Abstract
Introduction
Patients with chronic obstructive pulmonary disease (COPD) often have poor sleep quality and report a worsening of respiratory symptoms during night-time. However, current clinical guidelines for COPD management do not specifically consider nocturnal symptoms when recommending pharmacological treatment. This study aimed to better understand the burden of nocturnal symptoms in patients with COPD, and to evaluate the importance of nocturnal symptom control compared with daytime and overall symptom control.
Methods
Data were analyzed from the Adelphi Respiratory Disease Specific Programme, a point-in-time survey of physicians and their patients, conducted in the USA in 2019. Primary care physicians and pulmonologists who managed three or more patients with COPD per month were eligible for inclusion; eligible patients were ≥ 18 years old, with a physician-confirmed diagnosis of COPD.
Results
Surveys from 171 physicians and 800 patients were analyzed. Everyday symptoms were reported in 14% of patients. In total, 88% of patients reported daytime symptoms, and 74% of patients experienced nocturnal symptoms, with 7% reporting daily nocturnal symptoms. Patients experiencing nocturnal symptoms every day had the greatest impairment in their activity as per the Work Productivity and Activity Impairment questionnaire (mean total activity impairment, 66.9%; nocturnal symptoms once or twice a week, 41.1%; no nocturnal symptoms, 26.4%). Patients experiencing daily nocturnal symptoms also had the lowest quality of life (QoL) as per the EuroQoL 5-Dimension 3-Level score. Physicians reported prescribing therapy based on sustained 24-h symptomatic relief for the majority of patients (78%). They reported nocturnal symptom control as a factor in their choice of therapy for 38% of patients, and daytime symptom control as a reason for 61% of patients.
Conclusion
Daytime and nocturnal symptoms are common among patients with COPD. Frequency of nocturnal symptoms is related to a significant impairment in activity and health-related QoL.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41030-022-00196-7.
Keywords: Chronic obstructive pulmonary disease, Lung, Real-world survey, Sleep, Sleep quality, Symptoms
Key Summary Points
| Why carry out this study? |
| Sleep complaints among patients with chronic obstructive pulmonary disease (COPD) are common, ranking third after dyspnea and fatigue. Despite this, sleep disturbances and/or nocturnal symptoms are rarely mentioned in current COPD treatment guidelines |
| This study aimed to investigate the burden of nocturnal symptoms among patients with COPD, and to evaluate the importance of nocturnal symptom control |
| What was learned from the study? |
| In total, 74% of patients included in this analysis reported experiencing nocturnal symptoms, with 7% of patients experiencing daily nocturnal symptoms. Patients experiencing daily nocturnal symptoms had the greatest activity impairment per the Work Productivity and Activity Impairment questionnaire, and lowest quality of life per the EuroQoL 5-Dimension 3-Level score. Physicians reported that they prescribed therapy based on sustained 24-h relief for most of their patients (78%), and they prescribed therapy based on nocturnal symptom relief for 38% of their patients |
| The results of this study bring new insights into the frequency and impact of nocturnal symptoms among patients with COPD in the USA. Health care professionals should seek to individualize treatment to maximize 24-h symptom control for their patients with COPD |
Introduction
Chronic obstructive pulmonary disease (COPD) is a common progressive condition characterized by persistent airflow limitation and increasing breathlessness [1]. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) provides treatment guidelines for the management of COPD, which aims to reduce the occurrence of respiratory symptoms and lower the risk of future exacerbations (episodes of acute worsening of respiratory symptoms). Pharmacological maintenance therapy for COPD can include the use of long-acting muscarinic antagonists (LAMA), long-acting β2 agonists (LABA), and/or inhaled corticosteroids (ICS; usually taken in combination with LABA). GOLD guidelines recommend an incremental approach to treatment, involving a combination of drug classes as disease state worsens [1].
Patients with COPD often have poor sleep quality and report a worsening of respiratory symptoms at night-time [2, 3]. Indeed, sleep complaints in COPD patients are common, ranking third after dyspnea and fatigue [2, 4]. Sleep has important effects on breathing and gas exchange that may exacerbate the already impaired respiratory system in COPD [3]. Nocturnal symptoms in COPD may also overlap with the presence of sleep-disordered breathing, such as obstructive sleep apnea, and nocturnal oxygen desaturation, which increase the morbidity and mortality in this group of patients [5–7]. Despite this, sleep disturbances and/or nocturnal symptoms are seldom mentioned in current COPD treatment guidelines [1].
The objective of this study was to further investigate the burden of nocturnal symptoms among patients with COPD, and to understand how nocturnal symptom control affects the patient and is assessed by the physician compared with daytime and overall symptom control.
Methods
Study Design
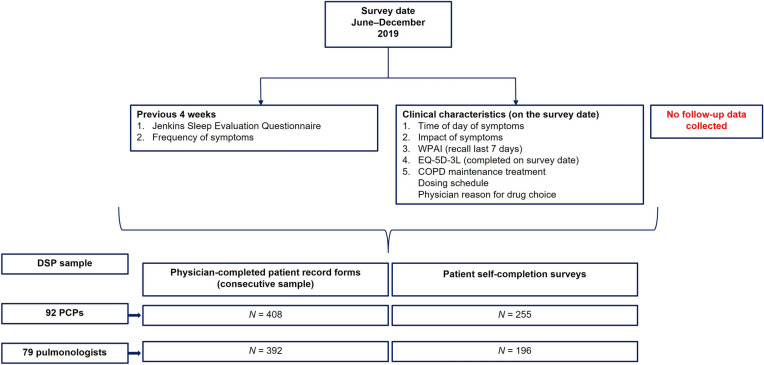
The study design is shown in Fig. 1. The data for this study were drawn from the Adelphi Respiratory Disease Specific Programme (DSP), a point-in-time survey of patients with COPD and their physicians, conducted in the USA from July to December 2019. DSP methodology has been previously published and validated [8], and it represents an established method for investigating symptom burden and treatment practices across a wide range of disease areas, including COPD [9]. All information was recorded on the survey date from available medical history or a specified recall period for physicians and patients, and no follow-up information was collected.
Fig. 1.
Respiratory DSP survey: population sampled and data captured for the burden of nocturnal COPD symptoms study. COPD chronic obstructive pulmonary disease, DSP Disease Specific Programme, EQ-5D-3L EuroQoL 5-Dimension 3-Level, PCP primary care physician, WPAI Work Productivity and Activity Impairment
The survey received an exemption determination by the Western Institutional Review Board, a central international review board for the USA (study number 1-1211337-1; 14 August 2019). Patients provided informed consent before completing the voluntary patient self-completion survey, and all data from physicians and patients were aggregated and de-identified before receipt. The survey was performed in accordance with the Helsinki Declaration of 1964, and its later amendments, and also adhered to the ICC/ESOMAR International code on observational research and Health Insurance Portability and Accountability Act (HIPAA) guidelines.
Physician and Patient Eligibility Criteria
Data were collected from patients and physicians [primary care physicians (PCPs) and pulmonologists]. To participate, physicians were required to manage three or more patients with COPD per month. Patients had to be at least 18 years old with a confirmed diagnosis of COPD; patients currently enrolled in a clinical research study were excluded. Physicians were instructed to complete a record form for the next five consecutively consulting patients. Each patient for whom the physician completed a form was then invited to fill in a self-completion form.
Study Outcomes and Data Sources
The primary objective of this study was to describe the proportion of COPD patients with nocturnal symptoms, their frequency relative to daytime symptoms, and the association of nocturnal symptom frequency with overall quality of life (QoL) and work and activity impairment. Patients were asked to complete the Jenkins Sleep Evaluation Questionnaire (JSEQ) to provide data on sleep disturbances (recall over past 4 weeks [10]) and the Work Productivity and Activity Impairment (WPAI) questionnaire (recall over last 7 days). Only patients in current employment completed the work-related questions in the WPAI questionnaire. Overall health-related QoL was assessed by patient completion of the EuroQoL 5-Dimension 3-Level (EQ-5D-3L) utility score and the EQ-5D visual analog scale (VAS), on the day of the survey.
Secondary objectives were to describe the relationship between nocturnal symptoms, frequency and timing of COPD maintenance therapy, and choice of COPD medications by treating physicians. The following data were extracted from the DSP: patient-reported variables including timing, frequency, and dosing of daily maintenance treatment; physician-reported reasons for current drug choice (physician response on survey date); and frequency of daily dosing of maintenance therapy (based on medical records).
An exploratory objective was to describe the demographics and clinical characteristics of the surveyed COPD patients with and without nocturnal symptoms, which were obtained from physician-completed surveys/medical records. Where appropriate, and depending on the variable, the timeframe for collection of this information was either the survey date (e.g., for age, sex, employment status) or based on available medical records [comorbidities, body mass index (BMI); Charlson Comorbidity Index (CCI)].
Data Analysis
Descriptive analyses were generated using data extracted from the Respiratory DSP. Categorical variables are reported as frequency and percentage of patients within each response; numerical variables are reported as number of responses, mean, and standard deviation (SD). Each variable is described using the maximum sample available to that variable, which may differ depending on whether the variable is physician- or patient-reported and the level of the missing data. The number of missing data is reported. An explanation of outcome variables is provided as supplementary material.
Results
Figure 1 shows the overall sample captured in the DSP and the data extracted for the current study. Completed surveys from 171 physicians (n = 92 PCPs, n = 79 pulmonologists) and 800 patients were available. Table 1 summarizes patient demographics and disease characteristics according to the presence and frequency of nocturnal COPD symptoms as reported by physicians. Data were available for 690/800 patients, 33 of whom (4.8%) were noted as experiencing nocturnal symptoms every day; these patients were on average older (69.5 years) than other patients (mean age: 66.9, 66.5, 66.3, and 67.2 years for patients with no nocturnal symptoms, symptoms less than one time per week, one to two times per week, and three to six times per week, respectively), and a lower proportion were in full-time employment (9.1% versus 24.8%, 23.2%, 21.4%, and 26.7% for patients with no nocturnal symptoms, symptoms less than one time per week, one to two times per week, and three to six times per week, respectively). Mean BMI and the proportion of males/females were comparable across the different frequencies of nocturnal symptoms.
Table 1.
Demographics and characteristics of patients with COPD according to presence and frequency of nocturnal symptoms
| Frequency of nocturnal COPD symptomsa | ||||||
|---|---|---|---|---|---|---|
| None N = 161 |
< 1 time per week N = 243 |
1–2 times per week N = 193 |
3–6 times per week N = 60 |
Daily N = 33 |
Total N = 690 |
|
| Physician setting, n (%) | ||||||
| Primary care | 81 (50.31) | 115 (47.33) | 94 (48.70) | 36 (60.00) | 19 (57.58) | 345 (50) |
| Pulmonologist | 80 (49.69) | 128 (52.67) | 99 (51.30) | 24 (40.00) | 14 (42.42) | 345 (50) |
| Patient age, years, mean (SD) | 66.9 (10.39) | 66.5 (10.91) | 66.3 (10.56) | 67.2 (9.61) | 69.5 (11.97) | 66.8 (10.63) |
| Female, n (%) | 75 (46.58) | 112 (46.09) | 91 (47.15) | 19 (31.67) | 15 (45.45) | 312 (45.22) |
| BMI, kg/m2, mean (SD) | 26.9 (5.03) | 27.8 (5.49) | 27.6 (6.54) | 27.5 (5.40) | 26.4 (7.04) | 27.5 (5.77) |
| CCI, mean (SD) | 1.43 (1.13) | 1.51 (1.18) | 1.48 (1.09) | 1.78 (0.99) | 1.85 (1.35) | 1.52 (1.14) |
| Employment status, n (%) | N = 161 | N = 241 | N = 192 | N = 60 | N = 33 | N = 687 |
| Working full-time | 40 (24.84) | 56 (23.24) | 41 (21.35) | 16 (26.67) | 3 (9.09) | 156 (22.71) |
| Working part-time | 12 (7.45) | 20 (8.30) | 16 (8.33) | 5 (8.33) | 2 (6.06) | 55 (8.00) |
| On long-term sick leave | 0 (0.00) | 3 (1.24) | 3 (1.56) | 0 (0.00) | 0 (0.00) | 6 (0.87) |
| Homemaker | 11 (6.83) | 13 (5.39) | 10 (5.21) | 0 (0.00) | 4 (12.12) | 38 (5.53) |
| Retired | 94 (58.39) | 140 (58.09) | 116 (60.42) | 35 (58.33) | 22 (66.67) | 407 (59.24) |
| Unemployed | 4 (2.48) | 9 (3.73) | 6 (3.13) | 4 (6.67) | 2 (6.06) | 25 (3.64) |
| Smoking status, n (%) | N = 160 | N = 239 | N = 192 | N = 57 | N = 32 | N = 680 |
| Current smoker | 38 (23.75) | 42 (17.57) | 47 (24.48) | 19 (33.33) | 8 (25.00) | 154 (22.65) |
| Ex-smoker | 108 (67.50) | 177 (74.06) | 127 (66.15) | 35 (61.40) | 19 (59.38) | 466 (68.53) |
| Never smoked | 14 (8.75) | 20 (8.37) | 18 (9.38) | 3 (5.26) | 5 (15.63) | 60 (8.82) |
BMI body mass index, CCI Charlson Comorbidity Index, COPD chronic obstructive pulmonary disease, SD standard deviation
aData provided are physician-reported frequencies of nocturnal COPD symptoms
Timing and Frequency of COPD Symptoms
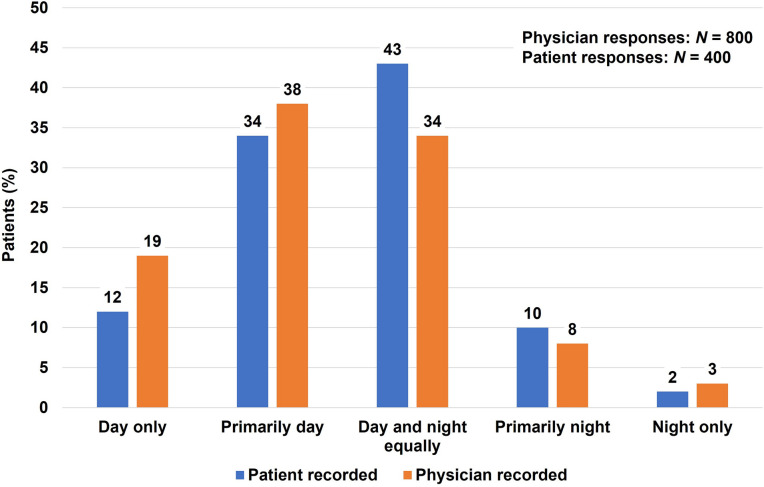
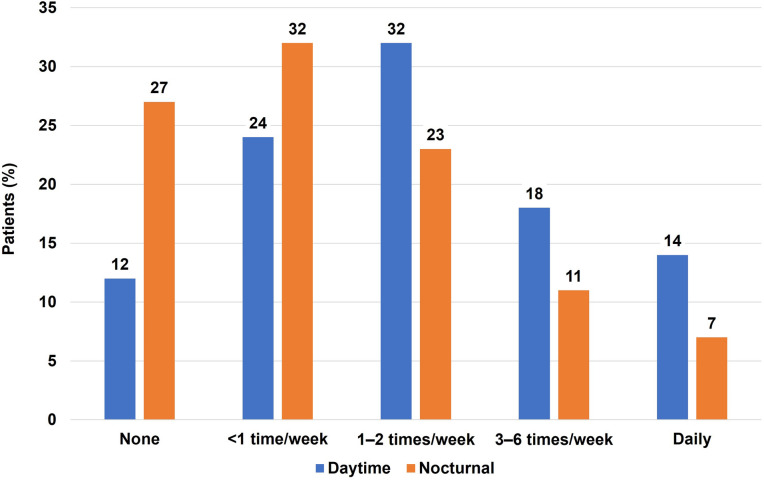
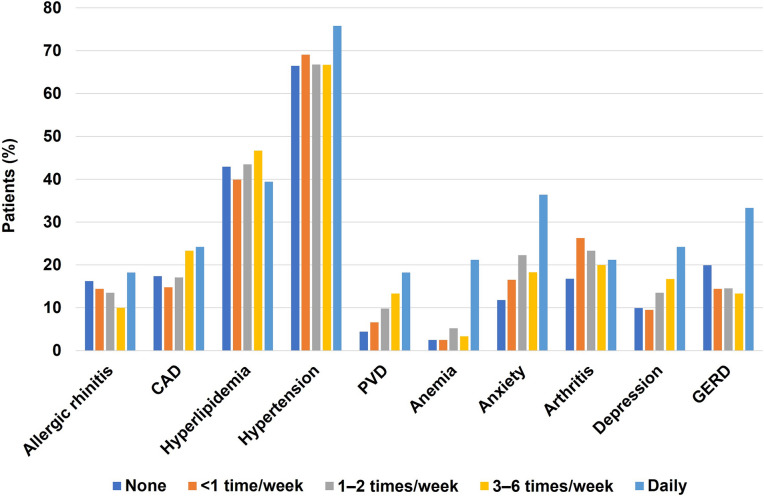
Daytime symptoms were reported more frequently by patients than nocturnal symptoms. In total, 12% of patients reported daytime symptoms only, 34% reported primarily daytime symptoms, 43% reported symptoms occurring equally during the day and night, 10% had primarily night-time symptoms, and 2% reported symptoms occurring only during the night (Fig. 2). Overall, 74% of patients reported that they experienced nocturnal symptoms, with 7% reporting daily nocturnal symptoms (Fig. 3). Most patients (88%) reported daytime symptoms, with daily symptoms reported in 14% of patients. A higher proportion of patients experiencing nocturnal symptoms every day, as reported by their physician, had comorbidities such as hypertension (76%), anxiety (36%), depression (24%), anemia (21%), and gastrointestinal reflux disease (GERD; 33%) compared with patients experiencing less frequent nocturnal symptoms (Fig. 4).
Fig. 2.
Time of day when patients are bothered most by COPD symptoms, as reported by patients and their treating physicians. COPD chronic obstructive pulmonary disease
Fig. 3.
Patient-reported frequency of symptoms
Fig. 4.
Ten most frequent physician-reported comorbidities occurring in patients with nocturnal symptoms. CAD coronary artery disease, GERD gastroesophageal reflux disease, PVD peripheral vascular disease
Impact of Nocturnal COPD Symptoms on Patients’ Daily Lives and QoL
Data on sleep disruption experienced by patients were captured by the JSEQ (which assesses the frequency of sleep disturbances; lower scores indicate less disturbance). Mean JSEQ scores increased with increasing frequency of nocturnal symptoms; these ranged from 3.2 in patients with no reported COPD nocturnal symptoms to 9.5 in patients experiencing nocturnal symptoms every day (Table 2).
Table 2.
Association between frequency of nocturnal COPD symptoms and overall activity impairment and health-related QoL
| Frequency of nocturnal COPD symptomsa | |||||
|---|---|---|---|---|---|
| None N = 161 |
< 1 time per week N = 243 |
1–2 times per week N = 193 |
3–6 times per week N = 60 |
Daily N = 33 |
|
| JSEQb | N = 78 | N = 136 | N = 116 | N = 31 | N = 17 |
| Mean score (SD)c | 3.2 (4.60) | 3.5 (3.80) | 5.1 (3.49) | 6.9 (5.09) | 9.5 (5.16) |
| WPAI questionnaireb | |||||
| Absenteeismd | N = 21 | N = 43 | N = 32 | N = 9 | N = 0 |
| Mean % (SD) | 0.4 (1.98) | 2.1 (6.47) | 4.4 (17.91) | 4.8 (14.29) | N/A |
| Presenteeismd | N = 26 | N = 46 | N = 39 | N = 11 | N = 0 |
| Mean, % (SD) | 15 (17.72) | 22.2 (15.34) | 26.7 (19.65) | 24.5 (9.34) | N/A |
| Overall work impairmentd | N = 21 | N = 43 | N = 31 | N = 9 | N = 0 |
| Mean (%) impairment (SD) | 15.4 (19.01) | 23.5 (17.18) | 24.5 (16.29) | 27.8 (15.63) | N/A |
| Total activity impairment | N = 81 | N = 134 | N = 114 | N = 31 | N = 16 |
| Mean (%) impairment (SD) | 26.4 (24.41) | 32.1 (21.97) | 41.1 (22.76) | 35.2 (21.11) | 66.9 (27.98) |
| EQ-5D-3Lb | N = 83 | N = 140 | N = 117 | N = 32 | N = 17 |
| Mean score (SD) | 0.882 (0.157) | 0.836 (0.160) | 0.800 (0.173) | 0.808 (0.164) | 0.602 (0.230) |
| EQ-5D VASb | N = 83 | N = 138 | N = 119 | N = 31 | N = 18 |
| Mean score (SD) | 75.3 (17.71) | 73.1 (15.11) | 68.6 (17.04) | 68.5 (17.74) | 44.2 (23.65) |
COPD chronic obstructive pulmonary disease, EQ-5D(-3L) EuroQoL 5-Dimension (3-Level), JSEQ Jenkins Sleep Evaluation Questionnaire, N/A not applicable, QoL quality of life, SD standard deviation, VAS visual analog scale, WPAI Work Productivity and Activity Impairment
aData provided are physician-reported frequencies of nocturnal COPD symptoms
bData are presented for patients who completed the voluntary self-completion survey
cPatients with COPD had a mean JSEQ score of 4.2
dOnly patients in current employment completed work-related questions in the WPAI questionnaire
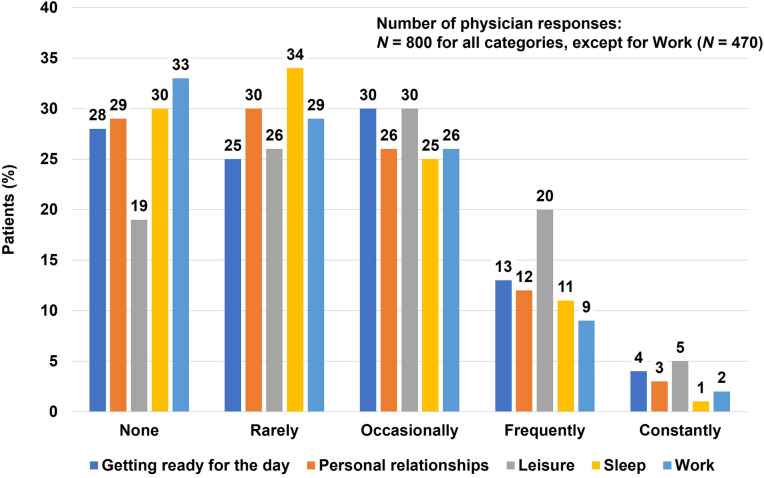
Of the patients who completed the WPAI questionnaire, those experiencing nocturnal symptoms every day had the greatest impairment in their activity, and none of these patients was working (Table 2). Their total activity impairment was 66.9% (versus 41.1% or lower in patients with less frequent nocturnal symptoms, and 26.4% in patients who did not experience nocturnal symptoms). Patients experiencing daily nocturnal symptoms also had the lowest QoL as per the EQ-5D-3L score. Patients experiencing nocturnal symptoms every day had a mean EQ-5D-3L score of 0.602 compared with a mean of 0.882 in patients who did not experience any nocturnal symptoms. Physicians also reported that COPD impacted many aspects of a patient’s life (Fig. 5), including getting up and getting ready for the day, personal relationships, leisure, sleep, and work. COPD was judged to impact sleep occasionally, frequently, or constantly in 37% of patients.
Fig. 5.
Physician-reported impact of COPD on patients’ daily life and activities. COPD chronic obstructive pulmonary disease
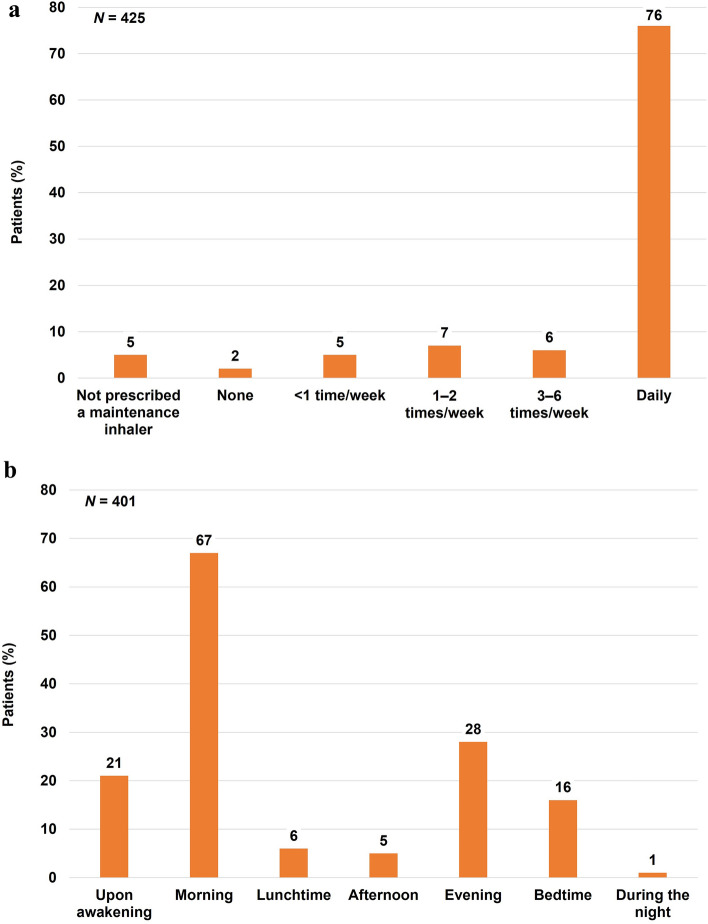
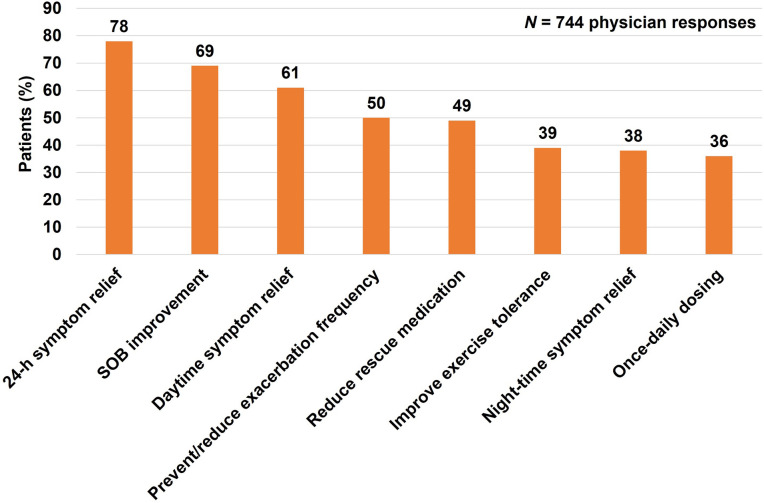
Frequency and Timing of COPD Maintenance Therapy; Physicians’ Reasons for Treatment Choice
The frequency and timing of COPD maintenance medication taken and reported by patients is summarized in Fig. 6A, B, respectively. Most patients (76%) took their maintenance medication every day (Fig. 6A), and this proportion was the same among patients reporting daily nocturnal symptoms. Overall, 60% of patients were taking their maintenance medication twice daily, while 39% of patients took theirs once daily. Physicians reported nocturnal symptom control as a reason for their choice of maintenance therapy for 38% of patients, and daytime symptom control as a reason for 61% of patients (Fig. 7). Improvement of nocturnal symptom burden was cited by physicians as a reason for treatment choice in 40% of patients taking once-daily maintenance treatment versus 42% taking twice-daily treatment.
Fig. 6.
Patient-reported frequency (A) and timing (B) of maintenance medication for COPD during the past 4 weeks. COPD chronic obstructive pulmonary disease
Fig. 7.
Physician-reported reasons for choosing the COPD maintenance therapy prescribed for patients (only responses > 25% shown). Other reasons for choosing COPD maintenance therapy (reported in ≤ 25% of patients) were: immediate onset of action; improvement in symptomatic relief on awakening; clinically relevant improvement in lung function test values; reduce levels of inflammation; reduce response to allergic triggers; penetration of drug in the lower and peripheral airways; well-tolerated side-effect profile; good cardiovascular profile; avoid using high-dose inhaled steroid medications; avoid using LABA medication; limit the use of additional oral steroid medication; maximize patient compliance; ease of use/suitability of inhaler device; acts as both a reliever and as a maintenance therapy; option to upward or downward titrate when required; drug familiarity and personal experience; in accordance with clinical guidelines; request by patient. COPD chronic obstructive pulmonary disease, LABA long-acting β2 agonist, SOB symptoms of breathlessness
Discussion
This study investigated nocturnal symptoms and the association between prescription patterns and quality of sleep among patients with COPD. It brings new insights into the frequency and impact of nocturnal symptoms in patients with COPD, and their relationship with the use of COPD maintenance therapies in the USA.
Our study found that daytime COPD symptoms are commonly experienced by patients with COPD. Furthermore, 74% of patients also experienced nocturnal symptoms during the 4 weeks prior to the survey, and 7% of patients reported having symptoms every night. Patients reported that nocturnal COPD symptoms impaired their sleep quality, thus impacting their overall QoL. Results of the JSEQ showed that patients’ sleep disruption became more pronounced with increasing frequency of nocturnal COPD symptoms. Patients with COPD had a mean JSEQ score of 4.2, and the mean score increased to 9.5 in patients experiencing nocturnal symptoms every day. Previous research has indicated that a JSEQ score ≥ 3 is suggestive of frequent sleep complaints (i.e., sleep disturbances at least once per week during the previous month) [11]. JSEQ scores have also been shown to be positively correlated with COPD symptoms (as measured by the COPD Assessment Test) [3], suggesting that patients with frequent nocturnal symptoms may have poor overall symptom control. We found that increasing frequency of nocturnal symptoms was also associated with impairment of patients’ work and daily activities. Of the patients with daily nocturnal symptoms who completed the WPAI questionnaire, none was working, and WPAI results showed they had a mean of 67% total activity impairment. Patients with less frequent nocturnal symptoms also had substantial impairment (mean ranging from 32% to 41%) versus patients reporting no nocturnal symptoms (mean 26% impairment). The detrimental effect of frequent nocturnal symptoms was also indicated by QoL assessments; patients with nocturnal symptoms every day had the lowest health-related QoL as per the EQ-5D-3L score.
Our results indicate that health care providers are aware of the detrimental effects to sleep in patients with COPD. Physicians reported that they prescribed therapy based on sustained 24-h symptomatic relief for the majority of their patients (78%). Treatment choice based on nocturnal symptom control was a factor in physicians’ choice of medication for 38% of their patients. This study suggests that a significant proportion of patients have frequent nocturnal symptoms, and these appear to be the patients with the worst COPD burden.
Given the detrimental effects of nocturnal symptoms on sleep quality and patients’ daily life and QoL, physicians should consider working with their patients with COPD to maximize 24-h symptom control. Current GOLD guidelines recommend optimizing treatment if a patient remains symptomatic [1]. As nocturnal symptoms may be a consequence of poor disease control, the first step in treating sleep disorders should be to optimize COPD treatment. Physicians should seek to individualize treatment to maximize 24-h symptom control and support patients’ adherence to maintenance treatment (e.g., by consolidating any multiple inhaler use into a single inhaler, where fixed dose combinations allow). COPD inhalers are typically dosed once or twice a day. It was suggested that once-a-day treatment may negatively influence sleep quality; however, studies have since shown that both once- and twice-daily medications offer similar bronchodilation during the evening [12].
The results of our study complement those of previous studies investigating sleep disturbances in patients with COPD [13, 14], and there appears to be a bidirectional association between poor sleep and COPD symptoms. COPD symptoms such as cough and dyspnea may lead to poor sleep, and poor sleep can contribute to poor COPD-related outcomes [13]. Our results also showed that a higher proportion of patients with COPD experiencing nocturnal symptoms every day suffered from comorbidities such as hypertension, anxiety, depression, anemia, and GERD, compared with patients experiencing less frequent night-time symptoms, consistent with previous findings [14].
A previous observational study showed that more than half of patients experience COPD symptoms throughout a 24-h period, with a significant relationship between nocturnal, early-morning, and daytime symptoms [15]. In each period, symptoms were associated with worse patient-reported outcomes, suggesting that improving 24-h symptoms should be an important consideration in the management of COPD.
Our study has some limitations. First, patients participating in DSP may not reflect the general COPD population. Diagnosis of COPD was required by a physician; however, some patients may not have had spirometry on their diagnosis algorithm. While minimal inclusion criteria governed the selection of participating physicians, participation was influenced by willingness to complete the survey and by pragmatic geographical considerations such as a concentration of recruitment in urban areas. However, our study represents a large variety of individuals, and demographics from our study are similar to those reported in other published COPD studies [3, 16]. Recall bias may have affected the responses of both patients and physicians. However, the data for these analyses were collected at the time of each patient’s appointment, which should theoretically reduce the likelihood of recall bias. In addition, not all patients agreed to participate in the voluntary self-completion survey; as a result, JSEQ, EQ-5D-3L, and WPAI questionnaire data were not available for all patients described in other summaries. Finally, JSEQ quantification of sleep disturbances is based on a recall of the past 4 weeks, whereas the EQ-5D-3L is measured on the survey date and WPAI is based on patient recall over the last 7 days; hence, these variables were measured at different timepoints. As the collecting dates were very similar, it can be considered acceptable temporal disparity for making comparisons.
Despite these limitations, real-world studies can provide valuable insights and play an important role in identifying areas of concern that may not be captured in a clinical trial. Clinical trials often have stringent eligibility criteria, and, as a result, participating patients often represent a small proportion of the real-world population [17]. In addition, adherence to therapy is likely to be lower among patients treated in a real-life clinical setting compared with clinical trials [18]. Data from real-world studies can therefore complement clinical trial data and provide insights into the effectiveness of interventions in patients commonly treated in routine clinical practice.
Conclusions
Daytime and nocturnal symptoms are common among patients with COPD. Frequency of nocturnal symptoms was related to significant impairment in activity and health-related QoL. As a first step to reduce sleep complaints and increase sleep quality among patients with COPD, health care professionals should optimize COPD treatment as recommended in current guidelines. Maximizing 24-h symptom control will likely minimize both daytime and nocturnal symptoms in patients with COPD.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Funding
This study was funded by GSK (study number 209574) based on subscription to the DSP dataset. GSK was involved in study conception and design, data interpretation, and the decision to submit the article for publication. GSK was also given the opportunity to review the manuscript for medical and scientific accuracy as well as intellectual property considerations. All publication fees were funded by the sponsor.
Medical Writing, Editorial, and Other Assistance
Editorial support (in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing and referencing) was provided by Tony Reardon of Aura, a division of Spirit Medical Communications Group Limited (Manchester, UK), and was funded by GSK. Trademarks are the property of their respective owners.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
James Siddall, Mark Small, and Michael Bogart contributed to study conception and/or design. James Siddall and Mark Small contributed to acquisition of data. Xavier Soler, James Siddall, Mark Small, Marjorie Stiegler, and Michael Bogart contributed to data analysis and/or interpretation.
Prior Presentation
The abstract of this paper was presented at the 2020 American College of Chest Physicians Congress as a poster presentation. The poster’s abstract was published in Chest. 2020;158(4):A1775. Available from: https://journal.chestnet.org/article/S0012-3692(20)33735-1/fulltext. https://doi.org/10.1016/j.chest.2020.08.1549.
Disclosures
The authors declare the following conflicts of interest during the last three years in relation to this article: Xavier Soler and Michael Bogart are former full-time GSK employees and held stocks/shares in the company. Marjorie Stiegler is a GSK employee and holds stocks/shares. James Siddall and Mark Small are current employees of Adelphi Real World; Adelphi Real World received subscription funds to the DSP dataset from GSK to conduct this study. Current affiliation details for Xavier Soler: UC San Diego Health, La Jolla, CA, USA. Current affiliation details for Michael Bogart: Gilead Sciences, Foster City, CA, USA.
Compliance with Ethics Guidelines
The survey received an exemption determination by the Western Institutional Review Board, a central international review board for the US (Study Number: 1–1211337-1; August 14, 2019). Patients provided informed consent before completing the voluntary patient self-completion survey and all data from physicians and patients were aggregated and de-identified before receipt. The survey was performed in accordance with the Helsinki Declaration of 1964, and its later amendments, and also adhered to the ICC/ESOMAR International code on observational research and Health Insurance Portability and Accountability Act (HIPAA) guidelines.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Global Initiative for Chronic Obstructive Lung Disease. 2021 Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease. 2021. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf. Accessed 30 Sept 2021.
- 2.Agusti A, Hedner J, Marin J, Barbé F, Cazzola M, Rennard S. Night-time symptoms: a forgotten dimension of COPD. Eur Respir Rev. 2011;20(121):183–194. doi: 10.1183/09059180.00004311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ding B, Small M, Bergström G, Holmgren U. A cross-sectional survey of night-time symptoms and impact of sleep disturbance on symptoms and health status in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:589–599. doi: 10.2147/COPD.S122485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinsman RA, Yaroush R, Fernandez E, Dirks JF, Schocket M, Fukuhara J. Symptoms and experiences in chronic bronchitis and emphysema. Chest. 1983;83(5):755–761. doi: 10.1378/chest.83.5.755. [DOI] [PubMed] [Google Scholar]
- 5.Lewis CA, Fergusson W, Eaton T, Zeng I, Kolbe J. Isolated nocturnal desaturation in COPD: prevalence and impact on quality of life and sleep. Thorax. 2009;64(2):133–138. doi: 10.1136/thx.2007.088930. [DOI] [PubMed] [Google Scholar]
- 6.Machado MC, Vollmer WM, Togeiro SM, et al. CPAP and survival in moderate-to-severe obstructive sleep apnoea syndrome and hypoxaemic COPD. Eur Respir J. 2010;35(1):132–137. doi: 10.1183/09031936.00192008. [DOI] [PubMed] [Google Scholar]
- 7.Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR. Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med. 2010;182(3):325–331. doi: 10.1164/rccm.200912-1869OC. [DOI] [PubMed] [Google Scholar]
- 8.Anderson P, Benford M, Harris N, Karavali M, Piercy J. Real-world physician and patient behaviour across countries: disease-specific programmes–a means to understand. Curr Med Res Opin. 2008;24(11):3063–3072. doi: 10.1185/03007990802457040. [DOI] [PubMed] [Google Scholar]
- 9.Vestbo J, Vogelmeier C, Small M, Higgins V. Understanding the GOLD 2011 Strategy as applied to a real-world COPD population. Respir Med. 2014;108(5):729–736. doi: 10.1016/j.rmed.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Jenkins CD, Stanton B-A, Niemcryk SJ, Rose RM. A scale for the estimation of sleep problems in clinical research. J Clin Epidemiol. 1988;41(4):313–321. doi: 10.1016/0895-4356(88)90138-2. [DOI] [PubMed] [Google Scholar]
- 11.Lallukka T, Rahkonen O, Lahelma E, Arber S. Sleep complaints in middle-aged women and men: the contribution of working conditions and work–family conflicts. J Sleep Res. 2010;19(3):466–477. doi: 10.1111/j.1365-2869.2010.00821.x. [DOI] [PubMed] [Google Scholar]
- 12.Ferguson GT, Brown N, Compton C, et al. Once-daily single-inhaler versus twice-daily multiple-inhaler triple therapy in patients with COPD: lung function and health status results from two replicate randomized controlled trials. Respir Res. 2020;21:131. doi: 10.1186/s12931-020-01360-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omachi TA, Blanc PD, Claman DM, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med. 2012;13(5):476–483. doi: 10.1016/j.sleep.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah A, Ayas N, Tan W-C, et al. Sleep quality and nocturnal symptoms in a community-based COPD cohort. COPD. 2020;17(1):40–48. doi: 10.1080/15412555.2019.1695247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miravitlles M, Worth H, Cataluña JJS, et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res. 2014;15(1):122. doi: 10.1186/s12931-014-0122-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price D, Small M, Milligan G, Higgins V, Gil EG, Estruch J. Impact of night-time symptoms in COPD: a real-world study in five European countries. Int J Chron Obstruct Pulmon Dis. 2013;8:595–603. doi: 10.2147/COPD.S48570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saunders C, Byrne CD, Guthrie B, et al. External validity of randomized controlled trials of glycaemic control and vascular disease: how representative are participants? Diabet Med. 2013;30(3):300–308. doi: 10.1111/dme.12047. [DOI] [PubMed] [Google Scholar]
- 18.Hubbard TE, Paradis R. Real world evidence: a new era for health care innovation. The Network for Excellence in Health Innovation. 2015. https://www.nehi-us.org/writable/publication_files/file/rwe_issue_brief_final.pdf. Accessed 30 Sept 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.