Abstract
Background
Total hip arthroplasty (THA) in younger patients is projected to increase by a factor of 5 by 2030 and will have important implications for clinical practice, policymaking, and research. This scoping review aimed to synthesize and summarize THA implants' survival, reoperation, and wear rates and identify indications and risk factors for reoperation following THA in patients ≤55 years old.
Material and methods
Standardized scoping review methodology was applied. We searched 4 electronic databases (Medline, Embase, CINAHL, and Web of Science) from January 1990 to May 2019. Selection criteria were patients aged ≤55 years, THA survival, reoperation, and/or wear rate reported, a minimum of 20 reoperations included, and minimum level III based on the Oxford Level of Evidence. Two authors independently reviewed the citations, extracted data, and assessed quality.
Results
Of the 2255 citations screened, 35 retrospective cohort studies were included. Survival rates for THA at 5 and 20 years were 90%-100% and 60.4%-77.7%, respectively. Reoperation rates at ≤5-year post THA ranged from 1.6% to 5.4% and increased at 10-20 years post THA (8.2%-67%). Common causes for reoperation were aseptic loosening of hip implants, osteolysis, wear, and infection. Higher reoperation and lower survival rates were seen with hip dysplasia and avascular necrosis than with other primary diagnoses.
Conclusions
Over time, THA prosthetic survival rates decreased, and reoperation increased in patients ≤55 years. Aseptic loosening of hip implants, osteolysis, wear, and infection were the most frequent reasons for the reoperation.
Keywords: Hip, Arthroplasty, Joint replacement, Survival, Revision, Reoperation
Introduction
Over the past 20 years, the number of patients undergoing total hip arthroplasty (THA) for end-stage osteoarthritis (OA) has dramatically increased [[1], [2], [3]]. By the year 2030, the demand for THA among young patients is projected to grow by a factor of 5 [1,4]. THA provides substantial pain relief and resumption of many activities, including sporting activities such as hiking, skiing, swimming, and cycling in younger patients [5]. Previous reviews [6,7], including a recent systematic review, reported a 15-year survival rate of 87.9% (95% confidence interval [CI]: 87.2 to 88.5) for patients aged between 58 and 74 years [6]. The 15- to 20-year survival rate for THA, however, poses a challenge for young patients who likely will need multiple reoperations in their lifetime [[8], [9], [10], [11]]. Besides the longer duration that young patients will have with their THA, they tend to adopt an active lifestyle when pain and stiffness are relieved after THA.
Unlike older patients who often require THA for OA, indications in patients younger than 55 years include pathologies such as rheumatoid arthritis, avascular necrosis (AVN) of the hip, and developmental dysplasia of the hip (DDH) [12,13]. Thus, a greater proportion of younger patients undergo complex primary THA, which can be more technically demanding due to anatomic abnormalities and bone loss [14]. With different THA indications and procedures in the younger patient population, survivorship and reoperation rates may differ from older patients with THA [[6], [8], [15], [16], [17]]. It is also uncertain if younger patients with more active lifestyle accelerate polyethylene wear rates (annual erosion of polyethylene of THA implant based on radiographic view), leading to increased reoperation rate [18].
Although systematic reviews have determined survivorship and reoperation rates in the general THA population, examining a younger subset with unique characteristics is needed to develop appropriate surgical indications, inform care planning, and develop monitoring strategies. The financial and economic impact of revision THA is substantially greater than that of primary THA [19], due to longer times of surgery, more expensive prostheses, longer length of stay, and higher rates of complications and burden on the healthcare system [1,20,21]. Studies examining survival rates of THA in younger adults are needed to provide an outlook on the future burden of revision THA. Based on the rising number of primary THA, it is hypothesized that the volume of revision procedures will rapidly increase in the future, which will place an immense burden on future healthcare systems and also raises the question if current clinical standards and treatment strategies have to be reconsidered.
The overall aim of this scoping review is to synthesize evidence regarding THA in younger patients and identify any existing gaps in knowledge. Specifically, the objectives are to 1) summarize the survival, reoperation, and wear rates of THA and 2) identify indications for reoperation following THA, including factors associated with reoperation in individuals who are 55 years of age or younger.
Material and methods
As our overall aim was to provide a detailed overview of studies that examined the survival, reoperation, and wear rates in THA in younger patients, the scoping review methodology best fit our objectives [28]. The framework proposed by Arksey and O'Malley [28] and Levac [29] was used to guide the scoping review methodology. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews guidelines were followed to ensure a high and consistent quality of research reporting [30]. This review's protocol was registered a priori on the Open Science Framework (OSF) (Protocol ID#:osf.io/u4gpn).
Development of research questions
The main concept of interest is THA survival, reoperation, and wear rates, regardless of the implant used or surgical approach in adults aged 55 years or younger who underwent THA. The outcomes of interest were 1) survival, reoperation, and wear rate of THA and 2) reasons for THA reoperation and factors associated with reoperation.
Survivorship of THA is defined by the cumulative incidence of any surgical procedure that involves removal or exchange of an implant (the cup and/or stem or the liner) [22], while reoperation rates are defined as surgical procedures after the primary THA for any reason but do not necessarily involve implant removal. Reoperation reasons can be patient-related, implant-related, and failures related to surgical technique [[23], [24], [25], [26], [27]].
Identifying relevant studies
A health sciences librarian developed and implemented literature searches in Medline, Embase, CINAHL, and Web of Science from 1990 to May 31, 2019. The search dates were chosen to reflect more recent implants and surgical techniques. Our multidisciplinary study members helped conceptualize the search strategy, which was based on the concepts of joint replacement, reoperation, adults 55 years old or younger, with multiple text words and subject headings (eg, Medical Subject Headings) describing each concept. This search strategy was limited to English. The search strategies are detailed in Appendix A.
Selection criteria
Studies were included if 1) the patient group was ≤55 years of age or the cohort reported findings stratified by age groups with a group meeting the age requirement; 2) THA survival, reoperation, or wear rate for any reason was reported; 3) there was a minimum of 20 reoperations reported; and 4) the minimum level III evidence (based on the Oxford Level of Evidence) was attained. Studies of hemiarthroplasty surgical procedures were excluded.
Screening and study selection
Search results were uploaded to the Covidence platform [31]. After removing duplicates, 2 team members independently reviewed the titles and abstracts and applied the inclusion and exclusion criteria. If there were insufficient details to make an informed decision, the article was retrieved for review. To confirm eligibility, 2 team members independently assessed the full-text articles using the same inclusion and exclusion criteria. Any disagreement was resolved through consensus or third-party adjudication.
Data extraction
A standardized data abstraction form was created by the research team. Two team members then used the pretested data abstraction form to abstract data from included full-text articles.
Quality assessment
One reviewer evaluated the quality of selected full-text articles using the Oxford Level of Evidence [32], which is recommended to determine a hierarchy of the best evidence [33]. The Scottish Intercollegiate Guidelines Network guidelines were used to assess study quality through the completion of their cohort checklist, including items such as subject selection, assessment, confounding, and statistical analysis [34].
Summarizing and reporting the findings
Data were organized to report information regarding authors, study design, population characteristics, THA indication, THA surgical characteristics (implant and surgical approach), outcome measures, and tools used to measure the outcome of interest.
Results
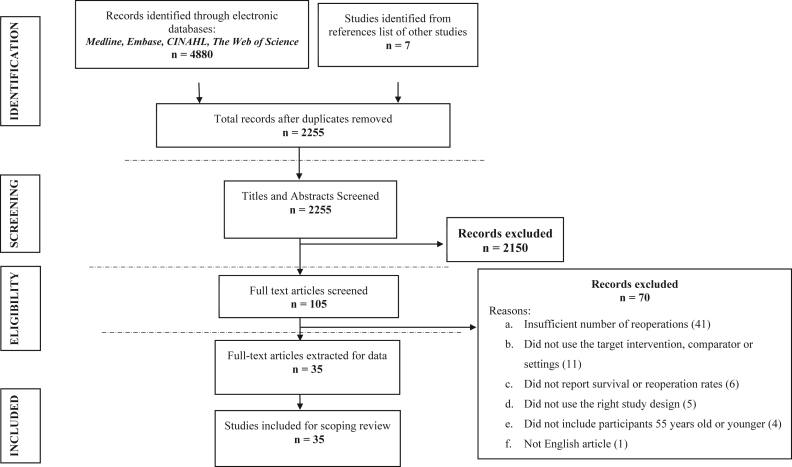
Of the 4887 citations retrieved, 2255 were eligible for screening after deduplication, of which 2150 were excluded based on the title and the abstract. Of the 105 full-text articles assessed, 70 were excluded, leaving 35 studies included in the review [[8], [11], [12], [13], [15], [16], [22], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61]] (Fig. 1).
Figure 1.
PRISMA flow diagram describing identification and selection of studies.
Study characteristics
In 33 of the 35 included studies, 69,219 THAs were performed. Two studies did not report the number of THAs in patients 55 years old or younger. The authors of these studies were contacted by email to request the number of patients of this subgroup, but they did not respond. All included studies were published between 1994 and 2019, with 18 (51.4%) conducted in Europe [8,13,15,16,22,35,37,38,[40], [41], [42],[46], [47], [48], [49], [50], [51],54,56,61,62], 8 (22.9%) conducted in the USA [11,12,36,52,53,55], 4 (11.4%) in Korea [43,45,58,59], and single studies conducted in Australia [44] and New Zealand [39]. All articles were prognostic retrospective articles with level III quality, of which 11 studies used national or international data registries. Four studies used the Finnish Arthroplasty Register, 2 used the nationwide hip arthroplasty registries in Sweden, Norway, Denmark, and Finland; and another 2 studies used the National Joint Registry of England and Wales. The New Zealand Joint Registry, Australian Orthopaedic Association National Joint Replacement Registry, and the Norwegian Arthroplasty Register were used in 1 study.
After assessing the quality of the included studies using the Scottish Intercollegiate Guidelines Network guidelines, 16 (45.7%) articles were classified as good quality [8,11,12,15,16,22,[38], [39], [40], [41], [42], [43], [44],46,56], 16 (45.7%) articles were regarded as fair quality [35,37,45,[48], [49], [50],[52], [53], [54], [55],[57], [58], [59], [60], [61], [62]], and 4 (11.4%) articles were deemed poor quality [13,36,47,51] often due to incomplete reporting or not conducting multivariate analyses (Appendix B, Table B.1).
Cohort characteristics
Different age groupings were used as inclusion criteria. While several studies evaluated patients who were 55 years old or younger (n = 10, 28.6%; 57,401 THAs) [8,15,16,22,[38], [39], [40],46,47,55], others reported findings on patients 50 years of age or younger (n = 10, 28.6%; 1893 THAs) [11,12,37,43,50,51,54,58,59,61]. Ten studies (n = 10) did not report the mean or median age of the included participants; however, an age-related inclusion criterion of 55 years or younger was reported. Of those reporting age, the mean (standard deviation) age of participants was 36.76 (10.39) years. Males comprised 40.8%-100% [12,13,22,40,44,45,[47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62]] of the 22 (62.9%) studies that reported sex distribution (Table 1). Thirty-four (97.1%) studies reported reoperation and/or survival rate [8,[11], [12], [13],15,16,22,[35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62]], while 5 (14.3%) studies reported an annual wear rate of the revised hip arthroplasty components [11,41,43,58,59].
Table 1.
Included study characteristics.
| Author | Year | Country | Data source | Age groups (y) | Sex (% male) |
|---|---|---|---|---|---|
| Registry data | |||||
| Eskelinen et al. [38] | 2005 | Finland | The Finnish Arthroplasty Register | <55 | NR |
| Eskelinen et al. [8] | 2006 | Finland | The Finnish Arthroplasty Register | <55 | NR |
| Eskilenen et al. [16] | 2006 | Finland | The Finnish Arthroplasty Register | <55 | NR |
| Hooper et al. [39] | 2009 | New Zealand | The New Zealand Joint Registry | <55c | NR |
| Makela et al. [22] | 2011 | Finland | The Finnish Arthroplasty Register | 49.7 (16-54)b | 50.5 |
| Bolland et al. [15] | 2012 | England | The National Joint Registry of England and Wales | <55 (55.1-72.7)d | NR |
| McMinn et al. [40] | 2012 | England | The National Joint Registry of England and Wales | <55c | 100 |
| Sedrayken et al. [44] | 2014 | Australia | Australian Orthopaedic Association National Joint Replacement Registry | <20 | 45 |
| Pedersen et al. [47] | 2014 | Scandinavia | The nationwide hip arthroplasty registries in Sweden, Norway, Denmark, and Finland. | 35-55d | 52.1 |
| Tsukanaka et al. [49] | 2016 | Norway | The Norwegian Arthroplasty Register | 17 (11-19)b | 44.1 |
| Halvorsen et al. [56] | 2019 | Denmark, Finland, Norway, Sweden | The Nordic Arthroplasty Register Association (a collaboration between the national joint replacement registers in Denmark, Finland, Norway, and Sweden) | 18 (2.4)a | 47 |
| Hospital/Institutional Data | |||||
| Sochart et al. [41] | 1999 | United Kingdom | Institutional data, Centre for Hip Surgery, Wrightington Hospital, UK | 31.7a | NR |
| Duffy et al. [57] | 2001 | USA | Institutional data, Department of Orthopedics, Mayo Clinic | 32 (17-39)b | 54.2 |
| McAuley et al. [11] | 2004 | USA | Institutional data, Anderson Orthopaedic Research Institute | 40 (16-50)b | NR |
| Gallo et al. [35] | 2008 | Czech Republic | Institutional data, Olomouc, Czech Republic | 46.5 (6.7)a | NR |
| Struders et al. [13] | 2016 | Latvia | Institutional data, Department of Orthopaedic Surgery, Riga Stradins University, | 47.4 (18-77)b | 40.8 |
| Abdel et al. [50] | 2016 | USA | Institutional data, Department of Orthopedics, Mayo Clinic | <50c | 50 |
| Philippot et al. [51] | 2017 | France | Institutional data, Orthopaedic Surgery Unit of the Saint Etienne, University Hospital, France | 41 (18-50)b | 57.9 |
| Swarup et al. [52] | 2017 | USA | A hospital-based registry, Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA | 27.3 (13-35)b | 52.5 |
| Halawi et al. [55] | 2018 | USA | Institutional data, Department of Orthopaedic Surgery, Cleveland Clinic, Cleveland, USA. | 46.9 (7.1)a | 53.7 |
| Swarup et al. [53] | 2018 | USA | Institutional data, Department of Orthopaedic Surgery, Hospital for Special Surgery, New York, USA | 27 (8-35)b | 41.4 |
| Dessyn et al. [54] | 2019 | France | Institutional data, Department of Orthopaedics and Traumatology, St. Marguerite Hospital, France | 42.6 (4)a | 50 |
| Single Surgeon Data | |||||
| Kim et al. [58] | 2011 | Korea | Single-surgeon clinic | 45.1 (21-50)b | 76.4 |
| Suh et al. [45] | 2013 | Korea | Single-surgeon clinic | 46.8 (22-77)b,c | 69.8 |
| Kim et al. [43] | 2014 | Korea | Single-surgeon clinic | 45.6 (11.1)a | NR |
| Kim et al. [59] | 2016 | Korea | Single-surgeon clinic | 47.7 (10.7)a | 73.1 |
| Martin et al. [12] | 2016 | USA | Single-surgeon clinic | <50 | 45 |
| Other Data Sources | |||||
| Stromberg et al. [46] | 1994 | Sweden | National prospective multicenter study data | 47 (31-55)b | NR |
| Dorr et al. [36] | 1994 | USA | NR | 31.1 (16-45)b | NR |
| Emery et al. [37] | 1997 | England | NR | 41 (17-49)b | NR |
| Sochart et al. [42] | 1997 | United Kingdom | NR | 31.7a | NR |
| Chiu et al. [60] | 2001 | Hong Kong | NR | 28.8 (6.2)a | 60.6 |
| Wangen et al. [62] | 2008 | Norway | NR | 25 (15-30)b | 42.9 |
| Girard et al. [48] | 2011 | France | Multicenter trial conducted in 23 French centers specializing in THA for young patients | 19.7 (12-29)b | 52.6 |
| Pakvis et al. [61] | 2011 | The Netherlands | NR | 42.4 (16-50)b | 48.9 |
NR, not reported.
mean with or without slandered deviation.
mean and range.
a study included participants older than 55 y, but only the subgroup aged 55 y or younger was included in the review.
range.
Nearly all studies (n = 33, 94.3%) reported the primary reason for THA. Only 5 (14.3%) studies included participants with a primary diagnosis of OA [8,22,38,40,47], 1 (2.9%) included AVN [52], and another (2.9%) included rheumatoid arthritis [16]. The remaining studies (n = 28, 80%) included cohorts with multiple indications for THA such as degenerative (OA, AVN), inflammatory (inflammatory arthritis, rheumatoid arthritis, ankylosing spondylitis, septic arthritis, autoimmune arthritis, juvenile inflammatory arthritis), developmental (dysplastic hip, slipped capital femoral epiphysis, Legg-Calve-Perthes disease), post-traumatic, oncologic, and neurologic diseases [[11], [12], [13],[35], [36], [37],[41], [42], [43], [44], [45], [46],[48], [49], [50], [51],[53], [54], [55], [56], [57], [58], [59], [60], [61], [62]] (Table 2).
Table 2.
Total hip arthroplasty primary diagnosis and reasons for reoperation.
| Author | Year | Diagnosis and percentage of each diagnosis | Reason for revisions |
|---|---|---|---|
| Dorr et al. [36] | 1994 | Osteonecrosis Osteoarthritis Inflammatory collagen disease |
Aseptic loosening (100%, n = 33) |
| Stromberg et al. [46] | 1994 | Not rheumatoid | Aseptic loosening |
| Emery et al. [37] | 1997 | Osteoarthritis Rheumatoid arthritis Dysplastic hip Osteoarthritis Hip disease in childhood |
Mainly for aseptic loosening |
| Sochart et al. [42] | 1997 | Rheumatoid arthritis (44.2%, n = 100) Degenerative osteoarthrosis (29.2%, n = 66) Congenital hip dislocation (26.5%, n = 60) |
Aseptic loosening Excessive wear Broken femoral component |
| Sochart et al. [41] | 1999 | Rheumatoid arthritis (37%, n = 87) Degenerative arthrosis (25.1%, n = 59) Congenital dislocation the hip (24.3%, n = 57) Ankylosing spondylitis (13.6%, n = 32) |
Implant fracture (3%, n = 8) Dislocation with marked acetabular wear (1.3%, n = 3) |
| Chiu et al. [60] | 2001 | Ankylosing spondylitis (44.7%) AVN (40.4%) Rheumatoid arthritis (16.4%) Juvenile chronic arthritis (4.3%) Post-traumatic osteoarthritis (2.2%) Hemophilia (2.2%) |
Infection Migration of acetabular component Instability Femoral component loosening |
| Duffy et al. [57] | 2001 | Developmental dysplasia (36.1%) Osteonecrosis of femoral head (19.5%) Post-traumatic osteoarthritis (18.1%) Rheumatoid arthritis (8.3%) Ankylosing spondylitis (8.3%) Degenerative joint disease (2.7%) Psoriatic arthritis (2.7%) Reiter's syndrome (1.4%) |
Aseptic failure (91.7%) Infection (8.3%) |
| McAuley et al. [11] | 2004 | Osteoarthritis (44%, n = 249) Developmental dysplasia (20%, n = 109) Osteonecrosis (20%, n = 111) Rheumatoid arthritis (9%, n = 53) Fracture (7%, n = 39) |
Any reason |
| Eskelinen et al. [38] | 2005 | Primary osteoarthritis | Aseptic loosening (82%, n = 581) Fracture of the implant (3%, n = 21) Infection (2.7%, n = 19) Prosthesis dislocation (2.7%, n = 19) Malposition of the prosthesis (2.3%, n = 16) Periprosthetic fracture (1.1%, n = 8) Other miscellaneous reasons (6.3%, n = 45) |
| Eskelinen et al. [8] | 2006 | Primary osteoarthritis | Aseptic loosening (range from 0.2%-23%) Infection (range from 0.2%-2.4%) Dislocation (range from 0.7%-12%) Malposition (range from 0.3%-1.6%) Fracture of stem (range from 0.6%-3%) Fracture of bone (range from 0.1%-0.9%) Other reasons for cup reoperation including exchange of liner (range from 0.6%-15%) |
| Eskilenen et al. [16] | 2006 | Rheumatoid arthritis | Aseptic loosening (82%) Prosthesis dislocation (3.3%) Infection (2.8%) Periprosthetic fracture (1.8%) Fracture of the stem (1.2%) Malposition of the prosthesis (1.0%) Other, miscellaneous reasons (including exchange of liner) (8.3%) |
| Wangen et al. [62] | 2008 | Secondary osteoarthrosis due to congenital dislocation (54.6%) AVN (13.6%) Coxitis (9.1%) Acetabular fractures (9.1%) Calve-Legg-Perthes disease (6.8%) Epiphyseal dysplasia (4.6%) Chondrodystrophia (2.3%) |
Loosening (58.3%) Polyethylene wear (29.2%) Repeated dislocations (12.5%) |
| Gallo et al. [35] | 2008 | Osteoarthritis (44%), Dysplastic hip (40%) Traumatic hip (7%) AVN Inflammatory arthritis Slipped capital femoral epiphysis |
Osteolysis (57%) Cup loosening (25.5%) Periprosthetic fracture (7.8%) Instability (5.9%) Stem loosening (2%) Deep sepsis (2%) |
| Hooper et al. [39] | 2009 | NR | Loosening acetabular component Loosening femoral Component Dislocation Deep infection |
| Makela et al. [22] | 2011 | Primary osteoarthritis | Aseptic loosening (46.2%, n = 232) Dislocation (5.1%, n = 46) Malposition (4.8%, n = 24) Fracture of the prosthesis (4.4%, n = 22) Infection (3.8%, n = 19) Periprosthetic fracture (3%, n = 15) Other reasons (including, liner revisions due to excessive wear) (30.7%, n = 154) |
| Girard et al. [48] | 2011 | AVN (25.4%, n = 228) Inflammatory disease (20.3%, n = 182) Pediatric disease (18.5%, n = 166) Septic sequelae (8.6%, n = 77) Neurologic disease (6.6%, n = 59) Primary osteoarthritis (6.1%, n = 55) |
Aseptic loosening (51%, n = 40) Wear (24%, n = 19) Infection (8%, n = 6) Osteolysis (7%, n = 5) Recurrent dislocation (6%, n = 4) Implant breakage (4%, n = 3) |
| Pakvis et al. [61] | 2011 | Primary osteoarthritis (30.4%) Hip dysplasia (24.1%) Rheumatoid disease (18.4%) Trauma (10.1%) Other causes (10.1%) Osteonecrosis (8.2%) |
Wear and osteolysis (63.6%) Trauma (18.2%) Aseptic loosening (9.1%) Malposition cup (9.1%) |
| Kim et al. [58] | 2011 | Osteonecrosis (66.2%) Osteoarthritis (14.0%) Childhood pyogenic arthritis (11.5%) Ankylosing spondylitis (3.2%) Multiple epiphyseal dysplasia (2.5%) Developmental dysplasia (1.9%) Rheumatoid arthritis (0.6%) |
Polyethylene wear and osteolysis Recurrent dislocation Aseptic loosening Infection |
| Bolland et al. [15] | 2012 | NR | Aseptic loosening Lysis Infection Periprosthetic fracture Pain Malalignment Dislocation Poly wear Dissociation liner Implant fracture Mismatch |
| McMinn et al. [40] | 2012 | Osteoarthritis | Any reason |
| Suh et al. [45] | 2013 | AVN Osteoarthritis Dysplastic hip Trauma Post-septic hip |
Aseptic loosening of the femoral stem |
| Kim et al. [43] | 2014 | Osteonecrosis Dysplastic hip Osteoarthritis Septic arthritis Post-traumatic arthritis |
Aseptic loosening |
| Sedrayken et al. [44] | 2014 | Osteonecrosis (29%) Osteoarthritis (28%) Autoimmune arthritis (15%) Various types of dysplasia (12%) Bone tumor (9%) |
First reoperation for any reason: Loosening and/or osteolysis Prosthesis dislocation Infection |
| Pedersen et al. [47] | 2014 | Primary osteoarthritis | Aseptic loosening (53.4%, n = 1290) Unspecified (17.2%, n = 415) Dislocation (11.9%, n = 288) Deep infection (9.1%, n = 219) Periprosthetic fracture (3.8%, n = 91) Pain only (3.2%, n = 78) |
| Kim et al. [59] | 2016 | Osteonecrosis (57%) Developmental dysplastic hip (20%) Osteoarthritis (13%) Osteoarthritis secondary to childhood sepsis (7%) Multiple epiphyseal dysplasia (3%) |
Polyethylene wear and osteolysis Recurrent dislocation Aseptic loosening Infection |
| Martin et al. [12] | 2016 | Degenerative arthrosis Post-traumatic arthritis Rheumatoid arthritis Dysplastic hip |
Aseptic loosening |
| Struders et al. [13] | 2016 | Osteoarthritis Dysplastic hip AVN Fracture Rheumatoid arthritis |
Any reason Wear/aseptic loosening (54.2%, n = 13) Wear (12.5%, n = 3) Infection (4.2%, n = 1) Malpositioning cup (4.2%, n = 1) Femoral head fracture (4.2%, n = 1) |
| Tsukanaka et al. [49] | 2016 | Pediatric disease (40.9%, n = 54) Systemic inflammatory disease (34.1%, n = 45) sequelae of trauma (8.3%, n = 11) sequelae of infection (5.3%, n = 7) |
Aseptic loosening (44.9%, n = 31) Wear (20.3%, n = 14) Infection (11.6%, n = 8) Osteolysis (8.7%, n = 6) Dislocation (5.8%, n = 4) Pain only (1.5%, n = 1) 2-stage reoperation (1.5%, n = 1) Fracture (1.4%, n = 1) Other (4.3%, n = 3) |
| Abdel et al. [50] | 2016 | Osteoarthritis (72.1%, n = 1441) Rheumatoid arthritis (9.9%, n = 198) Developmental dysplasia (8.3%, n = 165) post-traumatic (7.3%, n = 145) Others (2.6%, n = 51) |
Any reason including: aseptic loosening instability infection |
| Philippot et al. [51] | 2017 | Dysplastic hip (27%) Post-traumatic hip OA (23%) AVN (23%) slipped capital femoral epiphysis (12%) Osteoarthritis (4%) Neurogenic osteoma (1%) |
Aseptic loosening (13.9%, n = 19) Intraprostatic dislocation (10.9%, n = 15) Femoral loosening (1.46%, n = 2) Acetabular loosening (0.79%, n = 1) Femoral stem fracture (0.79%, n = 1) Infection (0.79%, n = 1) |
| Swarup et al. [52] | 2017 | AVN | Any reasons Aseptic loosening (58%, n = 22) other reasons included: polyethylene wear periprosthetic fracture instability pain infection |
| Halawi et al. [55] | 2018 | Primary osteoarthritis (49.7%) AVN (23.7%) Dysplastic hip (14.3%) Slipped capital femoral epiphysis (5.5%) Posttraumatic arthritis (3.7%) Inflammatory arthritis (3.1%) |
Periprosthetic infection (4.9%) Aseptic loosening of the acetabular component (4.6%) Periprosthetic fractures (1.5%) Aseptic loosening of the femoral component (0.9%) |
| Swarup et al. [53] | 2018 | AVN of the hip (34%) Dysplastic hip (15%) Juvenile inflammatory arthritis (14%) Post-traumatic arthritis (11%). |
Any reason |
| Dessyn et al. [54] | 2019 | Secondary osteoarthritis (49.4%, n = 115) Developmental dysplasia of the hip (37.8%, n = 88) AVN (33%, n = 77) Primary osteoarthritis (11.6%, n = 41) Post-traumatic (11.6%, n = 27) |
13 were isolated cup revisions: Loosening (3%, n = 7) Isolated polyethylene wear (2.6%, n = 6) Deep infection (2.6%, n = 6) Aseptic loosening of both components (1.3, n = 3) Chronic instability (0.4%, n = 1) |
| Halvorsen et al. [56] | 2019 | Pediatric (33%) Systemic inflammatory disease (23%) AVN (12%) Hip fracture (6.5%) Osteoarthritis (4.1%) Other (22%) |
Aseptic loosening (52%, n = 61) Dislocation (9.3%, n = 11) Deep infection (5.1%, n = 6) Periprosthetic fracture (2.5%, n = 3) Pain only (0.8%, n = 1) Other (31%, n = 36) |
NR, not reported; AVN, avascular necrosis.
Surgical characteristics
Of those few studies (n = 7, 20%) that reported surgeon characteristics [12,35,43,45,55,58,59], most were performed by a single orthopaedic surgeon (n = 5, 14.3%) [12,43,45,58,59]. Nineteen (54.3%) studies reported the THA surgical approach, with 7 studies reporting multiple surgical approaches [11,13,[55], [56], [57],60,62] and 12 studies using a single approach [12,35,37,41,42,45,50,54,59,61]. The most commonly used surgical approaches were the anterolateral (n = 7, 20%) [11,13,35,54,55,57,60] and lateral (n = 6, 17.1%) [11,41,42,50,55,62] approaches (Appendix B, Table B.2). Thirty-one studies reported the types of THA implants and/or fixation methods [[11], [12], [13],15,16,22,[35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45],47,[49], [50], [51],[53], [54], [55], [56], [57], [58], [59], [60], [61], [62]] (Appendix B, Table B.2) with wide variety of THA implants and fixation methods.
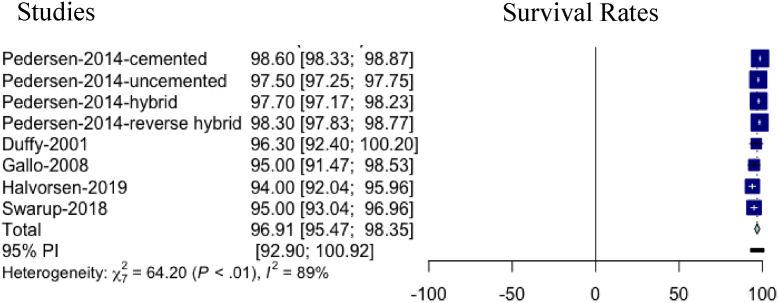
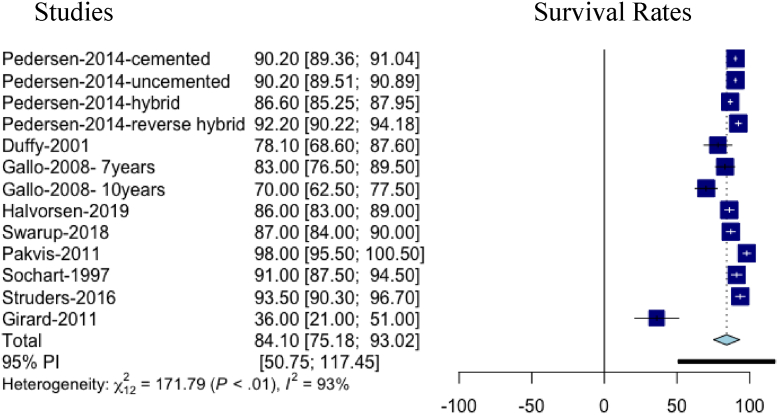
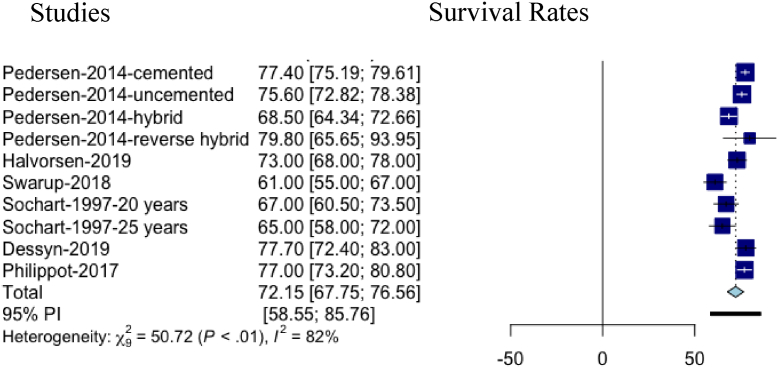
Survival rate of hip arthroplasty implants
Of 27 (77.1%) studies that reported THA survival rates [8,11,13,16,22,35,37,38,42,43,[45], [46], [47], [48], [49],[51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61]], the majority (21, 60%) reported the survival rate for at least 2 time points [8,11,13,16,22,35,37,38,42,46,47,[52], [53], [54],[56], [57], [58], [59], [60], [61]] and 6 (17.1%) studies reported the survival rate at a single time point [43,45,48,49,51,55]. Survival rates were reported at 5 (n = 11, 31.4%), 10 (n = 21, 60%), and 15-20 (15, 42, 9%) years (Table 3). The survival rates of primary THAs ranged from 90% to 100% at 5 years and from 62% to 98% at 10 years and were expectedly lower at 20 years (ranged from 60.4% to 77.7%) (Table 3). The survival rates of primary THAs conducted after 2010 appear to be higher than rates of THAs conducted between 1990-2000 and 2001-2010 in 10, 15, or 20 years (Table 3). This may reflect the modern techniques and implants used after 2010. The primary indications of THA appeared to impact the survival rates. A study showed that a primary diagnosis of AVN is associated with lower survival than other primary diagnoses (P = .001) [59]. Appendix C shows forest plots of survival rates at 5, 10, and 20 years of follow-up.
Table 3.
Total hip arthroplasty survival and reoperation rates.
| Authors, y | Follow-up duration (y) | Index procedure (n) | Reoperation % (n) | Survivorship (y) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2-4 | 5 s | 7 | 10 s | 12-14 | 15-20 s | 25+ | ||||
| Dorr et al., 1994 [36] | 16.2 (13-20)b | 49 | 67% (n = 33) | |||||||
| Stromberg et al., 1994 [46] a | 10 (8-13)b | 59 | %86 | 48% | ||||||
| Emery et al., 1997 [37] | 13 (0.25- 21)b | 46 | 39% | 90% | 68% | |||||
| Sochart et al., 1997 [42] | 19.7 (2-30.1)b | 226 | 91% (CI, 88-95) | 67% (CI, 61-74) | 65% (CI, 58-72) | |||||
| Summary of studies between 1990-2000c | 10-19.7 | 46-226 | 39%-67% | 90%-91% | 67%-68% | 58%-72% | ||||
| Chiu et al., 2001 [60] | 14.9 (6.9-21.1)b | 47 | 63% (30) | 97.8% | 84.5% | 27% | ||||
| Duffy et al., 2001 [57] | 10.3 (10-14)d | 82 | 29.3 (24) | 96.3% (CI, 92.2-100) | 78.1% (CI, 69-88) | |||||
| McAuley et al., 2004 [11] | 6.92 (0-19)b | 561 | 97.40% | 88.76% | 60.4% | |||||
| Eskelinen et al., 2005 [38] | 6.2 (0-22)d | 4661 | 15% (n = 709) | Stem 88% (CI, 85-91) to 95% (91-99)c Cup 83% (CI, 80-86) to 95% (CI, 91-99)c |
Stem 80% (CI, 75-84) to 91% (CI, 89-93)c Cup87% (CI, 85-90) to 93% (CI, 88-98)c |
|||||
| Eskelinen et al., 2006 [8] | 5-15c | 5607 | Stem reoperation: 1.5%-12% Cups reoperation: 0.4-28% |
90% (CI, 84-95) to 100% (99-100)c | 62% (CI, 46-79) to 86% (CI, 80-93)c | 60% (CI, 50-70) to 74% (CI, 69-79)c | Stems only: 88% (CI, 82-95) to 92% (CI, 90-94)c | |||
| Eskilenen et al., 2006 [16] | 9.7 (0-24)d | 2557 | 19% (n = 605) | 86% (CI, 76-95) to 93% (CI, 91-95)c | 85% (CI, 82-89) to 87% (CI, 84-90)c | 65% (CI, 58-72) to 74% (CI, 70-77)c | ||||
| Wangen et al., 2008 [62] | 13 (10-16)b | 49 | 49.0% (24) | |||||||
| Gallo et al., 2008 [35] | 9.7 (0.02-12.44)b | 127 | 95% (CI, 92-99) | %83 (CI, 76-89) | %70 (CI 63-78) | 55 (CI, 44-66) | ||||
| Hooper et al., 2009 [39] | NR | 6430 | 3% (n = 193) | |||||||
| Summary of studies between 2001-2010c | 5-15 | 47-6430 | 3%-63% | 90%-100% | 83%-95% | 62%-93% | 55%-74% | 27%-92% | ||
| Makela et al., 2011 [22] | 0-20c | 3668 | 13.7% (n = 502) | 95% (CI, 91-99) to 97% (CI, 95-99)c | 79% (CI, 62-96) to 81% (CI, 74-88)c | 58% (CI, 52-64) to 71% (CI, 62-80)c | ||||
| Girard et al., 2011 [48] a | 1-15c | 77 | 55% (n = 42) | 36% (CI, 21-51) | ||||||
| Pakvis et al., 2011 [61] | 13.2 (10-18)b | 158 | Acetabular 14% (22) | 98% (95% CI, 95-100) | 80% (95% CI, 72-89) | |||||
| Kim et al., 2011 [58] | 18.4 (16-19)b | 219 | Acetabular component: cemented, 13% (14), uncemented 16% (18) Femoral component: cemented, 3% (3), uncemented, 4% (4) |
Hybrid group, 93.6% Cementless group, 93.6%. |
Acetabular component: cemented 87 (95% CI, 80-93), uncemented 84 (95% CI, 78-92) Femoral component: cemented, 97 (95% CI, 91-100), uncemented, 96 (95% CI, 93-100) |
|||||
| Bolland et al., 2012 [15] | 3 | NR | Cemented THA: 1.6 (CI, 1.0-2.2), Uncemented THA: 2.1 (CI, 1.7-2.5), Hybrid THA: 1.6 (CI, 1.0-2.2), Resurfacing THA 2.8 (CI, 2.4-3.2) |
|||||||
| McMinn et al., 2012 [40] | Cemented THA, 3.6 (0.001-9.7)d Uncemented THA, 2.6 (range 0.001-8.6)d | 11,483 | 1.7% (n = 195) | |||||||
| Suh et al., 2013 [45] | 15.5 (14-19.5)b | 43 | 65.2% | |||||||
| Kim et al., 2014 [43] | 28.4, (27-29)b | 88 | Acetabulum 66% (CI, 61-91) Femur 90% (CI, 85-100) |
|||||||
| Sedrayken et al., 2014 [44] | 5 | 297 | In patients <21 y, 4.5% (CI, 2.2-8.9). In patients 21-30 y, 5.4% (CI, 3.9-7.3) | |||||||
| Pedersen et al., 2014 [47] | 2-16c | 29,558 | 16-y follow-up: 8.2% (n = 2413) 2-y follow-up: 2.0% (n = 590) |
Cemented THA 98.6 (SE, 0.14) Uncemented THA 97.5 (SE, 0.13) Hybrid THA 97.7 (SE, 0.27) Reverse hybrid THA 98.3 (SE, 0.24) |
Cemented THA 90.2 (SE, 0.43) Uncemented THA 90.2 (SE, 0.35) Hybrid THA 86.6 (SE, 0.69) Reverse hybrid THA 92.2 (SE, 1.01) |
Cemented THA 77.4 (SE, 1.13) Uncemented THA 75.6 (SE, 1.42) Hybrid THA 68.5 (SE, 2.12) Reverse hybrid THA 79.8 (SE, 7.22) |
||||
| Kim et al., 2016 [59] | 26.1 (25-27)b | 342 | Acetabular component: cemented, 21% (36), uncemented 22% (38) Femoral component: cemented, 4% (7), uncemented, 5% (8) |
Acetabular component: cemented 79 (95% CI, 75-94), uncemented 78 (95% CI, 75-94) Femoral component: cemented, 96 (95% CI, 91-100), uncemented, 95 (95% CI, 92-100) |
||||||
| Martin et al., 2016 [12] | ≥20 | 109 | 19% (CI, 13-27), (n = 21) | |||||||
| Struders et al., 2016 [13] | 12.6 (10.9-15.8)b | 311 | 93.5% (CI, 89.6-96) | 89.6 (CI, 84.2-93.2) | ||||||
| Tsukanaka et al., 2016 [49] | 14 (3-26)b | 132 | 30% (n = 39) | 70% | ||||||
| Abdel et al., 2016 [50] | 40 | NR | 30-y follow-up: 35% (CI, 28-42) | |||||||
| Philippot et al., 2017 [51] | 21.9 (3.3-30.9)b | 137 | 32.1% (n = 44) | 77% (CI 74.4-82) | ||||||
| Swarup et al., 2017 [52] | 14 (2-27)b | 204 | 21.1% (n = 43) | 96% | 85.6% | 15-y follow-up: 76.7% 20-y follow-up: 66.3% |
||||
| Halawi et al., 2018 [55] | 7.7 (0-10.3)b | 378 | 9.2% (n = 35) | 90.8% | ||||||
| Swarup et al., 2018 [53] | 14 (2-29.7)b | 400 | 23% (n = 128) | 95% (CI, 93-97) | 87% (CI, 84-90) | 61% (CI, 55-67) | ||||
| Dessyn et al., 2019 [54] | 20 (15-27)b | 233 | 10.8% (n = 23) | 77.7% (CI, 72.4-83) | Stem reoperation for aseptic loosening: 94.5% (CI, 91.7-97.3) | |||||
| Halvorsen et al., 2019 [56] | 5-20c | 881 | 13% (n = 118) | 94% (CI, 92-96) | 86% (CI, 83-89) | 73% (CI, 68-78) | ||||
| Summary of studies between 2011 and presentc | 2-28.4 | 43-29,558 | 2%-35% | 97.5%-98.6% | 90.8%-97% | 70%-98% | 80%-89.6% | 58%-97% | 66%-96% | |
NR, not reported; CI, 95% confidence interval; SE, standard error.
studies that examined rerevision of total hip arthroplasty.
mean and range.
range.
median and range.
Reoperation rate
Twenty-nine (82.9%) studies reported reoperation rates at different follow-up periods ranging from 2 to 40 years, with the majority occurring within 10 years [8,12,15,16,22,[36], [37], [38], [39], [40],44,[47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62]]. The THA reoperation rate increased over time with rates at ≤ 5 years ranging from 1.6% to 5.4% as compared to rates from 10 to 20 years ranging from 8.2% to 67% (Table 3). The lowest reoperation rates were in studies conducted after 2010 (range: 2%-35%) as compared to reoperation rates reported in studies between 1990 and 2000 (39% to 67%) and between 2001 and 2010 (3% to 63%) (Table 3). Primary indications of THA appeared to impact the reoperation rates. Two studies showed that individuals with a pre-THA diagnosis of DDH had a higher reoperation rate than those with other diagnoses [35].
Wear rate
Five (14.3%) studies reported the annual wear rate of the hip arthroplasty components, which ranged from 0.19 to 0.29 mm for the revised components and 0.09 to 0.14 mm for the surviving components [11,41,43,58,59]. In the study by Sochart et al., the average annual wear rate of revised components was 0.19 mm, more than twice that of the 0.09 mm for surviving original components (P = .004) [41]. No statistically significant differences in annual wear rates were reported with sex (male: 0.12 mm, female: 0.11 mm per year; P > .5) or age. McAuley et al. reported that the annual wear rate among the revised hips was 0.29 mm (±0.18) and that among the unrevised hips was 0.14 mm (±0.12) (P < .001) [11]. Kim et al. examined polyethylene wear rates in 3 studies and showed that the mean annual rate of linear wear of the polyethylene liner was 0.18 ± 0.03 mm [43]. There were no significant differences in the annual wear rate between cemented (0.210-0.212 mm/y) and cementless THA (0.120-0.130 mm/y) [58,59].
Indications for reoperation
The most common indications of reoperation were aseptic loosening of femoral or acetabular components, osteolysis, infection, periprosthetic fracture, malalignment, dislocation, wear, implant fracture, and malposition (Table 3). Six (17.1%) studies included only THA reoperations due to aseptic loosening of hip implants [12,36,37,43,45,46], and 29 (82.9%) studies included hip reoperation due to several or any reasons [8,11,13,15,16,22,35,[38], [39], [40], [41], [42],44,[47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62]].
Although all studies included young cohorts, only 8 of the 29 studies that addressed reoperation specifically examined the effect of age on the reoperation rates using subgroup comparisons or risk stratification [16,36,38,39,45,48,50,53], and age categories varied among the studies. For example, Eskelinen et al. [16] concluded that THA candidates who were 46 years old or younger had a 1.2-fold (95% CI: 1.0-1.5; P = .03) increased risk of reoperation compared to older patients aged between 46 and 54 years. Similarly, Dorr et al. [36] found that the reoperation rate of individuals under 30 years of age was 82%, while it was 56% for those who were 30-45 years of age. Additionally, 3 studies (10%) tested the differences in THA survival rates in different age groups [43,52,53]. The 3 studies found that younger age groups had shorter implant survivals. In the study by Kim et al., the rate of survival of THA implant at 28.4 years was 53% (CI: 0.48-0.89) in patients younger than 30 years and 79% (CI: 0.71-0.93) in patients older than 30 years [43]. In 2 studies conducted by Swarup et al., patients under the age of 25 years at the time of primary THA had worse implant survival than older patients [52,53].
No consistent finding was reported as to whether survival and reoperation rates were higher in males or females. Three studies concluded that the reoperation rate was significantly higher in males [16,45,50], while 2 other studies found a higher reoperation rate in females [38,53]. Kim et al. reported that the rate of survival of the THA implant was 55% (CI: 50%-89%) in male patients and 77% (CI: 71%-95%) in female patients [43]. Similarly, Chiu et al. also reported a lower survival rate of the femoral component in males (P = .011) [60]. However, the other 2 studies found that the survival rates were lower in female participants [52,53].
Discussion
Younger patients with THA had reoperations increased over time, with THA survival rates higher at 5 years (90% to 100%) than at 20-year follow-up (60.4% to 77.7%). Similar to older cohorts [63], the most common causes of THA reoperation were aseptic loosening of hip implants, osteolysis, wear, and infection. Conflicting results were seen with survivorship and reoperation rates of males and females across studies. Although data were limited, DDH or AVN may have lower survival rates [35,60].
A recent systematic review by Mei et al. assessed THA implant selection and long-term survivorship in patients younger than 55 years [64]. They searched 2 electronic databases and included 32 studies (3219 THAs) [64], of which most were evidence level IV (29 studies) and had a small number of reoperations (0-19 reoperations) (22 studies). Mei et al. reported higher THA survival rates at 5 and 10 years (95%-100% and 78.1%-100%, respectively) and lower reoperation rates (0%-63.8%) than our review and did not report THA wear rate. Their higher survival and lower reoperation rates could be explained by the lower number of the studies, participants, and lower quality and level of evidence of the included studies.
A recent systematic review and meta-analysis of THA survival rate at 15, 20, and 25 years in older adults (mean age range: 57,·9-74 years; n = 58,932) reported THA survival rates at 15 (87.9%, 95% CI: 87.2-88.5) and 20 years (78.9%, 95% CI: 77·9-80.0) that were substantially higher than the rates we reported (62.9% and 60.4%) [6]. In an older cohort (mean age: 69 years; n = 63,158), Bayliss et al. reported 20-year survival of 85.0% (95% CI: 83·2-86.6) with a maximum follow-up of 20 years in older adults [18]. A higher reoperation and lower survival rates in the younger patient population may be related to more complicated primary surgeries related to congenital, developmental, or traumatic anatomical abnormalities causing the early OA. Another reason for higher reoperation rates could be the higher demands of younger population, leading to wear and secondary loosening, which may affect the longevity of THA [[8], [9], [10], [11],65,66]. To optimize surgical outcomes of THA in patients who are 55 years of age or younger, more research is needed to determine a tailored THA care path (surgical technique, implants, or rehabilitation protocols) for this specific age group.
Although surgeon characteristics are important determinants of THA survival and reoperation rates, inconsistency in reporting surgical characteristics of THA was seen across all included studies. For example, descriptions of orthopaedic surgeons who performed the THA or surgical approach were not consistently included. Surgeons with low volumes (<35 THA per year) had an increased risk for hip dislocation and early reoperation when compared to higher volume surgeons [67]. Other inconsistencies of surgical characteristics included implant types and size, fixation mechanisms, and bearing surface.
A particular strength of this review included the rigor used to search and review a broad realm of evidence [17,68,69]. In comparison to systematic review methodology [64], the broader scoping review framework facilitated the development of a comprehensive summary of THA reoperation rate and reasons for reoperation to help clinicians and patients make informed decisions about THA in younger age groups [17].
Our scoping review has some limitations. As the majority of data were taken from registry data, the data were often limited to basic demographic information such as age and sex and did not evaluate pain, functional measures, or physical activities. Most of the included studies were conducted in Europe and USA. External validity to other populations living in other geographical areas is uncertain because of different healthcare systems and potentially different prostheses. These limitations emphasize the need for future research to improve the reliability and survivorship of THA [4,70].
Findings from this review provide researchers, clinicians, and policymakers with a synthesis of the literature and the gaps in reporting of THA reoperation and survival rates in young patients. With the projected increase of THA in a younger population [24], reoperation and survival rate summaries will provide synthesized evidence that can be integrated into surgeons' and patients' discussion about THA timing. Consequently, using key strategies, such as prevention programs and the use of nonoperative treatment options to delay primary THA should be considered more frequently by researchers and healthcare providers (despite the limitations of patients with OA) [65,71].
Information on reoperation rates and reasons following THAs draws attention to the important problem of rapidly growing need for revision THA and its associated challenges, which will certainly impact clinical care and add financial strain on healthcare systems. As the longevity of revision THAs is far inferior to primary total knee arthroplasty, a growing population of multiple-revised patients has to be expected in the future. It is necessary for policymakers to plan appropriate interventions in a timely manner and for the development of effective healthcare policy.
Conclusions
The primary THA survival rates appear to be lower in younger individuals than the rates reported in older age groups. Aseptic loosening of hip implants, osteolysis, wear, and infection were the most frequent reasons for the reoperation. THA with a primary diagnosis of DDH or AVN had a higher reoperation and lower survival rate than other primary diagnoses. Because of the inconsistencies reported, consensus reporting guideline is warranted to standardize arthroplasty research reports and allow for robust statistical data synthesis studies, development of a higher level of research evidence, and optimize evidence-based orthopaedic care.
Funding
Ahmed Negm was funded by Alberta Innovates Postdoctoral Fellowship.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2019.12.004.
Appendix A. Supplementary Data
Appendix A. Search Strategy
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
-
1.
hip joint/ or hip/
-
2.
“prostheses and implants”/ or joint prosthesis/
-
3.
arthroplasty/ or arthroplasty, replacement/
-
4.
1 and (2 or 3)
-
5.
hip prosthesis/
-
6.
arthroplasty, replacement, hip/
-
7.
((total or complete) adj6 (hip or hips) adj6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)).mp.
-
8.
(((total or complete) adj6 joint adj6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)) and (hip or hips)).mp.
-
9.
(THA or TJA or TJR or THR).ti.
-
10.
or/4-9
-
11.
Reoperation/
-
12.
Prosthesis Failure/
-
13.
(fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗).mp.
-
14.
or/11-13
-
15.
14 and 10
-
16.
((predict∗ or rate or risk) adj6 (fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗)).mp.
-
17.
(survival adj2 rate).mp.
-
18.
(failure∗ adj2 analysis).mp.
-
19.
(survival or non-survival or failure or prognos∗ or predict∗ or risk factor∗).ti.
-
20.
prognosis/
-
21.
survival/ or survival rate/ or survival analysis/
-
22.
or/16-21
-
23.
15 and 22
-
24.
limit 23 to yr = “1990 -Current”
-
25.
Epidemiologic studies/
-
26.
exp case control studies/
-
27.
exp cohort studies/
-
28.
Case control.tw.
-
29.
(cohort adj (study or studies)).tw.
-
30.
Cohort analy$.tw.
-
31.
(Follow up adj (study or studies)).tw.
-
32.
(long-term or longterm).ti.
-
33.
(observational adj (study or studies)).tw.
-
34.
(Longitudinal or prospective or Retrospective or Cross sectional).mp.
-
35.
Cross-sectional studies/
-
36.
(regist∗ or matched-pair∗ or matched pair∗).mp.
-
37.
or/25-36
-
38.
case reports/
-
39.
((case not (case control or case-control or case series or case-series or case-cohort or case cohort or case-crossover)) adj4 (study or report∗)).tw.
-
40.
((year∗ old or month∗ old or day∗ old or yr∗ old or y old) adj3 (child or woman or man or girl or boy or baby)).ab.
-
41.
case report∗.jw.
-
42.
or/38-41
-
43.
37 not 42
-
44.
24 and 43
-
45.
∗arthroplasty, replacement, hip/ or ∗arthroplasty, replacement, knee/
-
46.
(THA or TJA or TJR or THR or cruciate retaining or cruciate substituting or ((hip or hips or joint or regist∗) and (total or arthroplast∗ or prosthe∗ or replace∗ or implant∗))).ti.
-
47.
44 and (46 or 45)
-
48.
(resurfacing or hemiarthroplast∗ or hemi arthroplast∗).ti.
-
49.
47 not 48
-
50.
limit 49 to ed = 20131206-20160608
-
51.
49 and (201312∗ or 2014∗ or 2015∗ or 2016∗).dc.
-
52.
50 or 51
Embase
-
1.
total hip prosthesis/
-
2.
hip prosthesis/
-
3.
hip arthroplasty/
-
4.
(arthroplasty/ or joint prosthesis/) and hip/
-
5.
((total or complete) adj6 (hip or hips) adj6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)).mp.
-
6.
(((total or complete) adj6 joint adj6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)) and (hip or hips)).mp.
-
7.
(THA or TJA or TJR or THR).ti.
-
8.
or/1-7
-
9.
reoperation/
-
10.
exp prosthesis failure/
-
11.
(fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗).mp.
-
12.
or/9-11
-
13.
((predict∗ or rate or risk) adj6 (fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗)).mp.
-
14.
(survival adj2 rate).mp.
-
15.
(failure∗ adj2 analysis).mp.
-
16.
(survival or non-survival or failure or prognos∗ or predict∗ or risk factor∗).ti.
-
17.
prognosis/
-
18.
long term survival/ or event free survival/ or survival prediction/ or survival factor/ or survival/ or failure free survival/ or survival rate/
-
19.
or/13-18
-
20.
8 and 12 and 19
-
21.
limit 20 to yr = “1990 -Current”
-
22.
clinical study/
-
23.
exp case control study/
-
24.
family study/
-
25.
longitudinal study/
-
26.
retrospective study/
-
27.
prospective study/
-
28.
cohort analysis/
-
29.
(Cohort adj (study or studies)).mp.
-
30.
(Case control adj (study or studies)).tw.
-
31.
(follow up adj (study or studies)).tw.
-
32.
(observational adj (study or studies)).tw.
-
33.
(epidemiologic$ adj (study or studies)).tw.
-
34.
(cross sectional adj (study or studies)).tw.
-
35.
(long-term or longterm).ti.
-
36.
regist∗.mp.
-
37.
matched pair∗.tw.
-
38.
or/22-27,28-37
-
39.
case report/
-
40.
((case not (case-crossover or case control or case-control or case series or case-series or case-cohort or case cohort)) adj4 (study or report∗)).tw.
-
41.
((year∗ old or month∗ old or day∗ old or yr∗ old or y old) adj3 (child or woman or man or girl or boy or baby)).ab.
-
42.
case report∗.jw.
-
43.
or/39-42
-
44.
21 not 43
-
45.
38 and 44
-
46.
(resurfacing or hemiarthroplast∗ or hemi arthroplast∗).ti.
-
47.
45 not 46
-
48.
limit 47 to conference abstract
-
49.
47 not 48
-
50.
limit 49 to em = 201347-201623
Web of Science core collection
#1 TI=(THA OR TJA OR TJR OR THR)
#2 TS=((total or complete) NEAR/4 joint NEAR/4 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)) AND TS=(hip or hips)
#3 TS=((total or complete) NEAR/4 (hip or hips) NEAR/4 (arthroplast∗ or prosthe∗ or replace∗ or implant∗))
#4 TS=(THA or TJA or TJR OR THR) AND TS=((joint or hip or hips) NEAR/4 (arthroplast∗ or prosthe∗ or replace∗ or implant∗))
#5 #1 OR #2 OR #3 OR #4
#6 TS=(fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗)
#7 TS=((predict∗ OR rate OR risk OR factor∗) NEAR/6 (fail∗ OR revis∗ OR reoperat∗ OR reoperat∗ OR repeat∗ OR reimplant∗ OR reconstruct∗ OR survival)) OR TS=(“survival rate” or “failure analysis” or non-survival or “longterm survival” or “long-term survival”) OR TI=(survival or non-survival or failure or prognos∗ or predict∗ or factor∗)
#8 #5 AND #6 AND #7
#9 TI=(resurfacing or hemiarthroplast∗ or hemi arthroplast∗)
#10 #8 NOT #9
#11 TS=(cohort or follow-up or “long term” or longterm or longitudinal or prospective or retrospective or register or registry or “matched pair∗” or “cross sectional” or cross-sectional or observational or case-control or “case control”) NOT TS=(“case study” or (case NEAR/3 report))
#12 #10 AND #11
CINAHL Plus with Full Text (EBSCO Interface)
S1 ((MH “Arthroplasty, Replacement, Hip”)) OR ((total or complete) n6 (hip or hips) n6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)) OR (((total or complete) n6 joint n6 (arthroplast∗ or prosthe∗ or replace∗ or implant∗)) and (hip or hips)) OR (THA or TJA or TJR or THR )
S2 (MH “Reoperation”) OR ( ( MH “Prosthesis Failure”) OR (MH “Equipment Failure”) ) OR ( fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗ )
S3 ( (MH “Prognosis”) OR (MH “Survival Analysis”) OR (MH “Survival”) ) OR ( ((predict∗ or rate or risk) n6 (fail∗ or revis∗ or re-operat∗ or reoperat∗ or repeat∗ or reimplant∗ or reconstruct∗)) ) OR ( longterm survival or long-term survival or survival rate or failure analysis or ) OR TI ( survival or non-survival or failure or prognos∗ or predict∗ or factor∗ )
S4 S1 AND S2 AND S3
S5 TI (resurfacing or hemiarthroplast∗ or hemi arthroplast∗)
S6 S4 NOT S5
S7 ( (MH “Prospective Studies+”) OR (MH “Case Control Studies+”) OR (MH “Correlational Studies”) OR (MH “Cross Sectional Studies”) ) OR ( cohort∗ or observational stud∗ or longterm or retropective∗ or long-term or longitudinal or follow-up or cross-sectional ) OR TI regist∗
S8 S6 AND S7
Appendix B. Tables of study qualities, level of evidence and surgical characteristics
Table B.1.
Study quality and level of evidence.
| Author | Year | Oxford level of evidence | Study quality |
|---|---|---|---|
| Dorr et al. [36] | 1994 | Level III | Poor |
| Stromberg et al. [46] | 1994 | Level III | Good |
| Emery et al. [37] | 1997 | Level III | Fair |
| Sochart et al. [42] | 1997 | Level III | Good |
| Sochart et al. [41] | 1999 | Level III | Good |
| Chiu et al. [60] | 2001 | Level III | Fair |
| Duffy et al. [57] | 2001 | Level III | Fair |
| McAuley et al. [11] | 2004 | Level III | Good |
| Eskelinen et al. [38] | 2005 | Level III | Good |
| Eskelinen et al. [8] | 2006 | Level III | Good |
| Eskilenen et al. [16] | 2006 | Level III | Good |
| Wangen et al. [62] | 2008 | Level III | Fair |
| Gallo et al. [35] | 2008 | Level III | Fair |
| Hooper et al. [39] | 2009 | Level III | Good |
| Makela et al. [22] | 2011 | Level III | Good |
| Girard et al. [48] | 2011 | Level III | Fair |
| Pakvis et al. [61] | 2011 | Level III | Fair |
| Kim et al. [58] | 2011 | Level II | Fair |
| Bolland et al. [15] | 2012 | Level III | Good |
| McMinn et al. [40] | 2012 | Level III | Good |
| Suh et al. [45] | 2013 | Level III | Fair |
| Kim et al. [43] | 2014 | Level III | Good |
| Sedrayken et al. [44] | 2014 | Level III | Good |
| Pedersen et al. [47] | 2014 | Level III | Poor |
| Kim et al. [59] | 2016 | Level II | Fair |
| Martin et al. [12] | 2016 | Level III | Good |
| Struders et al. [13] | 2016 | Level III | Poor |
| Tsukanaka et al. [49] | 2016 | Level III | Fair |
| Abdel et al. [50] | 2016 | Level III | Fair |
| Philippot et al. [51] | 2017 | Level III | Poor |
| Swarup et al. [52] | 2017 | Level III | Fair |
| Halawi et al. [55] | 2018 | Level III | Fair |
| Swarup et al. [53] | 2018 | Level III | Fair |
| Dessyn et al. [54] | 2019 | Level III | Fair |
| Halvorsen et al. [56] | 2019 | Level III | Good |
Table B.2.
Surgical characteristics of included studies.
| Author | Year | Surgeons characteristics | Surgical approach | Implant and fixation | Outcome measures |
|---|---|---|---|---|---|
| Studies used posterolateral or posterior surgical approach | |||||
| Emery et al. [37] | 1997 | NR | Posterior approach | Femoral prostheses were mark-9 stem or long-stem reoperation prostheses. The head size was 25 mm in all cases. The cups were standard Stanmore cups or the Portsmouth design, which was a hybrid of the Charnley with a Stanmore bearing surface. First- and second-generation cementing techniques were used |
Survivorship at 10 and 15 y |
| Pakvis et al. [61] | 2011 | NR | Posterolateral approach | The cementless RM monoblock socket was used in all patients. In 99 hips, a CLS Spotorno femoral stem was used, 38 hips received an isoelastic RM stem, 16 hips a Wagner SL stem, and in 5 hips, a Wagner cone stem was used. Articulation: metal on polyethylene in 58 hips and ceramic on polyethylene in 100 hips. |
Implant survivorship at 10, and 14 y. |
| Suh et al. [45] | 2013 | A single surgeon | Postero-lateral approach | Hybrid total hip arthroplasty using third-generation cementing techniques and precoat stems. | Survivorship of the femoral component at 10 and 19 y |
| Kim et al. [59] | 2016 | A senior surgeon | Posterolateral approach | Cemented Elite-plus stem (Ortron 90) Cementless Profile stem Cementless Duraloc 100 or 1200 series acetabular component Polyethylene liner The cementless femoral components were inserted with a press-fit Cement was applied using an intramedullary plug, pulsatile lavage, vacuum mixing, injection with a cement gun, a proximal rubber seal, and a distal centralizer on the femoral component |
Implant survivorship at a minimum follow-up of 25 y. |
| Studies used anterolateral or anterior surgical approach | |||||
| Sochart et al. [42] | 1997 | NR | Lateral approach with planar trochanteric osteotomy | Standard Charnley reattachment with stainless-steel wires | Survivorship at 25 y |
| Sochart et al. [41] | 1999 | NR | Lateral approach with planar trochanteric osteotomy | Charnley prostheses were used, and both components were cemented using first-generation techniques | Average annual wear rate |
| Gallo et al. [35] | 2008 | Four experienced surgeons | Anterolateral approach | The Anatomique Benoist Girard hip prosthesis was used in this study Fixation was achieved initially by press-fit which was followed by osseous integration mediated by HAC. |
Implant survivorship at 5, 7, 10, and 12 y |
| Martin et al. [12] | 2016 | A single surgeon | Trans trochanteric approach | Cemented Charnley stem. Three generations of cementing techniques were used | Survivorship at 20 y |
| Abdel et al. [50] | 2016 | NR | Lateral approach | Cemented charnley monoblock with 22.25 head | Reoperation rate at 30 y |
| Dessyn et al. [54] | 2019 | NR | Anterolateral Watson-Jones approach | Uncemented Ti-alloy hydroxyapatite-coated cup with a conventional ultra-high-molecular-weight polyethylene liner was used for all patients combined with a 28-mm-diameter alumina femoral head | Reoperation rate and hip implant survivorship at 20 and 25 y |
| Studies used multiple surgical approaches | |||||
| Chiu et al. [60] | 2001 | NR | Posterolateral (68.1%) Transtrochanteric (14.9%) Transgluteal (10.6%) Anterolateral (6.4%) |
Cemented Charnley stainless steel round-back femoral stem with a Vaquasheen surface and an all-polyethylene nonflanged acetabular component with a long posterior wall | Implant survivorship at 5, 10, and 15 y. |
| Duffy et al. [57] | 2001 | NR | Anterolateral (74.4%), Posterior (17.1%), Transtrochanteric (8.5%). | The porous-coated anatomic THA, Harris-Galante Porous-I THA, Osteonics Dual Geometry THA |
Implant survivorship at a minimum follow-up of 10 y. |
| McAuley et al. [11] | 2004 | NR | Posterior approach Anterolateral approach Lateral approach |
Extensively porous-coated femoral components | Survivorship at 5, 10, and 15 y |
| Wangen et al. [62] | 2008 | NR | Posterior or direct lateral approach, without trochanteric osteotomy | A straight stem designed for press-fit insertion A hemispherical HA-coated cup inserted with press-fit in 36 cases, an HA-coated screw cup in 7 cases, a hemispherical cup designed for press-fit insertion in 6 cases |
Reoperation rates at a mean of 13 y |
| Struders et al. [13] | 2016 | NR | Multiple approaches used, most commonly: Anterolateral (74%) Anterior (19%) Tran gluteal (5%) |
Third-generation Zweymuller stem with uncemented press-fit cup | Survivorship of the implant at 10 and 13 y |
| Halawi et al. [55] | 2018 | High-volume arthroplasty surgeons (defined as performing at least 50 THAs per year) | Posterolateral (48.1%) Anterolateral (32.8%) Lateral (19%) |
Cementless total hip arthroplasty. The most common femoral implants: Citation (50.7%), Accolade TMZF (17.1%), Synergy (8.8%), Corail and S-ROM (4.9%). The most common acetabular implants: Trident (74%), Pinnacle (9.1%), and Reflection (8.8%). Articulation: ceramic on ceramic (48.5%), ceramic on polyethylene, control 44 (13.4%), metal on metal (22.6%), metal on polyethylene (15.5%) | Reoperation rate and implant survivorship at 5 y |
| Halvorsen et al. [56] | 2019 | NR | Posterior approach (47%) Trochanteric osteotomy (2.4%) |
The number of different brands varied from 9 to 22 for cups and 10 to 21 for stems for each of the participating countries. Articulation: metal/metal (17%), metal/ceramic (0.1%), ceramic/ceramic (11%), Poly-XL/metal (23%), Poly-XL/ceramic (15%), poly/metal (8.9%), poly/ceramic (6.1%), missing (19%). Head size: < 32 mm (46%), 32 mm (25%), >32 mm (20%), missing (8.5%). Fixations: cemented (7.0%), uncemented (74%), hybrid (4.1%), reverse hybrid (8.9%), resurfacing (3.5%), missing (1.7) |
Implant survivorship at 5, 10, and 15 y and Reoperation rate at 20 y |
| Surgical approach was not Reported | |||||
| Dorr et al. [36] | 1994 | NR | NR | Charnley, Charnley-Miiller, Aufranc-Turner or LeGrange- Letournel | Reoperation rates at 4.5 and 9.2 y |
| Stromberg et al. [46] | 1994 | NR | NR | NR | Survivorship at 4 and 10 y |
| Eskelinen et al. [38] | 2005 | NR | NR | The stems were classified as uncemented proximally circumferentially porous-coated, uncemented extendedly porous-coated, uncemented proximally circumferentially Hydroxyapatite coated, uncemented uncoated, and cemented. The cups were classified as uncemented porous-coated press-fit, uncemented hydroxyapatite-coated press-fit, uncemented smooth-threaded, and cemented all-polyethylene. | Survivorship at 10 y |
| Eskelinen et al. [8] | 2006 | NR | NR | Uncemented stem designs were included, uncemented cup designs or cup-stem combinations were included | Survivorship at 7, 10, 13, 15 y |
| Eskilenen et al. [16] | 2006 | NR | NR | NR | Survivorship at 7, 10, 15 y |
| Hooper et al. [39] | 2009 | NR | NR | Cemented, uncemented implants | Reoperation rate per 100 component years |
| Kim et al. [58] | 2011 | One surgeon | NR | Cementless acetabular component for all THA, 78 cemented femoral component, and 79 cementless femoral components (inserted with press-fit). The Charnley Elite or Elite-plus stem (Ortron 90) was used in the cemented (hybrid) group and the Profile Stem in the cementless group. A cementless Duraloc 100 or 1200 series acetabular used in all THA. |
Implant survivorship at 10, 15, and 20 y. |
| Makela et al. [22] | 2011 | NR | NR | The implants were implants with a cementless, straight, proximally circumferentially porous-coated stem and a porous-coated press-fit cup, implants with a cementless, anatomic, proximally circumferentially porous-coated stem, with or without hydroxyapatite, and a porous-coated press-fit cup with or without hydroxyapatite, or a cemented stem combined with a cemented all-polyethylene cup | 5, 10, and 15 y survival |
| Girard et al. [48] | 2011 | NR | NR | NR | Revisions rate at a minimum of 1 y |
| Bolland et al. [15] | 2012 | NR | NR | Cemented, uncemented, hybrid implant, and resurfacing categories | Reoperation rates at 3 y |
| McMinn et al. [40] | 2012 | NR | NR | Cemented, uncemented and Birmingham implants | Reoperation rate in person-years |
| Kim et al. [43] | 2014 | A single surgeon | NR | Porous-coated anatomic total hip arthroplasty components | Survival at 28,.4 y Radiographic loosening Wear Rates Harris Hip Scores |
| Sedrayken et al. [44] | 2014 | NR | NR | Conventional uncemented total hip arthroplasty, hip resurfacing, or hybrid fixation was performed | Survivorship at 5 y |
| Pedersen et al. [47] | 2014 | NR | NR | Cementless, cemented, and hybrid implants | Survivorship at 2, 10, and 16 y |
| Tsukanaka et al. [49] | 2016 | NR | NR | 24 different cups and 17 different stems were used. 89% cups and 95% stems were uncemented. Ceramic or metal on polyethylene bearings was chosen for 89% of the total hip replacements |
Survivorship and reoperation rate at 10 y |
| Philippot et al. [51] | 2017 | NR | NR | Bousquet dual-mobility cup | Reoperation rate at mean 21.9 y |
| Swarup et al. [52] | 2017 | NR | NR | NR | Reoperation rate at 14 y |
| Swarup et al. [53] | 2018 | NR | NR | Implant type: Standard (80.4%), Custom (19.6%). Articulation: metal on plastic (61.2%), metal on metal (3.1%), ceramic on plastic (23.1%), ceramic on ceramic (12.6%). Fixation: cemented (30.8%), cementless (69.2%) |
Reoperation rate and implant survivorship at 5, 10, and 20 y |
NR, not reported.
Appendix C. Forest Plots of Total Hip Arthroplasty Survival Rates
Figure 1.
Forest plot of total hip arthroplasty at 2- to 5-y follow-up.
Figure 2.
Forest plot of total hip arthroplasty at 7- to 10-y follow-up.
Figure 3.
Forest plot of total hip arthroplasty at 20- to 25-y follow-up. Studies were presented in the forest plot if reported survival rates with a measure of variance.
References
- 1.Kurtz S.M., Lau E., Ong K., Zhao K., Kelly M., Bozic K.J. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maradit Kremers H., Larson D.R., Noureldin M., Schleck C.D., Jiranek W.A., Berry D.J. Long-term mortality trends after total hip and knee arthroplasties: a population-based study. J Arthroplasty. 2016;31:1163–1169. doi: 10.1016/j.arth.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maradit Kremers H., Larson D.R., Crowson C.S., Kremers W.K., Washington R.E., Steiner C.A., et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kurtz S., Mowat F., Ong K., Chan N., Lau E., Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 5.Vogel L.A., Carotenuto G., Basti J.J., Levine W.N. Physical activity after total joint arthroplasty. Sports Health. 2011;3:441–450. doi: 10.1177/1941738111415826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Evans J.T., Evans J.P., Walker R.W., Blom A.W., Whitehouse M.R., Sayers A. How long does a hip replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet. 2019;393:647–654. doi: 10.1016/S0140-6736(18)31665-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adelani M.A., Keeney J.A., Palisch A., Fowler S.A., Clohisy J.C. Has total hip arthroplasty in patients 30 years or younger improved? A systematic review. Clin Orthop Relat Res. 2013;471:2595–2601. doi: 10.1007/s11999-013-2975-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Uncemented total hip arthroplasty for primary osteoarthritis in young patients: a mid-to long-term follow-up study from the Finnish arthroplasty register. Acta Orthop. 2006;77:57–70. doi: 10.1080/17453670610045704. [DOI] [PubMed] [Google Scholar]
- 9.Röder C., Parvizi J., Eggli S., Berry D.J., Müller M.E., Busato A. Demographic factors affecting long-term outcome of total hip arthroplasty. Clin Orthop Relat Res. 2003;417:62–73. doi: 10.1097/01.blo.0000096812.78689.f0. [DOI] [PubMed] [Google Scholar]
- 10.Matharu G.S., McBryde C.W., Pynsent W.B., Pynsent P.B., Treacy R.B. The outcome of the Birmingham Hip Resurfacing in patients aged < 50 years up to 14 years post-operatively. Bone Joint J. 2013;95-B:1172–1177. doi: 10.1302/0301-620X.95B9.31711. [DOI] [PubMed] [Google Scholar]
- 11.McAuley J.P., Szuszczewicz E.S., Young A., Engh C.A. Total hip arthroplasty in patients 50 years and younger. Clin Orthop Relat Res. 2004;418:119–125. doi: 10.1097/00003086-200401000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Martin C.T., Callaghan J.J., Gao Y., Pugely A.J., Liu S.S., Warth L.C., et al. What can we learn from 20-year followup studies of hip replacement? Clin Orthop Relat Res. 2016;474:402–407. doi: 10.1007/s11999-015-4260-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Studers P., Belajevs D., Jurkevics V., Likums P. Ten to fifteen-year clinical and radiographic follow-up with a third-generation cementless stem in a young patient population. Int Orthop. 2016;40:465–471. doi: 10.1007/s00264-015-2846-z. [DOI] [PubMed] [Google Scholar]
- 14.Petis S., Howard J.L., Lanting B.L., Vasarhelyi E.M. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg. 2015;58:128–139. doi: 10.1503/cjs.007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bolland B.J., Whitehouse S.L., Timperley A.J. Indications for early hip revision surgery in the UK--a re-analysis of NJR data. Hip Int. 2012;22:145–152. doi: 10.5301/HIP.2012.9184. [DOI] [PubMed] [Google Scholar]
- 16.Eskelinen A., Paavolainen P., Helenius I., Pulkkinen P., Remes V. Total hip arthroplasty for rheumatoid arthritis in younger patients: 2,557 replacements in the Finnish Arthroplasty Register followed for 0-24 years. Acta Orthop. 2006;77:853–865. doi: 10.1080/17453670610013132. [DOI] [PubMed] [Google Scholar]
- 17.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bayliss L.E., Culliford D., Monk A.P., Glyn-Jones S., Prieto-Alhambra D., Judge A., et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. 2017;389:1424–1430. doi: 10.1016/S0140-6736(17)30059-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ackerman I.N., Bohensky M.A., Zomer E., Tacey M., Gorelik A., Brand C.A., et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord. 2019;20:90. doi: 10.1186/s12891-019-2411-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurtz S.M., Lau E., Schmier J., Ong K.L., Zhao K., Parvizi J. Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008;23:984–991. doi: 10.1016/j.arth.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz S.M., Lau E., Watson H., Schmier J.K., Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(8 Suppl):61–65.e1. doi: 10.1016/j.arth.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32. [Google Scholar]
- 23.Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 25.Mäkelä K.T., Eskelinen A., Pulkkinen P., Paavolainen P., Remes V. Results of 3,668 primary total hip replacements for primary osteoarthritis in patients under the age of 55 years. Acta Orthop. 2011;82:521–529. doi: 10.3109/17453674.2011.618908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Espehaug B., Havelin L.I., Engesaeter L.B., Langeland N., Vollset S.E. Patient-related risk factors for early revision of total hip replacements. A population register-based case-control study of 674 revised hips. Acta Orthop Scand. 1997;68:207–215. doi: 10.3109/17453679708996686. [DOI] [PubMed] [Google Scholar]
- 27.Kuijpers M.F.L., Hannink G., van Steenbergen L.N., Schreurs B.W. Total hip arthroplasty in young patients in The Netherlands: trend analysis of >19,000 primary hip replacements in the Dutch arthroplasty register. J Arthroplasty. 2018;33:3704–3711. doi: 10.1016/j.arth.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 28.Eingartner C. Current trends in total hip arthroplasty. Ortop Traumatol Rehabil. 2007;9:8–14. [PubMed] [Google Scholar]
- 29.Jonas K., Nils W., Alexander D., Stefan B., Henning W., Thilo F. The etiology of revision total hip arthroplasty: current trends in a retrospective survey of 3450 cases. Arch Orthop Trauma Surg. 2020;140:1265–1273. doi: 10.1007/s00402-020-03514-3. [DOI] [PubMed] [Google Scholar]
- 30.Dixon T., Shaw M., Ebrahim S., Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825–830. doi: 10.1136/ard.2003.012724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Covidence systematic review software, veritas health innovation, Melbourne, Australia. https://www.covidence.org [accessed 15.01.22]
- 32.Group OLoEW “The Oxford 2011 levels of evidence”. Oxford centre for evidence-based medicine. http://www.cebm.net/index.aspx?o=5653 [accessed 24.02.22]
- 33.Howick J CI, Greenhalgh T, Heneghan C, Greenhalgh, T., Heneghan, C., Liberati A., et al. “The 2011 Oxford CEBM Evidence Levels of Evidence (Introductory Document)”. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653 [accessed 01.03.22].
- 34.Scottish Intercollegiate Guidelines Network. SIGN Methodology Checklist 3: Cohort Studies. Checklists (sign.ac.uk). [accessed 03.01.22].
- 35.Gallo J., Langova K., Havranek V., Cechova I. Poor survival of ABG I hip prosthesis in younger patients. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2008;152:163–168. doi: 10.5507/bp.2008.027. [DOI] [PubMed] [Google Scholar]
- 36.Dorr L.D., Kane T.J., Conaty J.P. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplasty. 1994;9:453–456. doi: 10.1016/0883-5403(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 37.Emery D.F., Clarke H.J., Grover M.L. Stanmore total hip replacement in younger patients: review of a group of patients under 50 years of age at operation. J Bone Joint Surg Br. 1997;79:240–246. doi: 10.1302/0301-620x.79b2.7165. [DOI] [PubMed] [Google Scholar]
- 38.Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0-22 years. Acta Orthop. 2005;76:28–41. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 39.Hooper G.J., Rothwell A.G., Stringer M., Frampton C. Revision following cemented and uncemented primary total hip replacement: a seven-year analysis from the New Zealand Joint Registry. J Bone Joint Surg Br. 2009;91:451–458. doi: 10.1302/0301-620X.91B4.21363. [DOI] [PubMed] [Google Scholar]
- 40.McMinn D.J., Snell K.I., Daniel J., Treacy R.B., Pynsent P.B., Riley R.D. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sochart D.H. Relationship of acetabular wear to osteolysis and loosening in total hip arthroplasty. Clin Orthop Relat Res. 1999;363:135–150. [PubMed] [Google Scholar]
- 42.Sochart D.H., Porter M.L. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Joint Surg Am. 1997;79:1599–1617. doi: 10.2106/00004623-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Kim Y.H., Park J.W., Park J.S. The 27 to 29-year outcomes of the PCA total hip arthroplasty in patients younger than 50 years old. J Arthroplasty. 2014;29:2256–2261. doi: 10.1016/j.arth.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Sedrakyan A., Romero L., Graves S., Davidson D., de Steiger R., Lewis P., et al. Survivorship of hip and knee implants in pediatric and young adult populations: analysis of registry and published data. J Bone Joint Surg Am. 2014;96 Suppl 1(Suppl 1):73–78. doi: 10.2106/JBJS.N.00541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Suh D.H., Yun H.H., Chun S.K., Shon W.Y. Fifteen-year results of precoated femoral stem in primary hybrid total hip arthroplasty. Clin Orthop Surg. 2013;5:110–117. doi: 10.4055/cios.2013.5.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Strömberg C.N., Herberts P. A multicenter 10-year study of cemented revision total hip arthroplasty in patients younger than 55 years old. A follow-up report. J Arthroplasty. 1994;9:595–601. doi: 10.1016/0883-5403(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 47.Pedersen A.B., Mehnert F., Havelin L.I., Furnes O., Herberts P., Kärrholm J., et al. Association between fixation technique and revision risk in total hip arthroplasty patients younger than 55 years of age. Results from the Nordic Arthroplasty Register Association. Osteoarthritis Cartilage. 2014;22:659–667. doi: 10.1016/j.joca.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 48.Girard J., Glorion C., Bonnomet F., Fron D., Migaud H. Risk factors for revision of hip arthroplasties in patients younger than 30 years. Clin Orthop Relat Res. 2011;469:1141–1147. doi: 10.1007/s11999-010-1669-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsukanaka M., Halvorsen V., Nordsletten L., Ø EngesæTer I., EngesæTer L.B., Fenstad A.M., et al. Implant survival and radiographic outcome of total hip replacement in patients less than 20 years old. Acta Orthop. 2016;87:479–484. doi: 10.1080/17453674.2016.1212180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abdel M.P., Roth P.V., Harmsen W.S., Berry D.J. What is the lifetime risk of revision for patients undergoing total hip arthroplasty? a 40-year observational study of patients treated with the Charnley cemented total hip arthroplasty. Bone Joint J. 2016;98-B:1436–1440. doi: 10.1302/0301-620X.98B11.BJJ-2016-0337.R1. [DOI] [PubMed] [Google Scholar]
- 51.Philippot R., Neri T., Boyer B., Viard B., Farizon F. Bousquet dual mobility socket for patient under fifty years old. More than twenty year follow-up of one hundred and thirty one hips. Int Orthop. 2017;41:589–594. doi: 10.1007/s00264-016-3385-y. [DOI] [PubMed] [Google Scholar]
- 52.Swarup I., Shields M., Mayer E.N., Hendow C.J., Burket J.C., Figgie M.P. Outcomes after total hip arthroplasty in young patients with osteonecrosis of the hip. Hip Int. 2017;27:286–292. doi: 10.5301/hipint.5000457. [DOI] [PubMed] [Google Scholar]
- 53.Swarup I., Lee Y.Y., Chiu Y.F., Sutherland R., Shields M., Figgie M.P. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients. J Arthroplasty. 2018;33:2893–2898. doi: 10.1016/j.arth.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 54.Dessyn E., Flecher X., Parratte S., Ollivier M., Argenson J.N. A 20-year follow-up evaluation of total hip arthroplasty in patients younger than 50 using a custom cementless stem. Hip Int. 2019;29:481–488. doi: 10.1177/1120700018803290. [DOI] [PubMed] [Google Scholar]
- 55.Halawi M.J., Brigati D., Messner W., Brooks P.J. Total hip arthroplasty in patients 55 years or younger: risk factors for poor midterm outcomes. J Clin Orthop Trauma. 2018;9:103–106. doi: 10.1016/j.jcot.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Halvorsen V., Fenstad A.M., Engesæter L.B., Nordsletten L., Overgaard S., Pedersen Alma B., et al. Outcome of 881 total hip arthroplasties in 747 patients 21 years or younger: data from the Nordic Arthroplasty Register Association (NARA) 1995-2016. Acta Orthop. 2019;90:331–337. doi: 10.1080/17453674.2019.1615263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duffy G.P., Berry D.J., Rowland C., Cabanela M.E. Primary uncemented total hip arthroplasty in patients <40 years old: 10- to 14-year results using first-generation proximally porous-coated implants. J Arthroplasty. 2001;16(8 Suppl 1):140–144. doi: 10.1054/arth.2001.28716. [DOI] [PubMed] [Google Scholar]
- 58.Kim Y.H., Kim J.S., Park J.W., Joo J.H. Comparison of total hip replacement with and without cement in patients younger than 50 years of age: the results at 18 years. J Bone Joint Surg Br. 2011;93:449–455. doi: 10.1302/0301-620X.93B4.26149. [DOI] [PubMed] [Google Scholar]
- 59.Kim Y.H., Park J.W., Kim J.S., Kim I.W. Twenty-five- to twenty-seven-year results of a cemented vs a cementless stem in the same patients younger than 50 Years of age. J Arthroplasty. 2016;31:662–667. doi: 10.1016/j.arth.2015.09.045. [DOI] [PubMed] [Google Scholar]
- 60.Chiu K.Y., Ng T.P., Tang W.M., Poon K.C., Ho W.Y., Yip D. Charnley total hip arthroplasty in Chinese patients less than 40 years old. J Arthroplasty. 2001;16:92–101. doi: 10.1054/arth.2001.19156. [DOI] [PubMed] [Google Scholar]
- 61.Pakvis D., Biemond L., van Hellemondt G., Spruit M. A cementless elastic monoblock socket in young patients: a ten to 18-year clinical and radiological follow-up. Int Orthop. 2011;35:1445–1451. doi: 10.1007/s00264-010-1120-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wangen H., Lereim P., Holm I., Gunderson R., Reikerås O. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop. 2008;32:203–208. doi: 10.1007/s00264-006-0309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parvizi J., Suh D.H., Jafari S.M., Mullan A., Purtill J.J. Aseptic loosening of total hip arthroplasty: infection always should be ruled out. Clin Orthop Relat Res. 2011;469:1401–1405. doi: 10.1007/s11999-011-1822-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mei X.Y., Gong Y.J., Safir O., Gross A., Kuzyk P. Long-term outcomes of total hip arthroplasty in patients younger than 55 years: a systematic review of the contemporary literature. Can J Surg. 2019;62:249–258. doi: 10.1503/cjs.013118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schreurs B.W., Hannink G. Total joint arthroplasty in younger patients: heading for trouble? Lancet. 2017;389:1374–1375. doi: 10.1016/S0140-6736(17)30190-3. [DOI] [PubMed] [Google Scholar]
- 66.Te Stroet M.A., Rijnen W.H., Gardeniers J.W., van Kampen A., Schreurs B.W. Satisfying outcomes scores and survivorship achieved with impaction grafting for revision THA in young patients. Clin Orthop Relat Res. 2015;473:3867–3875. doi: 10.1007/s11999-015-4293-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ravi B., Jenkinson R., Austin P.C., Croxford R., Wasserstein D., Escott B., et al. Relation between surgeon volume and risk of complications after total hip arthroplasty: propensity score matched cohort study. BMJ. 2014;348:g3284. doi: 10.1136/bmj.g3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peters M.D., Godfrey C.M., Khalil H., McInerney P., Parker D., Soares C.B. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 69.Tricco A.C., Lillie E., Zarin W., O'Brien K., Colquhoun H., Kastner M., et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kurtz S.M., Ong K.L., Lau E., Bozic K.J. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96:624–630. doi: 10.2106/JBJS.M.00285. [DOI] [PubMed] [Google Scholar]
- 71.Rupp M., Lau E., Kurtz S.M., Alt V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin Orthop Relat Res. 2020;478:1622–1633. doi: 10.1097/CORR.0000000000001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.