Abstract
The deep fascia is intimately linked to skeletal muscle and may be involved in delayed onset muscle soreness (DOMS). The present study therefore explored the effect of eccentric exercise on fascia stiffness and its relation with DOMS. Healthy active male adults (n = 19, 27 ± 4 years) performed 6 x 10 maximal eccentric knee flexions using an isokinetic dynamometer. Before (baseline) as well as immediately (T0), 1 hour (T1), and each day up to 72 hours (T24 to T72) afterwards, shear wave elastography was used to measure the mechanical stiffness of the biceps femoris muscle and the overlying fascia. As a surrogate of DOMS, pain upon palpation was captured by means of a 100mm visual analogue scale. While muscle stiffness remained unchanged (p > 0.05), deep fascia stiffness increased from baseline to T24 (median: 18 kPa to 21.12 kPa, p = 0.017) and T72 (median: 18 kPa to 21.3 kPa, p = 0.001) post-exercise. Linear regression showed an association of stiffness changes at T24 and pressure pain at T72 (r2 = 0.22, p < 0.05). Maximal eccentric exercise leads to a stiffening of the fascia, which, in turn, is related to the magnitude of future DOMS. Upcoming research should therefore gauge the effectiveness of interventions modifying the mechanical properties of the connective tissue in order to accelerate recovery.
Key points.
Eccentric exercise increases the stiffness of the deep fascia
Stiffness increases correlate with DOMS palpation pain on subsequent days.
Interventions to prevent or treat DOMS may need to focus on the fascial connective tissue
Key words: DOMS, ultrasound, fatigue, connective tissue, exercise
Introduction
Eccentric contraction is one of the most frequent types of muscle action in both, activities of daily living and sports (Hody et al., 2019). When used as training method, it has been demonstrated to represent a potent stimulus triggering numerous morphological and functional adaptations in the soft tissue (Hedayatpour and Falla, 2015). However, while most of the available research on acute eccentric exercise effects has focussed on the skeletal muscle (particularly with regard to the pathogenesis of delayed onset muscle soreness/DOMS), less is known regarding the deep fascia (Wilke and Behringer, 2021). Contrary to earlier assumptions, the multi-layered, collagen-rich structure is not merely a passive envelope of the skeletal muscle. Fascia has a high proprioceptive capacity (Blottner et al., 2019), exhibits autonomous mechanisms of stiffness regulation such as cellular contraction or strain hardening (Schleip et al., 2019), and fuses tightly with the underlying muscle (Benjamin, 2009). Furthermore, owing to its direct linkages to neighbouring muscles, tendons, and ligaments, it has been suggested that fascia assists in the absorption and distribution of mechanical forces during heavy loading (Wilke et al., 2018). As a consequence, tissue lengthening, i.e., eccentric muscle action, could represent the main mechanism inducing tissue adaptation and/or injury of the deep fascia.
A systematic review with meta-analysis investigating the involvement of the connective tissue in muscle injury revealed fascial lesions in about one third of all injuries (Wilke et al., 2019). As muscle injuries, in many cases, occur during eccentric contraction, the frequent finding of connective tissue failure seems to support the above hypothesis that fascia may be damaged during excessive muscle lengthening. Moreover, in a randomized, controlled experiment, Tenberg et al. (2022) found increases of fascia thickness following a heavy-load eccentric exercise protocol and it has been assumed that this observation could reflect edema produced by fascial micro-injury (Wilke and Behringer, 2021, Tenberg et al., 2022). Yet, despite the initial evidence suggesting a possible mechanical impact of eccentric muscle action on the deep fascia, the viscoelastic properties of the deep fascia following eccentric contraction have not been examined. Stiffness, a tissue’s resistance to deformation, is of particular interest because it is increased in the presence of pain and after tissue injury (Zhou et al., 2020, Wilke and Behringer, 2021). The present study therefore aimed to investigate the effect of a maximal knee flexor eccentric exercise protocol on fascial stiffness.
Methods
Ethics and sample
This article is an explorative sub-analysis of data from the ELASTIC (Eccentric loading and soft tissue mechanics) project which examined the effects of maximal eccentric exercise during different states of fatigue (Register of Clinical Trials: DRKS00025243) using a repeated-measures, within-subject design. Approval was obtained from the local ethics committee and each participant provided written informed consent for study participation. Complete datasets were available for a total of N = 19 healthy active males (Table 1), either being fully rested (N = 5), acutely fatigued (1x 50 concentric leg curls, N = 6), or chronically fatigued (4 sessions of 1x 50 concentric leg curls within two weeks, N = 8). The enrolled individuals, who regularly performed resistance exercise (Table 1), had to be healthy, active (minimum of two sports sessions per week), and between 18 and 35 years of age. All were affiliated with the university’s exercise science program. Recruitment was performed by means of promotion during curricular teaching and poster advertising. Exclusion criteria encompassed severe cardiovascular, metabolic, endocrine, neural, and psychiatric diseases, unhealed orthopaedic injuries and overuse disorders of the lower limb, local inflammation, intake of painkillers and other substances modifying perception, and contact allergies (particularly against ultrasound gel).
Table 1.
Characteristics of the sample.
| Mean ± SD | |
|---|---|
| Age [years] | 27 ± 4 |
| Height [m] | 1.82 ± 0.07 |
| Body Mass [kg] | 83 ± 9 |
| Body Mass Index [kg/m2] | 25 ± 3 |
| Body Fat [%] | 15 ± 5 |
| Fat-free mass [kg] | 21 ± 2 |
| Total sports activity [h/week] | 8 ± 4 |
| Resistance training [h/week] | 4 ± 3 |
SD = standard deviation, cm = centimetre, kg = kilogram, m = meter, h = hours. Fat-free mass assessed using a 3D bodyscanner (Scaneca, Scaneca GmbH, Berlin, Germany). Sports activity and hours spent performing resistance exercise were documented using simple open questions.
Eccentric exercise protocol
All participants underwent an eccentric knee flexor exercise protocol using an isokinetic dynamometer (ISOMED 2000, D. & R. Ferstl GmbH, Hemau, Germany). We decided to target the knee flexors vs. the knee extensors because this muscle group is more vulnerable to muscle soreness and damage (Franklin et al., 1993). After a brief warm-up (5 minutes ergometer cycling at 100 Watt), they performed 6 x 10 maximal eccentric leg curls (interest rest: 1 minute) in sitting position (Brusco et al., 2018). Trunk flexion was set to 85° and the movement amplitude was 90° knee flexion to 10° knee extension. To prevent unwanted secondary body movement, shoulder and pelvic straps were used. A one-minute rest interval was applied between sets. As high angular velocities have been demonstrated to better mimic exhaustion in sports (i.e. football) while still causing muscle damage (Chapman et al., 2006), we used a velocity of 210° per second. No rest interval was used in transitions from eccentric to concentric phases, thus ensuring a fluent movement. To isolate the effects of eccentric contraction, the dynamometer passively returned the leg of the participants back to knee flexion after each repetition (50°/s).
Outcomes
Soft tissue stiffness and pain upon palpation were measured before (PRE), immediately after (T0), 1 hour after (T1) as well as on the 3 successive days (T24-T72) after eccentric exercise. Times of assessment on consecutive days were kept constant to prevent influences of circadian rhythm. Participants were instructed to maintain their habitual activity and training habits during the entire study period.
Soft tissue stiffness
To evaluate soft tissue stiffness, we used shear-wave elastography (SWE), an ultrasound-based technique exhibiting high inter-rater (ICC: 0.89 to 0.95) and test-retest (ICC: 0.70 to 0.97) reliability in the assessment of musculoskeletal structures (Dubois et al., 2015, Taş et al., 2017, Rosskopf et al., 2016). Briefly, SWE produces an acoustic radiation force impulse whose resulting shear waves propagate perpendicularly through the tissue. Detection pulses are used to measure their speed of displacement. As softer tissues reduce and harder tissues increase the speed of shear wave propagation (Sigrist et al, 2017), velocity can serve as a proxy of tissue stiffness. Based on the raw data of a measurement, SWE generates a color-coded map overlying the normal ultrasound image with blue representing low stiffness, and red indicating high stiffness (Taljanovic et al., 2017, Figure 1).
Figure 1.
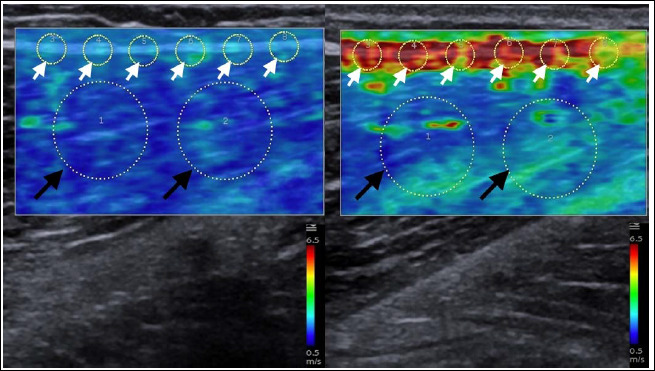
Ultrasound elastography of the dorsal thigh before (left) and 24 hours after (right) eccentric exercise. For stiffness measurements, a rectangular region of interest (ROI) was selected. Measurements were then performed in equidistant circular areas within the biceps femoris muscle (black arrows) and its overlying deep fascia (white arrows).
For the measurements, participants adopted a prone position with 5° knee flexion on a treatment table (Calderón Pellegrino et al., 2020). A trained investigator then identified the origin (ischial tuberosity) and insertion (fibular head) of the BF muscle using manual palpation and, if needed, ultrasound imaging. To ensure consistency between repeated measurements, the point of interest at 50% of the distance between the two bony landmarks was marked with a water-resistant pen. The 10L4 linear array probe (50mm width) of an ultrasound elastography device (ACUSON Redwood, Siemens Healthineers, Erlangen, Germany) was positioned longitudinally on the marked point of the dorsal thigh. Special care was given to match probe orientation and course of the BF muscle fibers (Akagi et al., 2017). Within the rectangular 5x10 mm region of interest (ROI) for SWE, two equidistant circular areas with a 10-mm diameter were defined for quantification of stiffness in the BF muscle (Figure 1). As similarly sized circles would be too large to include the deep fascia only, we used six equidistant 3-mm circles for the fascia. Three measurements, averaged for analysis, were taken for both, muscle and fascia stiffness.
Self-reported DOMS
To quantify DOMS, we used the method from Lau et al. (2015), which has been shown to exhibit good test-retest reliability. A trained investigator palpated the BF muscle (longitudinal orientation), applying a constant pressure of approximately 400 kPA with the tips of the index and middle fingers of one hand. The procedure was repeated three times and the average was used for analysis. The location of palpation (50% of the distance between origin and insertion of the muscle) was identical to that of the elastography measurements. The participants were asked to indicate pressure pain on a 100-mm visual analogue scale (VAS) with 0 representing no pain and 100 representing maximal pain. Palpation was always performed by the same investigator. To constantly achieve the same pressure in all measurements, the investigator received a thorough training before study initiation. Here, the applied pressure was quantified by means of a handheld dynamometer. Only when the examiner was able to consistently achieve the required pressure and less than 5% variation occurred between trials (Lau et al. 2015), the training was terminated.
Statistical analysis
The Kolmogorov-Smirnoff test with Dallal-Wilkinson correction was applied to check the normal distribution of data and variance homogeneity was examined using the Box test. Due to violation of the assumptions for parametric testing, we used Friedman tests for omnibus comparisons of mechanical stiffness between measurements (pre, T0, T1, T24, T48, T72) and Durbin-Conover tests for pairwise post hoc comparisons. The same procedure (Friedman and Durbin-Conover testing) was applied with regard to DOMS.
Associations between systematic changes in tissue stiffness and pain were examined by means of Spearman and Pearson correlations, as appropriate. In case of significance and if testing assumptions were met, linear regression was added. All analyses were performed using Jamovi 1.8 (The jamovi project, https://www.jamovi.org) and the significance level was set to α = 0.05.
Results
Stiffness
No significant changes over time were found for muscle stiffness (x2 = 6.32, p = 0.277, Table 2, Figure 2). Conversely, there was an increase in the deep fascia (x2 = 11.9, p = 0.036, Table 2, Figure 2). Pairwise post hoc comparisons showed that stiffness was systematically higher at 24h (18 kPa to 21.12 kPa, p = 0.017) and 72 h (18 kPa to 21.3 kPa, p = 0.001) after exercise (Figure 3). No differences of deep fascia or muscle stiffness were observed between the rested and acutely or chronically fatigued participants (p > 0.05).
Table 2.
Stiffness (kPa) of the biceps femoris muscle (top) and deep fascia (bottom).
| Muscle (Pre) | Muscle (T0) | Muscle (T1) | Muscle (T24) | Muscle (T48) | Muscle (T72) | |
|---|---|---|---|---|---|---|
| Median | 8.3 | 8.5 | 7.9 | 8.9 | 8.5 | 9.7 |
| Mean | 9.0 | 8.7 | 9.0 | 9.5 | 8.9 | 10.4 |
| 25th percentile | 7.4 | 7.8 | 7.3 | 7.6 | 8.0 | 7.7 |
| 75th percentile | 9.6 | 9.4 | 9.3 | 9.8 | 9.1 | 10.8 |
| Fascia (Pre) | Fascia (T0) | Fascia (T1) | Fascia (T24) | Fascia (T48) | Fascia (T72) | |
| Median | 18.0 | 18.2 | 19.6 | 21.2* | 17.8 | 21.3** |
| Mean | 17.9 | 20.3 | 21.3 | 21.3 | 24.8 | 24.1 |
| 25th percentile | 13.3 | 16.7 | 15.4 | 16.3 | 14.8 | 15.6 |
| 75th percentile | 21.9 | 22.7 | 25.8 | 24.9 | 29.1 | 29.7 |
Asterisks mark statistical significance vs. baseline (pre) data.
* = p <. 005
** = p < 0.01.
Figure 2.
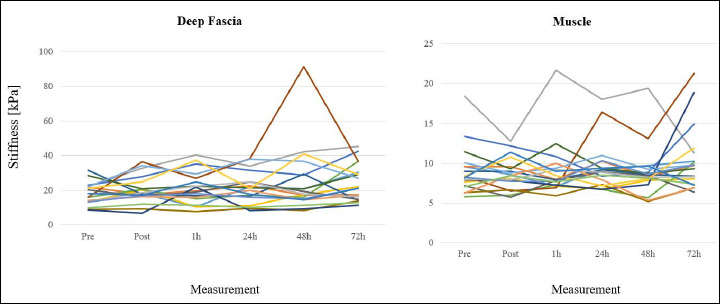
Individual changes [WJC1]of fascia (left) and muscle (right) stiffness in response to the eccentric loading protocol. kPa = kilopascal.
Figure 3.
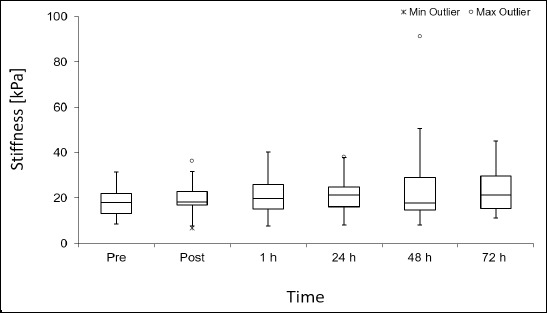
Stiffness of the biceps femoris fascia before and after maximal eccentric loading. Figure shows box plots with medians and maximal (open circles)/ minimal (asterisks) outliers. kPa = kilopascal.
DOMS
As expected, soft tissue pressure pain increased following eccentric exercise (x2 = 50.2, p < 0.001, Figure 4), showing higher values at all time points (p < 0.01) with a peak at 48 h (19 vs 1 mm). Correlation analyses demonstrated moderate associations between changes in fascial stiffness and pain reported on the days following exercise (p < 0.05).
Figure 4.
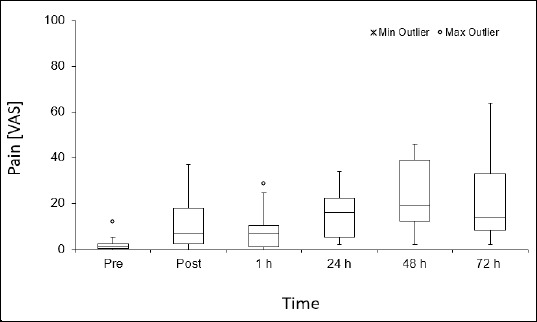
Palpation pain (visual analogue scale, VAS) before and after maximal eccentric loading. Figure shows box plots with medians and maximal (open circles)/ minimal (asterisks) outliers.
In detail, correlations were found between Δ stiffness at 1h and VAS72 (rho = 0.40, p = 0.046), Δ stiffness at 24h and VAS48 (rho = 0.50, p = 0.015), as well as Δ stiffness at 24h and VAS72 (r = 0.47, p = 0.04). Linear regression showed that Δ stiffness at 24h predicted VAS72 with a variance explanation of 22% (b = 1.07, r2 = 0.22, p = 0.045).
Discussion
The deep fascia surrounding the skeletal muscle has repeatedly been claimed to adapt to mechanical stimuli (Schleip and Müller, 2013; Zügel et al. 2018); however, so far, there has been a lack of physiological investigations following exercise. To the best of our knowledge, the present study is the first to examine the material properties of the deep fascia in response to maximal eccentric loading. We demonstrate that loaded muscle elongation causes a fascial stiffening of about 18% while no such observation could be made in the skeletal muscle. The deep fascia is densely populated with proprioceptors and pain receptors and therefore, this magnitude may have an impact on perception and mechanics.
Interestingly, a previous study of Tenberg et al. (2022), using a similar training protocol, found an increase in elbow flexor fascia thickness post-eccentric exercise and suggested that fascial micro-injury and edema could represent the underlying causes. Because edema is associated with increased stiffness (Mridha and Ödman, 1985; Vexler et al., 1999), our findings provide some support for their hypothesis. As an alternative to the micro-injury theory, it could also be argued that exercise increases the production of hyaluronic acid (HA, Piehl-Aulin et al., 1985). A higher volume of HA is associated with higher viscosity, which, in turn, results in higher stiffness (Pavan et al., 2014). However, as HA, due to its thixotropic behaviour, reduces its viscosity (meaning lower stiffness) upon mechanical stimulation, the general stiffness increase due to HA production may be counteracted by the stiffness reduction caused by thixotropy. For this reason, at present, we consider the occurrence of micro-injury and subsequent swelling a more probable explanation for the observed stiffness increases following eccentric exercise.
As expected, palpation pain increased following the eccentric exercise protocol, reaching highest values on the following days. This phenomenon, also referred to as delayed onset muscle soreness (DOMS), has traditionally been ascribed to a variety of processes associated with the skeletal muscle such as excessive lactate production (Gleeson et al., 1998), structural sarcomere damage at the z-disk (Fridén et al., 1981), accumulation of free radicals (Close et al. 2004) However, their association with self-reported pain and their causal value within the pathogenesis of DOMS are questionable (Wilke and Behringer, 2021). In our analysis, we found that increases in fascia stiffness at 1 and 24 hours post-exercise were associated with the intensity of palpation pain on the following days. This (1) again fits with the data of Tenberg et al. (2022) who also showed an association of exercise-induced fascial thickness increases and self-reported pain and (2) strengthens the evidence for the relevance of changes in fascia morphology and mechanics in DOMS.
As mentioned, we did not observe a change in muscle stiffness after eccentric exercise leading to DOMS. This is surprising because some previous studies reported increases after similar experiments (Green et al., 2011; Agten et al. 2017; Yanagisawa et al., 2015; Konrad et al., 2022). Possibly, this discrepancy is due to the fact that these trials either examined different muscles (i.e., of the calf; Green et al., 2011; Agten et al. 2017; Yanagisawa et al., 2015) or used different measurement methods (e.g., Konrad et al. 2022). Additionally, it may be that the exercise protocol was not sufficiently fatiguing to create muscle damage. In any case, besides further elucidating changes in fascial properties after eccentric loading, the response of skeletal muscle tissue also merits additional investigation.
Exercise professionals and coaches may benefit from our results in two ways. Firstly, screening athletes by means of ultrasound elastography could become a useful prognostic tool in order to predict DOMS magnitude and to accordingly select recovery strategies. Secondly, related to this, a focus could be laid more on treatments targeting the connective tissue rather than the muscle when aiming to prevent or reduce tissue soreness. For instance, foam rolling has been demonstrated to prevent fascial inflammation (Pablos et al., 2020) and to improve intrafascial mobility (Krause et al., 2019) which may explain its effectiveness in reducing DOMS (Cheatham et al. 2015).
The findings made in the present study should be interpreted in the light of some shortcomings. Most importantly, we examined fascial stiffness as an additive outcome in a sub-sample of a larger experiment and our participants hence represented a group of acutely fatigued, chronically fatigued, or non-fatigued participants. Although the general tissue response of fascial stiffening following eccentric exercise occurred in all sub-groups and individuals, the magnitude could have been subject to variation. As the sample size was insufficient to test this hypothesis convincingly, future research should aim to investigate fascial stiffness changes at different fatigue states. In general, our data showed some variation. Possibly, this was partly due to the abovementioned issue of different pre-fatigue states and may also explain why no significant stiffness change of the deep fascia was detected at 48 hours post-exercise. Yet, an alternative reason for the variability could be that the connective tissue, from an inter-individual perspective, may react very differently to mechanical loading as a function of its state (e.g. differences in fibre composition or hyaluronan concentration, Pavan et al., 2014; Zügel et al., 2018). A third aspect relates to the intensity of DOMS. Our participants reported substantial increases of palpation pain. However, considering that the magnitude of such change was higher in other studies,19 the fascial stiffening response and its predictive value may even have been underestimated by our data. Upcoming trials should hence aim to evoke a stronger DOMS response. Furthermore, as fascial stiffness peaked at 72 hours post-exercise, it would be of interest to implement additional follow-up assessments (e.g., at 96, and 120 hours post-exercise). Fourth, we applied a validated palpation method to examine DOMS in the knee extensors. Whilst our piloting works suggested a high reliability between measurements, it needs to be acknowledged that the original study of Lau et al. (2015) was performed in the elbow flexors and hence, the results need to be considered with some caution. Finally, we did not perform an a priori sample size calculation for this research question. However, although our findings should thus be considered exploratory, our study was sufficiently powered to make significant observations in both outcomes (change in stiffness, correlation of stiffness changes and pain).
Conclusion
Maximal eccentric loading of the knee flexors leads to a stiffness increase of the deep fascia, which correlates with the magnitude of delayed-onset muscle soreness (DOMS). These observations (1) demonstrate that the extramuscular connective tissue is highly adaptable to mechanical loading and (2) strengthen the hypothesis that fascia plays a role in the origin of DOMS. Exercise professionals and conditioning coaches may therefore consider the application of interventions targeting fascia when aiming to improve recovery following training sessions incorporating high quantities of eccentric muscle action.
Acknowledgements
The authors received no financial support for the research, authorship, and/or publication of this article. The experiments complied with the current laws of the country in which they were performed. The datasets generated and analyzed during the current study are not publicly available, but are available from the corresponding author who was an organizer of the study. The authors have no conflicts of interest to declare.
Biographies
Jan WILKE
Employment
University of Klagenfurt, Department of Movement Sciences, Klagenfurt am Wörthersee, Austria
Degree
PhD
Research interests
Exercise & Training
E-mail: wilke@sport.uni-frankfurt.de
Carsten SCHWIETE
Employment
Goethe University Frankfurt, Institute of Sports Sciences, Department of Sports Medicine and Exercise Physiology, Frankfurt/Main, Germany
Degree
M.A.
Research interests
Muscle Physiology
E-mail:
Michael BEHRINGER
Employment
Goethe University Frankfurt, Institute of Sports Sciences, Department of Sports Medicine and Exercise Physiology, Frankfurt/Main, Germany
Degree
MD, PhD
Research interests
Muscle Physiology
E-mail: behringer@sport.uni-frankfurt.de
References
- Agten C.A., Buck F.M., Dyer L., Flück M. (2017) Delayed-onset muscle soreness: temporal assessment with quantitative MRI and shear-wave ultrasound elastography. American Journal of Radiology 2, 402-412. https://doi.org/10.2214/AJR.16.16617 10.2214/AJR.16.16617 [DOI] [PubMed] [Google Scholar]
- Akagi R., Fukui T., Kubota M., Nakamura M., Ema R. (2017) Muscle shear moduli changes and frequency of alternate muscle activity of plantar flexor synergists induced by prolonged low-level contraction. Frontiers in Physiology 8, 708. https://doi.org/10.3389/fphys.2017.00708 10.3389/fphys.2017.00708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjamin M. (2009) The fascia of the limbs and back - a review. Journal of Anatomy 214, 1-18. https://doi.org/10.1111/j.1469-7580.2008.01011.x 10.1111/j.1469-7580.2008.01011.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blottner D., Huang Y., Trautmann G., Sun L. (2019) The fascia: continuum linking bone and myofascial bag for global and local body movement control on Earth and in Space. A scoping review. Reach 14, 100030. https://doi.org/10.1016/j.reach.2019.100030 10.1016/j.reach.2019.100030 [DOI] [Google Scholar]
- Brusco C.M., Blazevich A.J., Radaelli R., Botton C.E., Cadore E.L., Baroni B.M., Trajano G.S., Pinto R.S. (2018) The effects of flexibility training on exercise-induced muscle damage in young men with limited hamstrings flexibility. Scandinavian Journal of Medicine and Science in Sports 28, 1671-1680. https://doi.org/10.1111/sms.13068 10.1111/sms.13068 [DOI] [PubMed] [Google Scholar]
- Calderón Pellegrino G., Paredes-Hernández V., Sánchez-Sánchez J., García-Unanue J., Gallardo L. (2020) Effect of the fatigue on the physical performance in different small-sided games in elite football players. Journal of Strength and Conditioning Research 34, 2338-2346. https://doi.org/10.1519/JSC.0000000000002858 10.1519/JSC.0000000000002858 [DOI] [PubMed] [Google Scholar]
- Chapman D., Newton M., Sacco P., Nosaka K. (2006) Greater muscle damage induced by fast versus slow velocity eccentric exercise. International Journal of Sports Medicine 27, 591-598. https://doi.org/10.1055/s-2005-865920 10.1055/s-2005-865920 [DOI] [PubMed] [Google Scholar]
- Cheatham S.W., Kolber M.J., Cain M., Lee M. (2015) The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. International Journal of Sports Physical Therapy 10, 827-838. [PMC free article] [PubMed] [Google Scholar]
- Close G.L., Ashton T., Cable T., Doran D., MacLaren D.P.M. (2004) Eccentric exercise, isokinetic muscle torque and delayed onset muscle soreness: the role of reactive oxygen species. Euopean Journal of Applied Physiology 91, 615-621. https://doi.org/10.1007/s00421-003-1012-2 10.1007/s00421-003-1012-2 [DOI] [PubMed] [Google Scholar]
- Dubois G., Kheireddine W., Vergari C., Bonneau D., Thoreux P., Rouch P., Tanter M., Gennisson J.L., Skalli W. (2015) Reliable protocol for shear wave elastography of lower limb muscles at rest and during passive stretching. Ultrasound in Medicine and Biology 41, 2284-2291. https://doi.org/10.1016/j.ultrasmedbio.2015.04.020 10.1016/j.ultrasmedbio.2015.04.020 [DOI] [PubMed] [Google Scholar]
- Franklin M.E., Chamness M.S., Chenier T.C., Mosteller G.C., Barrow L.A. (1993) A comparison of isokinetic eccentric exercise on delayed-onset muscle soreness and creatine kinase in the quadriceps versus the hamstrings. Isokinetics and Exercise Science 3, 68-73. https://doi.org/10.3233/IES-1993-3201 10.3233/IES-1993-3201 [DOI] [Google Scholar]
- Fridén J., Sjöström M., Ekblom B. (1981) A morphological study of delayed muscle soreness. Experientia 37, 506-507. https://doi.org/10.1007/BF01986165 10.1007/BF01986165 [DOI] [PubMed] [Google Scholar]
- Gleeson M., Blannin A.K., Walsh N.P., Field C.N.E., Pritchard J.C. (1998) Effect of exercise-induced muscle damage on the blood lactate response to incremental exercise in humans. European Journal of Applied Physiology 77, 292-295. https://doi.org/10.1007/s004210050336 10.1007/s004210050336 [DOI] [PubMed] [Google Scholar]
- Green M.A., Sinkus R., Gandevia S.C., Herbert R.D., Bilston L.E. (2011) Measuring changes in muscle stiffness aftereccentric exercise using elastography. NMR in Biomedicine 25, 852-858. https://doi.org/10.1002/nbm.1801 10.1002/nbm.1801 [DOI] [PubMed] [Google Scholar]
- Hedayatpour N., Falla D. (2015) Physiological and neural adaptations to eccentric exercise: mechanisms and considerations for training. BioMed Research International, (serial online) 1(7). https://doi.org/10.1155/2015/193741 10.1155/2015/193741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hody S., Croisier J.L., Bury T., Rogister B., Leprince P. (2019) Eccentric muscle contractions: risks and benefits. Frontiers in Physiology 10, 536. https://doi.org/10.3389/fphys.2019.00536 10.3389/fphys.2019.00536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Kasahara K., Yoshida R., Yahata K., Sato S., Murakami Y., Aizawa K., Nakamura M. (2022) Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness. Healthcare 10, 96. https://doi.org/10.3390/healthcare10010096 10.3390/healthcare10010096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause F., Wilke J., Niederer D., Vogt L., Banzer W. (2019) Acute effects of foam rolling on passive stiffness, stretch sensation and fascial sliding: A randomized controlled trial. Humam Movement Science 67, 102514. https://doi.org/10.1016/j.humov.2019.102514 10.1016/j.humov.2019.102514 [DOI] [PubMed] [Google Scholar]
- Lau W.Y., Blazevich A.J., Newton M.J., Wu S.S.X., Nosaka K. (2015) Assessment of muscle pain induced by elbow-flexor eccentric exercise. Journal of Athletic Training 50, 1140-1148. https://doi.org/10.4085/1062-6050-50.11.05 10.4085/1062-6050-50.11.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mridha M., Ödman S. (1985) Characterization of subcutaneous edema by mechanical impedance measurements. Journal of Investigative Dermatology 85, 575-578. https://doi.org/10.1111/1523-1747.ep12283588 10.1111/1523-1747.ep12283588 [DOI] [PubMed] [Google Scholar]
- Pablos A., Ceca D., Jorda A., Rivera P., Colmena C., Elvira L., Martínez-Arnau F.M., Valles S.L. (2020) Protective effects of foam rolling against inflammation and notexin induced muscle damage in rats. International Journal of Medicine and Science 17, 71-81. https://doi.org/10.7150/ijms.37981 10.7150/ijms.37981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavan P., Stecco A., Stern R., Stecco C. (2014) Painful connections: densification versus fibrosis of fascia. Current Headache and Pain Reports 18, 441. https://doi.org/10.1007/s11916-014-0441-4 10.1007/s11916-014-0441-4 [DOI] [PubMed] [Google Scholar]
- Piehl-Aulin K., Laurent C., Engström-Laurent A., Hellström S., Henriksson J. (1985) Hyaluronan in human skeletal muscle of lower extremity: concentration, distribution, and effect of exercise. Journal of Applied Physiology 71, 2493-2498. https://doi.org/10.1152/jappl.1991.71.6.2493 10.1152/jappl.1991.71.6.2493 [DOI] [PubMed] [Google Scholar]
- Rosskopf A.B., Ehrmann C., Buck F.M., Gerber C., Flück M., Pfirrmann C.W.A. (2016) Quantitative shear-wave US elastography of the supraspinatus muscle: reliability of the method and relation to tendon integrity and muscle quality. Radiology 278, 465-474. https://doi.org/10.1148/radiol.2015150908 10.1148/radiol.2015150908 [DOI] [PubMed] [Google Scholar]
- Schleip R., Müller D.G. (2013) Training principles for fascial connective tissues: Scientific foundation and suggested practical applications. Journal of Bodywork and Movement Therapy 17, 103-115. https://doi.org/10.1016/j.jbmt.2012.06.007 10.1016/j.jbmt.2012.06.007 [DOI] [PubMed] [Google Scholar]
- Schleip R., Gabbiani G., Wilke J., Naylor I., Hinz B., Zorn A., Jäger H., Breul R., Schreiner S., Klingler W. (2019) Fascia is able to actively contract and may thereby influence musculoskeletal dynamics: A histochemical and mechanographic investigation. Frontiers in Physiology 10, 336. https://doi.org/10.3389/fphys.2019.00336 10.3389/fphys.2019.00336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sigrist R.M.S., Liau J., Kaffas A.E., Chammas M.C., Willmann J.K. (2017) Ultrasound elastography: review of techniques and clinical applications. Theranostics 7, 1303-1329. https://doi.org/10.7150/thno.18650 10.7150/thno.18650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taljanovic M.S., Gimber L.H., Becker G.W., Latt L.D., Klauser A.S., Melville D.M., Gao L., Witte R.S. (2017) Shear-wave elastography: basic physics and musculoskeletal applications. RadioGraphics 37, 855-870. https://doi.org/10.1148/rg.2017160116 10.1148/rg.2017160116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taş S., Onur M.R., Yılmaz S., Soylu A.R., Korkusuz F. (2017) Shear wave elastography is a reliable and repeatable method for measuring the elastic modulus of the rectus femoris muscle and patellar tendon. Journal of Ultrasound in Medicine 36, 565-570. https://doi.org/10.7863/ultra.16.03032 10.7863/ultra.16.03032 [DOI] [PubMed] [Google Scholar]
- Tenberg S., Nosaka K., Wilke J. (2022) Fascia thickness increases following eccentric exercise leading to delayed onset muscle soreness. Sports Medicine Open, in press https://doi.org/10.21203/rs.3.rs-826566/v1 10.21203/rs.3.rs-826566/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vexler A., Polyansky I., Gorodetsky R. (1999) Evaluation of skin viscoelasticity and anisotropy by measurement of speed of shear wave propagation with viscoelasticity skin analyzer. Journal of Investigative Dermatology 113, 732-739. https://doi.org/10.1046/j.1523-1747.1999.00751.x 10.1046/j.1523-1747.1999.00751.x [DOI] [PubMed] [Google Scholar]
- Wilke J., Behringer M. (2021) Is “delayed onset muscle soreness” a false friend? The potential implication of the fascial connective tissue in post-exercise discomfort. International Journal of Molecular Sciences 22, 9482. https://doi.org/10.3390/ijms22179482 10.3390/ijms22179482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilke J., Schleip R., Yucesoy C.A., Banzer W. (2018) Not merely a protective packing organ? A review of fascia and its force transmission capacity. Journal of Applied Physiology 124, 234-244. https://doi.org/10.1152/japplphysiol.00565.2017 10.1152/japplphysiol.00565.2017 [DOI] [PubMed] [Google Scholar]
- Wilke J., Hespanhol L., Behrens M. (2019) Is it all about the fascia? A systematic review and meta-analysis of the prevalence of extramuscular connective tissue lesions in muscle strain injury. Orthopedic Journal of Sports Medicine 7. https://doi.org/10.1177/2325967119888500 10.1177/2325967119888500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yanagisawa O., Sakuma J., Kawakami Y., Szuzuki K., Fukubayashi T. (2015) Effect of exercise-induced muscle damage on muscle hardness evaluated by ultrasound real-time tissue elastography. SpringerPlus 4. https://doi.org/10.1186/s40064-015-1094-4 10.1186/s40064-015-1094-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou J.P., Yu J.F., Feng Y.N., Liu C.L., Shen S.H., Zhang Z.J. (2020) Modulation in the elastic properties of gastrocnemius muscle heads in individuals with plantar fasciitis and its relationship with pain. Scientific Reports 10. https://doi.org/10.1038/s41598-020-59715-8 10.1038/s41598-020-59715-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zügel M., Maganaris C.N., Wilke J., Jurkat-Rott K., Klingler W., Wearing S.C., Findley T., Barbe M.F., Steinacker J.M., Vleeming A., Bloch W., Schleip R., Hodges P.W. (2018) Fascial tissue research in sports medicine: from molecules to tissue adaptation, injury and diagnostics: consensus statement. British Journal of Sports Medicine 52, 1497. https://doi.org/10.1136/bjsports-2018-099308 10.1136/bjsports-2018-099308 [DOI] [PMC free article] [PubMed] [Google Scholar]


