Abstract
Background
The COVID-19 pandemic and its accompanying containment measures can be conceptualized as traumatic events. This review systematically investigates trauma-related symptoms in the course of the COVID-19 pandemic and the association of the pandemic and its containment measures with trauma-related disorders or symptoms.
Methods
The EBSCO (MEDLINE, PsycINFO, PsycARTICLES, PSYNDEX), Cochrane Library, and Web of Science databases were searched in June 2021. The Quality Assessment Tool for Quantitative Studies (EPHPP-QAT; Thomas et al., 2004) was applied. Studies conceptualizing the COVID-19 pandemic as a traumatic event and assessing typically developing children and adolescents (under 18 years), and/or caregivers (at least 18 years) were included.
Results and limitations
22 primary studies including 27,322 participants were evaluated. Only three primary studies executed a statistical comparison with pre-pandemic or retrospective data, showing a negative impact of the COVID-19 pandemic and its associated measures on children's and caregiver's internalizing symptoms and hyperactivity. In the majority of the remaining studies, prevalence rates of various trauma sequelae in children, adolescents, and caregivers were reported to be descriptively higher in the context of the COVID-19 pandemic when compared to other pre-pandemic studies. However, due to numerous methodological differences between these studies the statement that the pandemic is associated with higher prevalence rates of trauma-associated symptoms cannot be validly answered at this point.
Conclusion
Due to some methodological shortcomings of the primary studies, our results might be cautiously interpreted as a first indicator of an association between the COVID-19 pandemic and trauma sequelae.
Keywords: COVID-19, Trauma, Child, Adolescent, Parent, Families
1. Introduction
On December 31, 2019, the WHO was notified of cases of pneumonia with unknown cause in the Chinese city of Wuhan. In early January 2020, scientists succeeded in identifying the cause, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; WHO, 2021). In February 2020, the WHO named the illness caused by SARS-CoV-2 COVID-19 (WHO, 2021). There have been 281,808,270 confirmed cases of COVID-19 infection worldwide, with at least 5,411,759 deaths, since the beginning of the pandemic through 2021, December 29 (WHO, 2021). To control transmission of the disease, public health sanitary and social measures have been implemented in countless countries, including so-called “lockdowns”, travel restrictions, hygiene measures such as the use of masks, and the closure of non-essential businesses and services, including schools (Robert Koch-Institut, 2021).
The pandemic and associated measures pose a serious threat not only to physical but also to mental health. Current research suggests that in the aftermath of the COVID-19 pandemic and associated measures, one in five people could develop clinically relevant psychological distress - specifically, depression, anxiety disorders, and post-traumatic stress disorder (PTSD; Cavicchioli et al., 2021; Cenat et al., 2021; Fan et al., 2021).
Special attention should be paid to children and their caregivers. The prevalence of COVID-19 in children is low, and most children show only mild physical symptoms or are asymptomatic (Lou et al., 2021; Ludvigsson, 2020; as cited in Robert Koch-Institut, 2021). Although COVID-19 is not as severe and deadly in children as in adults, they may be particularly vulnerable to the psychological effects of the COVID-19 pandemic. Coping with the current situation and adhering to current restrictions may be stressful for children and adolescents, as these circumstances may be experienced as incongruent with their developmental tasks (Fegert et al., 2020). A rapid systematic review by Loades et al. (2020), which aimed to answer the question how loneliness and disease containment measures impact children's and adolescents' mental health, revealed that children and adolescents are probably more likely to show high rates of depression and most likely anxiety during and after enforced isolation (like quarantine) ends. The authors suggest that this may be due to the important role of the peer group for identity and support at this developmental stage. At this point, however, it should be mentioned that the COVID-19 restrictions are also intended to reduce worries and to increase beliefs in the ability to control the outbreak (Mækelæ et al., 2020). Additionally, it may be possible that some children and adolescents experience less mental health problems due to reduced school and/or social stress (Cost et al., 2022).
Children and adolescents' well-being is also closely linked to the physical, mental, and social health of their caregivers (Prime et al., 2020). In addition to their own stresses and strains, including their own health concerns, as well as some major changes in their working environment, they carry the responsibility for the safety of their children (Russell et al., 2020). Hence, it is not surprising that in a retrospective study design parents reported worsening mental health for themselves in June 2020 compared to March 2020 during the beginning of the pandemic (Patrick et al., 2020). Additionally, the UK Household Longitudinal Study (UKHLS) panel reported rising levels of clinically significant mental distress, especially in people living with young children (Pierce et al., 2020).
As illustrated, diverse emotional reactions and psychological distress can be seen as common consequences of a global health crisis. Furthermore, recent meta-analyses indicate that infectious disease epidemics and pandemics can lead to trauma-related symptoms (Fan et al., 2021; Qiu et al., 2021; Yuan et al., 2021). Numerous articles refer to the COVID-19 pandemic and its associated measures as traumatic experiences (Cénat and Dalexis, 2020; Liang et al., 2020; Masiero et al., 2020; Restauri and Sheridan, 2020). At this point, it must be emphasized that there are discussions about the extent to which the COVID-19 situation can actually be defined as trauma (e.g., Bridgland et al., 2021). This discussion is based on the difficulty that currently no universally valid definition of trauma exists. For instance, the ICD-10 (WHO, 2016) categorizes trauma as an event or series of events of extraordinary threat or catastrophic magnitude that would cause deep distress in almost any person. The DSM-5, on the other hand, defines trauma as a confrontation with actual or threatened death, serious injury, or sexual violence (APA, 2013). Thus, exposure to the pandemic does not entirely fit every trauma definition such as the DSM-5 trauma definition (APA, 2013). However, Bridgland et al. (2021) suggest a rethinking of this understanding of trauma. The authors assume that people's traumatic stress responses to the COVID-19 pandemic may relate more to the future than to the past, more to indirect (e.g., media coverage) than to direct exposure (e.g., contact with the virus), and to stressful events (e.g., isolation) which do not meet DSM-5 Criterion A (e.g., actual or threatened death). Moreover, other trauma definitions may be suitable and more specifically depict the COVID-19 experience. Fischer and Riedesser (2009) define a psychotrauma as a vital experience that raises a discrepancy between a threat and the individual's coping capabilities. In addition, it is accompanied by feelings of defenselessness and powerlessness, and thus leads to permanent changes in the perception of the world and the self (Fischer and Riedesser, 2009).
Further, some authors refer to the COVID-19 pandemic and its measures as a “collective trauma” (Duane et al., 2020; Horesh and Brown, 2020; Watson et al., 2020), defined as the psychological response of an entire group to a traumatic event, such as the Holocaust (Watson et al., 2020). In this way, the experience of the COVID-19 pandemic is shared globally and emotionally connects people around the world through helplessness, uncertainty, loss, and grief. Ultimately, collective trauma can unsettle community connections, and fundamentally alter aspects of community functioning.
Based on the foregoing, the issue of trauma and its associated disorders and symptoms is particularly central to the context of the COVID-19 pandemic. Child and adolescent health are one of the most important issues in the Sustainable Development Goals (SDGs; United Nations, 2017), and in stressful situations such as a pandemic, maintaining the well-being of children and adolescents requires special attention. At this point, caregiver mental health also plays a critical role, as it is strongly associated to child well-being (Prime et al., 2020). Several reviews exist that have examined the psychological impact of the COVID-19 pandemic and related interventions on children, adolescents, and caregivers (Araújo et al., 2020; Fong and Iarocci, 2020; Fegert et al., 2020; Guessoum et al., 2020; Imran et al., 2020; Marques de Miranda et al., 2020; Stavridou et al., 2020).
However, to the authors' knowledge, there are no systematic reviews to date that consider studies that conceptualize COVID-19 and its associated measures as traumatic events, as well as examine the trauma-related psychological consequences for families (children, adolescents, and caregivers). In addition, several months have passed since the above reviews were conducted and more recent studies have most likely been published within this time frame. As COVID-19 as a traumatic event may alter aspects of community functioning (Watson et al., 2020) and lead to permanent changes in the perception of the world and the self (Fischer and Riedesser, 2009) which may cause a high level of suffering, a systematic study of these longer lasting effects and symptoms is of particular importance. A systematic review may provide a first idea and overview of how highly COVID-19 as a traumatic event is associated with trauma-related disorders and symptoms.
1.1. Objectives and research question
Accordingly, the research gap on the crucial topic of trauma and associated psychological impact on families in the context of the COVID-19 pandemic will be addressed. Results could potentially play a key role in guiding future policy decisions regarding the organization of public health systems, and as well as in informing the development and adaptation of both prevention measures and interventions for families.
Therefore, this systematic review aimed to answer the pre-registered question whether the COVID-19 pandemic and its containment measures are associated with trauma-related disorders or symptoms in children, adolescents, and caregivers. As not enough primary studies including pre-pandemic control groups could be found to validly draw conclusions on changes in the prevalence of traumatic symptoms, we additionally provide a narrative summary of studies which have measured trauma-related disorders or symptoms during the pandemic. Thus, this study primarily serves as a narrative description of the state of research on studies that have addressed trauma symptoms in the context of the COVID-19 pandemic.
2. Methods
2.1. Protocol and preregistration
The recommendations for the reproducibility of meta-analyses by Lakens et al. (2016) will be adapted for the procedure of this systematic review:
-
(1)
To ensure structured and thorough reporting, this systematic review adheres to the PRISMA guidelines (Page et al., 2021).
-
(2)
Prior to commencing the systematic literature search and data collection, the theory and methods sections of this paper were preregistered on the Open Science Framework (OSF; https://osf.io/j5atd), specifying and documenting the research questions, search strategies, inclusion and exclusion criteria, and outcome measures.
-
(3)
Any relevant data and results involved in this systematic review were disclosed on the OSF (https://osf.io/u98n2/) to encourage re-analysis and verification of results by independent researchers.
-
(4)
Expert librarian knowledge was not used within this work. Nevertheless, to ensure the traceability of the research process, previously proven search terms were used for the literature search and all results of the literature search were made available in common data formats on OSF (https://osf.io/u98n2/).
2.2. Outcome measures
To provide a broad overview of the field of research on trauma sequelae disorders in the context of the COVID-19 pandemic, outcome measures were defined in a broad manner. Different developmental pathways exist after a traumatic event, whereby trauma can be reflected in trauma sequelae as well as in other disorder patterns (Maercker, 2019). For a comprehensive description of the psychological consequences of a pandemic conceptualized as a trauma, outcome measures of trauma sequelae were primarily considered. Additionally, measurement instruments of other disorders and their symptoms, associated with trauma were included.
Clinical interviews based on international diagnostic manuals such as ICD-10 (WHO, 2016) and DSM-5 (APA, 2013) represent reliable and valid measurement tools for assessing psychological consequences after traumatic events such as the Structured Clinical Interview for DSM-5 (SCID-5; First et al., 2015). These can be used to identify trauma sequelae disorders such as PTSD, as well as diagnoses associated with trauma, such as depression. Additionally, there are numerous validated instruments based on self-reports to assess trauma sequelae in children, adolescents, and adults, such as the Impact of Event Scale in its revised form (IES-R; Weiss and Marmar, 1996) regarding adults and the Children's Revised Impact of Event Scale (CRIES; Perrin et al., 2005) for children eight years of age and older.
2.3. Eligibility criteria
Following the PICOS specifications for systematic reviews (Page et al., 2021) the population of interest (P), the intervention (I), the comparison group (C), the outcomes examined (O), and the study design (S) were defined. Therefore, the following inclusion criteria were established to select primary studies:
P: Children and adolescents (under 18 years) and/or caregivers (at least 18 years) were studied. Within the concept of caregiving, all forms of primary parenting within the family were considered, such as adoptive parents, foster parents, or parenting grandparents. Studies focusing on pregnancy were not included. Children, adolescents, and caregivers were physically healthy prior to the COVID-19 pandemic. Individuals with previous traumatic experiences and mental disorders were included. However, participants suffering from autism spectrum disorder, or a mental disability were excluded.
I: Intervention studies were not considered in this systematic review.
C: No exclusion criteria for comparison groups have been specified.
O: The authors conceptualized the COVID-19 pandemic and its associated measures as traumatic events. Trauma sequelae or trauma-associated disorders in children, adolescents, and caregivers were assessed in the context of the COVID-19 pandemic, applying reliable and valid measurement instruments.
S: No exclusion criteria were established for the study design of quantitative studies. Qualitative studies were not included. The publication date was set to the time frame of the COVID-19 pandemic starting in December 2019.
Additionally: Studies could be conducted in any region of the world. However, study results needed to be published in English or German (whereas the keywords and abstracts had to have been published in English). According to the research question, randomization to experimental and control groups and blinding of subjects are not possible. Consequently, comparative nonrandomized primary studies and primary studies without control groups were included in this systematic review to comprehensively answer the research question.
2.4. Information sources and search
Electronic online databases EBSCO (MEDLINE, PsycINFO, PsycARTICLES, PSYNDEX), Cochrane Library, and Web of Science were searched on June 17 and June 18, 2021. Within the EBSCO database, the search was limited to the document types of journals and academic journals, within the Cochrane Library to cochrane reviews and trials, and at Web of Science to article, review, proceedings paper and meeting abstract. Apart from these restrictions, no other default settings of the databases were changed. The search terms were adapted to the research question investigated in this work based on a combination of already established search terms from previous systematic reviews with similar topics (Araújo et al., 2020; Fong and Iarocci, 2020; Fegert et al., 2020; Guessoum et al., 2020; Imran et al., 2020; Stavridou et al., 2020). A detailed listing of the search terms can be found in the Supplementary material, with the following keywords mentioned at this point: (corona* OR covid* OR pandem* OR sars-cov-2 OR coronavirus 2019 OR COVID* OR severe acute respiratory syndrome coronavirus 2) AND (trauma* OR posttraumatic OR peritraumatic) AND (paternal OR maternal OR parent* OR mother OR father OR caregiver OR child* OR kid* OR adolescen* OR youth OR teen* OR infan* OR postpartum OR postnatal OR famil* OR pediatric OR pediatric OR preadolesc* OR pubert*). In addition, a manual search of the references of relevant articles and systematic reviews was performed.
2.5. Study selection
Titles and abstracts of the identified studies were reviewed in the literature software EndNote 20 to check their relevance. If the information in the titles and abstracts were insufficient, the full texts were additionally explored. Study selection was conducted by the first author (LK) and checked by the last author (CW). In case of ambiguity, a four-person consensus was sought with the two additional researchers (AvT and CR).
2.6. Data collection
This systematic review was guided by previous reviews with similar questions and topics in terms of the data collection process (Araújo et al., 2020; Fong and Iarocci, 2020; Fegert et al., 2020; Guessoum et al., 2020; Imran et al., 2020; Stavridou et al., 2020). The following data was collected in each case: author name, publication year, place of study conduct (country), time of collection, study design, sample size, recruitment setting, measurement instrument used, age of participants, and other relevant characteristics of the sample and comparison group (marital status, education, gender, etc.), as well as relevant outcome data, such as prevalence rates, sum scores/cut-off scores of respective outcome measures, and comparisons between subsamples. Data was extracted by the first author (LK) using a standardized form on Microsoft Excel and was then checked by the last author (CW). Discrepancies were resolved through discussion. Furthermore, all extracted data and literature files were made available on the OSF (https://osf.io/u98n2/) to enable traceability of our entire study selection and data collection process.
2.7. Assessment of the risk of bias in individual trials
The methodological quality of the included trials was assured via the Quality Assessment Tool for Quantitative Studies by the Effective Public Health Practice Project (EPHPP-QAT; Thomas et al., 2004). It is an established instrument suitable for assessing the quality of studies with different study designs in health-related topics (Jackson and Waters, 2005; Thomas et al., 2004). The evaluation of the individual primary studies was performed by the first author and last author (LK, CW) for the following six components: Selection Bias (A), Study Design (B), Confounders (C), Blinding (D), Data Collection Methods (E), and Withdrawals and Dropouts (F). Each category contains subordinate items. Within the items, different scoring options are given. For instance, in the first item (Q1) of Selection Bias (A), the response options are Very likely, Somewhat likely, Not likely, and Can't tell. The instrument guidelines state that to score the study, each of the six sections (A – F) is rated as having a strong (1), moderate (2), or weak (3) methodological quality. Based on these component ratings, a global rating is formed, which depends on the sum of the components rated as weak (3) which is described in Table 1 . The rating will inform the interpretation of our results.
Table 1.
Overall assessment of methodological quality within a primary study and across all primary studies following Higgins et al. (2011).
| Methodical quality | Within trial | Across trials |
|---|---|---|
| Weak Methodical quality (3) |
Two or more weak (3) component ratings |
More than 50 % of the studies have a weak (3) global rating |
| Moderate Methodical quality (2) |
One weak (3) component rating | More than 50 % of the studies have a moderate (2) global rating |
| Strong Methodical quality (3) |
No weak (3) component rating | More than 50 % of the studies have a strong (1) global rating |
2.8. Changes to the pre-registration
The search term for the literature search had to be slightly altered to include additional relevant keywords (see Supplementary material). In addition, the inclusion criterion for control groups was relaxed as very few studies with group comparisons had been conducted. As a consequence, the focus and scope of this systematic review has shifted as mentioned at the end of the introduction section.
3. Results
3.1. Study and outcome selection
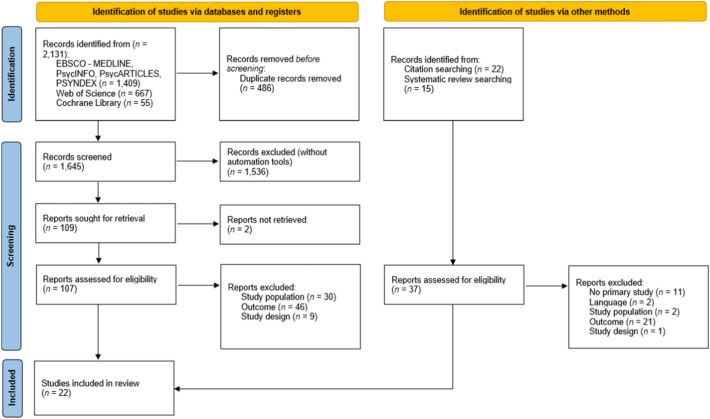
A total of 2131 articles were identified via the database search of EBSCO (MEDLINE, PsycINFO, PsycARTICLES, PSYNDEX; 1409), Cochrane Library (667), and Web of Science (55). Once duplicates were removed, 1645 articles remained to screen for inclusion. See Fig. 1 for a flow diagram of the full study selection process according to PRISMA (Page et al., 2021). Consequently, 22 studies were included in the systematic review. Notably, even though the search was conducted on June 17/18, 2021, all included primary studies in this systematic review were conducted prior to August 2020.
Fig. 1.
PRISMA 2020 (Page et al., 2021) flow diagram for included studies. Figure available at https://osf.io/u98n2/, under a CC-BY 4.0 license.
3.2. Overall summary of the included studies
Table 2, Table 3, Table 4 provide an overview of the main characteristics and main findings of the 22 included primary studies. More detailed versions of these tables (containing information regarding containment measures, which event was conceptualized as traumatic, sampling strategy, data collection method, and outcome measures, as well as their cut-off scores) were made available on the OSF (https://osf.io/u98n2/).
Table 2.
Main characteristics of included studies on trauma-related symptoms in the course of the COVID-19 pandemic among children and adolescents.
| Authors/date of publication | Study design; Country; Date of data collection; Sample characteristics |
Main findings |
|---|---|---|
| Cetin et al., 2020 | Cross-sectional (with comparison groups); Turkey; 2020, May 7–14; n = 76; Children (ADHD); Age range: 8–12 years; Age: M = 10.09 years (SD = 2.23); Gender ratio: 30.3 % female Parental marital status: 89.5 % married |
No prevalence rates reported; Children with ADHD and the Evening-chronotype exhibited significantly higher trauma symptoms and sleep problems compared to children with ADHD and the non-Evening-chronotype during the COVID-19 pandemic |
| Duan et al., 2020 | Cross-sectional; China (mainland); Not reported (during the spread of COVID-19 in China); n = 3613 students (359 children and 3254 adolescents); Age range: 7–18 years; Age: not reported; Gender ratio: 49.85 % female; Parental marital status: 68.56 % in nuclear family |
Depressive symptoms: 22.28 % (n = 805); Anxiety symptoms: reported to be descriptively higher than before the pandemic; Smartphone addiction: 13.06 % of females and 10.30 % of males; Internet addiction: 6.03 % (n = 218) |
| Guo et al., 2020 | Cross-sectional; China; 2020, February 8–27; n = 6196 students (with and without adverse childhood experiences); Age range: 11–18 years; Age: not reported; Gender ratio: 52.10 % female; Parental marital status: not reported |
No prevalence rates reported; Larger number of adverse childhood experiences predicted substantial higher levels of PTSS (effect size beta = 0.16 ∼ 0.27, respectively, p < .001) and anxiety (effect size beta = 0.32 ∼ 0.47, respectively, p < .001) during the COVID-19 pandemic |
| Karaman et al., 2021 | Cross-sectional; Turkey; 2020, May 15–25; n = 549 high school students; Age range: in grades 9–11; Age: M = 16.1 years (SD = 1.01); Gender ratio: 72.5 % female; Parental marital status: not reported |
PTSS: 36.6 % (n = 201) high impact of COVID-19 pandemic, and of these, 19.50 % (n = 107) severe impact of event/trauma symptomologies; SEM analysis indicated that IES-R scores had a total effect of 0.79 on anxiety, 0.75 on depression, 0.74 on negative self-concept, 0.68 on somatization, and 0.66 on hostility scores (respectively, p < .001) |
| Li et al., 2020 | Not reported; China (mainland; Hubei); 2020, January 31–February 8; n = 1172 children and adolescents (PTSD score of >17 (Perrin et al., 2005); and perceived COVID-19 as major stressful event experienced in the past 2 weeks); Age range: 8–18 years; Age: M = 12.80 years (SD = 1.64); Gender ratio: 58.28 % female; Parental marital status: not reported |
No prevalence rates reported; Total PTSD score was positively correlated with GAD (r = 0.16, p < .001), perceived threat of COVID-19 (r = 0.08, p < .01), and COVID-19-related courtesy stigma (r = 0.14, p < .001) |
| Ma et al., 2021 | Cross-sectional; China; 2020, April 11–17; n = 668 parents with children; Age range: 7–15 years; Age: not reported; Gender ratio: 49.7 % female; Parental marital status: 96.3 % married |
PTSD: 20.66 %; Depressive symptoms: 7.16 %; PTSD symptoms were significantly more prevalent in middle school (p = .05) and boarding school students (p = .004) compared to primary school and day school students, respectively; Depressive symptoms were also significantly more prevalent in middle school (p = .032) and boarding school students (p = .02) compared to primary and day school students, respectively |
| Moulin et al., 2021 | Cross-sectional in a longitudinal cohort study (over a duration of 5 weeks); France; 2020, March 24–April 28; n = 432 children; Age range: not reported; Age: M = 6.8 years (SD = 4.1); Gender ratio: 48.9 % female; Parental marital status: 59.8 % living together |
Emotional difficulties: 7.2 % (n = 31); Hyperactivity/inattention symptoms: 24.8 % (n = 107) |
| Shek et al., 2021 | Longitudinal (short-term); China (Chengdu); 2019, December 23–2020, January 13 January and 2020, June 16–2020, July 8; n = 4981 adolescents; Age range: 11–20 years; Age: M = 13.15 years (SD = 1.32); Gender ratio: 48.5 % female; Parental marital status: not reported |
PTSD: 10.4 % (n = 517); As expected, perceived threat of COVID-19 was positively associated with PTSD (r = 0.14, p < .001) |
| Wang et al., 2021 | Cross-sectional; China (Central China); 2020, May; n = 1488 adolescents; Age range: 12–16 years; Age: M = 13.85 years (SD = 0.891); Gender ratio: 43.88 % female; Parental marital status: not reported |
No prevalence rates reported; Female students (M = 9.38, SD = 6.11) scored higher than males (M = 8.61, SD = 5.71) on intrusive rumination (p < .05) during COVID-19 pandemic; Significant negative relationship (r = −0.14, p < .01) between emotional resilience and intrusive rumination; Creativity was positively related to adolescents' intrusive rumination (r = 0.21, p < .001) |
| Yang et al., 2020 | Not reported; China (Wuhan City); 2020, February 4–March 9; n = 286 high school students; Age range: in 10–12 grades; Age: not reported; Gender ratio: 53.8 % female; Parental marital status: not reported |
No prevalence rates reported; Psychological trauma was a negative predictor of mental health (Zhang et al., 2013) among high school students (p < .01) |
| Zhang et al., 2020 | Cross-sectional (with comparison groups); China (Guangdong); 2020, April 7–24; n = 1025 (493 junior high and 532 high school students); Age range: not reported; Age: M = 15.56 years (SD = 1.89); Gender ratio: 48.5 % female; Parental marital status: not reported |
PTSS: 20.5 % (n = 101) of junior high school students, 22.7 % (n = 121) of high school students; Depressive symptoms: 9.1 % of junior high school students, 6.8 % of high school students (moderate); 5.3 % of junior high school students, 2.6 % of high school students (severe to extremely severe); Anxiety symptoms: 10.3 % of junior high school students, 10.9 % of high school students (moderate); 10.0 % of junior high school students, 7.2 % of high school students (severe to extremely severe); significant between-group difference (p = .015); Stress symptoms: 5.9 % of junior high school students, 6.8 % of high school students (moderate); 3.0 % of junior high school students, 2.6 % of high school students (severe to extremely severe); significant between-group difference (p = .028) |
Note. M = mean; SD = standard deviation; p = p-value; n = sample size; PTSD = post-traumatic stress disorder; PTSS = post-traumatic stress symptoms; GAD = generalized anxiety disorder; ADHD = attention deficit hyperactivity disorder.
Table 3.
Main characteristics of included studies on trauma-related symptoms in the course of the COVID-19 pandemic and the association between COVID-19 and trauma-related symptoms among caregivers.
| Authors/date of publication | Study design; Country; Date of data collection; Sample characteristics |
Main findings |
|---|---|---|
| Loret de Mola et al., 2021 | Longitudinal in a birth cohort; Brazil; 2019, January 1–December 31 December and 2020, May 11–July 20; n = 1136 women (postpartum); Age: M = 27.5 years (SD = 6.5); Children's age: M = 11.4 months (SD = 3.7); Gender ratio: 100 % female; Parental marital status: not reported |
PTSS: 40.6 % (n = 431) of mothers; Depressive symptoms: 29.5 % (n = 305) of mothers; Anxiety symptoms: 25.9 % (n = 266) of mothers as probable GAD cases; Compared to baseline, the prevalence of depression and anxiety was 5.7- and 2.4-fold higher, respectively (p < .001) |
| Molgora and Accordini, 2020 | Cross-sectional; Italy; 2020, March 1–May 3; n = 186 women (postpartum); Age: M = 33.01 years (SD = 4.19); Children's age: under 6 months; Gender ratio: 100 % female; Parental marital status: 58.6 % married to the father of their child, 41.4 % cohabiting |
PTSD: 16.7 % of women with high risk for PTSD; Depressive symptoms: 26.3 % (n = 49) of women affected by clinical depression; Anxiety symptoms: 57.7 % (n = 98) of women affected by clinical state anxiety, 46.2 % (n = 86) of women affected by clinical trait anxiety |
| Orsini et al., 2021 | Cross-sectional; Italy (Pisa, Bologna, Pavia); 2020, 1 April 1–30; n = 96 parents; Age: M = 40.79 years (SD = 8.22); Children's age: not reported; Gender ratio: 62.5 % female; Parental marital status: 78.1 % married or cohabiting |
PTSS: 39.6 % (n = 38) of parents affected by moderate to severe PTSS, mothers higher than fathers (p = .013); Depressive symptoms: 24 % (n = 23) of parents affected by moderate to severe depressive symptoms; Anxiety symptoms: 40.6 % (n = 39) of parents affected by moderate to severe anxiety symptoms; |
| Ostacoli et al., 2020 | Cross-sectional; Italy (Torino); 2020, June 15–29; n = 163 women (postpartum); Age: M = 34.77 years (SD = 5.01); Children's age: under 3 months; Gender ratio: 100 % female; Parental marital status: 93.3 % married or cohabiting |
PTSS: 42.9 % (n = 70) of women affected by mild PTSS, and 29.4 % (n = 48) of women concerning moderate PTSS; Depressive symptoms: 44.2 % (n = 72) of women (≥11) 30.7 % (n = 50) of women (≥13) affected by presence of depressive symptoms |
| Stallard et al., 2021 | Cross-sectional; Portugal & UK; 2020, May–27 June; n = 385 caregivers (Portuguese: n = 185; UK: n = 200); Age: not reported; Children's age: 6–16 years; Gender ratio: 88.6 % mothers; Parental marital status: 79.7 % intact nuclear family |
Well-being: 25.7 % (n = 99) of caregivers with high risk of depression, more caregivers in the UK falling below the threshold for risk of depression than in Portugal (p = .003); GAD: 21.6 % (n = 83) of caregivers affected by moderate anxiety |
| Wade et al., 2021 | Cross-sectional (with baseline two months earlier); UK, USA, Canada, Australia; 2020, May–July; n = 491 caregivers (Information for 549 assessed caregivers): Age: M = 41.33 years (SD = 6.33); Children's age: 5–18 years; Gender ratio: 68 % female; Parental marital status: 90 % married/common-law |
No prevalence rates reported; Female caregivers reported higher COVID stress/disruption compared to male caregivers (p < .001); Female caregivers reported more distress (p < .001), anxiety (p < .001), and PTSS (p = .002) compared to male caregivers |
Note. M = mean; SD = standard deviation; p = p-value; n = sample size; PTSD = post-traumatic stress disorder; PTSS = post-traumatic stress symptoms; GAD = generalized anxiety disorder.
Table 4.
Main characteristics of included studies on trauma-related symptoms in the course of the COVID-19 pandemic and the association between COVID-19 and trauma-related symptoms among families.
| Authors/date of publication | Study design; Country; Date of data collection; Sample characteristics |
Main findings |
|---|---|---|
| Crescentini et al., 2020 | Not reported (but reported to be retrospective, before pandemic); Italy (Northern & central Italy); 2020, April 16–May 7; n = 721 parents and their children; Caregiver's age: M = 42.80 years (SD = 5.47); Children's age: M = 10.08 years (SD = 5.47), 6–18 years; Gender ratio: 85.71 % female, 48.4 % of children female; Parental marital status: 72.6 % married |
PTSS: 27.0 % (n = 195) of parents affected by moderate to severe PTSS; Depressive Symptoms: 8.8 % (n = 64) of parents affected by elevated depressive symptoms, 24.2 % (n = 175) of children affected by elevated depression (withdrawn/depressed); Anxiety: 12.4 % (n = 90) of parents affected by elevated anxiety, 26.4 % (n = 191) of children affected by elevated anxiety (anxious/depressed); Somatic complaints: 9.0 % (n = 65) of children affected by elevated somatic complaints |
| Cusinato et al., 2020 | Not reported; Italy; 2020, April 25–May 8; n = 463 parents and their children; Caregiver's age: M = 43.3 years (SD = 5.88); Children's age: M = 9.72 years (SD = 3.29), 5–17 years; Gender ratio: 90.5 % female, 43.8 % of children female; Parental marital status: 87.7 % in nuclear family |
No prevalence rates reported; Well-being caregivers: Mothers significantly lower average scores in total score (p < .001), anxiety (p < .001), and self-control (p < .001) compared to pre-pandemic normative population; Well-being children: No significant differences in terms of well-being between children (6–10 years) compared to pre-pandemic normative population, but there might be higher hyperactivity levels (p = .036) |
| Davico et al., 2021 | Cross-sectional; Italy; 2020, March 20–26; n = 786 children and their parents; Caregiver's age: not reported; Children's age: M = 12.3 years (SD = 3.29); Gender ratio: 49.9 % of children female; Parental marital status: not reported |
PTSS: 30.9 % of the children at high risk for PTSD; PTSS scores among children were related to their parents' PTSS scores (p < .001) |
| Romero et al., 2020 | Cross-sectional; Spain; 2020, April 8–27; n = 1049 caregivers and their children; Caregiver's age: not reported; Children's age: M = 7.29 years (SD = 2.39), 3–12 years; Gender ratio: 89.6 % mothers, 50.4 % of children female; Parental marital status: not reported |
No prevalence rates reported regarding caregivers; Negative child behavior: >55 % of children did not show a relevant change in problematic behaviors, 30–40 % displayed an increase in conduct problems, emotional problems, and hyperactivity |
| Yue et al., 2020 | Not reported; China (Jiangsu province; classified as one of the non-severely impacted areas); 2020, February 13–29; n = 1360 children and their parent; Caregiver's age: M = 37.78 years (SD = 4.99); Children's age: M = 10.56 years (SD = 1.79), 3–12 years; Gender ratio: 41.03 % mothers, 46.03 % of children female; Parental marital status: not reported |
PTSS: 3.53 % of parents with high risk for PTSD, 3.16 % of children with high risk for PTSD; Depressive symptoms: 22.79 % of parents mildly depressed, 3.60 % of parents moderately depressed, 0.01 % of parents severely depressed; 2.22 % of children depressed; Anxiety symptoms: 4.41 % of parents (mild anxiety), 1.18 % of parents (moderate anxiety); 5.66 % of children (mild anxiety) and 1.84 % of children (moderate anxiety) |
Note. M = mean; SD = standard deviation; p = p-value; n = sample size; PTSD = post-traumatic stress disorder; PTSS = post-traumatic stress symptoms; GAD = generalized anxiety disorder.
All 22 studies were observational, of which the majority was described as cross-sectional (n = 15), one as longitudinal (n = 1), and one as a cohort study (n = 1). Five studies did not provide detailed information on study design. Another study integrated a retrospective design (Crescentini et al., 2020). Most studies did not have comparison groups – apart from five studies (Cetin et al., 2020; Davico et al., 2021; Molgora and Accordini, 2020; Wade et al., 2021; Zhang et al., 2020).
The studies were conducted in eleven different countries: China (n = 9), Italy (n = 6), Turkey (n = 2), UK (n = 2), Brazil (n = 1), France (n = 1), Spain (n = 1), Portugal (n = 1), USA (n = 1), Canada (n = 1), Australia (n = 1). Sample sizes ranged from 76 to 6196 participants. Studies were published from July 2020 to March 2021. Study participants were recruited in diverse ways such as schools (n = 7), hospitals (n = 3), or through social media (n = 2).
The weighted mean age of assessed children and adolescents was 12.27 years (SD weighted = 2.44 years) with a maximum age of 20 years. This number was obtained from twelve out of 16 studies assessing children and adolescents, as four studies (Duan et al., 2020; Guo et al., 2020; Ma et al., 2021; Yang et al., 2020) did not provide precise information regarding the age of the participants. The (weighted) mean age of assessed caregivers was 36.18 years (SD weighted = 6.48 years) with a range of 18 to over 50 years. This number was obtained from five out of eight studies assessing caregivers, as three studies (Davico et al., 2021; Stallard et al., 2021; Wade et al., 2021) did not provide clear information regarding the age of the participants or specified inclusion criteria. However, after careful consideration, we decided to include these studies with missing or insufficient information as we regarded their inclusion of minors as very unlikely.
50.23 % (SD weighted = 4.87 %) of children and adolescents were female (calculated from 16 studies) - while the sex ratio was not balanced in two studies (Cetin et al., 2020; Karaman et al., 2021). Based on nine out of eleven studies, 76.19 % (SD weighted = 24.94 %) caregivers were female. Wade et al. (2021) included male caregivers but did not provide clear information about the sex ratio. Davico et al. (2021) did not report the caregivers' gender ratio. Three studies (Loret de Mola et al., 2021; Molgora and Accordini, 2020; Ostacoli et al., 2020) included only female caregivers assessing their symptoms in the postpartum phase.
Eleven articles reported information whether the caregivers were living together or married. 74.99 % (SD weighted = 11.51 %) were either married or living together, or the children or adolescents were living with their (nuclear) family.
3.3. Outcome measures
All studies were conducted between the onset of the COVID-19 pandemic and July 2020, and most articles reported on the lockdowns/home confinements taken at the time of the survey in each country (n = 16). In two studies, mental health outcomes were collected before and after the outbreak (Loret de Mola et al., 2021; Shek et al., 2021), another study was examined over a 5-week period (Moulin et al., 2021), and one study integrated a baseline in May 2020 (Wade et al., 2021). Further, Crescentini et al. (2020) asked caregivers to rate their symptoms – and those of their children – twice: once referring to the COVID-19 period and once recalling how they and their children felt before the COVID-19 outbreak.
15 out of 22 studies specifically asked about various factors related to the COVID-19 pandemic (e.g., perceived threat, family member or friend infected; number and type of stressful life events experienced at the time of data collection, experience of quarantine). Two studies (Molgora and Accordini, 2020; Ostacoli et al., 2020) explicitly addressed birth experiences during COVID-19 and Orsini et al. (2021) referred to the suspected COVID-19 infection of the caregivers' children.
Since the studies were conducted in several different countries, the respective version of measurement instruments in each country's language was used within the studies. In most cases, these versions were both valid and reliable with a few exceptions such as the use of the self-report PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) by Guo et al. (2020). These studies were nevertheless included as their additional survey instruments were reliable and valid, and the original questionnaires had good psychometric properties.
Various measurement instruments were administered to assess explicit trauma symptoms in children and adolescents. The most used instrument was the CRIES (CRIES-8 and CRIES-13; Perrin et al., 2005). Furthermore, numerous other trauma-associated symptoms were examined, such as depressive symptomatology by the Child Depression Inventory (CDI; Kovacs and Beck, 1977), or anxiety symptoms by the Generalized Anxiety Disorder Scale (GAD-2; Kroenke et al., 2007). Several self-report questionnaires were applied to evaluate explicit trauma symptoms in caregivers. PTSS were mostly investigated via the IES-R (Weiss and Marmar, 1996). Moreover, several studies assessed anxiety symptoms, e.g., using the Generalized Anxiety Disorder 7-item scale (GAD-7; Spitzer et al., 2006), or depressive symptoms, e.g., using the Edinburgh Postnatal Depression Scale (EPDS; Cox et al., 1987). The specific implemented questionnaires can be found in the more detailed versions of the tables which were made available on the OSF (https://osf.io/u98n2/).
In all cases, self-report questionnaires were used. Regarding symptoms of children/adolescents these were completed by the children/adolescents themselves (n = 9), by the children/adolescents and their caregivers together (n = 2), or by the caregivers as an observer rating (n = 5).
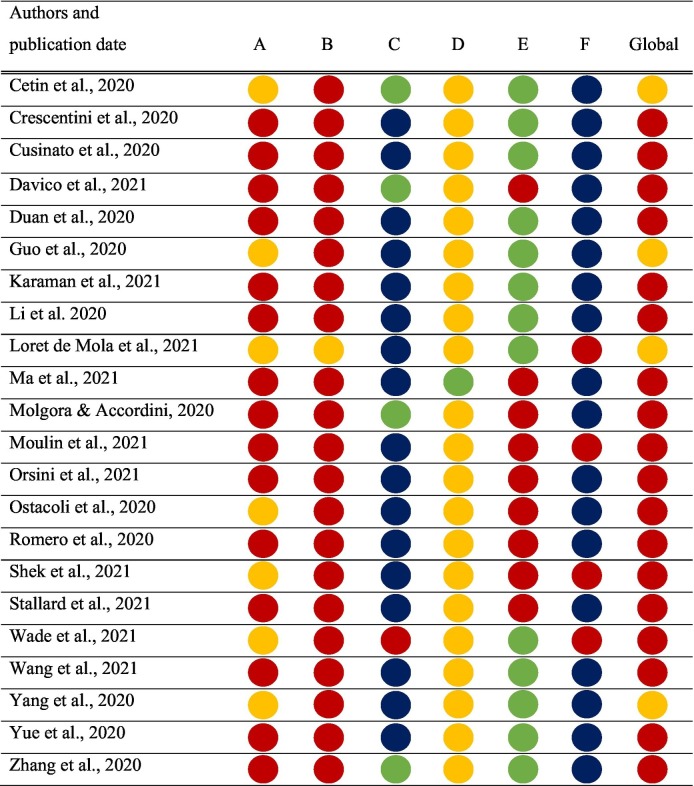
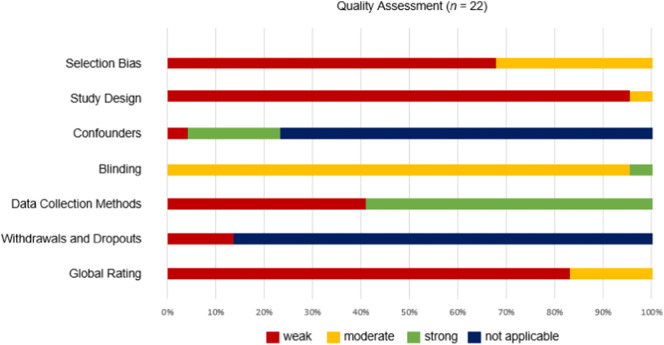
3.4. Risk of bias in individual trials and overall quality
Table 5 and Fig. 2 provide an overview of the methodological quality of the primary studies using the EPHPP-QAT (see Supplementary material for barrier-free presentations). In the majority of studies (n = 18; 82 %), the global rating of the EPHPP-QAT was classified as weak (3), with the remaining studies (n = 4) having a global rating of moderate (2). Consequently, following Higgins et al. (2011), an overall assessment of the included primary studies, and thus the current body of studies on the topic of trauma-associated consequences of the COVID-19 pandemic on families is evaluated as weak.
Table 5.
Quality of included studies and assessment of risk of bias based on the EPHPP-QAT (Thomas et al., 2004).
Note. Selection Bias (A), Study Design (B), Confounders (C), Blinding (D), Data Collection Methods (E), Withdrawals and Dropouts (F), and Global Rating (Global); red = weak (3), yellow = moderate (2), green = strong (1), blue = not applicable.
Fig. 2.
Percentage of component ratings among included studies based on the Quality Assessment Tool for Quantitative Studies (EPHPP-QAT). Figure available at https://osf.io/u98n2/, under a CC-BY 4.0 license.
In particular, the assessment of the studies regarding the domain Study Design (B) revealed a weak result, as all studies were observational studies and only one study fell into the category of a cohort study. In addition to the study design, the recruitment methods of the studies were mostly inadequate such as word-of-mouth and contacting teachers (Crescentini et al., 2020). This resulted in a rating of weak methodological quality for Selection Bias (A) in most studies (n = 15).
Notably, in most studies (n = 17) no group comparison was included. The EPHPP-QAT does not in fact allow a “not applicable” rating in the category Confounders (C). Nevertheless, primary studies without comparison groups were given a rating of “not applicable”. Only one (Wade et al., 2021) out of five studies, which included group comparisons, was rated as weak due to unclear information. A strong rating was assigned to the other four studies (Cetin et al., 2020; Davico et al., 2021; Molgora and Accordini, 2020; Zhang et al., 2020). However, it is noteworthy that most authors reported to have considered covariates. Nonetheless, five studies did not provide information on this topic (Karaman et al., 2021; Li et al., 2020; Ma et al., 2021; Stallard et al., 2021; Yang et al., 2020).
The criteria of the EPHPP-QAT were primarily established to assess clinical intervention studies, which is why these criteria may have been too strict for the assessment of the included studies. Moreover, the COVID-19 pandemic restricted many research teams as well which is why many studies had to deal with their respective limitations. Due to the weak overall evaluation regarding methodological quality and systematic bias of the primary studies, the results of this systematic review should be interpreted with caution.
3.5. Main findings
This systematic review followed the preregistered research question whether the COVID-19 pandemic and its containment measures are associated with trauma-related disorders or symptoms in children, adolescents, and caregivers. However, to answer this question the included studies would need a pre-pandemic control sample or at the very least test correlations between pandemic and pre-pandemic symptom severity. Hence, only three studies were found within the original scope of this review. Only one study included data on trauma-related symptoms before versus during the pandemic (Loret de Mola et al., 2021). Another study included a retrospective assessment of symptoms prior to the pandemic (Crescentini et al., 2020) and a third study statistically compared data collected during the COVID-19 pandemic with a pre-pandemic Italian norm sample (Cusinato et al., 2020).
Notably, some studies suggest that they found “higher (or lower) prevalence numbers of trauma symptoms during the COVID-19 pandemic than other studies found prior to the pandemic” (Duan et al., 2020; Molgora and Accordini, 2020; Ostacoli et al., 2020; Shek et al., 2021; Stallard et al., 2021; Yue et al., 2020; Zhang et al., 2020). Although many of the included studies of this systematic review found prevalence rates which are above those conducted prior to the pandemic, this difference has not been statistically compared and is limited by numerous methodological differences (e.g., sampling methods, assessment instruments, timeframe) between the studies. For these studies, we had to remain on a descriptive level assessing trauma symptoms in the context of the COVID-19 pandemic without drawing any causal conclusions. Therefore, we clearly state in the following sections which studies statistically tested differences with pre-pandemic samples and which studies remain on a descriptive level.
In the following section, the articles will now be divided into studies involving (1) children and/or adolescents, (2) caregivers, or (3) both populations mixed.
3.5.1. Studies on children and/or adolescents
Eleven studies addressed the traumatic impact of the COVID-19 pandemic on children and adolescents (see Table 3). Some studies found descriptively higher prevalence rates compared to studies conducted before the COVID-19 pandemic, for trauma-associated symptoms in children and adolescents. In particular, PTSS (Karaman et al., 2021; Ma et al., 2021; Zhang et al., 2020), depressive symptoms (Duan et al., 2020; Ma et al., 2021; Zhang et al., 2020), anxiety symptoms (Duan et al., 2020; Zhang et al., 2020), and additional other symptoms such as hyperactivity (Duan et al., 2020; Moulin et al., 2021; Zhang et al., 2020) were examined. No study was identified in which the results indicated descriptively lower prevalence rates for trauma-associated symptoms in children in the context of the COVID-19 pandemic compared to the pre-pandemic situation. However, some studies included in this systematic review did not report prevalence rates, but instead focused on other research questions relevant to the topic of trauma (Cetin et al., 2020; Guo et al., 2020; Li et al., 2020; Wang et al., 2021; Yang et al., 2020). Yang et al. (2020), for instance, investigated in their cross-sectional study whether COVID-19 as a traumatic event affects adolescents' mental health – assessed via a specific mental health instrument (Zhang et al., 2013) finding that the psychological trauma of the COVID-19 pandemic explained 4 % of the variance in mental health (γ = −0.20, p < .01) among high school students. This finding emphasizes the relevance of considering COVID-19 as a traumatic event and its relationship to adolescent mental health. Additionally, some studies also explored risk and protective factors regarding the associations between the COVID-19 pandemic and trauma-associated symptoms in children and adolescents (Duan et al., 2020; Karaman et al., 2021; Ma et al., 2021; Yang et al., 2020; Zhang et al., 2020): Demographic characteristics (e.g., sex, age, residency in urban region), children's psychological factors (e.g., emotion-focused coping style, resilience, emotion regulation), and COVID-19 related factors (i.e., close ones infected, implementation of control measures, financial difficulties).
3.5.2. Studies on caregivers
Six studies examined trauma-associated symptoms in caregivers during the COVID-19 pandemic (see Table 4; Loret de Mola et al., 2021; Molgora and Accordini, 2020; Orsini et al., 2021; Ostacoli et al., 2020; Stallard et al., 2021; Wade et al., 2021).
In each study which considered the traumatic impact of the COVID-19 pandemic on caregivers, descriptively higher prevalence rates in comparison to pre-pandemic measurement points were found for the following symptom domains: PTSS (Molgora and Accordini, 2020; Orsini et al., 2021; Ostacoli et al., 2020), anxiety symptoms (Molgora and Accordini, 2020; Orsini et al., 2021; Stallard et al., 2021), and depressive symptomatology (Molgora and Accordini, 2020; Orsini et al., 2021; Ostacoli et al., 2020; Stallard et al., 2021). Loret de Mola et al. (2021) even showed that the prevalence of depression increased 5.7-fold and of anxiety increased 2.4-fold during the pandemic (p < .001), statistically comparing pandemic data to a pre-pandemic baseline. As an exception, Wade et al. (2021) did not address prevalence rates of trauma-associated symptoms but examined differences between male and female caregivers in distress, anxiety, substance use, and PTSS. More specifically, female caregivers reported more distress-related mental health difficulties compared to male caregivers during the current pandemic.
Most studies went a step further by examining risk and protective factors for trauma-associated symptoms in caregivers (Loret de Mola et al., 2021; Molgora and Accordini, 2020; Orsini et al., 2021; Wade et al., 2021). In this regard, variables such as sex, age, prior psychological distress or disorders, attachment styles, perceived support, birth complications, or infections in close ones during COVID-19 were investigated.
3.5.3. Studies on both children/adolescents and caregivers
Five studies examined trauma-associated symptoms in both children/adolescents and caregivers (see Table 5; Crescentini et al., 2020; Cusinato et al., 2020; Davico et al., 2021; Romero et al., 2020; Yue et al., 2020). In this regard, descriptively higher prevalence rates of trauma-associated symptoms were found – explicit trauma symptoms in children (Davico et al., 2021) and other symptomatology in children (Romero et al., 2020). Cusinato et al. (2020) tested the presence of statistically significant differences between the Italian normal population and their sample in regard of parents' and children's well-being. Therefore, they executed one-sample t-tests with the means of the normative samples of the respective questionnaires as test values. The authors did not report on precise prevalence rates, but no statistical difference regarding well-being of children compared to a pre-pandemic normative population was found. However, they suggested that there might be higher levels of hyperactivity among children during lockdown statistically compared to the normative population (t = 2.18, p = .036). Additionally, they showed that mothers reported lower levels of well-being (t = −14.3, p < .001) and perceived self-control (t = −5.63, p < .001) and higher levels of anxiety (t = −6.40, p < .001) statistically compared to the normal pre-pandemic population. In a retrospective study by Crescentini et al. (2020), analyses of variance showed that internalizing symptoms of parents as depressive symptoms (F(1,719) = 109.11, p < .01, η2 p = 0.131) and anxiety (F(1,719) = 38.53, p < .01, η2 p = 0.051) and children as withdrawn/depressed (F(1,719) = 48.01, p < .01, η2 p = 0.062), anxiety (F(1,719) = 3.88, p < .05, η2 p = 0.005) and somatic complaints (F(1,719) = 15.06, p < .01, η2 p = 0.021) were significantly higher during the Covid-19 pandemic than before it started. Notably, they also stated that the sequence with which parents had to rate their own anxiety and depression symptoms (and those of their children) significantly influenced their assessments. Findings in a study by Yue et al. (2020) showed that <4 % of the respondents experienced moderate or severe levels of psychological problems. The authors concluded that children and their parents living in a not severely affected area did not suffer from major psychological distress during the outbreak, descriptively comparing their findings with previous studies on the psychological impact of pandemics where 30 % of quarantined children and 25 % of their quarantined parents experienced severe psychological trauma (Sprang and Silman, 2013).
In addition to the existence of trauma-associated symptoms in children/adolescents and their parents, some studies also examined risk and protective factors (Crescentini et al., 2020; Cusinato et al., 2020; Davico et al., 2021; Romero et al., 2020). Specific demographic characteristics (i.e., sex, age), psychological factors of children and parents (i.e., fear of contagion, parental stress, existing parental psychological, physical, or genetic problems, the opportunity to think about possible secondary positive effects of the pandemic), and parent's and children's behaviors during the lockdown period (i.e., employment status, sport, and media exposure) were associated to trauma-associated symptoms of caregivers and children. However, divergent results were often reported as, for example, Davico et al. (2021) did not find age to be a significant moderator of psychological distress in children during the COVID-19 pandemic, but Romero et al. (2020) did find age to be negatively related to specific outcomes such as parenting distress or hyperactive behaviors. However, it should be noted that in the former study children/adolescents in an age range between eight to 18 years were considered (Davico et al., 2021), and the latter three- to twelve-year-old children (Romero et al., 2020).
4. Discussion
The present systematic review aimed to answer the preregistered question if the COVID-19 pandemic and its containment measures are associated with trauma-related disorders or symptoms in children, adolescents, and caregivers. As not enough studies could be found to validly answer this question, we widened the scope of our review, and additionally reported on studies that have addressed trauma symptoms in the context of the COVID-19 pandemic.
After a comprehensive systematic literature search, 22 studies were ultimately reviewed. Due to the unprecedented situation of the COVID-19 pandemic and to control transmission of the disease, public health sanitary and social measures have been implemented in countless countries, including lockdowns and the closure of schools. Moreover, COVID-19 itself is a threatening disease with mild to severe progressions which may even lead to death (WHO, 2021). All these adverse conditions may be described as traumatic events (e.g., Bridgland et al., 2021) and might predispose numerous children, adolescents, and caregivers to develop trauma-associated symptoms.
According to the results of this systematic review, only three primary studies (Crescentini et al., 2020; Cusinato et al., 2020; Loret de Mola et al., 2021) executed a statistical comparison with pre-pandemic or retrospective data, and thus, allowed to answer our preregistered research question. These three studies showed a negative impact of the COVID-19 pandemic and its associated measures on children's and caregivers' trauma-associated symptoms, more specifically on internalizing symptoms and hyperactivity. In the majority of the remaining studies, prevalence rates of various trauma-associated symptoms in children, adolescents, and caregivers were globally reported to be descriptively higher in the context of the COVID-19 pandemic when compared to other pre-pandemic studies. These symptoms include PTSS (Davico et al., 2021; Karaman et al., 2021; Ma et al., 2021; Molgora and Accordini, 2020; Orsini et al., 2021; Ostacoli et al., 2020; Zhang et al., 2020), depressive symptoms (Duan et al., 2020; Ma et al., 2021; Molgora and Accordini, 2020; Orsini et al., 2021; Ostacoli et al., 2020; Stallard et al., 2021; Zhang et al., 2020), anxiety symptoms (Duan et al., 2020; Molgora and Accordini, 2020; Orsini et al., 2021; Stallard et al., 2021; Zhang et al., 2020), and additional other symptoms such as hyperactivity in children (Duan et al., 2020; Moulin et al., 2021; Romero et al., 2020; Zhang et al., 2020). Only two studies revealed contrasting results. Cusinato et al. (2020) did not provide any precise information on prevalence rates but reported that no significant differences regarding the well-being of children compared to the pre-pandemic normative population could be found in their study – except hyperactivity. In another study, <4 % of the respondents (children and their caregivers) experienced moderate or severe levels of psychological problems in an area with low incidence rates (Yue et al., 2020). Therefore, many of the primary studies of this systematic review find prevalence rates which are above those found prior to the pandemic. However, these differences have not been statistically compared and are limited by numerous methodological differences between the studies. Thus, based on these descriptive differences, a clear link between the COVID-19 pandemic and trauma-associated symptoms cannot be drawn.
Furthermore, some of the included studies did not report prevalence rates, but instead focused on other research questions relevant to this topic area (Cetin et al., 2020; Guo et al., 2020; Li et al., 2020; Wade et al., 2021; Wang et al., 2021; Yang et al., 2020). One aspect that should be emphasized at this point is that the children's/adolescents' symptoms are related to the caregivers' concurrently assessed symptoms (Davico et al., 2021; Moulin et al., 2021; Romero et al., 2020). These results converge with prior findings suggesting that children's and adolescents' mental health would be affected by the impact on their caregivers, their interactions with them, and their family environment (Cobham et al., 2016; Spinelli et al., 2020).
In conclusion, the results of this systematic review are in line with previous findings highlighting the possible traumatic consequences of health emergencies such as SARS, Ebola, the H1N1 influenza pandemic and its related measures such as lockdown periods on both adults and children/adolescents (Brooks et al., 2020; Cavicchioli et al., 2021; Luo et al., 2020). Nevertheless, based on the state of studies to date, in which only three studies have drawn statistical comparisons with the pre-pandemic situation (Crescentini et al., 2020; Cusinato et al., 2020; Loret de Mola et al., 2021), it is not possible to validly assess the extent to which the COVID-19 pandemic and its accompanying policies may have a traumatic impact on families. Our results might be cautiously interpreted as a first indicator of an association between the COVID-19 pandemic and trauma sequelae.
4.1. Strengths and limitations
To the authors' knowledge, this is the first systematic review aiming at providing an overview of the association between the COVID-19 pandemic and trauma-associated symptoms in children, adolescents, and caregivers and additionally summarizing the state of research that has addressed trauma symptoms in the context of the COVID-19 pandemic. However, certain limitations need to be discussed. First, it is noteworthy that the extent of available evidence-based literature on this topic was sparse. Thus, it was not possible to validly answer the preregistered research question whether the COVID-19 pandemic was clearly correlated with trauma-associated symptoms. A larger number of studies, however, addressed trauma-symptoms in the context of the pandemic.
Second, the weak methodological quality of the included primary studies should be addressed. Regarding the methodological quality, it should be noted that the research conditions within the COVID-19 pandemic have been extremely difficult, i.e., infrastructures could not be used or could only be partially used due to the necessary hygiene and containment measures. Hence, mainly self-report questionnaires were administered via online formats. In addition, given the narrow timeframe, primarily cross-sectional designs could be realized so far, which do not allow to conclude that the COVID-19 pandemic and related containment measures are the undoubted primary causes of the onset of trauma-related symptoms. These limitations represent just a few of the difficulties researchers have had to deal with in the course of the COVID-19 pandemic. For this reason, on the one hand, previous research on the psychological impact of the COVID-19 pandemic should not be evaluated too harshly; on the other hand, the mentioned limitations, especially the methodological shortcomings, should be considered in future research.
Although the publication process for COVID-19-related research has been sped up, none of these studies within the systematic review were conducted after July 2020. As the pandemic is still ongoing, several triggers such as financial loss, grief, or parental mental health problems are still omnipresent. Ultimately, longitudinal studies are needed to allow the precise evaluation of the course of trauma-related symptoms after health emergencies such as COVID-19. Moreover, most studies did not ascertain which aspects of the COVID-19 pandemic were experienced as traumatic. Thus, it is not possible to distinguish which proportion of symptoms was due to the disease or the containment measures, or synergistic effects of both. Additionally, the COVID-19 pandemic might increase the risk for multiple traumas such as physical, sexual and psychological violence, physical and emotional neglect, and exposure to inter-parental violence in families (Bryant et al., 2020; Kaukinen, 2020; Ramaswamy and Seshadri, 2020), which is why these traumatic experiences should be assessed as possible primary factors for the increase in PTSS along with depressive and anxiety symptoms.
Last, it should be reiterated that some studies have drawn the conclusions based on their data that the prevalence rates of trauma symptoms are higher within the COVID-19 pandemic compared to the pre-pandemic situation (Duan et al., 2020; Molgora and Accordini, 2020; Ostacoli et al., 2020; Shek et al., 2021; Stallard et al., 2021; Yue et al., 2020; Zhang et al., 2020). These conclusions might be inaccurate because these differences have not been statistically tested within these studies.
Limitations of the systematic review itself should also be taken into consideration. As noted previously, the EPHPP-QAT may be too strict for the included studies, as the criteria were primarily constructed to assess clinical intervention studies. The fact that the quality assessment was not carried out by two independent reviewers, but only double checked by the last author, must also be taken into account. However, as we uploaded the transparent process of quality assessment on the OSF (https://osf.io/u98n2/) providing citations of the primary studies to justify the respective code, the quality and bias rating stands on solid ground.
While infectious disease pandemics can be highly stressful for many individuals, COVID-19 may be particularly disruptive for some individuals due to certain sociodemographic and risk factors, such as age, gender, or significant stressors in their pre-pandemic lives, which were still too sparsely investigated in the primary studies. These factors should be more specifically addressed in future studies.
It is noteworthy that the current results revealed that the majority of children, adolescents, and caregivers did not show a relevant change in trauma-related symptoms during the COVID-19 pandemic. Thus, research on protective factors, resilience, emotion regulation strategies, and post-traumatic growth should be studied in more detail – as they were only considered in a few included primary studies (Cusinato et al., 2020; Shek et al., 2021; Stallard et al., 2021; Yang et al., 2020; Zhang et al., 2020).
Finally, the findings of this review should initiate further discussions on whether the COVID-19 pandemic may be conceptualized as a traumatic event. There are divergent views on whether COVID-19 should be considered as a traumatic event or merely a stressful situation as in the DSM-5 trauma definition (APA, 2013). Particularly its specific effects on an individual and societal level should be differentiated.
4.2. Implications for policies and therapy
More research on risk and protective factors regarding trauma-associated symptoms in families is fundamentally needed to enhance and provide improved mental health strategies during the current crisis and future health emergencies. Additionally, findings from this systematic review suggest that policies need to be revised or put in place to reduce the traumatic impact. Such policies may include more or faster financial support, flexible childcare, individual working arrangements or community support (Fegert et al., 2020; Fong and Iarocci, 2020). Furthermore, mental health services – providing educational materials on COVID-19 and its traumatic impact – should be integrated in schools. Especially regarding the prevention and intervention of traumatic sequelae psychoeducational measures have been proven to support those affected (Cohen et al., 2016). Further important aspects are basic guidelines for caregivers on how to communicate about a pandemic and its containment measures, to maintain family routines, to support their children, to address their mental health, to monitor an appropriate screen time, etc. (Fegert et al., 2020; Fong and Iarocci, 2020).
Finally, it is of particular importance that effective interventions adapted to the specific needs of children, adolescents and caregivers are researched in more detail. Especially, the required adaptions, such as online formats for prevention and intervention due to lockdowns or school closures, should be carefully assessed.
5. Conclusion
To sum up, most included primary studies do not allow drawing conclusions whether the COVID-19 pandemic and trauma sequelae are associated as only three studies employ a pre-pandemic statistical comparison. These three studies found a negative impact of the COVID-19 pandemic and its associated measures on families' and children's internalizing symptoms and hyperactivity. All other included studies did not statistically assess changes in trauma-associated symptoms in comparison to the pre-pandemic situation. The majority of the included studies remained on a descriptive level when stating higher prevalence rates of various trauma-associated symptoms such as PTSS, depression or anxiety symptoms in children, adolescents, and caregivers during the COVID-19 pandemic than in other pre-pandemic studies. Due to numerous methodological differences between these studies the statement that the pandemic is associated with higher prevalence rates of trauma-associated symptoms cannot be validly answered at this point. Additionally, our results should be interpreted cautiously due to some methodological shortcomings of the primary studies. Our systematic review may therefore be primarily regarded as a summary of studies which have measured trauma-related disorders or symptoms during the pandemic. Even though we could not comprehensively answer our preregistered research question, our results could be cautiously interpreted as a first indicator of an association between the COVID-19 pandemic and trauma sequelae. Especially, risk and protective factors should more specifically be investigated in the context of the traumatic impact of COVID-19 on families. In conclusion, the present review highlights the need to develop adequate methods for early identification of those at risk and to implement adapted interventions and therapy services. Finally, the systematic review could possibly lead to the classification of pandemics and its associated measures as traumatic events and thus contribute to the discussion on trauma definitions.
Availability of data and material
Any relevant data and results involved in this systematic review are disclosed on the Open Science Framework (https://osf.io/u98n2/) to encourage re-analysis and verification of results by independent researchers.
Context
This work was a master thesis to obtain the academic degree Master of Science in the study program “Clinical Psychology and Cognitive Neuroscience” at Ludwig-Maximilans-University Munich, Germany. The associated supervisors were Prof. Dr. Corinna Reck (Ludwig-Maximilans-University Munich, Germany) and Christian Woll, M.Sc. (Ludwig-Maximilans-University Munich, Germany). Alexandra von Tettenborn, Dipl.-Soc.Ped (Ludwig-Maximilans-University Munich, Germany) also supported the theoretical framework of the review.
Statement of ethics
An ethics statement is not applicable as this study is based exclusively on published literature.
Funding sources
This research received no specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
This work is based on a master thesis conducted by LK. The associated supervisors were CR, CW, and AvT. LK selected studies, extracted data, conducted the quality assessment, and prepared a first draft of the manuscript. CW double-checked extracted data as well as the ratings of the quality assessment, guided the systematic review methodologically, and provided a major revision of the manuscript. AvT primarily guided the selection of outcome measures. CR set up the focus and theoretical outline of the review. All authors critically revised the manuscript.
Conflict of interest
The authors have no conflicts of interest to declare.
Acknowledgement
The authors would like to express their gratitude to the authors and researchers of the primary studies who conducted crucial research under extremely difficult circumstances. They would also like to thank the reviewers for their very helpful feedback.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.08.109.
Appendix A. Supplementary data
Supplementary material
References
- APA (American Psychiatric Association) 5th ed. American Psychiatric Publishing; Arlington: 2013. Diagnostic and Statistical Manual of Mental Disorders. [DOI] [Google Scholar]
- Araújo L.A.D., Veloso C.F., Souza M.D.C., Azevedo J.M.C.D., Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. J. Pediatr. 2020 doi: 10.1016/j.jped.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridgland V.M.E., Moeck E.K., Green D.M., Swain T.L., Nayda D.M., Matson L.A., Hutchison N.P., Takarangi M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE. 2021;16(1) doi: 10.1371/journal.pone.0240146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant D.J., Oo M., Damian A.J. The rise of adverse childhood experiences during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy. 2020;12(S1):S193–S194. doi: 10.1037/tra0000711. (COVID-19: Insights on the Pandemic’s Traumatic Effects and Global Implications) [DOI] [PubMed] [Google Scholar]
- Cavicchioli M., Ferrucci R., Guidetti M., Canevini M.P., Pravettoni G., Galli F. What will be the impact of the Covid-19 quarantine on psychological Distress? Considerations based on a systematic review of pandemic outbreaks. Healthcare (Basel, Switzerland) 2021;9(1) doi: 10.3390/healthcare9010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Dalexis R.D. The complex trauma Spectrum during the COVID-19 pandemic: a threat for children and Adolescents' physical and mental health. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenat J.M., Blais-Rochette C., Kokou-Kpolou C.K., Noorishad P.G., Mukunzi J.N., McIntee S.E., Dalexis R.D., Goulet M.A., Labelle P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis [Review] Psychiatry Res. 2021;295(16) doi: 10.1016/j.psychres.2020.113599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cetin F.H., Ucar H.N., Turkoglu S., Kahraman E.M., Kuz M., Gulec A. Chronotypes and trauma reactions in children with ADHD in home confinement of COVID-19: full mediation effect of sleep problems [Article] Chronobiol. Int. 2020;37(8):1214–1222. doi: 10.1080/07420528.2020.1785487. [DOI] [PubMed] [Google Scholar]
- Cobham V.E., McDermott B., Haslam D., Sanders M.R. The role of parents, parenting and the family environment in Children’s post-disaster mental health. Curr. Psychiatry Rep. 2016;18(6):53. doi: 10.1007/s11920-016-0691-4. [DOI] [PubMed] [Google Scholar]
- Cohen J.A., Mannarino A.P., Deblinger E. Guilford Publications; New York: 2016. Treating Trauma and Traumatic Grief in Children and Adolescents. [Google Scholar]
- Cost K.T., Crosbie J., Anagnostou E., Birken C.S., Charach A., Monga S., Kelley E., Nicolson R., Maguire J.L., Burton C.L., Schachar R.J., Arnold P.D., Korczak D.J. Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. Eur Child Adolesc Psychiatry. 2022;31(4):671–684. doi: 10.1007/s00787-021-01744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Crescentini C., Feruglio S., Matiz A., Paschetto A., Vidal E., Cogo P., Fabbro F. Stuck outside and inside: an exploratory study on the effects of the COVID-19 outbreak on italian parents and Children's internalizing symptoms. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.586074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cusinato M., Iannattone S., Spoto A., Poli M., Moretti C., Gatta M., Miscioscia M. Stress, resilience, and well-being in italian children and their parents during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020;17(22) doi: 10.3390/ijerph17228297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davico C., Ghiggia A., Marcotulli D., Ricci F., Amianto F., Vitiello B. Psychological impact of the COVID-19 pandemic on adults and their children in Italy. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.572997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Shao X.J., Wang Y., Huang Y.L., Miao J.X., Yang X.P., Zhu G. An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19 [Article] J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duane A.M., Stokes K.L., DeAngelis C.L., Bocknek E.L. Collective trauma and community support: lessons from Detroit. Psychol. Trauma Theory Res. Pract. Policy. 2020;12(5):452–454. doi: 10.1037/tra0000791. [DOI] [PubMed] [Google Scholar]
- Fan F.C., Zhang S.Y., Cheng Y. Incidence of psychological illness after coronavirus outbreak: a meta-analysis study. J. Epidemiol. Community Health. 2021 doi: 10.1136/jech-2020-215927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M.B., Williams J.B.W., Karg R.S., Spitzer R.L. American Psychiatric Association; Arlington, VA: 2015. Structured Clinical Interview for DSM-5: Research Version. [Google Scholar]
- Fischer G., Riedesser P. E. Reinhardt; Stuttgart: 2009. Lehrbuch der Psychotraumatologie. [Google Scholar]
- Fong V.C., Iarocci G. Child and family outcomes following pandemics: a systematic review and recommendations on COVID-19 policies. J. Pediatr. Psychol. 2020;45(10):1124–1143. doi: 10.1093/jpepsy/jsaa092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Fu M., Liu D., Zhang B., Wang X., van Ijzendoorn M.H. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020;110(Part 2) doi: 10.1016/j.chiabu.2020.104667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savović J., Schulz K.F., Weeks L., Sterne J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D., Brown A.D. Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol. Trauma Theory Res. Pract. Policy. 2020;12(4):331–335. doi: 10.1037/tra0000592. [DOI] [PubMed] [Google Scholar]
- Imran N., Aamer I., Sharif M.I., Bodla Z.H., Naveed S. Psychological burden of quarantine in children and adolescents: a rapid systematic review and proposed solutions. Pak. J. Med. Sci. 2020;36(5):1106–1116. doi: 10.12669/pjms.36.5.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson N., Waters E. Criteria for the systematic review of health promotion and public health interventions. Health Promot. Int. 2005;20(4):367–374. doi: 10.1093/heapro/dai022. [DOI] [PubMed] [Google Scholar]
- Karaman M.A., Eşici H., Tomar İ.H., Aliyev R. COVID-19: are school counseling services ready? Students' psychological symptoms, school counselors' views, and solutions. Front. Psychol. 2021;12 doi: 10.3389/fpsyg.2021.647740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaukinen C. When stay-at-home orders leave victims unsafe at home: exploring the risk and consequences of intimate partner violence during the COVID-19 pandemic. Am. J. Crim. Justice. 2020;1–12 doi: 10.1007/s12103-020-09533-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M., Beck A.T. Depression in Childhood: Diagnosis, Treatment, and Conceptual Models. 1977. An empirical-clinical approach toward a definition of childhood depression; pp. 1–25. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Lakens D., Hilgard J., Staaks J. On the reproducibility of meta-analyses: six practical recommendations. BMC Psychol. 2016:4. doi: 10.1186/s40359-016-0126-3. http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2016-27242-001&site=ehost-live [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Duan W., Chen Z. Latent profiles of the comorbidity of the symptoms for posttraumatic stress disorder and generalized anxiety disorder among children and adolescents who are susceptible to COVID-19. Child Youth Serv. Rev. 2020;116 doi: 10.1016/j.childyouth.2020.105235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang L.L., Gao T.T., Ren H., Cao R.L., Qin Z.Y., Hu Y.Y., Li C.E., Mei S.L. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency [Article] J. Health Psychol. 2020;25(9):1164–1175. doi: 10.1177/1359105320937057. Article 1359105320937057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59(11):1218–1239. doi: 10.1016/j.jaac.2020.05.009. e1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loret de Mola C., Martins-Silva T., Carpena M.X., Del-Ponte B., Blumenberg C., Martins R.C., Dias I.M., Terribele F.B., de Avila A.B., Marmitt L.P., Meucci R., Cesar J.A. Maternal mental health before and during the COVID-19 pandemic in the 2019 Rio Grande birth cohort. Rev. Bras. Psiquiatr. 2021 doi: 10.1590/1516-4446-2020-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou L., Zhang H., Tang B., Li M., Li Z., Cao H., et al. Clinical characteristics of COVID-19 in children and adolescents: A systematic review and meta-analysis. medRxiv. 2021 [Google Scholar]
- Ludvigsson J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paedia. Inter. J. Paedia. 2020 doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Chua C.R., Xiong Z., Ho R.C., Ho C.S.H. A systematic review of the impact of viral respiratory epidemics on mental health: an implication on the coronavirus disease 2019 pandemic. Front Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.565098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z., Idris S., Zhang Y., Zewen L., Wali A., Ji Y., Pan Q., Baloch Z. The impact of COVID-19 pandemic outbreak on education and mental health of chinese children aged 7–15 years: an online survey. BMC Pediatr. 2021;21(1):95. doi: 10.1186/s12887-021-02550-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mækelæ M.J., Reggev N., Dutra N., Tamayo R.M., Silva-Sobrinho R.A., Klevjer K., Pfuhl G. Perceived efficacy of COVID-19 restrictions, reactions and their impact on mental health during the early phase of the outbreak in six countries. R. Soc. Open Sci. 2020;7(8) doi: 10.1098/rsos.200644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maercker A. Springer; Berlin: 2019. Traumafolgestörungen. [DOI] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A.C., Simoes-E-Silva A.C. How is COVID-19 pandemic impacting mental health of children and adolescents? Int. J. Disaster Risk Reduct. 2020;51 doi: 10.1016/j.ijdrr.2020.101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masiero M., Mazzocco K., Harnois C., Cropley M., Pravettoni G. From individual to social trauma: sources of everyday trauma in Italy, the us and Uk during the covid-19 pandemic. J. Trauma Dissociation. 2020 doi: 10.1080/15299732.2020.1787296. [DOI] [PubMed] [Google Scholar]
- Molgora S., Accordini M. Motherhood in the time of coronavirus: the impact of the pandemic emergency on expectant and postpartum Women's psychological well-being. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.567155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulin F., El-Aarbaoui T., Bustamante J.J.H., Héron M., Mary-Krause M., Rouquette A., Galéra C., Melchior M. Risk and protective factors related to children's symptoms of emotional difficulties and hyperactivity/inattention during the COVID-19-related lockdown in France: results from a community sample. Eur. Child Adolesc. Psychiatry. 2021 doi: 10.1007/s00787-021-01752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orsini A., Corsi M., Pedrinelli V., Santangelo A., Bertelloni C., Dell'Oste V., Cordelli D., Perrone A., Parini L., Lanari M., Massimetti G., Bonuccelli A., Foiadelli T., Trabatti C., Savasta S., Marseglia G., Striano P., Peroni D.G., Dell'Osso L., Carmassi C. Post-traumatic stress, anxiety, and depressive symptoms in caregivers of children tested for COVID-19 in the acute phase of the italian outbreak. J. Psychiatr. Res. 2021;135:256–263. doi: 10.1016/j.jpsychires.2021.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostacoli L., Cosma S., Bevilacqua F., Berchialla P., Bovetti M., Carosso A.R., Malandrone F., Carletto S., Benedetto C. Psychosocial factors associated with postpartum psychological distress during the Covid-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2020;20(1):703. doi: 10.1186/s12884-020-03399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., Chou R., Glanville J., Grimshaw J.M., Hróbjartsson A., Lalu M.M., Li T., Loder E.W., Mayo-Wilson E., McDonald S., McGuinness L.A., Stewart L.A., Thomas J., Tricco A.C., Welch V.A., Whiting P., Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., Letterie M., Davis M.M. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Perrin S., Meiser-Stedman R., Smith P. The children's revised impact of event scale (CRIES): validity as a screening instrument for PTSD. Behav. Cogn. Psychother. 2005;33(4):487–498. doi: 10.1017/S1352465805002419. (A Festschrift for William Yule) [DOI] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Qiu D., Li Y., Li L., He J., Ouyang F., Xiao S. Prevalence of post-traumatic stress symptoms among people influenced by COVID-19 outbreak: a meta-analysis. Eur. Psychiatry. 2021:1–42. doi: 10.1192/j.eurpsy.2021.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaswamy S., Seshadri S. Children on the brink: risks for child protection, sexual abuse, and related mental health problems in the COVID-19 pandemic. Indian J. Psychiatry. 2020;62(Suppl. 3):S404–S413. doi: 10.4103/psychiatry.IndianJPsychiatry_1032_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restauri N., Sheridan A.D. Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: intersection, impact, and interventions [Article] J. Am. Coll. Radiol. 2020;17(7):921–926. doi: 10.1016/j.jacr.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert Koch-Institut Epidemiologischer Steckbrief zu SARS-CoV-2 und COVID-19. 2021. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Steckbrief
- Romero E., Lopez-Romero L., Dominguez-Alvarez B., Villar P., Gomez-Fraguela J.A. Testing the effects of COVID-19 confinement in Spanish children: the role of parents' distress, emotional problems and specific parenting [Article] Int. J. Environ. Res. Public Health. 2020;17(19):23. doi: 10.3390/ijerph17196975. Article 6975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B.S., Hutchison M., Tambling R., Tomkunas A.J., Horton A.L. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum. Dev. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shek D.T.L., Zhao L., Dou D., Zhu X., Xiao C. The impact of positive youth development attributes on posttraumatic stress disorder symptoms among chinese adolescents under covid-19. J. Adolesc. Health. 2021 doi: 10.1016/j.jadohealth.2021.01.011. [DOI] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Setti A., Fasolo M. Parenting stress during the covid-19 outbreak: socioeconomic and environmental risk factors and implications for children emotion regulation. Fam. Process. 2020 doi: 10.1111/famp.12601. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Stallard P., Pereira A.I., Barros L. Post-traumatic growth during the COVID-19 pandemic in carers of children in Portugal and the UK: cross-sectional online survey [Article] BJPsych Open. 2021;7(1):5. doi: 10.1192/bjo.2021.1. Article e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavridou A., Stergiopoulou A.A., Panagouli E., Mesiris G., Thirios A., Mougiakos T., Troupis T., Psaltopoulou T., Tsolia M., Sergentanis T.N., Tsitsika A. Psychosocial consequences of COVID-19 in children, adolescents and young adults: a systematic review. Psychiatry Clin. Neurosci. 2020;74(11):615–616. doi: 10.1111/pcn.13134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas B., Ciliska D., Dobbins M., Micucci S. A process for systematically reviewing the literature: providing the research evidence for public health nursing interventions. Worldviews Evid.-Based Nurs. 2004;1(3):176–184. doi: 10.1111/j.1524-475X.2004.04006.x. https://sigmapubs.onlinelibrary.wiley.com/doi/abs/10.1111/j.1524-475X.2004.04006.x [DOI] [PubMed] [Google Scholar]
- United Nations . 2017. Resolution Adopted by the General Assembly on 6 July 2017, Work of the Statistical Commission Pertaining to the 2030 Agenda for Sustainable Development (A/RES/71/313) [Google Scholar]
- Wade M., Prime H., Johnson D., May S.S., Jenkins J.M., Browne D.T. The disparate impact of COVID-19 on the mental health of female and male caregivers. Soc. Sci. Med. 2021;275 doi: 10.1016/j.socscimed.2021.113801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Zhao X., Yuan Y., Shi B. The relationship between creativity and intrusive rumination among chinese teenagers during the COVID-19 pandemic: emotional resilience as a moderator. Front. Psychol. 2021;11 doi: 10.3389/fpsyg.2020.601104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson M.F., Bacigalupe G., Daneshpour M., Han W.J., Parra-Cardona R. Covid-19 interconnectedness: health inequity, the climate crisis, and collective trauma. Fam. Process. 2020 doi: 10.1111/famp.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F., Litz B., Keane T., Palmieri P., Marx B., Schnurr P. 2013. The PTSD Checklist for DSM-5 (PCL-5) National Center for PTSD. [DOI] [Google Scholar]
- Weiss D.S., Marmar C.R. In: Assessing Psychological Trauma and PTSD: A Handbook for Practioners. Wilson J.P., Keane T.M., editors. 1996. The impact of event scale – revised; pp. 399–411. S. Guilford. [Google Scholar]
- WHO (World Health Organisation) International statistical classification of diseases and related health problems. ICD-10. 2016. https://icd.who.int/browse10/2016/en
- WHO (World Health Organisation) WHO Coronavirus (COVID-19) dashboard. 2021. https://covid19.who.int/
- Yang D., Swekwi U., Tu C.-C., Dai X. Psychological effects of the COVID-19 pandemic on Wuhan’s high school students. Child Youth Serv. Rev. 2020;119 doi: 10.1016/j.childyouth.2020.105634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K., Gong Y.-M., Liu L., Sun Y.-K., Tian S.-S., Wang Y.-J., Zhong Y., Zhang A.-Y., Su S.-Z., Liu X.-X., Zhang Y.-X., Lin X., Shi L., Yan W., Fazel S., Vitiello M.V., Bryant R.A., Zhou X.-Y., Ran M.-S., Bao Y.-P., Shi J., Lu L. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including covid-19: a meta-analysis and systematic review. Mol. Psychiatry. 2021 doi: 10.1038/s41380-021-01036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yue J., Zang X., Le Y., An Y. Anxiety, depression and ptsd among children and their parent during 2019 novel coronavirus disease (covid-19) outbreak in china. Curr. Psychol. 2020 doi: 10.1007/s12144-020-01191-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Cheng Y., Chin H., Lee H. A study on the test of validity and reliability of WHOQOL-BREF when it was applied to adults with severe visual impairments. Bull. Educ. Psychol. 2013;44(S):521–536. [Google Scholar]
- Zhang C., Ye M., Fu Y., Yang M., Luo F., Yuan J., Tao Q. The psychological impact of the COVID-19 pandemic on teenagers in China. J. Adolesc. Health. 2020;67(6):747–755. doi: 10.1016/j.jadohealth.2020.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
Any relevant data and results involved in this systematic review are disclosed on the Open Science Framework (https://osf.io/u98n2/) to encourage re-analysis and verification of results by independent researchers.