Abstract
Background:
Whole-muscle electromyography (EMG) data of the rotator cuff support external rotation (ER) strengthening exercises during shoulder rehabilitation. However, distinct neuroanatomic regions in the supraspinatus and infraspinatus exist. Differences in regional muscle activity occur during rehabilitation exercises, but little information is available for ER exertions.
Hypothesis:
Regional infraspinatus and supraspinatus muscle activity during standing ER exertions will differ with posture and intensity.
Study Design:
Descriptive laboratory study.
Level of Evidence:
Level 5.
Methods:
Twenty healthy individuals (12 men, 8 women) participated. Fine wire electrodes were inserted into 2 supraspinatus and 3 infraspinatus muscle regions. EMG data were recorded during standing isometric ER exertions at 2 intensities (maximal, submaximal) and in 7 postures defined by the angle (0°, 30°, 90°) and plane (abduction, scaption, flexion) of arm elevation. EMG data were normalized to maximum voluntary isometric contraction (% MVIC) to examine the influences of posture, intensity and their interaction on muscle activity.
Results:
Superior infraspinatus activity was higher in 0° of elevation (50.9% ± 5.7% MVIC) versus 30° of flexion (37.4% ± 3.9% MVIC) at maximal intensity. Inferior infraspinatus activity was higher in 90° of scaption (max = 59.8% ± 2.8% MVIC, submax = 29.4% ± 1.9% MVIC) versus 0° of elevation (max = 42.3% ± 4.5% MVIC, submax = 22.4% ± 2.8% MVIC) (P = 0.02, P = 0.05, respectively). Anterior supraspinatus activity was highest in 90° of adbuction (max = 61.6% ± 3.1% MVIC; submax = 39.1% ± 3.8% MVIC) and lowest in 30° of flexion (max = 29.0% ± 3.4% MVIC, submax = 15.6% ± 1.7% MVIC) and 90° of flexion (max = 34.6% ± 2.4% MVIC, submax = 14.8% ± 1.9% MVIC). Posterior suprasptinatus activity was lowest in 0° of elevation (34.2% ± 3.0% MVIC), 30° of flexion (33.0% ± 3.6% MVIC) and highest in 90° of abduction (56.2% ± 4.1% MVIC) and 90° of scaption (46.7% ± 2.8% MVIC) (all Ps < 0.04).
Conclusion:
Regional infraspinatus and supraspinatus muscle activity differed with posture and intensity. Superior and middle infraspinatus muscle activities were similar across postures, but inferior infraspinatus activity was highest in 90° of arm elevation. Anterior and posterior supraspinatus activities were higher in the abduction and scaption planes, especially at 90° of elevation, as compared with the flexion plane.
Clinical Relevance:
In shoulder rehabilitation of supraspinatus tendon injuries, ER exercises in the flexion plane challenge the whole infraspinatus muscle and require lower supraspinatus muscle activity.
Keywords: electromyography, rotator cuff, rehabilitation
Rotator cuff pathology limits functional abilities and quality of life, but approaches to mitigating its consequences are equivocal. Rehabilitation exercise programs are an integral part of the treatment plan3,18 and are designed to build muscular strength while minimizing excessive tendon overloading. The appropriate level of muscular challenge that achieves a balance between strength and excessive tendon load 18 can be difficult to quantify.
Rotator cuff electromyography (EMG) provides muscular demand information during rehabilitation exercises, but existing data are incomplete. A progressive rotator cuff rehabilitation protocol 11 was recently developed based on a systematic review of EMG data measured during rehabilitation exercises.8,27,28,30,31,34 However, most available rotator cuff EMG data have used single electrode pairs to represent entire anatomic muscles. Distinct anatomic, artchitectural, and innervational regions exist in the infraspinatus (superior, middle, inferior)7,14,24 and supraspinatus (anterior, posterior) muscles.17,21,22 Recent regional EMG studies verified differences during rehabilitation exercises, supporting varied regional function.4,9,10,19
Rotator cuff strengthening dominates rehabilitation programs, but currently is not regionally specific. Resisted external rotation (ER) exercises are commonly included in rotator cuff rehabilitation and tend to recruit the entire cuff as indicated by EMG, with slight postural variations.11,13,15,31,33 However, regional muscle activation during ER excercises performed in different postures and at different intensities is unknown. The aim of this research was to quantify regional muscular activations of the infraspinatus and supraspinatus across postures and intensities, to refine rehabilitation exercise prescription.
Methods
Twenty right-handed, healthy individuals (12 men, 8 women; mean age 22.1 ± 2.3 years; mean body mass index 23.8 ± 3.4 kg/m2), free of history of injury, surgery, or neuromuscular disease in the right upper limb, participated. All participants provided informed consent and the study was approved by the university office of research ethics.
Electrodes were inserted into the 5 muscle regions following established procedures.4,27 Insertion was achived using either 30 mm (27 gauge) or 50 mm (25 gauge) manufactured needles (Chalgren Enterprises, Inc) or a 75 mm (23 gauge) custom-made needle (Quinke Point, Kimberly Clark Spinal QP Needle). A reference electrode was placed on the right clavicle. EMG data were collected using a Noraxon telemyo 2400 G2 system (Noraxon). Raw EMG data were bandpass-filtered (10-1000 Hz), differentially amplified (common-mode rejection ratio >100 dB at 60 Hz, input impedance 100 Mohm), sampled at 3000 Hz, and converted to a digital signal (16-bit A/D card, maximum ±5 V range).
Participants performed a maximum voluntary isometric contraction (MVIC) protocol, as described in Alenabi et al. 5 Each exertion was 5 seconds in duration and separated by 1 minute of rest. Next, participants performed standing isometric ER exertions in 7 postures (Figure 1), verified by a goniometer, at 2 intensity levels. A moveable cuff on the forearm allowed 90° of elbow flexion during all exertions. The cuff was attached to a triaxial force transducer (“force cube”; MC3A, AMTI) mounted on a robotic arm that was adjusted to participants’ individual anthropometrics (height, arm length) (Figure 1) to ensure exerted force was perpendicular to the transducer midpoint. Exertions were completed in a randomized order with 2 repititions in each posture. Participants gradually produced their maximum voluntary force (MVF) for 2 seconds and then gradually returned to rest. Force data were sampled at 1500 Hz (1000× gain) and converted to a digital signal (12-bit A/D card) using a customized LabView program (National Instruments). After performing the MVF exertions, participants performed submaximal (50% MVF) efforts in the same postures. Force signals (calibrated from volts to % MVF) were provided as real-time visual feedback to help participants maintain submaximal force levels at 50% MVF (±10% MVF) during the middle 3 seconds of the exertion. Practice achieving submaximal forces using visual feedback preceded the experimental trials. All exertions were separated by 2 minutes of rest.
Figure 1.
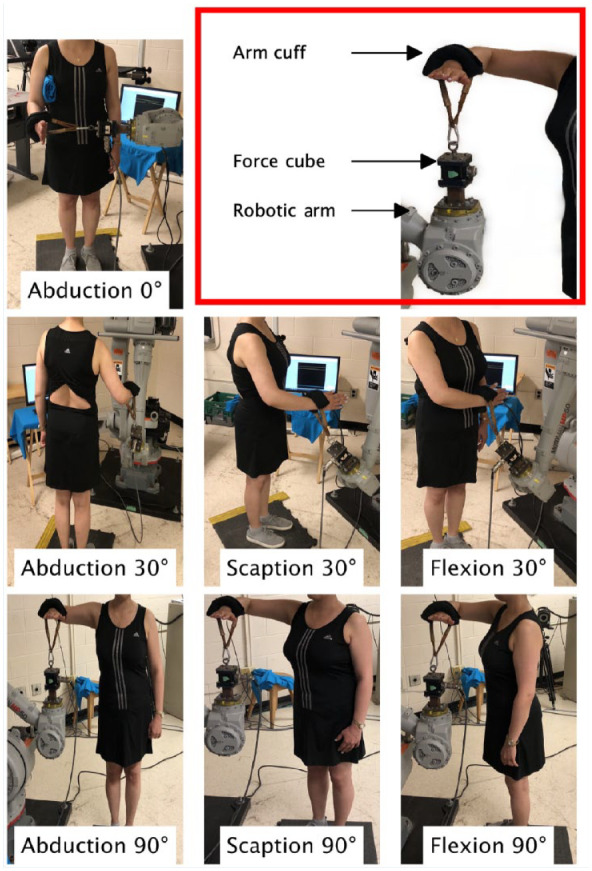
The postures used in this study, identified by the humeral plane of elevation (abduction, scaption, and flexion) and elevation angles (0°, 30°, and 90°). The set up used to measure external rotation force is shown in the red box. A cuff, which was attached to a triaxial force transducer (force cube), was positioned on participants’ forearm. The force cube was mounted on an adjustable robotic arm that was positioned based on participants’ anthropometrics (ie, arm length, height).
Raw force data (volts) were smoothed using a 0.5-second moving average. Then, a moving standard deviation (1 second) was calculated from 0.5 to 4.5 seconds of each 5-second trial. The 1-second interval with the smallest moving standard deviation was identified as that with the least force variability and EMG data during this 1 second was analyzed.
Band-passed EMG signals were full wave rectified and linear enveloped using a low pass Butterworth filter (second order, fc = 2Hz). A maximum value from each muscle region was extracted from each MVIC exertion, and the maximum of these was defined as the global muscle-specific maximum activity. A mean of the filtered EMG data from each muscle region was calculated during the 1-second windows identified above. These means were normalized to the global muscle-specific maximum activity (% MVIC), and then categorized as low (0%-15% MVIC), low to moderate (16%-20% MVIC), moderate (21%-40% MVIC), high (41%-61% MVIC), and very high (>61% MVIC). 11
Two-way repeated-measures analyses of variance examined each muscle region (5 total), to detect differences in normalized muscle activity (% MVIC) between the postures (7) and intensities (2). The assumption of sphericity was tested using Mauchly’s test of sphericity, and when violated, a Greenhouse-Geisser correction was used. Tukey honestly significant difference post hoc tests were performed on significant main effects and interactions (P < 0.05). Posture and intensity were treated as categorical variables.
Results
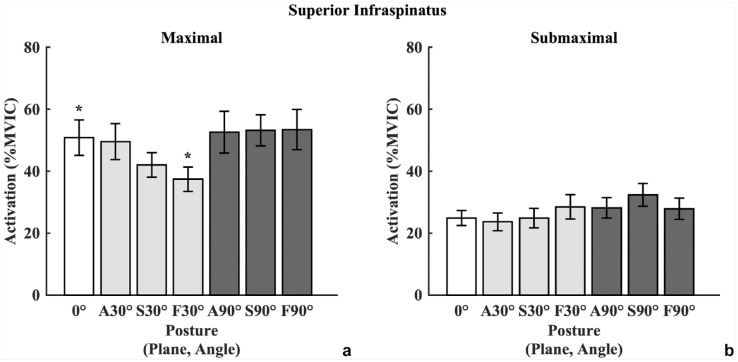
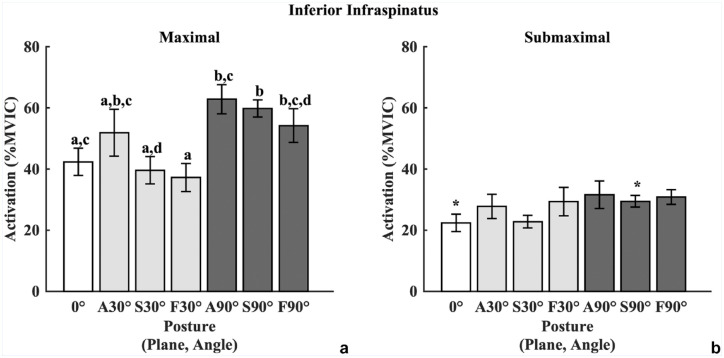
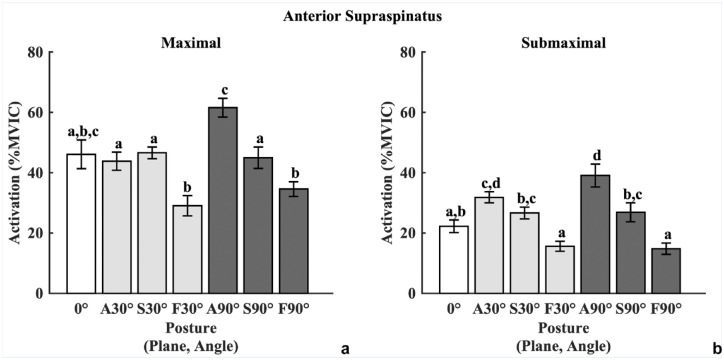
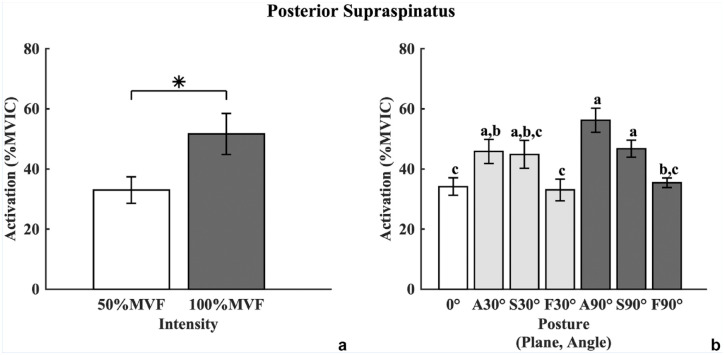
All regions were influenced by either intensity, posture, or an interaction of both (full data set; Table 1). Superior infraspinatus muscle activation was influenced by an interaction between posture and intensity (P < 0.001; Figure 2). Middle infraspinatus muscle activation was only influenced by exertion intensity. Inferior infraspinatus muscle activation was influenced by an interaction between posture and intensity (P < 0.01; Figure 3). Anterior supraspinatus muscle activation was influenced by an interaction between posture and intensity (P < 0.01; Figure 4), while posterior supraspinatus was influenced by main effects of posture and intensity (both Ps <0.01; Figure 5).
Table 1.
The mean and 95% confidence intervals of the mean (95%CI) activation of the infraspinatus and supraspinatus muscle regions at each intensity and posture combination. The range of activation categories, based on those recommended by Edwards et. al, 2017 are included above the mean. The shading reflects the range of activation categories encompassed by the 95% CI of the mean at each posture. For example, the lightest grey shade indicates the 95% CI of the mean activity in that posture fell within the Low to Moderate – Moderate categories whereas the darkest shade indicates the 95% CI of the mean activity in that posture fell within the High – Very High categories. Posture is described by the plane of elevation (Abd = Abduction, Scap = Scaption, Flex = Flexion) and angle of elevation within the plane. Note that the 0° elevation posture indicates the arm is at the participants side and thus not described by a plane of elevation
| Infraspinatus | Supraspinatus | |||||
|---|---|---|---|---|---|---|
| Load | Posture | Superior | Middle | Inferior | Anterior | Posterior |
| 50 | 0° | Low to Moderate - Moderate24.9[19.7, 30.1] | Low to Moderate - Moderate26.9[20.4, 33.3] | Low to Moderate - Moderate22.4[16.1, 28.7] | Low to Moderate - Moderate22.2[17.8, 26.7] | Low to Moderate - Moderate26.5[20.4, 32.5] |
| Abd 30° | Low to moderate - Moderate23.6[17.5, 29.8] | Low to Moderate - Moderate27.7[19.9, 35.4] | Low to Moderate - Moderate27.8[19, 36.6] | Moderate31.9[28, 35.7] | Moderate - High37.8[29.6, 46.0] | |
| Scap 30° | Low to Moderate - Moderate24.8[18.1, 31.6] | Low to Moderate - Moderate28.6[20.3, 36.9] | Low to Moderate - Moderate22.8[18.2, 27.3] | Moderate26.7[22.6, 30.8] | Moderate - High35.3[25.2, 45.4] | |
| Flex 30° | Low to Moderate - Moderate28.5[20, 37] | Low to Moderate - Moderate27.2[19.7, 34.7] | Low to Moderate - Moderate29.4[19, 39.8] | Low - Low to Moderate15.6[12.1, 19.1] | Low to Moderate - Moderate24.9[18.3, 31.5] | |
| Abd 90° | Moderate28.2[21.1, 35.3] | Low to Moderate - Moderate27.8[20.3, 35.3] | Moderate - High31.6[21.6, 41.7] | Moderate - High39.1[31.1, 47.1] | Moderate - High44.4[36.9, 51.9] | |
| Scap 90° | Moderate - High32.4[24.4, 40.3] | Moderate31.5[23.9, 39] | Moderate29.4[25.2, 33.7] | Low to Moderate - Moderate26.9[20.2, 33.5] | Moderate - High38.6[31.3, 45.9] | |
| Flex 90° | Low to Moderate - Moderate27.9[20.4, 35.3] | Moderate28.6[23.7, 33.4] | Moderate30.9[25.5, 36.2] | Low - Low to Moderate14.8[10.9, 18.8] | Low to Moderate - Moderate23.6[19.9, 27.2] | |
| 100 | 0° | Moderate - Very High50.8[38.5, 63.2] | Moderate - High48.3[39.7, 56.9] | Moderate - High42.3[32.4, 52.3] | Moderate - High46.1[36, 56.2] | Moderate - High41.8[34.3, 49.4] |
| Abd 30° | Moderate - Very High49.5[37.0, 62.1] | Moderate - Very High56.2[40.9, 71.5] | Moderate - Very High51.9[34.8, 69] | Moderate - High43.8[37.5, 50.1] | High - Very High53.9[43.4, 64.3] | |
| Scap 30° | Moderate - High42[33.5, 50.6] | Moderate - Very High52.2[38.3, 66] | Moderate - High39.6[29.6, 49.5] | High46.6[42.5, 50.7] | High - Very High54.4[43.8, 65] | |
| Flex 30° | Moderate - High37.4[28.9, 46] | Moderate - High46.2[34.4, 57.9] | Moderate - High37.2[27.1, 47.4] | Moderate29[21.9, 36.1] | Moderate - High41.1[30.3, 52] | |
| Abd 90° | Moderate - Very High52.6[38.0, 67.1] | High - Very High53.3[45.3, 61.4] | High - Very High62.8[52.2, 73.5] | High - Very High61.6[55.0, 68.1] | High - Very High68[58, 78] | |
| Scap 90° | High - Very High53.2[42.4, 64] | High - Very High57.1[48.3, 65.9] | High - Very High59.8[53.6, 66.1] | Moderate - High45[37.4, 52.6] | High - Very High54.9[48.2, 61.6] | |
| Flex 90° | Moderate - Very High53.5[39.5, 67.4] | High - Very High54.4[42.9, 65.8] | High - Very High54.2[41.9, 66.5] | Moderate34.6[29.5, 39.7] | High47.3[41.2, 53.3] | |
Abd, abduction; Flex, flexion; Scap, scaption.
The range of activation categories from Edwards et al 11 are included above the mean. The shading reflects the range of activation categories encompassed by the 95% CI of the mean at each posture. For example, the lightest grey shade indicates the 95% CI of the mean activity in that posture fell within the Low to Moderate - Moderate categories whereas the darkest shade indicates the 95% CI of the mean activity in that posture fell within the High - Very High categories. Posture is described by the plane of elevation and angle of elevation within the plane. Note that the 0° elevation posture indicates the arm is at the participants side and thus not described by a plane of elevation.
Figure 2.
The mean (± standard error) superior infraspinatus muscle activity (% MVIC) at each intensity (maximal, submaximal) and posture. Color shading of the bars corresponds to the 3 elevation angles (0° white, 30° gray, and 90° dark gray). On the X-axis, the plane of elevation is represented as follows: A, abduction; S, scaption; F, flexion. Superior infraspinatus muscle activity at a maximal intensity was significantly higher in the 0° of elevation posture, as compared with the FLEX30° (F30°) posture (P = 0.03) as denoted by an asterisk. MVIC, maximum voluntary isometric contraction.
Figure 3.
The mean (± standard error) infraspinatus inferior muscle activity (% MVIC) at each intensity (maximal, submaximal) and posture. Color shading of the bars corresponds to the 3 elevation angles (0° white, 30° gray, and 90° dark gray). On the X-axis, the plane of elevation is represented as follows: A, abduction; S, scaption; F, flexion. At the maximal intensity, a lettering scheme is used to denote significantly different means (P < 0.05). Means with the different letters are significantly different than one another. At the submaximal level, infraspinatus inferior activity was significantly higher in the SCAP90° (S90°) posture, as compared with the 0° of elevation posture (P = 0.05) as denoted by an asterisk. MVIC, maximum voluntary isometric contraction.
Figure 4.
The mean (± standard error) anterior supraspinatus muscle activity (% MVIC) at each intensity (maximal, submaximal) and posture. Color shading of the bars corresponds to the 3 elevation angles (0° white, 30° gray, and 90° dark gray). On the X-axis, the plane of elevation is represented as follows: A, abduction; S, scaption; F, flexion. At both intensities, a lettering scheme is used to denote significantly different means (P < 0.05). Means with the different letters are significantly different than one another.
Figure 5.
The mean (± standard error) posterior supraspinatus muscle activity (% MVIC) at each intensity (A) and posture (B). Supraspinatus posterior activation was significantly higher at 100% MVF versus 50% MVF (P < 0.001). On the right graph, color shading of the bars corresponds to the 3 elevation angles (0° white, 30° gray, and 90° dark gray). On the X-axis, the plane of elevation is represented as follows: A, abduction; S, scaption; F, flexion. A lettering scheme is used to denote significantly different means (P < 0.05). Means with different letters are significantly different than one another. MVF; maximum voluntary force; MVIC, maximum voluntary isometric contraction.
Discussion
Exertion intensity and arm posture influenced regional activations of the infraspinatus and supraspinatus during standing ER exertions, with the lone exception of the middle infraspinatus where only intensity was influential. The data presented help confirm which exercises can recruit certain muscle regions.
Two guiding principles emerge for infraspinatus: the middle region is only sensitive to intensity, and the inferior and superior regions vary with arm elevation. Similar middle infraspinatus activity occurred during ER exertions performed in different postures at both intensities. Prior studies have also found middle infraspinatus activity is similar across arm postures during submaximal ER exertions,6,31 and this study shows this occurs during maximal ER exertions too. A relatively consistent rotational moment arm of the middle infraspinatus across elevation angles (0°-60°) may explain the postural insensitivity. 29 Thus, intensity is the most useful parameter to adjust when targeting middle infraspinatus activity levels. In contrast, the activity of the superior and inferior infraspinatus regions exhibited postural differences modulated by exertion intensity. At a maximal intensity, superior infraspinatus activity was only higher in 0° of elevation versus 30° of elevation in the flexion plane. The large pennation angle and muscle fiber orientation of the superior region make it a humeral abductor instead of an external rotator.16,25 Thus, during ER exertions, superior infraspinatus activity may primarily generate glenohumeral stability instead of an ER moment. Last, the inferior infraspinatus region contributes to ER of the humerus.16,25 The inferior infraspinatus ER moment arm decreases with increasing elevation angle, 2 and this aligns with observed higher activity at 90° versus 30° of elevation in the flexion and scaption planes during maximal exertions.
Postural sensitivity of supraspinatus regional activity is also likely related to muscle architecture, and reflects postural sensitivity of their moment generating capacities. ER exertions at either intensity in the flexion plane elicited lower anterior supraspinatus activities versus the other planes. In the flexion plane anterior supraspinatus has an internal rotation moment arm across elevations. 2 Thus, anterior supraspinatus activity during ER in the flexion plane results from a line of action that generates stabilizing humeral head compression in the glenoid fossa. 1 The muscle volume of the anterior supraspinatus region exceeds the posterior region, and thus it generates most of the longitudinal loading on the tendon.21,32 Therefore, in the rehabilitation of a torn supraspinatus tendon, it is important to limit anterior supraspinatus activity. In the flexion plane, the posterior supraspinatus ER moment arm is close to zero at low elevation and acts in internal rotation at higher elevation. 2 However, in the abduction plane, posterior supraspinatus creates an ER moment across elevation angles.2,26,29 Anatomic studies of supraspinatus tendon tears have identified structural changes in the posterior supraspinatus muscle region, such as a reduction in muscle fiber bundle length, that may contribute to functional impairments.20,23 The data from this study show that posterior supraspinatus activity ranges from moderate to very high levels (Table 1) and is challenged in many postures at both intensities.
This exploratory study assessed young individuals without upper extremity pathology. Differences in muscle activity due to pathology and age exist. 12 Thus, a next step is evaluating pathological and older shoulders. The current study focused on isometric standing ER exertions, commonly used in the early stages of rehabilitation. 11 Regional differences in infraspinatus and supraspinatus muscle activity have been observed in dynamic exertions 19 often used in mid to late rehabilitation stages. 11 Future research should include study of regional muscle activity during various dynamic or isotonic exertions.
Collectively, these results can help guide exercise prescription. In general, maximal ER efforts elicit moderate to very high activity in all regions of the supraspinatus and infraspinatus. Currently, ER at 0° of elevation is recommended to isolate and strengthen the infraspinatus muscle,15,33 but is predicated on data from the middle infraspinatus region. 24 Current data suggest that this approach ineffectively engages the inferior infraspinatus region. Standing ER exertions at higher elevations (ie, 90°) elicit moderate to high or very high levels of activity in all 3 infraspinatus muscle regions (Table 1). Eliciting posterior supraspinatus activity while limiting anterior supraspinatus activity can be achieved through performing flexion plane exercises. These new regionally specific findings can be applied in concert to beneficially and selectively recruit muscle regions in exercises.
Acknowledgments
The authors thank Ranjit Joseph for his assistance with data collection.
Footnotes
The following author declared potential conflicts of interest: C.R.D. reports grants from the Natural Sciences and Engineering Research Council (NSERC) of Canada during the conduct of the study.
References
- 1. Ackland DC, Pandy MG. Lines of action and stabilizing potential of the shoulder musculature. J Anat. 2009;215:184-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ackland DC, Pandy MG. Moment arms of the shoulder muscles during axial rotation. J Orthop Res. 2011;29:658-667. [DOI] [PubMed] [Google Scholar]
- 3. Agout C, Berhouet J, Spiry C, Bonnevialle N, Joudet T, Favard L. Functional outcomes after non-operative treatment of irreparable massive rotator cuff tears: prospective multicenter study in 68 patients. Orthop Traumatol Surg Res. 2018;104(8S):S189-S192. [DOI] [PubMed] [Google Scholar]
- 4. Alenabi T, Whittaker RL, Kim SY, Dickerson CR. Arm posture influences on regional supraspinatus and infraspinatus activation in isometric arm elevation efforts. J Electromyogr Kinesiol. 2019;44:108-116. [DOI] [PubMed] [Google Scholar]
- 5. Alenabi T, Whittaker RL, Kim SY, Dickerson CR. Maximal voluntary isometric contraction tests for normalizing electromyographic data from different regions of supraspinatus and infraspinatus muscles: identifying reliable combinations. J Electromyogr Kinesiol. 2018;41:19-26. [DOI] [PubMed] [Google Scholar]
- 6. Alizadehkhaiyat O, Hawkes DH, Kemp GJ, Frostick SP. Electromyographic analysis of the shoulder girdle musculature during external rotation exercises. Orthop J Sport Med. 2015;3:232596711561398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bacle G, Gregoire JM, Patat F, et al. Anatomy and relations of the infraspinatus and the teres minor muscles: a fresh cadaver dissection study. Surg Radiol Anat. 2017;39:119-126. [DOI] [PubMed] [Google Scholar]
- 8. Boettcher CE, Ginn KA, Cathers I. Which is the optimal exercise to strengthen supraspinatus? Med Sci Sports Exerc. 2009;41:1979-1983. [DOI] [PubMed] [Google Scholar]
- 9. Calver R, Alenabi T, Cudlip A, Dickerson CR, Mondal P, Kim SY. Regional activation of supraspinatus and infraspinatus sub-regions during dynamic tasks performed with free weights. J Electromyogr Kinesiol. Published online May 2019, doi: 10.1016/j.jelekin.2019.05.009 [DOI] [PubMed] [Google Scholar]
- 10. Cudlip AC, Kim SY, Dickerson CR. The ability of surface electromyography to represent supraspinatus anterior and posterior partition activity depends on elevation angle, hand load and plane of elevation. J Biomech. 2020;99:109526. [DOI] [PubMed] [Google Scholar]
- 11. Edwards PK, Ebert JR, Littlewood C, Ackland T, Wang A. A systematic review of electromyography studies in normal shoulders to inform postoperative rehabilitation following rotator cuff repair. J Orthop Sports Phys Ther. 2017;47:931-944. [DOI] [PubMed] [Google Scholar]
- 12. Ellsworth AA, Mullaney M, Tyler TF, McHugh M, Nicholas S. Electromyography of selected shoulder musculature during un-weighted and weighted pendulum exercises. N Am J Sports Phys Ther. 2006;1:73-79. [PMC free article] [PubMed] [Google Scholar]
- 13. Escamilla RF, Yamashiro K, Paulos L, Andrews JR. Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sport Med. 2009;39:663-685. [DOI] [PubMed] [Google Scholar]
- 14. Fabrizio PA, Clemente FR. Anatomical structure and nerve branching pattern of the human infraspinatus muscle. J Bodyw Mov Ther. 2014;18:228-232. [DOI] [PubMed] [Google Scholar]
- 15. Ganderton C, Pizzari T. A systematic literature review of the resistance exercises that promote maximal muscle activity of the rotator cuff in normal shoulders. Shoulder Elbow. 2013;5:120-135. [Google Scholar]
- 16. Hermenegildo J. Neuromuscular Partitioning of Supraspinatus and Infraspinatus [Unpublished master’s thesis]. University of Western Ontario; 2013.
- 17. Hermenegildo JA, Roberts SL, Kim SY. Innervation pattern of the suprascapular nerve within supraspinatus: a three-dimensional computer modeling study. Clin Anat. 2014;27:622-630. [DOI] [PubMed] [Google Scholar]
- 18. Huang T-S, Wang S-F, Lin J-J. Comparison of aggressive and traditional postoperative rehabilitation protocol after rotator cuff repair: a meta-analysis. J Novel Physiother. 2013;3:170. [Google Scholar]
- 19. Joseph R, Alenabi T, Lulic T, Dickerson CR. Activation of supraspinatus and infraspinatus partitions and periscapular musculature during rehabilitative elastic resistance exercises. Am J Phys Med Rehabil. 2019;98:407-415. [DOI] [PubMed] [Google Scholar]
- 20. Kim SY, Bleakney RR, Rindlisbacher T, Ravichandiran K, Rosser BWC, Boynton E. Musculotendinous architecture of pathological supraspinatus: a pilot in vivo ultrasonography study. Clin Anat. 2013;26:228-235. [DOI] [PubMed] [Google Scholar]
- 21. Kim SY, Boynton EL, Ravichandiran K, Fung LY, Bleakney R, Agur AM. Three-dimensional study of the musculotendinous architecture of supraspinatus and its functional correlations. Clin Anat. 2007;20:648-655. [DOI] [PubMed] [Google Scholar]
- 22. Kim SY, Ko JB, Dickerson CR, Collins DF. Electromyographic investigation of anterior and posterior regions of supraspinatus: a novel approach based on anatomical insights. Int Biomech. 2017;4:60-67. [Google Scholar]
- 23. Kim SY, Sachdeva R, Li Z, Lee D, Rosser BWC. Change in the pathologic supraspinatus: a three-dimensional model of fiber bundle architecture within anterior and posterior regions. Biomed Res Int. 2015;2015:564825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kim SY, Shakeri S, Dickerson CR, Alenabi T, Agur AMR. Verification of intramuscular electromyography electrode placement for neuromuscular partitions of infraspinatus. J Electromyogr Kinesiol. 2019;49:102354. [DOI] [PubMed] [Google Scholar]
- 25. Kuwahara Y, Yuri T, Fujii H, Kiyoshige Y. Functions of the subregions of the infraspinatus during lateral rotation. Surg Radiol Anat. 2017;39:1331-1336. [DOI] [PubMed] [Google Scholar]
- 26. Langenderfer JE, Patthanacharoenphon C, Carpenter JE, Hughes RE. Variability in isometric force and moment generating capacity of glenohumeral external rotator muscles. Clin Biomech (Bristol, Avon). 2006;21:701-709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. McCann P, Wootten ME, Kabada MP, Bigliani LU. A kinematic and EMG study of shoulder rehabilitation exercises. Clin Orthop Relat Res. 1993;288:179-188. [PubMed] [Google Scholar]
- 28. Myers JB, Pasquale MR, Laudner KG, Sell TC, Bradley JP, Lephart SM. On-the-field resistance-tubing exercised for throwers: an electromyographic analysis. J Athl Train. 2005;40:15-22. [PMC free article] [PubMed] [Google Scholar]
- 29. Otis JC, Jiang CC, Wickiewicz TL, Peterson MGE, Warren RF, Santner TJ. Changes in the moment arms of the rotator cuff and deltoid muscles with abduction and rotation. J Bone Joint Surg Am. 1994;76:667-676. [DOI] [PubMed] [Google Scholar]
- 30. Reinold MM, Macrina LC, Wilk KE, Fleisig GS. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J Athl Train. 2007;42:464-469. [PMC free article] [PubMed] [Google Scholar]
- 31. Reinold MM, Wilk KE, Fleisig GS, et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34:385-394. [DOI] [PubMed] [Google Scholar]
- 32. Roh MS, Wang VM, April EW, Pollock RG, Bigliani LU, Flatow EL. Anterior and posterior musculotendinous anatomy of the supraspinatus. J Shoulder Elbow Surg. 2000;9:436-440. [DOI] [PubMed] [Google Scholar]
- 33. Ryan G, Johnston H, Moreside J. Infraspinatus isolation during external rotation exercise at varying degrees of abduction. J Sport Rehabil. 2018;27:334-339. [DOI] [PubMed] [Google Scholar]
- 34. Wattanaprakornkul D, Cathers I, Halaki M, Ginn KA. The rotator cuff muscles have a direction specific recruitment pattern during shoulder flexion and extension exercises. J Sci Med Sport. 2011;14:376-382. [DOI] [PubMed] [Google Scholar]