Abstract
Although the combination of nanoliposomal irinotecan plus fluorouracil/folinic acid (nal-IRI/FF) exhibited survival benefits in gemcitabine-refractory patients with advanced pancreatic cancer (APC) in the phase III NAPOLI-1 trial, there is limited data on the efficacy and safety of this regimen in real-world settings in Japan. This multicenter, prospective observational study enrolled patients with APC who received nal-IRI/FF after a gemcitabine-based regimen from July 2020 to June 2021. We collected and analyzed clinical data and conducted survival and multivariate analyses. Thirty-one (78%) of the 40 patients had metastases. Nal-IRI/FF was the second-line therapy in 36 patients (90%). The median duration was 3.2 months. The disease control rate was 57%. The median progression-free survival and overall survival (OS) were 4.5 months (95% confidence interval [CI]: 2.8–5.5) and 7.4 months (95% CI: 5.1–10.6), respectively. Common ≥grade 3 toxicities included neutropenia (28%) and fatigue (23%). Fatigue led to treatment discontinuation in 6 out of 10 patients. Multivariate analysis showed that a neutrophil-to-lymphocyte ratio > 4 was a significant risk factor for a short OS (hazard ratio (HR) = 3.08, 95% CI: 1.21–7.85, p = 0.02). In conclusion, nal-IRI/FF is an appropriate treatment option for APC following gemcitabine-containing regimens.
Keywords: nanoliposomal irinotecan, advanced pancreatic cancer, second-line therapy
1. Introduction
According to the 2018 Global Cancer Analysis, pancreatic cancer (PC) remains the fourth leading cause of cancer-related deaths. PC’s 5-year relative survival rate is 8%, which is the lowest among all types of cancer [1]. Approximately 80% of patients with PC are diagnosed at an unresectable, locally advanced, or metastatic disease stage [2] and have only one treatment option: chemotherapy.
Over the past two decades, gemcitabine (GEM) has been the standard first-line therapy for patients with advanced PC (APC). Subsequently, the FOLFIRINOX (FFX; a combination of oxaliplatin, folinic acid, irinotecan, and fluorouracil) [3] and GEM plus nab-paclitaxel (GnP) [4] demonstrated a considerable survival advantage in patients with metastatic PC (MPC) and have been accepted as the most common first-line therapies. However, there is an increasing demand for second-line therapies for those with unavoidable disease progression or drug intolerance. Nanoliposomal irinotecan (nal-IRI) is a new antitumor drug consisting of irinotecan sucralfate salt, a topoisomerase I inhibitor, encapsulated in liposome nanoparticles. Liposomal encapsulation facilitates a more efficient conversion of irinotecan to SN-38 (an active metabolite of irinotecan) than non-liposomal irinotecan [5]. This nal-IRI formulation contributes to drug stabilization by prolonging the circulation time and increasing the accumulation of SN-38 in the tumor [6,7].
In 2016, the global randomized phase III study NAPOLI-1 showed that the combination of nal-IRI and fluorouracil/folinic acid (nal-IRI/FF) resulted in significant survival benefits compared with nal-IRI alone or FF monotherapy in patients with MPC who previously received GEM-based therapy [8]. A randomized phase II trial targeting Japanese patients [9] also revealed that nal-IRI/FF provides a considerable survival benefit compared to FF alone.
Although some studies have reported the use of nal-IRI/FF in patients with APC, there are limited prospective studies that aim to record real-world data. In the present study, we conducted a multicenter prospective analysis to assess the therapeutic effects and safety of nal-IRI/FF in patients with APC after GEM-based therapy in Japan.
2. Materials and Methods
2.1. Patient Population and the Study Design
This study was a multi-institutional, prospective, observational analysis of patients with APC. Patients with unresectable PC who had previously received GEM-containing therapy and were administered nal-IRI/FF between July 2020 and June 2021 were enrolled. Patients who received regimens that included irinotecan, such as modified FFX, were excluded. Patients with a history of secondary malignancy in the previous five years were also excluded.
2.2. Treatment
As a standard regimen, the patients received an intravenous infusion of 70 mg/m2 nal-IRI over 90 min, followed by 2400 mg/m2 5-FU and 200 mg/m2 levoleucovorin calcium as the initial doses every two weeks. Dose reduction was performed based on the toxicity (described in Section 2.3). We calculated the cumulative relative dose intensity (cRDI), which was defined as the average ratio (%) of the actual delivered nal-IRI and 5-FU to the planned amount throughout the treatment period, as in a previous study [10].
Therapy was discontinued if disease progression or unacceptable adverse events occurred. Continuation of the nal-IRI/FF treatment regimen after disease progression was allowed if the physician judged it feasible.
2.3. Evaluation of Efficacy and Toxicity
The primary endpoint was overall survival (OS), defined as the interval from the first administration of nal-IRI/FF until death or the occurrence of censoring. Secondary endpoints were progression-free survival (PFS), disease control rate (DCR), and safety. We performed serial computed tomography (CT) scans every 2.5 months or shorter, according to the Response Evaluation Criteria in Solid Tumors version 1.0 (RECIST, v1.0). The serum carbohydrate antigen 19-9 (CA19-9) response was defined as a decrease in the level of CA19-9 by more than 50% from baseline during nal-IRI/FF therapy. All surviving patients were censored at the last follow-up date, 28 February 2022.
All adverse effects were evaluated according to the National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.0 (CTCAE, v4.0).
2.4. Ethical Standards
This human study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all patients, and the study was approved by the ethics committees of the Kyushu Cancer Center (approval number: 2020-30), Kitakyushu Municipal Medical Center (approval number: 202008006), and Kyushu University (approval number: 2020-290).
2.5. Statistics
Categorical variables are expressed as frequencies and proportions. Fisher’s exact test was used for comparison between the groups. A two-sided p < 0.05 was considered significant. Continuous variables are expressed as medians and interquartile ranges [IQRs], and values were compared using the Mann–Whitney U test. The Kaplan–Meier curve was drawn, and differences in survival were evaluated using the log-rank test. Univariate and multivariate analyses for survival time were performed using the Cox proportional hazard regression model. Significant variables with a p-value < 0.1 in the univariate analysis were included in the multivariate analysis. All statistical analyses were performed using the Easy R program version1.3.6 (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [11].
3. Results
3.1. Patient Characteristics
Forty patients were enrolled in this study. Patient characteristics are shown in Table 1. The median age was 70.5 [62.5–72.0] years, and 19 patients (48%) were male. Nine patients had disease recurrence after curative surgical resection. The median disease-free survival of patients with surgical resection was 11.0 [9.2–30.2] months. The numbers of patients with an Eastern Cooperative Oncology Group (ECOG) Performance Status (PS) 0, 1, and 2 were 21 (52%), 18 (45%), and 1 (3%), respectively. Most of the patients (78%) had metastases. The numbers of patients with 1, 2, and ≥3 metastatic sites were 12 (30%), 14 (35%), and 5 (13%), respectively. One patient was homozygous for UGT1A1*6, and another was heterozygous for UGT1A1*28 and *6.
Table 1.
Patient characteristics.
| n/Median | (%)/[IQR] | |
|---|---|---|
| Age | 70.5 | [62.5–72.0] |
| Sex-Male | 19 | (47.5) |
| Body Mass Index | 20.9 | [14.3–26.5] |
| Primary site | ||
| Head/Body/Tail | 17/12/11 (43/30/27) | |
| Diameter of the primary tumor (mm) | 32 | [18–75] |
| Presence of history of biliary drainage | 9 | (23) |
| History of surgical resection | 9 | (23) |
| Distant metastases | 31 | (78) |
| Metastatic site | ||
| Liver | 16 | (40) |
| Peritoneum | 13 | (3) |
| Lung | 6 | (15) |
| Number of metastatic sites | ||
| 1 | 12 | (30) |
| 2 | 14 | (35) |
| ≥3 | 5 | (13) |
| ECOG PS | ||
| 0/1/2 | 21/18/1 (52/45/3) | |
| Presence of UGT1A1 polymorphism | 2 | (5) |
| Reason for the discontinuation of the previous therapy | ||
| Progressive disease | 36 | (90) |
| Toxicity | 4 | (10) |
| Line of therapy where nal-IRI/FF was administered | ||
| Second-line | 36 | (90) |
| Third-line | 4 | (10) |
| First-line regimen | ||
| Gemcitabine + nab-paclitaxel | 39 | (98) |
| Gemcitabine + S-1 | 1 | (3) |
| Second-line regimen * | ||
| S-1 | 3 | (8) |
| Gemcitabine + nab-paclitaxel | 1 | (3) |
| The duration between the diagnosis and initiation of nal-IRI/FF (months) | ||
| 6.9 | [5.0–10.7] | |
| Post-study anticancer therapy | ||
| modified FOLFIRINOX | 7 | (18) |
| Gemcitabine + nab-paclitaxel | 3 | (8) |
| Oxaliplatin + fluorouracil/folinic acid | 7 | (18) |
| S-1 | 1 | (3) |
| Observation period (months) | 7.3 | [4.4–10.6] |
ECOG PS, Eastern Cooperative Oncology Group Performance Status; nal-IRI/FF, irinotecan plus fluorouracil/folinic acid. * Second-line regimen, regimen administered to patients who received nal-IRI/FF as third-line therapy.
Thirty-six (90%) and four (10%) patients received nal-IRI/FF as second- and third-line therapies, respectively. Progressive disease and toxicity led to discontinuation of the previous therapy in 36 (90%) and four (10%) patients.
The median interval from the diagnosis with unresectable PC to the initiation of nal-IRI/FF was 6.6 [5.0–10.7] months. The median observation period was 7.4 [4.4–0.6] months.
3.2. Treatment Delivery and Dose Reduction or Discontinuation
The median treatment period was 3.2 [1.7–6.2] months, and the median number of cycles was 6 [3–10]. The administered doses and attributed reasons for dose reduction or discontinuation are summarized in Table 2. Twenty-eight (70%), nine (22%), and three (8%) patients received 100%, 80%, and 70% of the initial nal-IRI dose, respectively. The median overall cRDI score was 69.0% [54.5–86.5%].
Table 2.
Administered dose and attributed reasons for dose reduction or discontinuation.
| Median | (%)/[IQR] | |
|---|---|---|
| The initial dose of nal-IRI | ||
| 100% | 28 | (70) |
| 90% | 0 | (0) |
| 80% | 9 | (21.5) |
| 70% | 3 | (7.5) |
| Duration of treatment (months) | 3.2 | [1.7–6.2] |
| Cycles of treatment (n) | 6 | [3–10] |
| Relative dose intensity (%) | 69.0 | [54.5–86.5] |
| Dose reduction during all cycles | 20 | (50) |
| Dose reduction due to AE in the first 4 cycles | 14 | (35) |
| Discontinuation due to AE | 10 | (40) |
3.3. Treatment Response
The treatment responses are summarized in Table 3. Among the evaluable 35 patients, partial response (PR) was observed in three patients (9%), stable disease (SD) in 17 patients (49%), and progressive disease (PD) in 15 patients (43%). The DCR was 57%. There were 8 CA19-9 responders (25%) among 32 patients with evaluable CA19-9 values.
Table 3.
Overall response to treatment with irinotecan plus fluorouracil/folinic acid (nal-IRI/FF).
| Tumor Response § | n | (%) |
|---|---|---|
| PR | 3 | (9) |
| SD | 17 | (49) |
| PD | 15 | (43) |
| DCR | 20 | (57) |
| CA19-9 response | n | (%) |
| responder | 8 | (25) |
| non-responder | 24 | (75) |
PR, partial response; SD, stable disease; PD, progressive disease; NE, not evaluable; DCR, disease control rate. CA19-9, carbohydrate antigen 19-9. Responders: patients with a reduction rate of CA19-9 > 50%; non-responders: patients without a reduction rate of CA19-9 > 50%. § Five patients were not evaluable due to treatment discontinuation before the follow-up CT. Eight patients were not evaluable.
3.4. Survival
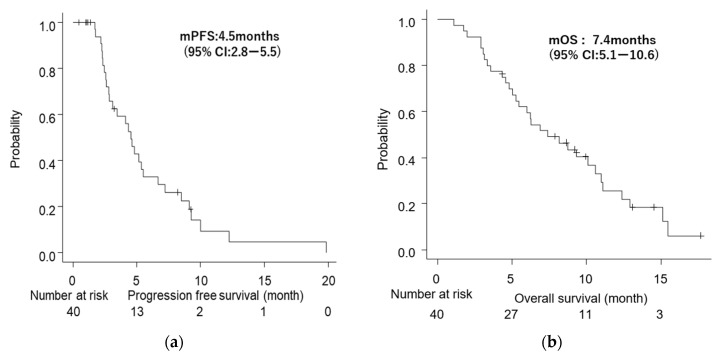
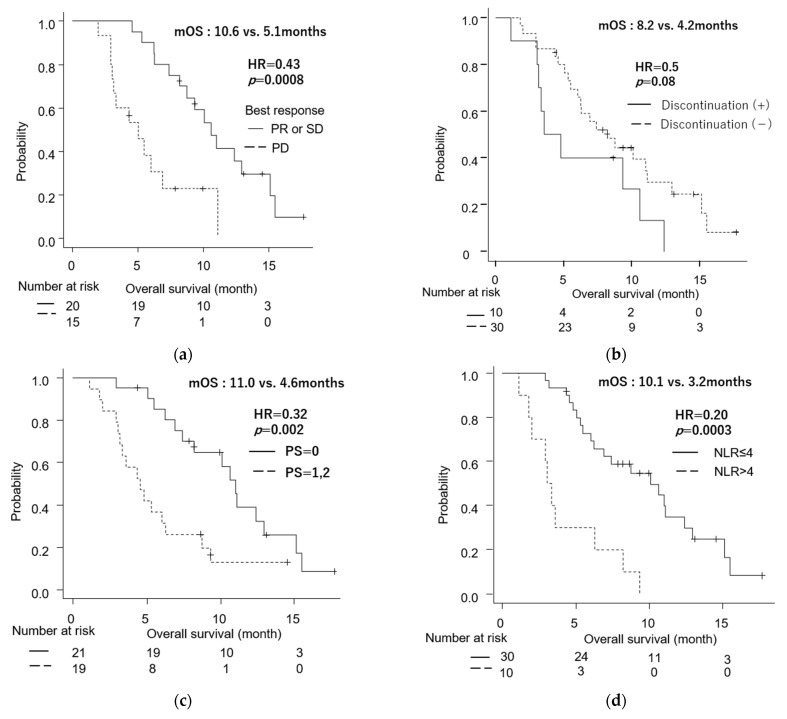
Median PFS (mPFS) was 4.5 months (95% CI: 2.8–5.5), and median OS (mOS) was 7.4 months (95% CI: 5.1–10.6) (Figure 1a,b). The mOS from the diagnosis with unresectable status was 16 months (95% CI: 13.2–19.5). There was no difference in OS between patients with metastasis and locally advanced disease (6.3 vs. 10.6 months, p = 0.51) (Figure S1). Regarding the relationship between treatment response and survival, the OS of patients with PD was significantly shorter than that of patients with SD and PR (5.1 vs. 10.6 months), with an HR of 0.43 (95% CI: 0.20–0.94; p = 0.0008) (Figure 2a). On the other hand, there was no significant difference in OS between CA19-9 responders and non-responders (11.1 vs. 7.4 months, p = 0.42).
Figure 1.
Kaplan–Meier survival analyses. (a) Progression-free survival (PFS) of all patients. (b) Overall survival (OS) of all patients; CI, confidence interval, and p-value were calculated using the log-rank test.
Figure 2.
Kaplan–Meier survival analyses. (a) Overall survival (OS) with the best response = progressive disease (PD) versus stable disease (SD) or partial response (PR). (b) OS with treatment discontinuation versus without discontinuation. (c) OS with performance status (PS) = 0 versus PS = 1, 2. (d) OS with neutrophil-lymphocyte ratio (NLR) > 4 versus NLR ≤ 4. mOS, median overall survival; HR, hazard ratio. p-value was calculated using the log-rank test.
3.5. Safety
Table 4 shows the adverse events (AE) during nal-IRI/FF treatment. The most common AEs included neutropenia (63%), general fatigue (63%), and leukopenia (60%). Eleven patients had grade 3 neutropenia. None of the patients experienced febrile neutropenia or ≥grade 3 thrombocytopenia. Regarding the severe (≥grade3) non-hematologic AEs, general fatigue was observed in nine patients, anorexia in two patients, and diarrhea, which led to acute renal dysfunction in one patient. Dose reduction was conducted due to neutropenia in nine (23%), general fatigue in nine (23%), and diarrhea in two (5%) patients. Ten patients (25%) required discontinuation of treatment. Six out of ten patients stopped the therapy due to general fatigue, and the treatment for the remaining was discontinued due to diarrhea, hemobilia, septic shock, and ileus. Six of the patients were moved to another line of chemotherapy.
Table 4.
Adverse events during irinotecan plus fluorouracil/folinic acid (nal-IRI/FF) treatment.
| All Grade | Grade 3/4 | Required Dose Reduction |
Required Discontinuation | |||||
|---|---|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | |||||
| Hematologic | ||||||||
| Neutropenia | 25 | (63) | 11 | (28) | 9 | (23) | ||
| Leukocytopenia | 24 | (60) | 5 | (13) | ||||
| Thrombocytopenia | 11 | (28) | 0 | (0) | ||||
| Anemia | 14 | (35) | 2 | (5) | ||||
| Non-hematologic | ||||||||
| General fatigue | 25 | (63) | 9 | (23) | 9 | (23) | 6 | (15) |
| Anorexia | 16 | (40) | 2 | (5) | ||||
| Diarrhea | 11 | (28) | 1 | (3) | 2 | (5) | 1 | (3) |
| Hypokalemia | 2 | (5) | 0 | (0) | ||||
| Dysgeusia | 2 | (5) | 0 | (0) | ||||
| Hemobilia | 1 | (3) | 1 | (3) | ||||
| Septic shock | 1 | (3) | 1 | (3) | ||||
| Ileus | 1 | (3) | 1 | (3) | ||||
| Infusion reaction | 1 | (3) | 0 | (0) | ||||
3.6. Comparison between Patients Who Continued and Discontinued the Treatment Regimen
Although not significant, patients who discontinued therapy due to AEs (n = 10) tended to have worse survival than patients who continued treatment until disease progression (mOS: 8.2 vs. 4.2 months, HR = 2.0; 95% CI: 0.90–4.5, p = 0.08) (Figure 2b).
We compared the clinical characteristics of patients who discontinued nal-IRI/FF due to AEs with those of the patients who did not (Table S1). The rate of patients with ECOG PS ≥ 1 was significantly higher in those who discontinued the treatment than in those who did not. Furthermore, the interval from the diagnosis to initiation of nal-IRI/FF tended to be longer in patients who discontinued the treatment than in those who did not (median interval: 9.9 vs. 6.5 months, p = 0.08).
3.7. Univariate and Multivariate Analyses
We performed univariate and multivariate analyses to identify the possible predictive factors of PFS (Table S2) and OS (Table 5). There were no significant prognostic factors for PFS. Meanwhile, PS ≥ 1 (hazard ratio [HR]: 3.1, 95% CI: 1.4–6.6, p = 0.004), neutrophil-lymphocyte ratio (NLR) > 4 (HR: 4.9, 95% CI: 2.1–11.3, p = 0.0002), and body weight loss > 5% from diagnosis (HR: 2.3, 95% CI: 1.1–4.9, p = 0.03) were associated with worse OS in the univariate analysis. The Kaplan–Meier curve (Figure 2c) showed that the mOS in patients with ECOG PS ≥ 1 (4.6 months) at the start of nal-IRI/FF treatment was significantly shorter than that in patients with PS = 0 (11.0 months). Metastatic disease was not a poor prognostic factor. Multivariate analysis showed that NLR > 4 (HR = 3.1, 95% CI: 1.2–7.9, p = 0.02) was an independent predictive factor for shorter survival. There was a significant difference in OS between patients with NLR > 4 and NLR ≤ 4 (p = 0.00003), as shown in Figure 2d.
Table 5.
Univariate and multivariate analyses of clinical factors at the start of irinotecan plus fluorouracil/folinic acid (nal-IRI/FF) treatment for predicting overall survival.
| Variables at the Start of nal-IRI/FF Treatment | n | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|---|
| HR | (95% CI) | p-Value | HR | (95% CI) | p-Value | ||
| Age | |||||||
| ≥70 y.o. | 20 | 1.17 | (0.57–2.38) | 0.67 | |||
| <70 y.o. | 20 | ||||||
| Sex | |||||||
| male | 19 | 1.06 | (0.52–2.17) | 0.86 | |||
| female | 21 | ||||||
| ECOG PS | |||||||
| =1 or 2 | 19 | 3.08 | (1.43–6.63) | 0.004 | 2.24 | 0.86–5.73 | 0.09 |
| =0 | 21 | ||||||
| Stage | |||||||
| metastatic | 31 | 1.40 | (0.57–3.46) | 0.51 | |||
| locally advanced | 9 | ||||||
| Liver metastasis | |||||||
| present | 19 | 1.12 | (0.54–2.32) | 0.67 | |||
| absent | 21 | ||||||
| Peritoneal metastasis | |||||||
| present | 14 | 1.12 | (0.54–2.33) | 0.76 | |||
| absent | 26 | ||||||
| Carcinomatosis * | |||||||
| present | 19 | 1.44 | (0.71–2.93) | 0.31 | |||
| absent | 21 | ||||||
| NLR | |||||||
| >4 | 10 | 4.88 | (2.10–11.3) | 0.0002 | 3.08 | 1.21–7.85 | 0.02 |
| ≤4 | 30 | ||||||
| CA19-9 | |||||||
| >1000 U/dL | 20 | 1.38 | (0.67–2.80) | 0.37 | |||
| ≤1000 U/dL | 16 | ||||||
| GPS | |||||||
| =2 | 11 | 2.08 | (0.94–4.59) | 0.07 | |||
| =0.1 | 29 | ||||||
| LMR | |||||||
| <3 | 27 | 1.18 | (0.55–2.52) | 0.67 | |||
| ≥3 | 13 | ||||||
| PLR | |||||||
| >150 | 32 | 0.80 | (0.35–1.83) | 0.60 | |||
| ≤150 | 8 | ||||||
| PNI | |||||||
| <45 | 30 | 0.78 | (0.35–1.71) | 0.53 | |||
| ≥45 | 10 | ||||||
| Bodyweight decrease from the diagnosis as an unresectable disease | |||||||
| >5% | 14 | 2.29 | (1.09–4.85) | 0.03 | 1.46 | 0.64–3.32 | 0.37 |
| ≤5% | 23 | ||||||
| The interval from the diagnosis to the administration of nal-IRI/FF | |||||||
| >6.6months | 20 | 1.04 | 0.51–2.14 | 0.95 | |||
| ≤6.6months | 20 | ||||||
* Carcinomatosis, presence of multi-metastatic sites; GPS, Glasgow prognostic score. NLR, neutrophil-lymphocyte ratio; PLR, platelet-lymphocyte ratio; LMR, lymphocyte-monocyte ratio; PNI, prognostic nutritional index.
4. Discussion
In line with previous studies [9,12], this multicenter prospective analysis confirmed the survival benefits and manageable safety profile of the naI-IRI/FF regimen in patients with APC who previously received a GEM-containing regimen in Japan.
Although there was no difference in the CA19-9 response, the PFS and OS observed in the current study were longer than in previous reports. There may be several reasons for this finding. First, the patient population included only a small number of patients with PS = 2 (only one), a high proportion (90%) who received nal-IRI/FF as a second-line therapy, and a relatively high proportion (45%) who received post-study anti-cancer treatment.
The subpopulation analysis of NAPOLI-1 [12] reported the baseline characteristics of the Asian subgroup vs. the overall population: the higher rate of patients with baseline Karnofsky PS ≥ 90 (65% vs. 59%), ≤1 previous line of metastatic therapy (74% vs. 66%), and post anti-cancer treatment (50% vs. 31%), which were similar to the findings in our study population. These contributed to better outcomes in Asian patients than in the overall study population. The outcome of this study also might be attributed to the patient characteristics.
Second, in a previous study on the efficacy of nal-IRI/FF [11], patients who experienced no cancer progression with irinotecan treatment showed improved survival compared to those with prior cancer progression with irinotecan (mOS: 7.7 vs. 3.9 months). Smith et al. [13] and Yu et al. [14] showed a similar result in patients with APC who had been treated with irinotecan. Thus, we excluded patients who had received prior irinotecan-containing therapy to assess the effect of nal-IRI/FF without being confounded by the history of irinotecan administration. This exclusion criterion might have contributed to the better PFS and OS in the current study (mPFS = 4.5, mOS = 7.2) compared with those reported in the NAPOLI-1 trial (mPFS = 2.3, mOS = 6.1) or other studies [15,16,17]. Third, the inclusion of locally advanced PC, which was distinct from the inclusion criteria of the NAPOLI-1 study, might have caused a better outcome. However, there was no significant difference between patients with or without metastasis. Finally, there is the possibility that a lower frequency of CT assessment and a relatively high rate of censored patients due to longer OS might have affected the longer PFS found in this study.
Contrary to the NAPOLI-1 study, wherein more than 10% of all patients died during the study, or within 30 days of the last dose, there were no deaths within 30 days of the last dose in the present study. Thus, based on this finding and the fact that ten patients (25%) in our study could continue therapy for more than half a year, the nal-IRI/FF regimen can generally be considered well-tolerated in Japanese clinical practice. Neutropenia and anorexia were common AEs of nal-IRI/FF, as reported in a previous study; there were no significant differences in incidence between this study and the NAPOLI-1 trial [8]. The incidence of diarrhea was lower than that of the overall intention-to-treat population in the NAPOLI-1 study, and the incidence was comparable to that of the Asian sub-population in the NAPOLI-1 study [12]. However, fatigue had a much higher incidence and was the leading cause of therapy discontinuation. Other AEs with fatal outcomes, such as hemobilia and ileus, could not be considered treatment-related AEs, as they were probably complications of cancer itself. These incidences of various complications during the study might be explained as a result of the second-line setting where most patients have advanced diseases.
Intriguingly, the prognosis in disease-controlled patients with the best response of SD or PR was significantly better than that in patients with progressive disease. The results indicate that the response to the nal-IRI/FF regimen in patients previously treated with a GEM-based regimen considerably impacts prognosis.
The survival curve indicated that the discontinuation of nal-IRI/FF due to AEs was possibly associated with shorter OS, although it was not significant in this small population. The PS of patients who discontinued treatment was lower than that of patients who continued the treatment. This finding may help anticipate the clinical benefits of this regimen in individual patients.
The present study showed no significant difference in the starting doses of nal-IRI between the patients who continued and discontinued the treatment. However, clinical studies that involved starting dose reductions revealed that these reductions were not significantly associated with PFS or OS [18]. Moreover, they showed that the PS at the start of nal-IRI/FF treatment was not a poor prognostic factor when administered via a sufficiently reduced dose. Thus, a pre-emptive dose reduction should be considered to prevent serious AEs, especially in patients with low PS, as recommended in a Taiwanese study [15].
PS was associated with a short OS, consistent with a meta-analysis reporting that the baseline PS is a potent prognostic factor of PC after progression while on first-line GEM-based regimens [19]. Additionally, our multivariate analysis revealed that a high NLR was an independent poor prognostic factor. A high NLR (at the start of first-line therapy) has been widely reported to be associated with poor OS in APC [20,21]. In addition, a high NLR was a negative prognostic factor in the survival analysis of the NAPOLI-1 trial [22], which indicates the utility of NLR as a prognostic factor in second-line and first-line therapies.
Meanwhile, other reported factors, such as older age (≥65 years) and the presence of liver metastasis [22], related to poor prognosis, were not associated with short OS in our study. The difference in patient age distribution and liver metastasis volume might have affected the results. Further studies with larger sample sizes are required to develop a consensus on the prognostic factors of patients with APC receiving nal-IRI/FF treatment.
This study had several limitations. First, the sample size was too small to reach a definitive conclusion. Second, there was heterogeneity in the treatment dose and schedule due to the observational study design, where modification of the nal-IRI/FF regimen was allowed based on the physician’s decision. Third, we could not compare the efficacy of nal-IRI/FF therapy with that of other regimens such as FFX or modified FFX due to the single-arm fashion of our study. Further comparative studies are required to decide on an optimal regimen for patients with GnP failure. However, our real-world data might help establish an appropriate direction for using nal-IRI/FF.
Nal-IRI/FF is an effective sequential treatment after GEM-based treatment in patients with APC. This therapy should be administered under the careful management of AEs, including those triggered by an advanced disease state. The NLR may be a prognostic indicator of the therapeutic effect of nal-IRI/FF.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11175084/s1: Figure S1: Kaplan–Meier survival analysis. Overall survival (OS) with metastatic pancreatic cancer versus locally advanced pancreatic cancer; Table S1: Comparison of clinical factors at the start of irinotecan plus fluorouracil/folinic acid (nal-IRI/FF) treatment between patients who continued and discontinued the treatment due to adverse events; Table S2: Univariate analysis of clinical factors at the start of irinotecan plus fluorouracil/folinic acid (nal-IRI/FF) treatment for predicting progression-free survival.
Author Contributions
Conceptualization, Formal Analysis, Original Draft Preparation, M.M. (Masami Miki); Supervision, management of study material or patients, and writing—review & editing, N.F.; Methodology, management of study material or patients, and writing—review & editing, K.U.; Conceptualization and Methodology, L.L.; Management of the patients’ study materials, data collection, and assembly, M.M. (Masatoshi Murakami), Y.T., Y.S. and Y.N.; Supervision, management of the patients’ study materials, T.O.; Methodology and management of the patients’ study materials, T.H.; Project Administration, M.F.; Supervision and approval of the final version of the manuscript, Y.O. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics committees of the Kyushu Cancer Center (approval number: 2020-30), Kitakyushu Municipal Medical Center (approval number: 202008006), and Kyushu University (approval number: 2020-290).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer Statistics, 2018. CA Cancer J. Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Vincent A., Herman J., Schulick R., Hruban R.H., Goggins M. Pancreatic Cancer. Lancet. 2011;378:607–620. doi: 10.1016/S0140-6736(10)62307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conroy T., Desseigne F., Ychou M., Bouché O., Guimbaud R., Bécouarn Y., Adenis A., Raoul J.L., Gourgou-Bourgade S., de la Fouchardière C., et al. FOLFIRINOX Versus Gemcitabine for Metastatic Pancreatic Cancer. N. Engl. J. Med. 2011;364:1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 4.Von Hoff D.D., Ervin T., Arena F.P., Chiorean E.G., Infante J., Moore M., Seay T., Tjulandin S.A., Ma W.W., Saleh M.N., et al. Increased Survival in Pancreatic Cancer with Nab-Paclitaxel plus Gemcitabine. N. Engl. J. Med. 2015;36918:1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drummond D.C., Noble C.O., Guo Z., Hong K., Park J.W., Kirpotin D.B. Development of a Highly Active Nanoliposomal Irinotecan Using a Novel Intraliposomal Stabilization Strategy. [(accessed on 10 August 2022)];Cancer Res. 2006 66:3271–3277. doi: 10.1158/0008-5472.CAN-05-4007. Available online: http://www.aacrjournals.org. [DOI] [PubMed] [Google Scholar]
- 6.Kalra A.V., Kim J., Klinz S.G., Paz N., Cain J., Drummond D.C., Nielsen U.B., Fitzgerald J.B. Preclinical Activity of Nanoliposomal Irinotecan Is Governed by Tumor Deposition and Intratumor Prodrug Conversion. [(accessed on 10 August 2022)]. Available online: http://cancerres.aacrjournals.org/ [DOI] [PubMed]
- 7.Chiang N.J., Chao T.Y., Hsieh R.K., Wang C.H., Wang Y.W., Yeh C.G., Chen L.T. A Phase I Dose-Escalation Study of PEP02 (Irinotecan Liposome Injection) in Combination with 5-Fluorouracil and Leucovorin in Advanced Solid Tumors. BMC Cancer. 2016;16:907. doi: 10.1186/s12885-016-2933-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang-Gillam A., Li C.P., Bodoky G., Dean A., Shan Y.S., Jameson G., Macarulla T., Lee K.-H., Cunningham D., Schwartsmann G., et al. Nanoliposomal Irinotecan with Fluorouracil and Folinic Acid in Metastatic Pancreatic Cancer After Previous Gemcitabine-Based Therapy (NAPOLI-1): A Global, Randomised, Open-Label, Phase 3 Trial. Lancet. 2016;387:545–557. doi: 10.1016/S0140-6736(15)00986-1. [DOI] [PubMed] [Google Scholar]
- 9.Ueno M., Nakamori S., Sugimori K., Kazuya K.M., Kawabe K., Furuse J., Komatsu Y., Ishii H., Sato S., Shimizu S., et al. Nal-IRI+5-FU/LV Versus 5-FU/LV in Post-Gemcitabine Metastatic Pancreatic Cancer: Randomized Phase 2 Trial in Japanese Patients. Cancer Med. 2020;924:9396–9408. doi: 10.1002/cam4.3558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J.C., Kim J.W., Ahn S., Kim H.W., Lee J., Kim Y.H., Paik K.H., Kim J., Hwang J.H. Optimal Dose Reduction of FOLFIRINOX for Preserving Tumour Response in Advanced Pancreatic Cancer: Using Cumulative Relative Dose Intensity. Eur. J. Cancer. 2017;76:125–133. doi: 10.1016/j.ejca.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 11.Kanda Y. Investigation of the Freely Available Easy-to-Use Software “EZR” for Medical Statistics. Bone Marrow Transplant. 2013;48:452–458. doi: 10.1038/bmt.2012.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bang Y.J., Li C.P., Lee K.H., Chiu C.F., Park J.O., Shan Y.S., Kim J.S., Chen J.S., Shim H.J., Rau K.M., et al. Liposomal Irinotecan in Metastatic Pancreatic Adenocarcinoma in Asian Patients: Subgroup Analysis of the NAPOLI-1 Study. Cancer Sci. 2020;111:513–527. doi: 10.1111/cas.14264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith C.J., Bekaii-Saab T.S., Cook K.D., Eiring R.A., Halfdanarson T.R., Hanna M., Jin Z., Jochum J.A., Ma W.W., Mitchell J.L., et al. Nanoliposomal Irinotecan (Nal-IRI)-Based Chemotherapy After Irinotecan -Based Chemotherapy in Patients with Pancreas Cancer. Pancreatology. 2021;21:379–383. doi: 10.1016/j.pan.2020.10.042. [DOI] [PubMed] [Google Scholar]
- 14.Yu H.Y., Lee C.Y., Lin L.G., Chao Y., Li C.P. Nanoliposomal irinotecan with 5-fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy: A real-world experience. J. Chin. Med. Assoc. 2022;85:42–50. doi: 10.1097/JCMA.0000000000000650. [DOI] [PubMed] [Google Scholar]
- 15.Park S.J., Kim H., Shin K., Hong T.H., Suh J.H., Lee M.A. Nanoliposomal Irinotecan plus Fluorouracil and Folinic Acid as a Second-Line Treatment Option in Patients with Metastatic Pancreatic Ductal Adenocarcinoma: A Retrospective Cohort Study. BMC Cancer. 2021;21:211. doi: 10.1186/s12885-021-08887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Su Y.Y., Chiang N.J., Tsai H.J., Yen C.J., Shan Y.S., Chen L.T. The Impact of Liposomal Irinotecan on the Treatment of Advanced Pancreatic Adenocarcinoma: Real-World Experience in a Taiwanese Cohort. Sci. Rep. 2020;10:101. doi: 10.1038/s41598-020-64421-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kasi A., McGinnis T., Naik G., Handa S., Williams G., Paluri R. Efficacy and Tolerability of the Combination of Nano-liposomal Irinotecan and 5-Fluorouracil/Leucovorin in Advanced Pancreatic Adenocarcinoma: Post-approval Clinic Experience. J. Gastrointest. Oncol. 2021;12:464–473. doi: 10.21037/jgo-20-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glassman D.C., Palmaira R.L., Covington C.M., Desai A.M., Ku G.Y., Li J., Harding J.J., Varghese A.M., O’Reilly E.M., Yu K.H. Nanoliposomal Irinotecan with Fluorouracil for the Treatment of Advanced Pancreatic Cancer, a Single Institution Experience. BMC Cancer. 2018;18:693. doi: 10.1186/s12885-018-4605-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wainberg Z.A., Feeney K., Lee M.A., Muñoz A., Gracián A.C., Lonardi S., Ryoo B.Y., Hung A., Lin Y., Bendell J., et al. Meta-analysis Examining Overall Survival in Patients with Pancreatic Cancer Treated with Second-Line 5-Fluorouracil and Oxaliplatin-Based Therapy After Failing First-Line Gemcitabine-Containing Therapy: Effect of Performance Status and Comparison with Other Regimens. BMC Cancer. 2020;20:633. doi: 10.1186/s12885-020-07110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh D., Pyo J.S., Son B.K. Prognostic Roles of Inflammatory Markers in Pancreatic Cancer: Comparison Between the Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio. Gastroenterol. Res. Pract. 2018;2018:9745601. doi: 10.1155/2018/9745601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu R.J., Ma J.Y., Hu G. Lymphocyte-to-Monocyte Ratio in Pancreatic Cancer: Prognostic Significance and Meta-analysis. Clin. Chim. Acta. 2018;481:142–146. doi: 10.1016/j.cca.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 22.Wang-Gillam A., Hubner R.A., Siveke J.T., Von Hoff D.D., Belanger B., de Jong F.A., Mirakhur B., Chen L.-T. NAPOLI-1 Phase 3 Study of Liposomal Irinotecan in Metastatic Pancreatic Cancer: Final Overall Survival Analysis and Characteristics of Long-Term Survivors. Eur. J. Cancer. 2019;108:78–87. doi: 10.1016/j.ejca.2018.12.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.