Abstract
Open reduction and internal fixation is the gold standard treatment for tibial plateau fractures. However, the procedure is not free of complications such as knee stiffness, acute infection, chronic infection (osteomyelitis), malunion, non-union, and post-traumatic osteoarthritis.
The treatment options for knee stiffness are mobilisation under anaesthesia (MUA) when the duration is less than 3 months, arthroscopic release when the duration is between 3 and 6 months, and open release for refractory cases or cases lasting more than 6 months. Early arthroscopic release can be associated with MUA.
Regarding treatment of acute infection, if the fracture has healed, the hardware can be removed, and lavage and debridement can be performed along with antibiotic therapy. If the fracture has not healed, the hardware is retained, and lavage, debridement, and antibiotic therapy are performed (sometimes more than once until the fracture heals). Fracture stability is important not only for healing but also for resolving the infection.
In cases of osteomyelitis, treatment should be performed in stages: aggressive debridement of devitalised tissue and bone, antibiotic spacing and temporary external fixation until the infection is resolved (first stage), followed by definitive surgery with grafting or soft tissue coverage depending on the bone defect (second stage).
Intra-articular or extra-articular osteotomy is a good option to correct malunion in young, active patients without significant joint damage. When malunion is associated with extensive joint involvement or the initial cartilage damage has resulted in knee osteoarthritis, the surgical option is total knee arthroplasty.
Keywords: tibial plateau fractures, surgical treatment, complications
Introduction
Tibial plateau fractures constitute 1% of all fractures and have a bimodal distribution: a peak incidence in young patients following high-energy mechanisms and the second peak in elderly patients with osteoporotic bone (1, 2).
The most widely used classification for tibial plateau fractures was established by Schatzker et al. in 1979 (3) and was later modified by Luo et al. (4) and Kfuri and Schatzker (5) to distinguish injuries involving the posterior column, which is important for planning the surgical management of these fractures. The Müller AO (Arbeitsgemeinschaft für Osteosynthesefragen) classification of fractures is also commonly used (6).
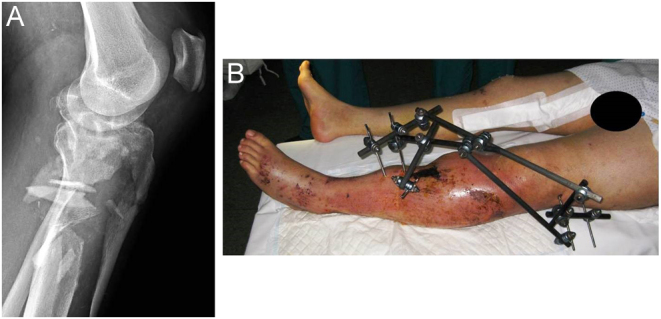
Considering that tibial plateau fractures are intra-articular, the gold standard for treatment is surgery by open reduction and internal fixation (ORIF) with locked plates to restore joint congruence and to achieve an adequate mechanical axis, a stable knee, and early mobilisation (6, 7, 8). In cases with extensive soft tissue damage, definitive treatment with a hybrid external fixator may also be considered (Fig. 1). Several studies have supported the use of the fixator in cases where surgical approaches to healthy areas are not considered for ORIF (9, 10, 11, 12, 13, 14, 15).
Figure 1.

Schatzker type VI tibial plateau fracture (A). An external fixator was placed (first stage of treatment) for soft tissue control. The extensive soft tissue involvement resulted in compartment syndrome.
One of the earliest studies on the treatment, outcomes, and complications of tibial plateau fractures was by Schatzker et al. in 1979, which showed a 27% complication rate (3). In 1987, Moore and Patzakis reported poor functional outcomes in bituberosity fractures (Schatzker V, VI) than in Schatzker I–IV fractures (16). The authors also observed a high rate of complications after surgical treatment (19%), with the most frequent being infection. Over the years, these complications have decreased, mainly due to the introduction of the sequential management of these fractures in high-energy cases: external fixation (first stage) followed by delayed definitive treatment (second stage). The evolution of ORIF has led to the use of new materials such as low-profile locked plates and new minimally invasive approaches that achieve a better reduction of posterolateral and posteromedial fragments, which, although requiring a greater number of incisions, involve less soft tissue debonding (6, 15, 16). Figure 2 shows an example of sequential treatment, with the first stage of external fixation. Figure 3 shows a case treated with external fixation (first stage) for soft tissue control.
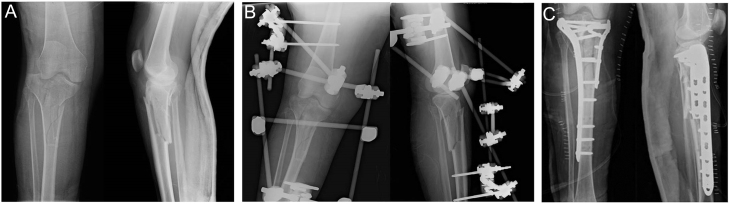
Figure 2.
(A, B and C). Schatzker type VI tibial plateau fracture (A). An external fixator was placed (first stage of treatment) for soft tissue control (B). In a second stage (definitive surgery), open reduction and internal fixation (ORIF) was performed (C).
Figure 3.
(A and B). Tibial plateau fracture (A) treated definitively with a hybrid fixator (B) due to the poor condition of the soft tissue, which prevented an open reduction and internal fixation (ORIF) approach in the healthy area.
The aim of this article is to describe the specific complications associated with the surgical treatment of tibial plateau fractures (Table 1), their prevalence, causes, and management.
Table 1.
Complications of the surgical treatment of fractures of the tibial plateau.
| Knee stiffness |
| Acute infection |
| Chronic infection (osteomyelitis) |
| Malunion |
| Non-union |
| Post-traumatic osteoarthritis |
| Residual knee instability secondary to ligaments damage that was not addressed initially, during fixation |
Knee stiffness
Gaston et al. reported that after the fracture of the tibial plateau, 20% of the patients have stiffness (a residual knee flexion contracture of >5º) at 12 months after surgery (17). According to Pujol et al., the causes of post-traumatic knee stiffness can be divided into flexion contractures, extension contractures, and combined contractures. Post-traumatic stiffness can be due to the presence of dense intra-articular adhesions and/or fibrotic transformation of periarticular structures. From a general point of view, a flexion contracture is due to posterior adhesions and/or anterior impingement. On the other hand, extension contractures are due to anterior adhesions and/or posterior impingement (18).
Incidence, aetiology, and risk factors
The incidence of knee stiffness after tibial plateau fracture is 3–18% depending on the series (19, 20, 21, 22), although the need for surgical re-intervention for this reason is low (0–5%) (20, 23). The aetiology is multifactorial and can be enhanced by intra-articular (inflammation, adhesions, intra-capsular scarring, and bone irregularities after malunion causing impingement) and extra-articular factors (extensor apparatus lesions and fibrosis, and scarring of skin and periarticular soft tissue) (23, 24). Stiffness-related risk factors include external fixator use, open fractures, polytrauma, the need for fasciotomies, wound complications requiring increased immobilisation, extensor apparatus injuries, and the need for more than two surgical procedures (20, 21, 25). Prolonged immobilisation associated with all these factors appears to be a key element in the development of stiffness. Immobilisation must therefore be prevented, which means achieving stable osteosynthesis and mobilisation as soon as possible.
Diagnosis and evaluation
The diagnosis of stiffness should be based on anamnesis and physical examination, both in its objective assessment and in the patient’s subjective limitation, which will depend on their lifestyle and work activity (26, 27). Stiffness manifests as contracture in flexion or extension or as a combined contracture. Defining the type of contracture is essential for choosing the treatment modality. It is also important to rule out the presence of a complex regional syndrome, in which case the surgical treatment of the stiffness should be delayed until the syndrome has resolved (28). It is important to assess the duration of the stiffness so as to properly choose the type of treatment and ensure a good prognosis (20).
Treatment
The treatment options for knee stiffness are summarised in Table 2, from least to most surgically aggressive, although these options can be used in combination.
Table 2.
Treatment options for knee stiffness after tibial plateau fractures.
| Mobilisation under anaesthesia (MUA) |
| Arthroscopic release |
| • Anterior (contracture in extension = deficit of flexion) |
| • Posterior (contracture in flexion = deficit of extension) |
| Open release |
| • Anterior (contracture in extension = deficit of flexion) |
| • Posterior (contracture in flexion = deficit of extension) |
Manipulation under anaesthesia
A manipulation under anaesthesia (MUA) is a non-invasive way of restoring the range of movement at the knee. While the patient is under anaesthesia, the surgeon will ‘manipulate’ or move the knee joint through flexion and extension in order to loosen it and reduce pain and stiffness. Sassoon et al. analysed 22 patients with a mean age of 40 who experienced closed MUA for post-traumatic knee arthrofibrosis (29). Injuries included fractures of the femur, tibia, and patella, as well as ligamentous injuries and traumatic arthrotomies. The mean time from treatment to MUA was 90 days. Mean follow-up after manipulation was 7 months. The mean pre-manipulation ROM arc was 59 ± 25°. The mean intraoperative arc of motion, achieved at the time of the manipulation, was 123 ± 14°. No complications took place during the MUA procedure. At the most recent follow-up, the mean range of motion (ROM) arc was 110 ± 19°. Manipulations performed 90 days or more after surgical treatment provided a benefit equaling those carried out more acutely (29).
In early cases lasting less than 12 weeks (30, 31), MUA may be considered. MUA is a simple and effective technique that has been shown to reduce stiffness and has been widely documented in cases of total knee arthroplasty (TKA) (30, 32, 33). MUA is not free from complications such as fractures, implant failure with loss of reduction (in cases of very early mobilisation prior to fracture healing), tendon rupture, and articular cartilage damage (31). MUA should therefore be performed with caution.
Arthroscopic release
Arthroscopic release may be considered as an option when the stiffness lasts longer than 12 weeks or even earlier if there is a clear halt in the progression of joint range gain (34). A number of authors have suggested routine MUA associated with arthroscopic release, arguing that arthroscopic release of adhesions can reduce the complications associated with MUA (35).
Release will be anterior, posterior, or combined, depending on the type of stiffness. Numerous studies have demonstrated statistically significant gains in mobility with these arthroscopic techniques (36, 37, 38, 39, 40, 41, 42, 43). In a number of these studies, joint gain was somewhat reduced from the immediate postoperative period to months into the follow-up, although significant improvement was still maintained.
In general, it is preferable to perform arthroscopic release before 6 months of stiffness have passed, although there is evidence of improvement in procedures performed later (44).
Open release
In cases where the cause of stiffness is extra-articular (retractile scarring and fibrosis of the extensor apparatus) or for patients who have not been treated with early arthroscopic techniques and/or MUA, open surgery might be necessary.
The most frequently used technique is the anterior release of the extensor apparatus, which was described by Judet et al. in 1956 (45). The technique is surgically aggressive and employs a lateral approach that largely detaches the quadriceps from the femur and adjacent structures; therefore, the potential benefits should be weighed against possible complications (bleeding, infection, and recurrent stiffness) before employing the technique (46, 47).
Several authors have proposed techniques to treat extensor contractures without the need for open surgery, such as the quadriceps pie-crusting technique associated with an arthroscopic technique (48, 49, 50). Endoscopic quadricep release has also been proposed (42, 51, 52, 53). Table 3 summarises the treatments described and their indication according to the duration of knee stiffness.
Table 3.
Treatment of knee stiffness after tibial plateau fractures according to its chronicity.
| Duration of stiffness | |||
|---|---|---|---|
| <3 months | 3–6 months | >6 months | |
| Treatment | MUA | Arthroscopic release | Open release |
| Considerations | Some authors routinely associate it with arthroscopic release. | Some authors propose it with a shorter evolution time. | Assess the type of stiffness (flexion/extension) to decide the adequate surgical technique. |
| Some authors associate endoscopic extra-articular quadriceps release or pie-crusting. | |||
MUA, manipulation under anaesthesia
Infection
In the early 1990s, the infection rates for this type of fracture were exceedingly high, and the surgical technique was based on large single anterior approaches requiring extensive soft tissue debonding with severe healing problems (54). However, these rates have been improving thanks to the evolution of surgical techniques in terms of planning CT scans, new minimally invasive approaches, the reduced tendency to desperiostisation, the evolution of implants, and sequential treatment with external fixator for soft tissue control prior to definitive surgery (55). There is also the fact that if the fracture is open, there is a greater risk of infection.
In 1994, Young and Barrack analysed eight comminuted/bicondylar displaced tibial plateau fractures treated by open reduction and internal fixation; seven of eight (87.5%) knees became infected (54). In 2004, Barei et al. reported an 8.4% rate of deep wound infections. Of the infected patients, 3.6% had associated septic arthritis. Clinical resolution of infection occurred after an average of 3.3 additional procedures (55). In 2000 patients treated with ORIF by henkelman et al. in 2020, the rate of surgical site infection was 4.7% (93/2000) (56). In 2022, the rate of deep infection in OTA/AO type C tibial plateau reported by Bullock et al. was 6% (57).
Risk factors and prevention
The risk factors for infection are open fractures, compartment syndrome, external fixation, surgical time, and tobacco use, with infection rates ranging from 3 to 26%, with a cumulative incidence of 9.9% (58).
Proper wound cleansing and debridement are important for open fractures, as is proper antibiotic therapy. There is no universal protocol on which antibiotics to use or on the exact duration of antibiotic therapy. There is consensus that antibiotic therapy should be started as early as possible. The antibiotic of choice should cover gram-positive organisms in Gustilo type I and II (59) fractures, such as cefazolin, and additional coverage for gram-negative organisms in patients with high-energy open fractures (Gustilo III), usually with an aminoglycoside. Some authors have stated that antibiotics should not be continued for more than 72 h after wound closure (59, 60, 61). However, in case of prolonged antibiotics therapy after 72 h, the participation of an infectious disease specialist will be required.
A number of authors recommend using local antibiotics in combination with systemic antibiotic therapy, although the literature is mixed and there is no strong evidence of their use (60, 61, 62). In terms of the form of lavage, antibacterial and antiseptic solutions and pulsatile lavage have not been shown to be superior to saline lavage; solutions can add toxicity, and pulsatile lavage can spread microorganisms to deeper areas (61). The authors advise that wound closure should be performed first if technically possible because this reduces the rate of infection and non-union. If this is not possible and soft tissue coverage is needed, it should be performed within the first 7 days. However, this is almost never done. Regarding negative pressure therapy, a number of studies have shown a decreased infection rate in open tibial fractures, the possibility of extending the time to definitive coverage, and a lower failure rate of definitive flaps (63, 64). However, other studies have shown no clear evidence for the advantage of this type of system over classic coverage (65, 66, 67, 68). There are authors who value its use only temporarily until definitive coverage and no longer than 1 week due to the risk of colonisation with resistant microorganisms (69).
Careful management of fasciotomy wounds after compartment syndrome is also important, and there are still contradictory results regarding whether it is better to close the wounds simultaneously with definitive osteosynthesis or to close them prior to the latter (70, 71).
As for the external fixator in sequential treatment, the potential relationship between pin overlap with the definitive osteosynthesis site and infection has not been demonstrated (72). Another surgeon-dependent factor is surgical time, which is clearly related to fracture complexity; each extra hour of surgery in tibial plateau fractures can increase the infection rate by 78% (73).
Early infection vs late infection and osteomyelitis
As for the chronicity of infection, there are specific classifications according to the time of evolution: early infection (<2 weeks), delayed infection (2–10 weeks), and late infection (>10 weeks) (62). However, rather than determining a figure in weeks, it is important to understand certain aspects of pathogenesis. The biofilm has not yet formed in the first 2 weeks. After that point, it forms and adheres to the implant, and such that if the infection is not eradicated, bone involvement (osteomyelitis) will occur. At this point, the therapeutic strategy needs to be changed.
Early and delayed post-surgical infection
Diagnosis
The diagnosis of an acute infection is eminently clinical: inflammation, flushing, increased temperature, fluctuation, purulent drainage or dehiscence of the surgical wound, accompanied or not by systemic symptoms such as general malaise and fever, with analytical data (leucocytosis, elevated C-reactive protein, and erythrocyte sedimentation rate) supporting the diagnosis (74). In terms of culture collection, it is preferable to take deep cultures (five samples) during surgical debridement (75); if performed superficially, there is a risk of skin germ contamination.
Treatment
Once the diagnosis has been performed, there are two possible situations: the fracture has consolidated or the fracture has not consolidated. If the fracture has not yet healed (often the case when the onset of infection is very early), aggressive lavage and debridement of the devitalised areas, removal of unnecessary foreign bodies (broken screws, sutures, etc.), and hardware retention should be performed (76, 77). Despite the dilemma of maintaining hardware in an area of infection, fracture stability is important not only for fracture healing but also for resolving the infection (78, 79). If the fracture has healed, the hardware can be removed during lavage and debridement. If there is suspected joint extension and secondary septic arthritis (either clinically or by arthrocentesis), joint lavage (usually arthroscopic) should be performed. Antibiotic therapy should ideally begin once samples have been taken unless the patient is in a septic state. The treatment will be empirical until a microbiological diagnosis of the pathogen has been reached, the most frequent being S. aureus (76). After determining the pathogen, a specific antibiotic should be chosen. The duration of the antibiotic therapy is unclear, and there appears to be no difference between prolonged courses (6–12 weeks) of i.v. antibiotics with 1-week courses of i.v. antibiotics followed by oral antibiotics (80). It is paramount to respect antimicrobial local and international guidelines, the notion of multidisciplinary approach, or the referral of patient to reference centres.
If maintaining the hardware fails to eradicate the infection, more aggressive debridement, hardware removal, and placement of an external fixator should be considered until the infection; reconstructive surgery should then be considered, depending on the state of consolidation and the bone defect to be addressed (19). In cases of bone defects, the literature suggests local antibiotic therapy in the form of polymethyl methacrylate (PMMA) or resorbable antibiotic-eluting ceramic bone substitutes combined with systemic antibiotherapy until definitive surgery (81, 82). Figure 4 presents a case of surgical wound infection.
Figure 4.
(A, B and C). Surgical wound infection after open reduction and internal fixation (ORIF) of a tibial plateau fracture (A). This infection resulted in a soft tissue defect requiring debridement. Wound after debridement (B). To resolve the soft tissue defect, gastrocnemius rotational flap coverage was performed (C).
Late infections. Osteomyelitis
When the infection has not been eradicated, bone involvement and subsequent osteomyelitis can occur after a few weeks. In these cases, the clinical picture might not be as striking as in acute infection, and the inflammatory laboratory parameters might not be elevated. Persistent pain and the development of a fistula are common (60). To diagnose bone involvement, the imaging tests of choice are MRI and PET (83).
Septic non-union is defined as the absence of evidence of fracture healing and persistence of infection at the fracture site for 6–8 months (84, 85). The core principles are removal of infected tissue, dead-space management, and antibiotic therapy. The majority (84.5%) of patients presented with stage III or IV disease according to the Cierny–Mader classification (86), and Staphylococcus aureus was the most commonly isolated organism. The proportion of patients achieving remission with no recurrence during follow-up varies from 67.7 to 100% (87). The treatment of osteomyelitis requires a multidisciplinary approach. It is therefore advisable to send these patients to a center that has an 'Infectious Disease Unit'.
Often sequential treatment will be needed with the first stage of debridement and placement of an external fixator and PMMA spacers with an antibiotic, and a second stage, when the infection is resolved, to repair the bone defect and perform soft tissue coverage, generally with the collaboration of a plastic surgeon (83). Recently, a number of authors have suggested the possibility of performing radical debridement and reconstruction of both the bone defect and soft tissue in the same stage, with good results (88).
Malunion
Collapse or irregularity of the articular surface or deformity of the metaphyseal–diaphyseal junction after surgical treatment of tibial plateau fractures can trigger a malunion of the fracture, resulting in knee osteoarthritis or alteration of the mechanical axis of the lower limb. A suboptimal result after surgery justifies early re-osteosynthesis, otherwise, the result will inevitably be malunion (89).
No clear incidence of malunions after these fractures has been reported, probably because there is no clear radiological definition of malunion (90). Age over 60 years, osteoporosis, early weight-bearing, and fracture displacement and comminution have been reported as risk factors (23). A study of 44 malunions found that 79% of the patients older than 60 years experienced malunions vs 7% of the patients younger than 60 years (8).
Evaluation and diagnosis
The type of malunion depends on the type of tibial plateau fracture and can be intra-articular, extra-articular, or combined, an important consideration for treatment options. Extra-articular fractures of type A2 or A3 of the AO classification (5) will have extra-articular malunions in varus, valgus, flexion, or extension. Partial articular fractures (B1, B2, or B3) will have intra-articular malunions, which if associated with subsidence (B2, B3), will also produce malalignments in varus or valgus depending on the plateau affected (lateral or medial), with valgus malalignment more frequent due to subsidence of the lateral plateau. Type C fractures can give rise to a combined intra-articular and extra-articular malunion, given their metaphyseal extension (91).
To correctly diagnose the type of malunion, anterior-posterior (AP), lateral, and long-leg standing radiographs of the lower limbs are recommended to quantify the alteration of the mechanical axis, if present (92). The angles established by Paley et al. between the joint line and mechanical axis can also be measured (93). CT scans should be included to analyse the irregularity of the articular surface and confirm fracture healing (94). MRI can be useful to detect associated meniscal or ligamentous injuries (95).
Treatment
For elderly patients or those with previous knee osteoarthritis who have significant joint damage that cannot be reconstructed, the tendency will be to perform a TKA. In active and young patients, conservative surgery will be considered, based on the various types of corrective osteotomies. A joint collapse >5 mm, a varus or valgus malalignment >5°, and a change in posterior tibial slope >10° have been established as limits for considering malunion correction (7, 94).
In intra-articular malunions with plate collapse, usually lateral (Schatzker III sequelae), an intra-articular lateral tibial condyle elevation osteotomy supported by bone graft or bone substitute and fixed by plate should be performed. A number of authors have suggested the addition of an extra-articular osteotomy for further axis correction (96). If there is subsidence separation (Schatzker II sequelae), it is advisable to first perform an osteotomy in the sagittal plane of the separation area, and after elevating the subsided area, compress the fragment with a plate to narrow the widened metaphyseal area. In cases of small subsidence (<3 mm), a number of authors have advocated for simply performing an extra-articular osteotomy, which is technically less demanding (91). Isolated medial plateau subsidence is exceptional. The medial plateau usually has fracture patterns with large posteromedial fragments without major comminution (90). Figure 5 shows a case of an intra-articular valgus malunion and its treatment.
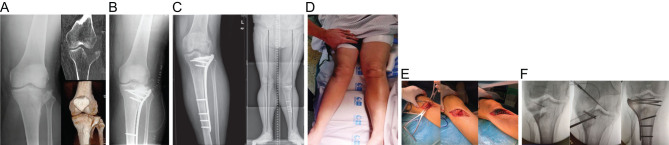
Figure 5.
(A, B, C, D, E and F). Schatzker type II tibial plateau fracture with extensive involvement of the external tibial plateau (A). Open reduction and internal fixation (ORIF) was performed (B). At 4 months, an intra-articular malunion was detected resulting in a valgus deformity (C). A clinical image of this deformity (D). The decision was made to perform an intra-articular osteotomy. Intraoperative images of the intra-articular osteotomy (E). Radiological images during correction and the final result of the operation (F).
In extra-articular malunions in varus, a medial tibial opening osteotomy is performed. In extra-articular malunions in valgus, a lateral tibial opening osteotomy is performed. In less common cases of recurvatum, a flexion osteotomy may be considered, and a deflexion osteotomy is an option in cases of flexion (91). Figure 6 shows a case of extra-articular varus malunion and its treatment. In combined malunions, several techniques can be combined, and treatment should be performed in two stages separated by 3–6 months to ensure consolidation (91). Table 4 shows a summary of the results from the literature on the treatment of malunions (94, 96, 97, 98, 99, 100).
Figure 6.

(A, B and C). Patient operated on in another country for bilateral tibial plateau fracture. An extra-articular varus malunion occurred in the left knee (A). The decision was made to perform an extra-articular medial opening osteotomy. Intra-operative images of this osteotomy (B). The final result of the operation (medial and lateral plate fixation) (C).
Table 4.
Results in the literature of corrective osteotomies in malunions after tibial plateau fractures.
| Reference | Year | Cases, n | Type of malunion | Surgical procedure | Results |
|---|---|---|---|---|---|
| Kerkhoffs et al. (96) | 2008 | 23 | Malunion in valgus plus lateral tibial plateau collapse | Lateral opening varus osteotomy plus intra-articular osteotomy | 87% excellent and good results |
| Singh et al. (97) | 2011 | 7 | Varus malunion | Medial opening valgus osteotomy | 100% satisfaction |
| Sundararajan et al. (98) | 2017 | 18 | Varus malunion | Medial opening valgus osteotomy | 78% excellent and good results |
| Wang et al. (99) | 2017 | 13 | Postero-lateral fragment malunion | Intra-articular osteotomy by extended antero-lateral approach. | Lysholm score: 91.7 |
| Knee society score: 92.5 | |||||
| Visual analogue score: 0.5 | |||||
| Liangjun et al. (94) | 2019 | 25 | Different types | Technique according to type of malunion | 100% consolidation, no significant pain, and ambulation without aids. |
| Alm et al. (100) | 2020 | 23 | 16 lateral tibial plateau collapses, 7 medial plateau collapses | Intra-articular osteotomy | 73.9% excellent and good results |
In recent studies, a number of authors have performed these corrections using 3D printing models based on CT scans and patient-specific preformed guides, reporting that this method can help refine the design of osteotomies, especially in complex osteotomies with more than one plane (101, 102, 103, 104, 105). The method can also help reduce intraoperative bleeding, shorten surgical time, and improve outcomes.
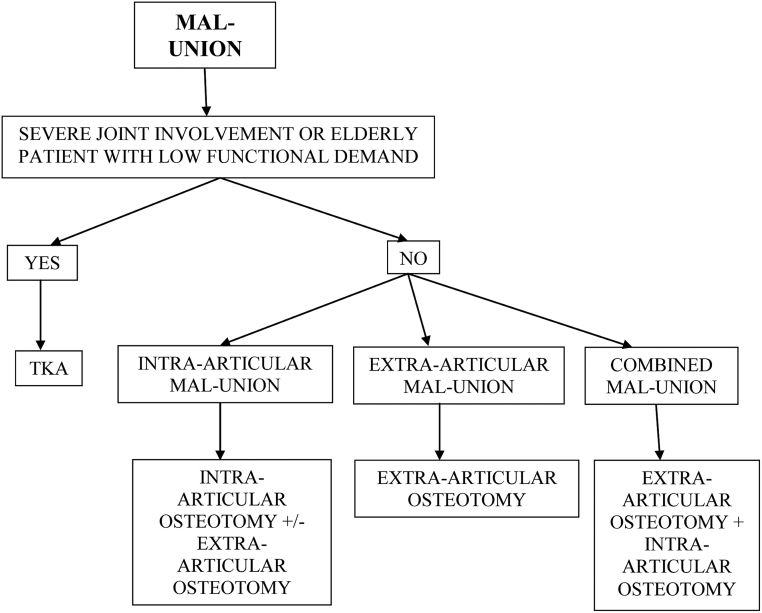
From the published results, it can be concluded that conservative surgery by intra-articular or extra-articular osteotomy is a useful technique for correcting malunions after tibial plateau fractures in young, active patients who do not have significant joint damage. Figure 7 summarises the surgical management of malunions.
Figure 7.
Management of malunions after the surgical treatment of tibial plateau fractures. TKA, total knee arthroplasty.
Non-union
Non-union is an infrequent complication in tibial plateau fractures treated with ORIF. The proximal tibia is a metaphyseal area with good vascularisation and abundant cancellous bone. In these fractures, there is generally good contact between the fragments, with wide fracture traces. Non-union rates in the literature range from 0.1 to 1.1%, depending on the series (1, 106). However, these rates might increase in high-energy fractures with extensive vascular and soft tissue involvement, raising the figure to 10–20% (1).
Diagnosis and management
The most common presenting symptom is pain (61.6%), followed by instability (22.6%) (107). An important diagnostic consideration is ruling out infection, based on clinical and laboratory parameters. If suspected, an MRI could detect a focus of osteomyelitis. There is not much data in the literature given the infrequency of this complication. Treatment is based on re-osteosynthesis with grafting, generally in the form of an iliac crest autograft (23, 108).
Post-traumatic osteoarthritis
In cases of severe joint involvement, the surgical option after the failure of conservative measures is TKA. In post-traumatic osteoarthritis; however, there are several aspects to consider that differ from primary TKA: possible soft tissue involvement, presence of hardware, possible occult infection given the history of surgery, possible malalignment, and knee instability and stiffness (108, 109, 110, 111).
Epidemiology
Although the rate of post-traumatic osteoarthritis following tibial plateau fractures ranges widely in the literature (21–44%) (111), the need for conversion to TKA is lower (0–15%) (104). Moreover, these figures seem to increase with time since the fracture. A study on a cohort of 8426 patients compared the rate of TKA after tibial plateau fracture with the rate in the general population at 2, 5, and 10 years (0.32% vs 0.29%, 5.3% vs 0.82%, and 7.3% vs 1.8%, respectively) (109). Advanced age, fracture severity, and limb malalignment were established as risk factors.
Results
A number of studies have reported high complication rates (26–33%), with high reoperation rates (21%) in TKA after tibial plateau fractures (43, 112, 113). However, improved understanding of the technique and the complications described in the first series seem to have helped to reduce these rates and bring them closer to those of primary TKA (111, 114).
Pinter et al. analysed 891 patients (933 knees) who experienced ORIF for a tibial plateau fracture. Of the 933 knees, a total of 20 knees (2.15%) required conversion from ORIF to TKA. Of the 20 knees that underwent conversion to TKA, 3 were performed as a 2-stage conversion. Of the 20 knees that underwent TKA, 7 experienced postoperative arthrofibrosis, 4 experienced postoperative infection, and 4 required revision (109).
Regarding the presence of previous hardware, a number of authors have recommended removing it months earlier to achieve proper soft tissue healing before definitive surgery and to reduce infection rates, which appear to be higher in cases of TKA with a history of osteosynthesis (114, 115). Previous surgery can lead to fibrosis and problems with the extensor apparatus, such as patella baja, which can hinder TKA placement and lead to serious complications such as patellar tendon pull-out. Therefore, in some cases, an anterior tibial tuberosity osteotomy should be considered, and patellar turn-down should be avoided (105). Metaphyseal bone defects might require filling with bone graft, metal supplements, metaphyseal cones, or sleeves. The use of tibial stems that extend beyond the osteosynthesis area may also be considered, especially if the hardware has been removed at the same time as the surgery (91). Regarding the type of prosthesis, previously known ligamentous instability might be encountered or detected during surgery, which will require more constrained designs such as a constrained condylar knee implant and a rotating hinge implant (114). Figures 8 and 9 show two cases of post-traumatic osteoarthritis of tibial plateau fractures treated with TKA.
Figure 8.
(A, B and C). Schatzker type II tibial plateau fracture with extensive involvement of the lateral tibial plateau (A), which was treated by open reduction and internal fixation (ORIF) (B). As a complication, the post-traumatic osteoarthritis was very painful and entailed significant functional limitation. It was therefore decided to implant a total knee arthroplasty (TKA) with a tibial metaphyseal sheath (C).
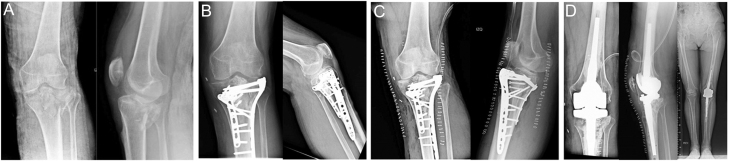
Figure 9.
(A, B, C and D). 67-year-old female patient with Schatzker type VI tibial plateau fracture (A) treated by open reduction and internal fixation (ORIF) (B). After 7 months of progression, an intra-articular malunion was detected with major joint involvement associated with obvious ligament instability at the varus-valgus (C). It was therefore decided to implant a rotating hinge total knee arthroplasty (TKA) (D).
Residual knee instability secondary to ligaments damage that was not addressed initially, during fixation
The reported incidence rates of ligament injuries in tibial plateau fractures are as follows: anterior cruciate ligament (ACL) 26%, posterior cruciate ligament (PCL) 7%, medial collateral ligament (MCL) 24%, and lateral collateral ligament (LCL) 14%. Medial collateral ligament injury was the most common in the Schatzker type 2 (50% of the injuries) (116).
According to Lin et al., tibial plateau fractures are often accompanied by ligamental and meniscal injuries (117). Among these, the combined existence of Schatzker type IV fracture with ACL avulsion has been published rarely. Ninety-nine Schatzker type IV tibial plateau fractures were analysed by quantitative three-dimensional measurements. ACL avulsions were diagnosed through the data of CT scan and MRI. There were more ACL avulsions and more displaced ACL avulsions associated with the knee in flexion in the setting of Schatzker type IV fracture. More ACL avulsions were encountered in the injury pattern of flexion-valgus than in the other injury patterns of the same level. The rotation of the tibial showed no significant difference in producing ACL avulsion fractures. This study observed that a flexed knee at the occurrence of a Schatzker type IV tibial plateau fracture is a high-risk factor for causing associated ACL avulsion and producing more displaced avulsions. Flexion-valgus pattern was the main cause of Schatzker type IV fractures associated with ACL avulsions. The findings will help orthopaedic surgeons understand the injury mechanism and augment their awareness of such injuries to avoid unfavourable prognosis (117).
Once the ACL tear has been diagnosed, it is reasonable to perform an ACL reconstruction (ACLR) (118). Some authors recommend adding a lateral extra-articular tenodesis to reduce anterolateral rotatory laxity. Anterolateral complex (ALC) deficiency has been shown to be a major cause of high-grade anterolateral rotatory laxity. The lateral extra-articular tenodesis (LET) procedure is therefore designed to augment ACLR and reduce anterolateral rotation. The aim of adding LET to ACLR is to reduce the strain on the ACLR graft, reduce the prevalence of the pivot shift, and thereby potentially reduce the rate of ACLR graft failure (119). Finally, there is much debate, which should be clarified in future research, as to whether any type of biological augmentation should be associated with ACLR such as platelet-rich plasma (PRP) (120).
Conclusions
The gold standard for treating tibial plateau fractures is surgical: ORIF to restore joint congruence and achieve an adequate mechanical axis, stable knee, and early mobilisation. The complications of this treatment have been decreasing over the decades due to the increased understanding and management of these fractures, especially with regard to advances in osteosynthesis techniques and the management of soft tissue, which is often severely affected in high-energy fractures. The treatment options for knee stiffness are MUA when the knee stiffness lasts less than 3 months, arthroscopic release when it lasts generally between 3 and 6 months, and open release for refractory cases or cases lasting more than 6 months. A number of authors have recommended early arthroscopic release in conjunction with MUA.
Infectious complication rates of tibial plateau fractures treated by ORIF have been decreasing in recent years thanks to sequential treatment in two stages and new osteosynthesis techniques, with new minimally invasive approaches, less tendency to desperiostisation, and improved implants. The treatment of infection will be based on two important issues: fracture healing and bone involvement in the form of osteomyelitis. If the fracture has healed, the hardware can be removed, and lavage and debridement combined with antibiotic therapy can be performed. If the fracture has not healed, the hardware is retained, and lavage, debridement, and antibiotic therapy are performed, sometimes more than once, until the fracture heals. Fracture stability is important not only for healing but also for resolving the infection. In cases of osteomyelitis, a two-stage treatment is recommended: aggressive debridement of devitalised tissue and bone, antibiotic spacer, and temporary external fixation until the infection has resolved (first stage), followed by definitive surgery with grafting or soft tissue coverage depending on the defect (second stage).
Conservative surgery employing intra-articular or extra-articular osteotomies is a good option for malunion correction in young, active patients without significant joint damage. When a malunion with extensive joint involvement has been established or the initial cartilage damage has resulted in knee osteoarthritis, the surgical option is TKA. It is reasonable to consider hardware removal months before TKA implantation, given that it appears to decrease infection rates after TKA.
ICMJE Conflict of Interest Statement
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding Statement
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
References
- 1.Reátiga Aguilar J, Rios X, González Edery E, De La Rosa A, Arzuza Ortega L. Epidemiological characterization of tibial plateau fractures. Journal of Orthopaedic Surgery and Research 202217 106. ( 10.1186/s13018-022-02988-8) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kugelman D, Qatu A, Haglin J, Leucht P, Konda S, Egol K. Complications and unplanned outcomes following operative treatment of tibial plateau fractures. Injury 2017482221–2229. ( 10.1016/j.injury.2017.07.016) [DOI] [PubMed] [Google Scholar]
- 3.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clinical Orthopaedics and Related Research 197913894–104. [PubMed] [Google Scholar]
- 4.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. Journal of Orthopaedic Trauma 201024683–692. ( 10.1097/BOT.0b013e3181d436f3) [DOI] [PubMed] [Google Scholar]
- 5.Kfuri M, Schatzker J. Revisiting the Schatzker classification of tibial plateau fractures. Injury 2018492252–2263. ( 10.1016/j.injury.2018.11.010) [DOI] [PubMed] [Google Scholar]
- 6.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. Journal of Orthopaedic Trauma 201832 (Supplement 1) S1–S170. ( 10.1097/BOT.0000000000001063) [DOI] [PubMed] [Google Scholar]
- 7.Mthethwa J, Chikate A. A review of the management of tibial plateau fractures. Musculoskeletal Surgery 2018102119–127. ( 10.1007/s12306-017-0514-8) [DOI] [PubMed] [Google Scholar]
- 8.Malik S, Herron T, Mabrouk A, Rosenberg N. Tibial plateau fractures. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022 [PubMed] [Google Scholar]
- 9.Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systematic review of the literature. Archives of Orthopaedic and Trauma Surgery 20081281169–1175. ( 10.1007/s00402-007-0520-7) [DOI] [PubMed] [Google Scholar]
- 10.Tahir M, Kumar S, Shaikh SA, Jamali AR. Comparison of postoperative outcomes between open reduction and internal fixation and Ilizarov for Schatzker type V and type VI fractures. Cureus 201911e4902. ( 10.7759/CUREUS.4902) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Subash Y.Evaluation of functional outcome following hybrid external fixation in the management of Schatzkers type V and VI tibial plateau fractures - a prospective study of 30 patients. Malaysian Orthopaedic Journal 20211548–54. ( 10.5704/MOJ.2103.008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raza A, Kumar S, Kumar D, Qadir A, Muzzammil M, Lakho MT. Complex tibial plateau fractures: primary fixation using the Ilizarov external fixator. A two-year study at civil hospital Karachi, Pakistan. Cureus 201911e5375. ( 10.7759/CUREUS.5375) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bertrand ML, Pascual-López FJ, Guerado E. Severe tibial plateau fractures (Schatzker V-VI): open reduction and internal fixation versus hybrid external fixation. Injury 201748 (Supplement 6) S81–S85. ( 10.1016/S0020-1383(1730799-4) [DOI] [PubMed] [Google Scholar]
- 14.Malakasi A, Lallos SN, Chronopoulos E, Korres DS, Efstathopoulos NE. Comparative study of internal and hybrid external fixation in tibial condylar fractures. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie 20132397–103. ( 10.1007/s00590-011-0911-x) [DOI] [PubMed] [Google Scholar]
- 15.Gross JB, Gavanier B, Belleville R, Coudane H, Mainard D. Advantages of external hybrid fixators for treating Schatzker V-VI tibial plateau fractures: a retrospective study of 40 cases. Orthopaedics and Traumatology, Surgery and Research 2017103965–970. ( 10.1016/j.otsr.2017.05.023) [DOI] [PubMed] [Google Scholar]
- 16.Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. Journal of Orthopaedic Trauma 1987197–119. ( 10.1097/00005131-198702010-00001) [DOI] [PubMed] [Google Scholar]
- 17.Gaston P, Will EM, Keating JF. Recovery of knee function following fracture of the tibial plateau. Journal of Bone and Joint Surgery. British Volume 2005871233–1236. ( 10.1302/0301-620X.87B9.16276) [DOI] [PubMed] [Google Scholar]
- 18.Pujol N, Boisrenoult P, Beaufils P. Post-traumatic knee stiffness: surgical techniques. Orthopaedics and Traumatology, Surgery and Research 2015101 (Supplement 1) S179–S186. ( 10.1016/j.otsr.2014.06.026) [DOI] [PubMed] [Google Scholar]
- 19.Muhm M, Schneider P, Ruffing T, Winkler H. Posterocentral approach to the posterior tibial plateau. Reconstruction of tibial plateau fractures and avulsions of the posterior cruciate ligament. Der Unfallchirurg 2014117813–821. ( 10.1007/s00113-013-2418-x) [DOI] [PubMed] [Google Scholar]
- 20.Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Reviews 20161225–232. ( 10.1302/2058-5241.1.000031) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury 200637475–484. ( 10.1016/j.injury.2005.06.035) [DOI] [PubMed] [Google Scholar]
- 22.Haller JM, Holt DC, McFadden ML, Higgins TF, Kubiak EN. Arthrofibrosis of the knee following a fracture of the tibial plateau. Bone and Joint Journal 201597–B109–114. ( 10.1302/0301-620X.97B1.34195) [DOI] [PubMed] [Google Scholar]
- 23.Kugelman DN, Qatu AM, Strauss EJ, Konda SR, Egol KA. Knee stiffness after tibial plateau fractures: predictors and outcomes (OTA-41). Journal of Orthopaedic Trauma 201832e421–e427. ( 10.1097/BOT.0000000000001304) [DOI] [PubMed] [Google Scholar]
- 24.Reahl GB, Marinos D, O'Hara NN, Howe A, Degani Y, Wise B, Maceroli M, O'Toole RV. Risk factors for knee stiffness surgery after tibial plateau fracture fixation. Journal of Orthopaedic Trauma 201832e339–e343. ( 10.1097/BOT.0000000000001237) [DOI] [PubMed] [Google Scholar]
- 25.Choo KJ, Morshed S, Morshed S. Postoperative complications after repair of tibial plateau fractures. Journal of Knee Surgery 20132711–19. ( 10.1055/s-0033-1363517) [DOI] [PubMed] [Google Scholar]
- 26.Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. Journal of Orthopaedic Trauma 200115312–320. ( 10.1097/00005131-200106000-00002) [DOI] [PubMed] [Google Scholar]
- 27.Bishop J, Agel J, Dunbar R. Predictive factors for knee stiffness after periarticular fracture: a case-control study. Journal of Bone and Joint Surgery: American Volume 2012941833–1838. ( 10.2106/jbjs.k.00659) [DOI] [PubMed] [Google Scholar]
- 28.Kraus TM, Martetschläger F, Müller D, Braun KF, Ahrens P, Siebenlist S, Stöckle U, Sandmann GH. Return to sports activity after tibial plateau fractures: 89 cases with minimum 24-month follow-up. American Journal of Sports Medicine 2012402845–2852. ( 10.1177/0363546512462564) [DOI] [PubMed] [Google Scholar]
- 29.Sassoon AA, Adigweme OO, Langford J, Koval KJ, Haidukewych GJ. Manipulation under anesthesia: a safe and effective treatment for posttraumatic arthrofibrosis of the knee. Journal of Orthopaedic Trauma 201529e464–e468. ( 10.1097/BOT.0000000000000395) [DOI] [PubMed] [Google Scholar]
- 30.Kraus TM, Abele C, Freude T, Ateschrang A, Stöckle U, Stuby FM, Schröter S. Duration of incapacity of work after tibial plateau fracture is affected by work intensity. BMC Musculoskeletal Disorders 201819281. ( 10.1186/S12891-018-2209-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. Journal of Bone and Joint Surgery. British Volume 200991426–433. ( 10.1302/0301-620X.91B4.20966) [DOI] [PubMed] [Google Scholar]
- 32.Rodríguez-Merchán EC.The stiff total knee arthroplasty: causes, treatment modalities and results. EFORT Open Reviews 20194602–610. ( 10.1302/2058-5241.4.180105) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zachwieja E, Perez J, Mack Hardaker WM, Levine B, Sheth N. Manipulation under anesthesia and stiffness after total knee arthroplasty. JBJS Reviews 20186 e2. ( 10.2106/JBJS.RVW.17.00113) [DOI] [PubMed] [Google Scholar]
- 34.Cheuy VA, Foran JRH, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis associated with total knee arthroplasty. Journal of Arthroplasty 2017322604–2611. ( 10.1016/j.arth.2017.02.005) [DOI] [PubMed] [Google Scholar]
- 35.Vaish A, Vaishya R, Bhasin VB. Etiopathology and management of stiff knees: a current concept review. Indian Journal of Orthopaedics 202155276–284. ( 10.1007/s43465-020-00287-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LaPrade RF, Pedtke AC, Roethle ST. Arthroscopic posteromedial capsular release for knee flexion contractures. Knee Surgery, Sports Traumatology, Arthroscopy 200816469–475. ( 10.1007/s00167-008-0496-z) [DOI] [PubMed] [Google Scholar]
- 37.Mariani PP.Arthroscopic release of the posterior compartments in the treatment of extension deficit of knee. Knee Surgery, Sports Traumatology, Arthroscopy 201018736–741. ( 10.1007/s00167-009-0920-z) [DOI] [PubMed] [Google Scholar]
- 38.Middleton AH, Perlewitz MA, Edelstein AI, Vetter CS. Knee arthrofibrosis following tibial plateau fracture treated with arthroscopic lysis of adhesions with manipulation. Journal of Knee Surgery 2020In press. ( 10.1055/s-0040-1718679) [DOI] [PubMed] [Google Scholar]
- 39.Kukreja M, Kang J, Curry EJ, Li X. Arthroscopic lysis of adhesions and anterior interval release with manipulation under anesthesia for severe post-traumatic knee stiffness: a simple and reproducible step-by-step guide. Arthroscopy Techniques 20198e429–e435. ( 10.1016/j.eats.2019.01.005) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gittings D, Hesketh P, Dattilo J, Zgonis M, Kelly J, Mehta S. Arthroscopic lysis of adhesions improves knee range of motion after fixation of intra-articular fractures about the knee. Archives of Orthopaedic and Trauma Surgery 20161361631–1635. ( 10.1007/s00402-016-2561-2) [DOI] [PubMed] [Google Scholar]
- 41.Kim YM, Joo YB. Prognostic factors of arthroscopic adhesiolysis for arthrofibrosis of the knee. Knee Surgery and Related Research 201325202–206. ( 10.5792/ksrr.2013.25.4.202) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Z, Li Y, Sun P, Sang P, Zhang C, Ren Y, Yang J, Zhu X, Huang W, Liu Y. All-arthroscopic release for treating severe knee extension contractures could improve the knee range of motion and the mid-term functional outcomes. Knee Surgery, Sports Traumatology, Arthroscopy 201927724–730. ( 10.1007/s00167-018-5022-3) [DOI] [PubMed] [Google Scholar]
- 43.Lunebourg A, Parratte S, Gay A, Ollivier M, Garcia-Parra K, Argenson JN. Lower function, quality of life, and survival rate after total knee arthroplasty for posttraumatic arthritis than for primary arthritis. Acta Orthopaedica 201586189–194. ( 10.3109/17453674.2014.979723) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klein W, Shah N, Gassen A. Arthroscopic management of postoperative arthrofibrosis of the knee joint: indication, technique, and results. Arthroscopy 199410591–597. ( 10.1016/s0749-8063(0580053-2) [DOI] [PubMed] [Google Scholar]
- 45.Judet J, Judet R, Lagrange J. Une technique de libération de l'appareil extenseur dans les raideurs du genou [Technique of liberation of the extensor apparatus in knee stiffness]. Memoires. Academie de Chirurgie 195682944–947. [PubMed] [Google Scholar]
- 46.Luo Y, Li H, Mei L, Mao X. Effects of Judet quadricepsplasty in the treatment of post-traumatic extension contracture of the knee. Orthopaedic Surgery 2021131284–1289. ( 10.1111/os.12950) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bidolegui F, Pereira SP, Pires RE. Safety and efficacy of the modified Judet quadricepsplasty in patients with post-traumatic knee stiffness. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie 202131549–555. ( 10.1007/s00590-020-02802-3) [DOI] [PubMed] [Google Scholar]
- 48.Shang P, Liu HX, Zhang Y, Xue EX, Pan XY. A mini-invasive technique for severe arthrofibrosis of the knee: a technical note. Injury 2016471867–1870. ( 10.1016/j.injury.2016.06.015) [DOI] [PubMed] [Google Scholar]
- 49.Zhang Y, Ye LY, Liu HX, Wen H. Quadriceps tendon pie-crusting release of stiff knees in total knee arthroplasty. Journal of Orthopaedic Science 201520669–674. ( 10.1007/s00776-015-0731-7) [DOI] [PubMed] [Google Scholar]
- 50.Burge JR, Sanchez HB, Wagner RA. Quadriceps and patellar tendon pie-crusting as a treatment for limited flexion in total knee arthroplasty. American Journal of Orthopedics 201443E83–E88. [PubMed] [Google Scholar]
- 51.Xu H, Ying J. A mini-invasive procedure for treating arthrofibrosis of the knee. Acta Orthopaedica et Traumatologica Turcica 201650424–428. ( 10.1016/j.aott.2016.06.006) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Blanco CE, Leon HO, Guthrie TB. Endoscopic quadricepsplasty: a new surgical technique. Arthroscopy 200117504–509. ( 10.1053/jars.2001.24062) [DOI] [PubMed] [Google Scholar]
- 53.Dhillon MS, Panday AK, Aggarwal S, Nagi ON. Extra articular arthroscopic release in post-traumatic stiff knees: a prospective study of endoscopic quadriceps and patellar release. Acta Orthopaedica Belgica 200571197–203. [PubMed] [Google Scholar]
- 54.Young MJ, Barrack RL. Complications of internal fixation of tibial plateau fractures. Orthopaedic Review 199423149–154. [PubMed] [Google Scholar]
- 55.Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. Journal of Orthopaedic Trauma 200418649–657. ( 10.1097/00005131-200411000-00001) [DOI] [PubMed] [Google Scholar]
- 56.Henkelmann R, Krause M, Alm L, Glaab R, Mende M, Ull C, Braun PJ, Katthagen C, Gensior TJ, Frosch KH, et al. Effect of fracturoscopy on the incidence of surgical site infections post tibial plateau fracture surgery. European Journal of Trauma and Emergency Surgery 2020461249–1255. ( 10.1007/s00068-020-01486-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bullock TS, Ornell SS, Naranjo JMG, Morton-Gonzaba N, Ryan P, Petershack M, Salazar LM, Moreira A, Zelle BA. Risk of surgical site infections in OTA/AO type C tibial plateau and tibial plafond fractures: a systematic review and meta-analysis. Journal of Orthopaedic Trauma 202236111–117. ( 10.1097/BOT.0000000000002259) [DOI] [PubMed] [Google Scholar]
- 58.Shao J, Chang H, Zhu Y, Chen W, Zheng Z, Zhabg H, Zhang Y. Incidence and risk factors for surgical site infection after open reduction and internal fixation of tibial plateau fracture: a systematic review and meta-analysis. International Journal of Surgery 201741176–182. ( 10.1016/j.ijsu.2017.03.085) [DOI] [PubMed] [Google Scholar]
- 59.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. Journal of Bone and Joint Surgery: American Volume 197658453–458. ( 10.2106/00004623-197658040-00004) [DOI] [PubMed] [Google Scholar]
- 60.Rupp M, Popp D, Alt V. Prevention of infection in open fractures: where are the pendulums now? Injury 202051 (Supplement 2) S57–S63. ( 10.1016/j.injury.2019.10.074) [DOI] [PubMed] [Google Scholar]
- 61.Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, Shohat N. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. Journal of Arthroplasty 2018331309, .e2–1314.e2. ( 10.1016/j.arth.2018.02.078) [DOI] [PubMed] [Google Scholar]
- 62.Metsemakers WJ, Kuehl R, Moriarty TF, Richards RG, Verhofstad MHJ, Borens O, Kates S, Morgenstern M. Infection after fracture fixation: current surgical and microbiological concepts. Injury 201849511–522. ( 10.1016/j.injury.2016.09.019) [DOI] [PubMed] [Google Scholar]
- 63.Blum ML, Esser M, Richardson M, Paul E, Rosenfeldt FL. Negative pressure wound therapy reduces deep infection rate in open tibial fractures. Journal of Orthopaedic Trauma 201226499–505. ( 10.1097/BOT.0b013e31824133e3) [DOI] [PubMed] [Google Scholar]
- 64.Sirisena R, Bellot GL, Puhaindran ME. The role of negative-pressure wound therapy in lower-limb reconstruction. Indian Journal of Plastic Surgery 20195273–80. ( 10.1055/s-0039-1687922) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu X, Zhang H, Cen S, Huang F. Negative pressure wound therapy versus conventional wound dressings in treatment of open fractures: a systematic review and meta-analysis. International Journal of Surgery 20185372–79. ( 10.1016/j.ijsu.2018.02.064) [DOI] [PubMed] [Google Scholar]
- 66.Iheozor-Ejiofor Z, Newton K, Dumville JC, Costa ML, Norman G, Bruce J. Negative pressure wound therapy for open traumatic wounds. Cochrane Database of Systematic Reviews 20187 CD012522. ( 10.1002/14651858.CD012522.pub2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Haidari S, Ijpma FFA, Metsemakers WJ, Maarse W, Vogely HC, Ramsde AJ, McNally MA, Govaert GAM. The role of negative-pressure wound therapy in patients with fracture-related infection: a systematic review and critical appraisal. BioMed Research International 20212021 7742227. ( 10.1155/2021/7742227) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jensen NM, Steenstrup S, Ravn C, Schmal H, Viberg B. The use of negative pressure wound therapy for fracture-related infections following internal osteosynthesis of the extremity: a systematic review. Journal of Clinical Orthopaedics and Trauma 202224 101710. ( 10.1016/j.jcot.2021.101710) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yusuf E, Jordan X, Clauss M, Borens O, Mäder M, Trampuz A. High bacterial load in negative pressure wound therapy (NPWT) foams used in the treatment of chronic wounds. Wound Repair and Regeneration 201321677–681. ( 10.1111/wrr.12088) [DOI] [PubMed] [Google Scholar]
- 70.Ruffolo MR, Gettys FK, Montijo HE, Seymour RB, Karunakar MA. Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. Journal of Orthopaedic Trauma 20152985–90. ( 10.1097/BOT.0000000000000203) [DOI] [PubMed] [Google Scholar]
- 71.Zura RD, Adams SB, Jeray KJ, Obremskey WT, Stinnett SS, Olson SA. & Southeastern Fracture Consortium Foundation. Timing of definitive fixation of severe tibial plateau fractures with compartment syndrome does not have an effect on the rate of infection. Journal of Trauma 2010691523–1526. ( 10.1097/TA.0b013e3181d40403) [DOI] [PubMed] [Google Scholar]
- 72.Laible C, Earl-Royal E, Davidovitch R, Walsh M, Egol KA. Infection after spanning external fixation for high-energy tibial plateau fractures: is pin site-plate overlap a problem? Journal of Orthopaedic Trauma 20122692–97. ( 10.1097/BOT.0b013e31821cfb7a) [DOI] [PubMed] [Google Scholar]
- 73.Colman M, Wright A, Gruen G, Siska P, Pape HC, Tarkin I. Prolonged operative time increases infection rate in tibial plateau fractures. Injury 201344249–252. ( 10.1016/j.injury.2012.10.032) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Metsemakers WJ, Morgenstern M, Senneville E, Borens O, Govaert GAM, Onsea J, Depypere M, Richards RG, Trampuz A, Verhofstad MHJ, et al. General treatment principles for fracture-related infection: recommendations from an international expert group. Archives of Orthopaedic and Trauma Surgery 20201401013–1027. ( 10.1007/s00402-019-03287-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Govaert GAM, Kuehl R, Atkins BL, Trampuz A, Morgenstern M, Obremskey WT, Verhofstad MHJ, McNally MA, Metsemakers WJ. & Fracture-Related Infection (FRI) Consensus Group. Diagnosing fracture-related infection: current concepts and recommendations. Journal of Orthopaedic Trauma 2020348–17. ( 10.1097/BOT.0000000000001614) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Morris BJ, Unger RZ, Archer KR, Mathis SL, Perdue AM, Obremskey WT. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. Journal of Orthopaedic Trauma 201327e196–e200. ( 10.1097/BOT.0b013e318284704e) [DOI] [PubMed] [Google Scholar]
- 77.Lin S, Mauffrey C, Hammerberg EM, Stahel PF, Hak DJ. Surgical site infection after open reduction and internal fixation of tibial plateau fractures. European Journal of Orthopaedic Surgery and Traumatology : Orthopedie Traumatologie 201424797–803. ( 10.1007/s00590-013-1252-8) [DOI] [PubMed] [Google Scholar]
- 78.Berkes M, Obremskey WT, Scannell B, Ellington JK, Hymes RA, Bosse M. & Southeast Fracture Consortium. Maintenance of hardware after early postoperative infection following fracture internal fixation. Journal of Bone and Joint Surgery: American Volume 201092823–828. ( 10.2106/JBJS.I.00470) [DOI] [PubMed] [Google Scholar]
- 79.Schmidt AH, Swiontkowski MF. Pathophysiology of infections after internal fixation of fractures. Journal of the American Academy of Orthopaedic Surgeons 20008285–291. ( 10.5435/00124635-200009000-00002) [DOI] [PubMed] [Google Scholar]
- 80.Li HK, Rombach I, Zambellas R, Walker AS, McNally MA, Atkins BL, Lipsky BA, Hughes HC, Bose D, Kümin M, et al. Oral versus intravenous antibiotics for bone and joint infection. New England Journal of Medicine 2019380425–436. ( 10.1056/NEJMoa1710926) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Pesch S, Hanschen M, Greve F, Ziskowski M, Seidl F, Kirchhoff C, Biberthaler P, Huber-Wagner S. Treatment of fracture-related infection of the lower extremity with antibiotic-eluting ceramic bone substitutes: case series of 35 patients and literature review. Infection 202048333–344. ( 10.1007/s15010-020-01418-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hake ME, Young H, Hak DJ, Stahel PF, Hammerberg EM, Mauffrey C. Local antibiotic therapy strategies in orthopaedic trauma: practical tips and tricks and review of the literature. Injury 2015461447–1456. ( 10.1016/j.injury.2015.05.008) [DOI] [PubMed] [Google Scholar]
- 83.Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. Journal of the American Academy of Orthopaedic Surgeons 200513417–427. ( 10.5435/00124635-200510000-00006) [DOI] [PubMed] [Google Scholar]
- 84.Meyer S, Weiland AJ, Willenegger H. The treatment of infected non-union of fractures of long bones. Study of sixty-four cases with a five to twenty-one-year follow-up. Journal of Bone and Joint Surgery. American Volume 197557836–842. ( 10.2106/00004623-197557060-00020) [DOI] [PubMed] [Google Scholar]
- 85.Struijs PA, Poolman RW, Bhandari M. Infected nonunion of the long bones. Journal of Orthopaedic Trauma 200721507–511. ( 10.1097/BOT.0b013e31812e5578) [DOI] [PubMed] [Google Scholar]
- 86.Cierny G, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clinical Orthopaedics and Related Research 20034147–24. ( 10.1097/01.blo.0000088564.81746.62) [DOI] [PubMed] [Google Scholar]
- 87.Arshad Z, Lau EJ, Aslam A, Thahir A, Krkovic M. Management of chronic osteomyelitis of the femur and tibia: a scoping review. EFORT Open Reviews 20216704–715. ( 10.1302/2058-5241.6.200136) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ruan W, Li M, Guo Q, Lin B. Gastrocnemius muscle flap with vancomycin/gentamicin-calcium sulfate and autogenous iliac bone graft for the phase I treatment of localized osteomyelitis after tibial plateau fracture surgery. Journal of Orthopaedic Surgery and Research 202116341. ( 10.1186/s13018-021-02496-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kloen P, Van Wulfften Palthe ODR, Nötzinger J, Donders JCE. Early revision surgery for tibial plateau fractures. Journal of Orthopaedic Trauma 201832585–591. ( 10.1097/BOT.0000000000001280) [DOI] [PubMed] [Google Scholar]
- 90.Van Nielen DL, Smith CS, Helfet DL, Kloen P. Early revision surgery for tibial plateau non-union and mal-union. HSS Journal 20171381–89. ( 10.1007/s11420-016-9529-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Saragaglia D, Rubens-Duval B, Pailhé R. Intra- and extra-articular proximal tibia malunion. Orthopaedics and Traumatology, Surgery and Research 2020106S63–S77. ( 10.1016/j.otsr.2019.03.018) [DOI] [PubMed] [Google Scholar]
- 92.Kfuri M, Schatzker J. Corrective intra-articular osteotomies for tibial plateau malunion. Journal of Knee Surgery 201730784–792. ( 10.1055/s-0037-1606261) [DOI] [PubMed] [Google Scholar]
- 93.Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthopedic Clinics of North America 199425425–465. ( 10.1016/S0030-5898(2031927-1) [DOI] [PubMed] [Google Scholar]
- 94.Liangjun J, Qiang Z, Zhijun P, Li H. Revision strategy for malunited tibial plateau fracture caused by failure of initial treatment. Acta Orthopaedica et Traumatologica Turcica 201953432–441. ( 10.1016/j.aott.2019.08.018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Miozari HH, Pagano F, Hoffmeyer P. Fractures du plateau tibial: rôle de l'Irm [Tibial head fractures: role of MRI?]. Revue Medicale Suisse 20073 2906–290, 2910–29. [PubMed] [Google Scholar]
- 96.Kerkhoffs GMMJ, Rademakers MV, Altena M, Marti RK. Combined intra-articular and varus opening wedge osteotomy for lateral depression and valgus malunion of the proximal part of the tibia. Journal of Bone and Joint Surgery: American Volume 2008901252–1257. ( 10.2106/JBJS.D.01816) [DOI] [PubMed] [Google Scholar]
- 97.Singh H, Singh VR, Yuvarajan P, Maini L, Gautam VK. Open wedge osteotomy of the proximal medial tibia for malunited tibial plateau fractures. Journal of Orthopaedic Surgery 20111957–59. ( 10.1177/230949901101900113) [DOI] [PubMed] [Google Scholar]
- 98.Sundararajan SR, Nagaraja HS, Rajasekaran S. Medial open wedge high tibial osteotomy for varus malunited tibial plateau fractures. Arthroscopy 201733586–594. ( 10.1016/j.arthro.2016.08.027) [DOI] [PubMed] [Google Scholar]
- 99.Wang Y, Luo C, Hu C, Sun H, Zhan Y. An innovative intra-articular osteotomy in the treatment of posterolateral tibial plateau fracture malunion. Journal of Knee Surgery 201730329–335. ( 10.1055/s-0036-1584922) [DOI] [PubMed] [Google Scholar]
- 100.Alm L, Frings J, Krause M, Frosch KH. Intraarticular osteotomy of malunited tibial plateau fractures: an analysis of clinical results with a mean follow-up after 4 years. European Journal of Trauma and Emergency Surgery 2020461203–1209. ( 10.1007/s00068-020-01440-y) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hsu CP, Lin SC, Nazir A, Wu Te CT, Chang SS, Chan YS. Design and application of personalized surgical guides to treat complex tibial plateau malunion. Computer Methods in Biomechanics and Biomedical Engineering 202124419–428. ( 10.1080/10255842.2020.1833193) [DOI] [PubMed] [Google Scholar]
- 102.Pagkalos J, Molloy R, Snow M. Bi-planar intra-articular deformity following malunion of a Schatzker V tibial plateau fracture: correction with intra-articular osteotomy using patient-specific guides and arthroscopic resection of the tibial spine bone block. Knee 201825959–965. ( 10.1016/j.knee.2018.05.015) [DOI] [PubMed] [Google Scholar]
- 103.Yang P, Du D, Zhou Z, Lu N, Fu Q, Ma J, Zhao L, Chen A. 3D printing-assisted osteotomy treatment for the malunion of lateral tibial plateau fracture. Injury 2016472816–2821. ( 10.1016/j.injury.2016.09.025) [DOI] [PubMed] [Google Scholar]
- 104.Wang H, Newman S, Wang J, Wang Q, Wang Q. Corrective osteotomies for complex intra-articular tibial plateau malunions using three-dimensional virtual planning and novel patient-specific guides. Journal of Knee Surgery 201831642–648. ( 10.1055/s-0037-1605563) [DOI] [PubMed] [Google Scholar]
- 105.Fürnstahl P, Vlachopoulos L, Schweizer A, Fucentese SF, Koch PP. Complex osteotomies of tibial plateau malunions using computer-assisted planning and patient-specific surgical guides. Journal of Orthopaedic Trauma 201529e270–e276. ( 10.1097/BOT.0000000000000301) [DOI] [PubMed] [Google Scholar]
- 106.King GJW, Schatzker J. Nonunion of a complex tibial plateau fracture. Journal of Orthopaedic Trauma 19915209–212. ( 10.1097/00005131-199105020-00016) [DOI] [PubMed] [Google Scholar]
- 107.Obana KK, Lee G, Lee LSK. Characteristics, treatments, and outcomes of tibial plateau nonunions: a systematic review. Journal of Clinical Orthopaedics and Trauma 202116143–148. ( 10.1016/j.jcot.2020.12.017) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wang JY, Cheng CY, Chen ACY, Chan YS. Arthroscopy-assisted corrective osteotomy, reduction, internal fixation and rtrut allograft augmentation for tibial plateau malunion or nonunion. Journal of Clinical Medicine 202091–12. ( 10.3390/jcm9040973) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pinter Z, Jha AJ, McGee A, Paul K, Lee S, Dombrowski A, Naranje S, Shah A. Outcomes of knee replacement in patients with posttraumatic arthritis due to previous tibial plateau fracture. European Journal of Orthopaedic Surgery and Traumatology: Orthopedie Traumatologie 202030323–328. ( 10.1007/s00590-019-02575-4) [DOI] [PubMed] [Google Scholar]
- 110.Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. Journal of Bone and Joint Surgery: American Volume 201496144–150. ( 10.2106/JBJS.L.01691) [DOI] [PubMed] [Google Scholar]
- 111.Abdel MP, von Roth P, Cross WW, Berry DJ, Trousdale RT, Lewallen DG. Total knee arthroplasty in patients with a prior tibial plateau fracture: a long-term report at 15 years. Journal of Arthroplasty 2015302170–2172. ( 10.1016/j.arth.2015.06.032) [DOI] [PubMed] [Google Scholar]
- 112.Weiss NG, Parvizi J, Trousdale RT, Bryce RD, Lewallen DG. Total knee arthroplasty in patients with a prior fracture of the tibial plateau. Journal of Bone and Joint Surgery: American Volume 200385218–221. ( 10.2106/00004623-200302000-00006) [DOI] [PubMed] [Google Scholar]
- 113.Saleh KJ, Sherman P, Katkin P, Windsor R, Haas S, Laskin R, Sculco T. Total knee arthroplasty after open reduction and internal fixation of fractures of the tibial plateau: a minimum five-year follow-up study. Journal of Bone and Joint Surgery: American Volume 2001831144–1148. ( 10.2106/00004623-200108000-00002) [DOI] [PubMed] [Google Scholar]
- 114.Lizaur-Utrilla A, Collados-Maestre I, Miralles-Muñoz FA, Lopez-Prats FA. Total knee arthroplasty for osteoarthritis secondary to fracture of the tibial plateau. A prospective matched cohort study. Journal of Arthroplasty 2015301328–1332. ( 10.1016/j.arth.2015.02.032) [DOI] [PubMed] [Google Scholar]
- 115.Suzuki G, Saito S, Ishii T, Motojima S, Tokuhashi Y, Ryu J. Previous fracture surgery is a major risk factor of infection after total knee arthroplasty. Knee Surgery, Sports Traumatology, Arthroscopy 2011192040–2044. ( 10.1007/s00167-011-1525-x) [DOI] [PubMed] [Google Scholar]
- 116.Ebrahimzadeh MH, Birjandinejad A, Moradi A, Fathi Choghadeh M, Rezazadeh J, Omidi-Kashani F. Clinical instability of the knee and functional differences following tibial plateau fractures versus distal femoral fractures. Trauma Monthly 201520 e21635. ( 10.5812/traumamon.21635) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Liu Z, Wang S, Tian X, Peng A. The relationship between the injury mechanism and the incidence of ACL avulsions in Schatzker type IV tibial plateau fractures: a 3D quantitative analysis based on mimics software. Journal of Knee Surgery 2022In press. ( 10.1055/s-0041-1740929) [DOI] [PubMed] [Google Scholar]
- 118.Rodriguez-Merchan EC.Evidence-based ACL reconstruction. Archives of Bone and Joint Surgery 201539–12. [PMC free article] [PubMed] [Google Scholar]
- 119.Jesani S, Getgood A. Modified Lemaire lateral extra-articular tenodesis augmentation of anterior cruciate ligament reconstruction. JBJS Essential Surgical Techniques 20199 e41.1-7. ( 10.2106/JBJS.ST.19.00017) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rodríguez-Merchán EC.Anterior cruciate ligament reconstruction: is biological augmentation beneficial? International Journal of Molecular Sciences 202122 12566. ( 10.3390/ijms222212566) [DOI] [PMC free article] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a