Abstract
Background:
There exists limited objective functional return-to-play criteria after surgical stabilization for anterior shoulder instability in the competitive athlete.
Hypothesis:
The proposed functional rehabilitation program and psychological evaluation after arthroscopic Bankart repair will help athletes return to sport with a decreased redislocation rate on return.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
Participants were contact or overhead athletes at the high school or collegiate level. Each underwent arthroscopic Bankart repair after a single dislocation event, with less than 10% glenoid bone loss. Western Ontario Shoulder Instability Index (WOSI) scores, Single Assessment Numeric Evaluation (SANE) scores, and American Shoulder and Elbow Surgeons (ASES) scores were evaluated pre- and postoperatively. Athletes were only allowed to return to competition after completing the proposed functional and psychological rehabilitation protocol.
Results:
A total of 62 participants were enrolled (52 male, 10 female; average age, 18.7 years (range 16-24 years); mean Instability Severity Index Score, 5.63 ± 0.55). All returned to sport for 1 full season and completed a minimum of 2 years of follow-up. The average time to pass functional testing was 6.2 ± 0.7 months, psychological testing was 5.2 ± 0.5 months, and return to sport was 6.5 ± 0.7 months. SANE scores improved from 44.3 to 90.0, ASES from 45.5 to 89.3, and WOSI from 1578.0 to 178.9 (all P < 0.001). Redislocation rate was 6.5% (4 of 62).
Conclusion:
The proposed functional rehabilitation and psychological assessment protocol is safe and effective in returning athletes to sport after arthroscopic surgical intervention for anterior shoulder instability. This demonstrated a low redislocation rate after 2-year follow-up.
Clinical Relevance:
Most return-to-play protocols after arthroscopic Bankart repair are centered on recovery time alone, with limited focus on functional rehabilitation, psychological assessment, and return-to-play testing parameters. To our knowledge, this is the first study to propose a dedicated rehabilitation program incorporating functional testing, psychological readiness, and return-to-play criteria for competitive athletes recovering from arthroscopic shoulder stabilization.
Keywords: shoulder instability, physical therapy/rehabilitation, Bankart repair, return-to-play protocol
Shoulder instability in the competitive athlete is a challenging clinical condition to successfully treat. The Multicenter Orthopaedic Outcomes Network Shoulder Instability Cohort identified key risk factors of shoulder instability including male sex, age less than 30 years, contact sports, and anterior instability. 15 Athletes younger than 25 years were at an especially increased risk of recurrent instability.15,24,26 Nonoperative management of traumatic anterior shoulder dislocations in adolescents also shows poor outcomes. In a noteworthy study with 25-year follow-up, Hovelius et al 13 demonstrated that recurrent dislocation rates in conservatively managed participants aged 12 to 25 years approached 50%. Additional studies indicated higher redislocation rates upward of 48% to 100% in the young, conservatively managed population.2,7,22,26 Contact athletes or those involved in overhead activities are at significantly increased risk.3,23 Because of these concerns, arthroscopic stabilization surgery is often recommended for young athletes with a history of primary instability to decrease the risk of recurrent instability. Redislocation rates for shoulder instability after arthroscopic repair trend lower at 10% to 19% in most studies.2,4,19 Competitive collision athletes represent a high-risk cohort despite repair, having demonstrated higher rates of redislocation of 51% after arthroscopic labral repair in a recent study. 30 Additional studies have stressed the importance for surgical management of first-time dislocations, demonstrating reduced complication risk.7,21,31
For athletes recovering from arthroscopic Bankart repairs, a rehabilitation protocol that allows expedient return to play while minimizing recurrence is paramount. There has been considerable research regarding optimal return-to-play criteria after shoulder stabilization surgery. In a systematic review by Ciccotti et al, 6 of 58 studies assessing return-to-play criteria, 75.8% used time as the only metric, while 18.9% used strength, 13.8% used range of motion, and only 1 used proprioceptive control as a metric for return to play. Despite American Society of Shoulder and Elbow Therapists’ consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder, which integrates range of motion, strengthening, and shoulder girdle stabilization exercises, only one-third of protocols available online include a timeline outlining rehabilitation steps for return to sport. 11 An important aspect of return to play for competitive athletes is functional rehabilitation centered on restoring proprioceptive capacity and neuromuscular control of the joint after injury.8,14,17,18,20
Unlike the shoulder, the importance of both neuromuscular control and kinesiophobia have been well-studied in the knee, especially regarding anterior cruciate ligament (ACL) injury risk mitigation and recovery from surgical reconstruction.1,12,28 Kinesiophobia demonstrated by elevated Tampa Scale of Kinesiophobia–11 (TSK-11) scores and reinjury levels decrease with continued ACL reconstruction rehabilitation as far as 1 year postoperatively. 5 Patients reporting decreased quadriceps strength, lower self-reported function, and lack of confidence in remaining injury-free at 6 months were less likely to return to sport at 1 year. 17 Additional data demonstrate that patients reporting greater fear were less active, demonstrated lower single-leg hop performance and isometric quadriceps strength, and had an increased risk of suffering a second ACL injury within 24 months after return to sport. 25 This evidence in the ACL population emphasizes the importance of physical, psychosocial, and functional recovery of patients in successfully returning to sport.
Unlike ACL reconstruction, there are no validated return-to-sport measures that focus on neuromuscular control after arthroscopic Bankart repair. The purpose of this case series study is to determine readiness for return to play using functional and psychological testing in athletes after arthroscopic Bankart repair following a single instability event.
Methods
This retrospective study was conducted and approved by the local institutional review board. All participants were treated by a single sports medicine fellowship–trained surgeon with greater than 20 years’ experience. A total of 172 arthroscopic anterior Bankart repairs were performed from July 2015 to October 2017. Inclusion criteria applied to this group were as follows: participation in either high school or collegiate full-contact, semicontact, or overhead sport (ice hockey, rugby, football, lacrosse, or basketball), a single dislocation event, arthroscopic Bankart repair, and completion of the postoperative rehabilitation protocol. Exclusion criteria were as follows: <2 years of follow-up, prior dislocations, Beighton score >5, posterior instability, superior labral tear from anterior to posterior (SLAP) or rotator cuff tear, off-track Hill-Sachs lesion, or glenoid bone loss greater than 10% (calculated either on preoperative magnetic resonance imaging or intraoperatively). Patients were routinely evaluated in clinic at 2, 12, and 20 ± 2 weeks postoperatively, and had a scheduled clinic evaluation on completion of both functional assessments. The final postoperative follow-up examination was performed at 2 years.
All participants were treated by an athletic training staff and a single physical therapist group. The goals and milestones of the postoperative rehabilitation protocol are included in tables later in the text. Postoperatively, participants were maintained in a sling for initial immobilization, limiting rotation for 4 weeks. Supervised therapy began at week 1, starting on active and passive elbow range of motion and shoulder forward flexion range of motion. From weeks 5 to 12, progressive range of motion and muscle strengthening was initiated, with the goal of full/painless range of motion at 8 to 12 weeks postoperatively. Muscular strengthening was started at the following intervals: forward flexion at 6 weeks, external rotation at neutral at 8 weeks, and external rotation in the scapular plane at 8 to 12 weeks. Compared with the contralateral extremity, approximately 75% to 80% muscular strength was achieved at 8 to 12 weeks.
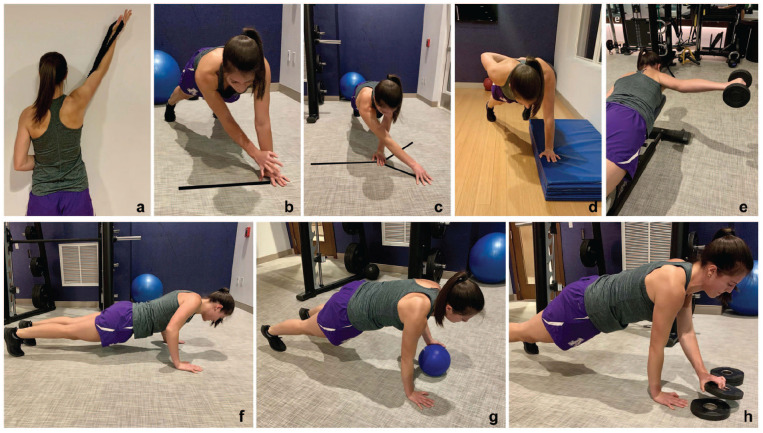
At 13 weeks postoperatively, light plyometric exercises were started. During week 16, functional rehabilitation was started, and patients were evaluated weekly starting at 20 weeks postoperatively. Key images noting the functional return-to-play assessment exercises are included in Figure 1. These exercises were selected to provide a comprehensive assessment of proprioception, strength, and stability of the core, scapula, and shoulder. Psychological assessments using the TSK-11 were completed week 16 and then weekly beginning at 20 weeks postoperatively. A score of 16 or less on the TSK-11 was considered a passing score for return-to-play consideration. 29 Last, sport-specific training was initiated at postoperative week 20. Participants were permitted to return to play once all physical and psychological tests were passed. All participants passed functional testing.
Figure 1.
Functional return-to-play assessments.* (a) Overhand band reach. (b) Closed kinetic chain extremity stability test. (c) Upper extremity Y balance. (d) One-arm hop test. (e) Posterior Shoulder Endurance Test. (f) Trunk stability push-up. (g) Long arm plank ball tap. (h) Plank weight stacking.
*See Supplemental Video available in the online version of this article.
The following parameters were recorded for all patients: time to pass functional testing, TSK-11, and time to return to sport. The postoperative level of play each athlete returned to was disclosed during clinical follow-up. We compared Western Ontario Shoulder Instability Index (WOSI) scores, Single Assessment Numeric Evaluation (SANE) scores, and the American Shoulder and Elbow Surgeons (ASES) Standardized Shoulder Assessment scores both preoperatively and at the 2-year postoperative follow-up visit.
Statistical analysis was performed using Stata/MP 13.1 for Mac (StataCorp). Descriptive statistics were used to summarize demographic and operative characteristics. Differences in preoperative and postoperative patient-reported outcome values were evaluated using paired t tests. Statistical significance was considered at P < 0.05 for all analyses.
Results
There were 73 participants meeting the inclusion criterion who were then retrospectively enrolled in the study. Eleven participants were lost to follow-up and 62 participants were followed through the completion of the study. The 11 participants were lost to follow-up because of graduation or relocation and thus subsequent inability to return for their 2-year follow-up assessment. Each participant returned to sport for at least 1 full season of competition and completed a minimum of 2-year follow-up.
Patient demographics are included in Table 1. There were 52 male and 10 female participants with an average age of 18.7 years. There were 52 nondominant arm shoulders and 10 dominant arm shoulders (48 left and 14 right). Average Instability Severity Index Score was 5.6 ± 0.6. Demographics of patients who sustained a redislocation event are listed in Table 2. The goals and milestones of the postoperative rehabilitation protocol are included in Tables 3 and 4, respectively.
Table 1.
Demographic characteristics
| Characteristic | % (n) |
|---|---|
| Age, y, mean ± SD (range) | 18.7 ± 2.0 (16-24) |
| Gender (N = 62) | |
| Male | 83.9 (52) |
| Female | 16.1 (10) |
| Primary sport | |
| Football | 38.7 (24) |
| Hockey | 38.7 (24) |
| Lacrosse | 14.5 (9) |
| Basketball | 6.5 (4) |
| Rugby | 1.6 (1) |
| Laterality | |
| Left | 77.4 (48) |
| Right | 22.6 (14) |
| Hand dominance | |
| Nondominant | 83.9 (52) |
| Dominant | 16.1 (10) |
Table 2.
Demographic characteristics—redislocation
| Patient | Age, y | Gender | Primary Sport | Laterality | Hand Dominance |
|---|---|---|---|---|---|
| 1 | 16 | Male | Lacrosse | Left | Nondominant |
| 2 | 20 | Female | Rugby | Right | Dominant |
| 3 | 20 | Female | Basketball | Right | Dominant |
| 4 | 17 | Male | Hockey | Left | Nondominant |
Table 3.
Rehabilitation program goals
| Weeks 1 to 4 Immediate postoperative phase |
• Protect repair • Mitigate consequences of immobilization • Promote dynamic stability and proprioception • Reduce pain and inflammation • No stretching • No active external rotation, abduction, or extension |
| Weeks 5 to 12 Intermediate phase |
• Gradually restore full ROM • Preserve repair integrity • Restore muscular strength and balance • Enhance neuromuscular control |
| Weeks 13 to 21 Minimal protection phase |
• Maintain full ROM • Improve muscular control, strength, power, and endurance • Practice core stabilization and conditioning • Weekly functional testing begins week 16 • Weekly TSK-11 begins week 16 • Sport-specific training begins week 20 |
| Weeks 22 to 26 Advance to strengthening phase |
• Maintain full ROM • Improve strength, power, and endurance • Advance functional activities |
| Weeks 26 to 32 Return-to-sport phase |
• Enhance strength, power, and endurance • Pass all functional assessments • Maintain mobility |
ROM, range of motion; TSK-11, Tampa Scale of Kinesiophobia–11.
Table 4.
Functional return-to-play assessment requirements
| Test | Goal | Pass |
|---|---|---|
| a. Overhand band reach | Demonstrate functional rotator cuff activity throughout multiplanar range of motion while avoiding trapezius dominance, trunk lean, and pelvic tilt | Maintain stability |
| b. Closed kinetic chain extremity stability test (CKCUEST) | Measure speed, agility, and power | 21 touches (male), 23 touches (female), 15 seconds |
| c. Upper extremity Y balance | Using the operative arm as a stabilizer, test mobility and stability of the extremity and core; combines scapular stability and functional range of motion with core stabilization and thoracic rotation | 3 consecutive progressions |
| d. One-arm hop test | Focus on stable core, maximum assessment of strength, and neuromuscular coordination | 5 repetitions |
| e. Posterior Shoulder Endurance Test (PSET) | Assess posterior rotator cuff and deltoid strength | 85% of contralateral arm |
| f. Trunk stability push-up | Stabilize spine and hips in sagittal plane during upper body symmetrical motion | 3 repetitions with control |
| g. Long arm plank ball tap | Assess stability, proprioception, and endurance | 10 bidirectional taps with body control |
| h. Plank weight stacking | Using the operative arm as a stabilizer, assess both proprioception and stability of the core and scapula | 4 repetitions × 1 lb |
Each procedure was performed using 3 to 4 PEEK (polyether ether ketone) anchors with knotted suture constructs totaling between 5 and 7 sutures. All repairs began posterior to the 6 o’clock position. A total of 53 (85.5%) patients had a 3-anchor repair, while 9 (14.5%) patients required a 4-anchor repair.
The time to pass functional testing was 6.19 ± 0.65 months (range 5-9 months) and psychological testing was 5.15 ± 0.54 months (range 4.5-6 months). All athletes passed psychological testing before or at the same time as passing functional assessments (range of 0-2 months prior). Athletes returned to full competition at 6.50 ± 0.66 months (range 6-10 months). The delay in completion of functional testing and returning to full competition is likely because of timing of follow-up appointments for confirmation of completion of functional tests by the treating surgeon.
SANE scores improved from 44.3 ± 2.5 to 90.0 ± 2.5, ASES from 45.5 ± 3.4 to 89.3 ± 3.2, and WOSI from 1578.0 ± 60.9 to 178.9 ± 32.3 (Table 5). The redislocation rate was 6.5% (4 of 62) after a minimum of 2-year follow-up, with all athletes returning to their prior level of competition for at least 1 season, which was confirmed at their final 2-year follow-up visit.
Table 5.
Patient-reported outcome scores
| Preoperative | Postoperative | Δ | P a | |
|---|---|---|---|---|
| SANE | 44.3 ± 2.5 | 90.0 ± 2.5 | 45.7 ± 3.2 | <0.001 |
| WOSI | 1578.0 ± 60.9 | 178.9 ± 32.3 | −1399.1 ± 63.2 | <0.001 |
| ASES | 45.5 ± 3.4 | 89.3 ± 3.2 | 43.8 ± 4.0 | <0.001 |
ASES, American Shoulder and Elbow Surgeons standardized assessment; SANE = Single Assessment Numeric Evaluation; WOSI, Western Ontario Shoulder Instability Index.
P value calculated using paired t tests.
Discussion
Using a multidisciplinary approach addressing an athlete’s perceived kinesiophobia, with a quantitative assessment of range of motion, strength, and neuromuscular control, we demonstrated a redislocation rate 6.5%. This is lower than what is currently published for a historically difficult-to-treat patient population. Only after successful completion of a return-to-play functional testing protocol incorporating 8 functional assessments (Figure 1) and a psychological assessment of each athlete’s confidence level was an athlete allowed to return to competition. Although the athletes in this study returned to play at a similar time frame compared with the current standard, the clinical significance of the lower redislocation rate is notable. Based on our data, participants were psychologically ready for return to play earlier (5.15 ± 0.5 months) than functional readiness (6.19 ± 0.7 months). All athletes completed the psychological testing either prior to or at the same time as the physical assessments. This finding supports the need for functional tests paired with a psychological test, in scenarios where an athlete may feel confident, but not yet be physically ready for safe return to play. Our observed redislocation rate highlights the importance of feeling both psychologically and functionally ready for return to sport as suggested by prior studies.5,17,25
Young, competitive athletes, specifically those playing collision sports, are at higher risk for dislocation and the sequelae of instability without appropriate treatment. 10 The current literature shows that several factors influence management of shoulder dislocations in athletes, including physical examination, radiographic review for Hill-Sachs lesions, glenoid bone loss, sport of choice, time in season, and the athlete’s long-term goals. 3 We have found that many athletes attempt nonoperative management in-season and are able to return to play shortly thereafter. However, Dickens et al 9 showed that only 27% of those who were able to return with nonoperative management were able to successfully complete their season without recurrence of instability. These high rates of redislocation stress the importance of considering early surgical intervention to mitigate the development of additional risk factors arising from further recurrent instability events.
Even with the significant number of athletes who undergo arthroscopic anterior stabilization procedures, there is a paucity in the literature of objective findings to help assess athletes returning to sport. 6 Unlike ACL reconstruction, there is no consensus on a return-to-play protocol that focuses on assessing kinesiophobia with a functional return-to-play criteria after arthroscopic Bankart repair. As athletes progress through their rehabilitation, having specific objective testing criteria that can gauge progression through the rehabilitation process can prove to be quite valuable. Classic teaching states that if athletes are confident and strong enough to compete and have completed 6 months of postoperative time, they are prepared to return to sports-specific activities. However, the associated redislocation rate upward of 19% to 51% in similar patient populations suggests that the current “objective tests” and 6-month postoperative time interval are not sufficient.16,27,30
We propose an objective set of tests that, once successfully completed, will enable an athlete to return to sport with mitigated redislocation risk. Although other factors such as age, gender, anterior instability, and repair technique affect redislocation rates, we believe that our program allows the athlete to feel both physically and psychologically strong enough to return to play and avoid recurrence.15,23,24 This also gives the surgeon additional objective data to confidently support an athlete’s return to play at one’s preoperative activity level.
There are several limitations to our study. First, this was a retrospective case series study without a defined control arm. Selection bias may affect the results, as all participants had glenoid bone loss <10%, which is lower than the typical 25% loss that warrants surgical repair. A smaller amount of bone loss and first-time dislocations are 2 factors associated with lower redislocation rates. All repairs were performed by a single experienced surgeon with minimal variation in technique, which may contribute to the observed lower recurrence rate in addition to the described rehabilitation protocol. Future studies may include multiple surgeons using this rehabilitation protocol to eliminate this limitation. Next, given the physically demanding rehabilitation protocol used, it may be unrealistic for athletes without access to an athletic training staff or specific weights, bands, and medicine balls to complete the protocol. We also recognize that not all athletes may be able to complete these tests because of baseline weakness unrelated to surgical repair. In this case, using the contralateral arm as a benchmark is important.
Conclusion
Return to sport after surgical intervention for anterior shoulder instability is possible at a high rate with proper surgical considerations and a judicious postoperative rehabilitation plan. The goals of postoperative rehabilitation for shoulder instability include the return of painless range of motion and strength, restoration of stability, and reinstated psychologic confidence in their shoulder. A key feature of the rehabilitation process is the functional restoration of proprioceptive feedback, which is critical for an athlete’s ability to return to sport and the confidence to return successfully. The current dogma of using time and strength for returning athletes to play after arthroscopic shoulder stabilization has led to less-than-ideal redislocation rates. Using functional rehabilitation and psychological evaluation gives providers objective data to confidently return athletes to sport. Future research will examine whether patients after this rehabilitation protocol return to sport sooner than their counterparts.
Supplementary Material
Acknowledgments
The authors to thank Ankur Narain, MD, for assistance with statistical analysis, and Jack Mazeika, James Duquette, and Anthony Fucillo, BA, for video contributions, audiovisual assistance, and technical support.
Footnotes
The following author declared potential conflicts of interest: B.D.B. reports personal fees from Depuy Synthes Mitek and Arthrex, outside the submitted work.
References
- 1. Abrams GD, Harris JD, Gupta AK, et al. Functional performance testing after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2014;2:2325967113518305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589-594. [DOI] [PubMed] [Google Scholar]
- 3. Balg F, Boileau P. The instability severity index score. J Bone Joint Surg Br. 2007;89-B:1470-1477. [DOI] [PubMed] [Google Scholar]
- 4. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576-580. [DOI] [PubMed] [Google Scholar]
- 5. Chmielewski TL, Jones D, Day T, Tillman SM, Lentz TA, George SZ. The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther. 2008;38:746-753. [DOI] [PubMed] [Google Scholar]
- 6. Ciccotti MC, Syed U, Hoffman R, Abboud JA, Ciccotti MG, Freedman KB. Return to play criteria following surgical stabilization for traumatic anterior shoulder instability: a systematic review. Arthroscopy. 2018;34:903-913. [DOI] [PubMed] [Google Scholar]
- 7. De Carli A, Vadalà AP, Lanzetti R, et al. Early surgical treatment of first-time anterior glenohumeral dislocation in a young, active population is superior to conservative management at long-term follow-up. Int Orthop. 2019;43:2799-2805. [DOI] [PubMed] [Google Scholar]
- 8. DeFroda SF, Mehta N, Owens BD. Physical therapy protocols for arthroscopic bankart repair. Sports Health. 2018;10:250-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability. Am J Sports Med. 2014;42:2842-2850. [DOI] [PubMed] [Google Scholar]
- 10. Donohue MA, Owens BD, Dickens JF. Return to play following anterior shoulder dislocation and stabilization surgery. Clin Sports Med. 2016;35:545-561. [DOI] [PubMed] [Google Scholar]
- 11. Gaunt BW, Shaffer MA, Sauers EL, et al. The American Society of Shoulder and Elbow Therapists’ consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther. 2010;40:155-168. [DOI] [PubMed] [Google Scholar]
- 12. Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141-150. [DOI] [PubMed] [Google Scholar]
- 13. Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. J Bone Joint Surg Am. 2008;90:945-952. [DOI] [PubMed] [Google Scholar]
- 14. Kibler WB, McMullen J, Uhl T. Shoulder rehabilitation strategies, guidelines, and practice. Orthop Clin North Am. 2001;32:527-538. [DOI] [PubMed] [Google Scholar]
- 15. Kraeutler MJ, Mccarty EC, Belk JW, et al. Descriptive epidemiology of the MOON Shoulder Instability Cohort. Am J Sports Med. 2018;46:1064-1069. [DOI] [PubMed] [Google Scholar]
- 16. Kramer J, Gajudo G, Pandya NK. Risk of recurrent instability after arthroscopic stabilization for shoulder instability in adolescent patients. Orthop J Sports Med. 2019;7:2325967119868995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lentz TA, Zeppieri G, Jr, George SZ, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345-353. [DOI] [PubMed] [Google Scholar]
- 18. Lephart SM, Henry TJ. Functional rehabilitation for the upper and lower extremity. Orthop Clin North Am. 1995;26:579-592. [PubMed] [Google Scholar]
- 19. Mazzocca AD, Brown FM, Jr, Carreira DS, Hayden J, Romeo AA. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52-60. [DOI] [PubMed] [Google Scholar]
- 20. Myers JB, Lephart SM. The role of the sensorimotor system in the athletic shoulder. J Athl Train. 2000;35:351-363. [PMC free article] [PubMed] [Google Scholar]
- 21. Nakagawa S, Hirose T, Uchida R, Tanaka M, Mae T. Postoperative recurrence of instability after arthroscopic Bankart repair for shoulders with primary instability compared with recurrent instability: influence of bipolar bone defect size. Am J Sports Med. 2019;48:48-55. [DOI] [PubMed] [Google Scholar]
- 22. Olds M, Ellis R, Donaldson K, Parmar P, Kersten P. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med. 2015;49:913-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37:1750-1754. [DOI] [PubMed] [Google Scholar]
- 24. Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91:791-796. [DOI] [PubMed] [Google Scholar]
- 25. Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10:228-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88:2326-2336. [DOI] [PubMed] [Google Scholar]
- 27. Shibata H, Gotoh M, Mitsui Y, et al. Risk factors for shoulder re-dislocation after arthroscopic Bankart repair. J Orthop Surg Res. 2014;9:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thomeé R, Kaplan Y, Kvist J, et al. Muscle strength and hop performance criteria prior to return to sports after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1798-1805. [DOI] [PubMed] [Google Scholar]
- 29. Tkachuk GA, Harris CA. Psychometric properties of the Tampa Scale for Kinesiophobia–11 (TSK-11). J Pain. 2012;13:970-977. [DOI] [PubMed] [Google Scholar]
- 30. Torrance E, Clarke CJ, Monga P, Funk L, Walton MJ. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. 2018;46:2969-2974. [DOI] [PubMed] [Google Scholar]
- 31. Yapp LZ, Nicholson JA, Robinson CM. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: long-term follow-up of a randomized, double-blinded trial. J Bone Joint Surg. 2020;102:460-467. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.