Abstract
Context:
Overtraining syndrome (OTS) is a condition characterized by a long-term performance decrement, which occurs after a persisting imbalance between training-related and nontraining-related load and recovery. Because of the lack of a gold standard diagnostic test, OTS remains a diagnosis of exclusion.
Objective:
To systematically review and map biomarkers and tools reported in the literature as potentially diagnostic for OTS.
Data Sources:
PubMed, Web of Science, and SPORTDiscus were searched from database inception to February 4, 2021, and results screened for eligibility. Backward and forward citation tracking on eligible records were used to complement results of database searching.
Study Selection:
Studies including athletes with a likely OTS diagnosis, as defined by the European College of Sport Science and the American College of Sports Medicine, and reporting at least 1 biomarker or tool potentially diagnostic for OTS were deemed eligible.
Study Design:
Scoping review following the guidelines of the Joanna Briggs Institute and PRISMA Extension for Scoping Reviews (PRISMA-ScR).
Level of Evidence:
Level 4.
Data Extraction:
Athletes’ population, criteria used to diagnose OTS, potentially diagnostic biomarkers and tools, as well as miscellaneous study characteristics were extracted.
Results:
The search yielded 5561 results, of which 39 met the eligibility criteria. Three diagnostic scores, namely the EROS-CLINICAL, EROS-SIMPLIFIED, and EROS-COMPLETE scores (EROS = Endocrine and Metabolic Responses on Overtraining Syndrome study), were identified. Additionally, basal hormone, neurotransmitter and other metabolite levels, hormonal responses to stimuli, psychological questionnaires, exercise tests, heart rate variability, electroencephalography, immunological and redox parameters, muscle structure, and body composition were reported as potentially diagnostic for OTS.
Conclusion:
Specific hormones, neurotransmitters, and metabolites, as well as psychological, electrocardiographic, electroencephalographic, and immunological patterns were identified as potentially diagnostic for OTS, reflecting its multisystemic nature. As exemplified by the EROS scores, combinations of these variables may be required to diagnose OTS. These scores must now be validated in larger samples and within female athletes.
Keywords: overtraining syndrome, athletes, diagnosis, biomarkers, tools
An overload in training is believed to be a necessary stimulus to enhance athletic performance. 39 However, adequate recovery balancing training and overall stress level are at least as important as training itself as an imbalance between training and recovery might lead to a decrement in performance.31,39 Functional overreaching is defined as a short-term decrease in performance (usually up to 2 weeks) followed by a supercompensation effect (adaptive improvement in performance). 52 In cases where the performance decrement is of a slightly longer duration (usually up to 3-4 weeks) and not followed by supercompensation, the term nonfunctional overreaching is used. 52 Finally, if reduced performance capacity lasts for more than 3 to 4 weeks and is followed by neither supercompensation nor improved athletic performance, the athlete is likely experiencing an overtraining syndrome (OTS). 52
Not only can OTS endanger athletes’ health, its detrimental effects can also extend to their career. 32 Athletes suffering from OTS might never again reach their previous level of performance. 6 With a prevalence of around 30% at age 15 years within young English athletes across different sports, OTS is not infrequent. 50 Because of the lack of a gold standard diagnostic test, OTS remains a challenging diagnosis of exclusion. 52
While systematic reviews aim to answer precise research questions, scoping reviews are appropriate to systematically summarize a field of research that has not been comprehensively reviewed yet. 59 With only 1 systematic review investigating the hormonal aspects of OTS, this field has exclusively been narratively reviewed to date. 11 Therefore, our study aims to systematically review the current literature and map biomarkers and tools reported as potentially diagnostic of OTS. In agreement with pertinent guidelines, this scoping review will not assess individual study quality. 59
Methods
Protocol and Registration
The present scoping review followed the guidelines of the Joanna Briggs Institute and the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Extension for Scoping Reviews (PRISMA-ScR).59,69 The protocol was registered on Open Science Framework on February 18, 2020. 19
Search Strategy and Studies Selection
The search strategy was developed in collaboration with an information specialist. Initial searches in PubMed were performed to identify articles on the topic. Words in titles and abstracts, MeSH (medical subject heading) terms, and author keywords were analyzed. Results of this initial search were used to develop single-concept OTS search strings for both PubMed and Web of Science (Appendix 1, available in the online version of this article). As there is no OTS-specific MeSH term, both strings were exclusively based on text word synonyms. In addition, SPORTDiscus was searched via EBSCOhost using a combination of subject headings and text word synonyms of OTS (Appendix 1, available online). All search strings were PRESS (Peer Review of Electronic Search Strategies) reviewed by an information specialist. 51
The search was conducted on February 19, 2020, and updated on January 20 and February 4, 2021. Retrieved references were exported to EndNote X9 and duplicates were removed. Two authors independently reviewed titles and abstracts against the selection criteria and deemed them as “include,” “exclude,” or “uncertain.” Discrepancies were resolved by discussion and consensus between the 2 authors, and with a third party in case a resolution could not be arrived at. For titles and abstracts marked as “include” or “uncertain,” the corresponding full-text articles were retrieved and reviewed independently by 2 authors for inclusion against the selection criteria.
To complement the results of direct database searching, the bibliographic references of all included articles (backward citation tracking), as well as the citing articles of those which are indexed in Scopus or the Web of Science (forward citation tracking), were screened.
Eligibility Criteria
Inclusion criteria included (1) original articles published until the date of last search, that is, February 4, 2021; (2) studies on humans only; (3) involving athletes with a diagnosis of OTS, as defined in the joint consensus statement by the European College of Sport Science and the American College of Sports Medicine 52 ; and (4) reporting at least 1 potential diagnostic test for OTS. Exclusion criteria included (1) nonoriginal articles; (2) studies written in a language other than English, French, or German (as authors have native-speaking expertise in these 3 languages); and (3) studies about medical conditions mimicking signs and/or symptoms of OTS.
Data Charting
The following information was extracted from the selected articles and mapped: (1) authorship, (2) publication date, (3) study design and duration, (4) studied population, (5) criteria used to diagnose OTS, and (6) biomarkers and tools reported as potentially diagnostic of OTS.
Results
Study Selection
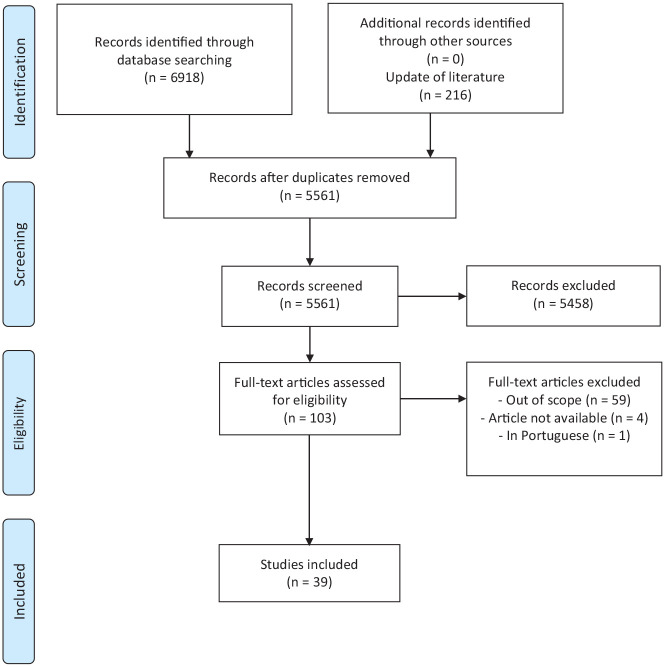
The search yielded unique 5561 results, of which 39 met the eligibility criteria (Figure 1). The authors agreed on all eligibility decisions on discussion without the need for a third party to be involved. Of note, 2 studies were included even though the inspected athletes were diagnosed by the authors with chronic fatigue syndrome and nonfunctional overreaching, respectively, as the pathological profiles described in these older publications matched the most recent OTS definition from 2013.52,57,65 Forward and backward citation tracking of the 39 included publications did not yield any additional publications.
Figure 1.
Study selection process according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Characteristics of Included Studies
The 39 included publications correspond to 30 independent studies (Appendix 2, available online; 3 studies were reported in eight,7-9,12,13,15-16-17 two36,37 and two43,44 publications, respectively). For ease of interpretation, studies’ characteristics are based on the 30 included studies, while biomarkers and tools are reported relatively to the 39 included publications. Thirty-seven publications were written in English and 2 were written in French.4,24 Publication year ranges from 1985 to 2020.
Sports Performed
As displayed in Table 1, 19 studies examined athletes from different sports,1,2,4-9,12,13,15-17,20,24,29,36,37,43-45,53,54,58,64,66,68,72 while 9 studies focused on 1 single sport. Two studies did not disclose the type of sport played.42,71 In terms of athletes per sport, running followed by endurance exercise (not further specified in the studies) and rowing were the most frequently examined sports (Table 2).
Table 1.
Number of studies per type of sport
| Type of Sport | No. of Studies (of Which Case Reports) |
|---|---|
| Multiple | 19 |
| Not specified | 2 (1) |
| Rowing | 3 (1) |
| Cross-country skiing | 2 (1) |
| Triathlon | 1 |
| Speed skating | 1 |
| Swimming | 1 (1) |
| Cycling | 1 (1) |
Table 2.
Number and proportion of subjects per type of sport
| OTS-Affected Subjects | Control Group Subjects | All Subjects | ||||
|---|---|---|---|---|---|---|
| Type of Sport Performed | n | Proportion, % | n | Proportion, % | n | Proportion, % |
| Not specified (multiple/unknown) | 123 | 37.5 | 333 | 53.4 | 456 | 47.9 |
| Running | 40 | 12.2 | 39 | 6.3 | 79 | 8.3 |
| Endurance exercise | 43 | 13.1 | 30 | 4.8 | 73 | 7.7 |
| Rowing | 25 | 7.6 | 39 | 6.3 | 64 | 6.7 |
| Swimming | 17 | 5.2 | 24 | 3.8 | 41 | 4.3 |
| CrossFit | 9 | 2.7 | 22 | 3.5 | 31 | 3.3 |
| Cross-country skiing | 5 | 1.5 | 22 | 3.5 | 27 | 2.8 |
| Speed skating | 3 | 0.9 | 22 | 3.5 | 25 | 2.6 |
| Triathlon | 13 | 4.0 | 10 | 1.6 | 23 | 2.4 |
| Cycling | 6 | 1.8 | 14 | 2.2 | 20 | 2.1 |
| Endurance and resistance exercise | 5 | 1.5 | 3 | 0.5 | 8 | 0.8 |
| Race walking | 4 | 1.2 | 4 | 0.6 | 8 | 0.8 |
| Resistance exercise | 8 | 2.4 | 0 | 0 | 8 | 0.8 |
| Ice hockey | 7 | 2.1 | 0 | 0 | 7 | 0.7 |
| Sprint running | 1 | 0.3 | 4 | 0.6 | 5 | 0.5 |
| Squash | 3 | 0.9 | 2 | 0.3 | 5 | 0.5 |
| Wrestling | 4 | 1.2 | 0 | 0 | 4 | 0.4 |
| Football | 3 | 0.9 | 0 | 0 | 3 | 0.3 |
| Motocross | 2 | 0.6 | 0 | 0 | 2 | 0.2 |
| Orienteering | 2 | 0.6 | 0 | 0 | 2 | 0.2 |
| Ballet | 1 | 0.3 | 0 | 0 | 1 | 0.1 |
| Biathlon | 1 | 0.3 | 0 | 0 | 1 | 0.1 |
| Rugby | 1 | 0.3 | 0 | 0 | 1 | 0.1 |
| Surfing | 1 | 0.3 | 0 | 0 | 1 | 0.1 |
| Tennis | 1 | 0.3 | 0 | 0 | 1 | 0.1 |
| Sedentary | 0 | 0 | 56 | 9.0 | 56 | 5.9 |
| Total | 328 | 100 | 624 | 100 | 952 | 100 |
OTS, overtraining syndrome.
Athletes and Control Group
In total, 952 subjects were examined including 328 athletes diagnosed with OTS and 624 healthy control subjects. In 24 studies, the athletes were already previously affected by OTS,2,4-9,12,15-17,20,24,29,30,34,36,37,42-45,47,53,54,56-58,64,65,68,72 while in 6 studies, OTS developed during the study.1,27,60,61,66,71 A total of 7 studies were uncontrolled: 2 studies did not have any control group,4,24 and 5 studies were case-reports with only 1 subject and no control.30,47,56,65,71 Eighteen studies enrolled healthy athletes as controls,1,2,5,6,19,29,34,36,37,42,45,54,57,58,60,61,66,68,72 3 studies had both healthy athletes and sedentary subjects as controls,7-9,12,13,15-17,27,43,44 1 study had sedentary controls only, 64 and 1 study compared OTS-affected athletes to athletes suffering from nonfunctional overreaching. 53
As shown in Table 3, 14 studies included both men and women.2,4-6,20,24,36,37,42,45,53,64,66,68,72 Ten studies, of which 3 were case reports, focused on men only1,7-9,12,13,15-17,27,30,34,54,56,60,61,71 and 2 studies, of which 1 was a case report, on women only.47,57 Four studies did not specify participants’ sex.29,43,44,58,65 The duration of performance decrement was at least 3 weeks in all the studies included.
Table 3.
Sex distribution among groups
| OTS-Affected Subjects | Control Group Subjects | Overall | ||||
|---|---|---|---|---|---|---|
| Sex | Absolute number | Proportion, % | Absolute number | Proportion, % | Absolute number | Proportion, % |
| Unknown | 91 | 27.8 | 398 | 63.8 | 489 | 51.4 |
| Male | 155 | 47.3 | 175 | 28.0 | 330 | 34.7 |
| Female | 82 | 25.0 | 51 | 8.2 | 133 | 14.0 |
| Total | 328 | 100 | 624 | 100 | 952 | 100 |
OTS, overtraining syndrome.
Findings From the Selected Publications
Diagnostic Scores
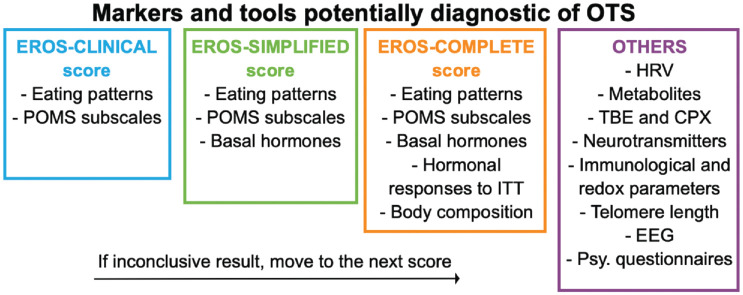
Three diagnostic scores, namely the EROS-CLINICAL, EROS-SIMPLIFIED, and EROS-COMPLETE scores, were identified (Appendix 3, available online). 7 As indicated in Appendix 3 (available online), the EROS-CLINICAL score is based on clinical items only, the EROS-SIMPLIFIED score includes clinical and biochemical tests, while the EROS-COMPLETE score consisted of clinical, biochemical, insulin tolerance test (ITT), and body composition variables. 7 Combined in a decision tree, these 3 scores could distinguish all apparently OTS-affected from healthy male athletes in the original study. 7
Basal Hormone Levels
Basal hormone levels, defined as hormone levels in a resting state, were the most frequently assessed biomarkers, as they were used to identify OTS in 17 publications.1,7,8,13,15-17,27,30,34,42,53,54,56,58,64,66 As indicated in Appendix 3 (available online), the most common hormonal alterations observed in OTS-affected compared with healthy athletes were the following: diminished serum testosterone to estradiol ratio (n = 4),7,8,15,16 diminished circulating testosterone level (n = 3),7,17,56 elevated serum estradiol level (n = 3),8,16,17 elevated plasma and salivary cortisol level (n = 4),1,13,30,53 elevated nocturnal urinary catecholamines (n = 3),8,16,17 elevated plasma adrenocorticotropic hormone (ACTH) level (n = 2),53,54 diminished serum prolactin (PRL) level (n = 2),7,12 and diminished serum growth hormone (GH) level (n = 2).7,12
Responses to Stimuli
Hormonal response to stimuli was evaluated in a total of 11 publications using either ITT (n = 7)1,7,12,13,15-17 or 2-bout exercise test (TBE, n = 4),6,53,54,57 which consists of 2 consecutive incremental exercise protocols to exhaustion with 4 hours of rest in between. 54 Blunted response to ITT in OTS-affected compared with healthy athletes was reported for ACTH (n = 5),1,7,13,15,16 cortisol (n = 5),1,7,13,15,17 GH (n = 5),1,7,12,15,17 and PRL (n = 4).1,7,12,17 Response to the first and second bouts of TBE was, respectively, reported to be increased and blunted for both ACTH and PRL.6,53,54 GH response to both bouts was reported to be blunted (n = 2).53,54 Cortisol response to both bouts was described as slightly increased (n = 2).54,57 Maximal lactate concentration less than 8 mmol/L at the end of both bouts showed high sensitivity for OTS. 53 Finally, decreased VO2peak, maximum workload, and anaerobic threshold as well as increased perception of effort were evidenced in an ultra-endurance cyclist suffering from OTS compared with his own previous values. 65
Psychological Questionnaires
Psychological questionnaires used to distinguish OTS-affected from control groups included the Profile of Mood States (POMS, n = 10),6,7,9,15-17,29,30,34,57 the overtraining questionnaire of the Société française de médecine du sport (French Society of Sport Medicine, SFMS, n = 2),4,24 the Hamilton Depression Scale (HAMD) and Montgomery-Åsberg Depression Rating Scale (MADRS, n = 1), 72 as well as the Recovery Stress Questionnaire for Athletes (RESTQ-Sport, n = 1). 56 Reported differences in POMS within OTS-affected compared with healthy athletes included increased total POMS score (n = 4),9,17,30,34 fatigue score (n = 5),7,9,16,29,30 tension score (n = 3),7,15,34 anger score (n = 3),7,29,34 depression score (n = 2),29,34 confusion score (n = 2),29,30 as well as decreased vigor score (n = 4).7,9,15,29 An SFMS score ≥20 was reported to be indicative of OTS.4,24 The HAMD and MADRS depression scales, as well as the RESTQ-Sport, appeared to be elevated in OTS-affected compared with healthy athletes.57,72
Heart Rate Variability
High and low periodic oscillations (ie, high and low frequency) of the RR interval (interval between QRS complexes of normal sinus depolarizations) 67 were elevated (n = 2)34,36 and reduced, respectively (n = 3),34,36,37 in OTS-affected versus healthy athletes. This speaks in favor of parasympathetic dominance. Conversely, 1 study reported elevated low frequency in OTS-affected athletes and sedentary controls compared with well-trained athletes. 43
Metabolic Alterations
One study used Fourier transform infrared spectroscopy, a technique using a mathematical process (Fourier transformation) to obtain an infrared absorption spectrum of a solid, liquid, or gas, 25 to investigate serum metabolic alterations in response to exercise. 60 Two rowers displayed a disturbed saccharide absorption spectrum after 5 weeks of training, followed by abnormal lipid and peptide absorption spectra on weeks 8 and 15, respectively, before being clinically diagnosed with OTS on week 15. The disturbed peptide metabolism persisted until the end of the study (week 37). Rowers suspected of suffering from nonfunctional overreaching were asked to rest before abnormal peptide absorption spectra appeared, and clinically recovered in 3 weeks. A disturbed peptide absorption spectrum was considered diagnostic for OTS. Plasma lipid profile was also reported to be altered in OTS-affected athletes, characterized by an increase in glycerol and a decrease in triglycerides, very low-density lipoprotein and apolipoprotein C3 concentration. 61 Diminished glutamine levels (n = 2),58,64 elevated glutamate levels (n = 2)58,66 as well as diminished glutamine to glutamate ratio (n = 1) 66 were evidenced in plasma in resting state. Additionally, higher levels of serum creatine kinase were also reported within OTS-affected compared with healthy athletes.8,15
Neurotransmitters
Decreased sensitivity of serotonin receptors was reported in OTS-affected athletes compared with well-trained controls, 5 while a reduced number of serotonin transporters was found in a single OTS-affected and depressed team athlete using single-photon emission computed tomography. 71 The latter was interpreted as decreased serotonin production and release. 71
Immunological and Redox Parameters
The ratio of neutrophils to lymphocytes was shown to be decreased, 15 while interleukin (IL)-1β, IL-6, and tumor necrosis factor-α were elevated in response to a single exercise bout. 42 Alterations in redox homeostasis, characterized by increased oxidant and reduced antioxidant capacities, were reported.44,47,68 Specifically, markers of protein oxidation and total oxidant capacity were elevated, while antioxidants such as red blood cell glutathione, coenzyme Q10, γ-tocopherol, and carotenoids were diminished.44,47,68
Muscular Alterations and Body Composition
Diminished telomere lengths, 20 focal necrosis, and myofibrillar disorganization 65 were observed within muscle fibers of OTS-affected compared with nonaffected athletes. Lower muscle mass and body water as well as higher fat mass were observed within OTS-affected compared with healthy athletes.7,15,42 Similar alterations were reported in OTS-affected CrossFit athletes. 17
Electroencephalography
Differences in electroencephalography (EEG) features were observed between 100 OTS-affected athletes and 100 healthy subjects. 2 OTS-affected athletes were characterized by decreased α-index, increased amplitude of β-waves, and slow wave occurrence (mainly θ-waves). Hyperventilation-induced EEG-responses in OTS-affected athletes included increased number of slow waves, increased slow wave index and blunted increase of α-wave amplitude. During exercise, α-wave amplitude increased in the control group, while no change was evidenced in the OTS group.
Discussion
The present work systematically reviewed and mapped tools and biomarkers that are potentially diagnostic for OTS. The obtained results are summarized in Figure 2. The diversity of the tools and biomarkers identified in the present work highlights the fact that OTS affects multiple body systems. 52 This diversity could also support the hypothesis made by Cadegiani et al 7 that OTS is an heterogenous clinical entity whose symptomatic presentation varies between athletes.
Figure 2.
Overview of the identified biomarkers and tools potentially diagnostic of overtraining syndrome (OTS). CPX, cardiopulmonary exercise test; EEG, electroencephalography; HRV, heart rate variability; ITT, insulin tolerance test; POMS, Profile of Mood State; psy. questionnaires, psychological questionnaires; TBE, 2-bout exercise test.
Cadegiani et al 7 conducted the Endocrine and Metabolic Responses on Overtraining Syndrome (EROS) study, which resulted in 11 publications.7-10,12-18 They evaluated 117 potential OTS markers and concluded that individually none of the markers accurately distinguished OTS-affected from healthy athletes. 7 Combining the most promising markers, they elaborated 3 diagnostic scores, namely the EROS-CLINICAL, EROS-SIMPLIFIED, and EROS-COMPLETE scores, which could distinguish all apparently OTS-affected from healthy male athletes, once combined in a decision tree. 7 While Cadegiani et al 7 reported a 100% diagnostic accuracy of these scores in the EROS study, this claim lacks a firm methodological foundation because of the absence of a gold standard diagnostic test for OTS. Furthermore, these scores should now be validated in larger samples and female athletes as highlighted by Cadegiani et al. 7 Other markers such as heart rate variability (HRV) variables or metabolite levels could be considered as potential additional items of the EROS scores.
The autonomous nervous system hypothesis posits dominance of parasympathetic activation and decreased sympathetic activation to be the underlying cause of the symptoms experienced in OTS. 46 Although comparing HRV data from different studies is challenging because of methodical heterogeneity, the findings of the present work support, at least partly, the autonomous nervous system hypothesis.32,52 Namely, elevated high-frequency power and reduced low-frequency power were observed within OTS-affected compared with healthy athletes.34,36,37
Alteration in metabolite levels represents another promising field of research. In addition to their roles as building blocks of cell components and fuels in cellular energetics, metabolites also act as signaling molecules and driving forces in the pathophysiology of human diseases.63,73 The successive alterations reported in saccharide, lipid, and peptide absorption spectra along the fatigue continuum are preliminary in nature and cannot yet be used in the diagnostic process of OTS. These findings should pave the way for future research investigating the metabolic determinants of OTS. Novel technologies such as metabolomics, a powerful metabolic phenotyping tool, could improve OTS-affected athletes’ profiling and ultimately contribute to the discovery of novel biomarkers. 40 For instance, diminished glutamine and elevated glutamate levels have often been linked to impaired immune system within athletes suffering from a disorder of the continuum fatigue spectrum.22,33,38,66
Basal hormone levels were frequently reported to be altered in OTS-affected compared with healthy athletes. Catabolic hormones, such as cortisol and catecholamines, tended to be elevated, while anabolic hormones, such as testosterone and estradiol, showed conflicting results. Several authors believe that hormonal responses to stimuli are more accurate than basal hormone levels in diagnosing OTS.11,70 Hormone levels did behave more homogenously on stimulation with ACTH, PRL, GH, and insulin-like growth factor-1 (IGF-1) being blunted in response to ITT or exercise stimuli within OTS-affected compared with healthy and overreached athletes. Only cortisol levels showed varied responses. OTS-affected athletes displayed dysfunctions in the hypothalamus-pituitary-adrenal axis in response to a stress situation.13,54 These dysfunctions are likely to be central (either in the hypothalamus and/or the pituitary), since the adrenals were reported to respond physiologically to ACTH stimulation tests in OTS-affected athletes. 13
Psychological questionnaires have long been used in the OTS research field, as mood disturbances are common in OTS-affected athletes. These athletes tend to display higher total POMS score, higher fatigue, tension, depression, anger, and confusion subscores as well as a lower vigor subscore. Similar psychological patterns were observed using other psychological questionnaires (SFMS, HAMD, MADRS, and RESTQ-Sport). Importantly, psychological questionnaires applied in isolation are probably more useful in the monitoring of both the training and recovery processes than in the diagnosis itself. 32 Neurobiologically, the reported diminished serotonin receptors’ sensitivity and transporters’ number are compatible with the observed psychological patterns.23,55
A potential diagnostic tool that has not received much attention so far is EEG. A variety of EEG patterns were reported to be different between OTS-affected athletes and healthy subjects. As EEG is noninvasive and relatively inexpensive, further research in this promising field is warranted. Similarly, diminished telomere length in muscle cells represents another sparsely researched feature observed in OTS-affected athletes. While reduction in telomere length naturally occurs with aging, certain factors such as exercise-related muscle damage can accelerate this process. 48 Interestingly, telomere length was inversely correlated to the number of running years and training hours. 62 Whether telomere length responds differently to physiological training adaptation and pathological training maladaptation remains to be determined.
Limitations
The field of OTS research faces several hurdles. First, the lack of standard definitions and terminologies in OTS, coupled with the fact that distinctions between nonfunctional overreaching and OTS are not always straightforward, make it difficult to characterize athletes that show a decrement in performance and ultimately compare studies. 52 Consequently, clinical studies investigating OTS should be viewed in this context and interpreted with caution. Second, conclusions of most included reports are limited by small samples sizes. 32 Of the 39 publications included for this scoping review, 8 were based on only 1 single subject. As a result, the overall quality of the scientific evidence is low, that is, level 4.
Athletes engaged in endurance sports were clearly overrepresented in the included publications. Although both endurance and non-endurance athletes are at risk for OTS, 49 this overrepresentation is common in the OTS research field.28,52 Interestingly, differences were observed between OTS-affected athletes engaged in endurance and resistance sports 26 with catecholamine levels being decreased in the former but increased in the latter. 11 Therefore, diagnostic tools and biomarkers for OTS might need to be specific to the type of sport. 28
Female athletes are underrepresented in OTS studies, as is the case in much of sports and exercise medicine research. 21 The study of female athletes with OTS is complicated by the biological complexity of the menstrual cycle. 3 Both the phases of the menstrual cycle and the use of oral contraceptives can affect hormonal testing in female athletes.35,52 Therefore, to provide female-specific biomarkers and normal values, it is necessary to not only investigate more female athletes suffering from OTS but also consider the hormone fluctuations throughout the menstrual cycle as well as the intake of oral contraceptives. 41
Conclusion
This scoping review included 39 publications reporting biomarkers and tools potentially diagnostic for OTS. The quality of evidence available was low as indicated by level 4 rating. The diversity of the identified markers and tools is in line with the fact that OTS affects multiple body systems. Moreover, it supports the hypothesis that OTS might be a heterogenous syndrome consisting of different clinical phenotypes. Thus, rather than using parameters in isolation, there is a trend toward combining multiple variables to diagnose OTS. This is demonstrated by the recently developed EROS-CLINICAL, EROS-SIMPLIFIED, and EROS-COMPLETE scores. These scores must now be validated in larger samples and within female athletes. Finally, omic scale profiling of OTS-affected athletes might contribute to a better understanding of this condition.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iD: Justin Carrard  https://orcid.org/0000-0002-2380-105X
https://orcid.org/0000-0002-2380-105X
References
- 1. Barron JL, Noakes TD, Levy W, Smith C, Millar RP. Hypothalamic dysfunction in overtrained athletes. J Clin Endocrinol Metab. 1985;60:803-806. [DOI] [PubMed] [Google Scholar]
- 2. Bian F. Electroencephalogram analysis of athletes with over-training syndrome. Neuroquantology. 2018;16:153-157. [Google Scholar]
- 3. Bruinvels G, Burden RJ, McGregor AJ, et al. Sport, exercise and the menstrual cycle: where is the research? Br J Sports Med. 2017;51:487-488. [DOI] [PubMed] [Google Scholar]
- 4. Brun JF, Varlet-Marie E, Faugoin C, Mercier J. Overtraining syndrome: clinical, laboratory and exercise-test presentation of six cases. Sci Sports. 2009;24:40-44. [Google Scholar]
- 5. Budgett R, Hiscock N, Arida RM, Castell LM. The effects of the 5-HT2C agonist m-chlorophenylpiperazine on elite athletes with unexplained underperformance syndrome (overtraining). Br J Sports Med. 2010;44:280-283. [DOI] [PubMed] [Google Scholar]
- 6. Buyse L, Decroix L, Timmermans N, Barbe K, Verrelst R, Meeusen R. Improving the diagnosis of nonfunctional overreaching and overtraining syndrome. Med Sci Sports Exerc. 2019;51:2524-2530. [DOI] [PubMed] [Google Scholar]
- 7. Cadegiani FA, da Silva PHL, Abrao TCP, Kater CE. Diagnosis of overtraining syndrome: results of the endocrine and metabolic responses on overtraining syndrome study: EROS-DIAGNOSIS. J Sports Med. 2020;2020:3937819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cadegiani FA, Kater CE. Basal hormones and biochemical markers as predictors of overtraining syndrome in male athletes: the EROS-BASAL study. J Athl Train. 2019;54:906-914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cadegiani FA, Kater CE. Body composition, metabolism, sleep, psychological and eating patterns of overtraining syndrome: results of the EROS study (EROS-PROFILE). J Sports Sci. 2018;36:1902-1910. [DOI] [PubMed] [Google Scholar]
- 10. Cadegiani FA, Kater CE. Enhancement of hypothalamic-pituitary activity in male athletes: evidence of a novel hormonal mechanism of physical conditioning. BMC Endocr Disord. 2019;19:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cadegiani FA, Kater CE. Hormonal aspects of overtraining syndrome: a systematic review. BMC Sports Sci Med Rehabil. 2017;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cadegiani FA, Kater CE. Hormonal response to a non-exercise stress test in athletes with overtraining syndrome: results from the Endocrine and metabolic Responses on Overtraining Syndrome (EROS)—EROS-STRESS. J Sci Med Sport. 2018;21:648-653. [DOI] [PubMed] [Google Scholar]
- 13. Cadegiani FA, Kater CE. Hypothalamic-pituitary-adrenal (HPA) axis functioning in overtraining syndrome: findings from Endocrine and Metabolic Responses on Overtraining Syndrome (EROS)–EROS-HPA axis. Sports Med Open. 2017;3:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cadegiani FA, Kater CE. Inter-correlations among clinical, metabolic, and biochemical parameters and their predictive value in healthy and overtrained male athletes: the EROS-CORRELATIONS study. Front Endocrinol (Lausanne). 2019;10:858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cadegiani FA, Kater CE. Novel causes and consequences of overtraining syndrome: the EROS-DISRUPTORS study. BMC Sports Sci Med Rehabil. 2019;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cadegiani FA, Kater CE. Novel insights of overtraining syndrome discovered from the EROS study. BMJ Open Sport Exerc Med. 2019;5:e000542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cadegiani FA, Kater CE, Gazola M. Clinical and biochemical characteristics of high-intensity functional training (HIFT) and overtraining syndrome: findings from the EROS study (the EROS-HIFT). J Sports Sci. 2019;37:1296-1307. [DOI] [PubMed] [Google Scholar]
- 18. Cadegiani FA, Silva PHL, Abrao TCP, Kater CE. Novel markers of recovery from overtraining syndrome: the EROS-LONGITUDINAL study. Int J Sports Physiol Perform. Published online January 5, 2021. doi: 10.1123/ijspp.2020-0248 [DOI] [PubMed] [Google Scholar]
- 19. Carrard J, Rigort A-C, Hinrichs T, Appenzeller-Herzog C, Schmidt-Trucksäss A. Diagnosing overtraining syndrome: a scoping review protocol. doi: 10.17605/OSF.IO/SHKU3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Collins M, Renault V, Grobler LA, et al. Athletes with exercise-associated fatigue have abnormally short muscle DNA telomeres. Med Sci Sports Exerc. 2003;35:1524-1528. [DOI] [PubMed] [Google Scholar]
- 21. Costello JT, Bieuzen F, Bleakley CM. Where are all the female participants in sports and exercise medicine research? Eur J Sport Sci. 2014;14:847-851. [DOI] [PubMed] [Google Scholar]
- 22. Coutts AJ, Reaburn P, Piva TJ, Rowsell GJ. Monitoring for overreaching in rugby league players. Eur J Appl Physiol. 2007;99:313-324. [DOI] [PubMed] [Google Scholar]
- 23. Dell’Osso L, Carmassi C, Mucci F, Marazziti D. Depression, serotonin and tryptophan. Curr Pharm Des. 2016;22:949-954. [DOI] [PubMed] [Google Scholar]
- 24. Favre-Juvin A, Flore P, Rousseaux Blanchi MP. Approche clinique du surentrainement [Clinical aspect of overtraining]. Sci Sports. 2003;18:287-289. [Google Scholar]
- 25. Finlayson D, Rinaldi C, Baker MJ. Is infrared spectroscopy ready for the clinic? Anal Chem. 2019;91:12117-12128. [DOI] [PubMed] [Google Scholar]
- 26. Fry AC, Kraemer WJ. Resistance exercise overtraining and overreaching. Neuroendocrine responses. Sports Med. 1997;23:106-129. [DOI] [PubMed] [Google Scholar]
- 27. Gouarne C, Groussard C, Gratas-Delamarche A, Delamarche P, Duclos M. Overnight urinary cortisol and cortisone add new insights into adaptation to training. Med Sci Sports Exerc. 2005;37:1157-1167. [DOI] [PubMed] [Google Scholar]
- 28. Grandou C, Wallace L, Impellizzeri FM, Allen NG, Coutts AJ. Overtraining in resistance exercise: an exploratory systematic review and methodological appraisal of the literature. Sports Med. 2020;50:815-828. [DOI] [PubMed] [Google Scholar]
- 29. Grant CC, Van Rensburg DCJ, Collins R, Wood PS, Du Toit PJ. The Profile of Mood State (POMS) questionnaire as an indicator of overtraining syndrome (OTS) in endurance athletes. Afr J Phys Health Educ Recreat Dance. 2012;suppl:23-32. [Google Scholar]
- 30. Gustafsson H, Holmberg HC, Hassmen P. An elite endurance athlete’s recovery from underperformance aided by a multidisciplinary sport science support team. Eur J Sport Sci. 2008;8:267-276. [Google Scholar]
- 31. Halson SL. Monitoring training load to understand fatigue in athletes. Sports Med. 2014;44(suppl 2):S139-S147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Halson SL, Jeukendrup AE. Does overtraining exist? An analysis of overreaching and overtraining research. Sports Med. 2004;34:967-981. [DOI] [PubMed] [Google Scholar]
- 33. Halson SL, Lancaster GI, Jeukendrup AE, Gleeson M. Immunological responses to overreaching in cyclists. Med Sci Sports Exerc. 2003;35:854-861. [DOI] [PubMed] [Google Scholar]
- 34. Hedelin R, Wiklund U, Bjerle P, Henriksson-Larsen K. Cardiac autonomic imbalance in an overtrained athlete. Med Sci Sports Exerc. 2000;32:1531-1533. [DOI] [PubMed] [Google Scholar]
- 35. Hertel J, König J, Homuth G, et al. Evidence for stress-like alterations in the HPA-axis in women taking oral contraceptives. Sci Rep. 2017;7:14111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hynynen E, Uusitalo A, Konttinen N, Rusko H. Cardiac autonomic responses to standing up and cognitive task in overtrained athletes. Int J Sports Med. 2008;29:552-558. [DOI] [PubMed] [Google Scholar]
- 37. Hynynen E, Uusitalo A, Konttinen N, Rusko H. Heart rate variability during night sleep and after awakening in overtrained athletes. Med Sci Sports Exerc. 2006;38:313-317. [DOI] [PubMed] [Google Scholar]
- 38. Ikonen JN, Joro R, Uusitalo AL, et al. Effects of military training on plasma amino acid concentrations and their associations with overreaching. Exp Biol Med. 2020;245:1029-1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Issurin VB. New horizons for the methodology and physiology of training periodization. Sports Med. 2010;40:189-206. [DOI] [PubMed] [Google Scholar]
- 40. Ivanisevic J, Thomas A. Metabolomics as a tool to understand pathophysiological processes. Methods Mol Biol. 2018;1730:3-28. [DOI] [PubMed] [Google Scholar]
- 41. Janse DEJX, Thompson B, Han A. Methodological recommendations for menstrual cycle research in sports and exercise. Med Sci Sports Exerc. 2019;51:2610-2617. [DOI] [PubMed] [Google Scholar]
- 42. Joro R, Uusitalo A, DeRuisseau KC, Atalay M. Changes in cytokines, leptin, and IGF-1 levels in overtrained athletes during a prolonged recovery phase: a case-control study. J Sports Sci. 2017;35:2342-2349. [DOI] [PubMed] [Google Scholar]
- 43. Kajaia T, Maskhulia L, Chelidze K, Akhalkatsi V, Kakhabrishvili Z. The effects of non-functional overreaching and overtraining on autonomic nervous system function in highly trained athletes. Georgian Med News. 2017;264:97-103. [PubMed] [Google Scholar]
- 44. Kajaia T, Maskhulia L, Chelidze K, Akhalkatsi V, McHedlidze T. Implication of relationship between oxidative stress and antioxidant status in blood serum. Georgian Med News. 2018;284:71-76. [PubMed] [Google Scholar]
- 45. Kiviniemi AM, Tulppo MP, Hautala AJ, Vanninen E, Uusitalo AL. Altered relationship between R-R interval and R-R interval variability in endurance athletes with overtraining syndrome. Scand J Med Sci Sports. 2014;24:e77-e85. [DOI] [PubMed] [Google Scholar]
- 46. Kreher JB, Schwartz JB. Overtraining syndrome: a practical guide. Sports Health. 2012;4:128-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lewis NA, Redgrave A, Homer M, et al. Alterations in redox homeostasis during recovery from unexplained underperformance syndrome in an elite international rower. Int J Sports Physiol Perform. 2018;13:107-111. [DOI] [PubMed] [Google Scholar]
- 48. Marques A, Gouveira ÉR, Peralta M, et al. Cardiorespiratory fitness and telomere length: a systematic review. J Sports Sci. 2020;38:1690-1697. [DOI] [PubMed] [Google Scholar]
- 49. Matos N, Winsley RJ. Trainability of young athletes and overtraining. J Sports Sci Med. 2007;6:353-367. [PMC free article] [PubMed] [Google Scholar]
- 50. Matos NF, Winsley RJ, Williams CA. Prevalence of nonfunctional overreaching/overtraining in young English athletes. Med Sci Sports Exerc. 2011;43:1287-1294. [DOI] [PubMed] [Google Scholar]
- 51. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40-46. [DOI] [PubMed] [Google Scholar]
- 52. Meeusen R, Duclos M, Foster C, et al. Prevention, diagnosis, and treatment of the overtraining syndrome: joint consensus statement of the European College of Sport Science and the American College of Sports Medicine. Med Sci Sports Exerc. 2013;45:186-205. [DOI] [PubMed] [Google Scholar]
- 53. Meeusen R, Nederhof E, Buyse L, Roelands B, de Schutter G, Piacentini MF. Diagnosing overtraining in athletes using the two-bout exercise protocol. Br J Sports Med. 2010;44:642-648. [DOI] [PubMed] [Google Scholar]
- 54. Meeusen R, Piacentini MF, Busschaert B, Buyse L, De Schutter G, Stray-Gundersen J. Hormonal responses in athletes: the use of a two bout exercise protocol to detect subtle differences in (over)training status. Eur J Appl Physiol. 2004;91:140-146. [DOI] [PubMed] [Google Scholar]
- 55. Meeusen R, Watson P, Hasegawa H, Roelands B, Piacentini MF. Brain neurotransmitters in fatigue and overtraining. Appl Physiol Nutr Metab. 2007;32:857-864. [DOI] [PubMed] [Google Scholar]
- 56. Narla A, Kaiser K, Tannock LR. Extremely low testosterone due to relative energy deficiency in sport: a case report. AACE Clin Case Rep. 2019;5:e129-e131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Nederhof E, Zwerver J, Brink M, Meeusen R, Lemmink K. Different diagnostic tools in nonfunctional overreaching. Int J Sports Med. 2008;29:590-597. [DOI] [PubMed] [Google Scholar]
- 58. Parry-Billings M, Budgett R, Koutedakis Y, et al. Plasma amino acid concentrations in the overtraining syndrome: possible effects on the immune system. Med Sci Sports Exerc. 1992;24:1353-1358. [PubMed] [Google Scholar]
- 59. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141-146. [DOI] [PubMed] [Google Scholar]
- 60. Petibois C, Cazorla G, Deleris G. FT-IR spectroscopy utilization to sportsmen fatigability evaluation and control. Med Sci Sports Exerc. 2000;32:1803-1808. [DOI] [PubMed] [Google Scholar]
- 61. Petibois C, Deleris G. Alterations of lipid profile in endurance over-trained subjects. Arch Med Res. 2004;35:532-539. [DOI] [PubMed] [Google Scholar]
- 62. Rae DE, Vignaud A, Butler-Browne GS, et al. Skeletal muscle telomere length in healthy, experienced, endurance runners. Eur J Appl Physiol. 2010;109:323-330. [DOI] [PubMed] [Google Scholar]
- 63. Rinschen MM, Ivanisevic J, Giera M, Siuzdak G. Identification of bioactive metabolites using activity metabolomics. Nat Rev Mol Cell Biol. 2019;20:353-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Rowbottom DG, Keast D, Goodman C, Morton AR. The haematological, biochemical and immunological profile of athletes suffering from the overtraining syndrome. Eur J Appl Physiol Occup Physiol. 1995;70:502-509. [DOI] [PubMed] [Google Scholar]
- 65. Rowbottom DG, Keast D, Green S, Kakulas B, Morton AR. The case history of an elite ultra-endurance cyclist who developed chronic fatigue syndrome. Med Sci Sports Exerc. 1998;30:1345-1348. [DOI] [PubMed] [Google Scholar]
- 66. Smith DJ, Norris SR. Changes in glutamine and glutamate concentrations for tracking training tolerance. Med Sci Sports Exerc. 2000;32:684-689. [DOI] [PubMed] [Google Scholar]
- 67. Sztajzel J. Heart rate variability: a noninvasive electrocardiographic method to measure the autonomic nervous system. Swiss Med Wkly. 2004;134:514-522. [DOI] [PubMed] [Google Scholar]
- 68. Tanskanen M, Atalay M, Uusitalo A. Altered oxidative stress in overtrained athletes. J Sports Sci. 2010;28:309-317. [DOI] [PubMed] [Google Scholar]
- 69. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467-473. [DOI] [PubMed] [Google Scholar]
- 70. Urhausen A, Kindermann W. Diagnosis of overtraining. Sports Med. 2002;32:95-102. [DOI] [PubMed] [Google Scholar]
- 71. Uusitalo AL, Valkonen-Korhonen M, Helenius P, Vanninen E, Bergstrom KA, Kuikka JT. Abnormal serotonin reuptake in an overtrained, insomnic and depressed team athlete. Int J Sports Med. 2004;25:150-153. [DOI] [PubMed] [Google Scholar]
- 72. Uusitalo AL, Vanninen E, Valkonen-Korhonen M, Kuikka JT. Brain serotonin reuptake did not change during one year in overtrained athletes. Int J Sports Med. 2006;27:702-708. [DOI] [PubMed] [Google Scholar]
- 73. Wishart DS. Metabolomics for investigating physiological and pathophysiological processes. Physiol Rev. 2019;99:1819-1875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_19417381211044739 for Diagnosing Overtraining Syndrome: A Scoping Review by Justin Carrard, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs and Arno Schmidt-Trucksäss in Sports Health: A Multidisciplinary Approach