Abstract
Changes in tissue stiffness are associated with pathological conditions such as myofascial pain and increased risk of muscle injury. Furthermore, they have been shown to modify performance indicators such as running economy or jump height. Indentometry is an affordable way to assess tissue stiffness. However, to date, there is a paucity of studies examining the measurement properties of available devices. With this trial, we aimed to evaluate the reliability of the “IndentoPro”. Two investigators repeatedly measured the stiffness of the lateral head of the gastrocnemius muscle in healthy participants (N = 35), using 5 and 10 mm indentation depths. Intraclass Correlation Coefficients (ICC) revealed moderate inter-rater reliability (5 mm: ICC3,1 0.74, 95%CI = 0.54 to 0.86, p < 0.001; 10 mm: ICC3,1 0.59, 95%CI = 0.27 to 0.78, p < 0.001) and good intra-rater reliability (5 mm: ICC3,1 0.84, 95%CI = 0.71 to 0.92, p < 0.001; 10 mm: ICC3,1 0.83, 95%CI = 0.69 to 0.91, p < 0.001). No correlations between age, height, weight, BMI, skinfold thickness and myofascial tissue stiffness were observed (p > 0.5). In conclusion, the IndentoPro is reliable in assessing calf tissue stiffness, but the predictors of stiffness remain unclear.
Keywords: myofascial tissue, tissue stiffness, indentometry
1. Introduction
In recent years, soft tissue stiffness, the resistance of biological structures to an external deforming force [1,2,3,4,5], has attracted increasing interest among researchers and clinicians working with patients and athletes. This is mainly due to early evidence suggesting that the stiffness of the muscular and connective tissue may help identify pathological tissue states [1,2,6,7,8,9,10,11,12], monitor therapy or training effects [13,14,15,16,17,18] or prevent sports injury [19,20,21]. However, in the daily routine, most physiotherapists or trainers do not have access to sophisticated and complex measurement technologies (e.g., elastography) and thus, there is a need for straightforward and easy-to-handle devices capturing biomechanical soft tissue properties.
Indentometry is based on the standardized application of a compressive force deforming the underlying structures [22]. Using the amount of applied pressure and assessing the degree of indentation, it allows the calculation of tissue stiffness. A variety of handheld indentation devices [5,23,24,25,26,27,28,29] have been used for research purposes. All of them represent portable and relatively inexpensive means for measuring tissue mechanics in the clinical routine or during the training process. Validation studies have shown that indentometry devices are generally reliable in healthy individuals [5,24,25], but also in patients [23]. In an evaluation trial, Wilke et al. [5] examined the reliability and validity of a custom-made, handheld Semi-electronic Tissue Compliance Meter (STCM), concluding that this type of indentometry is an affordable, time- and cost-efficient method to evaluate the soft tissue properties of the lower leg. However, the device was not easily available to the public and hence, it is uncertain if commercial instruments may be able to reproduce the observed findings.
Building on the basis of said STCM [5], a new-generation device (IndentoPro, Technical University of Chemnitz, Germany and Fascia Research Project of Technical University of Munich, Germany) has been developed, which can measure soft tissue stiffness and elasticity with an indentometer function and the pressure–pain threshold with an algometer function at various indentation depths from 2 to 15 mm. However, to date, no study has examined the reliability of the IndentoPro even though it was already used in studies gauging the effect of interventions [30,31]. The present trial was therefore geared to elucidate its inter-rater and intra-rater reproducibility in assessing myofascial tissue stiffness.
Several definitions exist for the term “myofascial tissue”, with some authors emphasizing the importance of the intramuscular and intermuscular fascial tissue [12,32,33,34], while others weigh more the skeletal muscle [35,36,37,38,39,40] or both fascial and muscular tissue in conjunction [41]. In this study, we assume that the myofascial tissue is composed of the superficial fascia, deep fascia and the skeletal muscle with its connective tissue (e.g., endomysium, perimysium). The term myofascial tissue was also chosen because there is no ability to measure the stiffness of the muscle in complete isolation from other surrounding tissues when using indentometry. As the thickness of the subcutaneous connective tissue varies between different locations [42], it may influence indentometric measurements of myofascial stiffness. Besides investigating reliability, we therefore aimed to test whether correlations exist between skinfold thickness measured with a caliper and myofascial tissue stiffness measured with the IndentoPro, and/or between anthropometric data (gender, age, weight, height, BMI) and myofascial tissue stiffness.
2. Materials and Methods
2.1. Design and Ethics
A repeated measurements reliability study was prospectively registered in the German Registry of Clinical Trials (ID number DRKS00027417) and conducted in accordance with the Guidelines for Reporting Reliability and Agreement Studies (GGRAS) [43]. Briefly, using the IndentoPro, two investigators repeatedly assessed myofascial tissue stiffness of the calf at standardized intervals (see Section 2.3). Approval of the Ethics Committee of DIPLOMA University (approval number EB 1010/2021) was obtained. All procedures aligned with the principles of the Declaration of Helsinki and its recent modifications. Each of the participants provided written informed consent.
2.2. Participants
Healthy participants were recruited based on a convenience sampling technique [44]. The inclusion criteria were (1) willingness and (2) availability to participate in the. Exclusion criteria were based on those used by Wilke et al. [5], including trauma in lower extremity; surgery in lower extremity; orthopedic complaints and diseases in lower extremity; severe neurological, rheumatic, pulmonary or cardiovascular diseases; psychiatric disease; pregnancy; being in a nursing period; and painkiller intake in the past 48 h. Individuals were personally invited and recruited to take part in the study. Based on inclusion and exclusion criteria, N = 35 healthy subjects were recruited. Sample size selection was based on availability in this trial and hence did not represent the general population. However, the frequently recommended minimum of N > 30 was reached, which has been demonstrated to be sufficient to achieve statistical approximation to the standard normal distribution of the variables, and to achieve a validation of the study results [45,46].
2.3. Measurements
All measurements were conducted in a standardized manner and in constant environmental conditions (room temperature constant between 20° and 24° Celsius). Participants were examined in a closed investigation room, respecting the local COVID-19 pandemic regulations. All measurements, per participant, were carried out on the same day, in the dominant leg, and in the prone position. The dominance of the leg was determined by asking the question, “If you would shoot a ball on a target, which leg would you use to shoot the ball?”, as it is a reliable and fast method to determine leg dominance [47].
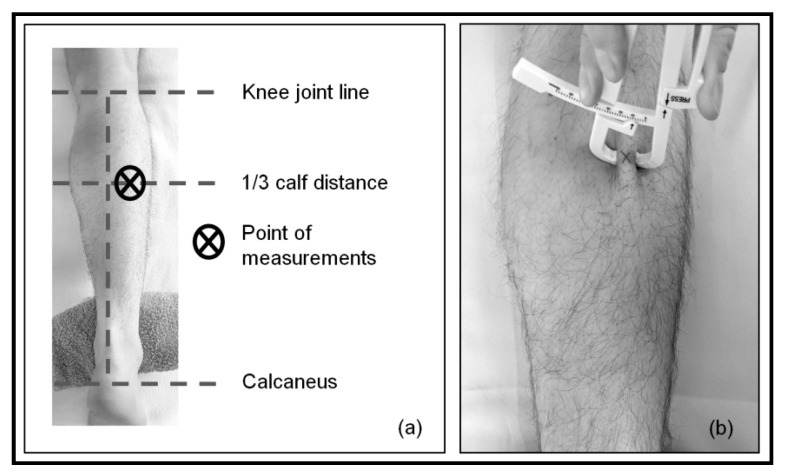
Measurements were performed on the lateral head of the gastrocnemius muscle, at one-third (cranially) of the distance between the knee joint line and the calcaneus. To ensure consistency, the measurement location was marked with a water-soluble marker. First, skinfold thickness was measured once with the skinfold caliper (Acczilla Personal Body Fat Tester, Acczilla, Hong Kong, China; Figure 1).
Figure 1.
Location of the measurements. (a) Determination of the measurement location: cranial 1/3 calf distance, lateral head of gastrocnemius muscle; (b) measurement of skinfold thickness with skinfold caliper at the point of measurements.
Skinfold measurements were conducted by one examiner. After the skinfold at the site of measurement was firmly pinched between the thumb and the index finger of the investigator’s non-dominant hand, the jaws of the skinfold caliper (hold with dominant hand) were placed over the skinfold. Pressure on a press handle was applied with the thumb of the examiner’s dominant hand until the arrow of the press handle matched the arrow on the gauge, and subsequently, pressure was released. The thickness values shown on the scale were registered and used for further analysis.
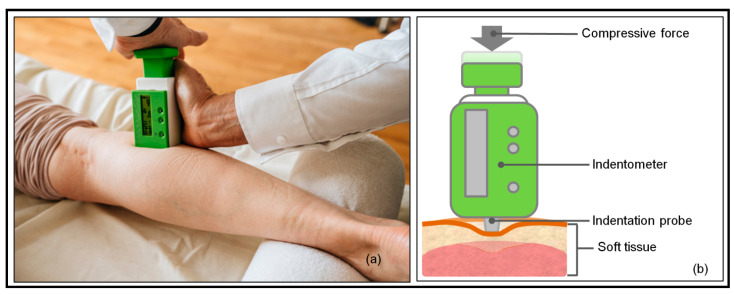
Subsequently, myofascial tissue stiffness measurements were performed. Indentation depth (5 and 10 mm) was chosen based on the possible thickness of the skin and subcutaneous connective tissue in the calf region [48,49,50], indicating that the indentation depth of at least 5 mm should be used when measuring myofascial tissue stiffness. Although the device is able to measure the stiffness up to 15 mm indentation depth, measurements at 15 mm indentation depth were not included in the current study since pilot testing revealed inconvenient sensations (close to pain) at that depth. Two raters with professional physiotherapist qualifications carried out the myofascial tissue stiffness measurements as illustrated in Figure 2.
Figure 2.
Myofascial tissue stiffness measurement with the IndentoPro. (a) Placement of the indentometer; (b) drawing of the stiffness measurement: after compressive force application, the indentation probe comes out of the indentometer body, indenting the soft tissue. The applied force (Newton) and resulting indentation depth (mm) are shown on a display.
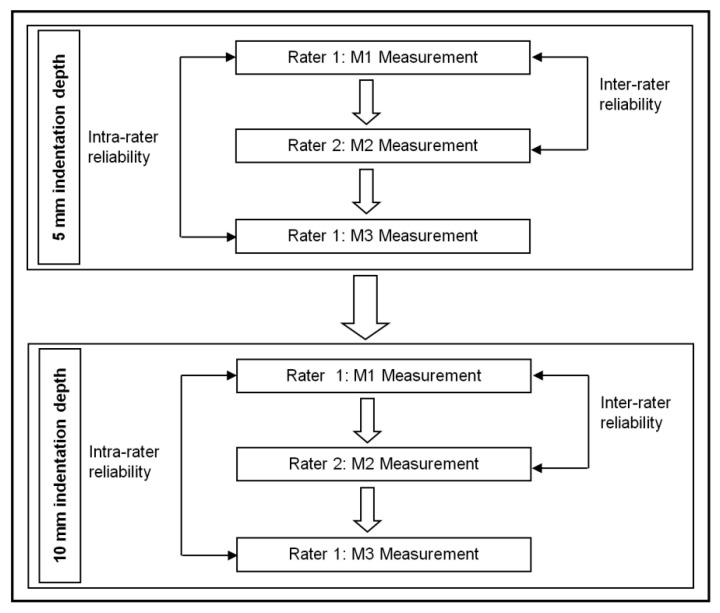
Three measurement sets were performed at both indentation depths (Figure 3). For each depth, the first rater performed the first (M1) and the last (M3) measurement set, while the second rater conducted the M2 measurements only. Each measurement set (M1 to M3) comprised 3 repetitions performed at 5 s intervals. Between the M1, M2 and M3 measurements, there was only a short break allowing for the change in raters. A 1 min break was used after all 5 mm indentation depth (M1, M2 and M3) measurements. Previous explorations confirmed that this amount of time between measurements was sufficient to avoid any noticeable viscoelastic adaptation processes (such as creep or hysteresis) due to repeated mechanical compression in this tissue region. Subsequently, the M1, M2 and M3 measurements were performed at a 10 mm indentation depth in the same sequence as the 5 mm indentation depth.
Figure 3.
Chart displaying the workflow of reliability testing.
A maximal coefficient of variation of 15% (calculated and displayed by the device itself) between the trials of each measurement set (M1 to M3) was used as a cut-off score to determine a valid measurement based on the guidelines of the tool producer. No measurement had to be excluded during the study based on that cut-off score. Intra-rater reliability was determined by comparing M1 and M3 measurements at 5 mm and 10 mm indentation depth (Rater 1). Inter-rater reliability was examined comparing M1 (Rater 1) and M2 (Rater 2) measurements at 5 mm and 10 mm indentation depths.
2.4. Data Analysis and Statistics
Arithmetic means, medians, standard deviations (SD) and the range of variability (extreme values) were calculated for the quantitative variables. For qualitative variables, the relative frequency of their occurrence (percentage) was used. All quantitative variables were checked for normality using the Shapiro–Wilk test [51,52].
Comparisons of the results obtained in M1, M2 and M3 of the stiffness measurements were performed using non-parametric Friedman tests as an alternative for repeated measures analysis of variance (ANOVA) in order to identify potential systematic differences [45,52,53]. Lin’s Concordance Correlation Coefficient (Lin’s CCC) and Intraclass Correlation Coefficient (ICC) were calculated to assess inter-rater reliability and intra-rater reliability [52,54,55,56,57,58]. A two-way mixed ICC model with the definition of absolute agreement and single-rating score (ICC3,1) was applied [59,60].
Standard errors of measurement (SEM) were estimated to determine the absolute reliability using the formula “SEM = Sp × √(1-ICC)” [53]. The pooled standard deviation (Sp was calculated as “Sp = √(n1 − 1)s12 + (n2 − 1)s22/(n1 + n2 − 2)” [61]. Bland–Altman plots provided visual information on how widely scores deviated from the mean and the extent of agreement, expecting that 95% of the difference scores would fall within ±1.96 SD [52,53,62,63].
To report the quantitative strength of associations between the variables such as skinfold thickness and myofascial tissue stiffness, anthropometric data and tissue stiffness, Spearman tests were chosen [52,53,64]. The significance level of α = 0.05 was assumed for all comparisons. Statistical analyses were performed using IBM SPSS Statistics 28.0 (IBM Corp, Armonk, NY, USA) and NCSS 2021 (NCSS, LLC, Kaysville, UT, USA).
3. Results
3.1. Study Group Characteristics
In total, n = 35 healthy individuals (11 females and 24 males) took part in the study. Detailed characteristics of the sample are presented in Table 1.
Table 1.
Sample characteristics and analysis of normal distribution.
| Variable | Mean | SD | Med | Q1 | Q3 | p-Value (Shapiro–Wilk) |
|---|---|---|---|---|---|---|
| Quantitative variable | ||||||
| Age, years | 26.6 | 12.6 | 21.0 | 19.0 | 27.0 | <0.001 |
| Height, m | 1.79 | 13.4 | 74.0 | 1.75 | 1.85 | 0.11 |
| Weight, kg | 74.8 | 0.09 | 1.79 | 65.0 | 85.0 | 0.68 |
| BMI, kg/m2 | 23.3 | 2.8 | 23.4 | 21.1 | 24.7 | 0.55 |
| Skinfold, mm | 12.6 | 4.7 | 12.0 | 8.0 | 16.0 | 0.053 |
| Quantitative variable | n | % | ||||
| Sex | Male | 24 | 69 | |||
| Female | 11 | 31 | ||||
| Dominant leg | Right | 33 | 94 | |||
| Left | 2 | 6 | ||||
SD—standard deviation; Med—median; Q1—first quartile; Q3—third quartile; BMI—body mass index; n—number of participants.
3.2. Reliability
Descriptive data are shown in Table 2. Analyses of testing assumptions revealed non-normality of the data in some cases.
Table 2.
Descriptive statistics and analysis of normal distribution for myofascial tissue stiffness measurements.
| Quantitative Variable | Mean | SD | Med | p-Value (Shapiro–Wilk) | |
|---|---|---|---|---|---|
| 5 mm indentation | M1, N/mm | 1.16 | 0.36 | 1.09 | 0.004 |
| M2, N/mm | 1.26 | 0.41 | 1.26 | 0.06 | |
| M3, N/mm | 1.12 | 0.30 | 1.16 | 0.01 | |
| 10 mm indentation | M1, N/mm | 3.40 | 1.38 | 3.22 | 0.16 |
| M2, N/mm | 2.80 | 1.24 | 2.39 | 0.002 | |
| M3, N/mm | 3.16 | 1.36 | 3.05 | 0.10 | |
SD—standard deviation; Med—median; M1—first measurement; M2—second measurement; M3—third measurement.
Since M1 and M3 measurements at 5 mm indentation and M2 measurements at 10 mm indentation showed a non-normal distribution (<0.05), Friedman tests were used to compare the measurements at 5 and 10 mm indentation depths. No significant differences (p < 0.001) were found between the different assessments of calf myofascial tissue stiffness, neither at 5 mm indentation (N = 35; Fr = 4.7; p = 0.95) nor 10 mm indentation depth (N = 35; Fr = 5.31; p = 0.70).
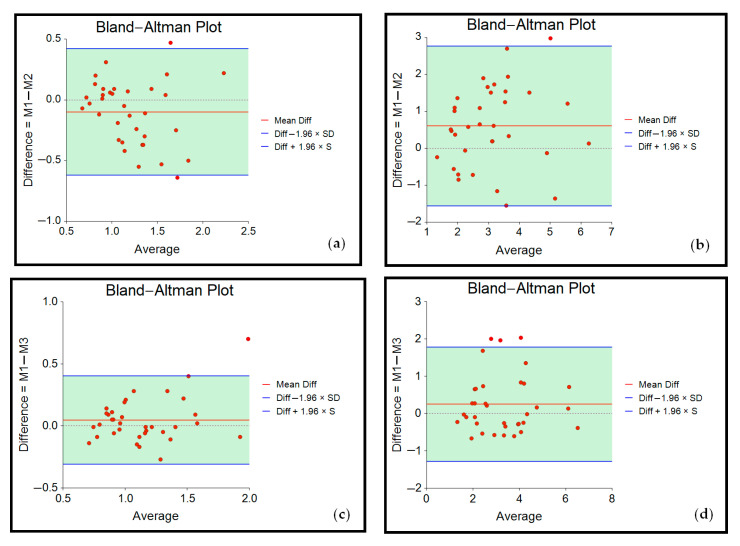
Bland–Altman plots depicting the respective measurements results are displayed below (Figure 4).
Figure 4.
Bland–Altman plots showing agreement of measurements for (a) M1 and M2 at 5 mm indentation depth; (b) M1 and M2 at 10 mm indentation depth; (c) M1 and M3 at 5 mm indentation depth; (d) M1 and M3 at 10 mm indentation depth.
Bland–Altman plots for inter-rater reliability (M1/M2, mean difference scores: −0.10 at 5 mm, 0.61 at 10 mm) and intra-rater reliability (M1/M3, mean difference scores: 0.05 at 5 mm, 0.25 at 10 mm) showed that the points were scattered in an unbiased pattern, with most of them falling within the limits of agreement.
Lin’s CCC (0.58 to 0.74, Table 3) indicated moderate inter-rater reliability (M1/M2) and substantial intra-rater reliability (M1/M3, 0.82 to 0.84) for both indentation depths. ICC3,1 analyses (Table 3) revealed almost identical results.
Table 3.
Inter-rater and intra-rater reliability of the IndentoPro in measuring tissue stiffness.
| Indentation Depth | M1/M2 (Inter-Rater) | M1/M3 (Intra-Rater) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lin’s CCC (95% CI) | MSE | ICC3,1 (95% CI) | p-Value | SEM | Lin’s CCC (95% CI) | MSE | ICC3,1 (95% CI) | p-Value | SEM | |
| 5 mm | 0.74 (0.55–0.85) |
0.05 | 0.74 (0.54–0.86) |
<0.001 | 0.20 | 0.84 (0.71–0.91) |
0.03 | 0.84 (0.71–0.92) |
<0.001 | 0.13 |
| 10 mm | 0.58 (0.34–0.75) |
1.14 | 0.59 (0.27–0.78) |
<0.001 | 0.88 | 0.82 (0.68–0.91) |
0.56 | 0.83 (0.69–0.91) |
<0.001 | 0.56 |
M1—first measurement; M2—second measurement; M3—third measurement; CCC—Concordance Correlation Coefficient; CI—confidence interval; MSE—mean square error; ICC—Intraclass Correlation Coefficient; SEM—standard error of measurement.
3.3. Correlation between Skinfold Thickness, Anthropometric Data and Tissue Stiffness
Correlation analyses of anthropometric data (e.g., sex, age, weight, height, BMI) and myofascial tissue stiffness, in most cases, did not reveal significant associations (p > 0.05). Likewise, there was no correlation between skinfold thickness and myofascial tissue stiffness (p > 0.05, Table 4).
Table 4.
Correlations between anthropometric data, skinfold thickness and myofascial tissue stiffness.
| Quantitative Variable |
Indentation Depth | M1 | M2 | M3 | |||
|---|---|---|---|---|---|---|---|
| rs | p-Value | rs | p-Value | rs | p-Value | ||
| Weight | 5 mm | 0.18 | 0.29 | 0.28 | 0.11 | 0.19 | 0.28 |
| 10 mm | 0.28 | 0.10 | 0.34 | 0.05 * | 0.21 | 0.23 | |
| Height | 5 mm | 0.3 | 0.82 | 0.20 | 0.25 | 0.26 | 0.13 |
| 10 mm | 0.13 | 0.47 | 0.08 | 0.65 | 0.13 | 0.47 | |
| BMI | 5 mm | 0.12 | 0.51 | 0.30 | 0.09 | 0.17 | 0.34 |
| 10 mm | 0.29 | 0.09 | 0.44 | 0.009 * | 0.17 | 0.32 | |
| Age | 5 mm | 0.03 | 0.86 | 0.08 | 0.64 | 0.04 | 0.80 |
| 10 mm | 0.06 | 0.77 | 0.08 | 0.63 | −0.08 | 0.67 | |
| Gender | 5 mm | 0.22 | 0.21 | 0.31 | 0.75 | 0.21 | 0.24 |
| 10 mm | 0.26 | 0.13 | 0.20 | 0.24 | 0.29 | 0.09 | |
| Skinfold thickness | 5 mm | −0.12 | 0.51 | −0.11 | 0.52 | −0.14 | 0.44 |
| 10 mm | 0.001 | 0.99 | −0.04 | 0.83 | −0.06 | 0.73 | |
* Significant at the 0.05 level (2-tailed). M1—first measurement; M2—second measurement; M3—third measurement; rs—Spearman’s rank correlation coefficient.
4. Discussion
The present study was the first to examine the reliability of the IndentoPro in the assessment of myofascial tissue stiffness. Our main finding is that the investigated device displays high reproducibility in repeated measurements by the same investigator and sufficient reproducibility when considering different investigators. With reference to intra-rater reliability, the results align closely with the previous study of Wilke et al. [5], who examined the previous generation of the IndentoPro. However, of note, contrarily to intra-rater reliability, inter-rater reliability values of the new device were slightly lower, which may be related to the increased complexity and the introduction of new functions. Notwithstanding, the IndentoPro can still be recommended for use in research and clinical practice. This is of significant clinical relevance, as this tool provides a time- and cost-efficient way of measuring myofascial tissue stiffness for practitioners in the field of musculoskeletal medicine within their daily clinical practice.
A second key observation of our study was that no association (only exception: M2 at 10 mm: weight) was found between tissue stiffness and person characteristics. This is in contrast to earlier studies reporting significant correlations between soft tissue stiffness and sex [18,65,66], age [17,65,66] or BMI [9]. Interestingly, the study by Wilke et al. [5] also failed to identify a relationship of stiffness and BMI or sex. Therefore, future studies further elucidating this issue may be of interest in order to clarify the role of potential factors moderating tissue stiffness.
Several studies [61,65,67,68,69,70,71] measuring skinfold or subcutaneous fat thickness with skinfold calipers or ultrasonography found negative correlations with tissue stiffness (mostly measured with the MyotonPro device [67,68,69]). Our study did not identify such associations. Besides being related to the assessment method, the lack of statistical significance in our study might be due to the small sample size and a consecutive lack of power.
Although no significant differences between the measurements at 5 mm and those at 10 mm were found, the data distribution at 10 mm depth seemed to indicate a trend towards a larger data variability. We suggest that this may be—at least partly—related to a larger variation in the manual pressure orchestration during the stronger tissue indentation process.
A variety of limitations must be recognized, and such limitations warrant future research. Firstly, we exclusively conducted stiffness measurements in the human calf region only. Expanding the focus to other body regions (i.e., trunk and upper limb) may be of value, particularly because this may allow direct comparisons to other studies using devices such as the MyotonometerTM [23,24,25] and MyotonPro [26,27,28,29,72,73,74]. A second limitation relates to the indentation. Our data are novel in not only assessing stiffness at one depth. However, adding even more depths would allow the calculation of stiffness curves as a function of compression strength. Possibly, such dynamic evaluation would correlate more strongly with the above-mentioned potential predictors. In addition, different indentation depths might provide more specific information on different tissue layers such as the dermis, subcutaneous connective tissue, fascia profunda or muscular tissue. This hypothesis is based on the assumption that pressure needs to be higher if deeper structures are intended to be affected during stiffness measurements. Future investigations might therefore explore the suitability and reliability of different indentation depths for the assessment of different tissue layers. A third limitation relates to the fact that we recruited healthy participants only. It would be of interest to assess test properties in patients (e.g., with myofascial pain syndrome), as the focus of stiffness measurements is frequently therapeutic rather than preventative. Finally, despite the intriguing findings pointing towards sufficient to high reliability of the IndentoPro, a validation study is needed (e.g., measurement in patients with hypertension and asymptomatic persons or during different contraction levels) in order to verify that measured values are truly related to the construct of biomechanical stiffness.
5. Conclusions
This study provides evidence that the IndentoPro is a reliable device to measure myofascial tissue stiffness in the calf region of healthy individuals. However, as no systematic association was observed between stiffness and potential moderators such as skinfold thickness, sex, weight, height, BMI or age, further research is warranted in order to substantiate assumptions on the validity of the tool.
Author Contributions
Conceptualization, V.K.; methodology, V.K.; software, V.K.; validation, V.K.; formal analysis, V.K.; investigation, V.K.; resources, V.K.; data curation, V.K.; writing—original draft preparation, V.K. and J.W.; writing—review and editing, V.K. and J.W.; visualization, V.K.; supervision, J.W. project administration, V.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Diploma University of Applied Sciences, Bad Sooden-Allendorf, Germany (approval number EB 1010/2021 and date of approval 20 July 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets used and/or analyzed in the current study or any query regarding the research process are available from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fischer A.A. Tissue Compliance Meter for Objective, Quantitative Documentation of Soft Tissue Consistency and Pathology. Arch. Phys. Med. Rehabil. 1987;68:122–125. [PubMed] [Google Scholar]
- 2.Al Mayah A. Biomechanics of Soft Tissues: Principles and Application. CRC Press; Boca Raton, FL, USA: 2018. [Google Scholar]
- 3.Baumgart E. Stiffness—An Unknown World of Mechanical Science? Injury. 2000;31((Suppl. 2)):S-B14-23. [PubMed] [Google Scholar]
- 4.Arokoski J.P.A., Surakka J., Ojala T., Kolari P., Jurvelin J.S. Feasibility of the Use of a Novel Soft Tissue Stiffness Meter. Physiol. Meas. 2005;26:215–228. doi: 10.1088/0967-3334/26/3/007. [DOI] [PubMed] [Google Scholar]
- 5.Wilke J., Vogt L., Pfarr T., Banzer W. Reliability and Validity of a Semi-Electronic Tissue Compliance Meter to Assess Muscle Stiffness. J. Back Musculoskelet. Rehabil. 2018;31:991–997. doi: 10.3233/BMR-170871. [DOI] [PubMed] [Google Scholar]
- 6.Sakai F., Ebihara S., Akiyama M., Horikawa M. Pericranial Muscle Hardness in Tension-Type Headache. A Non-Invasive Measurement Method and Its Clinical Application. Pt 2Brain. 1995;118:523–531. doi: 10.1093/brain/118.2.523. [DOI] [PubMed] [Google Scholar]
- 7.Ashina M., Bendtsen L., Jensen R., Olesen J. Muscle Hardness in Patients with Chronic Tension-Type Headache: Relation to Actual Headache State. Pain. 1999;79:201–205. doi: 10.1016/S0304-3959(98)00167-5. [DOI] [PubMed] [Google Scholar]
- 8.Arya S., Kulig K. Tendinopathy Alters Mechanical and Material Properties of the Achilles Tendon. J. Appl. Physiol. 2010;108:670–675. doi: 10.1152/japplphysiol.00259.2009. [DOI] [PubMed] [Google Scholar]
- 9.Kuo W.-H., Jian D.-W., Wang T.-G., Wang Y.-C. Neck Muscle Stiffness Quantified by Sonoelastography Is Correlated with Body Mass Index and Chronic Neck Pain Symptoms. Ultrasound Med. Biol. 2013;39:1356–1361. doi: 10.1016/j.ultrasmedbio.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 10.Chang Y.-J., Kulig K. The Neuromechanical Adaptations to Achilles Tendinosis. J. Physiol. 2015;593:3373–3387. doi: 10.1113/JP270220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dugailly P.-M., Coucke A., Salem W., Feipel V. Assessment of Cervical Stiffness in Axial Rotation among Chronic Neck Pain Patients: A Trial in the Framework of a Non-Manipulative Osteopathic Management. Clin. Biomech. 2018;53:65–71. doi: 10.1016/j.clinbiomech.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Schleip R., Gabbiani G., Wilke J., Naylor I., Hinz B., Zorn A., Jäger H., Breul R., Schreiner S., Klingler W. Fascia Is Able to Actively Contract and May Thereby Influence Musculoskeletal Dynamics: A Histochemical and Mechanographic Investigation. Front. Physiol. 2019;10:336. doi: 10.3389/fphys.2019.00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fletcher J.R., MacIntosh B.R. Changes in Achilles Tendon Stiffness and Energy Cost Following a Prolonged Run in Trained Distance Runners. PLoS ONE. 2018;13:e0202026. doi: 10.1371/journal.pone.0202026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dumke C.L., Pfaffenroth C.M., McBride J.M., McCauley G.O. Relationship between Muscle Strength, Power and Stiffness and Running Economy in Trained Male Runners. Int. J. Sports Physiol. Perform. 2010;5:249–261. doi: 10.1123/ijspp.5.2.249. [DOI] [PubMed] [Google Scholar]
- 15.Bojsen-Møller J., Magnusson S.P., Rasmussen L.R., Kjaer M., Aagaard P. Muscle Performance during Maximal Isometric and Dynamic Contractions Is Influenced by the Stiffness of the Tendinous Structures. J. Appl. Physiol. 2005;99:986–994. doi: 10.1152/japplphysiol.01305.2004. [DOI] [PubMed] [Google Scholar]
- 16.Kubo K., Yata H., Kanehisa H., Fukunaga T. Effects of Isometric Squat Training on the Tendon Stiffness and Jump Performance. Eur. J. Appl. Physiol. 2006;96:305–314. doi: 10.1007/s00421-005-0087-3. [DOI] [PubMed] [Google Scholar]
- 17.Gervasi M., Sisti D., Amatori S., Andreazza M., Benelli P., Sestili P., Rocchi M.B.L., Calavalle A.R. Muscular Viscoelastic Characteristics of Athletes Participating in the European Master Indoor Athletics Championship. Eur. J. Appl. Physiol. 2017;117:1739–1746. doi: 10.1007/s00421-017-3668-z. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman L.R., Koppenhaver S.L., MacDonald C.W., Herrera J.M., Streuli J., Visco Z.L., Wildermuth N., Albin S.R. Normative Parameters of Gastrocnemius Muscle Stiffness and Associations with Patient Characteristics and Function. Int. J. Sports Phys. Ther. 2021;16:41–48. doi: 10.26603/001c.18803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McHugh M.P., Connolly D.A., Eston R.G., Kremenic I.J., Nicholas S.J., Gleim G.W. The Role of Passive Muscle Stiffness in Symptoms of Exercise-Induced Muscle Damage. Am. J. Sports Med. 1999;27:594–599. doi: 10.1177/03635465990270050801. [DOI] [PubMed] [Google Scholar]
- 20.Tafazzoli F., Lamontagne M. Mechanical Behaviour of Hamstring Muscles in Low-Back Pain Patients and Control Subjects. Clin. Biomech. 1996;11:16–24. doi: 10.1016/0268-0033(95)00038-0. [DOI] [PubMed] [Google Scholar]
- 21.Hrysomallis C. Injury Incidence, Risk Factors and Prevention in Australian Rules Football. Sports Med. 2013;43:339–354. doi: 10.1007/s40279-013-0034-0. [DOI] [PubMed] [Google Scholar]
- 22.Schleip R., Bartsch K. Fascia in Sport and Movement. Handspring Publishing Limited; Pencaitland, UK: 2021. (Second) Mechanical Assessment; p. 599. [Google Scholar]
- 23.Aarrestad D.D., Williams M.D., Fehrer S.C., Mikhailenok E., Leonard C.T. Intra- and Interrater Reliabilities of the Myotonometer When Assessing the Spastic Condition of Children with Cerebral Palsy. J. Child Neurol. 2004;19:894–901. doi: 10.1177/08830738040190110801. [DOI] [PubMed] [Google Scholar]
- 24.Leonard C.T., Deshner W.P., Romo J.W., Suoja E.S., Fehrer S.C., Mikhailenok E.L. Myotonometer Intra- and Interrater Reliabilities11A Commercial Party with a Direct Financial Interest in the Results of the Research Supporting This Article Has Conferred or Will Confer a Financial Benefit upon One or More of the Authors. Arch. Phys. Med. Rehabil. 2003;84:928–932. doi: 10.1016/S0003-9993(03)00006-6. [DOI] [PubMed] [Google Scholar]
- 25.Pamukoff D.N., Bell S.E., Ryan E.D., Blackburn J.T. The Myotonometer: Not a Valid Measurement Tool for Active Hamstring Musculotendinous Stiffness. J. Sport Rehabil. 2016;25:111–116. doi: 10.1123/jsr.2014-0271. [DOI] [PubMed] [Google Scholar]
- 26.Agyapong-Badu S., Aird L., Bailey L., Mooney K., Mullix J., Warner M., Samuel D., Stokes M. Interrater Reliability of Muscle Tone, Stiffness and Elasticity Measurements of Rectus Femoris and Biceps Brachii in Healthy Young and Older Males. Work. Pap. Health Sci. 2013;4:1–11. [Google Scholar]
- 27.Davidson M.J., Bryant A.L., Bower W.F., Frawley H.C. Myotonometry Reliably Measures Muscle Stiffness in the Thenar and Perineal Muscles. Physiother. Can. 2017;69:104–112. doi: 10.3138/ptc.2015-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lo W.L.A., Yu Q., Mao Y., Li W., Hu C., Li L. Lumbar Muscles Biomechanical Characteristics in Young People with Chronic Spinal Pain. BMC Musculoskelet. Disord. 2019;20:559. doi: 10.1186/s12891-019-2935-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taş S., Salkın Y. An Investigation of the Sex-Related Differences in the Stiffness of the Achilles Tendon and Gastrocnemius Muscle: Inter-Observer Reliability and Inter-Day Repeatability and the Effect of Ankle Joint Motion. Foot. 2019;41:44–50. doi: 10.1016/j.foot.2019.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Kett A.R., Sichting F. Sedentary Behaviour at Work Increases Muscle Stiffness of the Back: Why Roller Massage Has Potential as an Active Break Intervention. Appl. Ergon. 2020;82:102947. doi: 10.1016/j.apergo.2019.102947. [DOI] [PubMed] [Google Scholar]
- 31.Weber P., Graf C., Klingler W., Weber N., Schleip R. The Feasibility and Impact of Instrument-Assisted Manual Therapy (IAMT) for the Lower Back on the Structural and Functional Properties of the Lumbar Area in Female Soccer Players: A Randomised, Placebo-Controlled Pilot Study Design. Pilot Feasibility Stud. 2020;6:47. doi: 10.1186/s40814-020-00592-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stecco C., Macchi V., Porzionato A., Duparc F., De Caro R. The Fascia: The Forgotten Structure. Ital. J. Anat. Embryol. 2011;116:127–138. [PubMed] [Google Scholar]
- 33.Schleip R., Wilke J., Schreiner S., Wetterslev M., Klingler W. Needle Biopsy-Derived Myofascial Tissue Samples Are Sufficient for Quantification of Myofibroblast Density. Clin. Anat. 2018;31:368–372. doi: 10.1002/ca.23040. [DOI] [PubMed] [Google Scholar]
- 34.Ganjaei K.G., Ray J.W., Waite B., Burnham K.J. The Fascial System in Musculoskeletal Function and Myofascial Pain. Curr. Phys. Med. Rehabil. Rep. 2020;8:364–372. doi: 10.1007/s40141-020-00302-3. [DOI] [Google Scholar]
- 35.Myers T.W. Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists. 3rd ed. Elsevier; Edinburgh, UK: 2014. [Google Scholar]
- 36.Masi A.T., Nair K., Evans T., Ghandour Y. Clinical, Biomechanical, and Physiological Translational Interpretations of Human Resting Myofascial Tone or Tension. Int. J. Ther. Massage Bodywork. 2010;3:16–28. doi: 10.3822/ijtmb.v3i4.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilke J., Krause F., Vogt L., Banzer W. What Is Evidence-Based About Myofascial Chains: A Systematic Review. Arch. Phys. Med. Rehabil. 2016;97:454–461. doi: 10.1016/j.apmr.2015.07.023. [DOI] [PubMed] [Google Scholar]
- 38.Bordoni B., Marelli F. Emotions in Motion: Myofascial Interoception. Complement. Med. Res. 2017;24:110–113. doi: 10.1159/000464149. [DOI] [PubMed] [Google Scholar]
- 39.Bordoni B., Sugumar K., Varacallo M. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2022. Myofascial Pain. [PubMed] [Google Scholar]
- 40.Langevin H.M. Fascia Mobility, Proprioception, and Myofascial Pain. Life. 2021;11:668. doi: 10.3390/life11070668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang T., Vahdatinia R., Humbert S., Stecco A. Myofascial Injection Using Fascial Layer-Specific Hydromanipulation Technique (FLuSH) and the Delineation of Multifactorial Myofascial Pain. Medicina. 2020;56:717. doi: 10.3390/medicina56120717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stecco C., Tiengo C., Stecco A., Porzionato A., Macchi V., Stern R., De Caro R. Fascia Redefined: Anatomical Features and Technical Relevance in Fascial Flap Surgery. Surg. Radiol. Anat. 2013;35:369–376. doi: 10.1007/s00276-012-1058-0. [DOI] [PubMed] [Google Scholar]
- 43.Kottner J., Audige L., Brorson S., Donner A., Gajewski B.J., Hróbjartsson A., Roberts C., Shoukri M., Streiner D.L. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) Were Proposed. Int. J. Nurs. Stud. 2011;48:661–671. doi: 10.1016/j.ijnurstu.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 44.Taherdoost H. Sampling Methods in Research Methodology. Social Science Research Network; Rochester, NY, USA: 2016. How to Choose a Sampling Technique for Research. [Google Scholar]
- 45.Corder G.W., Foreman D.I. Nonparametric Statistics for Non-Statisticians: A Step-by-Step Approach. Wiley; Hoboken, NJ, USA: 2009. [Google Scholar]
- 46.Kwak S.G., Kim J.H. Central Limit Theorem: The Cornerstone of Modern Statistics. Korean J Anesthesiol. 2017;70:144–156. doi: 10.4097/kjae.2017.70.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Melick N., Meddeler B.M., Hoogeboom T.J., Nijhuis-van der Sanden M.W.G., van Cingel R.E.H. How to Determine Leg Dominance: The Agreement between Self-Reported and Observed Performance in Healthy Adults. PLoS ONE. 2017;12:e0189876. doi: 10.1371/journal.pone.0189876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Beek E. In: Anatomie, Physiologie: Für die Pysiotherapie: Lehrbuch für Physiotherapeuten, Masseure/medizinische Bademeister und Sportwissenschaftler. Zalpour C., Beek E., Van Fritsch H., Raichle G., Friedel T., Schröder E., Menche N., editors. Elsevier, Urban & Fischer; München, Germany: 2016. Für die Physiotherapie. 4., Überarbeitete und Ergänzte Auflage. [Google Scholar]
- 49.Jain S.M., Pandey K., Lahoti A., Rao P.K. Evaluation of Skin and Subcutaneous Tissue Thickness at Insulin Injection Sites in Indian, Insulin Naïve, Type-2 Diabetic Adult Population. Indian J. Endocrinol. Metab. 2013;17:864–870. doi: 10.4103/2230-8210.117249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Müller W., Lohman T.G., Stewart A.D., Maughan R.J., Meyer N.L., Sardinha L.B., Kirihennedige N., Reguant-Closa A., Risoul-Salas V., Sundgot-Borgen J., et al. Subcutaneous Fat Patterning in Athletes: Selection of Appropriate Sites and Standardisation of a Novel Ultrasound Measurement Technique: Ad Hoc Working Group on Body Composition, Health and Performance, under the Auspices of the IOC Medical Commission. Br. J. Sports Med. 2016;50:45–54. doi: 10.1136/bjsports-2015-095641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ogunleye L.I., Oyejola B.A., Obisesan K.O. Comparison of Some Common Tests for Normality. Int. J. Probab. Stat. 2018;7:130–137. [Google Scholar]
- 52.Weiß C. Basiswissen medizinische Statistik. Springer; Berlin/Heidelberg, Germany: 2019. Lehrbuch 7., Vollständige und Überarbeitete Auflage. [Google Scholar]
- 53.Portney L.G. Foundations of Clinical Research: Applications to Evidence-Based Practice. 4th ed. F.A. Davis; Philadelphia, PA, USA: 2020. [Google Scholar]
- 54.Lin L.I. A Concordance Correlation Coefficient to Evaluate Reproducibility. Biometrics. 1989;45:255–268. doi: 10.2307/2532051. [DOI] [PubMed] [Google Scholar]
- 55.Nickerson C.A.E. A Note On “A Concordance Correlation Coefficient to Evaluate Reproducibility”. Biometrics. 1997;53:1503–1507. doi: 10.2307/2533516. [DOI] [PubMed] [Google Scholar]
- 56.Weir J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005;19:231–240. doi: 10.1519/15184.1. [DOI] [PubMed] [Google Scholar]
- 57.Gwet K.L. Intrarater Reliability. In: Balakrishnan N., editor. Methods and Applications of Statistics in Clinical Trials. John Wiley & Sons, Inc.; Hoboken, NJ, USA: 2014. pp. 340–356. [Google Scholar]
- 58.McBride G.B. A Proposal for Strength-of-Agreement Criteria for Lin’s Concordance Correlation Coefficient. NIWA Client Report: HAM2005-062; NIWA; Hamilton, New Zealand: 2005. [Google Scholar]
- 59.Koo T.K., Li M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liljequist D., Elfving B., Skavberg Roaldsen K. Intraclass Correlation—A Discussion and Demonstration of Basic Features. PLoS ONE. 2019;14:e0219854. doi: 10.1371/journal.pone.0219854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burkholder E., Walsh C., Holmes N.G. Examination of Quantitative Methods for Analyzing Data from Concept Inventories. Phys. Rev. Phys. Educ. Res. 2020;16:010141. doi: 10.1103/PhysRevPhysEducRes.16.010141. [DOI] [Google Scholar]
- 62.Bland J.M., Altman D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet. 1986;1:307–310. doi: 10.1016/S0140-6736(86)90837-8. [DOI] [PubMed] [Google Scholar]
- 63.Bland J.M., Altman D.G. Measuring Agreement in Method Comparison Studies. Stat. Methods Med. Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 64.Schober P., Boer C., Schwarte L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018;126:1763–1768. doi: 10.1213/ANE.0000000000002864. [DOI] [PubMed] [Google Scholar]
- 65.Agyapong-Badu S., Warner M., Samuel D., Stokes M. Measurement of Ageing Effects on Muscle Tone and Mechanical Properties of Rectus Femoris and Biceps Brachii in Healthy Males and Females Using a Novel Hand-Held Myometric Device. Arch. Gerontol. Geriatr. 2016;62:59–67. doi: 10.1016/j.archger.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 66.Wu R., Delahunt E., Ditroilo M., Lowery M., De Vito G. Effects of Age and Sex on Neuromuscular-Mechanical Determinants of Muscle Strength. Age. 2016;38:57. doi: 10.1007/s11357-016-9921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Viner A., Lee M., Adams R. Posteroanterior Stiffness in the Lumbosacral Spine. The Correlation between Adjacent Vertebral Levels. Spine. 1997;22:2724–2729. doi: 10.1097/00007632-199712010-00004. discussion 2729–2730. [DOI] [PubMed] [Google Scholar]
- 68.Lee M., Steven G.P., Crosbie J., Higgs R.J. Variations in Posteroanterior Stiffness in the Thoracolumbar Spine: Preliminary Observations and Proposed Mechanisms. Phys. Ther. 1998;78:1277–1287. doi: 10.1093/ptj/78.12.1277. [DOI] [PubMed] [Google Scholar]
- 69.Kinoshita H., Miyakawa S., Mukai N., Kono I. Measurement of Tissue Hardness for Evaluating Flexibility of the Knee Extensor Mechanism. Football Sci. 2006;3:15–20. [Google Scholar]
- 70.Fröhlich-Zwahlen A.K., Casartelli N.C., Item-Glatthorn J.F., Maffiuletti N.A. Validity of Resting Myotonometric Assessment of Lower Extremity Muscles in Chronic Stroke Patients with Limited Hypertonia: A Preliminary Study. J. Electromyogr. Kinesiol. 2014;24:762–769. doi: 10.1016/j.jelekin.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 71.Chino K., Takahashi H. Handheld Tissue Hardness Meters for Assessing the Mechanical Properties of Skeletal Muscle: A Feasibility Study. J. Manip. Physiol. Ther. 2016;39:518–522. doi: 10.1016/j.jmpt.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 72.Lo W.L.A., Zhao J.L., Li L., Mao Y.R., Huang D.F. Relative and Absolute Interrater Reliabilities of a Hand-Held Myotonometer to Quantify Mechanical Muscle Properties in Patients with Acute Stroke in an Inpatient Ward. Biomed. Res. Int. 2017;2017:4294028. doi: 10.1155/2017/4294028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yeo S.M., Kang H., An S., Cheong I., Kim Y., Hwang J.H. Mechanical Properties of Muscles around the Shoulder in Breast Cancer Patients: Intra-Rater and Inter-Rater Reliability of the MyotonPRO. PM R. 2020;12:374–381. doi: 10.1002/pmrj.12227. [DOI] [PubMed] [Google Scholar]
- 74.Taş S., Yaşar Ü., Kaynak B.A. Interrater and Intrarater Reliability of a Handheld Myotonometer in Measuring Mechanical Properties of the Neck and Orofacial Muscles. J. Manip. Physiol. Ther. 2021;44:42–48. doi: 10.1016/j.jmpt.2020.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed in the current study or any query regarding the research process are available from the corresponding author.