Abstract
The 17-beta-hydroxysteroid dehydrogenase type 3 (17-β-HSD3) enzyme converts androstenedione to testosterone and is encoded by the HSD17B3 gene. Homozygous or compound heterozygous HSD17B3 mutations block the synthesis of testosterone in the fetal testis, resulting in a Disorder of Sex Development (DSD). We describe a child raised as a female in whom the discovery of testes in the inguinal canals led to a genetic study by whole exome sequencing (WES) and to the identification of a compound heterozygous mutation of the HSD17B3 gene (c.608C>T, p.Ala203Val, and c.645A>T, p.Glu215Asp). Furthermore, we review all HSD17B3 mutations published so far in cases of 17-β-HSD3 deficiency. A total of 70 different HSD17B3 mutations have so far been reported in 239 patients from 187 families. A total of 118 families had homozygous mutations, 63 had compound heterozygous mutations and six had undetermined genotypes. Mutations occurred in all 11 exons and were missense (55%), splice-site (29%), small deletions and insertions (7%), nonsense (5%), and multiple exon deletions and duplications (2%). Several mutations were recurrent and missense mutations at codon 80 and the splice-site mutation c.277+4A>T each represented 17% of all mutated alleles. These findings may be useful to those involved in the clinical management and genetic diagnosis of this disorder.
Keywords: 17-beta-hydroxysteroid dehydrogenase type 3, HSD17B3, Disorder of Sex Development (DSD), pseudohermaphroditism, mutation
1. Introduction
17-beta-hydroxysteroid dehydrogenase type 3 (17-β-HSD3) deficiency (OMIM: 264300) is a rare autosomal recessive Disorder of Sex Development (DSD) [1]. 17-β-HSD3 is encoded by the HSD17B3 gene (chromosome 9q22.32) and expressed in the testis where it converts the inactive steroid androstenedione to the active androgen testosterone [2]. Homozygous or compound heterozygous HSD17B3 mutations block the synthesis of testosterone in the fetal testis, resulting in undervirilized genitalia in 46,XY newborns [3]. The clinical phenotype may range from the normal female appearance of the external genitalia to various degrees of genital ambiguity, including microphallus with hypospadias [1,4,5]. Due to normal anti-Mullerian hormone (AMH) secretion, patients lack Mullerian structures (uterus, fallopian tubes, cervix, and the upper part of the vagina), whereas Wolffian derivatives (epididymis, vas deferens, and seminal vesicles) are often normally developed and testes are located in the inguinal canal. As female external genitalia is common at birth, these children are usually assigned the female gender and raised as such [1,4,5]. The diagnosis may occur in childhood due to mild clitoromegaly, urogenital sinus or inguinal hernia with testes present along the inguinal canals or labioscrotal folds [1,4,5]. At the expected time of puberty, severe virilization usually occurs due to the significant increase in the testicular secretion of androstenedione that can presumably be partially converted to testosterone by 17-β-HSD3 residual activity or by other isoenzymes [6,7]. Thus, diagnosis before puberty allows early treatment by the removal of the abnormal testes, which should prevent the clinical signs of marked virilization.
The phenotype of 17-β-HSD3 deficiency is often clinically indistinguishable from other DSDs, namely that of androgen insensitivity syndrome and 5-α-reductase type 2 deficiency [8]. Measurements of basal and human chorionic gonadotropin (hCG)-stimulated levels of sex steroids, their precursors, and metabolites can help distinguish between these defects [8]. However, these biochemical studies are not always conclusive and molecular genetic studies can be used for a definitive diagnosis [9,10,11].
We present a case of DSD in whom a definitive diagnosis of 17-β-HSD3 deficiency was established only after whole exome sequencing (WES) revealed a compound heterozygous mutation of the HSD17B3 gene. Furthermore, we present an update on all HSD17B3 mutations reported so far in the literature.
2. Results
2.1. Clinical Studies
The patient was the first-born daughter of non-consanguineous Portuguese healthy parents. The pregnancy was uneventful and she was born full-term by Cesarean section with a weight, length, and head circumference of 2800 g, 49 cm, and 34 cm, respectively. She had normal development until the age of 5 years, when she was brought to medical attention due to an enlargement of the clitoris (approximately 2 cm length) and the presence of small bilateral inguinal masses. No other signs of virilization or pubertal development were present. A pelvic ultrasound exam and laparoscopy revealed the absence of uterus and ovaries. A biopsy of the inguinal masses revealed the presence of testicular tissue. A chromosomal analysis of peripheral blood revealed a male 46,XY karyotype. A 3-day human chorionic gonadotropin (hCG) stimulation test was performed, and this showed an increase in testosterone and dihydrotestosterone (DHT) plasma levels (Table 1). The testosterone to DHT ratio was normal. Androstenedione levels were not measured. A provisional clinical diagnosis of male pseudohermaphroditism due to partial androgen insensitivity was made. At this time, a genetic test through sequencing of the AR (Androgen Receptor) and the SRD5A2 (Steroid 5-Alpha-Reductase 2) genes revealed no coding sequence mutations. The child and her parents received psychological counselling and it was decided that she would maintain a female gender identity. At the age of 6 years, the child underwent bilateral orchiectomy and corrective surgery for the clitoromegaly. At the age of 12 years, she initiated transdermal estrogen therapy for the induction of puberty. She maintained normal growth and development and was last observed at the age of 18 years when she was referred for vaginoplasty due to short (~3 cm) vaginal length. There was no known family history of DSD.
Table 1.
Baseline and hCG-stimulated plasma hormone levels.
| Day 1 (Baseline) | Day 2 | Day 4 | |
|---|---|---|---|
| Total testosterone | <1 ng/dL (NR: 1–20) |
11.3 ng/dL | 36.9 ng/dL |
| DHT | 2.8 ng/dL (NR: 1.5–5.4) |
3.2 ng/dL | 6.0 ng/dL |
| T/DHT ratio | 0.4 (NR: <10) |
3.5 | 6.2 |
| SHBG | 85.8 nmol/L (NR: 48–142) |
88.6 nmol/L | 91.8 nmol/L |
| 3α-Androstanediol | 0.6 ng/mL (NR: 0.2–3.8) |
0.5 ng/mL | 1.0 ng/mL |
| Estradiol | <5 pg/mL (NR: <22) |
<5 pg/mL | <5 pg/mL |
| Estrone | 3.9 pg/mL (NR: <25) |
3.1 pg/mL | 5.8 pg/mL |
| FSH | 1.7 IU/L (NR: 0.25–1.92) |
- | - |
| LH | 0.1 IU/L (NR: 0.02–1.03) |
- | - |
The stimulation test consisted of subcutaneous administration of human chorionic gonadotropin (hCG) 2000 IU/day, during 3 consecutive days. NR, normal range values for males of same age (based on the laboratory-specific reference ranges for the pediatric population at the time of hormone measurements); T, total testosterone; DHT, dihydrotestosterone; SHBG, sex hormone-binding globulin; FSH, follicle-stimulating hormone; LH, luteinizing hormone.
2.2. Genetic Studies
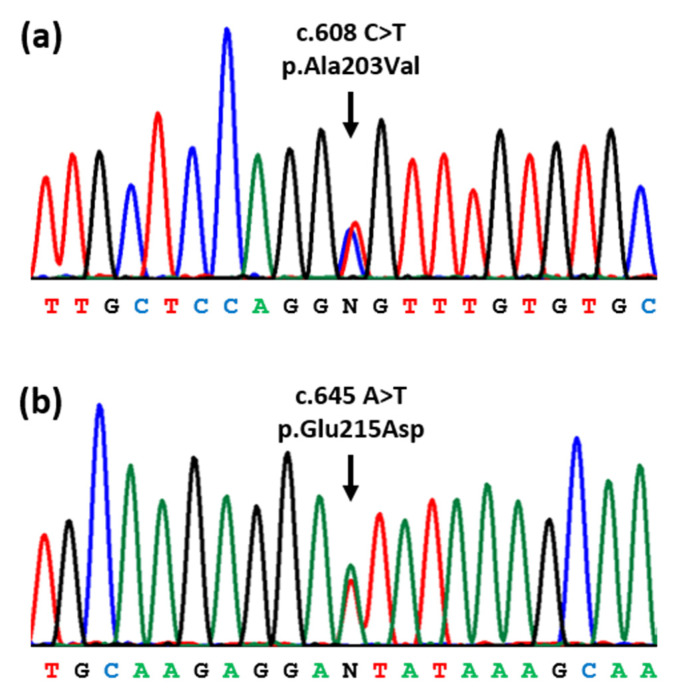
Due to the negative findings upon sequencing the AR and SRD5A2 genes, the genetic studies were completed by WES, followed by the analysis of a virtual panel of genes that were previously associated with DSDs [11]. This revealed that the patient was a compound heterozygote for two missense variants in exon 9 of the HSD17B3 gene (Figure 1). These variants consisted of NM_000197.2:c.608C>T, which changed an alanine to a valine at amino acid position 203 (p.Ala203Val), and NM_000197.2:c.645A>T, which changed a glutamic acid to an aspartic acid at amino acid position 215 (p.Glu215Asp). Both variants fulfilled the American College of Medical Genetics and Genomics (ACMG) criteria for “Pathogenic” [12] and have been reported as causative mutations in patients with 17-β-HSD3 deficiency [3,13].
Figure 1.
Partial DNA sequence of the 17-beta-hydroxysteroid dehydrogenase 3 (HSD17B3) gene. The patient was found to be compound heterozygous for two missense mutations (arrows) in exon 9: (a) NM_000197.2:c.608C>T, p.Ala203Val; (b) NM_000197.2:c.645A>T, p.Glu215Asp.
2.3. Mutations Reported in the Literature
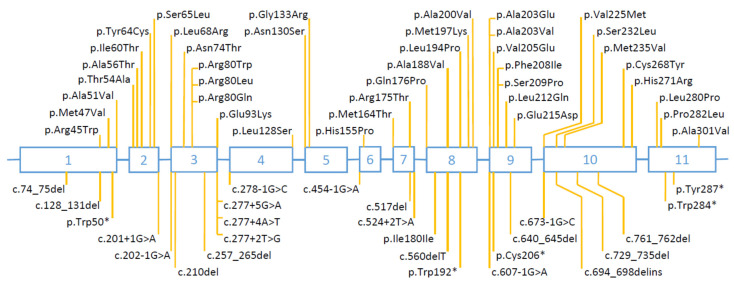
Sixty-eight articles reported one or more patients with HSD17B3 mutations (Supplemental Table S1) [1,3,4,5,9,10,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74]. A total of 187 families (239 patients) were reported, of which 118 had homozygous mutations, 63 had compound heterozygous mutations and six had heterozygous mutations without data on the second mutation. In the 187 families (374 alleles), the types of mutations were missense (55%), splice-site (29%), small deletions and insertions (7%), nonsense (5%), and multiple exon deletions and duplications (2%). Mutations were distributed across all 11 exons (Figure 2). Many mutations were recurrent (i.e., shared by two or more families) and some occurred at unusually high frequencies: missense mutations at codon 80 and the splice-site mutation c.277+4A>T, each represented 17% of all mutated alleles. Altogether, there have been a total of 70 different HSD17B3 mutations reported so far in the literature (Supplemental Table S1).
Figure 2.
Location of mutations reported in the literature. Open boxes (numbered 1 to 11) represent coding exons of the 17-beta-hydroxysteroid dehydrogenase 3 (HSD17B3) gene and intervening horizontal lines represent introns (not drawn to scale). Missense mutations are depicted above the gene structure and all other mutations are represented below. Gross rearrangements (whole exon deletions and duplications) are not represented. Please refer to Supplemental Table S1 for further details.
3. Discussion
We describe the clinical course and laboratory findings of a child with DSD in whom a genetic analysis revealed 17-β-HSD3 deficiency. The differential diagnosis with other similar 46,XY DSDs requires a high level of clinical suspicion and laboratory evaluation of the different hormones, their precursors, and metabolites that characterize each disorder, with confirmation by a molecular mutation analysis [8].
Patients with 17-β-HSD3 deficiency can vary in the appearance of their external genitals, which may be due to different residual enzyme activities [1,4,5]. In most cases, the 46,XY neonate presents apparently normal external female genitalia and is raised as a female [1,4,5]. In patients with lumps in the inguinal canals or labioscrotal folds, the palpation of gonads may lead to an early diagnosis, similar to our patient. If undiagnosed, these patients usually present during puberty with primary amenorrhea and varying degrees of virilization [1,4,5]. Timely removal of the gonads will prevent the virilization and risk of gonadal malignancy [75]. These clinical characteristics are similar to those of other conditions, such as partial androgen insensitivity syndrome and 5-α-reductase type 2 deficiency; therefore, misdiagnosis is not unusual for this disease [9,27,51,53,62,64,68,70]. In 17-β-HSD3 deficiency, the conversion of androstenedione to testosterone is reduced, leading to a decreased testosterone/androstenedione ratio [76]. Unfortunately, androstenedione measurements were not included in the investigation protocol at the time of the evaluation of our patient, and this led to a delay in the exact diagnosis. Furthermore, the increase in testosterone in response to hCG stimulation led to an erroneous diagnosis of partial androgen insensitivity. It was only after negative testing for AR and SRD5A2 mutations that other genetic causes were searched by a WES analysis. This allowed the identification of a compound heterozygous mutation in HSD17B3, which led to a final diagnosis of 17-β-HSD3 deficiency.
The p.Ala203Val and p.Glu215Asp mutations identified in our patient have already been reported as pathogenic in the literature [3,13], although this is the first time that both have been found in the same patient. Previous functional studies by site-directed mutagenesis and transfection into cultured mammalian cells demonstrated that these mutations completely abolish the enzyme’s ability to convert androstenedione to testosterone [3,13]. This contrasts with other mutations, such as the common p.Arg80Gln mutation, that were shown to maintain some residual activity [3,13], and this may explain the phenotypic variability observed among patients.
17-β-HSD3 deficiency is a rare disorder and only 187 families (239 patients) have been reported along with their causative mutations (Supplemental Table S1). A total of 70 different HSD17B3 mutations have been reported so far in the literature. However, many of these were shared by several families, suggesting the existence of either mutational hotspots or founder effects. In particular, the common p.Arg80Gln mutation has been found almost exclusively in patients originating from the Mediterranean and Middle East regions, and the common c.277+4A>T mutation has been found predominantly in patients originating from western Europe (Supplemental Table S1). Haplotype analyses of the chromosomal region of the HSD17B3 gene have suggested that these mutations are ancient and originate from genetic founders [70]. Reported mutations were most frequently missense (55%), followed by splice-site (29%), small deletions and insertions (7%), nonsense (5%), and gross rearrangements (2%). These are all expected to lead to loss of function of the 17-β-HSD3 enzyme. Interestingly, two families were reported to have partial gene duplications [51,56], although it remains to be elucidated how these affect the enzyme activity.
In conclusion, we present a case of DSD due to 17-β-HSD3 deficiency in whom the genetic diagnosis was established through a WES analysis. We also present a comprehensive list of all published HSD17B3 mutations that may be of use to those involved in the clinical management and genetic diagnosis of this disorder.
4. Materials and Methods
The genetic studies were approved by the Institutional Ethics Committee of the Faculty of Health Sciences, University of Beira Interior, Covilha, Portugal (Ref: CE-FCS-2013-017). Written informed consent was obtained from the patient’s legal guardian. Genomic deoxyribonucleic acid (DNA) was extracted from the peripheral blood leucocytes of the patient and used for a WES analysis. Targeted enrichment was performed using the Agilent V6 Exon Kit (Agilent Technologies, Santa Clara, CA, USA), and the target regions were sequenced on a DNBSEQ sequencing platform (BGI Tech Solutions, Hong Kong) with paired-end reads of 100 bp and 100 × raw read coverage. The reads were mapped to the human reference genome GRCh37/hg19 using the Burrows–Wheeler Aligner (BWA-MEM, v0.7.17) software [77,78]. Variant calling and annotation was performed using the Genome Analysis Toolkit v3.5 (GATK, v4.1.4.1) [79,80]. Variants were selected if they were cumulatively: (a) located in genes previously associated with DSDs [11]; (b) located in coding exons or adjacent splice sites; (c) non-synonymous; and (d) absent or rare (population frequency <0.1%) in the Genome Aggregation Database (gnomAD) [81]. Pathogenic variants were confirmed by conventional Sanger sequencing using a CEQ DTCS sequencing kit (Beckman Coulter, Fullerton, CA, USA) and an automated capillary DNA sequencer (GenomeLab TM GeXP, Genetic Analysis System, Beckman Coulter, Fullerton, CA, USA).
Published HSD17B3 germline mutations were identified by searching the PubMed database (National Center for Biotechnology Information, U.S. National Library of Medicine, National Institutes of Health) (https://www.ncbi.nlm.nih.gov/pubmed, accessed on 9 June 2022) for articles, using the keywords “mutation” combined with “HSD17B3” or “17 beta hydroxysteroid dehydrogenase 3”. Reference lists of articles were also searched to identify further articles. The articles were analyzed for evidence of data duplication and patients that had been included in previous mutation studies were excluded from the analysis. Each published mutation was checked for accuracy by comparison to the HSD17B3 wild-type sequence. Errors due to the incorrect assignment of nucleotide or codon numbers, or translation errors between codon and amino acid residues were corrected whenever possible. The mutations shown only at the amino acid level were converted to single-nucleotide changes when it was possible to predict the altered base using the genetic code. When more than one nucleotide change could account for the amino acid change or when other ambiguous changes were indicated, the precise mutation was considered unavailable. The numbering of each nucleotide was changed, whenever necessary, to comply with current recommendations for mutation nomenclature [41], whereby nucleotide +1 was the A of the ATG-translation initiation codon. The mutations were described in relation to the HSD17B3 cDNA reference sequence (GenBank accession number NM_000197.2).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms231710026/s1.
Author Contributions
Conceptualization, M.C.L.; investigation, C.I.G., J.C. and M.B.; resources, M.B.; writing—original draft preparation, M.C.L.; writing—review and editing, C.I.G., J.C. and M.B.; supervision, M.C.L.; project administration, M.C.L.; funding acquisition, M.C.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Faculty of Health Sciences, University of Beira Interior, Portugal (reference CE-FCS-2013-017, approved 12 June 2013).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Portuguese Foundation for Science and Technology (FCT, project grant UIDB/00709/2020), and by Programa Operacional Regional do Centro (project grants CENTRO-08-5864-FSE-000039 and CENTRO-01-0145-FEDER-000019).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mendonca B.B., Gomes N.L., Costa E.M., Inacio M., Martin R.M., Nishi M.Y., Carvalho F.M., Tibor F.D., Domenice S. 46,XY disorder of sex development (DSD) due to 17beta-hydroxysteroid dehydrogenase type 3 deficiency. J. Steroid Biochem. Mol. Biol. 2017;165:79–85. doi: 10.1016/j.jsbmb.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Andersson S. 17 beta-hydroxysteroid dehydrogenase: Isozymes and mutations. J. Endocrinol. 1995;146:197–200. doi: 10.1677/joe.0.1460197. [DOI] [PubMed] [Google Scholar]
- 3.Geissler W.M., Davis D.L., Wu L., Bradshaw K.D., Patel S., Mendonca B.B., Elliston K.O., Wilson J.D., Russell D.W., Andersson S. Male pseudohermaphroditism caused by mutations of testicular 17 beta-hydroxysteroid dehydrogenase 3. Nat. Genet. 1994;7:34–39. doi: 10.1038/ng0594-34. [DOI] [PubMed] [Google Scholar]
- 4.George M.M., New M.I., Ten S., Sultan C., Bhangoo A. The clinical and molecular heterogeneity of 17betaHSD-3 enzyme deficiency. Horm. Res. Paediatr. 2010;74:229–240. doi: 10.1159/000318004. [DOI] [PubMed] [Google Scholar]
- 5.Yang Z., Ye L., Wang W., Zhao Y., Wang W., Jia H., Dong Z., Chen Y., Wang W., Ning G., et al. 17beta-Hydroxysteroid dehydrogenase 3 deficiency: Three case reports and a systematic review. J. Steroid Biochem. Mol. Biol. 2017;174:141–145. doi: 10.1016/j.jsbmb.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 6.Rosler A., Belanger A., Labrie F. Mechanisms of androgen production in male pseudohermaphroditism due to 17 beta-hydroxysteroid dehydrogenase deficiency. J. Clin. Endocrinol. Metab. 1992;75:773–778. doi: 10.1210/jcem.75.3.1325474. [DOI] [PubMed] [Google Scholar]
- 7.Werner R., Kulle A., Sommerfeld I., Riepe F.G., Wudy S., Hartmann M.F., Merz H., Dohnert U., Bertelloni S., Holterhus P.M., et al. Testosterone synthesis in patients with 17beta-hydroxysteroid dehydrogenase 3 deficiency. Sex. Dev. 2012;6:161–168. doi: 10.1159/000336605. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed S.F., Achermann J., Alderson J., Crouch N.S., Elford S., Hughes I.A., Krone N., McGowan R., Mushtaq T., O’Toole S., et al. Society for Endocrinology UK Guidance on the initial evaluation of a suspected difference or disorder of sex development (Revised 2021) Clin. Endocrinol. 2021;95:818–840. doi: 10.1111/cen.14528. [DOI] [PubMed] [Google Scholar]
- 9.Lee Y.S., Kirk J.M., Stanhope R.G., Johnston D.I., Harland S., Auchus R.J., Andersson S., Hughes I.A. Phenotypic variability in 17beta-hydroxysteroid dehydrogenase-3 deficiency and diagnostic pitfalls. Clin. Endocrinol. 2007;67:20–28. doi: 10.1111/j.1365-2265.2007.02829.x. [DOI] [PubMed] [Google Scholar]
- 10.Khattab A., Yuen T., Yau M., Domenice S., Frade Costa E.M., Diya K., Muhuri D., Pina C.E., Nishi M.Y., Yang A.C., et al. Pitfalls in hormonal diagnosis of 17-beta hydroxysteroid dehydrogenase III deficiency. J. Pediatr. Endocrinol. Metab. 2015;28:623–628. doi: 10.1515/jpem-2014-0295. [DOI] [PubMed] [Google Scholar]
- 11.Delot E.C., Vilain E. Towards improved genetic diagnosis of human differences of sex development. Nat. Rev. Genet. 2021;22:588–602. doi: 10.1038/s41576-021-00365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richards S., Aziz N., Bale S., Bick D., Das S., Gastier-Foster J., Grody W.W., Hegde M., Lyon E., Spector E., et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015;17:405–424. doi: 10.1038/gim.2015.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andersson S., Geissler W.M., Wu L., Davis D.L., Grumbach M.M., New M.I., Schwarz H.P., Blethen S.L., Mendonca B.B., Bloise W., et al. Molecular genetics and pathophysiology of 17 beta-hydroxysteroid dehydrogenase 3 deficiency. J. Clin. Endocrinol. Metab. 1996;81:130–136. doi: 10.1210/jcem.81.1.8550739. [DOI] [PubMed] [Google Scholar]
- 14.von Spreckelsen B., Aksglaede L., Johannsen T.H., Nielsen J.E., Main K.M., Jorgensen A., Jensen R.B. Prepubertal and pubertal gonadal morphology, expression of cell lineage markers and hormonal evaluation in two 46,XY siblings with 17beta-hydroxysteroid dehydrogenase 3 deficiency. J. Pediatr. Endocrinol. Metab. 2022;35 doi: 10.1515/jpem-2021-0713. [DOI] [PubMed] [Google Scholar]
- 15.Rafigh M., Salmaninejad A., Sorouri Khorashad B., Arabi A., Milanizadeh S., Hiradfar M., Abbaszadegan M.R. Novel Deleterious Mutation in Steroid-5alpha-Reductase-2 in 46, XY Disorders of Sex Development: Case Report Study. Fetal Pediatr. Pathol. 2022;41:141–148. doi: 10.1080/15513815.2020.1745974. [DOI] [PubMed] [Google Scholar]
- 16.Globa E., Zelinska N., Shcherbak Y., Bignon-Topalovic J., Bashamboo A., Msmall es C.K. Disorders of Sex Development in a Large Ukrainian Cohort: Clinical Diversity and Genetic Findings. Front. Endocrinol. 2022;13:810782. doi: 10.3389/fendo.2022.810782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garcia A., Legendre M., Chantot-Bastaraud S., Siffroi J.P., Christin-Maitre S. Unravelling a case of 46,XY DSD due to 17ss-Hydroxysteroid Dehydrogenase type 3 mutations at the age of 49. Ann. Endocrinol. 2022 doi: 10.1016/j.ando.2022.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Cocchetti C., Baldinotti F., Romani A., Ristori J., Mazzoli F., Vignozzi L., Maggi M., Fisher A.D. A Novel Compound Heterozygous Mutation of HSD17B3 Gene Identified in a Patient With 46,XY Difference of Sexual Development. Sex. Med. 2022;10:100522. doi: 10.1016/j.esxm.2022.100522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ciftci N., Kayas L., Camtosun E., Akinci A. 46,XY Sex Development Defect due to a Novel Homozygous (Splice Site) c.673_1G>C Variation in the HSD17B3 Gene: Case Report. J. Clin. Res. Pediatr. Endocrinol. 2022;14:233–238. doi: 10.4274/jcrpe.galenos.2020.2020.0249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu S., Zheng B., Liu T., Zhu Z., Gu W., Liu Q. 17 beta-hydroxysteroid dehydrogenase 3 deficiency due to novel compound heterozygous variants of HSD17B3 gene in a sib pair. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2021;38:787–790. doi: 10.3760/cma.j.cn511374-20200527-00392. [DOI] [PubMed] [Google Scholar]
- 21.Manyas H., Eroglu Filibeli B., Ayranci I., Guvenc M.S., Dundar B.N., Catli G. Early and late diagnoses of 17beta-Hydroxysteroid dehydrogenase type-3 deficiency in two unrelated patients. Andrologia. 2021;53:e14017. doi: 10.1111/and.14017. [DOI] [PubMed] [Google Scholar]
- 22.Ea V., Bergougnoux A., Philibert P., Servant-Fauconnet N., Faure A., Breaud J., Gaspari L., Sultan C., Paris F., Kalfa N. How Far Should We Explore Hypospadias? Next-generation Sequencing Applied to a Large Cohort of Hypospadiac Patients. Eur. Urol. 2021;79:507–515. doi: 10.1016/j.eururo.2020.12.036. [DOI] [PubMed] [Google Scholar]
- 23.De Falco L., Piscopo C., D’Angelo R., Evangelista E., Suero T., Sirica R., Ruggiero R., Savarese G., Di Carlo A., Furino G., et al. Detection of 46, XY Disorder of Sex Development (DSD) Based on Plasma Cell-Free DNA and Targeted Next-Generation Sequencing. Genes. 2021;12:1890. doi: 10.3390/genes12121890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ata A., Ozen S., Onay H., Uzun S., Goksen D., Ozkinay F., Ozbaran N.B., Ulman I., Darcan S. A large cohort of disorders of sex development and their genetic characteristics: 6 novel mutations in known genes. Eur. J. Med Genet. 2021;64:104154. doi: 10.1016/j.ejmg.2021.104154. [DOI] [PubMed] [Google Scholar]
- 25.Alswailem M., Alsagheir A., Abbas B.B., Alzahrani O., Alzahrani A.S. Molecular genetics of disorders of sex development in a highly consanguineous population. J. Steroid Biochem. Mol. Biol. 2021;208:105736. doi: 10.1016/j.jsbmb.2020.105736. [DOI] [PubMed] [Google Scholar]
- 26.Levy-Khademi F., Zeligson S., Lavi E., Klopstock T., Chertin B., Avnon-Ziv C., Abulibdeh A., Renbaum P., Rosen T., Perlberg-Bengio S., et al. The novel founder homozygous V225M mutation in the HSD17B3 gene causes aberrant splicing and XY-DSD. Endocrine. 2020;69:650–654. doi: 10.1007/s12020-020-02327-z. [DOI] [PubMed] [Google Scholar]
- 27.Faienza M.F., Baldinotti F., Marrocco G., TyuTyusheva N., Peroni D., Baroncelli G.I., Bertelloni S. 17beta-hydroxysteroid dehydrogenase type 3 deficiency: Female sex assignment and follow-up. J. Endocrinol. Investig. 2020;43:1711–1716. doi: 10.1007/s40618-020-01248-y. [DOI] [PubMed] [Google Scholar]
- 28.Hughes L.A., McKay-Bounford K., Webb E.A., Dasani P., Clokie S., Chandran H., McCarthy L., Mohamed Z., Kirk J.M.W., Krone N.P., et al. Next generation sequencing (NGS) to improve the diagnosis and management of patients with disorders of sex development (DSD) Endocr. Connect. 2019;8:100–110. doi: 10.1530/EC-18-0376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galli-Tsinopoulou A., Serbis A., Kotanidou E.P., Litou E., Dokousli V., Mouzaki K., Fanis P., Neocleous V., Skordis N. 46,XY Disorder of Sex Development due to 17-Beta Hydroxysteroid Dehydrogenase Type 3 Deficiency in an Infant of Greek Origin. J. Clin. Res. Pediatr. Endocrinol. 2018;10:74–78. doi: 10.4274/jcrpe.4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yu B., Liu Z., Mao J., Wang X., Zheng J., Xiong S., Cui M., Ma W., Huang Q., Xu H., et al. Novel mutations of HSD17B3 in three Chinese patients with 46,XY Disorders of Sex Development. Steroids. 2017;126:1–6. doi: 10.1016/j.steroids.2017.07.009. [DOI] [PubMed] [Google Scholar]
- 31.Ozen S., Onay H., Atik T., Solmaz A.E., Ozkinay F., Goksen D., Darcan S. Rapid Molecular Genetic Diagnosis with Next-Generation Sequencing in 46,XY Disorders of Sex Development Cases: Efficiency and Cost Assessment. Horm. Res. Paediatr. 2017;87:81–87. doi: 10.1159/000452995. [DOI] [PubMed] [Google Scholar]
- 32.Hiort O., Marshall L., Birnbaum W., Wunsch L., Holterhus P.M., Dohnert U., Werner R. Pubertal Development in17Beta-Hydroxysteroid Dehydrogenase Type 3 Deficiency. Horm. Res. Paediatr. 2017;87:354–358. doi: 10.1159/000453613. [DOI] [PubMed] [Google Scholar]
- 33.Engeli R.T., Tsachaki M., Hassan H.A., Sager C.P., Essawi M.L., Gad Y.Z., Kamel A.K., Mazen I., Odermatt A. Biochemical Analysis of Four Missense Mutations in the HSD17B3 Gene Associated With 46,XY Disorders of Sex Development in Egyptian Patients. J. Sex. Med. 2017;14:1165–1174. doi: 10.1016/j.jsxm.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 34.de Calais F.L., Smith L.D., Raponi M., Maciel-Guerra A.T., Guerra-Junior G., de Mello M.P., Baralle D. A study of splicing mutations in disorders of sex development. Sci. Rep. 2017;7:16202. doi: 10.1038/s41598-017-16296-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bertalan R., Admoni O., Bashamboo A., Tenenbaum-Rakover Y., McElreavey K. A novel HSD17B3 gene mutation in a 46,XY female-phenotype newborn identified by whole-exome sequencing. Clin. Endocrinol. 2017;87:407–408. doi: 10.1111/cen.13396. [DOI] [PubMed] [Google Scholar]
- 36.Ben Rhouma B., Kallabi F., Mahfoudh N., Ben Mahmoud A., Engeli R.T., Kamoun H., Keskes L., Odermatt A., Belguith N. Novel cases of Tunisian patients with mutations in the gene encoding 17beta-hydroxysteroid dehydrogenase type 3 and a founder effect. J. Steroid Biochem. Mol. Biol. 2017;165:86–94. doi: 10.1016/j.jsbmb.2016.03.007. [DOI] [PubMed] [Google Scholar]
- 37.Hassan H.A., Mazen I., Gad Y.Z., Ali O.S., Mekkawy M., Essawi M.L. Mutational Profile of 10 Afflicted Egyptian Families with 17-beta-HSD-3 Deficiency. Sex. Dev. 2016;10:66–73. doi: 10.1159/000445311. [DOI] [PubMed] [Google Scholar]
- 38.Grimbly C., Caluseriu O., Metcalfe P., Jetha M.M., Rosolowsky E.T. 46,XY disorder of sex development due to 17-beta hydroxysteroid dehydrogenase type 3 deficiency: A plea for timely genetic testing. Int. J. Pediatr. Endocrinol. 2016;2016:12. doi: 10.1186/s13633-016-0030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Engeli R.T., Rhouma B.B., Sager C.P., Tsachaki M., Birk J., Fakhfakh F., Keskes L., Belguith N., Odermatt A. Biochemical analyses and molecular modeling explain the functional loss of 17beta-hydroxysteroid dehydrogenase 3 mutant G133R in three Tunisian patients with 46, XY Disorders of Sex Development. J. Steroid Biochem. Mol. Biol. 2016;155:147–154. doi: 10.1016/j.jsbmb.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 40.Eggers S., Sadedin S., van den Bergen J.A., Robevska G., Ohnesorg T., Hewitt J., Lambeth L., Bouty A., Knarston I.M., Tan T.Y., et al. Disorders of sex development: Insights from targeted gene sequencing of a large international patient cohort. Genome Biol. 2016;17:243. doi: 10.1186/s13059-016-1105-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.den Dunnen J.T., Dalgleish R., Maglott D.R., Hart R.K., Greenblatt M.S., McGowan-Jordan J., Roux A.F., Smith T., Antonarakis S.E., Taschner P.E. HGVS Recommendations for the Description of Sequence Variants: 2016 Update. Hum. Mutat. 2016;37:564–569. doi: 10.1002/humu.22981. [DOI] [PubMed] [Google Scholar]
- 42.Tuhan H.U., Anik A., Catli G., Ceylaner S., Dundar B., Bober E., Abaci A. A novel missense mutation in HSD17B3 gene in a 46, XY adolescent presenting with primary amenorrhea and virilization at puberty. Clin. Chim. Acta. 2015;438:154–156. doi: 10.1016/j.cca.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 43.Sagsak E., Aycan Z., Savas-Erdeve S., Keskin M., Cetinkaya S., Karaer K. 17betaHSD-3 enzyme deficiency due to novel mutations in the HSD17B3 gene diagnosed in a neonate. J. Pediatr. Endocrinol. Metab. 2015;28:957–959. doi: 10.1515/jpem-2014-0354. [DOI] [PubMed] [Google Scholar]
- 44.Phelan N., Williams E.L., Cardamone S., Lee M., Creighton S.M., Rumsby G., Conway G.S. Screening for mutations in 17beta-hydroxysteroid dehydrogenase and androgen receptor in women presenting with partially virilised 46,XY disorders of sex development. Eur. J. Endocrinol. 2015;172:745–751. doi: 10.1530/EJE-14-0994. [DOI] [PubMed] [Google Scholar]
- 45.Demir K., Yildiz M., Elmas O.N., Korkmaz H.A., Tunc S., Olukman O., Hazan F., Ozkan K.U., Ozkan B. Two different patterns of mini-puberty in two 46,XY newborns with 17beta-hydroxysteroid dehydrogenase type 3 deficiency. J. Pediatr. Endocrinol. Metab. 2015;28:961–965. doi: 10.1515/jpem-2014-0365. [DOI] [PubMed] [Google Scholar]
- 46.Baxter R.M., Arboleda V.A., Lee H., Barseghyan H., Adam M.P., Fechner P.Y., Bargman R., Keegan C., Travers S., Schelley S., et al. Exome sequencing for the diagnosis of 46,XY disorders of sex development. J. Clin. Endocrinol. Metab. 2015;100:E333–E344. doi: 10.1210/jc.2014-2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Al-Sinani A., Mula-Abed W.A., Al-Kindi M., Al-Kusaibi G., Al-Azkawi H., Nahavandi N. A Novel Mutation Causing 17-beta-Hydroxysteroid Dehydrogenase Type 3 Deficiency in an Omani Child: First Case Report and Review of Literature. Oman. Med. J. 2015;30:129–134. doi: 10.5001/omj.2015.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alikasifoglu A., Vuralli D., Hiort O., Gonc N., Ozon A., Kandemir N. Severe Undervirilisation in a 46,XY Case Due to a Novel Mutation in HSD17B3 Gene. J. Clin. Res. Pediatr. Endocrinol. 2015;7:249–252. doi: 10.4274/jcrpe.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ellaithi M., Werner R., Riepe F.G., Krone N., Kulle A.E., Diab T., Kamel A.K., Arlt W., Holterhus P.M., Sabir O., et al. 46,XY disorder of sex development in a sudanese patient caused by a novel mutation in the HSD17B3 gene. Sex. Dev. 2014;8:151–155. doi: 10.1159/000363201. [DOI] [PubMed] [Google Scholar]
- 50.Costa C., Castro-Correia C., Mira-Coelho A., Monteiro B., Monteiro J., Hughes I., Fontoura M. The dilemma of the gender assignment in a Portuguese adolescent with disorder of sex development due to 17beta-hydroxysteroid-dehydrogenase type 3 enzyme deficiency. Endocrinol. Diabetes. Metab. Case. Rep. 2014;2014:140064. doi: 10.1530/EDM-14-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Massanyi E.Z., Gearhart J.P., Kolp L.A., Migeon C.J. Novel mutation among two sisters with 17beta hydroxysteroid dehydrogenase type 3 deficiency. Urology. 2013;81:1069–1071. doi: 10.1016/j.urology.2012.12.024. [DOI] [PubMed] [Google Scholar]
- 52.Hassan H.A., Mazen I., Gad Y.Z., Ali O.S., Mekkawy M., Essawi M.L. A novel nonsense mutation in exon 1 of HSD17B3 gene in an Egyptian 46,XY adult female presenting with primary amenorrhea. Sex. Dev. 2013;7:277–281. doi: 10.1159/000351822. [DOI] [PubMed] [Google Scholar]
- 53.Chuang J., Vallerie A., Breech L., Saal H.M., Alam S., Crawford P., Rutter M.M. Complexities of gender assignment in 17beta-hydroxysteroid dehydrogenase type 3 deficiency: Is there a role for early orchiectomy? Int. J. Pediatr. Endocrinol. 2013;2013:15. doi: 10.1186/1687-9856-2013-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ben Rhouma B., Belguith N., Mnif M.F., Kamoun T., Charfi N., Kamoun M., Abdelhedi F., Hachicha M., Kamoun H., Abid M., et al. A novel nonsense mutation in HSD17B3 gene in a Tunisian patient with sexual ambiguity. J. Sex. Med. 2013;10:2586–2589. doi: 10.1111/j.1743-6109.2012.02763.x. [DOI] [PubMed] [Google Scholar]
- 55.Russo G., di Lascio A., Ferrario M., Meroni S., Hiort O., Chiumello G. 46,XY karyotype in a female phenotype fetus: A challenging diagnosis. J. Pediatr. Adolesc. Gynecol. 2012;25:e77–e79. doi: 10.1016/j.jpag.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 56.Neocleous V., Sismani C., Shammas C., Efstathiou E., Alexandrou A., Ioannides M., Argyrou M., Patsalis P.C., Phylactou L.A., Skordis N. Duplication of exons 3-10 of the HSD17B3 gene: A novel type of genetic defect underlying 17beta-HSD-3 deficiency. Gene. 2012;499:250–255. doi: 10.1016/j.gene.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 57.Castro C.C., Guaragna-Filho G., Calais F.L., Coeli F.B., Leal I.R., Cavalcante-Junior E.F., Monlleo I.L., Pereira S.R., Silva R.B., Gabiatti J.R., et al. Clinical and molecular spectrum of patients with 17beta-hydroxysteroid dehydrogenase type 3 (17-beta-HSD3) deficiency. Arq. Bras. Endocrinol. Metabol. 2012;56:533–539. doi: 10.1590/S0004-27302012000800012. [DOI] [PubMed] [Google Scholar]
- 58.Alikasifoglu A., Hiort O., Gonc N., Demirbilek H., Isik E., Kandemir N. 17beta-hydroxysteroid dehydrogenase type 3 deficiency as a result of a homozygous 7 base pair deletion in 17betaHSD3 gene. J. Pediatr. Endocrinol. Metab. 2012;25:561–563. doi: 10.1515/jpem-2012-0009. [DOI] [PubMed] [Google Scholar]
- 59.Omrani M.D., Adamovic T., Grandell U., Saleh-Gargari S., Nordenskjold A. 17-beta-hydroxysteroid dehydrogenase type 3 deficiency in three adult Iranian siblings. Sex. Dev. 2011;5:273–276. doi: 10.1159/000335006. [DOI] [PubMed] [Google Scholar]
- 60.George M.M., Sinha S., Mamkin I., Philibert P., New M.I., Wilson R.C., Sultan C., Ten S., Bhangoo A. Isolated mild clitoral hypertrophy may reveal 46,XY disorders of sex development in infancy due to 17betaHSD-3 defect confirmed by molecular analysis. Gynecol. Endocrinol. 2011;27:890–894. doi: 10.3109/09513590.2010.544134. [DOI] [PubMed] [Google Scholar]
- 61.Mueller O.T., Coovadia A. Novel human pathological mutations. Gene symbol: HSD17B3. Disease: 17 beta-hydroxysteroid dehydrogenase-3 deficiency. Hum. Genet. 2009;125:335. [PubMed] [Google Scholar]
- 62.Bertelloni S., Balsamo A., Giordani L., Fischetto R., Russo G., Delvecchio M., Gennari M., Nicoletti A., Maggio M.C., Concolino D., et al. 17beta-Hydroxysteroid dehydrogenase-3 deficiency: From pregnancy to adolescence. J. Endocrinol. Invest. 2009;32:666–670. doi: 10.1007/BF03345738. [DOI] [PubMed] [Google Scholar]
- 63.Mains L.M., Vakili B., Lacassie Y., Andersson S., Lindqvist A., Rock J.A. 17beta-hydroxysteroid dehydrogenase 3 deficiency in a male pseudohermaphrodite. Fertil. Steril. 2008;89:228 e213-227. doi: 10.1016/j.fertnstert.2007.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bertelloni S., Maggio M.C., Federico G., Baroncelli G., Hiort O. 17beta-hydroxysteroid dehydrogenase-3 deficiency: A rare endocrine cause of male-to-female sex reversal. Gynecol. Endocrinol. 2006;22:488–494. doi: 10.1080/09513590600921358. [DOI] [PubMed] [Google Scholar]
- 65.Bel J., Mainou A., Blanco J.A., Bilbao J.R. [Male pseudohermaphroditism due to 17 beta-hydroxysteroid dehydrogenase deficiency] Med. Clin. 2003;120:795. doi: 10.1016/S0025-7753(03)73848-2. [DOI] [PubMed] [Google Scholar]
- 66.Twesten W., Johannisson R., Holterhus P.M., Hiort O. [Severe 46,XY virilization deficit due to 17beta-hydroxysteroid dehydrogenase deficiency] Klin. Padiatr. 2002;214:314–315. doi: 10.1055/s-2002-34015. [DOI] [PubMed] [Google Scholar]
- 67.Lindqvist A., Hughes I.A., Andersson S. Substitution mutation C268Y causes 17 beta-hydroxysteroid dehydrogenase 3 deficiency. J. Clin. Endocrinol. Metab. 2001;86:921–923. doi: 10.1210/jcem.86.2.7172. [DOI] [PubMed] [Google Scholar]
- 68.Twesten W., Holterhus P., Sippell W.G., Morlot M., Schumacher H., Schenk B., Hiort O. Clinical, endocrine, and molecular genetic findings in patients with 17beta-hydroxysteroid dehydrogenase deficiency. Horm. Res. 2000;53:26–31. doi: 10.1159/000023509. [DOI] [PubMed] [Google Scholar]
- 69.Mendonca B.B., Inacio M., Arnhold I.J., Costa E.M., Bloise W., Martin R.M., Denes F.T., Silva F.A., Andersson S., Lindqvist A., et al. Male pseudohermaphroditism due to 17 beta-hydroxysteroid dehydrogenase 3 deficiency. Diagnosis, psychological evaluation, and management. Medicine. 2000;79:299–309. doi: 10.1097/00005792-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 70.Boehmer A.L., Brinkmann A.O., Sandkuijl L.A., Halley D.J., Niermeijer M.F., Andersson S., de Jong F.H., Kayserili H., de Vroede M.A., Otten B.J., et al. 17Beta-hydroxysteroid dehydrogenase-3 deficiency: Diagnosis, phenotypic variability, population genetics, and worldwide distribution of ancient and de novo mutations. J. Clin. Endocrinol. Metab. 1999;84:4713–4721. doi: 10.1210/jcem.84.12.6174. [DOI] [PubMed] [Google Scholar]
- 71.Moghrabi N., Hughes I.A., Dunaif A., Andersson S. Deleterious missense mutations and silent polymorphism in the human 17beta-hydroxysteroid dehydrogenase 3 gene (HSD17B3) J. Clin. Endocrinol. Metab. 1998;83:2855–2860. doi: 10.1210/jcem.83.8.5052. [DOI] [PubMed] [Google Scholar]
- 72.Can S., Zhu Y.S., Cai L.Q., Ling Q., Katz M.D., Akgun S., Shackleton C.H., Imperato-McGinley J. The identification of 5 alpha-reductase-2 and 17 beta-hydroxysteroid dehydrogenase-3 gene defects in male pseudohermaphrodites from a Turkish kindred. J. Clin. Endocrinol. Metab. 1998;83:560–569. doi: 10.1210/jcem.83.2.4535. [DOI] [PubMed] [Google Scholar]
- 73.Bilbao J.R., Loridan L., Audi L., Gonzalo E., Castano L. A novel missense (R80W) mutation in 17-beta-hydroxysteroid dehydrogenase type 3 gene associated with male pseudohermaphroditism. Eur. J. Endocrinol. 1998;139:330–333. doi: 10.1530/eje.0.1390330. [DOI] [PubMed] [Google Scholar]
- 74.Rosler A., Silverstein S., Abeliovich D. A (R80Q) mutation in 17 beta-hydroxysteroid dehydrogenase type 3 gene among Arabs of Israel is associated with pseudohermaphroditism in males and normal asymptomatic females. J. Clin. Endocrinol. Metab. 1996;81:1827–1831. doi: 10.1210/jcem.81.5.8626842. [DOI] [PubMed] [Google Scholar]
- 75.Morin J., Peard L., Saltzman A.F. Gonadal malignancy in patients with differences of sex development. Transl. Androl. Urol. 2020;9:2408–2415. doi: 10.21037/tau-19-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Faisal Ahmed S., Iqbal A., Hughes I.A. The testosterone:androstenedione ratio in male undermasculinization. Clin. Endocrinol. 2000;53:697–702. doi: 10.1046/j.1365-2265.2000.01166.x. [DOI] [PubMed] [Google Scholar]
- 77.Li H., Durbin R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics. 2009;25:1754–1760. doi: 10.1093/bioinformatics/btp324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li H., Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–595. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.DePristo M.A., Banks E., Poplin R., Garimella K.V., Maguire J.R., Hartl C., Philippakis A.A., del Angel G., Rivas M.A., Hanna M., et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 2011;43:491–498. doi: 10.1038/ng.806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.McKenna A., Hanna M., Banks E., Sivachenko A., Cibulskis K., Kernytsky A., Garimella K., Altshuler D., Gabriel S., Daly M., et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010;20:1297–1303. doi: 10.1101/gr.107524.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karczewski K.J., Francioli L.C., Tiao G., Cummings B.B., Alfoldi J., Wang Q., Collins R.L., Laricchia K.M., Ganna A., Birnbaum D.P., et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581:434–443. doi: 10.1038/s41586-020-2308-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request.