Abstract
Purpose of Review
The population is aging, and recent epidemiologic work reveals that an increasing number of older adults are presenting to the intensive care unit (ICU) with preexisting geriatric syndromes. In this update, we discuss recent literature pertaining to the long-term recovery of older ICU patients and highlight gaps in current knowledge.
Recent Findings
A recent longitudinal study demonstrated that the incidence of frailty, disability, and multimorbidity among older ICU patients is rising; these geriatric syndromes have all previously been shown to impact long-term recovery. Recent studies have demonstrated the impact of social factors in long-term outcomes after critical illness; for example, social isolation was recently shown to be associated with disability and mortality among older adults in the year after critical illness. Socioeconomic disadvantage is associated with higher rates of dementia and disability following critical illness impacting recovery, and further studies are necessary to better understand factors influencing this disparity. The COVID-19 pandemic disproportionately impacted older adults resulting in worse outcomes and increased rates of functional decline and social isolation. In considering how to best facilitate recovery for older ICU survivors, transitional care programs may address the unique needs of older adults and help them adapt to new disability if recovery has not been achieved.
Summary
Recent work demonstrates increasing trends of geriatric syndromes in the ICU, all of which are known to confer increased vulnerability among critically ill older adults and decrease the likelihood of post-ICU recovery. Risk factors are now known to extend beyond geriatric syndromes and include social risk factors and structural inequity. Strategies to improve post-ICU recovery must be viewed with a lens across the continuum of care, with post-ICU recovery programs targeted to the unique needs of older adults.
Keywords: long-term recovery, older adults, geriatric syndromes, post-ICU syndrome
Introduction
By 2040 the number of Americans aged 65 years or older will be 80.8 million, a doubling of the older adult population in the United States since 2000 [1], when more than half of intensive care unit (ICU) days were already contributed by older adults [2]. As the population ages, we expect to see an increase in the number of older adults in the ICU as well as a shift towards the “oldest old;” indeed, a longitudinal study found that the proportion of ICU admissions among patients aged 85-94 had increased from 14.1% to 20.1% between 1996-2010 alone [3]. The vast majority (88%, according to the same study) of older adults survive their ICU hospitalization and must then begin the journey of long-term recovery in function and cognition, very often with vulnerability factors that pose additional challenges to recovery. Indeed, nearly half of older ICU survivors will not achieve functional recovery (defined as a return to their pre-ICU functional baseline) within 6 months of critical illness [4]. The COVID-19 pandemic highlighted many of these challenges to recovery due to its disproportionate impact on older adults [5]. In this review, we provide an update on the science of long-term recovery after critical illness among older adults.
Geriatric Syndromes in the ICU: Increasing Trends Over Time
Geriatric syndromes include conditions such as frailty, disability, multimorbidity, and cognitive impairment, which confer increased vulnerability to adverse outcomes among older adults [6]. It is well-established that the presence of one or more geriatric syndromes before ICU admission is associated with poorer long-term outcomes among older ICU survivors, including disability, mortality, and a loss of functional independence [7, 8, 9, 10, 11]. Using data from the Health and Retirement Study, Cobert and colleagues recently evaluated epidemiologic trends in geriatric syndromes among older adults admitted to the ICU between 1998 and 2015 [12**]. The study found that the adjusted prevalence of disability increased from 15% to 24%, frailty increased from 37% to 45%, and multimorbidity increased from 54% to 72%. The increasing prevalence of geriatric syndromes among older adults admitted to the ICU highlights the pressing need to integrate geriatrics principles and management concepts into critical care medicine education and practice [13*, 14].
Frailty
The association of frailty with increased in-hospital and long-term mortality is well-established among adult ICU patients [15], and among older ICU patients, frailty is additionally associated with increased disability and incident nursing home admission, signaling a loss of independence [7, 8, 16]. Recent literature on frailty has also underscored its impact during the pandemic. The COPE Study Collaborators leveraged an existing network of 10 clinical centers in the United Kingdom (U.K) and one in Italy that had experience in collecting frailty data using the Clinical Frailty Scale (CFS) [17] to investigate the prevalence of frailty and its association with outcomes among hospitalized COVID patients [18*]. At each site, the frailty assessment was overseen by a team that included a geriatrician, intensivist, and emergency medicine physician. Among the 1564 enrolled patients, approximately half were frail (772, 49.4%), and worsening frailty was associated with time to death and 7-day mortality. Although this study was not limited to older adults, most participants were older (median age 74 years, interquartile range [IQR] 61-83). The association of frailty with higher 30-day mortality among critically ill older adults with COVID was confirmed by the COVIP study investigators in a prospective multicenter study of 1346 adults aged ≥70 [19*].
One knowledge gap that had not previously been addressed was whether frailty is associated with persistent critical illness or chronic critical illness. In a recent retrospective study of adults admitted to 168 ICUs in Australia and New Zealand, Darvall and colleagues sought to answer this question in the 269,785 patients with complete CFS scores, using a primary outcome of persistent critical illness, defined as an ICU stay of ≥10 days [20*]. Each one unit increase in the CFS was associated with increased odds of developing persistent critical illness (adjusted odds ratio 1.08, 95% CI 1.06-1.1). In a different study, the same group demonstrated that addition of frailty scores to the APACHEIII score at ICU admission modestly improves discrimination for mortality in a cohort of adult ICU patients [21].
Studies in the last decade have stressed the influence of pre-hospitalization frailty on mortality and morbidity, but less is known about frailty after the ICU. Using CFS scores measured in the ICU and at 3 and 12 months among a cohort of 567 adults with a median age of 61 years (IQR 51-70), Brummel and colleagues demonstrated that frailty (defined as a CFS ≥5) was newly acquired in 61% of participants [22]. In a subsequent study, Baldwin and colleagues characterized post-ICU frailty subtypes using pre-ICU frailty, post-ICU frailty phenotype, and serum biomarkers in a prospective cohort study of 185 older survivors with acute respiratory failure [23*], and tested associations between frailty subtypes and functional recovery. Five frailty subtypes were identified with a 49% recovery rate across subtypes. The three subtypes with the slowest recovery were characterized by greater systemic inflammation and anabolic hormone deficiencies at hospital discharge.
Despite the widespread use of frailty measures in ICU research, and the implications of frailty for the long-term recovery potential of older ICU patients, the feasibility of implementation of routine frailty screening in clinical practice remains uncertain. Although the Clinical Frailty Scale remains the most widely used frailty measure in ICU research, a systematic review assessed the interrater reliability of CFS across ICU frailty studies and found that most studies relied on proxies for scoring, and reliability of measurements was not usually assessed [24]. Surkan and colleagues conducted a single-center observational study that compared CFS scores of patients between geriatricians and intensivists and found an interrater reliability of 0.29, suggesting that the CFS is inconsistent and operator-dependent [25]. Even groups that have successfully evaluated frailty across large swaths of the population have had high levels of missingness in frailty data collected in the ICU [20*, 21]. Given the strong link between frailty and short- and long-term outcomes among critically ill older adults, future work should determine whether routine frailty assessments upon ICU admission by clinicians are feasible and reliable, or whether more objective measures of baseline vulnerability, such as baseline functional status, should be used instead.
Functional Status and Preventing In-Hospital Functional Decline
Baseline functional status and pre-ICU functional trajectories are important determinants of post-ICU outcomes [10, 26] and new literature published during the pandemic has highlighted the centrality of functional status in predicting outcomes among critically ill older adults. In a prospective international study of older adults (age ≥70 years) hospitalized with COVID, the COVIP study investigators demonstrated the association of baseline disability in activities of daily living (ADL) with 3-month mortality, whether operationalized as a continuous variable or any disability [27*]. Participants with both frailty (defined as a CFS score ≥5) and any ADL disability had the highest mortality (72% at 3 months) in the cohort. Another study evaluated the association of mild and moderate COVID and mobility and physical function among 51,338 community-dwelling adults (41.9% older adults), and found that adults with a confirmed or probable COVID diagnosis had greater odds of worsening ability to engage in household activity (OR 1.89, 95% CI, 1.11-3.22) or participate in physical activity (OR 1.91, 95% CI, 1.32-2.76) compared to adults without a COVID diagnosis during the same period [28*]. Of note, the majority (94.2%) of participants diagnosed with COVID were not hospitalized.
Up to 65% of critically ill survivors suffer weakness, loss of muscle mass, and polyneuropathy; and among hospitalized older adults there is a high prevalence of acute and chronic sarcopenia [29]. As such, the prevention of in-hospital functional decline remains a top priority among older adults in the hospital and ICU. In a meta-analysis evaluating 60 trials investigating physical rehabilitation among adult ICU patients, Wang and colleagues found that physical rehabilitation focused on functional exercises up to 5 days per week improved physical function at the time of discharge [30]. While this study did not exclusively assess physical rehabilitation among older adults, it considered the dose and type of rehabilitation in its evaluation. Among hospitalized older adults, Martínez-Velilla and colleagues conducted a multicenter, randomized controlled trial of an exercise intervention among patients aged 75 and older [31*]. The exercise intervention included twice daily physical rehabilitation sessions of 20 minutes’ duration, 5-7 days per week, compared to usual care (which did include physical rehabilitation). The exercise intervention significantly improved the two primary outcomes, both of which were functional outcomes: the score on the Short Performance Physical Battery (SPPB) and ADLs as measured with the Barthel Index.
Multimorbidity and Polypharmacy
Multimorbidity, the coexistence of two or more chronic conditions, is a recognized geriatric syndrome that is heterogenous in phenotype and outcome [32]. In 2008, 62% of older adults had multimorbidity [33], and the prevalence of multimorbidity among older ICU patients continues to rise [12**]. McPeake and colleagues conducted a matched cohort study of 3,112 mostly older adults in the non-ICU and ICU setting [34*]. The study found that ICU survivors had higher hospital readmission rates in the year following critical illness. Additionally, multimorbidity was strongly associated with long-term mortality (hazard ratio [HR] 2.17; 95% CI 1.51-3.13) compared to no comorbidities.
Multimorbidity often leads to polypharmacy, defined as the long-term use of five or more prescribed drugs. A recent population-wide cohort study assessed preadmission polypharmacy prior to ICU admission among 23,844 mostly older adults admitted to ICUs across Scotland [35*]. The study found that polypharmacy was present in nearly 30% of all patients, and that polypharmacy patients were more likely to be older (median age 66, IQR 55-75). In the multivariable analysis, including adjustment for multimorbidity, polypharmacy was associated with a 22% relative increase in the hazard of one-year emergency hospital readmission (adjusted HR 1.22, 95% CI 1.16-1.28).
Given the prevalence of multimorbidity in older patients and the accompanied downstream effects, Blum and colleagues conducted a cluster randomized control trial of inpatient wards in four European countries inclusive of more than two thousand older adults with multimorbidity (≥3 chronic conditions) and polypharmacy (≥5 long-term medications) to assess the outcomes of a structured pharmacotherapy optimization intervention [36*]. The study found that five out of six participants experienced inappropriate prescribing, and 62% of the intervention group were able to implement medication changes. Although the intervention reduced polypharmacy and inappropriate prescribing, it did not significantly reduce drug-related hospital admissions at one year. Future work will need to evaluate similar interventions among older ICU patients to see if a reduction in polypharmacy can improve long-term outcomes.
Delirium and Cognitive Impairment
Long-term cognitive impairment has shown to persist in a quarter of patients up to a year after critical illness, with a longer duration of delirium associated with poor cognitive outcomes [37]. During the COVID-19 pandemic, Kennedy and colleagues found that delirium was the primary symptom in 28% of 817 older adults presenting to the emergency department with COVID and the sixth most common presenting sign or symptom [38]. During the pandemic, delirium was further perpetuated in hospitalized older adults due to restriction of visitors, masked faces and muffled voices affecting communication, and prolonged periods of social isolation [39*].
One evidence-based approach for delirium prevention is the Hospital Elder Program (HELP) [40]. The program was designed for hospitalized older adults and emphasizes strategies to prevent or reduce delirium including frequent orientation, therapeutic activities, pain control, and vision and hearing enhancement. In a cluster randomized trial of six surgical floors at a hospital in China, older adults admitted for a scheduled elective surgery who received the HELP program had a lower incidence of post-operative delirium within 7 days post-procedure than those who did not receive the program (2.6% [n=4] intervention vs. 19.4% [n=25] control; relative risk 0.14, 95% CI 0.05-0.38). Implementation of the exact program may be challenging in the ICU, but similar principles can be adopted. For example, hearing impairment is associated with lack of functional recovery among older adult ICU survivors and can perpetuate delirium, yet is recognized as a modifiable factor [41*]. Future work should evaluate the feasibility and effectiveness of the HELP program and other geriatric models of care in the ICU [42*].
Given the risk of long-term cognitive impairment after critical illness, particularly for older ICU survivors, Palakshappa and colleagues evaluated the rate of screening for and diagnosis of cognitive impairment among older adults in post-ICU outpatient clinical care using data from the Medicare Annual Wellness Visit (AWV) at their clinical center [43*]. Among 696 older adults followed for one year after critical illness, 172 (24.7%) completed the AWV, and the cumulative incidence of cognitive impairment detected at the AWV was only 3.4%. These findings suggest a large burden of unrecognized cognitive impairment and highlight the need to develop feasible and sustainable screening modalities for post-ICU cognitive impairment.
Social Isolation
Social isolation is the objective state of having few social relationships, while loneliness is the subjective feeling of isolation [44]. Prior to the COVID-19 pandemic in the United States, one quarter of older adults were socially isolated and 43% reported loneliness [45]. Though exact numbers are not known, the COVID-19 pandemic increased the number of older adults in social isolation due to global bans on social interaction [46]. In a longitudinal cohort study using nationally representative data from the National and Aging Trends Study (NHATS) prior to the pandemic, Falvey and colleagues evaluated the association of social isolation with disability and mortality over the year after critical illness among older adults. Worsening social isolation was associated with an increased risk of post-ICU disability and mortality, such that the most severely socially isolated older adults experienced a 50% higher disability burden and 119% higher hazard of death in the year after critical illness [47*].
Future work in this area should focus on three key areas: screening for social isolation, interventions to treat social isolation, and the role of the healthcare system in screening and intervening upon social isolation. As stated by the National Academy of Medicine [45], healthcare systems remain a relatively untapped partner in this area; yet, contact with the healthcare system may represent the only opportunity for socially isolated persons to be identified. Some studied interventions include virtual and in-person social support groups, weekly phone check-in phone-calls for isolated older adults, and a “Geriatric Buddy Program” [48*, 49*]. Additionally, hearing impairment, which is common among older adults, is associated with limited social engagement and may represent an additional target for intervention [50*].
Socioeconomic Disadvantage
In 2019, a systemic review of ten studies found patients with socioeconomic disadvantage had higher mortality across critical illness continuum; the authors advocated for inclusion of socioeconomic demographics in future critical care studies [51]. In a recent longitudinal study, Jain and colleagues evaluated the association of individual-level socioeconomic disadvantage, represented by dual-eligibility for Medicaid and Medicare, with the three outcomes of the post-ICU syndrome: physical function (operationalized as disability in ADLs), cognitive function, and mental health symptoms [52*, 53]. Socioeconomic disadvantage was associated with a 28% increase in disability and 9.8-fold greater odds of developing probable dementia in the year after critical illness. Another innovative study by Falvey and colleagues assessed neighborhood-level socioeconomic disadvantage using the Area Deprivation Index [54*]. Authors found that increased socioeconomic neighborhood deprivation was associated with increased disability among older adults during the year after critical illness.
The COVID-19 pandemic has drawn sharp attention to structural inequity in our health care system [55*]. Although many studies have evaluated associations with important short-term outcomes, including a Scottish study demonstrating the association of socioeconomic deprivation with higher rates of ICU admission and increased 30-day mortality [56], less has been published on associations with long-term recovery among older adults who have survived a critical illness with COVID. This will undoubtedly be a focus of work in the coming months and years, and studies should evaluate long-term outcomes among the most vulnerable older adults as well as interventions to reduce disparities in long-term recovery.
Illnesses and injuries after critical illness
Gill and colleagues conducted a prospective study of 209 adults aged 70 years or older that found that illnesses and injuries leading to hospitalizations and emergency department (ED) visits are common in the year following critical illness [57*]. Of the events analyzed, hospitalizations were significantly associated with a lower likelihood of functional recovery; additionally, hospitalizations and ED visits were associated with episodes of functional decline over the year after critical illness. Functional status is dynamic, however, and older adults have the potential to recover from an episode of functional decline due to illness or injury. This study highlights the need for older ICU survivors to maintain access to care during the vulnerable post-ICU period to prevent illnesses and injuries that may present additional barriers to recovery. Unfortunately, access to health care services during the COVID-19 pandemic was particularly difficult for older adults. In a study of a home-based primary care program for older adults which shifted to telehealth visits during the pandemic, Kalicki and colleagues found that 65% of patients were not able to attend healthcare encounters due to barriers including advanced dementia, vision and hearing impairment, or other cognitive impairments [58*]. Other studies evaluating barriers to telemedicine use among older adults found that older adults faced challenges including difficulty with platform use, language barriers, lack of desire to meet virtually, and lack of caregiver assistance [59*, 60].
Post-ICU Recovery and Transitional Care Programs
Despite a growing interest in post-ICU clinics, these remain relatively uncommon in the United States. Transitional care programs may be better suited to older adults who are more likely to have mobility limitations and a higher existing burden of clinic visits, which may affect their ability or willingness to attend a post-ICU clinic.
In a multi-center randomized control trial, Taylor and colleagues implemented the Sepsis Transition and Recovery (START) program in middle-aged and older adults with suspected sepsis [61*]. The program included best practices of post-sepsis care including screening for new impairments, anticipation and mitigation of health deterioration, and palliative care when appropriate. The intervention group had a reduced primary composite outcome of 30-day mortality or rehospitalization compared to usual care, and the effect remained in a subgroup analysis of older adults (age ≥65). Major and colleagues conducted a feasibility study of a home-based rehabilitation program called REACH (Rehabilitation After Critical illness and Hospital Discharge). REACH tailored exercises by physical and occupational therapists to improve ability in ADLs and increase muscle strength [62*]. The study showed that an early individualized home-based rehabilitation program was feasible for survivors of critical illness and improved satisfaction and adherence. Future work should build on these studies by developing and testing comprehensive home-based programs that are designed to address the unique needs of older adults during post-ICU recovery. Moreover, future work should evaluate whether these programs are most effective among vulnerable older adults, such as those with frailty, as frailty is associated with gaps in care coordination [63*].
Caregivers of Older ICU Survivors
Caregivers are essential stakeholders in the ICU recovery process, particularly for older adults [64]. Sevin and colleagues conducted semi-structured interviews with 20 caregivers of ICU survivors and found two major themes: unmet needs of caregivers and poor transitions of care [65*]. Caregivers found that during post-discharge period there was fragmentation of care resulting in undue burden on caregivers. A cross-sectional study surveyed eighty caregivers of community-living older adults and found that a higher degree of frailty among older adults was correlated with higher levels of overall burden among caregivers [66*]. Findings in these studies reveal the pitfalls in transitions of care and elucidate the need for a comprehensive care pathway with support for both caregivers and older ICU survivors.
Perceptions of Recovery
When discussing long-term recovery after critical illness, it is essential that we consider both objective measures of recovery and patient perceptions of recovery. Thurston and colleagues interviewed 35 adult ICU survivors and found that among survivors who described themselves as recovered, there were themes of acceptance of illness, strong support from social networks, and dedication to goals of recovery including active involvement with rehabilitation [67]. Another cross-sectional study evaluated self-perceived long-term recovery and satisfaction among older ICU survivors who had been admitted for abdominal sepsis and found that though survivors may report incomplete recovery following critical illness, they were still satisfied with their level of function [68*]. These findings highlight the potential of adapting to new disability or impairments after critical illness for the approximately half of older ICU survivors who will not achieve functional recovery after critical illness. Although we (as a field) should keep working across the continuum of ICU care to improve the likelihood of functional recovery for older adults, we can also help older ICU survivors adapt to new impairments.
Conclusion
Recent epidemiologic work has demonstrated the rising trend of geriatric syndromes (disability, frailty, and multimorbidity) among older adults admitted to the ICU, highlighting the need for attention to these factors during ICU care and adaptation of geriatric models of care in the ICU. Aside from geriatric syndromes, social isolation and socioeconomic disadvantage are additional factors that contribute to baseline vulnerability and adversely affect long-term recovery among older ICU survivors (figure 1). The impact of these factors on long-term recovery were highlighted during the COVID-19 pandemic, which disproportionately affected older adults. Transitional care programs after discharge may be uniquely suited to older ICU survivors; however, there are many opportunities across the continuum of ICU and post-ICU care for future work to improve the long-term recovery of older ICU survivors.
Figure. Barriers to long-term recovery for older ICU survivors across the continuum of critical illness.
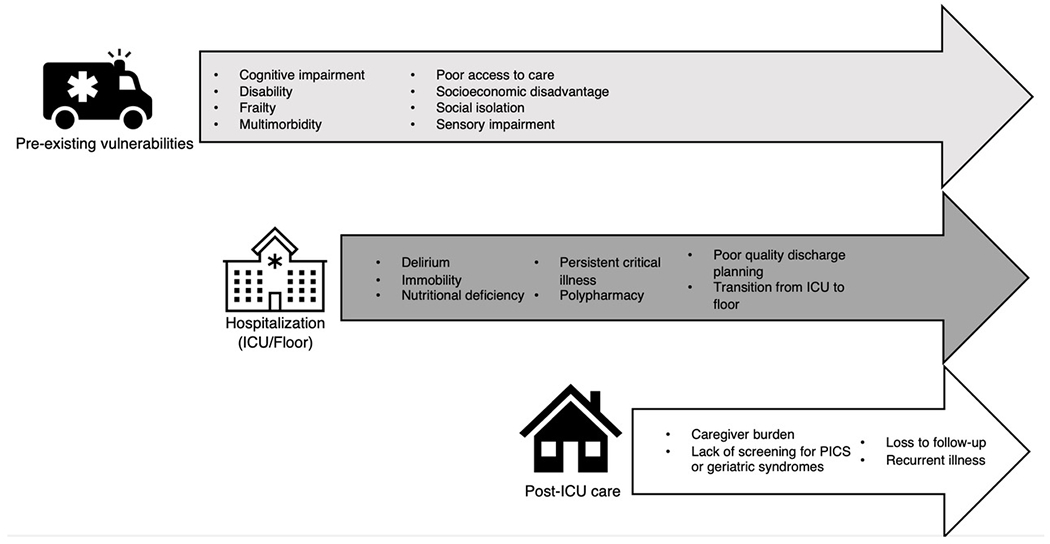
The bulleted lists present factors associated with a lower likelihood of long-term recovery and barriers to long-term recovery after a critical illness among older adults. The arrows represent time across the continuum of critical illness.
Source: Original
Key points:
Recent epidemiologic work has demonstrated the rising trend of geriatric syndromes (disability, frailty, and multimorbidity) among older adults admitted to the ICU, highlighting the need for attention to these factors during ICU care and adaptation of geriatric models of care in the ICU.
Social and structural factors, such as social isolation and socioeconomic disadvantage, are associated with a decreased likelihood of long-term recovery after critical illness among older adults.
The COVID-19 pandemic disproportionately affected older adults and exacerbated many of the factors (social isolation, delirium, etc.) associated with poor long-term outcomes after critical illness.
Transitional care programs may be uniquely suited to facilitating the post-ICU recovery of older adults, and attention should be paid to preventing recurrent illnesses and supporting caregivers.
Acknowledgments
Dr. Ferrante is supported by a Paul B. Beeson Emerging Leaders in Aging Career Development Award from the National Institute on Aging (K76AG057023) and the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342).
Footnotes
Conflicts of Interest: None.
References and recommended reading:
Papers of particular interest, published within the annual period of review, (18 months/2021-2022) have been highlighted as:
*special interest
** of outstanding interest
- 1.US Department of Health and Human Services. [Internet]. acl.gov US Department of Health and Human Services; May, 2020. Available from: acl.gov/sites/default/files/Aging%20and%20Disability%20in%20America/2020ProfileOlderAmericans.Final.pdf [DOI] [PubMed]
- 2.Angus DC, Kelley MA, Schmitz RJ, et al. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762–70. [DOI] [PubMed] [Google Scholar]
- 3.Somme D, Maillet JM, Gisselbrecht M, et al. Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Intensive Care Med. 2003;29(12):2137–43. [DOI] [PubMed] [Google Scholar]
- 4.Ferrante LE, Pisani MA, Murphy TE, et al. Factors Associated with Functional Recovery among Older Intensive Care Unit Survivors. Am J Respir Crit Care Med. 2016;194(3):299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murthy S, Archambault PM, Atique A, et al. Characteristics and outcomes of patients with COVID-19 admitted to hospital and intensive care in the first phase of the pandemic in Canada: a national cohort study. CMAJ Open 2021. Jan-Mar; 9(1): E181–E188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–63. [DOI] [PubMed] [Google Scholar]
- 7.Ferrante LE, Pisani MA, Murphy TE, et al. The Association of Frailty with Post-ICU Disability, Nursing Home Admission, and Mortality: A Longitudinal Study. Chest. 2018;153(6):1378–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brummel NE, Bell SP, Girard TD, et al. Frailty and Subsequent Disability and Mortality among Patients with Critical Illness. Am J Respir Crit Care Med. 2017;196(1):64–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferrante LE, Murphy TE, Leo-Summers LS, et al. The Combined Effects of Frailty and Cognitive Impairment on Post-ICU Disability among Older ICU Survivors. Am J Respir Crit Care Med. 2019;200(1):107–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrante LE, Pisani MA, Murphy TE, et al. Functional trajectories among older persons before and after critical illness. JAMA Intern Med. 2015;175(4):523–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidet B, de Lange DW, Boumendil A, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.**.Cobert J, Jeon SY, Boscardin J, et al. Trends in Geriatric Conditions Among Older Adults Admitted to U.S. ICUs Between 1998 and 2015. Chest. 2022;161(6):1555–65. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used data from Medicare-linked Health and Retirement Survey to evaluate trends in geriatric syndromes among older adults admitted to the from 1998 and 2015. The prevalence of frailty, disability, and multimorbidity increased during this time, emphasizing the need for attention to these factors during the care of older adults in the ICU.
- 13.*.Brummel NE. Increasing Vulnerability in Older Adults With Critical Illness: Implications for Clinical Care and Research. Chest. 2022;161(6):1436–7. [DOI] [PMC free article] [PubMed] [Google Scholar]; This editorial comments on Cobert et al. study “Trends in Geriatric Conditions Among Older Adults Admitted to the US ICUs Between 1998 and 2015” and advocates for better assessment strategies for baseline vulnerability and a better understanding of geriatric syndromes across critical care illness and survivorship.
- 14.Brummel NE, Ferrante LE. Integrating Geriatric Principles into Critical Care Medicine: The Time Is Now. Ann Am Thorac Soc. 2018;15(5):518–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muscedere J, Waters B, Varambally A, et al. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43(8):1105–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hope AA, Law J, Nair R, et al. Frailty, Acute Organ Dysfunction, and Increased Disability After Hospitalization in Older Adults Who Survive Critical Illness: A Prospective Cohort Study. J Intensive Care Med. 2020;35(12):1505–12. [DOI] [PubMed] [Google Scholar]
- 17.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5(8):e444–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]; This multicenter observational study evaluated the prevalence of frailty and its association with outcomes among hospitalized COVID patients in Europe. Approximately half of the participants were frail, and worsening frailty was associated with time to death and 7-day mortality.
- 19.*.Jung C, Flaatten H, Fjolner J, et al. The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care. 2021;25(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this prospective, multicenter study of 1346 critically ill older adults with COVID, frailty was associated with higher 30-day mortality.
- 20.*.Darvall JN, Bellomo R, Bailey M, et al. (2022). “Impact of frailty on persistent critical illness: a population-based cohort study.” Intensive Care Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated the association between frailty and persistent critical illness in a large cohort of adult ICU patients across Australia and New Zealand.
- 21.Darvall JN, Bellomo R, Paul E, et al. Routine Frailty Screening in Critical Illness: A Population-Based Cohort Study in Australia and New Zealand. Chest. 2021;160(4):1292–303. [DOI] [PubMed] [Google Scholar]
- 22.Brummel NE, Girard TD, Pandharipande PP, et al. Prevalence and Course of Frailty in Survivors of Critical Illness. Crit Care Med. 2020;48(10):1419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.*.Baldwin MR, Pollack LR, Friedman RA, et al. Frailty subtypes and recovery in older survivors of acute respiratory failure: a pilot study. Thorax. 2021;76(4):350–9. [DOI] [PMC free article] [PubMed] [Google Scholar]; This prospective study identified and characterized post-ICU frailty subtypes and found that the subtypes with the slowest recovery had greater systemic inflammation and more anabolic deficiencies.
- 24.Pugh RJ, Ellison A, Pye K, et al. Feasibility and reliability of frailty assessment in the critically ill: a systematic review. Crit Care. 2018;22(1):49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Surkan M, Rajabali N, Bagshaw SM, et al. Interrater Reliability of the Clinical Frailty Scale by Geriatrician and Intensivist in Patients Admitted to the Intensive Care Unit. Can Geriatr J. 2020;23(3):235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.*.Bruno RR, et al. (2022). “The association of the Activities of Daily Living and the outcome of old intensive care patients suffering from COVID-19.” Annals of Intensive Care 12(1). [DOI] [PMC free article] [PubMed] [Google Scholar]; This study analyzed data from COVIP database of older adults with COVID-19 to assess the impact of frailty, disability, or both on long-term outcomes. The study demonstrated that the overlap of disability and frailty was associated with higher rates of ICU and 3-month mortality.
- 28.*.Beauchamp MK, Joshi D, McMillan J, Erbas Oz U, Griffith LE, Basta NE, et al. Assessment of Functional Mobility After COVID-19 in Adults Aged 50 Years or Older in the Canadian Longitudinal Study on Aging. JAMA Netw Open. 2022;5(1):e2146168. [DOI] [PMC free article] [PubMed] [Google Scholar]; This observational study conducted during the COVID-19 pandemic used data from Canadian Study of Longitudinal Aging to assess the change of mobility and physical function among adults aged 50 years or older who were diagnosed with COVID-19, the majority (94.2%) of whom were not hospitalized. The study showed that even among individuals with mild and moderate COVID-19 there was nearly 2-fold odds of worsening mobility and physical function.
- 29.Welch C, Hassan-Smith ZK, Greig C, et al. Acute Sarcopenia Secondary to Hospitalisation - An Emerging Condition Affecting Older Adults. Aging Dis. 2018;9(1):151–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang YT, Lang JK, Haines KJ, et al. (2022). “Physical Rehabilitation in the ICU: A Systematic Review and Meta-Analysis*.” Critical Care Medicine 50(3): 375–388. [DOI] [PubMed] [Google Scholar]
- 31.*.Martínez-Velilla N, Abizanda P, Gómez-Pavón J, et al. Effect of an Exercise Intervention on Functional Decline in Very Old Patients During Acute Hospitalizations: Results of a Multicenter, Randomized Clinical Trial. JAMA Intern Med. 2022;182(3):345–347. doi: 10.1001/jamainternmed.2021.7654 [DOI] [PMC free article] [PubMed] [Google Scholar]; In this multicenter, randomized controlled trial of an exercise intervention among patients aged 75 and older, the exercise intervention significantly improved the two primary outcomes measured at hospital discharge: the score on the Short Performance Physical Battery (SPPB) and ADLs as measured with the Barthel Index.
- 32.Beil M, Flaatten H, Guidet B, et al. The management of multi-morbidity in elderly patients: Ready yet for precision medicine in intensive care? Crit Care. 2021;25(1):330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. [DOI] [PubMed] [Google Scholar]
- 34.*.McPeake J, Quasim T, Henderson P, et al. Multimorbidity and Its Relationship With Long-Term Outcomes After Critical Care Discharge: A Prospective Cohort Study. Chest. 2021;160(5):1681–92. [DOI] [PMC free article] [PubMed] [Google Scholar]; This cohort study of matched ICU and non-ICU hospitalized patients demonstrated that ICU survivors had higher hospital readmission rates in the year following critical illness. Additionally, multimorbidity was strongly associated with long-term mortality (hazard ratio [HR] 2.17; 95% CI 1.51-3.13) compared to no comorbidities.
- 35.*.Turnbull AJ, Donaghy E, Salisbury L, et al. Polypharmacy and emergency readmission to hospital after critical illness: a population-level cohort study. Br J Anaesth. 2021;126(2):415–22. [DOI] [PMC free article] [PubMed] [Google Scholar]; This longitudinal observational study including all patients admitted to Scotland ICUs from 2011-2013 demonstrated that polypharmacy at ICU admission was independently associated with emergency readmission within a year after discharge.
- 36.*.Blum MR, Sallevelt B, Spinewine A, et al. Optimizing Therapy to Prevent Avoidable Hospital Admissions in Multimorbid Older Adults (OPERAM): cluster randomized controlled trial. BMJ. 2021;374:n1585. [DOI] [PMC free article] [PubMed] [Google Scholar]; This multi-national randomized control trial examined the impact of a structured pharmacotherapy optimization intervention among 2008 adults aged 70 years and older. The intervention was found to result in discontinuation of unneeded drugs but did not reduce the number of drug-related hospitalizations or number of falls compared to standard of care.
- 37.Pandharipande PP, Girard TD, Jackson JC, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kennedy M, Helfand BKI, Gou RY, et al. Delirium in Older Patients With COVID-19 Presenting to the Emergency Department. JAMA Netw Open. 2020;3(11):e2029540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.*.Inouye SK. The Importance of Delirium and Delirium Prevention in Older Adults During Lockdowns. JAMA. 2021;325(17):1779–80. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this editorial, the author explains the interplay of mechanisms that result in a high prevalence of delirium in COVID-19 older adults. The author advocates for the use of screening tools, prevention strategies, and treatment of delirium in hospitalized older adults with COVID-19.
- 40.Wang YY, Yue JR, Xie DM, et al. Effect of the Tailored, Family-Involved Hospital Elder Life Program on Postoperative Delirium and Function in Older Adults: A Randomized Clinical Trial. JAMA Intern Med. 2020;180(1):17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.*.Morandi A, Inzitari M, Udina C, et al. Visual and Hearing Impairment Are Associated With Delirium in Hospitalized Patients: Results of a Multisite Prevalence Study. J Am Med Dir Assoc. 2021;22(6):1162–7 e3. [DOI] [PubMed] [Google Scholar]; This cross-sectional study assessed prevalence of delirium in older adults in multiple health care locations and identified modifiable risk factors associated with delirium. Patients with delirium had a higher incidence of hearing, visual, or bi-sensory impairment.
- 42.*.Wissanji T, Forget MF, Muscedere J, et al. Models of Care in Geriatric Intensive Care-A Scoping Review on the Optimal Structure of Care for Critically Ill Older Adults Admitted in an ICU. Crit Care Explor. 2022;4(4):e0661. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review article summarizes current literature describing or discussing implementation of geriatric-based models of care in critical care settings.
- 43.*.Palakshappa JA, et al. (2021). “Detection of Cognitive Impairment after Critical Illness with the Medicare Annual Wellness Visit: A Cohort Study.” Annals of the American Thoracic Society 18(10): 1702–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]; This retrospective study aimed to understand the rate of detection of cognitive impairment in older adults after one year following critical illness with use of the Medicare Annual Wellness Visit (AWV). The study found that the AWV was not a good enough screening tool for cognitive impairment following critical illness, and there was likely a large proportion of undiagnosed impairment.
- 44.Berkman LF. Assessing the physical health effects of social networks and social support. Annu Rev Public Health. 1984;5:413–32. [DOI] [PubMed] [Google Scholar]
- 45.National Academics of Sciences Engineering and Medicine. Social isolation and loneliness in older adults: opportunities for the health care system. Washington, DC: The National Academic Press; 2020. [PubMed] [Google Scholar]
- 46.Wu B Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Glob Health Res Policy. 2020;5:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.*.Falvey JR, Cohen AB, O’Leary JR, et al. Association of Social Isolation With Disability Burden and 1-Year Mortality Among Older Adults With Critical Illness. Jama Internal Medicine. 2021;181(11):1433–9 [DOI] [PMC free article] [PubMed] [Google Scholar]; This observational study demonstrated the association of social isolation with disability and 1-year mortality among older adults who have survived a critical illness.
- 48.*.Lassen-Greene CL, Nordness M, Kiehl A, et al. Peer Support Group for Intensive Care Unit Survivors: Perceptions on Supportive Recovery in the Era of Social Distancing. Ann Am Thorac Soc. 2021;18(1):177–82. [DOI] [PMC free article] [PubMed] [Google Scholar]; This assessment describes the implementation of a hybrid virtual and in-person peer support group for ICU survivors. The text summarizes the feasibility and value of patient-support groups, even when virtual.
- 49.*.Escalante E, Golden RL, Mason DJ. Social Isolation and Loneliness: Imperatives for Health Care in a Post-COVID World. JAMA. 2021;325(6):520–1. [DOI] [PubMed] [Google Scholar]; This editorial highlights the results of social isolation during the COVID-19 pandemic and addresses social isolation in the context of social determinants of health. Authors advocate that more should be done to address social isolation, including leveraging community level support.
- 50.*.Shukla A, Cudjoe TKM, Lin FR, Reed NS. Functional Hearing Loss and Social Engagement Among Medicare Beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2021;76(1):195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]; This was the first cross-sectional study to show that functional hearing loss is independently associated with limited social engagement in older adults.
- 51.Jones JRA, Berney S, Connolly B, et al. Socioeconomic Position and Health Outcomes Following Critical Illness: A Systematic Review. Crit Care Med. 2019;47(6):e512–e21. [DOI] [PubMed] [Google Scholar]
- 52.*.Jain S, Murphy TE, O’Leary JR, et al. Association Between Socioeconomic Disadvantage and Decline in Function, Cognition, and Mental Health After Critical Illness Among Older Adults A Cohort Study. Annals of Internal Medicine 2022; 175(5): 644–655. [DOI] [PMC free article] [PubMed] [Google Scholar]; This nationally representative study evaluated the association of individual-level socioeconomic status with the three post-ICU syndrome domains (physical function, cognitive function, and mental health) following critical illness. The study showed that socioeconomically disadvantaged individuals are at greater risk for decline in function and cognition after an ICU hospitalization than their more advantaged counterparts.
- 53.Park MS. The effect of socioeconomic status, insurance status, and insurance coverage benefits on mortality in critically ill patients admitted to the intensive care unit. Acute Crit Care. 2022;37(1):118–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.*.Falvey JR, Murphy TE, Leo-Summers L, et al. Neighborhood Socioeconomic Disadvantage and Disability After Critical Illness. Crit Care Med. 2022;50(5):733–41. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated the association between neighborhood socioeconomic disadvantage (measured using the Area Deprivation Index) with post-ICU disability burden over the year after critical illness among older adults.
- 55.*.McGrail K, Morgan J, Siddiqi A. Looking back and moving forward: Addressing health inequities after COVID-19. Lancet Reg Health Am. 2022;9:100232. [DOI] [PMC free article] [PubMed] [Google Scholar]; This editorial emphasizes the need for change given the large inequities in health by income and race that was seen in the COVID-19 pandemic. Authors urge that new policies and research tools are needed to address health inequality and address the unequitable health system at large.
- 56.Lone NI, McPeake J, Stewart NI, et al. Influence of socioeconomic deprivation on interventions and outcomes for patients admitted with COVID-19 to critical care units in Scotland: A national cohort study. Lancet Reg Health Eur. 2021;1:100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.*.Gill TM, Han L, Gahbauer EA, et al. Functional Effects of Intervening Illnesses and Injuries After Critical Illness in Older Persons. Crit Care Med. 2021;49(6):956–66. [DOI] [PMC free article] [PubMed] [Google Scholar]; This observational study examined the impact of intervening illness one year following critical illness among 209 older adults and found that illnesses or injuries leading to hospital readmissions or emergency visits led to adverse functional outcomes. This study suggests that more efforts should be in place to identify and prevent illness and injury after critical illness.
- 58.*.Kalicki AV, Moody KA, Franzosa E, et al. Barriers to telehealth access among homebound older adults. J Am Geriatr Soc. 2021;69(9):2404–11. [DOI] [PMC free article] [PubMed] [Google Scholar]; This large cross-sectional study assessed the barriers of implementing tele-health visits for older adults in a large home-based primary care program. The study found that among 873 older adults, primary barriers included heavy reliance on caregivers to help with technology.
- 59.*.Mao A, Tam L, Xu A, et al. Barriers to Telemedicine Video Visits for Older Adults in Independent Living Facilities: Mixed Methods Cross-sectional Needs Assessment. JMIR Aging. 2022;5(2):e34326. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study used mixed methods including surveys and semi-structured interviews of community-dwelling older adults to understand barriers to tele-medicine. Results showed that barriers included technology difficulties, hearing impairment, language barriers, and lack of desire to see providers virtually.
- 60.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–81. [DOI] [PubMed] [Google Scholar]
- 61.*.Taylor SP, et al. (2022). “Effect of a Multicomponent Sepsis Transition and Recovery Program on Mortality and Readmissions After Sepsis: The Improving Morbidity During Post-Acute Care Transitions for Sepsis Randomized Clinical Trial*.” Critical Care Medicine 50(3): 469–479. [DOI] [PMC free article] [PubMed] [Google Scholar]; This randomized control trial assessed the efficacy of the Sepsis Transition and Recovery program for adults who were recently hospitalized for sepsis. The 30-day multiservice program was found to effective, and patients in the intervention group experienced a lower proportion of either mortality or rehospitalization 30 days after discharge.
- 62.*.Major ME, Dettling-Ihnenfeldt D, Ramaekers SPJ, et al. Feasibility of a home-based interdisciplinary rehabilitation program for patients with Post-Intensive Care Syndrome: the REACH study. Crit Care. 2021;25(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]; This feasibility study aimed to assess the effectiveness of an interdisciplinary rehabilitation program designed for adults with post-intensive care syndrome. The study found that the home-based rehabilitation program was feasible and resulted in positive feedback from patients and health care workers.
- 63.*.Akinyelure OP, Colvin CL, Sterling MR, et al. Frailty, gaps in care coordination, and preventable adverse events. BMC Geriatr. 2022;22(1):476. [DOI] [PMC free article] [PubMed] [Google Scholar]; This cross-sectional study surveyed older adults to assess the correlation between frailty with gaps and coordination and preventable adverse events. The study is the first to find that more frail older adults had higher gaps in care coordination.
- 64.Haines KJ, Denehy L, Skinner EH, et al. Psychosocial outcomes in informal caregivers of the critically ill: a systematic review. Crit Care Med. 2015;43(5):1112–20. [DOI] [PubMed] [Google Scholar]
- 65.*.Sevin CM, Boehm LM, Hibbert E, et al. Optimizing Critical Illness Recovery: Perspectives and Solutions From the Caregivers of ICU Survivors. Crit Care Explor. 2021;3(5):e0420. [DOI] [PMC free article] [PubMed] [Google Scholar]; This qualitative study used content analysis to understand themes related to the unmet needs of caregivers.
- 66.*.Sardella A, Lenzo V, Alibrandi A, et al. A Clinical Bridge between Family Caregivers and Older Adults: The Contribution of Patients’ Frailty and Optimism on Caregiver Burden. Int J Environ Res Public Health. 2021;18(7). [DOI] [PMC free article] [PubMed] [Google Scholar]; This cross-sectional study assessed the impact of older adult frailty on caregiver burnout and found higher degrees of frailty were associated with higher overall burden among caregivers.
- 67.Thurston LM, Milnes SL, Hodgson CL, et al. Defining patient-centered recovery after critical illness - A qualitative study. J Crit Care. 2020;57:84–90 [DOI] [PubMed] [Google Scholar]
- 68.*.Cuijpers ACM, Coolsen MME, Schnabel RM, et al. Self-perceived recovery and quality of life in elderly patients surviving ICU-admission for abdominal sepsis. J Intensive Care Med. 2022;37(7):970–8. [DOI] [PMC free article] [PubMed] [Google Scholar]; This cross-sectional study surveyed older adults admitted to the ICU with abdominal sepsis between one to four years after ICU admission to understand patient perception of quality of life. The study found that despite a majority of patient experiencing loss of function, this did not equate to self-perceived unsatisfactory functioning.


