Abstract
Over two years into the COVID-19 pandemic, it is apparent that some populations across the world are more susceptible than others to SARS-CoV-2 infection and spread. Understanding how populations with varying demographic patterns are impacted by COVID-19 may highlight which factors are most important in targeting to combat global suffering. The first objective of this study was to investigate the association of various socioeconomic status (SES) parameters and confirmed COVID-19 cases in the state of Ohio, USA. This study examines the largest and capital city of Ohio (Columbus) and various small-medium-sized communities. The second objective was to determine the relationship between SES parameters and community-level SARS-CoV-2 concentrations using municipal wastewater samples from each city's respective wastewater treatment plants from August 2020 to January 2021. SES parameters include population size, median income, poverty, race/ethnicity, education, health care access, types of COVID-19 testing sites, and social vulnerability index. Statistical analysis results show that confirmed (normalized and/or non-normalized) COVID-19 cases were negatively associated with White percentage and registered hospitals, and positively associated with registered physicians and various COVID-19 testing sites. Wastewater viral concentrations were negatively associated with poverty, and positively associated with median income, community health centers, and onsite rapid testing locations. Additional analyses conclude that population is a significant factor in determining COVID-19 cases and SARS-CoV-2 wastewater concentrations. Results indicate that community healthcare parameters relate to a negative health outcome (COVID-19) and that demographic parameters can be associated with community-level SARS-CoV-2 wastewater concentrations. As the first study that examines the association between socioeconomic parameters and SARS-CoV-2 wastewater concentrations as well as confirmed COVID-19 cases, it is apparent that social determinants have an impact in determining the health burden of small-medium sized Ohioan cities. This study design and innovative approach are scalable and applicable for endemic and pandemic surveillance across the world.
Keywords: COVID-19, SARS-CoV-2, Social vulnerability index, Race, Healthcare parameters, Wastewater-based epidemiology
Graphical abstract
1. Introduction
By March 11, 2020, the World Health Organization (WHO) had classified the novel coronavirus disease 2019 (COVID-19) as a global pandemic (World Health Organization, 2020). As of January 14, 2022, WHO has reported over 585 million cases globally and 91.3 million cases in the United States alone (World Health Organization, 2022a). While the introduction of vaccinations began in December 2020, there are still large populations who remain vulnerable to SARS-CoV-2, the virus responsible for COVID-19.
Over the last few decades, many epidemiological studies have increasingly emphasized the role of socioeconomic status (SES) in determining health outcomes across the globe (Adler and Stewart, 2010). Communities with lower SES inequalities tend to be more susceptible to health inequalities (Fiscella and Williams, 2004). Amidst the pandemic crisis, it is also apparent that social vulnerability plays a significant role in COVID-19 infection and mortality (Aromí et al., 2021; Karmakar et al., 2021; Magesh et al., 2021; Sandhu et al., 2021; Zhu et al., 2021). Huang et al. (2021), determined that COVID-19 cases and mortality rates were positively associated with social vulnerability in South Carolina counties. This study hypothesized that public health resources were not fully utilized in rural South Carolina counties, which could explain the disproportionate COVID-19 cases in rural counties compared to urban counties. In addition to socioeconomic factors, researchers are also considering that healthcare systems serve as potential social determinants of health, which can affect and be affected by other social predictors of health (Baum et al., 2009; Marmot et al., 2008; O'Donnell et al., 2016). While the majority of studies have focused on country-level and large cities across the world, few studies examine the relationship between demographic parameters and confirmed COVID-19 clinical cases in small and medium-sized cities of the United States. The first objective of this study is to investigate the association of SES (median income, poverty, race/ethnicity [White, Black, Asian], education, access to health care [patient to clinician ratio, registered hospitals, registered physicians, without health insurance, COVID-19 testing sites], and social vulnerability index) on confirmed COVID-19 cases in the state of Ohio, USA.
In Ohio alone, 3,096,557 total cases, 125,230 hospitalizations, and 39,576 deaths have been reported through September 9, 2022 (Ohio Department of Health, 2022b). Franklin County, which includes the capital city (Columbus), represents the highest Ohio county count at 10.87% (336,627) of all Ohio confirmed cases (Ohio Department of Health, 2022b). This study will analyze data from Columbus and several other small-medium-sized Ohio cities varying in socioeconomic status.
In order to track SARS-CoV-2 levels at a community level, wastewater-based surveillance has successfully been used to monitor SARS-CoV-2 load in a given catchment area since majority of the infected (asymptomatic and symptomatic) individuals excrete the virus via their waste (Ahmed et al., 2020; Gonzalez et al., 2020; Hart and Halden, 2020; Lodder and Husman, 2020; Medema et al., 2020; Wurtzer et al., 2020). In central and southeastern Ohio, Ai et al., 2021 reported the significant correlation between SARS-CoV-2 concentrations detected from municipal wastewater and the confirmed COVID-19 cases within the nine Ohio sewersheds. Yet previous studies indicate rural and/or low SES communities are typically underserved by healthcare systems, which can include restricted COVID-19 testing availability and lower physician/hospital ratio per population density (Melvin et al., 2021; Rader et al., 2020). Therefore, this study acknowledges that wastewater-based surveillance is an efficient approach for tracking infectious diseases within communities, regardless of these potential healthcare barriers, and has the potential to serve as a complementary tool for evaluating community socioeconomics (Choi et al., 2020). Hence, the second objective of this study is to determine the association between socioeconomic status parameters and community level SARS-CoV-2 wastewater concentrations using municipal wastewater samples. While the approach and study design used in this study is scalable and applicable anywhere in the world, this study may aid in implementing future prevention strategies prior to the next epidemic.
2. Methods
2.1. Data collection
2.1.1. Clinical COVID-19 cases
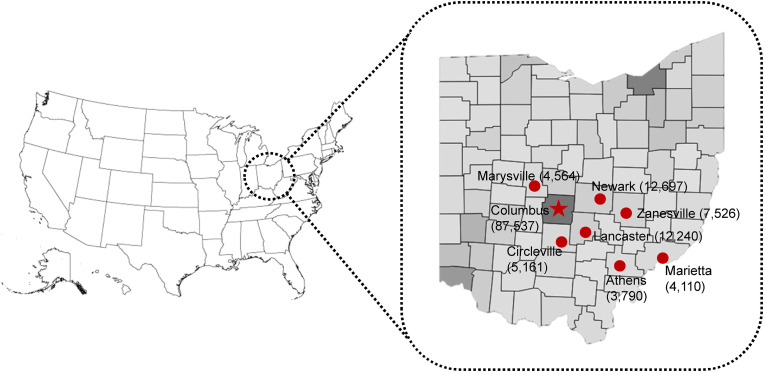
The eight cities (Athens, Circleville, Columbus, Lancaster, Marietta, Marysville, Newark, and Zanesville) covered in this study are located in central and southeastern Ohio (Fig. 1 ). Columbus is located in an urban county, while the remaining 7 cities are located in rural Ohio counties (Ohio State University, 2021). Confirmed COVID-19 case data was retrieved from the Ohio Department of Health Coronavirus Dashboard, Ohio Coronavirus Wastewater Monitoring Network (Ohio Department of Health, 2021a). For all eight cities, data collection includes August 1, 2020 through January 31, 2021. Confirmed COVID-19 case counts are defined as the total number of daily onset cases with residences located within the boundaries of each county's sewershed catchment area. For each city, daily case counts were summated to determine the total cases per month, which were then averaged into one value for each of the 6 months included. These 6 monthly averages were further averaged into one final case value (average monthly cases). The average monthly case value was further divided by each city's respective population and multiplied by 100,000 to calculate the normalized COVID-19 cases per 100,000.
Fig. 1.
Map of the eight city locations investigated in central and southeastern Ohio and cumulative COVID-19 case count. Confirmed COVID-19 case data, wastewater viral concentration data, and socioeconomic population parameters were collected from each of these eight locations. This study focuses on Columbus (star), which is the capital city of Ohio and the largest city in Ohio. The surrounding cities (Athens, Circleville, Lancaster, Marietta, Marysville, Newark, and Zanesville) vary in small-medium population size and socioeconomic status. Cities illustrated via red dot and their respective county borders outlined in light gray. Heat gradient of confirmed COVID-19 cases are shown with cumulative case count in parenthesis from August 1, 2020 through January 31, 2021. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
2.1.2. Socioeconomic parameters
The following socioeconomic status (SES) data were retrieved from the 2019 United States Census Bureau Quick Facts (United States Department of Commerce, 2019) for each of the 8 cities:
-
i.
Total city population and respective county population (July 1, 2019). All persons are “usually resident” in the corresponding city and county boundary.
-
ii.
Median Income (2015–2019). Income within the last 12 months of the householder and all other individuals 15 years and older within the household, regardless of being related.
-
iii.
Poverty (2015–2019). Percentage of city population in poverty is defined by a family's total income being less than the Census Bureau family's threshold, then every individual in the family is considered in poverty. For information on how the Census Bureau Measures Poverty: https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html
-
iv.Ethnicity (2019). Each of the following categories of race is in percentages.
- a. White alone: “A person having origins in any of the original peoples of Europe, the Middle East, or North Africa. It includes people who indicate their race as “White” or report entries such as Irish, German, Italian, Lebanese, Arab, Moroccan, or Caucasian.”
- b. Black or African American alone: “A person having origins in any of the Black racial groups of Africa. It includes people who indicate their race as “Black or African American,” or report entries such as African American, Kenyan, Nigerian, or Haitian.”
- c. Asian alone: “A person having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent including, for example, Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippine Islands, Thailand, and Vietnam. This includes people who reported detailed Asian responses such as: “Asian Indian,” “Chinese,” “Filipino,” “Korean,” “Japanese,” “Vietnamese,” and “Other Asian” or provide other detailed Asian responses.”
-
v.Education (2015–2019). Data are shown in percentages calculated by dividing the number of persons with an education degree (aged 25 and older) by the city population.
- a. High School Degree or Higher: Persons whose highest degree was a high school diploma or its equivalent, people who attended college but did not receive a degree, and people who received an associate's, bachelor's, master's, or professional or doctorate degree.
- b. Bachelor's Degree or Higher: Persons who have received a bachelor's degree from a college or university, or a master's, professional, or doctorate degree.
-
vi.
Without Health Insurance (2015–2019). Percent of the city population, below the age of 65 years, that do not have health insurance.
However, Columbus city boundaries, as denoted by the US Census Bureau, do not represent all populations served by the Jackson Pike and Southerly wastewater treatment plants. Thus, this study utilizes SES parameters from 14 additional districts, served by Jackson Pike or Southerly Wastewater Treatment Plants, to determine collective SES values that are representative of the entire Columbus area (Table 1 ).
Table 1.
Socioeconomic status parameters of 14 city districts that collectively represent Columbus area. These 14 districts are served by the Jackson Pike and/or Southerly wastewater treatment plants which together represent the greater Columbus area. Each individual district's data was retrieved from the 2019 U.S. Census Bureau. For each district, the following SES parameters, median income, poverty, ethnicity (White, Black, Asian), education (high school, bachelor's degree), and without health insurance were totaled to calculate one SES value representative of the greater Columbus area.
| District | Population | Median Income ($) | Poverty (%) | Poverty | White (%) | White | Black (%) | Black | Asian (%) | Asian | High school or higher (%) | High school or higher | BA degree or higher (%) | BA degree or higher | Without health insurance (%) | Without health insurance |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Columbus City | 898,553 | 53,745.00 | 0.20 | 175,217.84 | 0.59 | 526,552.06 | 0.29 | 260,580.37 | 0.06 | 52,116.07 | 0.90 | 806,900.59 | 0.37 | 328,870.40 | 0.10 | 88,058.19 |
| Dublin | 49,037 | 137,867.00 | 0.03 | 1,225.93 | 0.74 | 36,238.34 | 0.02 | 980.74 | 0.20 | 9,611.25 | 0.97 | 47,614.93 | 0.75 | 3,6581.60 | 0.13 | 6,374.81 |
| Hilliard | 36,534 | 96,959.00 | 0.05 | 1,790.17 | 0.87 | 31,711.51 | 0.05 | 1,753.63 | 0.06 | 2,045.90 | 0.96 | 35,109.17 | 0.55 | 1,9984.10 | 0.33 | 12,056.22 |
| Upper Arlington | 35,366 | 123,548.00 | 0.02 | 813.42 | 0.90 | 31,864.77 | 0.00 | 106.10 | 0.07 | 2,440.25 | 0.99 | 34,835.51 | 0.77 | 2,7267.19 | 0.02 | 742.69 |
| Worthington | 14,692 | 104,362.00 | 0.04 | 514.22 | 0.92 | 13,457.87 | 0.03 | 396.68 | 0.03 | 396.68 | 0.99 | 14,471.62 | 0.69 | 10,108.10 | 0.25 | 3,673.00 |
| Westerville | 41,103 | 93,717.00 | 0.07 | 2,671.70 | 0.87 | 35,554.10 | 0.07 | 3,041.62 | 0.02 | 904.27 | 0.97 | 40,034.32 | 0.52 | 21,537.97 | 0.05 | 1,849.64 |
| Gahanna | 35,483 | 88,475.00 | 0.05 | 1,809.63 | 0.81 | 288,83.16 | 0.12 | 4,222.48 | 0.03 | 1,135.46 | 0.97 | 34,347.54 | 0.49 | 17,209.26 | 0.04 | 1,561.25 |
| New Albany | 10,933 | 203,409.00 | 0.01 | 131.20 | 0.80 | 87,35.47 | 0.08 | 896.51 | 0.09 | 929.31 | 0.99 | 10,779.94 | 0.79 | 8,582.41 | 0.06 | 655.98 |
| Reynoldsburg | 38,327 | 67,120.00 | 0.09 | 3,487.76 | 0.63 | 24,184.34 | 0.26 | 9,850.04 | 0.04 | 1,456.43 | 0.92 | 35,375.82 | 0.31 | 12,034.68 | 0.07 | 2,644.56 |
| Whitehall | 18,926 | 42,526.00 | 0.21 | 3,974.46 | 0.44 | 8,289.59 | 0.39 | 7,456.84 | 0.01 | 189.26 | 0.85 | 16,011.40 | 0.15 | 2,744.27 | 0.15 | 2,895.68 |
| Bexley | 13,770 | 109,036.00 | 0.08 | 1,129.14 | 0.87 | 11,911.05 | 0.07 | 963.90 | 0.03 | 399.33 | 0.98 | 13,494.60 | 0.76 | 10,520.28 | 0.03 | 371.79 |
| Obetz Village | 5,196 | 65,466.00 | 0.13 | 680.68 | 0.84 | 4,375.03 | 0.11 | 545.58 | 0.01 | 36.37 | 0.87 | 4,541.30 | 0.14 | 717.05 | 0.08 | 394.90 |
| Grove City | 41,820 | 74,284.00 | 0.07 | 2,969.22 | 0.92 | 38,474.40 | 0.04 | 1,463.70 | 0.02 | 669.12 | 0.94 | 39,478.08 | 0.34 | 14,260.62 | 0.04 | 1,630.98 |
| Grandview Heights | 8,333 | 101,100.00 | 0.21 | 1,733.26 | 0.96 | 80,24.68 | 0.01 | 83.33 | 0.01 | 108.33 | 0.99 | 8,208.01 | 0.74 | 6,133.09 | 0.02 | 174.99 |
| Total | 1,248,073 | 97,258.14 | 1,4153.47 | 80,8256.36 | 29,2341.52 | 72,438.03 | 114,1202.84 | 516,551.00 | 123,084.68 | |||||||
| % of Columbus population | 0.01 | 0.65 | 0.23 | 0.06 | 0.91 | 0.41 | 0.10 |
In addition to the proportion of individuals without health insurance, the following healthcare parameters were utilized: patient-to-clinician ratio, registered hospitals, registered physicians, and COVID-19 testing sites. Patient to Clinician Ratio data were retrieved from Data USA (https://datausa.io/). The 2018 collection year data is based on 2015 County Health Rankings & Roadmaps county levels (https://www.countyhealthrankings.org/). For example, a patient to clinician ratio of 1,000 indicates that primary care physicians saw an average of 1,000 patients per year. The registered number of hospitals and physician data was retrieved from the Ohio Development Services Agency's 2020 County Profiles, prepared by the Office of Research (Ohio Development Services Agency, 2021). Hospital counts include facilities registered as general medical, surgical, or children's hospitals. During the 2020 collection of data, some hospitals were not “registered” and were therefore considered “pending.” Additionally, total number of registered physicians used supplementary data from the State Medical Board of Ohio, 2018) Annual Report (State Medical Board of Ohio, 2018). Registered hospital count and registered physicians count were divided by each county's respective population to determine normalized values.
COVID-19 testing site data was retrieved from the ODH COVID-19 Dashboard (Ohio Department of Health, 2021c). Testing sites consist of 4 types: testing location, community health center, rapid test – at home, and rapid test – onsite. Data includes all testing sites within each county border, but the majority of sites tend to be within city boundaries. Each of the 4 testing sites were summated and normalized using county population data for all 8 counties. For each county, an overall cumulative count of all 4 types of testing sites was summated as “cumulative testing centers” and then normalized. In addition, the 2 largest testing site counts (testing locations and community health centers) were summated and normalized together to create one final COVID-19 testing center parameter, “testing location and community health centers.”
The social vulnerability index (SVI) data retrieved from the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry (Agency For Toxic Substances and Disease Registry, 2021), ranks the social vulnerability of each county in Ohio. The SVI utilizes 15 social factors that may weaken a county's preparation and response to a hazardous event, natural disaster, and/or disease outbreak, such as COVID-19. The SVI ranks each of the individual 15 social factors and categorizes them into 4 related themes (Socioeconomic Status, Household Composition and Disability, Minority Status and Language, Housing Type and Transportation) and one Overall Vulnerability summary rank. Percentile rankings range from 0 to 1, with a higher value indicating higher social vulnerability and a lower value indicating low social vulnerability. For this study, the SVI rankings of the 4 themes and Overall Vulnerability were utilized.
2.1.3. Wastewater SARS-CoV-2 concentrations
All wastewater viral concentration data was recovered from the Lee Lab in the College of Public Health at The Ohio State University. Details on the cities' wastewater treatment plants can be seen in Ai et al., 2021's study. Timeline follows August 1, 2020 to January 21, 2021. Data from August 1, 2020, through the first week of January 2021 is a subset of data from Ai et al. (2021), with the addition of new data for the second and third week of January 2021. Influent wastewater composite samples were collected twice a week from each of the cities' wastewater treatment plant (Athens, Circleville, Columbus, Lancaster, Marietta, Marysville, Newark, and Zanesville). From Columbus, samples were collected from the two wastewater treatment plants, Jackson Pike and Southerly. Wastewater samples were transported to the lab where sample processing, filtration, viral concentration, and SARS-CoV-2 RNA extraction occurred.
As demonstrated in Ai et al. (2021), raw wastewater was centrifuged at 4 °C, 2,500×g for 10 min, and further filtered via 0.45 μM sterile filter units to remove large solid particles. Next, Hollow Fiber Polysulfone Concentrating Pipette Select tips (0.05 μm) concentrated the filtrate, producing the viral eluent concentrate. Nucleic acid extraction and reverse transcription were conducted to produce cDNA, which was further used for SARS-COV-2 gene quantification via droplet digital polymerase chain reaction (ddPCR) to target the SARS-CoV-2 nucleocapsid gene (N1 and N2) and envelope (E) gene. Genetic signaling allowed the quantification of wastewater viral load concentrations in gene copies per liter (GC/L). Positive and negative control assays for each of the three target genes were conducted and referenced when setting an appropriate threshold for quantifying positive droplets (Ai et al., 2021). In addition, regular testings of PCR inhibition, virus recovery efficiency, and human fecal viral indicators were performed.
Monthly averages of wastewater concentrations (GC/L) were calculated for each WWTP, which were then calculated into one total averaged value representative of all months (August 2021 through January 2021). This final wastewater concentration value (GC/L) of each WWTP was used for determining potential associations with SES parameters.
2.2. Statistical analysis
2.2.1. Univariate data analysis
Descriptive statistics suggested that COVID-19 case, SES parameter, and wastewater viral concentration data failed to meet normality assumptions. Therefore, the two non-parametric regression analyses utilized were the Spearman Rank Correlation and Kendall Rank Correlation to determine the individual association between each socioeconomic parameter and COVID-19 cases, and the association between each socioeconomic parameters and wastewater viral concentrations. Alpha levels of 0.05 and 0.10 were used to determine relative strong and weak significance.
Along with the statistical methods listed above, multiple linear regression was implemented to estimate the relationship between multiple independent variables and a single dependent variable. The independent variables of interest were city population, Social Vulnerability Index (SVI) Theme 3, median income, and White, while the dependent variables of interest were averaged monthly COVID-19 cases, N1, N2, and E gene SARS-CoV-2 wastewater concentrations. These independent variables were selected due to their linear relationships with the dependent variables. Specifically, SVI Theme 3 was chosen because including all races (White, Asian, Black) as predictors in the MLR model was desired, but was not possible due to collinearity. SVI Theme 3 represents all non-white and non-English speaking individuals. Independent variables were checked for multicollinearity using the variance inflation factor. Two models were made for each dependent variable of interest. One model utilized city population, SVI Theme 3, and median income as predictors, while the second used White, SVI Theme 3, and median income as the predictors. Data collection, organization, average calculations, and normalizations were performed with Microsoft Excel (V. 16.49 [21050901]). All statistical analyses were performed using RStudio software (V March 1, 1093). Variable abbreviations used for statistical analyses and respective figure generation can be found in Table 3.
Table 3.
Variable abbreviation of all socioeconomic parameters, confirmed COVID-19 cases, and SARS-CoV-2 wastewater concentrations.
| Abbreviation | Parameter |
|---|---|
| Location | Location |
| County | County |
| RvU | Rural vs. Urban |
| Population 1 | City Population |
| Population 2 | County Population |
| N1 | N1 conc. (GC/L) |
| N2 | N2 conc. (GC/L) |
| E | E conc. (GC/L) |
| COVID.19 | Averaged Monthly COVID-19 Cases (by WWTP) |
| NormCOVID | Normalized COVID-19 Cases Per 100,000 (by WWTP) |
| Income | Med. Income ($) |
| Poverty | Poverty (%) |
| White | White (%) |
| Black | Black (%) |
| Asian | Asian (%) |
| Education 1 | High school or higher (%) |
| Education 2 | BA degree or higher (%) |
| PCR | Patient to clinician ratio (population: 1 clinican) |
| WHI | Without health insurance (%) |
| Hospitals 1 | Registered Hospitals Count (by County) |
| Hospitals 2 | Registered Hospitals per pop. |
| Physicians 1 | Registered Physicians Count (by County) |
| Physicians 2 | Registered Physicians per pop. |
| CTC1 | Cumulative Testing Centers (by county) |
| CTC2 | Cumultaive Testing Centers per population |
| TL1 | Testing Locations Count |
| TL2 | Testing Locations per population |
| CHC1 | Community Health Centers Count |
| CHC2 | Community Health Centers per poppulation |
| RHT1 | Rapid Test - At Home Count |
| RHT2 | Rapid Test - At Home Tests per population |
| ROT1 | Rapid Test - Onsite Count |
| ROT2 | Rapid Test - Onsite Testing per population |
| TL.CHC1 | Testing Locations & Community Health Centers Count |
| TL.CHC2 | Testing Locations & Community Health Centers per population |
| Themes | Overall - RPL_THEMES |
| Theme 1 | Socioeconomic Status- RPL_THEME1 |
| Theme 2 | Household Composition & Disability - RPL_THEME2 |
| Theme 3 | Minority Status & Language - RPL_THEME3 |
| Theme 4 | Housing Type & Transportation - RPL_THEME4 |
2.2.2. Multivariate data analysis
Following the methods listed above, a multivariate data analysis technique was utilized to better analyze relationships and patterns within the dataset. The appropriate approach implemented for this study was Principal Component Analysis (PCA). This method was selected because it is useful for simplifying high-dimensional data, while retaining the patterns within the data. To prepare the data for PCA, categorical variables and normalized value columns were removed. The data was then standardized so that all variables had a variance and standard deviation of 1. After the data were prepared, PCA was applied, and principal components were determined.
3. Results
3.1. Confirmed COVID-19 cases
Averaged monthly COVID-19 cases and normalized COVID-19 cases per 100,000 are found in Table 2 . It should be noted that Columbus (the largest population) has the highest average monthly cases, but not the highest normalized cases. Zanesville has the 5th smallest population with the highest normalized case value, +1095.25 higher than Columbus. Meanwhile, Circleville has the lowest normalized COVID-19 cases (−158.75).
Table 2.
Confirmed cumulative COVID-19 monthly cases, averaged monthly cases, and normalized cases in each of the 8 city locations. Table is ranked by population size in descending order, with Columbus having the largest population. Confirmed COVID-19 case counts were totaled for each month within the boundary of each county's sewershed catchment area. Data includes August 1, 2020 to January 31, 2021 for all 8 cities. For each location, the individual monthly cumulative cases were averaged into one value. These averaged monthly cases were normalized per 100,000 population. Each city's normalized COVID-19 cases were compared to Columbus, the city with the highest normalized cases, to determine the difference in normalized cases.
| Location | City Population | Total Cumulative Monthly Cases |
Averaged Monthly Cases | Normalized Cases Per 100,000 | Normalized Difference vs. Columbus | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| August ‘20 | September | October | November | December | January ‘21 | |||||
| Columbus | 1,248,073 | 5,008 | 5,037 | 8,017 | 24,547 | 25,798 | 18,099 | 14,417.67 | 1,155.19 | 0.00 |
| Newark | 50,315 | 99 | 82 | 333 | 1,015 | 969 | 764 | 543.67 | 1,080.53 | −74.67 |
| Lancaster | 40,505 | 128 | 115 | 330 | 858 | 846 | 739 | 502.67 | 1,241.00 | 85.80 |
| Zanesville | 25,158 | 60 | 147 | 305 | 857 | 1138 | 890 | 566.17 | 2,250.44 | 1,095.25 |
| Marysville | 24,667 | 74 | 136 | 237 | 872 | 693 | 506 | 419.67 | 1,701.33 | 546.13 |
| Athens | 24,536 | 42 | 364 | 422 | 248 | 196 | 381 | 275.50 | 1,122.84 | −32.35 |
| Circleville | 14,050 | 14 | 14 | 69 | 201 | 235 | 307 | 140.00 | 996.44 | −158.75 |
| Marietta | 13,356 | 9 | 5 | 113 | 311 | 306 | 220 | 160.67 | 1,202.95 | 47.76 |
3.2. Univariate data
3.2.1. SES parameters and confirmed COVID-19 cases
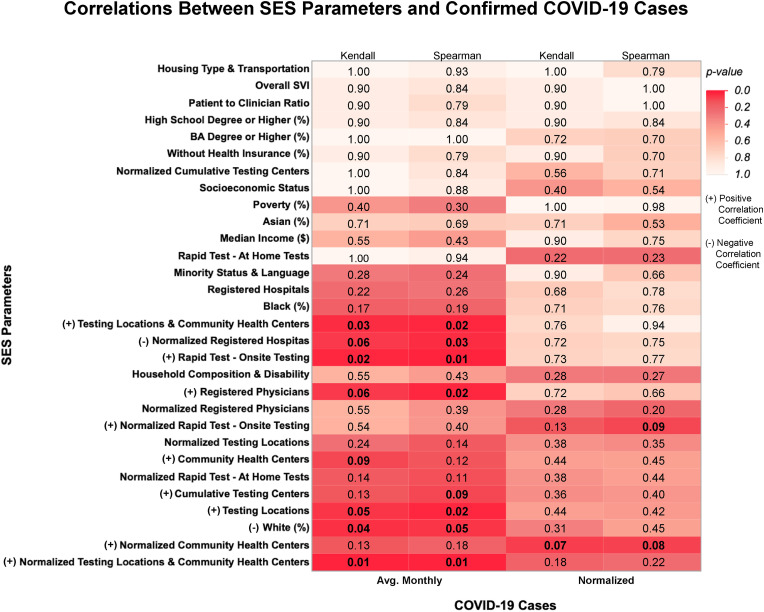
The two correlation analyses, Spearman's Rho (r S) and/or Kendall's Tau (r K) rank correlation, have determined that a total of nine socioeconomic parameters are significantly associated with averaged monthly COVID-19 cases: percent White (r s = −0.71, p = 0.05; r k = −0.59, p = 0.04) normalized registered hospitals (r s = −0.79, p = 0.03; r k = −0.57, p = 0.06), registered physicians (r s = 0.81, p = 0.02; r k = 0.57, p = 0.06), cumulative testing centers (r s = 0.68, p = 0.09), testing locations (r s = 0.82, p = 0.02; r k = 0.65, p = 0.05), community health centers (r k = 0.55, p = 0.09), rapid test – onsite (r s = 0.90, p = 0.01; r k = 0.82, p = 0.02), testing locations and community health centers (r s = 0.83, p = 0.02; r k = 0.68, p = 0.03), and normalized testing locations and community health centers (r s = 0.86, p = 0.01; r k = 0.71, p = 0.01) (Fig. 2 ). Meanwhile, two SES parameters, normalized community health centers (r s = 0.70, p = 0.08; r k = 0.59, p = 0.07) and normalized rapid test – onsite (r s = 0.68, p = 0.09), were found to be positively associated with normalized COVID-19 cases. The remaining population demographics (poverty, median income, education) were not associated with normalized or non-normalized COVID-19 cases. All p-values and correlation coefficients can be found in Supplemental Table 2.
Fig. 2.
Summary of correlations between socioeconomic status parameters and confirmed COVID-19 cases within the 8 city locations. Heat table represents associations between all eight cities' socioeconomic status parameters and (normalized and monthly averaged) COVID-19 cases from August 1, 2020 to January 31, 2021. For each location, the individual monthly cumulative cases were averaged into one value. These averaged monthly cases were normalized per 100,000 population. Spearman and Kendall correlation analyses were performed for each comparison to indicate respective p-values. SES parameters with a significant COVID-19 association (p-values less than or equal to 0.05 and/or 0.10) are denoted with a positive or negative correlation coefficient in parenthesis and exact pvalues are emphasized within table in bold. A positive coefficient value indicates a positive association while a negative coefficient indicates a negative association.
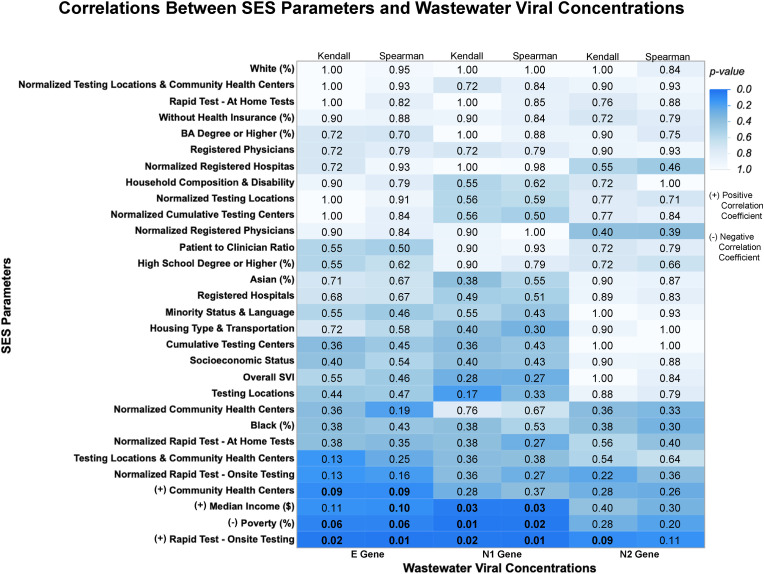
3.2.2. SES parameters and wastewater viral concentrations
The two correlation analyses (Spearman and Kendall) have determined that a total of four socioeconomic parameters are significantly (p < 0.05 and/or p < 0.10) associated with the wastewater SARS-CoV-2 gene concentrations (Fig. 3 ). Those SES parameters are median income, poverty, community health centers, and rapid test – onsite. Median income was found to be positively associated with targeted N1 (r S = 0.79, p = 0.03; r K = 0.64, p = 0.03) and E (r S = 0.64, p = 0.10) gene wastewater viral concentrations. Poverty is negatively associated with targeted N1 (r S = −0.83, p = 0.02; r K = −0.71, p = 0.01) and E (r S = −0.71, p = 0.06; r K = −0.57, p = 0.06) gene wastewater viral concentrations.
Fig. 3.
Summary of correlations between socioeconomic status parameters and wastewater viral concentrations within the 8 city locations. Heat table represents associations between all eight cities' socioeconomic parameters and municipal wastewater E, N1, and N2 gene concentrations from August 1, 2020 to January 21, 2021. All wastewater concentrations in gene copies per liter (GC/L). Spearman and Kendall correlation analyses were performed for each comparison to indicate respective p-values. SES parameters with a significant wastewater concentration association (p-values less than or equal to 0.05 and/or 0.10) are denoted with a positive or negative correlation coefficient in parenthesis and exact p-values are emphasized within table in bold. A positive coefficient value indicates a positive association while a negative coefficient indicates a negative association.
Additionally, community health centers were found to be positively associated with targeted E gene wastewater viral concentrations (r S = 0.69, p = 0.09; r K = 0.55, p = 0.09), while rapid test – onsite is positively associated with targeted N1 (r S = 0.90, p = 0.01; r K = 0.82, p = 0.02) and E (r S = 0.90, p = 0.01; r K = 0.82, p = 0.02) gene wastewater viral concentrations. All remaining p-values and correlation coefficients can be found in Supplemental Table 3.
This study also reveals that out of the three SARS-CoV-2 genetic targets, the E gene is found to have more associations with SES parameters compared to the N1 and N2 gene (Fig. 3). Collective descriptive statistics of SES parameters, confirmed COVID-19 cases, and SARS-CoV-2 wastewater concentrations can be found in Supplemental Table 1.
3.2.3. Multiple linear regression
To estimate the influence of combined effects by median income, city population, White, and SVI Theme 3 on COVID-19 cases and wastewater viral concentrations, multiple linear regression (MLR) was performed. Table 4 summarizes the models of best fit. The adjusted R2 coefficients were significant for all models with p < 0.05. When the city population was replaced by White as a prediction variable, adjusted R2 values decreased in all models, suggesting that population was better for predicting COVID-19 cases and wastewater viral concentrations. Supplemental Figure 1 also supports this claim and provides a visual. Out of all eight models, MLR Model 1 showed the best fit, with an adjusted R2 of 0.99 and a p < 0.001. Overall, MLR showed that the dataset contains many linear relationships, and that an MLR model using city population, median income, and SVI Theme 3 as predictors of COVID-19 cases and wastewater viral concentrations provides the best fit.
Table 4.
Summary results of various multiple linear regression models for predicting averaged monthly COVID-19 cases and SARS-CoV-2 wastewater concentrations within the 8 city locations. Predictor variables denoted with one asterisk (*) indicate a p-value < 0.05, two asterisk (**) indicate a p-value < 0.001, and three asterisk (***) indicate a p-value < 0.0001.
| Outcome | Predictors | Model | R2 | Adjusted R2 | p-value |
|---|---|---|---|---|---|
| COVID-19 cases | City Population***, Income, Theme 3 | Multiple Linear Regression 1 | 1.00 | 0.99 | 0.0004 |
| COVID-19 cases | White*, Income **, Theme 3 | Multiple Linear Regression 2 | 0.94 | 0.89 | 0.0228 |
| N1 conc. | City Population**, Income, Theme 3 | Multiple Linear Regression 3 | 0.96 | 0.92 | 0.0132 |
| N1 conc. | White*, Income, Theme 3 | Multiple Linear Regression 4 | 0.93 | 0.86 | 0.0309 |
| N2 conc. | City Population**, Income, Theme 3 | Multiple Linear Regression 5 | 0.96 | 0.93 | 0.0119 |
| N2 conc. | White, Income, Theme 3 | Multiple Linear Regression 6 | 0.91 | 0.82 | 0.0450 |
| E conc. | City Population*, Income, Theme 3 | Multiple Linear Regression 7 | 0.95 | 0.90 | 0.0176 |
| E conc. | White, Income, Theme 3 | Multiple Linear Regression 8 | 0.92 | 0.85 | 0.0348 |
3.3. Multivariate data
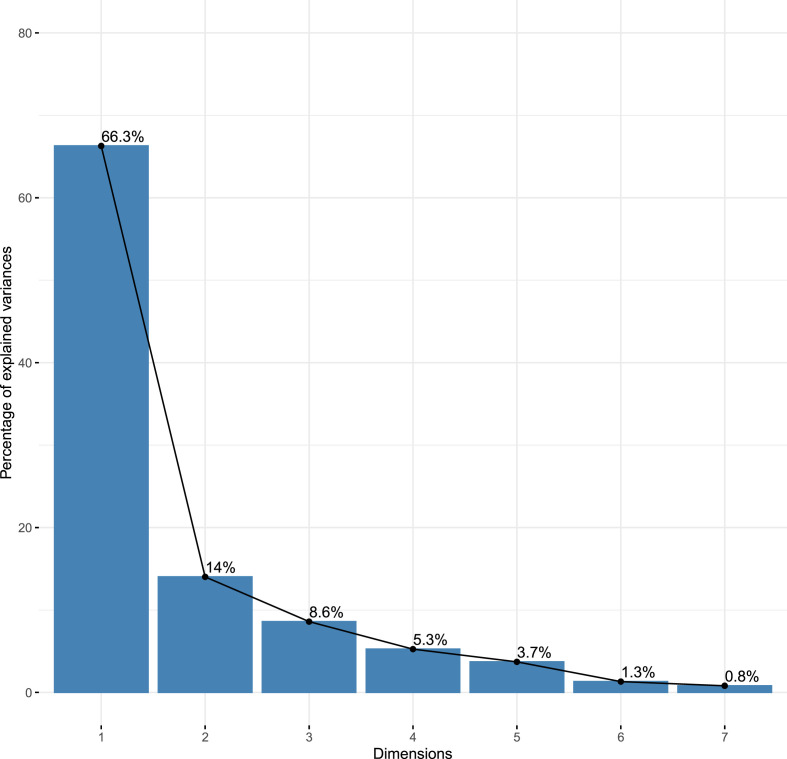
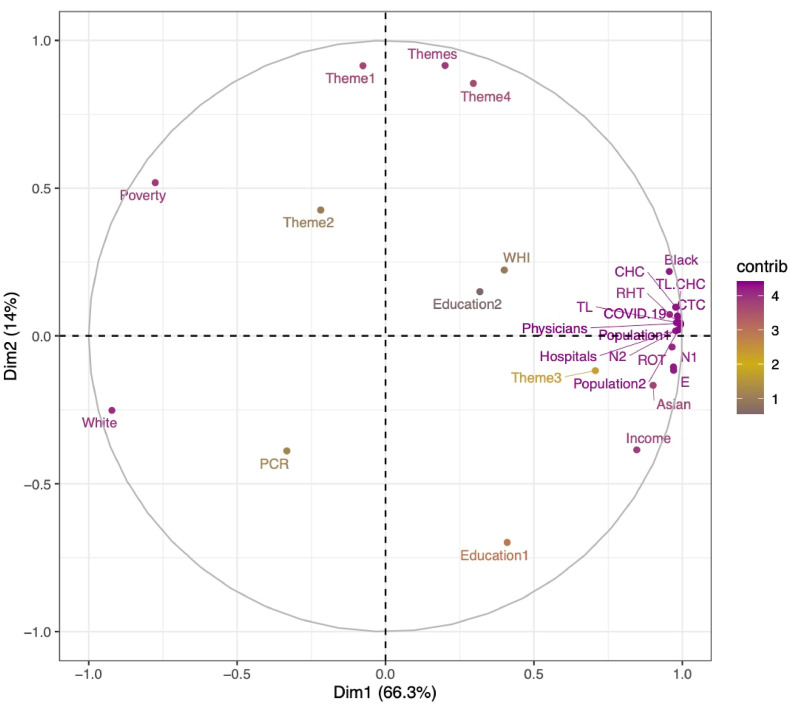
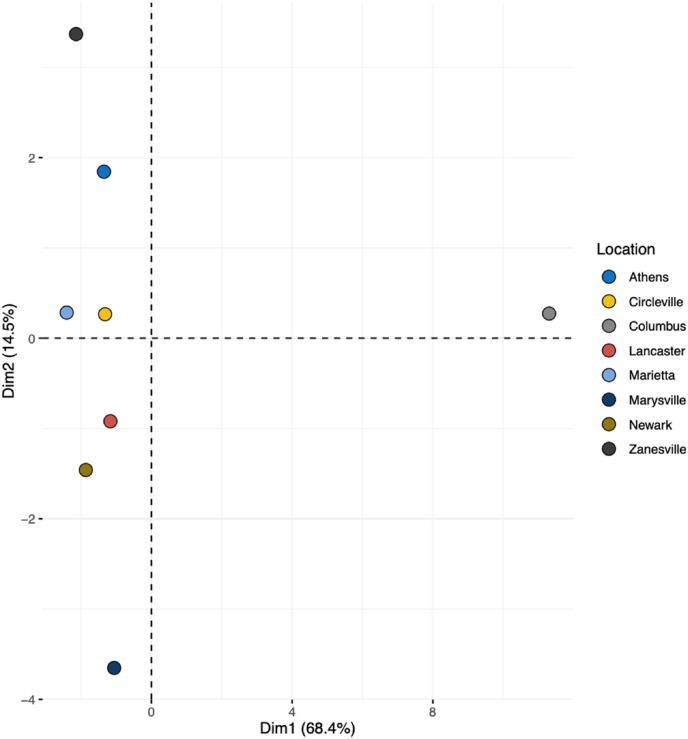
PCA results showed that principal component 1 (PC1) and 2 (PC2) accounted for 66.3% and 14% of the variance within the data set, respectively (Fig. 4 ). This means that the first two components alone account for 80.3% of the variance within the data set. Since the first two PCs account for such a large amount of variance in the data set, a 2-D PCA plot displaying all predictors was created to visualize the data (Fig. 5 ). The compact cluster of points on the right side of the graph is thought to correspond to the location Columbus, while the sparser points on the left side of the graph correspond to the other seven locations. To visualize this, a PCA plot was generated for all eight sampling locations (Fig. 6 ), illustrating that PC1 clearly separates Columbus from all other sampling locations. To examine this further, the contributions of the individuals for PC1 were viewed, and it was seen that Columbus contributes 86.4% to PC1.
Fig. 4.
Scree plot indicating the percentage of variances explained by principal components. Principal component 1 and principal component 2 account for 80.3% of the variance within all variables.
Fig. 5.
PCA plot displaying socioeconomic status parameters, confirmed COVID-19 cases, and wastewater viral concentrations within the 8 city locations. Refer to Table 3 for variable abbreviation.
Fig. 6.
2D PCA plot results for all 8 city locations. Plot indicates that principal component 1 clearly separates Columbus from other 7 sampling locations.
4. Discussion
The proportion of White residents, registered hospitals, registered physicians, and various testing sites are potentially related to COVID-19 cases in central and southeastern Ohio. The combined SES parameter, normalized testing locations and community health centers, and rapid test – onsite showed the highest Spearman rank correlation, r S = 0.86 and r S = 0.90. From these results, it is clear that an increase in COVID-19 testing sites (cumulative testing centers, testing locations, community health care centers, rapid test – onsite, testing locations and community health centers, and normalized testing locations and community health centers) are significantly associated with an increase in averaged monthly COVID-19 confirmed cases. Most notably, results indicate that two healthcare parameters (normalized registered hospitals and registered physicians) and various COVID-19 testing parameters are found to be associated with averaged monthly COVID-19 confirmed cases. All significant correlation coefficients between SES parameters and COVID-19 cases are positive, with the exception of normalized registered hospitals (r S = −0.79; r K = −0.57). This reveals a key finding, as the number of registered hospitals decreases in these small-medium-sized cities, respective to population size, confirmed COVID-19 cases are expected to increase. In cities with disproportionate access to hospitals, individuals may face greater barriers when receiving healthcare, including distance to travel, hospital bed availability, and quality of care. Considering Columbus has the highest median income and second highest normalized registered hospitals (data not shown), median income and hospital access could certainly be related. This discovery aligns with previous literature that low-income areas compared to high-income areas face substantial healthcare disparities and need to travel further distance for general acute hospital care (Nguyen et al., 2019).
In addition, results determined that COVID-19 cases increase in cities with an increasing proportions of White individuals. This result is unexpected since past evidence suggests that racial and ethnic minority groups typically face higher COVID-19 burdens, hospitalizations, and deaths (Abedi et al., 2021; Kim and Bostwick, 2020; Wrigley-Field et al., 2020). Interestingly, recent studies have begun to note changing perceptions about the COVID-19 pandemic and how they could be distinguished by racial/ethnic groups, while White individuals in the United States were more likely to disregard COVID-19 safety precautions compared to ethnic minorities (Harell and Lieberman, 2021; Kumar and Encinosa, 2021; Skinner-Dorkenoo et al., 2022). Though this study only investigated COVID-19 case incidence, it is possible that the proportion of Whites could test positive at higher rates compared to ethnic minorities, but Whites could face lower mortality rates compared to other ethnic minorities. Therefore, if plausible, future studies should ensure that COVID-19 incidence, hospitalization, mortality, and vaccination rates are investigated to fully cover the burden of the disease.
Although only two SES parameters are associated with normalized COVID-19 cases, this may represent a key finding. Various studies around the world have utilized either normalized or non-normalized COVID-19 case data to assess the relationship with SARS-CoV-2 wastewater concentration data. It is apparent that studies using non-normalized confirmed clinical COVID-19 cases tend to use raw daily, total, and/or moving weekly averages case counts across shorter study periods to more accurately detect significant changes in wastewater loads and COVID-19 cases (Hasan et al., 2021; Kumar et al., 2020; Srivastava et al., 2021). On the other hand, studies using normalized COVID-19 case data tend to monitor wastewater influent across longer time periods with a greater likelihood of employing other methods to normalize SARS-CoV-2 wastewater concentrations, such as human fecal viruses, crAssphage, and pepper mild mottle virus (PMMoV) Ai et al. (2021); Graham et al. (2021); Feng et al. (2021). While there is no universal agreement on to use of normalized or non-normalized COVID-19 data, this study explored the association of both COVID-19 data with socioeconomic parameters. Overall, non-normalized COVID-19 case counts were found to have more associations with SES parameters compared to normalized COVID-19 cases per 100,000.
Results reveal a negative relationship between poverty (%) and N1 and E gene wastewater viral concentrations, but a positive relationship between median income and N1 and E gene wastewater viral concentrations. This is an interesting discovery since univariate Spearman and Kendall correlations did not reveal an association between poverty and median income with confirmed clinical COVID-19 cases. Therefore, this reflects a key finding of this novel study, indicating the potential for using SES parameters as a tool for determining community wastewater infection. In addition, the direction of association between these SARS-CoV-2 wastewater concentrations with poverty and median income is also unique and unexpected. Nonetheless, there could be possible reasoning behind the relationship of SARS-CoV-2 target gene wastewater concentrations decreasing while poverty increases and median income decreases. It is acknowledged that septic tanks are not accounted for in this study since all the wastewater samples were obtained from wastewater treatment plants’ influents. Septic tank proportion should be considered a potential factor in the future. According to the USEPA, more than one in five households in the US utilize a septic system to treat small volumes of household and business wastewater, which tend to be in rural and suburban locations (USEPA, 2021). Septic systems require considerable amounts of land space for a functioning drainage field, depending on sewer volume and soil conditions. Thus, it may be more plausible for less populated, rural cities to have higher proportions of septic tanks compared to densely populated urban cities. In addition, there is a weak, negative association between city population size and poverty (Supplemental Table 5). In addition, typically, individuals within higher-income communities have more resources and spare income, allowing for increased travel, which may increase community viral infection and spread. For example, a recent study concluded that high-income communities tend to have higher rates of participation in daily activities compared to low-income communities (Hickman et al., 2017). Collectively, these factors may explain the relationship between cities with lower poverty and higher median income rates having increased wastewater viral concentrations. Future studies should aim to include septic systems as a potential influencer when exploring the association between SES and parameters and community level SARS-CoV-2 wastewater viral concentrations.
In addition, the SARS-CoV-2 target E gene was found to have more associations with SES parameters compared to the N1 and N2 targets genes. This is a unique and unexpected finding since a majority of recent SARS-CoV-2 wastewater studies primarily target the N1 and/or N2 regions of the SARS-CoV-2 nucleocapsid N gene to compare against COVID-19 cases (Feng et al., 2021; Graham et al., 2021; Rodríguez Rasero et al., 2022; Weidhaas et al., 2021; Wu et al., 2022; Yeager et al., 2021). In fact, a recent review summarized 92 studies across 34 countries that employed wastewater surveillance for COVID-19 community surveillance and concluded that the N gene was the most targeted (Shah et al., 2022). The previous Ai et al. (2021), a study that quantified SARS-CoV-2 gene concentration in the same nine Ohio sewersheds found that wastewater concentrations had the highest correlation and prediction of new confirmed COVID-19 cases with the N2 gene target. Therefore, future approaches should note this key finding and prioritize utilizing the E gene as a measure of SARS-CoV-2 wastewater concentrations, especially when comparing viral gene target concentrations to community demographic parameters. Most notably, this is the first and only study known to examine the strength and direction of association between community socioeconomic parameters and SARS-CoV-2 wastewater viral concentrations. Overall, these conclusions illustrate that wastewater-based monitoring has the potential to serve as a complementary tool for evaluating community socioeconomics and can be used for supplemental information when combating health burdens in communities served by wastewater treatment plants.
As expected, multiple linear regression (MLR) models further confirm our results. MLR models that included city population provided better fits than models that did not include population for both COVID-19 cases and SARS-CoV-2 wastewater concentrations, which was further supported through the PCA results. Notably, out of the four and overall CDC Social Vulnerability Themes, Minority Status and Language (Theme 3) correlated best with both COVID-19 cases and all SARS-CoV-2 wastewater concentrations (Table 4; Supplemental Figure 2). In other words, SVI Theme 3 accounts for the total percentile percentage of the minority population and individuals of non-proficient English speakers. This finding matches previous results and literature that race/ethnicity plays a key role in determining COVID-19 burden (Figueroa et al., 2021; Mude et al., 2021) and SARS-CoV-2 wastewater concentrations.
Meanwhile, the principal component analysis (PCA) has confirmed our univariate conclusions and revealed additional vital findings. As seen in Fig. 5, the following variables account for 80.3% of variability within the data set: median income, poverty, education, population, Asian, hospitals, SVI Theme 1, SVI Theme 2, SVI Theme 3, and all SARS-CoV-2 wastewater concentrations (N1, N2, E). This also displays a compact cluster of variables overlapping one another in quadrant 1 and 4. Note that the majority of these variables are the healthcare parameters (numerous types of COVID-19 testing sites, hospitals, physicians, and COVID-19 cases), meaning that all of these variables are very similar with little variance. Most notably, this key finding denotes that future research can save study time and resources by only selecting one or two healthcare parameters of interest. In addition, Fig. 6 visually conveys a definitive separation between Columbus (the capital, metropolitan city) and the other 7 cities, which may be explained by the city type (rural vs. urban) and respective population size. In Fig. 6, it is also important to note that the 7 cities are relatively spread out and do not cluster, meaning there are other variables causing this diversity within these cities. As a result, potential significant drivers for COVID-19 cases and SARS-CoV-2 wastewater concentrations could be more complex for cities with similar population sizes. These results confirm that city type (e.g. size, demographic composition) is a major delineator for determining both COVID-19 cases and SARS-CoV-2 community wastewater concentrations. Future research should utilize these key findings and either select city locations with a relatively balanced mix of rural and urban cities or select just one city type. For example, expanding our study design to encompass all rural cities within the state of Ohio monitored via SARS-CoV-2 wastewater surveillance may aid in further understanding the complex burden of disease in small-medium-sized communities.
5. Limitations
It is apparent that the sample set of this study is relatively small, focusing on 8 cities in 8 Ohio counties. This small data set (n = 8 counties) failed to meet normality assumptions, limiting the options for conducting further analyses beyond Spearman and Kendall Rank Correlation, Principal Component Analysis, and Multiple Linear Regression. Nonetheless, this pilot study's primary goal was accomplished by determining the preliminary strength and direction of association between each community's SES parameter with COVID-19 cases and SARS-CoV-2 wastewater concentrations.
To compare preliminary differences in a small and large data set, additional regression analyses were performed to determine any association between the social vulnerability index (SVI) and COVID-19 cases of all 88 Ohio counties. Overall SVI, in addition to all four SVI themes (Socioeconomic Status, Household Composition & Disability, Minority Status & language, and Housing Type & Transportation), were significantly (p < 0.005) associated with confirmed COVID-19 cases (Supplemental Table 4). Based on these results with a larger data set of statewide counties (n = 88), the CDC's SVI serves as a potential indicator of COVID-19 case incidence. Nonetheless, this pilot study should be used for future studies encompassing a more comprehensive range of cities and respective data. Since the use of SARS-CoV-2 wastewater monitoring is increasing worldwide, this also increases the potential of future study sites. Sample collection can expand to the entire state and/or regional areas to determine potential socioeconomic associations with SARS-CoV-2 wastewater concentrations and COVID-19 case incidence. However, in cities without pre-existing SARS-CoV-2 wastewater surveillance, this approach can easily be replicated to investigate the relationship between socioeconomic parameters and COVID-19 cases.
Another limitation exists within the confirmed COVID-19 case data posted at the state department. Studies have reported that in some areas in the United States, there is likely higher SARS-CoV-2 infection than those represented in confirmed case counts (Bendavid et al., 2021; Havers et al., 2020). This underreporting can be due to various factors such as variations in testing methods, laboratory capacity, access to healthcare settings, and individuals with mild symptoms who recover on their own without seeking medical care (Reese et al., 2021).
While the advantages of wastewater-based epidemiology (WBE) were previously presented, the limitations of wastewater surveillance are also apparent. WBE does not account for communities not served by sewer systems, including private septic systems or those lacking basic sanitation services. For example, it is estimated that 1.7 billion people worldwide lack access to safe disposal of human waste, and 494 million individuals practice open defecation (World Health Organization, 2022b; World Health Organization and UNICEF, 2021). A recent 2021 study determined that the majority (>75%) of North America, Europe, and Australia are connected to wastewater collection systems, while Africa has the largest proportion of communities not connected to any collection systems (Jones et al., 2021). Therefore, other regions of the world, such as Africa, will require other methods of COVID-19 surveillance. In addition, more research is needed to understand SARS-CoV-2 wastewater surveillance since the detection and quantification approaches are not standardized across the globe with communities served by sewer systems (Farkas et al., 2020). For example, limits of detection vary by gene target and lower levels of community infection may not be captured by gene detection.
6. Conclusion
To our knowledge, this is the first study that investigates the associations between SES parameters and community-level SARS-CoV-2 wastewater concentrations. This study has demonstrated that multiple healthcare parameters (number of hospitals, physicians, and COVID-19 testing sites) are associated with confirmed COVID-19 cases within 8 central and southeastern Ohioan cities. SARS-CoV-2 wastewater concentrations were also associated with two SES parameters, median income, and poverty (%), in addition to two COVID-19 testing sites. In addition, it was found that population is a significant factor in determining COVID-19 cases and SARS-CoV-2 wastewater concentrations. Based on these results, it is apparent that social determinants have an impact in evaluating the health burden of Ohioan cities. This study demonstrates the need for an expanded collection of SES parameters across the US, while emphasizing that small-town cities should not be forgotten during a public health crisis. Therefore, by determining additional sociodemographic parameters associated with COVID-19 cases and SARS-CoV-2 wastewater monitoring concentrations, necessary interventions may be implemented to target specific, vulnerable communities in need of combating present and future health burdens. Additionally, the scalable approach and study design used in this study can be applied to any city across the world.
Credit author statement
Emma Lancaster: Conceptualization, Methodology, Formal analysis, Data curation, Writing- Original Draft, Visualization. Kendall Byrd: Methodology, Writing- Review & Editing. Yuehan Ai: Methodology, Writing- Review & Editing. Jiyoung Lee: Conceptualization, Methodology, Supervision, Writing- Review & Editing, Funding acquisition
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments.
Acknowledgments
The Ohio Department of Health partially supported this study for the conduct of wastewater surveillance.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2022.114290.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Abedi V., Olulana O., Avula V., Chaudhary D., Khan A., Shahjouei S., et al. Racial, economic, and health inequality and COVID-19 infection in the United States. Journal of racial and ethnic health disparities. 2021;8(3):732–742. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler N.E., Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms: health disparities across the lifespan. Ann. N. Y. Acad. Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Agency For Toxic Substances and Disease Registry (ATSDR) 2021. CDC/ATSDR SVI Data and Documentation Download.https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html accessed 05.06.21. [Google Scholar]
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O'Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ai Y., Davis A., Jones D., Lemeshow S., Tu H., He F., Ru P., Pan X., Bohrerova Z., Lee J. Wastewater SARS-CoV-2 monitoring as a community-level COVID-19 trend tracker and variants in Ohio, United States. Sci. Total Environ. 2021;801 doi: 10.1016/j.scitotenv.2021.149757. 149757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aromí J.D., Bonel M.P., Cristia J., Llada M., Palomino L. IDB Working Paper Series. 2021. Socioeconomic status and mobility during the COVID-19 pandemic: An analysis of eight large Latin American cities (No. IDB-WP-1184) [DOI] [Google Scholar]
- Baum F.E., Bégin M., Houweling T.A., Taylor S. Changes not for the fainthearted: reorienting health care systems toward health equity through action on the social determinants of health. Am. J. Publ. Health. 2009;99(11):1967–1974. doi: 10.2105/AJPH.2008.154856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendavid E., Mulaney B., Sood N., Shah S., Bromley-Dulfano R., Lai C., et al. Covid-19 antibody seroprevalence in Santa Clara county, California. Int. J. Epidemiol. 2021;50(2):410–419. doi: 10.1093/ije/dyab010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi P.M., O'Brien J.W., Tscharke B.J., Mueller J.F., Thomas K.V., Samanipour S. Population socioeconomics predicted using wastewater. Environ. Sci. Technol. Lett. 2020;7(8):567–572. doi: 10.1021/acs.estlett.0c00392. [DOI] [Google Scholar]
- Farkas K., Hillary L.S., Malham S.K., McDonald J.E., Jones D.L. Wastewater and public health: the potential of wastewater surveillance for monitoring COVID-19. Current Opinion in Environmental Science & Health. 2020;17:14–20. doi: 10.1016/j.coesh.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S., Roguet A., McClary-Gutierrez J.S., Newton R.J., Kloczko N., Meiman J.G., McLellan S.L. Evaluation of sampling, analysis, and normalization methods for SARS-CoV-2 concentrations in wastewater to assess COVID-19 burdens in Wisconsin communities. ACS EST Water. 2021;1 doi: 10.1021/acsestwater.1c00160. 1955–1965. [DOI] [Google Scholar]
- Figueroa J.F., Wadhera R.K., Mehtsun W.T., Riley K., Phelan J., Jha A.K. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties. Healthcare. 2021;9(1) doi: 10.1016/j.hjdsi.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K., Williams D.R. Health disparities based on socioeconomic inequities: implications for urban health care. Acad. Med. 2004;79(12):1139–1147. doi: 10.1097/00001888-200412000-00004. [DOI] [PubMed] [Google Scholar]
- Gonzalez R., Curtis K., Bivins A., Bibby K., Weir M.H., Yetka K., Thompson H., Keeling D., Mitchell J., Gonzalez D. COVID-19 surveillance in Southeastern Virginia using wastewater-based epidemiology. Water Res. 2020;186 doi: 10.1016/j.watres.2020.116296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham K.E., Loeb S.K., Wolfe M.K., Catoe D., Sinnott-Armstrong N., Kim S., Yamahara K.M., Sassoubre L.M., Mendoza Grijalva L.M., Roldan-Hernandez L., Langenfeld K., Wigginton K.R., Boehm A.B. SARS-CoV-2 RNA in wastewater settled solids is associated with COVID-19 cases in a large urban sewershed. Environ. Sci. Technol. 2021;55:488–498. doi: 10.1021/acs.est.0c06191. [DOI] [PubMed] [Google Scholar]
- Harell A., Lieberman E. How information about race-based health disparities affects policy preferences: evidence from a survey experiment about the COVID-19 pandemic in the United States. Soc. Sci. Med. 2021;277 doi: 10.1016/j.socscimed.2021.113884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart O.E., Halden R.U. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci. Total Environ. 2020;730 doi: 10.1016/j.scitotenv.2020.138875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan S.W., Ibrahim Y., Daou M., Kannout H., Jan N., Lopes A., Alsafar H., Yousef A.F. Detection and quantification of SARS-CoV-2 RNA in wastewater and treated effluents: surveillance of COVID-19 epidemic in the United Arab Emirates. Sci. Total Environ. 2021;764 doi: 10.1016/j.scitotenv.2020.142929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havers F.P., Reed C., Lim T., Montgomery J.M., Klena J.D., Hall A.J., Thornburg N.J. Seroprevalence of antibodies to SARS-CoV-2 in 10 sites in the United States, March 23-May 12, 2020. JAMA Intern. Med. 2020;180(12):1576–1586. doi: 10.1001/jamainternmed.2020.4130. [DOI] [PubMed] [Google Scholar]
- Hickman R., Cao M., Lira B.M., Fillone A., Biona J.B. Understanding capabilities, functionings and travel in high and low income neighbourhoods in manila. Soc. Incl. 2017;5(4):161–174. doi: 10.17645/si.v5i4.1083. [DOI] [Google Scholar]
- Huang Q., Jackson S., Derakhshan S., Lee L., Pham E., Jackson A., Cutter S.L. Urban-rural differences in COVID-19 exposures and outcomes in the South: a preliminary analysis of South Carolina. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E.R., van Vliet M.T.H., Qadir M., Bierkens M.F.P. Country-level and gridded estimates of wastewater production, collection, treatment and reuse. Earth Syst. Sci. Data. 2021;13(2):237–254. doi: 10.5194/essd-13-237-2021. [DOI] [Google Scholar]
- Karmakar M., Lantz P.M., Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.36462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.J., Bostwick W. ? covid 19?> social vulnerability and racial inequality in COVID-19 deaths in chicago. Health Educ. Behav. 2020;47(4):509–513. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Patel A.K., Shah A.V., Raval J., Rajpara N., Joshi M., Joshi C.G. First proof of the capability of wastewater surveillance for COVID-19 in India through detection of genetic material of SARS-CoV-2. Sci. Total Environ. 2020;746 doi: 10.1016/j.scitotenv.2020.141326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar V., Encinosa W. Racial disparities in the perceived risk of COVID-19 and in getting needed medical care. Journal of racial and ethnic health disparities. 2021:1–10. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lodder W., Husman A.M. de R. SARS-CoV-2 in wastewater: potential health risk, but also data source. The Lancet Gastroenterology & Hepatology. 2020;5:533–534. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magesh S., John D., Li W.T., Li Y., Mattingly-App A., Jain S., et al. Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status: a systematic-review and meta-analysis. JAMA Netw. Open. 2021;4(11):e2134147. doi: 10.1001/jamanetworkopen.2021.34147. -e2134147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., Commission on Social Determinants of Health Closing the gap in a generation: health equity through action on the social determinants of health. The lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS- coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in The Netherlands. Environ. Sci. Technol. Lett. 2020;7:511–516. doi: 10.1021/acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- Melvin R.G., Chaudhry N., Georgewill O., Freese R., Simmons G.E. Predictive power of SARS-CoV-2 wastewater surveillance for diverse populations across a large geographical range. 2021. medRxiv. [DOI]
- Mude W., Oguoma V.M., Nyanhanda T., Mwanri L., Njue C. Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: a systematic review and meta-analysis. Journal of Global Health. 2021;11 doi: 10.7189/jogh.11.05015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen C.A., Chernew M.E., Ostrer I., Beaulieu N. Comparison of healthcare delivery systems in low-and high-income communities. Am J Accountable Care. 2019;7(4):11–18. [Google Scholar]
- Ohio Department of Health . 2021. COVID-19 Dashboard: Ohio Coronavirus Wastewater Monitoring Network.https://coronavirus.ohio.gov/wps/portal/gov/covid-19/dashboards/other-resources/wastewater accessed 02.17.21. [Google Scholar]
- Ohio Department of Health . 2022. COVID-19 Dashboard: Overview.https://coronavirus.ohio.gov/wps/portal/gov/covid-19/dashboards/overview accessed 09.09.2022. [Google Scholar]
- Ohio Department of Health . 2021. COVID-19 Dashboard: Testing and Community Health Centers.https://coronavirus.ohio.gov/wps/portal/gov/covid-19/dashboards/other-resources/testing-ch-centers accessed 04.28.21. [Google Scholar]
- O'Donnell C.A., Burns N., Mair F.S., Dowrick C., Clissmann C., van den Muijsenbergh M., RESTORE Team Reducing the health care burden for marginalised migrants: the potential role for primary care in Europe. Health Pol. 2016;120(5):495–508. doi: 10.1016/j.healthpol.2016.03.012. [DOI] [PubMed] [Google Scholar]
- Ohio Development Services Agency . 2021. County Profiles - 2020 Annual Edition.https://development.ohio.gov/reports/reports_countytrends_map.htm accessed 03.01.21. [Google Scholar]
- Ohio State University . 2021. CFAES: Urban Extension.https://urban-extension.cfaes.ohiostate.edu/positioning/ohio-urban-county-directory accessed 03.01.21. [Google Scholar]
- Rodríguez Rasero F.J., Moya Ruano L.A., Rasero Del Real P., Cuberos Gómez L., Lorusso N. Associations between SARS-CoV-2 RNA concentrations in wastewater and COVID-19 rates in days after sampling in small urban areas of Seville: a time series study. Sci. Total Environ. 2022;806 doi: 10.1016/j.scitotenv.2021.150573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rader B., Astley C.M., Sy K.T.L., Sewalk K., Hswen Y., Brownstein J.S., Kraemer M.U. Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates. J. Trav. Med. 2020;27:1–4. doi: 10.1093/jtm/taaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reese H., Iuliano A.D., Patel N.N., Garg S., Kim L., Silk B.J., et al. Estimated incidence of coronavirus disease 2019 (COVID-19) illness and hospitalization—United States, February–September 2020. Clin. Infect. Dis. 2021;72(12):e1010–e1017. doi: 10.1093/cid/ciaa1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu S., Lemmon M.E., Eisenson H., Crowder C., Bettger J.P. Addressing the social determinants of health during the COVID-19 pandemic: ensuring equity, quality, and sustainability. Fam. Community Health. 2021;44:78–80. doi: 10.1097/FCH.0000000000000290. [DOI] [PubMed] [Google Scholar]
- Shah S., Gwee S.X.W., Ng J.Q.X., Lau N., Koh J., Pang J. Wastewater surveillance to infer COVID-19 transmission: a systematic review. Sci. Total Environ. 2022;804 doi: 10.1016/j.scitotenv.2021.150060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner-Dorkenoo A.L., Sarmal A., Rogbeer K., André C., Patel B., Cha L. Highlighting COVID-19 racial disparities can reduce support for safety precautions among White US residents. Soc. Sci. Med. 2022;27:1–8. doi: 10.1016/j.socscimed.2022.114951. 114951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srivastava V., Gupta S., Patel A.K., Joshi M., Kumar M. Reflections of COVID-19 cases in the wastewater loading of SARS-CoV-2 RNA: a case of three major cities of Gujarat, India. Case Studies in Chemical and Environmental Engineering. 2021;4 doi: 10.1016/j.cscee.2021.100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State Medical Board of Ohio . 2018. Annual Report - Fiscal Year 2018.https://www.med.ohio.gov/Portals/0/Publications/Annual%20Reports/State%20Medical%20Board%20of%20Ohio%20FY18%20annual%20report.pdf accessed 03.01.21. [Google Scholar]
- United States Department of Commerce . 2019. U.S. Census Bureau QuickFacts: United States.https://www.census.gov/quickfacts/fact/table/US/PST045219 accessed 03.01.21. [Google Scholar]
- United States Environmental Protection Agency (USEPA) 2021. Septic Systems Overview.https://www.epa.gov/septic/septic-systems-overview accessed 06.21.21. [Google Scholar]
- Weidhaas J., Aanderud Z.T., Roper D.K., VanDerslice J., Gaddis E.B., Ostermiller J., Hoffman K., Jamal R., Heck P., Zhang Y., Torgersen K., Laan J.V., LaCross N. Correlation of SARS-CoV-2 RNA in wastewater with COVID-19 disease burden in sewersheds. Sci. Total Environ. 2021;775 doi: 10.1016/j.scitotenv.2021.145790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) 2020. Listings of WHO's Response to COVID-19.https://www.who.int/news/item/29-06-2020-covidtimeline accessed 05.13.21. [Google Scholar]
- World Health Organization (WHO) 2022. WHO Coronavirus Disease (COVID-19) Dashboard.https://covid19.who.int/ [Google Scholar]
- World Health Organization (WHO) Accessing Access to Water and Sanitation. 2022 https://www.cdc.gov/healthywater/global/assessing.html accessed 06.14.2022. [Google Scholar]
- World Health Organization (WHO) and UNICEF . World Health Organization; Geneva: 2021. Progress on Household Drinking Water, Sanitation and Hygiene 2000-2020: Five Years into the SDGs.https://washdata.org/sites/default/files/2021-07/jmp-2021-wash-households.pdf [PDF – 164 pages] (WHO) and the United Nations Children’s Fund (UNICEF) [Google Scholar]
- Wrigley-Field E., Garcia S., Leider J.P., Robertson C., Wurtz R. Racial disparities in COVID-19 and excess mortality in Minnesota. Socius. 2020;6 doi: 10.1177/2378023120980918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu F., Xiao A., Zhang J., Moniz K., Endo N., Armas F., Bonneau R., Brown M.A., Bushman M., Chai P.R., Duvallet C., Erickson T.B., Foppe K., Ghaeli N., Gu X., Hanage W.P., Huang K.H., Lee W.L., Matus M., et al. SARS-CoV-2 RNA concentrations in wastewater foreshadow dynamics and clinical presentation of new COVID-19 cases. Sci. Total Environ. 2022;805 doi: 10.1016/j.scitotenv.2021.150121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurtzer S., Marechal V., Mouchel J.-M., Maday Y., Teyssou R., Richard E., Almayrac J.L., Moulin L. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome quantification in Paris wastewaters. medRxiv. 2020;25:1–7. doi: 10.1101/2020.04.12.20062679. 2020 04.12.20062679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager R., Holm R.H., Saurabh K., Fuqua J.L., Talley D., Bhatnagar A., Smith T. Wastewater sample site selection to estimate geographically resolved community prevalence of COVID-19: a sampling protocol perspective. GeoHealth. 2021;5(7) doi: 10.1029/2021GH000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Duan M.-J., Dijk H.H., Freriks R.D., Dekker L.H., Mierau J.O. Association between socioeconomic status and self-reported, tested and diagnosed COVID-19 status during the first wave in the Northern Netherlands: a general population-based cohort from 49 474 adults. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-048020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.