The emphasis on timely coronary reperfusion in the setting of ST-segment elevation Myocardial Infarction (STEMI) comes from older studies suggesting a significant reduction in mortality among patients treated with fibrinolytic therapy during the first hours after onset of symptoms and a progressive increase in fatal events in those presenting later [1,2,3,4]. In the LATE (Late Assessment of Thrombolytic Efficacy) study, the benefit of fibrinolytic treatment observed in patients presenting early after STEMI onset was not consistent in those enrolled between 12 and 24 h after the onset of chest pain [5]. Later, with the advent and wide usage of percutaneous coronary intervention (PCI) as the preferred method of reperfusion, the question of timing has become more relevant ([6], and international guidelines, based on previous studies on thrombolysis, meta-regression analyses, and in vivo series, recommended coronary revascularization within the first 12 h from symptoms onset [7,8,9].
Pathophysiological studies in animal models suggested the development of irreversible myocardial damage in the first hours after coronary ligation [10,11]. In particular, in mouse models of myocardial infarction with temporary ligation (the so-called “ischemia-reperfusion model”), researchers found that ischemic periods up to 2 h resulted in ischemic-reperfusion infarct sizes of 30%, similarly to the permanent ligation [12,13]. These in vivo studies are in accordance with results from observational studies, which found a direct correlation between survival rates and long-term outcomes when patients were stratified by door-to-balloon time [14,15].
However, unlike what was found in experimental infarction models, a minimal blood flow in the culprit infarcted artery, the possibility of intermittent occlusion, and the presence of collateral vessels could ensure a blood supply sufficient to avoid total necrosis and preserve viable myocardium [16]. To note, rodent and pig models of myocardial infarction are characterized by a nearly complete absence of myocardial collateral circulation [17].
Notably, the overall individual risk profile can widely vary in relation to clinical presentation, cardiovascular risk, and comorbidities. In addition, the occurrence of several chronic ischemic episodes could lead to the development of collateral circulation, which is associated with a better outcome (i.e., lower incidence of cardiogenic shock) [18]. Finally, spontaneous preconditioning and postconditioning may slow the progression of ischemic myocardium to necrosis [19].
A pathological study conducted in 211 patients with STEMI to assess the intracoronary thrombi composition found that in almost half of patients the thrombus presented lytic or organized changes, compatible with an origin of days or weeks before the occlusive event [20]. A similar study showed lytic or organized thrombi in one-third of the cases early after symptom onset (<12 h) and no associations between thrombus composition and epicardial reperfusion grade or the presence of the no-reflow phenomenon [21]. It could therefore be hypothesized that the mechanisms underlying the instability of atherosclerotic plaque occurred several days before symptoms onset, without a strict correlation between them. Therefore, a benefit of mechanical reperfusion could be obtained even behind the recommended 12 h from the symptoms’ onset.
The evidence of myocardial salvage as a result of PCI in late presenters has been investigated in several studies using single-photon emission computed tomography (SPECT) or cardiac magnetic resonance (CMR) imaging. In a study by Schömig et al., 365 asymptomatic STEMI patients, presenting between 12 and 48 h, were randomized to a conservative or an invasive strategy. A significantly reduced infarct size on SPECT was found in the invasive-managed arm, with a not significant trend for a reduction in the secondary combined endpoint of death, recurrent MI, and stroke at 30 days [22]. Accordingly, other studies compared early (<12 h of symptom onset) and late (12–48 h of symptom onset) presenting STEMI patients using CMR. Although these studies documented a larger infarct size and a decreased myocardial salvage in late presenters, the revascularization was still beneficial in these patients, with the possible salvage of the area at risk of >25% [23,24].
Recently, in the FAST-MI (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) registry, 1169 STEMI patients presenting between 12 and 48 h from symptom onset were retrospectively compared with 5104 early comers with STEMI. Late presenters were less likely to receive revascularization. Among PCI-treated patients, compared to those treated medically, all-cause death was significantly lower at 30 days follow-up, with a survival benefit that persisted at 58 months. In multivariate analysis, revascularization of late-comers STEMI patients was independently associated with a significant reduction in mortality occurrence [25]. Accordingly, in an analysis of 910 STEMI patients presenting between 12 and 24 h, invasively treated patients had a significantly lower 12-month mortality compared to those managed conservatively [26].
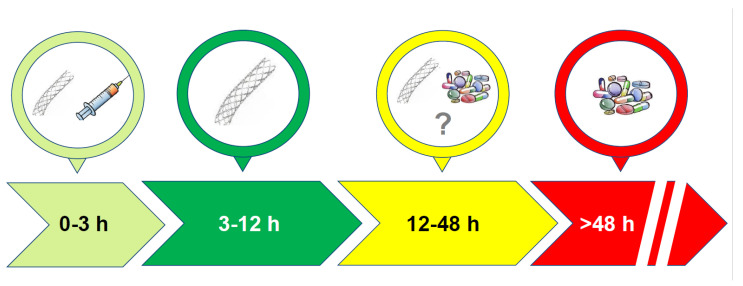
The overall incidence of late presenters amounts to 15–20% of patients [27,28], and they present with more severe symptoms compared to those who present within 12 h. According to observational studies and registries, these patients are more frequently older and female, with a major prevalence of diabetes mellitus, hypertension, and atypical chest pain at presentation that could be responsible for the delayed hospital admission or correct diagnosis [22,29]. Notably, during the outbreak of SARS-CoV-2, there was an increase in late presenters, as evidenced by some registries [30,31], that led to a significant reduction in the number of pPCIs and an unsurprising increase in AMI complications [32]. The increased likelihood of not undergoing coronary revascularization could contribute to the worse long-term prognosis of late presenters with STEMI [33]. Both in-hospital and up to 3 years of follow-up, the prognosis is worse in proportion to the onset of symptoms [34]. On the other side of the coin, the benefits of revascularization are dubious. Revascularization with PCI in very late presenters (3–28 days) in the OAT (Occluded Artery Trial) study neither led to less mortality rates nor improved left ventricle ejection fraction during 4-year follow-up compared with medical therapy [35]. Similarly, in the DECOPI (DEsobstruction COronaire en Post-Infarctus) study, in which 212 asymptomatic patients with Q-wave on ECG were randomized to PCI or medical therapy, even though invasive treatment was associated with significant improvement in the left ventricular ejection fraction, there was no benefit at 34 months of follow up in terms of cardiac death, non-fatal MI, or ventricular tachyarrhythmia [36]. Therefore, there is clear evidence for a lack of benefit for PCI in STEMI patients admitted to the hospital later than 3 days from symptoms’ onset, but pathophysiological and retrospective observational studies suggest an advantage of coronary revascularization in those presenting from 12 to 72 h from the onset of chest pain (Figure 1).
Figure 1.
Schematic representation of the evidence on the benefits of coronary revascularization according to patients’ presentation to hospital after the onset of symptoms.
In this regard, the European Guidelines recommend pPCI in patients presenting with ECG evidence or symptoms consistent with ongoing ischemia, heart failure, shock, or malignant arrhythmias (class I recommendation). In the time window of 12–48 h, routine PCI should be considered in all patients (class IIa). For those presenting beyond 48 h, as resulting from an OAT trial, the ESC discourages routine PCI of the culprit artery (class III), and, similar to chronic occlusion, it is possible to perform either angiography or a non-invasive test for the evaluation of residual myocardial ischemia/viability [7]. The North American Guidelines suggest pPCI between 12 and 24 h of onset only if there is clinical and/or ECG evidence of ongoing ischemia (class IIa) and recommend pPCI for patients with STEMI and cardiogenic shock or acute severe heart failure regardless of the time of onset of symptoms (class I) [8].
In conclusion, STEMI patients with symptoms occurring between 12 and 72 h are increasing and represent a challenge for clinical and interventional cardiologists, with scarce evidence regarding the benefit of revascularization and current pharmacological treatments [22,28]. Therefore, even more than in previous years, there is a need for dedicated prospective studies in order to identify the best management for late presenters with STEMI.
Author Contributions
Conceptualization, L.D.L.; writing—original draft preparation, L.D.L. and F.A.V.; writing—review and editing, L.D.L. and M.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gruppo Italiano per lo Studio della Streptochinasi nell’Infarto Miocardico (GISSI) Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986;1:397–402. [PubMed] [Google Scholar]
- 2.Fibrinolytic Therapy Trialists’ (FTT) Collaborative Group Indications for fibrinolytic therapy in suspected acute myocardial infarction: Collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet. 1994;343:311–322. doi: 10.1016/S0140-6736(94)91161-4. [DOI] [PubMed] [Google Scholar]
- 3.Nallamothu B.K., Bates E.R. Percutaneous coronary intervention versus fibrinolytic therapy in acute myocardial infarction: Is timing (almost) everything? Am. J. Cardiol. 2003;92:824–826. doi: 10.1016/S0002-9149(03)00891-9. [DOI] [PubMed] [Google Scholar]
- 4.Boersma E., Maas A.C., Deckers J.W., Simoons M.L. Early thrombolytic treatment in acute myocardial infarction: Reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 5.LATE Study Group Late Assessment of Thrombolytic Efficacy (LATE) study with alteplase 6-24 hours after onset of acute myocardial infarction. Lancet. 1993;342:759–766. doi: 10.1016/0140-6736(93)91538-W. [DOI] [PubMed] [Google Scholar]
- 6.Boersma E., Primary Coronary Angioplasty vs. Thrombolysis Group Does time matter? A pooled analysis of randomized clinical trials comparing primary percutaneous coronary intervention and in-hospital fibrinolysis in acute myocardial infarction patients. Eur. Heart J. 2006;27:779–788. doi: 10.1093/eurheartj/ehi810. [DOI] [PubMed] [Google Scholar]
- 7.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H., Caforio A., Crea F., Goudevenos J.A., Halvorsen S., et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 8.O’Gara P.T., Kushner F.G., Ascheim D.D., Casey D.E., Jr., Chung M.K., de Lemos J.A., Ettinger S.M., Fang J.C., Fesmire F.M., Franklin B.A., et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong P.W., Gershlick A.H., Goldstein P., Wilcox R., Danays T., Lambert Y., Sulimov V., Rosell Ortiz F., Ostojic M., Welsh R.C., et al. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N. Engl. J. Med. 2013;368:1379–1387. doi: 10.1056/NEJMoa1301092. [DOI] [PubMed] [Google Scholar]
- 10.Viehman G.E., Ma X.L., Lefer D.J., Lefer A.M. Time course of endothelial dysfunction and myocardial injury during coronary arterial occlusion. Am. J. Physiol. 1991;261:H874–H881. doi: 10.1152/ajpheart.1991.261.3.H874. [DOI] [PubMed] [Google Scholar]
- 11.Reimer K.A., Vander Heide R.S., Richard V.J. Reperfusion in acute myocardial infarction: Effect of timing and modulating factors in experimental models. Am. J. Cardiol. 1993;72:13G–21G. doi: 10.1016/0002-9149(93)90102-I. [DOI] [PubMed] [Google Scholar]
- 12.De Villiers C., Riley P.R. Mouse models of myocardial infarction: Comparing permanent ligation and ischaemia-reperfusion. Dis. Models Mech. 2020;13:dmm046565. doi: 10.1242/dmm.046565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michael L.H., Ballantyne C.M., Zachariah J.P., Gould K.E., Pocius J.S., Taffet G.E., Hartley C.J., Pham T.T., Daniel S.L., Funk E., et al. Myocardial infarction and remodeling in mice: Effect of reperfusion. Am. J. Physiol. 1999;277:H660–H668. doi: 10.1152/ajpheart.1999.277.2.H660. [DOI] [PubMed] [Google Scholar]
- 14.Rollando D., Puggioni E., Robotti S., De Lisi A., Ferrari Bravo M., Vardanega A., Pattaro I., De Benedetti F., Brignole M. Symptom onset-to-balloon time and mortality in the first seven years after STEMI treated with primary percutaneous coronary intervention. Heart. 2012;98:1738–1742. doi: 10.1136/heartjnl-2012-302536. [DOI] [PubMed] [Google Scholar]
- 15.Shiomi H., Nakagawa Y., Morimoto T., Furukawa Y., Nakano A., Shirai S., Taniguchi R., Yamaji K., Nagao K., Suyama T., et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: Observational study. BMJ. 2012;344:e3257. doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 16.Schömig A., Ndrepepa G., Kastrati A. Late myocardial salvage: Time to recognize its reality in the reperfusion therapy of acute myocardial infarction. Eur. Heart J. 2006;27:1900–1907. doi: 10.1093/eurheartj/ehl174. [DOI] [PubMed] [Google Scholar]
- 17.Maxwell M.P., Hearse D.J., Yellon D.M. Species variation in the coronary collateral circulation during regional myocardial ischaemia: A critical determinant of the rate of evolution and extent of myocardial infarction. Cardiovasc. Res. 1987;21:737–746. doi: 10.1093/cvr/21.10.737. [DOI] [PubMed] [Google Scholar]
- 18.Kern M.J., Seto A.H. Collaterals in STEMI patients: An uncommon but critical lifeline. Catheter. Cardiovasc. Interv. 2020;96:534–535. doi: 10.1002/ccd.29208. [DOI] [PubMed] [Google Scholar]
- 19.Reiter R., Henry T.D., Traverse J.H. Preinfarction angina reduces infarct size in ST-elevation myocardial infarction treated with percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 2013;6:52–58. doi: 10.1161/CIRCINTERVENTIONS.112.973164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rittersma S.Z., van der Wal A.C., Koch K.T., Piek J.J., Henriques J.P., Mulder K.J., Ploegmakers J.P., Meesterman M., de Winter R.J. Plaque instability frequently occurs days or weeks before occlusive coronary thrombosis: A pathological thrombectomy study in primary percutaneous coronary intervention. Circulation. 2005;111:1160–1165. doi: 10.1161/01.CIR.0000157141.00778.AC. [DOI] [PubMed] [Google Scholar]
- 21.Carol A., Bernet M., Curós A., Rodríguez-Leor O., Serra J., Fernández-Nofrerías E., Mauri J., Bayes-Genís A. Thrombus age, clinical presentation, and reperfusion grade in myocardial infarction. Cardiovasc. Path. 2014;23:126–130. doi: 10.1016/j.carpath.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 22.Schömig A., Mehilli J., Antoniucci D., Ndrepepa G., Markwardt C., Di Pede F., Nekolla S.G., Schlotterbeck K., Schühlen H., Pache J., et al. Mechanical reperfusion in patients with acute myocardial infarction presenting more than 12 hours from symptom onset: A randomized controlled trial. JAMA. 2005;293:2865–2872. doi: 10.1001/jama.293.23.2865. [DOI] [PubMed] [Google Scholar]
- 23.Stiermaier T., Eitel I., de Waha S., Pöss J., Fuernau G., Thiele H., Desch S. Myocardial salvage after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction presenting early versus late after symptom onset. Int. J. Cardiovasc. Imaging. 2017;33:1571–1579. doi: 10.1007/s10554-017-1143-x. [DOI] [PubMed] [Google Scholar]
- 24.Nepper-Christensen L., Lønborg J., Høfsten D.E., Ahtarovski K.A., Bang L.E., Helqvist S., Kyhl K., Køber L., Kelbæk H., Vejlstrup N., et al. Benefit from Reperfusion With Primary Percutaneous Coronary Intervention Beyond 12 Hours of Symptom Duration in Patients With ST-Segment-Elevation Myocardial Infarction. Circulation. Cardiovasc. Interv. 2018;11:e006842. doi: 10.1161/CIRCINTERVENTIONS.118.006842. [DOI] [PubMed] [Google Scholar]
- 25.Bouisset F., Gerbaud E., Bataille V., Coste P., Puymirat E., Belle L., Delmas C., Cayla G., Motreff P., Lemesle G., et al. Percutaneous Myocardial Revascularization in Late-Presenting Patients With STEMI. J. Am. Coll. Cardiol. 2021;78:1291–1305. doi: 10.1016/j.jacc.2021.07.039. [DOI] [PubMed] [Google Scholar]
- 26.Gierlotka M., Gasior M., Wilczek K., Hawranek M., Szkodzinski J., Paczek P., Lekston A., Kalarus Z., Zembala M., Polonski L. Reperfusion by primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction within 12 to 24 hours of the onset of symptoms (from a prospective national observational study [PL-ACS]) Am. J. Cardiol. 2011;107:501–508. doi: 10.1016/j.amjcard.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 27.Roberto M., Radovanovic D., de Benedetti E., Biasco L., Halasz G., Quagliana A., Erne P., Rickli H., Pedrazzini G., Moccetti M. Temporal trends in latecomer STEMI patients: Insights from the AMIS Plus registry 1997–2017. Rev. Esp. Cardiol. 2020;73:741–748. doi: 10.1016/j.recesp.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 28.De Luca L., Marini M., Gonzini L., Boccanelli A., Casella G., Chiarella F., De Servi S., Di Chiara A., Di Pasquale G., Olivari Z., et al. Contemporary Trends and Age-Specific Sex Differences in Management and Outcome for Patients With ST-Segment Elevation Myocardial Infarction. J. Am. Heart Assoc. 2016;5:e004202. doi: 10.1161/JAHA.116.004202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McNair P.W., Bilchick K.C., Keeley E.C. Very late presentation in ST elevation myocardial infarction: Predictors and long-term mortality. International journal of cardiology. Heart Vasc. 2019;22:156–159. doi: 10.1016/j.ijcha.2019.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiang D., Xiang X., Zhang W., Yi S., Zhang J., Gu X., Xu Y., Huang K., Su X., Yu B., et al. Management and Outcomes of Patients with STEMI During the COVID-19 Pandemic in China. J. Am. Coll. Cardiol. 2020;76:1318–1324. doi: 10.1016/j.jacc.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abdelaziz H.K., Abdelrahman A., Nabi A., Debski M., Mentias A., Choudhury T., Patel B., Saad M. Impact of COVID-19 pandemic on patients with ST-segment elevation myocardial infarction: Insights from a British cardiac center. Am. Heart J. 2020;226:45–48. doi: 10.1016/j.ahj.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kitahara S., Fujino M., Honda S., Asaumi Y., Kataoka Y., Otsuka F., Nakanishi M., Tahara Y., Ogata S., Onozuka D., et al. COVID-19 pandemic is associated with mechanical complications in patients with ST-elevation myocardial infarction. Open Heart. 2021;8:e001497. doi: 10.1136/openhrt-2020-001497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.De Luca L., Leonardi S., Smecca I.M., Formigli D., Lucci D., Gonzini L., Tuccillo B., Olivari Z., Gulizia M.M., Bovenzi F.M., et al. Contemporary antithrombotic strategies in patients with acute coronary syndromes managed without revascularization: Insights from the EYESHOT study. Eur. Heart J. Cardiovasc. Pharmacother. 2015;1:168–178. doi: 10.1093/ehjcvp/pvv006. [DOI] [PubMed] [Google Scholar]
- 34.Cho K.H., Han X., Ahn J.H., Hyun D.Y., Kim M.C., Sim D.S., Hong Y.J., Kim J.H., Ahn Y., Hwang J.Y., et al. Long-Term Outcomes of Patients with Late Presentation of ST-Segment Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2021;77:1859–1870. doi: 10.1016/j.jacc.2021.02.041. [DOI] [PubMed] [Google Scholar]
- 35.Udelson J.E., Pearte C.A., Kimmelstiel C.D., Kruk M., Kufera J.A., Forman S.A., Teresinska A., Bychowiec B., Marin-Neto J.A., Höchtl T., et al. The Occluded Artery Trial (OAT) Viability Ancillary Study (OAT-NUC): Influence of infarct zone viability on left ventricular remodeling after percutaneous coronary intervention versus optimal medical therapy alone. Am. Heart J. 2011;161:611–621. doi: 10.1016/j.ahj.2010.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Steg P.G., Thuaire C., Himbert D., Carrié D., Champagne S., Coisne D., Khalifé K., Cazaux P., Logeart D., Slama M., et al. DECOPI (DEsobstruction COronaire en Post-Infarctus): A randomized multi-centre trial of occluded artery angioplasty after acute myocardial infarction. Eur. Heart J. 2004;25:2187–2194. doi: 10.1016/j.ehj.2004.10.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.