specifically, he frequently engaged in comments such as “Hey, why are they on there?” and “No, I’m not doing that today” while orienting his gaze towards the camera and either attempted to or successfully closed the laptop or knocked it over. To address the reactivity (defined as George orienting his gaze towards the camera while engaging in the comments and behaviors described above), the practitioner turned off the video and microphone at the host site and delivered instructions to George’s mother via text messaging. Across four monthly scheduled appointments, the practitioner occasionally restored the video and audio feedback at the host site to evaluate the effects of this solution on George’s behavior. The percentage of 10-s intervals with reactive behavior during each 2-min to 5-min session across the four separate appointments are shown in Figure 5. George engaged in little to no reactive behaviors when the practitioner implemented these measures and in a mean of 28% of intervals when the practitioner restored the video and audio feed. Interestingly, the reactive effects appeared to diminish across appointments. Interobserver agreement on this behavior, collected during 26% of sessions, averaged 95% (range, 83% – 100%).
Figure 5.
Percentage of 10-s intervals with George’s reactive responses during sessions with the video and audio feed turned on versus off
Issues Related to Caregiver Behavior
The practitioner may find it difficult to navigate certain issues related to caregiver behavior when providing services remotely. For example, a caregiver may begin to engage in emotional responding (yelling, crying) while implementing treatments for problem behavior or when managing difficult client behavior. This can be challenging for the practitioner to address when not physically present with the caregiver. If possible, we recommend that the practitioner stop the session and speak with the caregiver in the absence of the client in the event of emotional responding. Practitioners also must be prepared to handle potential evidence of abuse or neglect that they observe remotely. Prior to services, we recommend that practitioners become familiar with the mandatory reporting procedures and processes in the states where their clients reside if different from their own and inform the caregiver that the practitioner is a mandatory reporter during the first meeting with the family.
Practitioners may find it particularly difficult to train some caregivers remotely due to the greater reliance on verbal stimuli during training sessions. The behavior of some caregivers may be relatively insensitive to the practitioner’s vocal instructions, leading to difficulties with treatment integrity and the acquisition of critical program components. Schieltz et al. (2018) described such an issue with one parent whose child’s problem behavior did not improve with FCT. Practitioners encountering this problem might consider a variety of strategies to supplement remote coaching and feedback. If the caregiver resides within reasonable proximity to the practitioner’s location, the practitioner could conduct some in-vivo outreach appointments in the caregiver’s home or arrange for the caregiver to receive at least one appointment in the practitioner’s location, where the practitioner could provide more intensive training (e.g., demonstrations, role-play) with or without the child present. If supplemental in-person trainings are not possible, the practitioner could send the caregiver more detailed written instructions prior to appointments and model the procedures via role-play with a colleague during appointments. The practitioner also might arrange for the caregiver to access prior video-recorded training sessions. Reviewing these sessions with the parent while pointing out correct and incorrect instances of implementation might increase the saliency of vocal feedback (e.g., Phaneuf & McIntyre, 2007)
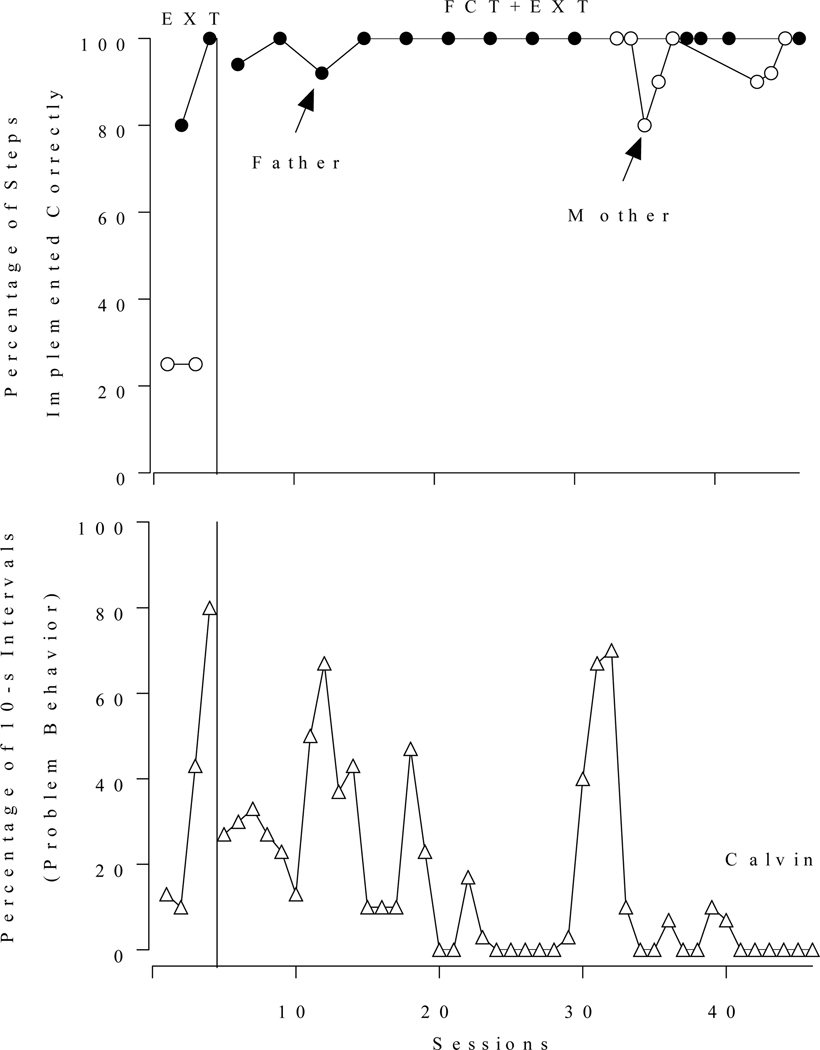
When two or more caregivers are available for the training, the practitioner might take advantage of another potential strategy for caregivers who have difficulty with remote coaching. The practitioner could include multiple caregivers in the training from the outset in case one or more of the caregivers find it particularly challenging to obtain or maintain adequate levels of procedural integrity. In such cases, the practitioner could dedicate the training time to the caregiver(s) making more progress, with the goal to enlist their assistance in training the other caregiver(s) at home. We took this approach with one case after both the mother and father of Calvin, a 5-year-old boy with autism, began to receive training to implement treatment for escape-maintained property destruction. The practitioner alternated sessions with the parents during initial training sessions that focused on implementing extinction for problem behavior (i.e., delivering instructions and prompts using a three-step prompting hierarchy and physical guidance contingent on problem behavior). As shown in Figure 6 (top panel), the father implemented the steps with 100% accuracy by the second training session, whereas the mother implemented just 25% of the steps correctly. To maximize the efficiency of the training, the practitioner focused on training the father to implement the remainder of the intervention (FCT) during subsequent appointments until he met the mastery criterion and the client’s problem behavior had decreased to low levels (bottom panel of Figure 6). At this point, the father trained the mother outside of the scheduled appointments. Subsequent observations of the mother (starting with session 33) indicated that the father successfully trained the mother to implement the intervention and that the client’s problem behavior decreased to low levels with both parents. Interobserver agreement data on the parents’ procedural integrity and on Calvin’s problem behavior were collected for 75% and 41% of the sessions, respectively, and averaged 99% (range, 89% – 100%) and 97% (range, 90% – 97%). When using this strategy, however, the practitioner likely will need to provide the caregiver trainer with some initial support and training on how to train others.
Figure 6.
Percentage of treatment steps implemented correctly by Calvin’s father versus m other (top panel) and percentage of 10-s intervals with problem behavior for Calvin (bottom panel) across treatment sessions
We also have found that some caregivers may appear overly causal during appointments (e.g., wear pajamas, underwear, or very little clothing) or engage in behaviors unrelated to the appointments (e.g., check their mail), which may be less likely to occur when the practitioner is physically present in the home. Such behaviors may make the practitioner feel uncomfortable or reduce the time available for services. Clarifying expectations at the outset of services, including the anticipated activities and roles of the caregiver and practitioner during each scheduled appointment, may help to prevent these issues.
Additional Issues for the Practitioner (Host) Site
Agencies providing telehealth services to families will need to consider additional logistical and practical issues that may arise at the host site. Practitioners who share an office with other staff members or who might be overheard by others during appointments must consider potential breeches to client confidentiality. If the agency cannot provide soundproofed dedicated space for telehealth sessions, the practitioner should use headsets and speak softly, place sound dampeners outside of the office, and arrange appointment times when no other staff will be nearby.
More important, even highly experienced practitioners should not assume that their skills will transfer from in-person to remote caregiver training without specialized training. As discussed throughout this paper, practitioners training caregivers via video conferencing likely will encounter some unique challenges. For example, practitioners may find it difficult to detect caregivers’ nonverbal cues and, as described previously, to train caregivers effectively with limited ability to use model, gesture, and physical prompts. Practitioners who are interested in providing telehealth services should receive training and supervision from someone with demonstrated success in training caregivers remotely.
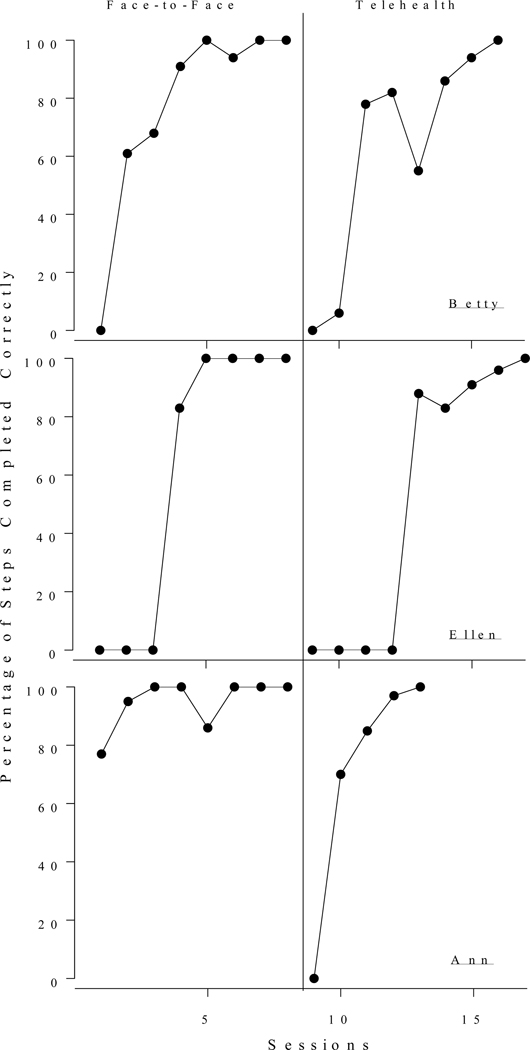
To assess these challenges more directly, two of the authors evaluated the extent to which practitioners’ fluency in face-to-face (i.e., in-person) caregiver training would generalize to caregiver training via the telehealth modality. Three in-practice BCBAs participated. The practitioners were all women between the ages of 27 and 28 years who had been practicing behavior analysts for 2 years. The trainer used a fidelity checklist (consisting of 14 core items) across modalities. The checklist included items such as “takes data on caregiver fidelity with procedures” and “concludes meeting with a recap of key concepts and next steps.” The telehealth fidelity checklist included the following nine supplemental steps specific to telehealth: (1) provides caregiver with a phone number to call in case of difficulty connecting and/or has a number for reaching the caregiver, (2) checks for a stable connection to internet prior to session (e.g., ensures direct line connected to the computer), (3) checks that speaker, mic, and camera are operational prior to session, (4) prepares room for optimal visibility and professionalism (e.g., adjusting lighting and removing distracting stimuli from camera view), (5) prepares environment for confidentiality (e.g., closes door of office), (6) begins video conference with a check of systems (e.g., “can you see and hear me ok?”), (7) provides extra time during pauses to allow for processing, response time, etc., compounded with internet delays during the videoconference, (8) provides enhanced verbal descriptions (given limited ability to model procedures), and (9) makes modifications to limit reactivity as necessary (e.g., texting as back-up communication, turning off camera, turning off video for observations, etc.). A step was marked as “prompted” if the BCBA required corrective feedback or modeling and “independent” if the BCBA completed the step without corrective feedback or modeling
A BCBA-D trainer first trained the BCBAs concurrently while they provided services to clients via the in-person modality. The trainer provided immediate feedback and modeling contingent on an incorrect or omitted step to ensure the families received quality services. Once all BCBAs completed all steps independently for a minimum of two consecutive sessions, the BCBAs initiated services to clients via telehealth while the trainer continued to provide immediate feedback and modeling. Figure 7 shows the percentage of steps completed independently for each BCBA across the training sessions. After the BCBAs reached the mastery criterion in the face-to-face modality, the percentage of steps completed independently dropped to 0% in the first telehealth session for all BCBAs. The BCBAs required additional training while providing services to clients in the telehealth modality to regain their prior levels of procedural fidelity. Interobserver agreement, collected for 37% of training sessions, averaged 92% (range, 70% – 100%). These findings provide support for our recommendation that practitioners seek additional training and supervision when initiating telehealth services with clients.
Figure 7.
Percentage of steps completed correctly for each BCBA across training sessions with face-to-face and telehealth modalities
Final Recommendations
We conclude with several additional strategies that practitioners may find helpful when providing telehealth services. One essential recommendation is to schedule an initial troubleshooting session with new clients before beginning services. To increase the efficiency of this initial appointment, practitioners might send the caregiver guidelines for selecting and preparing the location for the session; for ensuring that they have the necessary hardware, software, and internet speed; for positioning the camera and other equipment; and for gathering necessary materials (e.g., selecting highly preferred toys) in advance of the appointment. The goals of the initial appointment are to detect and resolve potential technological problems (e.g., adequacy of internet speed, compatibility of hardware and software), interferences with remote viewing (e.g., camera position, size of room), and likely disruptions in the client or host environments (e.g., presence of other family members). This initial appointment also may be beneficial for reducing the reactivity of the client and caregiver to the audio and video feed prior to formal data collection.
The practitioner may find it most efficient to work with the caregiver alone during the initial part of this troubleshooting appointment. The practitioner can discuss the terms of service, secure consent, identify clinical goals, resolve technical issues, and evaluate the location for the sessions. Following this, observations of the caregiver with the client in the selected location permits the practitioner to further troubleshoot potential challenges, such as difficulties viewing behavior or frequent client elopement from the location. For these initial observations, caregivers might engage in play or leisure activities with the client and complete assessments that help inform treatment planning. For example, the practitioner could coach the caregiver to conduct a preference assessment with the client. Although practitioners may not accomplish as much in terms of clinical service as compared to their typical, initial in-person appointments, they should be able to gather much of the information that is important for effective service provision.
We also recommend that practitioners modify their typical terms of service and consent forms to address issues that may arise when providing services via telehealth. These issues, discussed previously, include expectations about the activities and roles of the caregiver and practitioner during each scheduled appointment; agreements regarding the care, use, and return of loaned equipment; potential limitations of remote coaching (e.g., greater reliance on vocal instructions); and potential limits to confidentiality.
Several other strategies may help the practitioner manage technological issues. An IT professional who is available to assist with problems as they arise can help minimize treatment delays, becoming an invaluable member of the clinical team. Practitioners also should consider remaining in phone contact with caregivers during appointments to ensure adequate communication despite problems with technology. Finally, we recommend that practitioners video record all sessions, a capability that is available with some video conferencing software or with stand-alone screen recording software. By doing so, practitioners will have access to sessions for review and data collection purposes. These back-up recordings may be invaluable if practitioners are unable to attend to certain features of the appointment while troubleshooting issues with caregivers.
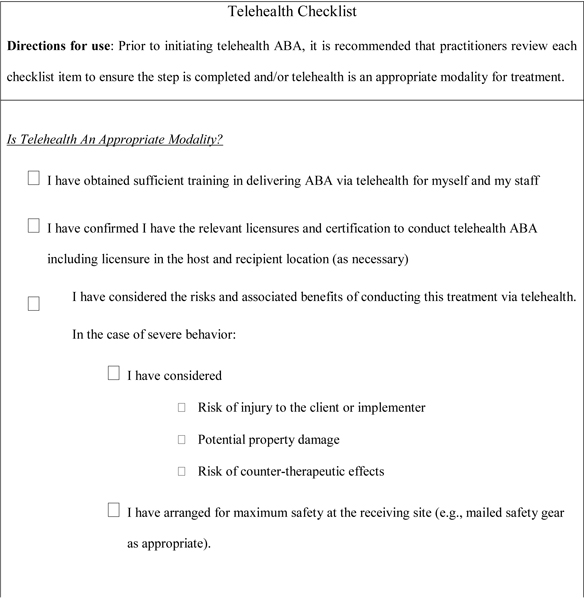
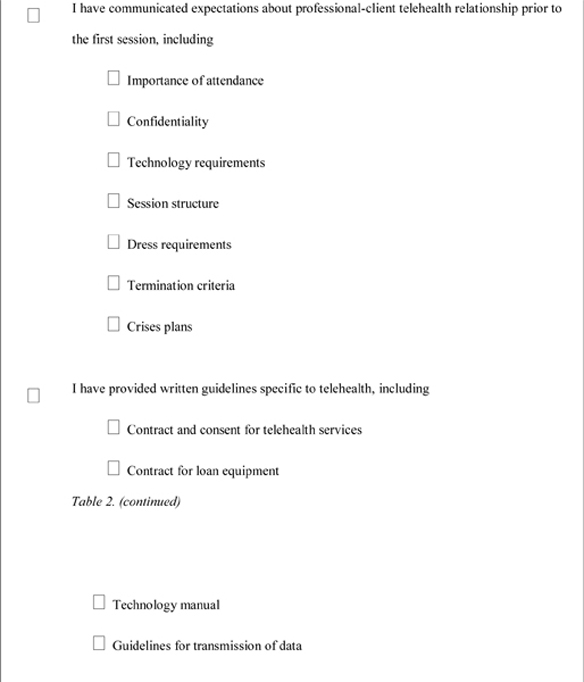
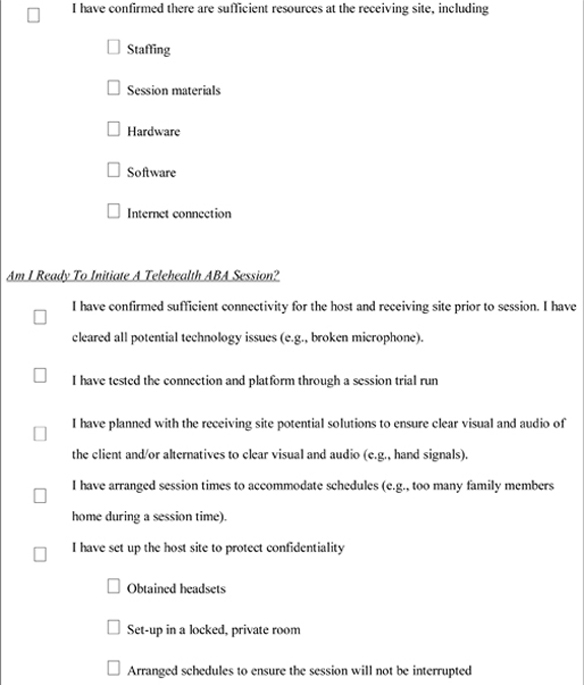
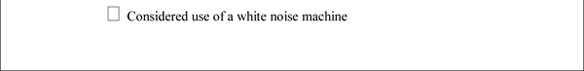
In Table 2, we provide a potential checklist for practitioners that summarizes many of the recommendations and considerations discussed in this paper. Practitioners might find it helpful to consult or complete this checklist prior to initiating telehealth services with clients.
Table 2.
Telehealth Checklist
|
|
|
|
Concluding Comments
An emerging literature suggests that remote coaching of caregivers is a promising approach for disseminating behavior-analytic interventions to individuals with autism and other developmental disabilities (Boisvert et al., 2010; Ferguson, Craig, & Dounavi, 2019; Neely et al., 2017; Tomlinson et al., 2018). Given the benefits of telehealth, a growing number of practitioners are likely to incorporate this modality into their clinical services. Nonetheless, reviews of research on telehealth-based services, including remote coaching of caregiver via video conferencing, suggest that the empirical basis for this approach is still in its infancy.
Authors have described the methodological quality of this research as “low” and noted that clinicians did not achieve positive outcomes for all clients and caregivers (e.g., Ferguson et al., 2019; Neely et al., 2017). These findings are not necessarily indicative of problems with remote coaching per se, as studies have not reported universally positive outcomes with in-person training (e.g., Wacker et al., 1998; see Lang, Machalicek, Rispoli, Regester, 2009; Patterson et al., 2012, for reviews). Furthermore, few studies have directly compared remote and in-person coaching (see Hay-Hansson & Eldevik, 2013, Lindgren et al., 2016; Sump, Richman, Schaefer, Grubb, & Brewer, 2018, for examples).
It is clear, however, that further research is needed on potential issues that could arise during remote coaching and on strategies to resolve them. Our potential solutions were not always successful. For some families, we needed to employ multiple strategies before resolving an issue. Although we plan to report our clinical outcomes elsewhere, 88% of families (range, 82% – 94% across the sites) receiving telehealth services across a 4 –year period met their goals despite these challenges. As such, the anecdotal description of challenges and solutions in this paper may be helpful for guiding further research, which, in turn, should guide the development of training curricula for practitioners. Although practitioners may benefit from greater knowledge of potential difficulties, our preliminary work with in-service BCBAs suggests that practitioners will need specific, hands-on training to provide these services effectively. The field also might benefit from research on a variety of contextual variables (e.g., socioeconomic status, family size, level of parental stress, geographic location) that could impact the success of telehealth-based parent training services.
Ultimately, further research on the outcomes of telehealth services may indicate that some caregivers and clients will not benefit from this approach, or that they may only benefit under certain conditions. For example, practitioners may find that telehealth services for some caregivers are only successful after the caregiver has received a certain amount of in-person training. If so, studies will be needed to determine the conditions under which telehealth services should and should not be prescribed for families of individuals with autism and other developmental disabilities.
Acknowledgments
Funding: This work was supported in whole or part by grants from the National Institutes of Mental Health (Award # R01MH104363) and the Texas Higher Education Coordinating Board (THECB) Autism Grant Program (Awards #17126, 20275). The opinions and conclusions expressed in this document are those of the authors and do not necessarily represent the opinions or policy of NIH or the THECB.
We thank Lauren Witthart, Ansley Reich, Naomi Alphonso, & Claire Wolken for their assistance with various aspects of this project.
Footnotes
Compliance with Ethical Standards:
Ethical approval: All procedures performed in this study with human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Boisvert M, Lang R, Andrianopoulos M, & Boscardin ML (2010). Telepractice in the assessment and treatment of individuals with autism spectrum disorders: A systematic review. Developmental Neurorehabilitation, 13, 423–432. doi: 10.3109/17518423.2010.499889 [DOI] [PubMed] [Google Scholar]
- Call NA, Zangrillo AN, Delfs CH, & Findley AJ (2013). A comparison of brief functional analyses with and without consequences. Behavioral Interventions, 28, 22–39. doi: 10.1002/bin.1353 [DOI] [Google Scholar]
- Derby KM, Wacker DP, Berg W, DeRaad A, Ulrich S, Asmus J, …Stoner EA (1997). The long- term effects of functional communication training in home settings. Journal of Applied Behavior Analysis, 30, 507–531. doi: 10.1901/jaba.1997.30-507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson J, Craig EA, & Dounavi K. (2019). Telehealth as a model for providing applied behaviour analytic interventions to individuals with autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders, 49, 582–616. doi: 10.1007/s10803-018-3724-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagopian LP, Crockett JL, Van Stone M, DeLeon IG, & Bowman LG (2000). Effects of noncontingent reinforcement on problem behavior and stimulus engagement: The role of satiation, extinction, and alternative reinforcement. Journal of Applied Behavior Analysis, 33, 433–449. doi: 10.1901/jaba.2000.33-433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay-Hansson AW, & Eldevik S. (2013). Training discrete trials teaching skills using videoconference. Research in Autism Spectrum Disorders, 7, 1300–1309. doi: 10.1016/j.rasd.2013.07.022 [DOI] [Google Scholar]
- Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, & Richman GS (1982/1994). Toward a functional analysis of self-injury. Journal of Applied Behavior Analysis, 27, 197–209. doi: 10.1901/jaba/1994.27-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang R, Machalicek W, Rispoli M, & Regester A. (2009). Training parents to implement communication interventions for children with autism spectrum disorders (ASD): A systematic review. Evidence-Based Communication Assessment and Intervention, 3, 174–190. Doi: 10.1080/17489530903338861 [DOI] [Google Scholar]
- Lee JF, Schieltz KM, Suess AN, Wacker DP, Romani PW, Lindgren SD, …Padilla Dalmau, Y. C. (2015). Guidelines for developing telehealth services and troubleshooting problems with telehealth technology when coaching parents to conduct functional analyses and functional communication training in their homes. Behavior Analysis in Practice, 8, 190–200. doi: 10.1007/s40617-014-0031-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindgren S, Wacker D, Suess A, Schieltz K, Pelzel K, Kopelman T, …Waldron D. (2016). Telehealth and autism: Treating challenging behavior at lower cost. Pediatrics, 137(S2), S167–S175. doi: 10.1542/peds.2015-2851O [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maglione MA, Gans D, Das L, Timbie J, & Kasari C. (2012). Non-medical interventions for children with ASD: Recommended guidelines and further research needs. Pediatrics, 130(S2), S169–S178. doi: 10.1542/peds.2012-0900O [DOI] [PubMed] [Google Scholar]
- Neely L, Rispoli M, Gerow S, Hong E, Hagan-Burke S. (2017). Fidelity outcomes for autism-focused interventionists coached via telepractice: A systematic literature review. Journal of Developmental and Physical Disabilities, 29, 849–874. doi: 10.1007/s10882-017-9550-4 [DOI] [Google Scholar]
- Nevill RE, Lecavalier L, & Stratis EA (2018). Meta-analysis of parent-mediated interventions for young children with autism spectrum disorder. Autism, 22, 84–98. doi: 10.1177/1362361316677838 [DOI] [PubMed] [Google Scholar]
- Parsons MB, Rollyson JH, & Reid DH (2012). Evidence-based staff training: A guide for practitioners. Behavior Analysis in Practice, 5, 2–11. doi: 10.1007/BF03391819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson SY, Smith V, & Mirenda P. (2012). A systematic review of training programs for parents of children with autism spectrum disorders: Single subject contributions. Autism, 16, 498–522. doi: 10.1177/1362361311413398 [DOI] [PubMed] [Google Scholar]
- Peterson KM, Piazza CC, Luczynski. K. C., & Fisher, W. W. (2017). Virtual-care delivery of applied behavior analysis services to children with autism spectrum disorder and related conditions. Behavior Analysis: Research and Practice, 17, 286–297. doi: 10.1037/bar0000030 [DOI] [Google Scholar]
- Phaneuf L, & McIntyre LL (2007). Effects of individualized video feedback combined with group parent training on inappropriate maternal behavior. Journal of Applied Behavior Analysis, 40, 737–741. doi: 10.1901/jaba.2007.737-741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard JS, Karimi KA, & Ficcaglia MB (2017). Ethical considerations in the design and implementation of a telehealth service delivery model. Behavior Analysis: Research and Practice, 17, 298–311. doi: 10.1037/bar0000053 [DOI] [Google Scholar]
- Reese RJ, Slone NC, Soares N, & Sprang R. (2015). Using telepsychology to provide a group parenting program: A preliminary evaluation of effectiveness. Psychological Services, 12, 274–282. doi: 10.1037/ser0000018 [DOI] [PubMed] [Google Scholar]
- Rios D, Kazemi E, & Peterson SM (2018). Best practices and considerations for effective service provision via remote technology. Behavior Analysis: Research and Practice, 18, 277–287. doi: 10.1037/bar0000072 [DOI] [Google Scholar]
- Romani PW, & Schieltz KM (2017). Ethical considerations when delivering behavior analytic services for problem behavior via telehealth. Behavior Analysis: Research and Practice, 17, 312–324. doi: 10.1037/bar0000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schieltz KM, Romani PW, Wacker DP, Suess AN, Huang P, Berg WK, … Kopelman TG (2018). Single-case analysis to determine reasons for failure of behavioral treatment via telehealth. Remedial and Special Education, 39, 95–105. doi: 10.1177/0741932517743791 [DOI] [Google Scholar]
- Schreibman L. (2000). Intensive behavioral/psychoeducational treatments for autism: Research needs and future directions. Journal of Autism and Developmental Disorders, 30, 373–378. doi: 10.1023/A:1005535120023 [DOI] [PubMed] [Google Scholar]
- Smith T, Eikeseth S, Klevstrand M, & Lovaas OI (1997). Intensive behavioral treatment for preschoolers with severe mental retardation and pervasive developmental disorder. American Journal on Mental Retardation, 102, 238–249. doi: [DOI] [PubMed] [Google Scholar]
- Sump LA, Richman DM, Schaefer AM, Grubb LM, & Brewer AT (2018). Telehealth and in-person training outcomes for novice discrete trial training therapists. Journal of Applied Behavior Analysis, 51, 466–481. doi: 10.1002/jaba.461 [DOI] [PubMed] [Google Scholar]
- Tomlinson SRL, Gore N. & McGill P. (2018). Training individuals to implement applied behavior analytic procedures via telehealth: A systematic review of the literature. Journal of Behavioral Education, 27, 172–222. doi: 10.1007/s10864-018-9292-0 [DOI] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, …Waldron DB (2013a). Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. Journal of Developmental and Physical Disabilities, 25, 35–48. doi: 10.1007/s10882-012-9314-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Lee JF, Padilla Dalmau YC, Kopelman TG, Lindgren SD, Kuhle J, …Waldron DB (2013b). Conducting functional analyses of problem behavior via telehealth. Journal of Applied Behavior Analysis, 46, 31–46. doi: 10.1002/jaba.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, & Healy A. (1998). Evaluation and long-term treatment of aberrant behavior displayed by young children with disabilities. Journal of Developmental and Behavioral Pediatrics, 19, 260–266. doi: 10.1097/00004703-199808000-00004 [DOI] [PubMed] [Google Scholar]
- Xie Y, Dixon JF, Yee OM, Zhang J, Chen YA, Deangelo S, …Schweitzer JB (2013). A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemedicine and e-health, 19, 192–199. doi: 10.1089/tmj.2012.0108 [DOI] [PubMed] [Google Scholar]
- Zarcone JR, Iwata BA, Vollmer TR, Jagtiani S, Smith RG, & Mazaleski JL (1993). Extinction of self- injurious escape behavior with and without instructional fading. Journal of Applied Behavior Analysis, 26, 353–360. doi: 10.1901/jaba.1993.26-353 [DOI] [PMC free article] [PubMed] [Google Scholar]