Abstract
Purpose:
Ensuring equitable access to augmentative and alternative communication (AAC) intervention services for children with complex communication needs (CCN) is crucial. Evidence suggests that racial disparities exist in access to communication interventions, disadvantaging Black children. However, no research has investigated specifically the evidence for racial disparities in AAC services for children with developmental disabilities and CCN.
Method:
The current study applied post hoc data analysis methods within a preexisting, open-access data set to explore preliminary evidence of racial disparities in AAC intervention. Amount of AAC intervention was compared for Black versus white 1 preschool students at study initiation (M age = 3;8 [years;months]) and 2 years later at study completion (M age = 5;10).
Results:
Black preschool students were reported to receive significantly less AAC intervention per week as compared to their white peers, both at study initiation and 2 years later. By study end, 75% of the Black children were receiving less than 60 min of AAC intervention per week, an inadequate amount to achieve meaningful gains given their significant disabilities.
Conclusions:
It is unclear what mechanisms may contribute to the observed disparities; however, it is critical that concrete steps are taken by individual speech-language pathologists, school districts, preservice preparation programs, and researchers to identify inequities in AAC services and take actions to rectify them. Future research is essential to investigate the potential factors contributing to inequalities and determine effective interventions to address them.
Though national demographic data are limited, some estimates suggest that at least 12% of preschoolers enrolled in special education in the United States have complex communication needs (CCN) and require augmentative and alternative communication (AAC) services (Binger & Light, 2006). Of those students with CCN, over 70% have an associated diagnosis of developmental delay or autism spectrum disorder (ASD; Binger & Light, 2006). In fact, some estimates suggest that up to half of children with ASD do not develop speech that is functional to meet their daily communication needs (Centers for Disease Control and Prevention, 2007) and thus require AAC intervention. For children with developmental disabilities and CCN, access to AAC services is essential to support their participation in education, social development, language and communication skills, and future life outcomes (e.g., Drager et al., 2010; Romski et al., 2015).
A growing body of evidence suggests that barriers to effective clinical and educational services are exacerbated for Black children and other children of color. Black and Asian children are less likely to receive a diagnosis of developmental delay by the time they reach preschool or kindergarten than white children, even when controlling for developmental level via standardized assessment (Gallegos et al., 2021). Parents report that delays in diagnosis for developmental disabilities are at least partly related to health care providers ignoring parent concerns and/or implicitly providing racially biased care (Dababnah et al., 2018). Clinical and special education services (such as speech-language pathology services, including AAC intervention) are not attained easily without a qualifying diagnosis, either in the education system or through outside service providers. Lower diagnosis rates thus lead to reduced access to services for Black and other children of color. However, even when a diagnosis is provided, Black and Hispanic/Latino children are still less likely than white children to receive related clinical services (Gallegos et al., 2021).
Preliminary evidence suggests that racial inequity in service delivery extends to school-based intervention services (e.g., speech-language pathology, occupational therapy, and physical therapy). From preschool through secondary education, though Black and Hispanic children are more likely than their white peers to have a communication disorder diagnosis, they are less likely to receive intervention services (Black et al., 2015). Black children are less likely to receive speech-language pathology services at ages 2, 4, and 5 years than their otherwise-similar white peers (Morgan et al., 2016). Black parents also report having access to fewer services for their children with developmental disabilities within and outside the school system, as compared to white parents (Taylor & Henninger, 2015; Thomas et al., 2007). Additionally, evidence-based practices for children with developmental disabilities have been researched overwhelmingly with white children (West et al., 2016); little empirical research has addressed effective service delivery within the school system for children with developmental disabilities from culturally and linguistically diverse backgrounds.
Research suggests that the prekindergarten years have a formative impact on the long-term racial disparities observed in educational achievement (Braun et al., 2010; Farkas, 2003). Thus, investigating service delivery inequality associated with race in preschool-age children is crucial. Children with developmental disabilities and CCN often have the most extensive service delivery needs and thus may be at the greatest risk from inequities in services. Given the importance of early AAC intervention specifically for young children with developmental disabilities and CCN, this study conducted a post hoc secondary data analysis to investigate the relationship between race and AAC service delivery for children with developmental disabilities and CCN using data originally collected by Brady (2016). Specifically, the current study addressed the following questions: Does the amount of AAC intervention per week reported by teachers for preschool children with developmental disabilities differ for Black children as compared to white children? Is the pattern consistent across time (i.e., at study initiation and study completion 2 years later)?
Method
Design
The current study employed a post hoc data analysis methodology to investigate associations between race and amount of AAC intervention reported by teachers within a preexisting data set. Post hoc data analysis addresses a novel, a priori research question using data previously collected for a different research aim (Hollenbeck & Wright, 2017). Given that no previous research has examined the evidence for racial disparities in AAC service delivery, post hoc methods are an appropriate place to start, as they allow for the initial exploration of a potential phenomenon, as well as the generation of hypotheses to be tested with more rigorous methods (Hollenbeck & Wright, 2017). The data set was accessed through the Archive of Data on Disability to Enable Policy and Research, a joint initiative between the Center for Large Data Research and Data Sharing in Rehabilitation and the Interuniversity Consortium for Political and Social Research, as well as with permission from the original principal investigator (Brady, 2016). All present analyses were completed post hoc using the publicly available data set from the original study.
Description of the Original Data Set From Brady (2016)
The original data set was part of a larger longitudinal study that aimed to identify positive predictors of improving communication skills for children with developmental disabilities and CCN (Brady, 2016). The full data set from the study by Brady (2016) included a sample of 93 children with developmental disabilities enrolled in preschool programs in Topeka, Kansas, or Wichita, Kansas, in 2007. Children were nominated for participation by their preschool teacher or speech-language pathologist (SLP), and adherence to inclusion criteria was determined via caregiver/teacher report and/or direct observation (Barker et al., 2013). Original inclusion criteria for the study included the following: (a) 3–5 years old; (b) enrolled in a preschool program; (c) functional vision, hearing, and motor skills for direct selection; (d) English as the primary language spoken at home; (e) teaching plans that included AAC (graphic symbols, sign language, and/or speech generating devices); and (f) vocabulary of < 20 words, including AAC vocabulary (Brady, 2016). All children had a developmental disability of some kind, and half of the children had a diagnosis of ASD.
Participant race was recorded in the original data set but was not considered as a predictor of communication skills in the original study. A variety of demographic, observational, survey, and assessment measures related to communication were collected periodically over a 2-year time period, beginning when participants were in preschool and ending in elementary school. Specifically, the open-access data set included the following participant demographic variables: age, gender, race, and autism diagnosis. Child-level variables also included measures of participant language and communication: Mullen Scales of Early Learning (MSEL; Mullen, 1995), Peabody Picture Vocabulary Test (PPVT; Dunn & Dunn, 2007), Preschool Language Scales (PLS; Zimmerman et al., 2011), and the rate of child communicative acts during home observations. Amount of AAC intervention per week was the only variable related to intervention services. Family-level variables were restricted to rate of adult input provided to the participants during home observations. Classroom-level measures included the Early Childhood Environment Rating Scale (Harms et al., 2005) and Design to Learn (Rowland & Schweigert, 2003). However, these scales were completed for less than a third of all participants.
Participants Included in the Current Study
The current study included all children from the Brady (2016) data set who met the following additional criteria: (a) had reported data on race indicating that they were either Black or white only and (b) had reported data on the amount of AAC intervention time per week at study initiation. A total of 78 children (14 Black and 64 white) from the original 93 participants in Brady's sample met these criteria (see Table 1 for participant demographics). Unfortunately, data related to caregiver report of Asian, Hispanic or Latino, Pacific Islander, and Native American race/ethnicity were masked in the publicly available data set in order to maintain confidentiality (Brady, 2016). Thus, although exploring potential disparities in intervention for all children of color—including multiethnic and multiracial children—is imperative, the current data set only allowed for comparisons of AAC intervention time between Black and white children. Fifteen participants from the Brady study were excluded from the current analyses due to missing data for race (one child) or amount of AAC intervention time at study initiation (one child); race masked in the data set (seven children); or multiple racial categories selected (six children). Based on the data provided in the original data set, there were no statistically significant differences at study initiation between the Black and white children included in this study in terms of age, child language skills (as measured by the MSEL, the PLS, and the PPVT), rate of children's communicative acts, or rate of adult input during home observations (see Table 1).
Table 1.
Participant demographics.
| Measure | Study initiation |
Study completion |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black (n = 14) | White (n = 64) | Black (n = 12) | White (n = 54) | |||||||||||
| Gender | ||||||||||||||
| Female | 4 | 14 | 4 | 12 | ||||||||||
| Male | 10 | 50 | 8 | 42 | ||||||||||
| Diagnosis | ||||||||||||||
| DD | 7 | 33 | 5 | 29 | ||||||||||
| ASD |
7 |
31 |
7 |
25 |
|
|||||||||
|
|
M
|
Range
|
SD
|
M
|
Range
|
SD
|
p
|
M
|
Range
|
SD
|
M
|
Range
|
SD
|
p
|
| Age (months) | 44.5 | 36–55 | 5.8 | 46.2 | 36–61 | 9.0 | .38 | — | — | — | — | — | — | — |
| MSEL-RL | 19.7 | 19–29 | 2.7 | 20.1 | 19–41 | 3.6 | .72 | 19.8 | 19–24 | 1.6 | 21.5 | 19–41 | 5.9 | .08 |
| MSEL-EL | 19.0 | 19–19 | 0.0 | 19.2 | 19–29 | 1.3 | .64 | 19.7 | 19–26 | 2.1 | 21.0 | 19–46 | 5.6 | .48 |
| PLS | 52.4 | 50–67 | 4.9 | 51.8 | 50–70 | 4.3 | .64 | 50.8 | 50–58 | 2.4 | 54.2 | 50–94 | 10.5 | .04* |
| PPVT | 65.0 | 40–94 | 22.2 | 58.4 | 0–105 | 21.8 | .57 | 54.7 | 20–83 | 17.0 | 47.4 | 0–92 | 28.3 | .41 |
| Child comm. | 1.7 | 0.2–5.3 | 1.6 | 1.9 | 0.0–7.6 | 1.8 | .65 | 2.7 | 0.4–4.8 | 1.4 | 2.7 | 0.1–8.6 | 2.0 | .96 |
| Adult input | 3.9 | 1.8–7.3 | 1.7 | 4.2 | 2.1–9.2 | 1.5 | .50 | 3.8 | 1.2–6.4 | 1.6 | 4.3 | 1.1–9.0 | 1.7 | .37 |
Note. Values for all variables drawn from Brady (2016). DD = developmental disability; ASD = autism spectrum disorder; MSEL = Mullen Scales of Early Learning (Mullen, 1995); RL = Receptive Language T score; EL = Expressive Language T score; PLS = Preschool Language Scales standard score (Zimmerman et al., 2011); PPVT = Peabody Picture Vocabulary Test standard score (Dunn & Dunn, 2007); Child comm = rate of participant communicative acts (initiations, responses, and repairs) during home observation; Adult input = rate of adult input to participant (initiations, prompts, and responses) during home observations.
p < .05.
An additional 12 participants (two Black; 10 white) from the sample of 78 were missing data for amount of AAC intervention at study completion; therefore, analyses at study completion only included 66 participants. Rates of attrition were relatively consistent across race (14% and 16% losses for Black children and white children, respectively).
Measures
The dependent variable in the current study was the amount of AAC intervention per week, as measured via report from each participant's classroom teacher. Specifically, in the original study, the teachers were asked, “During a typical school week, how often does this child receive direct AAC intervention?” (Brady et al., 2013, p. 12). The teachers were then presented with five ordinal categorical choices (i.e., never, less than 30 min/week, 30–59 min/week, 60–89 min/week, and 90+ min/week). 2 Teachers were instructed to include any AAC intervention provided throughout the day (e.g., not just specific speech therapy sessions) in their estimations and to exclude group activities that were not directed specifically to the target child's AAC use (Brady et al., 2013). These measures were collected every 6 months during the original study, but only values at study initiation and study completion (approximately 2 years apart) were included in the current analyses, in order to provide a general picture of the amount of AAC intervention over time.
Data Analysis
Given the ordinal nature of the response options for the dependent variable, nonparametric statistical methods were used (Hinton, 2014). Specifically, separate Mann–Whitney U tests were used to compare Black versus white participants' reported minutes of AAC intervention per week (on the ordinal scale) at (a) study initiation and (b) study completion. Mann–Whitney U tests are appropriate for comparing two independent samples of nonparametric data (Hinton, 2014), as in this research question.
Results
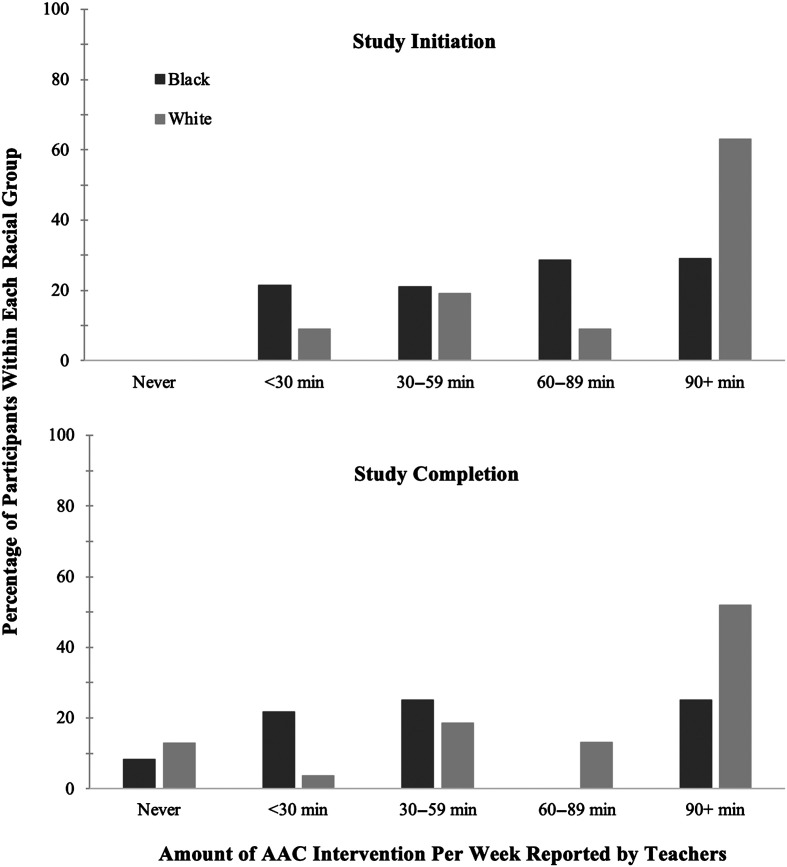
Figure 1 presents the percentage of Black and white students in each category of AAC intervention time at study initiation and completion according to teacher report. At the initiation of the study, the majority of white children (63%) were reported to receive 90+ min per week of AAC intervention, whereas only 29% of Black children received this much AAC intervention. The Mann–Whitney U test for AAC intervention time for Black participants compared to white participants at study initiation was statistically significant (U = 305.0, p = .039, r = .23). A similar discrepancy was apparent at the completion of the study: At this point, 52% of white children were reported to receive 90+ min, whereas only 25% of Black children were reported to receive this much AAC intervention per week. Notably, by the end of the study, the majority (75%) of Black children were receiving less than 60 min of AAC intervention per week. Again, the Mann–Whitney U test was statistically significant at study completion (U = 205.5, p = .036, r = .26). The factor of race approached a medium effect size at the 0.3 level at both time points, representing a degree of difference between the two groups “visible to the naked eye” (Cohen, 1992, p. 156).
Figure 1.
Percentage of participants in each racial group reported in each augmentative and alternative communication (AAC) intervention category.
Discussion
The results of this secondary data analysis showed that (a) Black children received less AAC intervention compared to their white peers (according to teacher report); (b) this disparity persisted over time (i.e., from the start of the study to the end, 2 years later); and (c) by study completion, 75% of Black children were receiving less than 60 min of AAC intervention per week (defined as all activities that incorporated AAC intervention, not just dedicated speech-language pathology services).
Racial Disparities in Amount of AAC Intervention
This preliminary evidence of persistent racial disparities in AAC service delivery is troubling, considering the importance of early AAC intervention (e.g., Drager et al., 2010), the formative role of early language development on long-term outcomes (Parsons et al., 2011), and the impact of kindergarten readiness on the chronic opportunity gap between white students and students of color that persists throughout K–12 education (Farkas, 2003; A. Flores, 2007). Without access to—and sufficient instruction in—AAC, children with developmental disabilities and CCN encounter significant barriers in education, language acquisition, and social development (Light & McNaughton, 2012) that persist into adulthood (Howlin et al., 2000). Furthermore, unmet communication needs increase the risk for challenging behaviors (Drager et al., 2010; Muharib et al., 2019), which may result in more punitive measures for Black children and other children of color, leading to less access to instruction (Gregory et al., 2010; Morris & Perry, 2016), greater communication challenges, and a vicious cycle of inequity.
Though troubling, the evidence for racial disparities in the amount of AAC intervention is perhaps not surprising. Research assessing racial inequality in school-based clinical services is limited, but the available studies consistently reveal the same general pattern. Black children are more likely to be diagnosed with a communication disorder but less likely to receive speech-language pathology services than their white peers (Black et al., 2015; Morgan et al., 2016). Black parents report having access to fewer intervention services for their children with developmental disabilities (Taylor & Henninger, 2015; Thomas et al., 2007) and are less likely to report receiving family-centered services (Montes & Halterman, 2011), a trend that reflects the experiences of Black youth with special health care needs generally (Chisolm et al., 2021). These disparities continue across the school years into adulthood, with Black and Hispanic transition-age youth with developmental disabilities having worse outcomes after high school than their white peers (e.g., lower rates of employment, independence, postsecondary enrollment, social participation, and access to health care; Eilenberg et al., 2019). The results of the current study thus reflect the overarching trend of inequality in services for Black children and other children of color with developmental disabilities and communication disorders.
Importantly, the results also suggest that these racial disparities persist across time (i.e., 2 years from study initiation to completion). It is likely that the children in this study transitioned to different classrooms, potentially at different schools, by study completion. Thus, different teachers may have reported the amount of AAC intervention for each participant at study completion versus study initiation, and participants' AAC services may have been coordinated by different SLPs. However, the same concerning trend of racial inequity in reported intervention services persisted, suggesting that the disparities extend beyond the scope of individual schools, classroom teams, SLPs, or teachers and offering evidence of the potential impact of structural racism on AAC intervention services.
Access to Sufficient AAC Intervention
The limited amount of AAC intervention provided each week is concerning, especially so for Black children. Importantly, teacher reports in this study included “all” activities in the classroom that incorporated AAC intervention—not simply dedicated speech-language services. Thus, the limited amount of AAC intervention reported is especially troubling. Empirical data on the required intensity of AAC intervention are sparse, but available research suggests that a minimum of 60 min per week of targeted AAC instruction is required to effect meaningful gains in communication for preschool children with CCN (Kasari et al., 2014; Logan et al., 2022; Romski et al., 2010) and children with more complex needs require significantly more than 60 min of targeted AAC intervention per week (Kasari et al., 2014). Unfortunately, 28% of white participants in the current study were reported to receive less than 60 min of AAC intervention throughout the week at study initiation, increasing to 35% at study completion. However, 42% of Black children received less than 60 min of AAC intervention at study initiation, and by study completion, 75% of Black children received less than 60 min of AAC intervention per week, an insufficient amount of intervention to attain meaningful gains.
Within this sample, insufficient AAC intervention intensity is a concern for both white and Black preschool children, but the degree of concern is greater for Black children. The participants were young children in the midst of the formative language-learning developmental period (mean age at study completion for all participants: 5;10 [years;months]), and they all had significant receptive and expressive language delays (see Table 1). Early language, communication, and AAC intervention are critical to support better long-term outcomes (Drager et al., 2010; Parsons et al., 2011; Romski et al., 2015). This paucity of AAC intervention might be expected to negatively impact language development, education, social skills, and future life outcomes for these children with CCN, disproportionately affecting Black children.
The current data set did not allow for investigation of what causal factors may have been associated with the decrease in AAC service provision over time for both white and Black participants observed in these data. Although research generally supports more intensive intervention, the decline in services—or differences in amount of AAC intervention generally—noted for these participants might have been related to a number of factors, including the increasing age of the children, improvements in communication skills, larger classes and/or caseloads (potentially related to the transition to elementary school), or even increasing proficiency with speech. Future research should explore patterns of change in AAC service provision over time for white and Black children.
It is important to recognize that the Black participants in this study may actually have had access to more AAC services than most preschool-age Black children with developmental disabilities and CCN typically receive. At the time of the study, participants already had a diagnosis, and the majority were receiving at least some AAC services during preschool. Research suggests that Black children in preschool and kindergarten are generally less likely to receive a diagnosis of developmental delay than their otherwise-similar white counterparts (Gallegos et al., 2021) and are less likely to receive services even with that diagnosis (Black et al., 2015; Gallegos et al., 2021; Morgan et al., 2016). Some evidence also indicates that Black parents are more likely to have developmental concerns about their child but are less likely to secure an Individualized Family Service Plan or an Individualized Education Program (Marshall et al., 2016). Thus, Black children may be less likely to get any services than their white peers. The results of this study suggest that even when Black children receive AAC services, there are significant racial disparities in the reported amount of AAC service delivery, and these disparities persist over time. Few Black participants received the amount of AAC intervention required to achieve meaningful gains. Furthermore, given racial inequities in diagnosis and service provision generally (Gallegos et al., 2021), the degree of disparity in access to AAC services for Black children with developmental disabilities who would benefit from AAC intervention is likely even greater than that observed in this study.
Potential Mediating Factors
The original study conducted by Brady (2016) from which the current data were drawn was not designed to address questions of racial inequality. This limits the degree to which factors that may mediate the relationship between race and reported amount of AAC intervention can be explored within this sample. Additionally, as the aims of the original study did not include comparing children of different racial groups, there may be random intrinsic factors that differ between Black and white participants, simply by chance. However, post hoc analyses indicated that there were no statistically significant differences between the two participant groups with respect to gender, age, diagnosis (ASD or other developmental disability), language skills at study initiation, rate of child communicative acts, or adult communicative input at home (see Table 1). Thus, it is unlikely that these child intrinsic factors explain the reported disparity in amount of AAC intervention per week within this sample.
Unreported family-, classroom-, provider-, and/or school-level factors may have potentially mediated the relationship between race and amount of AAC intervention observed in this sample. For example, family socioeconomic status, parental education, school/community resource level, or classroom staff experience/qualifications were not reported in the data set but may have all been mediating factors in the observed difference in amount of AAC intervention. These mediating factors are often referred to as the social determinants of health, which are defined as “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (Healthy People 2030, n.d.).
Rate of adult communicative input was the only variable reported in the original study at the caregiver/family level (Brady, 2016) and did not differ significantly for Black versus white participants at either study initiation or study completion (see Table 1). No data relating to participants' classrooms, teachers, SLPs, or schools were available within the original data set (excluding two classroom environment ratings, though these were only completed for less than a third of participants). Thus, the contributions of family, classroom, provider, or school factors to the observed relationship between race and amount of AAC intervention per week could not be explored in these data.
However, it is crucial to underscore that research consistently demonstrates that many potentially mediating factors at the child, family, classroom, and school levels systematically disadvantage Black children and other children of color (Merolla & Jackson, 2019; Reskin, 2012; Williams & Cooper, 2019), including child mental and physical health (Alegria et al., 2010; Magaña et al., 2012), income and housing inequality (Wagmiller & Adelman, 2009), rates of school disciplinary action (Cyphert, 2014; Gregory et al., 2010; Morris & Perry, 2016), teacher perceptions of student potential (Gershenson et al., 2016), and school resource level (Darling-Hammond, 2013). The disproportionately negative impact of these factors on Black and other children of color stems from a history of structural inequality established and maintained by systemic racism in the United States (Merolla & Jackson, 2019; Reskin, 2012; Williams & Cooper, 2019), or the “historical, cultural, institutional and interpersonal [dynamics] that routinely advantage whites while producing cumulative and chronic adverse outcomes for people of color” (Lawrence & Keleher, 2004, p. 1). Information regarding these types of factors was not available within this sample, and thus, the impact of these (or other) variables on the observed disparity in amount of AAC intervention per week could not be investigated.
Implications for Practice
Estimates suggest that at least half of the achievement gap in 12th-grade performance between white and Black students is attributable to differences already established at kindergarten entry (Farkas, 2003). This delineates the importance of equitable preschool education and services for Black children and other children of color. When a line is drawn connecting disparate race-related academic outcomes to race-related inequities in education, it becomes apparent that the achievement gap is better characterized as an opportunity gap (A. Flores, 2007). Unlike the achievement gap framework, which focuses on the perceived deficits of children who underperform on specific outcome measures, the opportunity gap framework focuses on the differential resources and experiences available to students in educational settings (A. Flores, 2007; O. J. Flores & Gunzenhauser, 2021; Smith et al., 2016). Access to AAC systems and services in the schools is one type of resource or opportunity that should be equitably offered to students with CCN, regardless of race.
Although the current research is preliminary and post hoc, the evidence of statistically significant and sustained racial disparities in reported amount of AAC services for preschool children with developmental disabilities is alarming. Given the large body of evidence for racial inequality in education generally, it is important to acknowledge that these results may reflect a larger ongoing pattern of racial inequity in access to AAC systems and services for Black and other children of color with developmental disabilities. What can be done to address these opportunity inequities? (See Table 2 for a summary list of recommendations for individual SLPs; classrooms, schools, and school districts; preservice preparation programs; and researchers in the field.)
Table 2.
Action steps to address racial disparities in augmentative and alternative communication (AAC) services.
| Target group | First steps |
|---|---|
| Speech-language pathologists |
|
|
Classrooms, schools, and school districts |
|
|
Preservice preparation programs |
|
|
ASHA |
|
|
Researchers in communication sciences and disorders |
|
Note. SLPs = speech-language pathologist; ASHA = American Speech-Language-Hearing Association; AAC = augmentative and alternative communication.
SLPs
The American Speech-Language-Hearing Association's (ASHA) Code of Ethics calls for equitable service delivery for all individuals (ASHA, 2016). Individual SLPs have a responsibility to protect against racial inequality in education and related services. Furthermore, SLPs need to ensure that they demonstrate family-centered and culturally responsive AAC practices such as the following (adapted from ASHA, 2021; Blanchett et al., 2009; Mandak et al., 2017; Soto & Yu, 2014).
Engage in self-reflection regarding perceptions and attitudes about racial, cultural, and linguistic factors (see ASHA's Cultural Competence Check-In; ASHA, 2021).
Evaluate the impact of race, class, culture, and language on access to AAC services; recognize that services often reflect white, middle-class, English-speaking values.
Acknowledge the family and individual with CCN as experts in their own lived experiences; establish collaborative relationships in planning and implementing services.
Integrate the family's and individual's goals into intervention plans.
Strive to address each individual's and family's unique needs; respect cultural, communication, and language norms for each community.
Communicate regularly with the individual with CCN and their family, utilizing their preferred communication methods and language.
Consider the trajectory of bilingual (or multilingual) language development when assessing the language and communication of bilingual (or multilingual) individuals.
Select and personalize AAC systems that reflect the individual's and family's needs and priorities including their language(s)/dialect(s) and culture(s).
Work with families to integrate AAC into existing routines within relevant family, school, and community contexts.
In addition to regularly engaging in self-reflection regarding perceptions and attitudes about cultural and linguistic factors, SLPs should complete regular checks (equity audits) of their own caseloads to critically assess whether they are providing services equitably (for further information on equity audits, readers are referred to Green, 2017; Skrla et al., 2004, 2009). If evidence of service disparities emerges (e.g., in access to AAC assessment, systems, or intervention services), SLPs should explore what barriers may be contributing to these disparities and develop action plans to address them. Barriers contributing to disparities may be present at any level. For example, implicit bias may unconsciously contribute to lower expectations and potentially fewer hours of intervention per week, or decreased carryover of intervention by classroom staff across the school day. Underfunding of schools serving Black or other communities of color may result in higher caseloads for SLPs and/or less funds available to acquire appropriate AAC systems. Addressing noted AAC service disparities may require collaboration with other professionals (e.g., AAC specialists, classroom teachers, administrators, and social workers) and families. This collaboration is especially critical to ensure that there is adequate training of family and educational professionals to support carryover of AAC in classrooms and homes, extending AAC intervention throughout the day to ensure sufficient intensity of services to effect meaningful gains. If no racial disparities are observed, these actions will simply reinforce best practice. However, if SLPs do identify evidence of racial disparities in service delivery within their caseloads, these practices can serve as a first step to effect positive change.
Classrooms, Schools, and School Districts
Action plans to reduce racial disparities should extend beyond the individual SLP to include entire classrooms, schools, and school districts. Equity audits should also be conducted at these levels to evaluate whether AAC services and systems are sufficient and whether they are distributed equitably. These audits should target all stages of AAC intervention to determine, for example, (a) whether students of all racial and ethnic backgrounds with CCN are equally likely to receive AAC assessments; (b) whether they are equally likely to be recommended for AAC systems; (c) whether the percentage of Black and other students of color receiving AAC services reflects their representation in populations at risk for CCN (e.g., ASD, cerebral palsy, Down syndrome, and multiple disabilities); (d) whether AAC systems provided are culturally and linguistically appropriate (vocabulary, symbol representation, output, etc.) for students and their families; (e) whether the frequency of AAC services is consistent for children of all racial and ethnic backgrounds with similar skills and needs within a classroom, school, school district, and across districts; and (f) whether students and families from all racial and ethnic communities are offered equal opportunities to participate in developing AAC intervention plans.
Disparities in AAC intervention may not be as apparent at the classroom or individual school level but become evident between schools within a district or across school districts. Racial inequities in services at these levels may be related (at least in part) to broader issues in equitable access to adequate facilities and funding (e.g., due to underfunding or insufficient facilities, some schools may have larger class sizes, and thus less time and personnel to integrate AAC intervention into classroom routines as consistently). However, schools and school districts can take a crucial step to increase awareness of racial inequities in service delivery by conducting equity audits to determine if and where these disparities may exist and investigate the potential direct causal factors (Williams & Cooper, 2019). The results of these audits can be leveraged to both increase awareness within that school or district about where disparities in service delivery may exist and guide the development of action plans to address them. Concrete data highlighting inequitable services can support the need for in-service training for school staff, buoy public support, facilitate requests for additional funding, put pressure on local or regional government agencies, or all of the above—depending upon the direct factors contributing to the disparity. Ultimately, educational leaders and policy makers should shift their orientation toward racial disparities from an achievement gap to an opportunity gap perspective. Leaders who do so are better equipped to develop clear, responsible, and focused plans of action to address racial inequities in their schools and districts (O. J. Flores & Gunzenhauser, 2021).
Preservice Preparation Programs
The problem of racial disparities must also be addressed proactively through changes to preservice preparation programs in speech-language pathology. One effective route to decreasing racial disparities in health care has been to diversify the health care workforce (Williams & Cooper, 2019). This same strategy may be effective in attaining greater equity in speech-language pathology services. Currently, over 90% of SLPs are white (ASHA, 2019). It is incumbent upon speech-language pathology preservice preparation programs to increase the diversity of their cohorts in order to bolster the cultural and linguistic diversity in the speech-language pathology workforce (see Guiberson & Vigil, 2021, for recommendations). In addition to diversifying the preservice student body and the clinical workforce, professional organizations such as ASHA should strive to diversify their leadership. Preliminary research in education suggests that white teachers' expectations for Black students may be 30%–40% lower than Black teachers' expectations (Gershenson et al., 2016). If this pattern of decreased expectations is similar for SLPs, increasing diversity of the workforce and leadership could have positive implications for addressing disparities in AAC and other communication services for children with disabilities. If diversifying the speech-language pathology workforce mirrors results in health care and education, it may lead to increased expectations for Black children with communication disorders, more service providers working in underserved populations, better clinician–family communication and outcomes for Black and other children of color, and greater student and caregiver satisfaction with services (Gershenson et al., 2016; Williams & Cooper, 2019). All of these factors could directly improve the quality and degree of access to speech-language pathology services generally and AAC services specifically for children of color.
Curriculum and clinical training in preservice preparation programs must also include meaningful opportunities to learn about and work with culturally and linguistically diverse communities. Although ASHA's standards for certification of clinical competence require practicum experiences with individuals from culturally and linguistically diverse backgrounds (Council for Clinical Certification in Audiology and Speech-Language Pathology of the American Speech-Language-Hearing Association, 2018), the degree to which all preservice programs can and do comprehensively provide these opportunities is inconsistent (Hammond et al., 2009). It is incumbent upon ASHA and preservice preparation programs themselves to develop program assessment methods and program supports to ensure that preservice professionals have experience during their training working with culturally and linguistically diverse clients. It is essential that these preservice experiences encompass more than simply learning facts about culturally and linguistically diverse groups. Research suggests that both promoting empathy for individuals from different communities and addressing issues of inequality from a social justice perspective have positive results on minimizing prejudice and discrimination (Stephens et al., 2021; Whitford & Emerson, 2019).
ASHA can provide greater support for preservice preparation programs to ensure that future clinicians develop the competencies to provide effective, culturally responsive services. This support may take the form of concrete guidelines for curriculum content related to family-centered and culturally responsive practice, as well as topics of inequality and social justice. ASHA could also provide resources for clinical opportunities for preservice clinicians to work with culturally and linguistically diverse communities. Preservice programs should engage in continuous quality improvement with regular input from students and graduates to assess preparation to work with culturally and linguistically diverse communities.
It is important to note that the data set used in this study is quite dated, and ASHA has made notable changes in preservice curricula and certification standards in the intervening time. For example, in 2018, ASHA added cultural competency and diversity, equity, and inclusion (DEI) within the certification standards (Council for Clinical Certification in Audiology and Speech-Language Pathology of the American Speech-Language-Hearing Association, 2018). Most recently, the Council on Academic Accreditation (CAA) for Audiology and Speech-Language Pathology established revised DEI standards for graduate program accreditation that will go into effect on January 1, 2023 (CAA, n.d.). Below are two of the revised standards:
The program must provide evidence that students are given opportunities to identify and acknowledge: i) the impact of both implicit and explicit bias on clinical service delivery and actively explore individual biases and how they relate to clinical services (p. 3);
ii) the social determinants of health and environmental factors for individuals served. These variables include, but are not limited to, health and healthcare, education, economic stability, social and community context, and neighborhood and built environment, and how these determinants relate to clinical services (p. 3).
The five aforementioned variables reflect the five domains of the social determinants of health (Healthy People 2030, n.d.). The current study's findings demonstrate the importance of implementing the revised CAA standards in preservice programs. Future research will be needed to explore best practices in preservice programs and to demonstrate the extent to which the CAA revised standards reduce the occurrence of race-based disparities in clinical practice.
Researchers in Communication Sciences and Disorders
Research addressing racial disparities in speech-language pathology services is limited. Future research is urgently required to tackle this critically important topic. Additionally, evidence suggests that children of color are underrepresented in the intervention research literature (Ellis et al., 2021; West et al., 2016). This lack of representation in research populations may mask issues of inequity in access to appropriate services or even aggravate the problem further, by failing to address the efficacy of interventions across culturally and linguistically diverse populations. Researchers in communication sciences and disorders (including AAC researchers specifically) can increase understanding of racial disparities by (a) actively recruiting culturally and linguistically diverse participants; (b) regularly collecting and reporting more extensive demographic data, including not only student racial and ethnic information but also family and community variables (social determinants of health) that have been linked to inequality as well (e.g., maternal education, socioeconomic status, and school district achievement); and (c) investigating the impact of race on services. Additionally, researchers in communication sciences and disorders can begin to create a more equitable landscape of empirical knowledge and evidence-based practice by partnering with families and communities of color in order to ensure that future research is responsive to the needs and priorities of culturally and linguistically diverse communities. For researchers who explore racial disparities in education and health care generally, inclusion of participants with CCN in these studies can help to address the intersectionality of disability, communication, race, and culture.
Implications for System Change
It is imperative that SLPs, educational staff, and administrators recognize and address racial inequity in individual classrooms and caseloads, schools, school districts, and communities. However, it is also essential to recognize that systemic racism in the United States is pervasive across domains and institutions—not only in education but also in health care, housing, law enforcement, child welfare, and so forth (Hayes-Greene & Love, 2018). These domains of systemic racism intersect, creating a dynamic, complex, mutually reinforcing set of subsystems across societal domains (Hayes-Greene & Love, 2018; Reskin, 2012; Williams & Cooper, 2019).
Large-scale change is needed to truly construct “communities of opportunity” (Williams & Cooper, 2019) across the United States for Black and other children of color, thereby closing existing system-wide opportunity gaps. Addressing racial inequality in only one domain (e.g., professionals' implicit bias) is unsustainable, as the influence of systemic racism in other intersecting, unaddressed social domains (e.g., underfunding of schools in Black communities) will continually seep back in (Hayes-Greene & Love, 2018). Initiatives focused on reducing racial disparities in health and health care have highlighted several potential avenues for creating communities of opportunity to combat systemic racism, including increasing early childhood development initiatives, improving community and housing conditions, creating equitable access to quality health care, and diversifying the health care workforce (Williams & Cooper, 2019). These types of initiatives offer avenues of system change to address disparities in education and speech-language pathology services, including AAC services specifically. Large-scale systemic change in the United States is vital.
Local initiatives can increase their power, impact, and longevity by extending collaborations as broadly as possible (Hayes-Greene & Love, 2018). For example, evidence suggests that developing family peer advocate relationships (i.e., when families with similar needs, such as supporting a child with ASD, provide knowledge and support to one another) can increase knowledge about relevant services, as well as empower families to access those services successfully (Jamison et al., 2017). Within a school system, an individual teacher could ally with their classroom team, other classrooms, related service providers, and school administration to address disparities in access to services. An individual school could ally with other schools in that district or outside organizations (e.g., social services, community organizations, and economic developers) to work toward restructuring the current systems in that community that disadvantage Black and other communities of color (Hayes-Greene & Love, 2018).
Limitations
This study represents an important first step in assessing racial inequities in AAC services for individuals with developmental disabilities, but there are several limitations that must be considered in interpreting the results.
Age of the Data
The original data set is dated (data at study initiation are from 2007) and may not reflect current practices within either these schools and school districts or the United States at large. Contemporary data addressing access to AAC systems and services are urgently required in order to determine the degree to which the observed disparities represent the current state of AAC service provision. However, more recent evidence indicates that racial disparities remain evident in other aspects of health care and education services (e.g., Dababnah et al., 2018; Gallegos et al., 2021), including in speech-language pathology services specifically (Morgan et al., 2016). Thus, it is likely that the racial disparities observed in this study persist as well.
AAC technology and access have changed substantially over the last decade (e.g., relatively greater access to free or lower cost tablet-based AAC applications), which may have impacted AAC systems and intervention within the schools. This increased access to AAC, along with a growing emphasis on training in AAC within preservice speech-language pathology programs, may have served to decrease disparities in access to AAC systems and services since these study data were collected. However, it is important to note that all participants in the present data set already had access to AAC systems and services as a part of their teaching plans, as a prerequisite for study enrollment, minimizing the impact of initial access to AAC systems and services on amount of intervention reported.
Participants
The ratio of white children as compared to Black children in this sample is notably unbalanced, though this ratio does represent the demographics of Topeka and Wichita per the 2010 Census (U.S. Census Bureau, n.d.). Overall, the study sample is quite small, insular, and especially lacking in sufficient numbers of Black participants. The small sample of Black children limits not only the statistical power of the results but also the generalizability of these data. With so few Black participants, it is difficult to generalize to the larger population of Black children with developmental disabilities and CCN. The sample in this study also only included children from English-speaking homes, neglecting issues of language and culture in AAC intervention. 3 Additionally, both Black and white participant groups experienced attrition from study initiation to study completion. However, though the number of participants lost varied by group, the percentage was similar and did not appear to differentially impact either gender or diagnostic categories.
Participants were not initially recruited with the aim of establishing equivalent groups of Black and white children. It is possible that, by chance, these two groups differed significantly on factors that could be impactful to the current study aims (communication skills, AAC proficiency, etc.). Unfortunately, data on these child-level characteristics are not comprehensive, and data on partner-level factors are minimal. However, no significant differences were found at study initiation across the child-level variables that were included in the data set: age, gender, diagnosis (ASD or other developmental disability), observations of child communicative acts or adult input to the child, or across a range of standardized language measures (MSEL, PLS, and PPVT; see Table 1). Nonetheless, children may have differed on unreported, relevant factors (length of time since AAC provision, AAC proficiency, type of AAC system, etc.). Prospective research is essential to better understand the complex interplay of these factors on any observed racial disparities in AAC service provision.
Data Set and Study Design
The current research used post hoc analysis methods. The original study by Brady (2016) was not designed to investigate the relationship between race and AAC services. Thus, results of the current study may have been impacted by potential confounding factors. For example, it is unclear whether any participants may have attended the same schools, been in the same classrooms, and/or had the same SLPs overseeing their AAC intervention services. Evidence suggests that racial segregation persists across public schools in the United States (Rothstein, 2019). Thus, nesting of students within this sample based on race is not inconceivable. If participants were nested in schools, in classrooms, or by providers in this way, it could impact interpretation of the findings.
Within Black communities, schools often have fewer resources than those in white communities (Darling-Hammond, 2013). Thus, whether or not Black or white participants were nested within particular schools or classrooms in this sample, it is possible that the schools attended by Black children were systematically underresourced compared to the schools attended by white children. Underresourced schools may have larger classrooms, less trained staff, or higher caseloads for teachers and SLPs. These factors could potentially impact not only the availability of material resources to provide AAC systems but also access to professionals with sufficient training in AAC intervention or the time in the school day to provide it. However, as noted earlier, the potential for nested data or differential school resource levels does not prevent the results of this study from serving as preliminary evidence of the influence of systemic racism on AAC service delivery. Nonetheless, these are critical factors to consider directly in future research.
Statistical Analyses
The results of the nonparametric statistical analysis were statistically significant at the α = .05 level. A conservative analytical approach might consider a smaller, corrected α level in order to determine statistical significance to control for multiple post hoc tests and decrease the probability of a Type I error (i.e., finding statistically significant results when in actuality there are no differences between groups). However, given the nature of the research questions (exploring the evidence for racial disparities in AAC services), the greater, more practical risk may be in committing a Type II error (i.e., accepting that there are no differences between groups when in actuality there are). If, on the basis of the current interpretation of results, SLPs, preservice preparation programs, schools, and school districts investigate the equity of their programs and find no racial disparities, little harm has been incurred. There is minimal risk involved in implementing the action plans recommended. However, if racial disparities in AAC services do exist but the current results are presented as insignificant in an abundance of statistical caution, harmfully inequitable practices may persist for Black and other children of color with developmental disabilities and CCN. In addition, given the small sample sizes (especially for Black participants), the statistical analyses in this study are underpowered. Thus, although more statistically conservative, applying a correction to the significance level for statistical analyses may do more harm than good in this case.
Measurement Scale
The manner in which the amount of AAC intervention per week was measured may have also impacted the interpretation of the results. The measurement scale relied on estimated reports from teachers, which could have differed from the actual, measurable amount of AAC intervention each participant received per week. The definition of “direct” AAC intervention provided to teachers by Brady (2016) could have also impacted estimates of the amount of intervention per week, if teachers misunderstood or interpreted “direct” intervention differently. Teachers were informed to consider all AAC instruction provided throughout the week, including direct intervention from an SLP, as well as carryover of instruction from classroom teachers and staff. However, what teachers considered carryover “instruction” within their classrooms may have differed. Additionally, classrooms that were larger or understaffed may have had a higher frequency of group-based activities, which teachers were told to disregard in their estimations if the activities did not directly target AAC intervention for the participating child.
Importantly, only the quantity of AAC instruction was measured, without addressing the quality of the AAC intervention provided. It is possible that the quality of intervention varied systematically across the two groups of children—either to bolster the impact of intervention for Black participants if they received higher quality services or to further disadvantage Black participants if they received lower quality AAC services. Regardless of quality, the discrepancy in the amount of AAC intervention provided still creates an opportunity barrier for Black children. However, future research is required that considers not only the quantity but also the quality of services provided.
The ordinal nature of the scale also minimizes the specificity of measurement. The actual amount of AAC intervention participants received per week represents a measure of time and is thus a continuous variable. However, it is reported in the data set as ordinal categories (i.e., never, less than 30 min, 30–59 min, 60–89 min, and 90+ min). Students who received 5 min of AAC intervention per week and those who received 25 min were all grouped into the same category of “less than 30 min per week.” Students who received 90 min of AAC intervention per week were grouped together with those who might have received substantially more (90+ min per week). These categories reduced the precision of the data and may have obscured the actual variability in amount of AAC intervention. It is possible that this process of categorization amplified or masked differences between Black and white students.
Future Research
Future research is essential to further investigate racial disparities across the spectrum of AAC services, within larger samples. Additionally, questions of disparity in AAC services must be extended to include all underrepresented racial and ethnic groups. Future research is also required to better understand the specific factors contributing to observed disparities in AAC or other speech-language pathology services and to suggest targeted avenues for intervention. These same questions surrounding the equity of AAC service provision should be explored in larger, more representative national databases to assess the generalizability of the current results. Larger educational databases also offer the opportunity to consider potential mediators (and moderators) of any observed inequities in AAC service delivery by including additional child, family, teacher, classroom, school, and community variables within statistical models.
Prospective studies are also a crucial next step, specifically designed to examine the evidence for racial disparities in AAC services, as well as potential direct causal factors. Future research should expand the focus of investigation to include multiple aspects of AAC assessment and intervention services (e.g., rates of referral for AAC assessments, provision of systems, quality of intervention, carryover by classroom staff, and family-centeredness of services). Intervention studies that aim to address inequities are critical. For example, prospective research is needed to assess the potential impact of equity audit processes in order to determine if these procedures can make a meaningful difference. It is also critical for researchers in communication sciences and disorders to work to develop partnerships with communities and families of color to ensure that research is consumer driven and is responsive to unmet needs and priorities. The evidence from health care and education suggests that large-scale change is needed to effectively address issues of racial inequality long term, given the pervasive, dynamic, mutually reinforcing nature of structural racism (Hayes-Greene & Love, 2018; Reskin, 2012; Williams & Cooper, 2019). Intervention research addressing direct causes of racial inequity in AAC services is one essential piece of this larger initiative.
Author Contributions
Lauramarie Pope: Conceptualization (Lead), Formal analysis (Lead), Methodology (Lead), Writing – original draft (Lead), Writing – review & editing (Lead). Janice Light: Conceptualization (Supporting), Formal analysis (Supporting), Methodology (Supporting), Supervision (Supporting), Writing – review & editing (Supporting). Amber Franklin: Writing – review & editing (Supporting).
Data Availability Statement
The data set analyzed during the current study is available in the Interuniversity Consortium for Political and Social Research repository, https://doi.org/10.3886/ICPSR36472.v1.
Acknowledgments
This article is based on open access data collected by Dr. Nancy Brady (2016; https://doi.org/10.3886/ICPSR36472.v1). Special thanks to Dr. Brady and her research team for making these data available for future research endeavors and providing additional information about the data collection process.
This research was completed in partial fulfillment of the requirements for the first author's doctoral program. It was supported in part by funding received from the U.S. Department of Education (The Penn State AAC Doctoral Leadership Grant H325D170024) and from the National Institute on Disability, Independent Living, and Rehabilitation Research (The RERC on AAC Grant 90REGE0014). The contents do not necessarily represent the policy of the funding agencies and you should not assume endorsement by the federal government.
Funding Statement
This article is based on open access data collected by Dr. Nancy Brady (2016; https://doi.org/10.3886/ICPSR36472.v1). This research was completed in partial fulfillment of the requirements for the first author's doctoral program. It was supported in part by funding received from the U.S. Department of Education (The Penn State AAC Doctoral Leadership Grant H325D170024) and from the National Institute on Disability, Independent Living, and Rehabilitation Research (The RERC on AAC Grant 90REGE0014). The contents do not necessarily represent the policy of the funding agencies and you should not assume endorsement by the federal government.
Footnotes
In this article, terms related to racial and ethnic identity are capitalized for all Black, Indigenous, and other people of color, whereas white is not capitalized. This choice reflects the “essential and shared sense of history, identity and community among people who identify as Black” (Associated Press, 2020), which is not reflected in the experiences of white people, as they “generally do not share the same history and culture, or the experience of being discriminated against because of skin color” (Associated Press, 2020).
It is important to note that this measure of AAC intervention per week reflects teacher report on an ordinal scale and thus does not directly represent the exact amount of time participants actually received AAC intervention in the classroom. However, for ease of reading, this variable is referred to as “amount of AAC intervention per week.” See the Limitations section for additional consideration of how the nature of this variable impacts interpretation of study results.
A second public access data set is available from the same original research project for children from Spanish-speaking homes but does not include reported amount of AAC intervention as a variable.
References
- Alegria, M. , Vallas, M. , & Pumariega, A. J. (2010). Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics, 19(4), 759–774. https://doi.org/10.1016/j.chc.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Speech-Language-Hearing Association. (2016). Code of ethics. http://www.asha.org/policy/
- American Speech-Language-Hearing Association. (2019). A demographic snapshot of SLPs: Data highlight some key characteristics of ASHA's SLP members. The ASHA Leader. https://leader.pubs.asha.org/doi/pdf/10.1044/leader.AAG.24072019.32 [Google Scholar]
- American Speech-Language-Hearing Association. (2021). Cultural competence checklist: Personal reflection. https://www.asha.org/siteassets/uploadedFiles/Cultural-Competence-Checklist-Personal-Reflection.pdf
- Associated Press. (2020, July 20). Explaining AP style on Black and white. https://apnews.com/article/9105661462
- Barker, R. M. , Akaba, S. , Brady, N. C. , & Thiemann-Bourque, K. (2013). Support for AAC use in preschool, and growth in language skills, for young children with developmental disabilities. Augmentative and Alternative Communication, 29(4), 334–346. https://doi.org/10.3109/07434618.2013.848933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binger, C. , & Light, J. (2006). Demographics of preschoolers who require AAC. Language, Speech, and Hearing Services in Schools, 37(3), 200–208. https://doi.org/10.1044/0161-1461(2006/022) [DOI] [PubMed] [Google Scholar]
- Black, L. I. , Vahratian, A. , & Hoffman, H. J. (2015). Communication disorders and use of intervention services among children aged 3–17 years: United States, 2012 (pp. 1–8). U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. [Google Scholar]
- Blanchett, W. J. , Klinger, J. K. , & Harry, B. (2009). The intersection of race, culture, language, and disability. Urban Education, 44(4), 389–409. https://doi.org/10.1177/0042085909338686 [Google Scholar]
- Brady, N. (2016). Language development of non-verbal children age 3 years through 7 years, 2007 to 2012 (ICPSR 36472). Interuniversity Consortium for Political and Social Research. https://doi.org/10.3886/ICPSR36472.v1 [Google Scholar]
- Brady, N. , Thiemann-Bourque, K. , Fleming, K. , & Matthews, K. (2013). Predicting language outcomes for children learning augmentative and alternative communication: Child and environmental factors. Journal of Speech, Language, and Hearing Research, 56(5), 1595–1612. https://doi.org/10.1044/1092-4388(2013/12-0102) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun, H. , Chapman, L. , & Vezzu, S. (2010). The Black–white achievement gap revisited. Education Policy Analysis Archives, 18, 21. https://doi.org/10.14507/epaa.v18n21.2010 [Google Scholar]
- Centers for Disease Control and Prevention. (2007). Prevalence of autism spectrum disorders—Autism and developmental disabilities monitoring network, 14 sites, United States, 2002. MMWR SS, 2007, 56(1). https://www.cdc.gov/mmwr/preview/mmwrhtml/ss5601a2.htm [PubMed] [Google Scholar]
- Chisolm, D. J. , Keedy, H. E. , Dolce, M. , Chavez, L. , Abrams, M. A. , & Sanders, L. (2021). Do health literacy disparities explain racial disparities in family-centered care for youths with special health care needs? Patient Education and Counseling, 104(4), 887–895. https://doi.org/10.1016/j.pec.2020.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. https://doi.org/10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Council for Clinical Certification in Audiology and Speech-Language Pathology of the American Speech-Language-Hearing Association. (2018). 2020 Standards for the certificate of clinical competence in speech-language pathology. http://www.asha.org/certification/2020-SLP-Certification-Standards
- Council on Academic Accreditation. (n.d.). Guidance to programs: How to demonstrate compliance with the expanded standard 3.4A and 3.4B diversity reflected in the curriculum. https://caa.asha.org/siteassets/files/2023-standard-3.4a-and-3.4b-guidance-to-programs.pdf
- Cyphert, A. B. (2014). Addressing racial disparities in preschool suspension and expulsion rates. Tennessee Law Review, 82, 893. [Google Scholar]
- Dababnah, S. , Shaia, W. E. , Campion, K. , & Nichols, H. M. (2018). “We had to keep pushing”: Caregivers' perspectives on autism screening and referral practices of Black children in primary care. Intellectual and Developmental Disabilities, 56(5), 321–336. https://doi.org/10.1352/1934-9556-56.5.321 [DOI] [PubMed] [Google Scholar]
- Darling-Hammond, L. (2013). Inequality and school resources: What it will take to close the achievement gap. In Carter P. L. & Welner K. G. (Eds.), Closing the opportunity gap: What America must do to give every child an even chance (pp. 77–97). Oxford University Press. https://doi.org/10.1093/acprof:oso/9780199982981.003.0006 [Google Scholar]
- Drager, K. , Light, J. , & McNaughton, D. (2010). Effects of AAC interventions on communication and language for young children with complex communication needs. Journal of Pediatric Rehabilitation Medicine, 3(4), 303–310. https://doi.org/10.3233/PRM-2010-0141 [DOI] [PubMed] [Google Scholar]
- Dunn, L. , & Dunn, D. (2007). The Peabody Picture Vocabulary Test–Fourth Edition (PPVT-4). The Psychological Corporation. [Google Scholar]
- Eilenberg, J. S. , Paff, M. , Harrison, A. J. , & Long, K. A. (2019). Disparities based on race, ethnicity, and socioeconomic status over the transition to adulthood among adolescents and young adults on the autism spectrum: A systematic review. Current Psychiatry Reports, 21(5), 32. https://doi.org/10.1007/s11920-019-1016-1 [DOI] [PubMed] [Google Scholar]
- Ellis, C. , Jacobs, M. , & Kendall, D. (2021). The impact of racism, power, privilege, and positionality on communication sciences and disorders research: Time to reconceptualize and seek a pathway to equity. American Journal of Speech-Language Pathology, 30(5), 2032–2039. https://doi.org/10.1044/2021_AJSLP-20-00346 [DOI] [PubMed] [Google Scholar]
- Farkas, G. (2003). Racial disparities and discrimination in education: What do we know, how do we know it, and what do we need to know? Teachers College Record, 105(6), 1119–1146. https://doi.org/10.1111/1467-9620.00279 [Google Scholar]
- Flores, A. (2007). Examining disparities in mathematics education: Achievement gap or opportunity gap? The High School Journal, 91(1), 29–42. https://doi.org/10.1353/hsj.2007.0022 [Google Scholar]
- Flores, O. J. , & Gunzenhauser, M. G. (2021). Justice in the gaps: School leader dispositions and the use of data to address the opportunity gap. Urban Education, 56(2), 261–288. https://doi.org/10.1177/0042085918801431 [Google Scholar]
- Gallegos, A. , Dudovitz, R. , Biely, C. , Chung, P. J. , Coker, T. R. , Barnert, E. , Guerrero, A. D. , Szilagyi, P. G. , & Nelson, B. B. (2021). Racial disparities in developmental delay diagnosis and services received in early childhood. Academic Pediatrics, 21(7), 1230–1238. https://doi.org/10.1016/j.acap.2021.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershenson, S. , Holt, S. B. , & Papageorge, N. W. (2016). Who believes in me? The effect of student–teacher demographic match on teacher expectations. Economics of Education Review, 52, 209–224. https://doi.org/10.1016/j.econedurev.2016.03.002 [Google Scholar]
- Green, T. L. (2017). Community-based equity audits. Educational Administration Quarterly, 53(1), 3–39. https://doi.org/10.1177/0013161X16672513 [Google Scholar]
- Gregory, A. , Skiba, R. J. , & Noguera, P. A. (2010). The achievement gap and the discipline gap: Two sides of the same coin? Educational Researcher, 39(1), 59–68. https://doi.org/10.3102/0013189X09357621 [Google Scholar]
- Guiberson, M. , & Vigil, D. (2021). Speech-language pathology graduate admissions: Implications to diversify the workforce. Communication Disorders Quarterly, 42(3), 145–155. https://doi.org/10.1177/1525740120961049 [Google Scholar]
- Hammond, C. , Mitchell, P. , & Johnson, M. (2009). Academic and clinical preparation for cultural and linguistic diversity in speech-language pathology: Program director perspectives. Contemporary Issues in Communication Science and Disorders, 36(Spring), 63–76. https://doi.org/10.1044/cicsd_36_S_63 [Google Scholar]
- Harms, T. , Clifford, R. M. , & Cryer, D. (2005). Early Childhood Environment Rating Scale. Teachers College Press. [Google Scholar]
- Hayes-Greene, D. , & Love, B. P. (2018). The groundwater approach: Building a practical understanding of structural racism. The Racial Equity Institute. [Google Scholar]
- Healthy People 2030. (n.d.). Social determinants of health. Retrieved June 1, 2022, from https://health.gov/healthypeople/priority-areas/social-determinants-health
- Hinton, P. R. (2014). Statistics explained (3rd ed.). Routledge. https://doi.org/10.4324/9781315797564 [Google Scholar]
- Hollenbeck, J. R. , & Wright, P. M. (2017). Harking, sharking, and tharking. Journal of Management, 43(1), 5–18. https://doi.org/10.1177/0149206316679487 [Google Scholar]
- Howlin, P. , Mawhood, L. , & Rutter, M. (2000). Autism and developmental receptive language disorder—A follow-up comparison in early adult life. II: Social, behavioural, and psychiatric outcomes. The Journal of Child Psychology and Psychiatry, 41(5), 561–578. https://doi.org/10.1111/1469-7610.00643 [DOI] [PubMed] [Google Scholar]
- Jamison, J. M. , Fourie, E. , Siper, P. M. , Trelles, M. P. , George-Jones, J. , Grice, A. B. , Krata, J. , Holl, E. , Shaoul, J. , Hernandez, B. , Mitchell, L. , McKay, M. M. , Buxbaum, J. D. , & Kolevzon, A. (2017). Examining the efficacy of a family peer advocate model for Black and Hispanic caregivers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(5), 1314–1322. https://doi.org/10.1007/s10803-017-3045-0 [DOI] [PubMed] [Google Scholar]
- Kasari, C. , Kaiser, A. , Goods, K. , Nietfeld, J. , Mathy, P. , Landa, R. , Murphy, S. , & Almirall, D. (2014). Communication interventions for minimally verbal children with autism: A sequential multiple assignment randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(6), 635–646. https://doi.org/10.1016/j.jaac.2014.01.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence, K. , & Keleher, T. (2004, October). Structural racism. In Race and Public Policy Conference, Berkeley, CA, United States. https://www.intergroupresources.com/rc/Definitions%20of%20Racism.pdf
- Light, J. , & McNaughton, D. (2012). Supporting the communication, language, and literacy development of children with complex communication needs: State of the science and future research priorities. Assistive Technology, 24(1), 34–44. https://doi.org/10.1080/10400435.2011.648717 [DOI] [PubMed] [Google Scholar]
- Logan, K. , Iacono, T. , & Trembath, D. (2022). A systematic search and appraisal of intervention characteristics used to develop varied communication functions in children with autism who use aided AAC. Research in Autism Spectrum Disorders, 90, 101896. https://doi.org/10.1016/j.rasd.2021.101896 [Google Scholar]
- Magaña, S. , Parish, S. L. , Rose, R. A. , Timberlake, M. , & Swaine, J. G. (2012). Racial and ethnic disparities in quality of health care among children with autism and other developmental disabilities. Intellectual and Developmental Disabilities, 50(4), 287–299. https://doi.org/10.1352/1934-9556-50.4.287 [DOI] [PubMed] [Google Scholar]
- Mandak, K. , O'Neill, T. , Light, J. , & Fosco, G. M. (2017). Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augmentative and Alternative Communication, 33(1), 32–41. https://doi.org/10.1080/07434618.2016.1271453 [DOI] [PubMed] [Google Scholar]
- Marshall, J. , Kirby, R. S. , & Gorski, P. A. (2016). Parent concern and enrollment in intervention services for young children with developmental delays. Exceptional Children, 82(2), 251–268. https://doi.org/10.1177/0014402915585563 [Google Scholar]
- Merolla, D. M. , & Jackson, O. (2019). Structural racism as the fundamental cause of the academic achievement gap. Sociology Compass, 13(6), e12696. https://doi.org/10.1111/soc4.12696 [Google Scholar]
- Montes, G. , & Halterman, J. S. (2011). White–Black disparities in family-centered care among children with autism in the United States: Evidence from the NS-CSHCN 2005–2006. Academic Pediatrics, 11(4), 297–304. https://doi.org/10.1016/j.acap.2011.02.002 [DOI] [PubMed] [Google Scholar]
- Morgan, P. L. , Hammer, C. S. , Farkas, G. , Hillemeier, M. M. , Maczuga, S. , Cook, M. , & Morano, S. (2016). Who receives speech/language services by 5 years of age in the United States? American Journal of Speech-Language Pathology, 25(2), 183–199. https://doi.org/10.1044/2015_AJSLP-14-0201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris, E. W. , & Perry, B. L. (2016). The punishment gap: School suspension and racial disparities in achievement. Social Problems, 63(1), 68–86. https://doi.org/10.1093/socpro/spv026 [Google Scholar]
- Muharib, R. , Correa, V. I. , Wood, C. L. , & Haughney, K. L. (2019). Effects of functional communication training using GoTalk Now™ iPad® application on challenging behavior of children with autism spectrum disorder. Journal of Special Education Technology, 34(2), 71–79. https://doi.org/10.1177/0162643418783479 [Google Scholar]
- Mullen, E. M. (1995). Mullen Scales of Early Learning (AGS ed.). AGS. [Google Scholar]
- Parsons, S. , Schoon, I. , Rush, R. , & Law, J. (2011). Long-term outcomes for children with early language problems: Beating the odds. Children & Society, 25(3), 202–214. https://doi.org/10.1111/j.1099-0860.2009.00274.x [Google Scholar]
- Reskin, B. (2012). The race discrimination system. Annual Review of Sociology, 38(1), 17–35. https://doi.org/10.1146/annurev-soc-071811-145508 [Google Scholar]
- Romski, M. , Sevcik, R. A. , Adamson, L. B. , Cheslock, M. , Smith, A. , Barker, R. M. , & Bakeman, R. (2010). Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. Journal of Speech, Language, and Hearing Research, 53(2), 350–364. https://doi.org/10.1044/1092-4388(2009/08-0156) [DOI] [PubMed] [Google Scholar]
- Romski, M. , Sevcik, R. A. , Barton-Hulsey, A. , & Whitmore, A. S. (2015). Early intervention and AAC: What a difference 30 years makes. Augmentative and Alternative Communication, 31(3), 181–202. https://doi.org/10.3109/07434618.2015.1064163 [DOI] [PubMed] [Google Scholar]
- Rothstein, R. (2019). The myth ofde factosegregation. Phi Delta Kappan, 100(5), 35–38. https://doi.org/10.1177/0031721719827543 [Google Scholar]
- Rowland, C. , & Schweigert, M. (2003). Design to Learn Inventory. OHSU Design to Learn Projects. [Google Scholar]
- Skrla, L. , McKenzie, K. B. , & Scheurich, J. J. (2009). Using equity audits to create equitable and excellent schools. Corwin Press. https://doi.org/10.4135/9781452218953 [Google Scholar]
- Skrla, L. , Scheurich, J. J. , Garcia, J. , & Nolly, G. (2004). Equity audits: A practical leadership tool for developing equitable and excellent schools. Educational Administration Quarterly, 40(1), 133–161. https://doi.org/10.1177/0013161X03259148 [Google Scholar]
- Smith, P. S. , Trygstad, P. J. , & Banilower, E. R. (2016). Widening the gap: Unequal distribution of resources for K–12 science instruction. Education Policy Analysis Archives, 24(8), 1–38. https://doi.org/10.14507/epaa.v24.2207 [Google Scholar]
- Soto, G. , & Yu, B. (2014). Considerations for the provision of services to bilingual children who use augmentative and alternative communication. Augmentative and Alternative Communication, 30(1), 83–92. https://doi.org/10.3109/07434618.2013.878751 [DOI] [PubMed] [Google Scholar]
- Stephens, J. M. , Rubie-Davies, C. , & Peterson, E. R. (2021). Do preservice teacher education candidates' implicit biases of ethnic differences and mindset toward academic ability change over time? Learning and Instruction, 78, 101480. https://doi.org/10.1016/j.learninstruc.2021.101480 [Google Scholar]
- Taylor, J. L. , & Henninger, N. A. (2015). Frequency and correlates of service access among youth with autism transitioning to adulthood. Journal of Autism and Developmental Disorders, 45(1), 179–191. https://doi.org/10.1007/s10803-014-2203-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, K. C. , Ellis, A. R. , McLaurin, C. , Daniels, J. , & Morrissey, J. P. (2007). Access to care for autism-related services. Journal of Autism and Developmental Disorders, 37(10), 1902–1912. https://doi.org/10.1007/s10803-006-0323-7 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. (n.d.). Quick facts: Wichita City, Kansas; Topeka City, Kansas. https://www.census.gov/quickfacts/fact/table/wichitacitykansas,topekacitykansas/PST04219
- Wagmiller, R. L. , & Adelman, R. M. (2009). Childhood and intergenerational poverty: The long-term consequences of growing up poor. The National Center for Children in Poverty. [Google Scholar]
- West, E. A. , Travers, J. C. , Kemper, T. D. , Liberty, L. M. , Cote, D. L. , McCollow, M. M. , & Stansberry Brusnahan, L. L. (2016). Racial and ethnic diversity of participants in research supporting evidence-based practices for learners with autism spectrum disorder. The Journal of Special Education, 50(3), 151–163. https://doi.org/10.1177/0022466916632495 [Google Scholar]
- Whitford, D. K. , & Emerson, A. M. (2019). Empathy intervention to reduce implicit bias in pre-service teachers. Psychological Reports, 122(2), 670–688. https://doi.org/10.1177/0033294118767435 [DOI] [PubMed] [Google Scholar]
- Williams, D. R. , & Cooper, L. A. (2019). Reducing racial inequities in health: Using what we already know to take action. International Journal of Environmental Research and Public Health, 16(4), 606. https://doi.org/10.3390/ijerph16040606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman, I. , Steiner, V. , & Pond, R. (2011). PLS-5: Preschool Language Scales, Fifth Edition. The Psychological Corporation. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set analyzed during the current study is available in the Interuniversity Consortium for Political and Social Research repository, https://doi.org/10.3886/ICPSR36472.v1.