Abstract
Purpose
Epileptic seizures frequently result in distinct physical injuries, fractures, traumatic brain injuries and minor trauma. The aim of this study was to retrospectively determine the frequent injury patterns due to seizure episode and to analyze consecutive acute medical care.
Methods
This retrospective mono-center study was conducted at Frankfurt University Hospital, Frankfurt am Main, Germany between January 2007 and December 2017. Epilepsy patients with seizure-related fractures admitted to the emergency department were identified via a retrospective systematic query in the hospital information system using the ICD-10 German modification codes G40.0–G40.9. Patients with an unclear diagnosis of epilepsy were excluded. Sociodemographic as well as disease specific aspects were analyzed. Descriptive and Kruskal–Wallis one-way analysis of variance were used for statistical analysis.
Results
A total number of 62 epilepsy patients were included. The mean age was 58.1 years. Fractures concerned the upper extremity most frequently (43.5%, n = 20), and 70.0% (14/20) were humerus fractures. Admission to intensive care unit for acute trauma care was necessary in 29.0% patients (n = 18), and surgery in 45.2% patients (n = 28). Twenty-five patients (26.6%) showed clinical or radiological signs of traumatic brain injury. Provoking factors were identified in 20 patients (32.3%), i.e., acute withdrawal or excess of alcohol (n = 15), relevant sleep deprivation (n = 2), and intoxication or withdrawal of other illegal drugs or trivial infect (n = 1 for each) and non-compliance with anti-seizure drugs (n = 1). A decreased T-score (−1.04 ± 1.15) and Z-score (−0.84 ± 0.75) compared to healthy subjects were found.
Conclusion
Fractures in upper extremities, trunk and craniocerebral trauma occur frequently as seizure-induced injuries. Alcohol excess and withdrawal are important provoking factors and should be targeted with preventive measurements to avoid seizure related injuries and accidents.
Keywords: Epilepsy, Wounds and injuries, Falls, Quality of life
Introduction
Epilepsy is a chronic neurological disorder characterized by sporadic and mostly unpredictable epileptic seizures affecting about 50 million people worldwide, accounting for 1% of the global burden of diseases.1,2 Clinical semiology of seizures differs depending on the individual etiology of epilepsy itself as well as the seizure onset and symptomatic zones, ranging from subclinical to clinical apparent seizures with or without motor symptoms or impaired awareness. Epileptic seizures frequently result in distinct physical injuries, fractures, traumatic brain injuries and minor trauma.3, 4, 5, 6 This has even been reported in the protected setting of an inpatient video-EEG-monitoring with maximum safety measures, e.g. padded bed grids, permanent video surveillance and rapid intervention after seizure onset.7
Seizure-related injuries have been shown to be associated with a decreased quality of life compared to healthy subjects and to go along with a high prevalence of depression and anxiety disorders.8, 9, 10, 11 Moreover, a two to six-fold increased risk for fractures in patients with epilepsy has been revealed.1,12,13 Additionally, compared to the general population, patients with epilepsy are more frequently admitted to hospitals following an injury.14,15 Due to frequent hospitalization, progressive disability and the need for continuous medical treatment, seizure-related injuries present a major medical and economic burden for patients, their caregivers and societies worldwide.16,17 Multiple studies have been performed to identify disease specific factors causing the increased injury-risk in patients with epilepsy, such as seizure semiology, impaired balance due to anti-seizure drugs (ASD) and ASD-induced reduced bone mineral density.13,15,18,19
The aim of this study was to determine the frequent injury patterns due to seizure-related injuries and to analyze consecutive acute medical care.
Methods
Study settings and design
This retrospective analysis was conducted at the Department of Trauma, Hand and Reconstructive Surgery at the University Hospital Frankfurt am Main, Germany in cooperation with the Epilepsy Center Frankfurt Rhine-Main. As a tertiary hospital and national trauma center with an associated nationwide epilepsy center as well as a large combined rural and metropolitan catchment area, the University Hospital Frankfurt provides specialized and interdisciplinary medical care for more than 320,000 patients per year. For the present analysis, all patients ≥ 18 years of age with confirmed epileptic seizures being admitted to our level I trauma center between January 2007 and December 2017 were suitable. To confirm the epileptic seizure and its etiology, cases were re-evaluated by a specialized neurologist from the Epilepsy Center Frankfurt Rhine-Main.
Approval of the local ethics committee was attained (Frankfurt am Main, approval 52/18), while this study followed the STROBE guidelines for observational studies (Strengthening the Reporting of Observational Studies in Epidemiology) as well as RECORD guidelines (REporting of studies Conducted using Observational Routinely-collected health Data).19, 20, 21
Data acquisition and statistical analysis
A retrospective systematic query in the hospital information system was performed using the International Statistical Classification of Diseases and Related Health Problems Version 10 (ICD-10) codes G40.0-G40.9 of the German Diagnosis Related Groups (G-DRG). All patients were double-checked in relation to the G-DRG code and clinical information by two independent raters. Patients with injuries that were not directly related to seizures or with unclear etiology were strictly excluded from the analysis to avoid a bias of the results due to the enrollment of subjects with psychogenic non-epileptic seizures, panic-attacks or other non-epileptic episodes. Patient's characteristics as well as disease specific aspects, including age, gender, mechanism of injury, injury pattern, length of stay and treatment options, were manually transferred from the hospital information system to a digital database. To minimize transcription errors, a double entry method was employed, and random sample checks were performed.
Statistical analyses were performed with IBM SPSS Statistics 22 (SPSS Inc., Chicago, IL, USA) by using Kruskal–Wallis one-way analysis of variance.
Results
Age, gender and disease specific characteristics
Following the given inclusion and exclusion criteria, a total number of 62 patients were enrolled in the study. The ratio of male to female patients was 1.8:1 with 22 (35.5%) female and 40 male (64.5%) subjects. The mean age was 58.1 years (SD 17.8 years, median 57 years, range 21–86 years). Overall, 26 patients (41.9%) were admitted to the hospital due to their first seizure, while 58.1% (n = 36) had an already known epilepsy at admission. Among these, an active epilepsy was diagnosed in 27.4% (n = 17) with a mean duration of 6 years (median 1 year, Q1 1 year, Q3 10 years, range 0–44 years). Regarding seizure semiology that led to the admission, focal seizures were documented in 19.4% (n = 12), primary generalized tonic-clonic seizures in 14.5% (n = 9) and secondary generalized tonic-clonic seizures in 66.1% (n = 41).
Mechanism of injury, setting and provoking factors
Most frequent mechanisms of injury were ictal or peri-ictal falls. In addition, one high-energy trauma due to a car accident was reported. Overall, most of seizure related injuries occurred at work or on the way to or from work, while fewer seizures took place in home environment. Seizure provoking factors were identified in approximately one third of the enrolled patients, i.e., withdrawal or excess of alcohol, sleep deprivation, intoxication or withdrawal of other illegal drugs, trivial infects and non-compliance with ASD. In patients with seizures due to alcohol intoxication, the mean blood alcohol level at admission was 3.2‰ (±1.2‰, median 3.5‰, range 1.5‰–5.0‰). More information on injury mechanism, setting and provoking factors are given in Table 1. Bone density measurements were available from 42 patients (67.7%) and were performed via standardized dual-energy X-ray absorptiometry scans. A lightly decreased T-score (−1.04 ± 1.15) and Z-score (−0.84 ± 0.75) was found in the patient collective compared to healthy subjects.
Table 1.
Injury mechanism, setting and provoking factors of the cohort of epilepsy patients (n = 62).
| Variables | n (%) |
|---|---|
| Injury mechanism | |
| Ictal or periictal fall | 61 (98.4) |
| High-speed trauma | 1 (1.6) |
| Injury setting | |
| Home environment | 26 (41.9) |
| Work environment | 35 (56.5) |
| Car accident | 1 (1.6) |
| Provoking factors | |
| Infection | 1 (1.6) |
| Sleep deprivation | 2 (3.2) |
| Non-compliance with medication | 1 (1.6) |
| Drugs | 1 (1.6) |
| Alcohol excess | 15 (24.2) |
Characteristics of hospitalization
The mean duration of hospital stay was 11.4 days (median 7 days, range 1–64 days, Q1 3 days, Q3 17 days). Admission to intensive care unit (ICU) for acute trauma care was necessary in 29.0% (n = 18), with a mean duration of ICU-stay of 1.7 days (median 0 days, range 0–24 days, Q1 0 days, Q3 2 days). More details on injury management and the length of stay are provided in Table 2. In-hospital-mortality within the study population was 1.6%, with only one patient deceased during the in-hospital observation period due to a seizure related fall with traumatic basal skull fracture and subdural hematoma (n = 1).
Table 2.
Injury management and hospitalization of 62 cases of epilepsy.
| Variables | n (%) |
|---|---|
| Injury management | |
| Operative | 28 (45.2) |
| Conservative | 34 (54.8) |
| Discharge | |
| Discharge to other hospital | 7 (11.3) |
| Rehabilitation | 9 (14.5) |
| Short-term care facility | 5 (8.1) |
| Home | 40 (64.5) |
Note: one patient deceased at hospital.
Characteristics of injuries and fractures
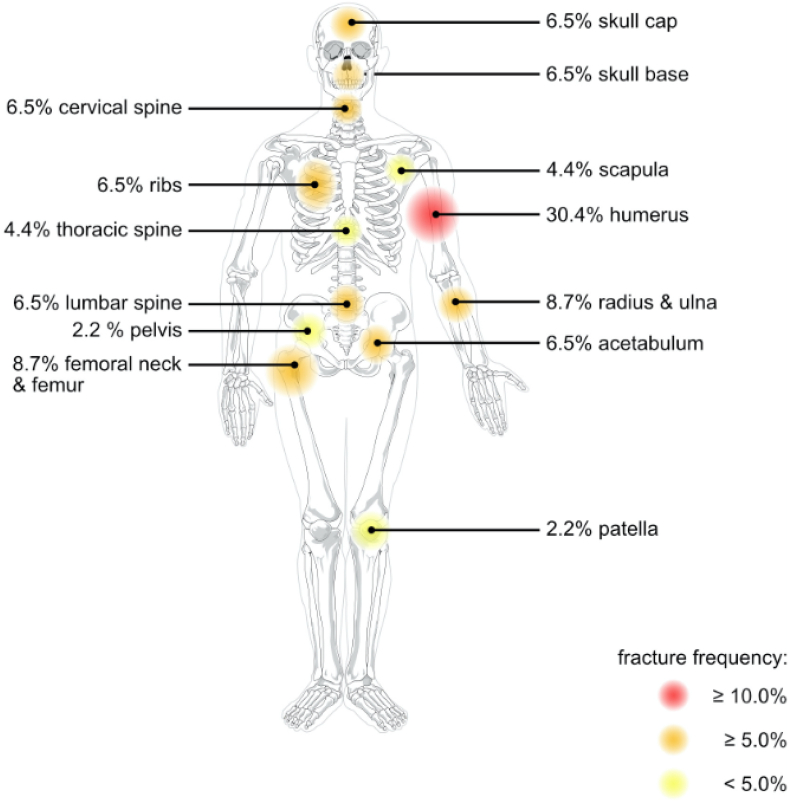
A total number of 94 injuries was reported within the study population which can be subdivided into fractures (48.9%, n = 46), craniocerebral trauma (26.6%, n = 25) and soft tissue injuries (24.5%, n = 23). Among soft tissue injuries, most frequent symptoms were laceration with 11.7% (n = 11), followed by luxations (6.4%, n = 6), sprains (4.3%, n = 4), cuts and compartment syndromes (each 1.1%, n = 1 for each). Regarding craniocerebral trauma, commotio cerebri was reported in 68.0% cases (17/25), followed by contusio cerebri (20.0%, n = 5) and compressio cerebri (8.0%, n = 2). In one patient (4.0%), subdural hemorrhage was diagnosed as seizure-related injury caused by a car accident. Detailed information on the specific fracture patterns is given in Table 3. Fracture localization is shown in Fig. 1.
Table 3.
Characteristics of fractures and craniocerebral trauma.
| Fractures | n (%) |
|---|---|
| Lower extremitiesa | 5 (10.9) |
| Femoral neck & femurb | 4 (80.0) |
| Patellab | 1 (20.0) |
| Upper extremitiesa | 20 (43.5) |
| Scapulaec | 2 (10.0) |
| Humerusc | 14 (70.0) |
| Radius & ulnac | 4 (20.0) |
| Trunka | 15 (32.6) |
| Spined | 8 (53.4) |
| Lumbare | 3 (37.5) |
| Thoracice | 2 (25.0) |
| Cervicale | 3 (37.5) |
| Ribsd | 3 (20.0) |
| Pelvisdd | 1 (6.6) |
| Acetabulumd | 3 (20.0) |
| Heada | 6 (13.0) |
| Skull capf | 3 (50.0) |
| Skull basef | 3 (50.0) |
Calculated per a fractures (n = 46), b lower extremities (n = 5),c upper extremities (n = 20); d trunk (n = 15),); e spine (n = 8); f head (n = 6).
Fig. 1.
Frequent seizure-related fracture pattern: percentage distribution of seizure-related fractures in the present cohort (n=46) with color-coded display of frequency categories (red ≥ 10.0%, orange ≥ 5.0%, yellow < 5.0%). The underlying scheme of a human male skeleton was published by the artist Mariana Ruiz Villarreal under an unrestricted public license and released into the public domain by its author.
Discussion
Seizure-related injuries have been shown to be a frequent and highly underreported consequence of patients with epilepsy as well as for people suffering from epileptic seizures due to other acute medical conditions, such as alcohol or drug withdrawal or electrolyte derailment.10,12,23,24 Mild craniocerebral traumata as well as minor or soft tissue trauma, e.g. sprains, abrasion, cuts, are by far the most frequent reported injuries related to epileptic seizures. Additionally, due to loss of consciousness and inadequate peri- or postictal behavior, rare but not less dangerous injuries, such as thermal or chemical burns as well as seizure-related fractures, represent a common complication of epileptic seizure and need urgent and skilled medical care.8,13
The finding that fractures were by far the most frequent injuries after seizures in the present cohort is probably due to the pre-selection of the included patients based on the conduction of the study at a level 1 trauma center. Compared to studies on other neurological diseases with frequent and unrestrained falls, such as Parkinson's disease, a different fracture pattern can be observed. This can most likely be attributed to specific pathomechanims and sociodemographic aspects of the underlying disease. While patients with Parkinson's disease are mostly elderly, more fragile and suffer from tripping falls leading to frequent fractures of the trunk or the proximal lower extremities, e.g. lumbar spine, pelvis and proximal femur25, patients with epilepsy are often younger, frequently have no other comorbidities and mostly show unrestricted falls due to a loss of consciousness and/or muscular toning of the body leading to fractures of the trunk and upper extremities.24 Moreover, during the tonic phase of generalized tonic-clonic seizures, fractures of the spine have also been reported in patients lysing flat in a secure environment, e.g. an inpatient video-EEG-monitoring. Due to a similar type of fall mechanism, fracture patterns associated with seizures or a syncope seem to be comparable.26,27
In our cohort, most injuries could be managed conservatively, however, a relevant fraction of the patients had to undergo surgery for advanced wound management or acute fracture care. Following national and international guidelines for acute dislocated or complex fractures, which should undergo timely surgery to avoid secondary tissue or joint damage, patients have to be transferred to specialized trauma centers in many cases. With a mean duration of stay of 11 days and a relevant proportion of patients being admitted to ICU with a mean duration of ICU stay of 2 days, seizure related injuries result in high treatment costs. Recently, a German study group calculated the direct costs of acute care due to seizure related injuries to approximately €9,300 ($11,000, £8,400),28 underlining the proclaimed health economic burden of secondary fractures. In the present cohort, 36% of the patients could not be discharged directly to their homes and had to be transferred to other hospitals, rehabilitation facilities or short-term care facilities. This demonstrates an additional relevant cost factor in the context of inpatient and outpatient follow-up treatment in seizure patients as in other patients already shown.28, 29, 30, 31, 32
Besides acute care, primary and secondary prophylaxis is important aspects to minimize the probability of seizure related injuries in general. In patients with known active epilepsy, seizure control represents the most important aspect, which may comprise treatment with ASD as well as an early evaluation of invasive therapeutic options, such as epilepsy surgery or neurostimulation. Moreover, general risk factors for bone weakness should be addressed, especially in postmenopausal women, elderly patients or patients taking enzyme inducing ASD increasing the risk for osteomalazia or osteoporosis.10,33 In the present cohort, dual energy X-ray absorptiometry scans of patients with fractures revealed a reduced T-score and Z-score, which suggest a potential benefit of an early prophylactic supplementation with calcium and vitamin D in high risk patients. In addition, factors triggering seizures, such as drugs, alcohol withdrawal, sleep deprivation or medicamentous non-compliance should be avoided in general and especially by patients with known epilepsy or seizures in the past. Here, especially epilepsy counselling sites or specialized epileptological outpatient clinics could help to raise awareness and improve primary and secondary prophylaxis.34
As all retrospective single-center studies, the present study suffers from several limitations due to its design that may have an influence on its results, transferability and comparability to other studies. Especially the conduction of the study at a level 1 trauma center could have led to an overrepresentation of severe or combined fractures. Additionally, the presented study lacks a control group for comparison, which is necessary to further confirm the conclusions obtained from this study. Moreover, the retrospective acquisition using the hospital information system could lead to missed cases due to false coding. To minimize these possible biases, STROBE and RECORD20,21 guidelines were closely followed and a double entry procedure with random cross-checks was performed.
In conclusion, fractures of the upper extremities and trunk as well as craniocerebral trauma occur frequently as seizure induced injuries. Alcohol excess and withdrawal are important provoking factors and should be targeted with preventive measurements like education, weaning therapy and support groups. The data from our cohort revealed a reduced T-score and Z-score, which suggest a potential benefit of an early prophylactic supplementation with calcium and vitamin D in high risk patients. Factors triggering seizures, such as drugs, alcohol withdrawal, sleep deprivation or medicamentous non-compliance should be avoided in general and especially by patients with known epilepsy. Further multi-center studies are needed to investigate the dependence of fractures, drug therapy for epilepsy and bone density in more detail.
Funding
Nil.
Ethical statement
Approval of the local ethics committee was attained (Frankfurt am Main, approval 52/18) and relative guidelines were followed.
Declaration of competing interest
The authors declared no competing interest.
Acknowledgments
We are grateful for the continuous support and comments of our valued collogues at the Department of Trauma, Hand and Reconstructive Surgery as well as the Department of Neurology at the University Hospital Frankfurt am Main.
Author contributions
René D. Verboket and Laurent M. Willems developed the idea for this project and performed the statistical analysis. Nils Mühlenfeld performed the data collection. Nils Mühlenfeld, René D. Verboket, Laurent M. Willems, Philipp Störmann, Ingo Marzi, Felix Rosenow and Adam Strzelczyk wrote the paper. Each author contributed important content-related aspects.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.World Health Organization Epilepsy. https://www.who.int/news-room/fact-sheets/detail/epilepsy
- 2.Murray C.J., Lopez A.D., Jamison D.T. The global burden of disease in 1990: summary results, sensitivity analysis and future directions. Bull World Health Organ. 1994;72:495–509. [PMC free article] [PubMed] [Google Scholar]
- 3.Camfield C., Camfield P. Injuries from seizures are a serious, persistent problem in childhood onset epilepsy: a population-based study. Seizure. 2015;27:80–83. doi: 10.1016/j.seizure.2015.02.031. [DOI] [PubMed] [Google Scholar]
- 4.Lagunju I.A., Oyinlade A.O., Babatunde O.D. Seizure-related injuries in children and adolescents with epilepsy. Epilepsy Behav. 2016;54:131–134. doi: 10.1016/j.yebeh.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 5.Burneo J.G., Antaya T.C., Allen B.N., et al. The risk of new-onset epilepsy and refractory epilepsy in older adult stroke survivors. Neurology. 2019;93:e568–e577. doi: 10.1212/WNL.0000000000007895. [DOI] [PubMed] [Google Scholar]
- 6.Mahr K., Bergmann M.P., Kay L., et al. Prone, lateral, or supine positioning at seizure onset determines the postictal body position: a multicenter video-EEG monitoring cohort study. Seizure. 2020;76:173–178. doi: 10.1016/j.seizure.2020.02.008. [DOI] [PubMed] [Google Scholar]
- 7.Frey K., Zöllner J.P., Knake S., et al. Risk incidence of fractures and injuries: a multicenter video-EEG study of 626 generalized convulsive seizures. J Neurol. 2020;267:3632–3642. doi: 10.1007/s00415-020-10065-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willems L.M., Watermann N., Richter S., et al. Incidence, risk factors and consequences of epilepsy-related injuries and accidents: a retrospective, single center study. Front Neurol. 2018;9:414. doi: 10.3389/fneur.2018.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riechmann J., Willems L.M., Boor R., et al. Quality of life and correlating factors in children, adolescents with epilepsy, and their caregivers: a cross-sectional multicenter study from Germany. Seizure. 2019;69:92–98. doi: 10.1016/j.seizure.2019.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Verboket R.D., Söhling N., Marzi I., et al. Prevalence, risk factors and therapeutic aspects of injuries and accidents in women with epilepsy. Eur J Trauma Emerg Surg. 2019;45:375–381. doi: 10.1007/s00068-018-1030-8. [DOI] [PubMed] [Google Scholar]
- 11.Willems L.M., Reif P.S., Knake S., et al. Noncompliance of patients with driving restrictions due to uncontrolled epilepsy. Epilepsy Behav. 2019;91:86–89. doi: 10.1016/j.yebeh.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Mattson R.H., Gidal B.E. Fractures, epilepsy, and antiepileptic drugs. Epilepsy Behav. 2004;5(Suppl 2):S36–S40. doi: 10.1016/j.yebeh.2003.11.030. [DOI] [PubMed] [Google Scholar]
- 13.Kwon C.S., Liu M., Quan H., et al. The incidence of injuries in persons with and without epilepsy--a population-based study. Epilepsia. 2010;51:2247–2253. doi: 10.1111/j.1528-1167.2010.02697.x. [DOI] [PubMed] [Google Scholar]
- 14.Téllez-Zenteno J.F., Nguyen R., Hernádez-Ronquillo L. Injuries, accidents and mortality in epilepsy: a review of its prevalence risk factors and prevention. Rev Invest Clin. 2010;62:466–479. [PubMed] [Google Scholar]
- 15.Nguyen R., Téllez Zenteno J.F. Injuries in epilepsy: a review of its prevalence, risk factors, type of injuries and prevention. Neurol Int. 2009;1 doi: 10.4081/ni.2009.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Strzelczyk A., Nickolay T., Bauer S., et al. Evaluation of health-care utilization among adult patients with epilepsy in Germany. Epilepsy Behav. 2012;23:451–457. doi: 10.1016/j.yebeh.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 17.Willems L.M., Richter S., Watermann N., et al. Trends in resource utilization and prescription of anticonvulsants for patients with active epilepsy in Germany from 2003 to 2013 - a ten-year overview. Epilepsy Behav. 2018;83:28–35. doi: 10.1016/j.yebeh.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 18.Persson H.B., Alberts K.A., By Farahmand, et al. Risk of extremity fractures in adult outpatients with epilepsy. Epilepsia. 2002;43:768–772. doi: 10.1046/j.1528-1157.2002.15801.x. [DOI] [PubMed] [Google Scholar]
- 19.Souverein P.C., Webb D.J., Weil J.G., et al. Use of antiepileptic drugs and risk of fractures: case-control study among patients with epilepsy. Neurology. 2006;66:1318–1324. doi: 10.1212/01.wnl.0000210503.89488.88. [DOI] [PubMed] [Google Scholar]
- 20.von Elm E., Altman D.G., Egger M., et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–1499. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Harron K., Benchimol E., Langan S. Using the RECORD guidelines to improve transparent reporting of studies based on routinely collected data. Int J Popul Data Sci. 2018;3:2. doi: 10.23889/ijpds.v3i1.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strzelczyk A., Griebel C., Lux W., et al. The burden of severely drug-refractory epilepsy: a comparative longitudinal evaluation of mortality, morbidity, resource use, and cost using German health insurance data. Front Neurol. 2017;8:712. doi: 10.3389/fneur.2017.00712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Desai K.B., Ribbans W.J., Taylor G.J. Incidence of five common fracture types in an institutional epileptic population. Injury. 1996;27:97–100. doi: 10.1016/0020-1383(95)00189-1. [DOI] [PubMed] [Google Scholar]
- 25.Mühlenfeld N., Söhling N., Marzi I., et al. Fractures in Parkinson's Disease: injury patterns, hospitalization, and therapeutic aspects. Eur J Trauma Emerg Surg. 2021;47:573–580. doi: 10.1007/s00068-019-01240-z. [DOI] [PubMed] [Google Scholar]
- 26.Porter K.J., Dartnell J., Richards A.M., et al. Delayed diagnosis of bilateral scapula fractures in a patient with cardiac syncope. Shoulder Elb. 2012;4:185–187. doi: 10.1111/j.1758-5740.2012.00188.x. [DOI] [Google Scholar]
- 27.Hino S., Yamada M., Araki R., et al. Effects of loss of consciousness on maxillofacial fractures in simple falls. Dent Traumatol. 2019;35:48–53. doi: 10.1111/edt.12452. [DOI] [PubMed] [Google Scholar]
- 28.Verboket R.D., Mühlenfeld N., Woschek M., et al. Inpatient treatment costs, cost-driving factors and potential reimbursement problems due to fall-related fractures in patients with Parkinson's disease. Chirurg. 2020;91:421–427. doi: 10.1007/s00104-019-01074-w. [DOI] [PubMed] [Google Scholar]
- 29.Woschek M., Schindler C.R., Sterz J., et al. Admission diagnosis contusion: etiology, epidemiology and cost-causing factors. Z Gerontol Geriatr. 2020 Dec 18 doi: 10.1007/s00391-020-01828-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mühlenfeld N., Schindler C.R., Sterz J., et al. Cost-proceeds deficit of outpatient treatment of head lacerations in the emergency department. Chirurg. 2021;92:274–280. doi: 10.1007/s00104-020-01276-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verboket R., Verboket C., Schöffski O., et al. Costs and proceeds from patients admitted via the emergency room with mild craniocerebral trauma. Unfallchirurg. 2019;122:618–625. doi: 10.1007/s00113-018-0566-8. [DOI] [PubMed] [Google Scholar]
- 32.Verboket R.D., Mühlenfeld N., Sterz J., et al. Inpatient treatment costs, cost-driving factors and potential reimbursement problems due to epileptic seizure-related injuries and fractures. Chirurg. 2021;92:361–368. doi: 10.1007/s00104-020-01257-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bauer S., Hofbauer L.C., Rauner M., et al. Early detection of bone metabolism changes under different antiepileptic drugs (ED-BoM-AED)--a prospective multicenter study. Epilepsy Res. 2013;106:417–422. doi: 10.1016/j.eplepsyres.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 34.Willems L.M., Kondziela J.M., Knake S., et al. Counseling and social work for people with epilepsy in Germany: a cross-sectional multicenter study on demand, frequent content, patient satisfaction, and burden-of-disease. Epilepsy Behav. 2019;92:114–120. doi: 10.1007/s00115-019-0676-8. [DOI] [PubMed] [Google Scholar]