Abstract
Background:
Female athletes are more predisposed to anterior cruciate ligament (ACL) injuries in comparison with their male counterparts. Research on ACL injury prevention strategies has demonstrated beneficial effects of plyometric exercises and feedback (FB) during the exercises. FB has resulted in reductions in vertical ground-reaction force and kinematic risk factors associated with ACL injury. Furthermore, taping (TP) may draw attention to the restriction created by the tape and serve as real-time biofeedback. The additional influence of FB and TP on plyometric exercises has not been determined.
Hypothesis:
FB and TP interventions delivered during plyometric exercises would result in positive changes in biomechanics and muscle onset in female athletes displaying dynamic knee valgus.
Design:
Controlled trial.
Setting:
University research laboratory.
Level of Evidence:
Level 2.
Methods:
Forty-eight active female athletes were divided into 3 groups: control (n = 16), plyometric training with FB (n = 16), and plyometric training with TP (n = 16). The 2 experimental groups performed a 6-week exercise program with either FB or TP. The control group continued its regular team schedule. Knee joint position sense, landing error scoring system (LESS), and the onset of muscle activation (the point at which muscle activation exceeds 3 standard deviations over baseline and continued above this threshold for at least 25 ms) before landing for the rectus femoris, vastus medialis, vastus lateralis, gluteus medius, semitendinosus, and biceps femoris during pre- and posttests were measured.
Results:
The vastus lateralis onset later in the TP group compared with the FB group (d [95% CI] = 0.64 [0.35-0.82], P = 0.01). Joint position sense accuracy improved only in the TP group (d = −0.63, P = 0.001). Both the FB (d = −0.85, P = 0.001), and TP (d = −0.82, P = 0.001) groups improved in LESS scores.
Conclusion:
The results of the present study showed that plyometric exercises with FB or TP affect LESS and the onset of the vastus lateralis in active uninjured women with dynamic knee valgus, while TP improves joint position sense. Therefore, when more accurate joint position sense is desired, practitioners may use plyometric with TP. If an improved LESS score is desired, plyometrics with either TP or FB are acceptable.
Clinical Relevance:
Our findings indicate that female athletes may benefit more when completing a plyometric training program with a TP versus an FB. Trainers, coaches, and clinicians should consider utilizing instructions that promote an external focus when implementing plyometric training programs with male athletes.
Keywords: electromyography, landing error scoring system, anterior cruciate ligament, joint position sense
An anterior cruciate ligament (ACL) injury is one of the most common knee injuries in athletics.6,43,55,65 It has been shown that dynamic knee valgus contributes to the noncontact ACL injury mechanism, particularly in female athletes.23,30,31 Dynamic knee valgus is defined as a combination of femoral adduction, femoral internal rotation, knee abduction, and tibial external rotation, a position that applies high loads on the knee.21,28 The landing error scoring system (LESS) is a good indicator of ACL injury risk, as it is clinically feasible and does not require specialized equipment. Studies have demonstrated that people who score low on the LESS are at higher risk of lower limb injury.49,50,60 The ability to evaluate athletes by performance tests can be very valuable to coaches and researchers as they assess the efficacy of prevention programs and target at-risk individuals. 39
Neuromuscular control plays an important role in supporting and stabilizing the knee joint by using sensory inputs from mechanical receptors and regulating the appropriate muscle responses. 66 Functional neuromuscular control, operationally defined as proper muscle timing and appropriate force generation, is essential for dynamic knee stiffness and protective stabilization. 3 Therefore, any factor that leads to a delay and inhibition of knee joint stabilizers will lead to knee instability and possibly ACL injury. 3 For instance, the magnitude and timing of muscle activation affects the joint’s ability to absorb and disperse forces and has been linked to injury. 56 Thus, effective neuromuscular control, resulting from proper muscle timing, is essential for dynamic knee control and protective stabilization. 35
Specific neuromuscular training programs such as plyometric training have been designed to improve feedforward and feedback (FB) muscle activity through the rapid application of force, thus challenging muscle and joint receptors. 25 These exercises are also reported to reduce ground-reaction force, reduce knee abduction and hip adduction during landing, 8 and improve LESS scores, 50 all aimed toward reduction of ligament injury incidence in female athletes.22,24-26,38,42,62 FB, both verbal and visual, is emerging as an important component of injury prevention programs and has resulted in reductions in vertical ground-reaction force and kinematic risk factors associated with ACL injury.16,52 Furthermore, continuous tactile FB to the skin around the knee can also provide cueing FB for specific changes in motion 52 such as dynamic knee valgus reduction. For instance, restricting skin stretch through taping (TP) may draw attention to the restriction created by the tape and serve as real-time biofeedback.19,52
While the LESS has been linked to ACL injury, 49 the LESS is performance evaluation test and previous study of Letafatkar et al 34 stated that timing of muscle onset is an important variable for preprogrammed motor strategies learned during the training. This observed neuromuscular adaptation during functional task could potentially reduce the risk for noncontact ACL injury. 34 Furthermore, Sheikhi et al 58 suggest that Kinesio TP application may improve knee abduction and sum of knee valgus and lateral trunk lean during single-leg drop landing, knee flexion during single-leg drop landing and single-leg vertical drop jump in individuals displaying risky single‑leg kinematics. Therefore, Kinesio TP application may marginally improve high‑risk landing kinematics in competitive male athletes, and a systematic review of Ericksen et al 15 concludes that combo FB generates the greatest reductions in peak vertical ground-reaction force during a jump-landing task. Therefore, by identifying women with dynamic knee valgus and conducting plyometric exercises with either FB or TP, LESS scores may be improved. The purpose of this study was to investigate the effect of plyometric exercises with valgus control FB or TP on LESS performance, joint position sense, and timing of muscle onset in lower limb muscles in women with dynamic knee valgus. We hypothesized that plyometric training with either FB or with TP would result in earlier muscle activation before landing, improved joint position sense, and improved LESS scores.
Methods
Participants
Fifty-one female athletes aged between 20 and 30 years with unilateral dynamic knee valgus from Tehran clubs in Tehran, Iran, volunteered to participate in this study. All participants completed regular physical activity for the past 3 years, defined as scoring 13 to 15 points on the Baecke Physical Activity Questionnaire (intraclass correlation coefficient [ICC] 0.65-0.89). 54 The number of participants was based on previous research and G*Power software (effect size [ES] = 0.40, alpha level = 0.05, power = 0.80, version 3.1.9.2).33,57 Inclusion criteria were peak knee valgus angle greater than 10° during a single-leg squat test 29 (Kinovea software version 0.8.15) and the prerequisites for plyometric training found in Table 1. Exclusion criteria included any lower extremity reconstructive surgery in the prior 2 years and any lower-extremity injury or unresolved musculoskeletal disorder that currently prohibited subjects from sports participation. This study was approved by the Kharazmi University’s Institutional Review Board (IR.KHU.REC.1398.017).
Table 1.
Plyometric prerequisites (inclusion criteria for participation in the plyometric exercises)
| Variables | Tests | Position |
|---|---|---|
| Static stability testing (30 s each position) | Single-leg stance | Eyes open |
| Eyes closed | ||
| Single-leg 25% squat | Eyes open | |
| Eyes closed | ||
| Single-leg 50% squat | Eyes open | |
| Eyes closed | ||
| Dynamic stability testing | Jump from box | No feel pain |
| Power testing (squat) | 60% Body weight | 5 Repetitions in 5 s |
Experimental Procedure
Participants were randomly divided into 3 groups: a control group (n = 16, height 165.1 ± 3.5 cm, mass 60.9 ± 5.2 kg), a plyometric training with the FB group (n = 16, height 165.7 ± 3.6 cm, mass 59.13 ± 6.7 kg), and a plyometric training with the TP group (n = 16, height 164.2 ± 3.4 cm, mass 60.5 ± 6.1 kg). Random assignment was performed by participants selecting a sealed envelope to determine group allocation. For baseline testing, subjects first performed a general warm-up program consisting of running slowly and dynamic stretching of lower extremities for 5 to 10 minutes,34,64 followed by joint position sense and LESS measures. Participants were then outfitted with electromyography (EMG) sensors before performing a single-leg jump-landing task.
Participants returned for the training program, which consisted of 2 sessions a week for 6 weeks. In the TP group, Mulligan TP was used during all exercises. They also received scripted verbal cueing at the beginning of each session, Subjects received additional verbal FB during each training session if they were not maintaining the desired modifications 67 and visual FB via a full-length mirror was used for the FB group.
After 6 weeks, posttest measurements were performed, and the results were statistically analyzed. Baseline and posttests were completed within 48 hours of initiating or completing the 6-week training program for the athletes in the FB and TP groups. Athletes in the control group also completed baseline and posttests over a similar period and continue with their normal activities but did not complete the plyometric training program.
Electromyographic Assessment
Data were collected by a portable wireless EMG system (Biometrics Ltd; Canada). The EMG onset data were collected from 6 muscles: rectus femoris (RF), vastus medialis (VM), vastus lateralis (VL), gluteus medius (GM), biceps femoris (BF), and semitendinosus (ST). Wireless surface electrodes were placed on the participant’s dominant leg, defined as the leg used to kick a ball for maximum distance. The skin at the electrode sites was shaved, exfoliated, and cleaned with 70% isopropyl alcohol before electrode application.36,52 Wireless surface electrodes were placed over the prepared skin in the direction of the muscle fibers according to the SENIAM (surface EMG for noninvasive assessment of muscles) method. The EMG electrode for the RF was placed on the midpoint of the muscle belly. For the VM, the electrode was placed at 80% of the distance from the anterior superior iliac spine to the joint space anterior to the anterior border of the medial collateral ligament. For the VL, the electrode was placed at two-thirds the distance from the anterior superior iliac spine to the lateral side of the patella. The EMG electrode for the GM was placed halfway between the iliac crest and the greater trochanter. For the BF, the electrode was placed halfway between the ischial tuberosity and the lateral epicondyle of the tibia; and finally, the EMG electrode for the ST was placed halfway between the ischial tuberosity and the medial epicondyle of the tibia. EMG data were sampled at 1000 Hz. 20
For processing, raw EMG signals recorded from the jump-landing task were converted and saved in ASCII format by Biometrics Data LITE version 10.12, and the data were exported to MATLAB software version R2017b for further analysis. All EMG data were rectified, bandpass filtered (10-350 Hz), and notch filtered (60 Hz at 1-Hz width) using a Butterworth filter (fourth-order, zero-phase lag). 34
The initial muscle activity was when the EMG signal exceeded 3 standard deviations over baseline and continued above this threshold for at least 25 ms. The software automatically calculates the starting point of the activity and then calculates the time interval from this point to the moment of foot contact with the ground (measured with a footswitch that is placed under the forefoot) during single-leg jump-landing task and reports the onset of activation as milliseconds before landing.10,26,34
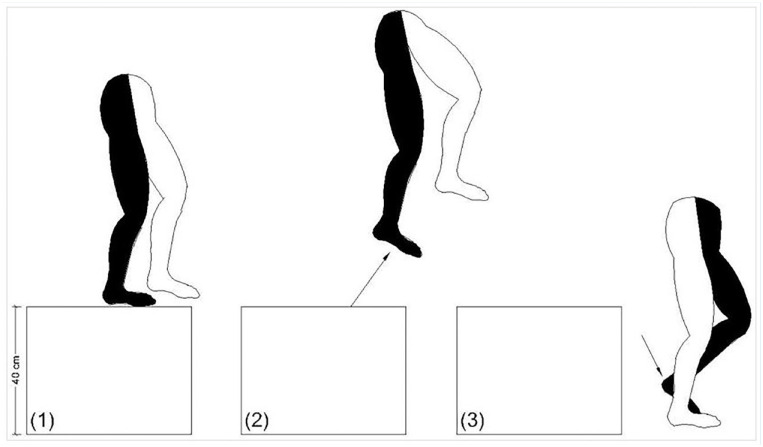
Single-Leg Jump-Landing Task
To record the moment of foot contact with the ground, the footswitch was attached to the subject’s forefoot, then the subject was asked to stand in a balanced position near the anterior edge of a 40-cm-high box with hands on the waist. They stood on the nondominant limb. Then, the subject was asked to jump off the box, land on the dominant foot and maintain her balance for 3 seconds. To jump correctly, the subject was asked to first contact the toe and then the heel. Three correct tasks were recorded for each subject and muscle EMG indices were calculated and their mean was analyzed (Figure 1F).9,34
Figure 1.
Single-leg jump-landing task. (1) Subject stands on a 40-cm box with test leg relaxed and nonweightbearing. (2) Subject propels from box with opposite leg. (3) Subject lands on test leg.
LESS Assessment
The LESS is a valid and reliable tool for identifying potentially high-risk movement patterns during a jump-landing task. Overall LESS score reliability, assessed by ICC, was excellent (ICC2,1 = 0.835, P < 0.001).46,50 The LESS score is a measurement of landing technique errors. A higher LESS score demonstrates poor technique. The LESS includes 17 scored items. Items 1 to 6 assess the condition of the lower limbs and trunk at the time of initial contact with the ground. Items 7 to 11 evaluate positioning errors of the feet. Items 12 to 15 evaluate lower limb and trunk movements between initial ground contact and the moment of maximum knee flexion. Last, items 16 and 17 assess the overall movement quality.
To complete the LESS, participants jumped from a 30-cm-high box to a distance of 50% of their height away from the box, down to a platform, and immediately rebounded for a maximal vertical jump. Participants performed 3 successful trials of the jump-landing task. If the participant did not reach the designated horizontal distance or did not appear to maximally perform the vertical countermovement jump, the trial was repeated.49,50
Two standard video cameras captured a frontal plane and sagittal plane view of each subject as she performed the testing procedures. Video cameras were 3 m away from the landing spot. Kinovea software (Kinovea; Canada) was used to examine the films at a very low speed. Each landing was scored by an experienced voter from the sum of all points 0 to 15. Items 16 and 17 were omitted during the statistical analysis because of their generality. The average of the 3 jumps was recorded as the final score for each participant.49,50
Joint Position Sense Assessment
A digital goniometric imaging technique, with validity and reliability (ICC) of 0.99 and 0.97, respectively, was used to assess knee joint position sense. 45 This evaluation was performed in a standing position. Joint position sense was measured for the dominant knee joint of each participant. Four reference markers were placed on each participant:
Upper thigh: junction of the proximal one-quarter and distal three-quarters of a line joining the apex of the greater trochanter to the midpoint of the lateral knee joint line.
Lower thigh: over the iliotibial tract, with its distal edge proximal to the level of the posterior crease of the 90° flexed knee.
Neck of fibula: anterior border of neck of the fibula.
Supralateral malleolus: lateral aspect of the shaft of fibula proximal to the lateral malleolus.
The subject was asked to place her hands on a chair back for stability and her dominant foot flat on the floor. With her eyes closed, the participant was asked to move her body weight to the evaluated leg, and progress to 45° of knee flexion angle, which was the target angle (a goniometer was used to determine the 45° target angle and participant was told when she had reached 45°), hold for 5 seconds, and then return the knee to 0°.
In the next step, the subject was asked to return to the previous angle (with no FB regarding accuracy), hold for 3 seconds, and then return the knee to 0°. Each subject repeated this procedure 3 times. The knee was photographed each time by cameras placed at a standard distance and height from the participant (Figure 2F). Digital imaging was used to assess the amount of error. After transferring the images to the computer using Kinovea software, the numerical value of the angle was calculated by the software.2,61
Figure 2.

Joint position testing.
Plyometric Training With FT and TP
For training groups, the modified protocol of plyometric exercises of Chimera et al 11 was used. The exercises were completed twice a week for 6 weeks, with 1-minute rest between all sets and exercises. The exercises included wall touches, lateral jumps, jump squats, lateral cone jumps, and 180° squat jumps (Table 2).
Table 2.
Sample of plyometric training progression
| Week | Exercises a |
|---|---|
| 1 | Wall touch (2 × 10) Lateral jump (2 × 10) Jump squat (2 × 10) Lateral cone jump (2 × 10) |
| 2 | Wall touch (2 × 12) Lateral jump (2 × 12) Jump squat (2 × 12) Lateral cone jump (2 × 12) |
| 3 | Wall touch (2 × 15) Lateral jump (2 × 15) Jump squat (2 × 15) Lateral cone jump (2 × 15) |
| 4 | Wall touch (3 × 12) Lateral jump (3 × 12) Jump squat (3 × 12) Lateral cone jump (3 × 12) |
| 5 | Wall touch (3 × 10) Lateral jump (3 × 10) Jump squat (3 × 10) Lateral cone jump (3 × 10) 180° Squat jump (3 × 10) |
| 6 | Wall touch (3 × 12) Lateral jump (3 × 12) Jump squat (3 × 12) Lateral cone jump (3 × 12) 180° Squat jump (3 × 12) |
Resting 1 minute between sets and 1 minute between exercises.
For the FB group during plyometric training, visual FB was provided by a full-length mirror placed directly in front of the participants. They also received scripted verbal cueing at the beginning of each session, consisting of “keep your knees apart from each other,” “keep your kneecaps pointing straight ahead,” and “squeeze your buttocks.” Subjects received additional verbal FB during each training session if they were not maintaining the desired modifications. 68 For the TP group, Mulligan tape was performed before each training session, and the tape was used during training. Participants were required to stand with the selected knee positioned in 25° of flexion and hip in slight internal rotation. The tape was applied in a spiral fashion from the fibula neck, across the front of the tibia while applying an internal tibial torsion force. The tape then passed posterior, inferior to the medial knee joint line then centrally over the posterior aspect of the knee joint. The tape continued in this direction to finish at the lateral lower third of the thigh (Figure 3F).19,27 The exercises were bilateral to avoid causing asymmetries. One of the investigators monitored adherence.
Figure 3.
Taping technique.
Data Analysis
The Shapiro-Wilk test was used to determine data normality. One-way analysis of variance (ANOVA) was used to compare the group demographics and differences at baseline. Multivariate repeated-measures ANOVA was used to examine time and group interactions. In the event of significant interactions, Bonferroni post hoc test analysis was used to examine between-group changes. ES using partial eta squared (η2p) were calculated. ES were classified as small (0.01), moderate (0.06), and large (0.14). 13 The alpha level was set at P ≤ 0.05 for statistical significance. All data were analyzed in SPSS (IBM Corporation; Armonk, NY). 17
Results
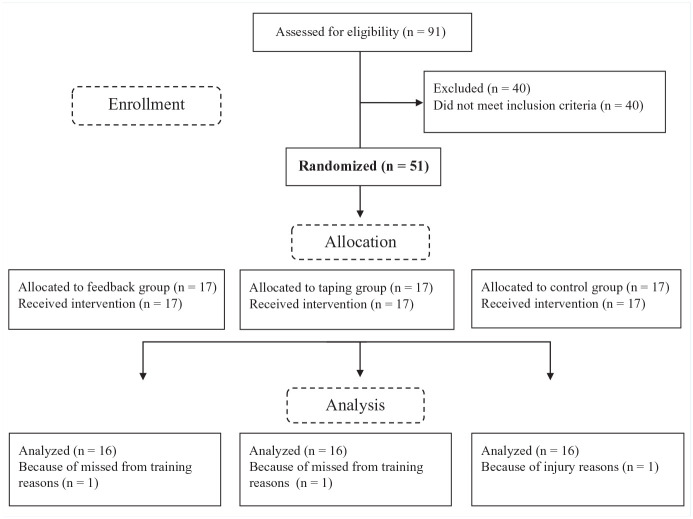
One participant from the TP group and 1 participant from the FB group were removed from the study because they missed more than 1 training session. One participant from the control group was removed because of injury and was unable to participate in the posttest (Figure 4F).
Figure 4.
Flow diagram of the study.
The Shapiro-Wilk test results indicated that all data were normally distributed (P ≥ 0.05). There were no significant differences between the groups in mass (P = 0.68), height (P = 0.51), age (P = 0.84), or exercise experience (P = 0.94) (Table 3).
Table 3.
Demographics of participants, reported as mean ± standard deviation
| Feedback | Taping | Control | P | |
|---|---|---|---|---|
| Age, y | 24.0 ± 3.9 | 24.9 ± 4.5 | 24.4 ± 4.0 | 0.84 |
| Weight, kg | 59.1 ± 6.7 | 60.5 ± 6.1 | 60.9 ± 5.2 | 0.68 |
| Height, cm | 165.7 ± 3.6 | 164.25 ± 3.4 | 165.1 ± 3.5 | 0.51 |
| Exercise experience, y | 6.3 ± 1.6 | 6.1 ± 1.7 | 6.4 ± 2.0 | 0.94 |
A significantly group-by-time interaction reported for VM onset (F = 91.48, P = 0.001, η2p = 0.806). From pre- to posttesting, VM onset occurred earlier in the FB group (d = 0.47, P = 0.001) and TP group (d = 0.56, P = 0.001), while no change was observed in the control group (d = −0.10, P = 0.12). For VL onset, there was a significant group-by-time interaction (F = 57.94, P = 0.001, η2p = 0.725). From pre- to posttesting, there were no changes in VL onset in the FB group (d = −0.01, P = 0.90) and control group (d = 0.05, P = 0.37), while a decrease in the TP group was observed (d = −0.67, P = 0.001). Differences between experimental groups for VL were significant, the time interval from the starting point to the moment of foot contact with the ground was decrease in the TP group, which mean the onset activation is closer to landing than pretest (d = 0.64, P = 0.01). For GM onset, there was a significant group-by-time interaction (F = 68.04, P = 0.001,η2p = 0.756). From pre- to posttesting, GM onset occurred earlier in the FB group (d = 0.29, P = 0.001) and TP group (d = 0.57, P = 0.001), while no change was observed in the control group (d = 0.01, P = 0.72). A significant group-by-time interaction was observed for ST onset (F = 74.09, P = 0.001, η2p = 0.771). From pre- to posttesting, ST onset occurred earlier in the FB group (d = 0.35, P = 0.001) and TP group (d = 0.59, P = 0.001), while no change was observed in the control group (d = −0.6,P = 0.39). For BF onset, there was a significant group-by-time interaction (F = 11.74, P = 0.001, η2p = 0.348). From pre- to posttesting, BF onset occurred earlier in the FB group (d = 0.29, P = 0.001) and TP group (d = 0.21, P = 0.001), while no change was observed in the control group (d = 0.04, P = 0.56). Full results are presented in Table 4.
Table 4.
Onset of muscle activations
| Within-Group | Between-Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Muscles | Groups | Pretest (Mean ± SD) | Posttest (Mean ± SD) | Change Relative to Pretest, a % | P | F (P) | P |
| Onset of activation, ms | RF | FB | 324.1 ± 35.6 | 248.4 ± 35.8 | 23.4 ↓ | 0.001 | F = 182.0 | 0.002
b
|
| TP | 322.4 ± 39.7 | 254.8 ± 38.9 | 21.0 ↓ | 0.001 | (P = 0.001) | 0.006 c | ||
| Control | 313.1 ± 59.5 | 312.4 ± 68.1 | 0.2 ↓ | 0.89 | ||||
| VM | FB | 208.8 ± 63.6 | 276.4 ± 62.1 | 32.4 ↑ | 0.001 | F = 82.4 | 0.001
b
|
|
| TP | 193.7 ± 57.7 | 269.4 ± 55.6 | 39.1 ↑ | 0.001 | (P = 0.001) | 0.002 c | ||
| Control | 206.4 ± 69.4 | 194.0 ± 59.9 | 6.0 ↓ | 0.12 | ||||
| VL | FB | 264.4 ± 50.1 | 262.9 ± 51.4 | 0.6 ↓ | 0.90 | F = 48.6 | 0.001 c | |
| TP | 267.4 ± 49.4 | 179.5 ± 48.5 | 32.9 ↓ | 0.001 | (P = 0.001) | |||
| Control | 260.4 ± 76.8 | 266.8 ± 60.7 | 2.5 ↑ | 0.37 | ||||
| GM | FB | 190.6 ± 47.2 | 219.3 ± 47.8 | 15.1 ↑ | 0.001 | F = 69.4 | 0.004 c | |
| TP | 185.9 ± 42.7 | 246.8 ± 45.0 | 32.8 ↑ | 0.001 | (P = 0.001) | |||
| Control | 188.3 ± 48.7 | 189.9 ± 49.4 | 0.8 ↑ | 0.72 | ||||
| ST | FB | 162.4 ± 42.9 | 194.4 ± 41.4 | 19.7 ↑ | 0.001 | F = 75.1 | 0.001 c | |
| TP | 164.5 ± 44.1 | 229.1 ± 45.2 | 39.3 ↑ | 0.001 | (P = 0.001) | |||
| Control | 160.2 ± 54.8 | 153.7 ± 58.7 | 4.1 ↓ | 0.32 | ||||
| BF | FB | 124.2 ± 57.7 | 159.2 ± 58.6 | 28.2 ↑ | 0.001 | F = 12.0 | ||
| TP | 114.4 ± 56.8 | 139.3 ± 59.7 | 21.8 ↑ | 0.001 | (P = 0.001) | |||
| Control | 117.4 ± 51.1 | 121.8 ± 62.3 | 3.7 ↑ | 0.56 | ||||
BF, biceps femoris; FB, feedback group; GM, gluteus medius; RF, rectus femoris; ST, semitendinosus; TP, taping group; VL, vastus lateralis; VM, vastus medialis.
Percent change (↓decrease, ↑ increase).
Significant between FB and control groups.
Significant between TP and control groups.
For joint position sense, there was a significant group-by-time interaction (F = 4.83, P = 0.13, η2p = 0.180). From pre- to posttesting, joint position sense accuracy improved in the TP group (d = −0.63, P = 0.001), but there were no changes in the FB group (d = −0.11, P = 0.55) or control group (d = −0.05,P = 0.61). Differences between experimental groups were significant, and the amount of error was low in the TP group (d = 0.45, P = 0.011) (Table 5).
Table 5.
Proprioception
| Within-Group | Between-Group | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Groups | Pretest (Mean ± SD) | Posttest (Mean ± SD) | Change Relative to Pretest, a % | P | F (P) | P |
| Joint position sense | FB | 4.6 ± 2.1 | 4.1 ± 2.4 | 10.9 ↓ | 0.55 | F = 4.1 (P = 0.02) | 0.55 |
| TP | 4.4 ± 1.2 | 2.0 ± 1.7 | 54.5 ↓ | 0.001 | 0.28 | ||
| Control | 3.4 ± 2.1 | 3.2 ± 1.7 | 5.9 ↓ | 0.61 | |||
FB, feedback group; TP, taping group.
Percent change (↓ decrease, ↑ increase).
There was a significant group-by-time interaction for the LESS (F = 140.92, P = 0.001, η2p = 0.865). From pre- to posttesting, both the FB (d = −0.85, P = 0.001) and TP (d = −0.82, P = 0.001) groups improved in LESS score, while no change was observed in the control group (d = −0.11, P = 0.36) (Table 6).
Table 6.
Landing error scoring system
| Within-Group | Between-Group | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Groups | Pretest (Mean ± SD) | Posttest (Mean ± SD) | Change Relative to Pretest, a % | P | F (P) | P |
| LESS | FB | 9.3 ± 1.8 | 4.6 ± 1.0 | 50.5 ↓ | 0.001 | F = 65.9 (P = 0.001) | 0.001 b |
| TP | 7.9 ± 1.5 | 3.6 ± 1.5 | 54.4 ↓ | 0.001 | 0.001 c | ||
| Control | 8.8 ± 2.1 | 8.4 ± 1.3 | 4.5 ↓ | 0.36 | |||
FB, feedback group; LESS, landing error scoring system; TP, taping group.
Percent change (↓ decrease, ↑ increase).
Significant between FB and control groups.
Significant between TP and control groups.
Discussion
The purpose of this study was to examine the effect of plyometric training with FB or TP on onset of lower limb muscle activation, knee joint position sense, and LESS scores in female athletes with dynamic knee valgus. The result showed that short-term training can make significant positive changes in the onset of muscle activation, joint position sense, and LESS.
Muscle Onset Time
During the pretest, it was generally observed that hamstring muscles have a more delayed onset than quadriceps muscles. After performing plyometric exercises with FB or TP, the hamstrings activated earlier. This suggests that the hamstrings can be trained to act as an ACL agonist during flight, helping to maintain the integrity of this ligament and surrounding structures in preparation for landing.4,14,17
After training, we saw that the VL muscle was activated later in TP group and VM and GM muscles activated earlier in both experimental groups. This may help prevent knee valgus during landing. During the pretests, earlier activation was observed in the RF, VL, and BF (lateral compartment) and delayed activation in ST and VM (medial compartment), which may have led to a slight bending of the knee during the descent, which can cause damage to the ACL.32,36,41,44,53 After the 6-week plyometric exercises, later activations (closer to landing) were observed in the RF, VL, and ST and earlier activation in the BF and VM in both experimental groups.
Also, gluteal activity limits knee valgus motion by controlling hip adduction and hip internal rotation.51,62 Hamstring activation, especially on the medial side, may also limit knee valgus motion by controlling frontal plane knee motion. Subjects who exhibit earlier and greater medial hamstring activation during both the preparatory and loading phases of landing display lesser knee valgus motion than those with lesser medial hamstring activity. 62 Also, since proper timing of knee flexor muscle activation is a basic requirement for knee flexion, proper hamstring muscle activation timing is a benefit in the performance of a high-risk landing. 32 It appears that earlier hamstring action at low flexion angles leads to proper stabilization of the knee joint and proper support of knee structures. 40 Therefore, it appears that earlier hamstring activity resulting from 6 weeks of plyometric exercises with FB or TP is a beneficial adaptation for proper knee loading.
Joint Position Sense
A comparison of pre- and posttest joint position sense errors of the 3 groups showed increasing knee joint position sense accuracy in the TP group at 45° (10.9% decrease in FB group vs 54.5% decrease in TP group).
The calculated minimal detectable change (MDC) for the joint position sense is 2.72°. 37 In the current data, the change from pre- to posttest exceeded the MDC for the TP group in 12 of 16 participants, and for 4 of 16 FB group participants.
Our findings are consistent with previous studies that have highlighted the advantages of training of joint position sense12,47,59 and seem to support the premise that the effectiveness of plyometric training for ACL injury prevention could be enhanced by providing FB. The evidence also demonstrates that participants with poorer joint position sense derive the most benefit from intervention.5,7
Unfortunately, we are unable to determine why athletes in the FB group did not exhibit improvements in knee joint position sense because we did not examine exercise technique, 3-dimensional kinematics of hip, and knee moments, and so on during training.
However, it is possible that athletes in the FB group performed exercises with suboptimal technique, which resulted in less hip muscle recruitment, force production, and so forth, and limited training-related strength gains.
TP can improve proprioception through tactile stimulation; as some studies have suggested, skin stimulation is effective for betterment of position sense and movement. 8 Applying an elastic bandage or tape can provide additional proprioceptive and kinesthetic information by stimulating cutaneous receptors and improve proprioception. 63
Eccentric loading like plyometrics increase training muscle tone and stiffness via an increase in muscle spindle activation and sensitivity that can increase proprioception. Using plyometric training, Swanik et al 63 demonstrated improvements in swimmers’ proprioception, kinesthesia, and muscle performance characteristics that were consistent with our results.
Plyometric exercises with TP can improve knee joint position sense in female athletes with dynamic knee valgus at 45° of knee flexion. The athletes in the TP group were able to translate their training into safer landing kinematics and better joint position sense even though the squat tasks were not included as part of their training program. This type of “transfer” is indicative of motor learning and may be key to preventing ACL injuries in sports where athletes need to perform maneuvers under varying circumstances. By contrast, athletes in the FB group were less able to successfully adapt their movement pattern or transfer their training into improved performance during posttest.
Based on these results, it is recommended that TP and plyometrics, regardless of the presence of injury, may be helpful in people who have a poor joint position sense for improving their proprioception. Regardless, there is a need to continue to explore the influence of attentional focus on training adaptations because most studies related to attentional focus have only examined immediate differences in task performance or short-term retention of a motor skill.
Landing Error Scoring System
Plyometric training can improve joint awareness, balance, and neuromuscular properties. Multiple studies demonstrate that plyometric training may have a significant effect on knee stability and prevention of non-contact ACL injury among female athletes. It improves athletic performance by increasing neuromuscular adaptations and correcting faulty jumping or cutting mechanics, 1 helping increase knee flexion angles, and decreasing knee valgus at landing. Plyometric training may facilitate neural adaptations that enhance proprioception, kinesthesia, and muscle performance characteristics as well. The current findings support this, 1 showing that our interventions reduced LESS errors in active women with dynamic knee valgus. It is possible that the LESS scores improved in the TP and FB groups because the hamstrings limited knee valgus motion. So, plyometric training with instructional FB or TP is recommended to improve landing techniques and thus reduce future injuries. The reported MDC for the LESS was 5 in the literature. 18 The change from pre- to posttest exceeded the MDC for the TP group in 7 of 16 participants and for the FB group in 8 of 16 participants.
A previous study showed that increasing the angle of knee flexion at ground contact can reduce the forces and load on the knee during landing movements. 68 Thus, reducing knee flexion increases the probability of injury to the knee and the ACL. 1 Laboratory motion analysis systems are the most accurate way to examine such motor patterns, but because of financial considerations and time constraints, their use to identify individuals with risky movement patterns in large groups is not practical. The LESS is a very inexpensive field tool that calculates landing jumping errors for a range of obvious items in human movement. 50 This system has the high-performance capability to clinically evaluate hazardous landing techniques.48,50
Study Limitations and Strengths
Our findings indicate that the effects of a 6-week plyometric exercises with valgus control FB or TP on LESS performance, joint position sense, and timing of muscle onset in lower limb muscles may depend on an athlete’s attentional focus during training.
Athletes who trained with an external focus demonstrated superior improvements in timing of muscle onset, and LESS performance and reductions in joint position sense error than athletes who trained with plyometric exercises alone. It appears that clinicians, trainers, and coaches should consider utilizing instructions that promote an external focus when plyometric training programs with female athletes.
However, there are also limitations that must be considered. First, our study only included female athletes. Although the number of ACL injuries is higher in male athletes (male athletes sustain ACL injuries), most neuromuscular training programs have been specifically designed for both athletes. In addition, only the joint position sense of the knee joint was examined. The ankle joint is important for functional activities (jump landing), but because of time constraints, the proprioception of this joint was not evaluated. Finally, our study did not examine hip and knee via 3-dimensional motion analysis, which could have provided additional insight regarding control during landing.
Conclusion
Plyometric training with FB or TP improved LESS scores; resulted in earlier activity of the VM, GM, ST, and BF muscles; and later activation of the RF and VL (TP group) muscles. Also, plyometric training with TP improves joint position sense.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
ORCID iDs: Malihe Hadadnezhad  https://orcid.org/0000-0002-5826-1524
https://orcid.org/0000-0002-5826-1524
Amir Letafatkar  https://orcid.org/0000-0002-5612-8340
https://orcid.org/0000-0002-5612-8340
References
- 1. Alikhani R, Shahrjerdi S, Golpaigany M, Kazemi M. The effect of a six-week plyometric training on dynamic balance and knee proprioception in female badminton players. J Can Chiropr Assoc. 2019;63:144-153. [PMC free article] [PubMed] [Google Scholar]
- 2. Baker V, Bennell K, Stillman B, Cowan S, Crossley K. Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res. 2002;20:208-214. [DOI] [PubMed] [Google Scholar]
- 3. Baratta R, Solomonow M, Zhou BH, Letson D, Chuinard R, D’Ambrosia R. Muscular coactivation. The role of the antagonist musculature in maintaining knee stability. Am J Sports Med. 1988;16:113-122. [DOI] [PubMed] [Google Scholar]
- 4. Besier T, Lloyd D, Ackland T. Muscle activation strategies at the knee during running and cutting maneuvers. Med Sci Sports Exerc. 2003;35:119-127. [DOI] [PubMed] [Google Scholar]
- 5. Birmingham TB, Kramer JF, Inglis JT, et al. Effect of a neoprene sleeve on knee joint position sense during sitting open kinetic chain and supine closed kinetic chain tests. Am J Sports Med. 1998;26:562-566. [DOI] [PubMed] [Google Scholar]
- 6. Caine D, Maffulli N, Caine C. Epidemiology of injury in child and adolescent sports: injury rates, risk factors, and prevention. Clin Sports Med. 2008;27:19-50. [DOI] [PubMed] [Google Scholar]
- 7. Callaghan MJ, Selfe J, Bagley PJ, Oldham JA. The effects of patellar taping on knee joint proprioception. J Athl Train. 2002;37:19-24. [PMC free article] [PubMed] [Google Scholar]
- 8. Cameron ML, Adams RD, Maher CG. The effect of neoprene shorts on leg proprioception in Australian football players. J Sci Med Sport. 2008;11:345-352. [DOI] [PubMed] [Google Scholar]
- 9. Caulfield B, Garrett M. Changes in ground reaction force during jump landing in subjects with functional instability of the ankle joint. Clin Biomech (Bristol, Avon). 2004;19:617-621. [DOI] [PubMed] [Google Scholar]
- 10. Cesar GM, Pereira VS, Santiago PRP, et al. Variations in dynamic knee valgus and gluteus medius onset timing in non-athletic females related to hormonal changes during the menstrual cycle. Knee. 2011;18:224-230. [DOI] [PubMed] [Google Scholar]
- 11. Chimera NJ, Swanik KA, Swanik CB, Straub SJ. Effects of plyometric training on muscle-activation strategies and performance in female athletes. J Athl Train. 2004;39:24-31. [PMC free article] [PubMed] [Google Scholar]
- 12. Clark NC, Röijezon U, Treleaven J. Proprioception in musculoskeletal rehabilitation. Part 2: clinical assessment and intervention. Man Ther. 2015;20:378-387. [DOI] [PubMed] [Google Scholar]
- 13. Cohen J. A power primer. Psychol Bull. 1992;112:155-159. [DOI] [PubMed] [Google Scholar]
- 14. DeMont RG, Lephart SM. Effect of sex on preactivation of the gastrocnemius and hamstring muscles. Br J Sports Med. 2004;38:120-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ericksen HM, Gribble PA, Pfile KR, Pietrosimone BG. Different modes of feedback and peak vertical ground reaction force during jump landing: a systematic review. J Athl Train. 2013;48:685-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ericksen HM, Thomas AC, Gribble PA, Doebel SC, Pietrosimone BG. Immediate effects of real-time feedback on jump-landing kinematics. J Orthop Sport Phys Ther. 2015;45:112-118. [DOI] [PubMed] [Google Scholar]
- 17. Ghanati HA, Letafatkar A, Almonroeder TG, Rabiei P. Examining the influence of attentional focus on the effects of a neuromuscular training program in male athletes. J Strength Cond Res. Published online June 17, 2020. doi: 10.1519/JSC.0000000000003681 [DOI] [PubMed] [Google Scholar]
- 18. Hanzlíková I, Hébert-Losier K. Is the landing error scoring system reliable and valid? A systematic review. 2020;12:181-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hendry D, Campbell A, Ng L, Grisbrook TL, Hopper DM. Effect of Mulligan’s and Kinesio knee taping on adolescent ballet dancers knee and hip biomechanics during landing. Scand J Med Sci Sport. 2015;25:888-896. [DOI] [PubMed] [Google Scholar]
- 20. Hermens HJ, Freriks B, Merletti R, et al. European Recommendations for Surface Electromyography: Results of the SENIAM Project. Roessingh Research and Development; 1999. [Google Scholar]
- 21. Hewett TE, Ford KR, Hoogenboom BJ, Myer GD. Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations—update 2010. N Am J Sports Phys Ther. 2010;5:234-251. [PMC free article] [PubMed] [Google Scholar]
- 22. Hewett TE, Lindenfeld TN, Riccobene JV., Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699-706. [DOI] [PubMed] [Google Scholar]
- 23. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492-501. [DOI] [PubMed] [Google Scholar]
- 24. Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765-773. [DOI] [PubMed] [Google Scholar]
- 25. Hewett TE, Zazulak BT, Myer GD, Ford KR. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br J Sports Med. 2005;39:347-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hodges PW, Bui BH. A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electroencephalogr Clin Neurophysiol. 1996;101:511-519. [DOI] [PubMed] [Google Scholar]
- 27. Howe A, Campbell A, Ng L, Hall T, Hopper D. Effects of two different knee tape procedures on lower-limb kinematics and kinetics in recreational runners. Scand J Med Sci Sport. 2015;25:517-524. [DOI] [PubMed] [Google Scholar]
- 28. Ireland ML. Anterior cruciate ligament injury in female athletes: epidemiology.J Athl Train. 1999;34:150-154. [PMC free article] [PubMed] [Google Scholar]
- 29. Kianifar R, Lee A, Raina S, Kulić D. Automated assessment of dynamic knee valgus and risk of knee injury during the single leg squat. IEEE J Transl Eng Health Med. 2017;5:2100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. Am J Sports Med. 2010;38:2218-2225. [DOI] [PubMed] [Google Scholar]
- 31. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359-367. [DOI] [PubMed] [Google Scholar]
- 32. Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Gender differences exist in neuromuscular control patterns during the pre-contact and early stance phase of an unanticipated side-cut and cross-cut maneuver in 15-18 years old adolescent soccer players. J Electromyogr Kinesiol. 2009;19:e370-e379. [DOI] [PubMed] [Google Scholar]
- 33. Lephart SM, Abt JP, Ferris CM, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39:932-938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Letafatkar A, Rajabi R, Minoonejad H, Rabiei P. Efficacy of perturbation-enhanced neuromuscular training on hamstring and quadriceps onset time, activation and knee flexion during a tuck-jump task. Int J Sports Phys Ther. 2019;14:214-227. [PMC free article] [PubMed] [Google Scholar]
- 35. Levinger P, Gilleard W, Coleman C. Femoral medial deviation angle during a one-leg squat test in individuals with patellofemoral pain syndrome. Phys Ther Sport. 2007;8:163-168. [Google Scholar]
- 36. Medina JM, Valovich McLeod TC, Howell SK, Kingma JJ. Timing of neuromuscular activation of the quadriceps and hamstrings prior to landing in high school male athletes, female athletes, and female non-athletes. J Electromyogr Kinesiol. 2008;18:591-597. [DOI] [PubMed] [Google Scholar]
- 37. Mehta SP, Barker K, Bowman B, Galloway H, Oliashirazi N, Oliashirazi A. Reliability, concurrent validity, and minimal detectable change for iPhone goniometer app in assessing knee range of motion. J Knee Surg. 2016;30:577-584. [DOI] [PubMed] [Google Scholar]
- 38. Momeni S, Barati A, Letafatkar A, Jamshidi A, Hovanlo F. The effects of plyometric training on performance and the feed-forward activation of calf muscles in active females with functional ankle instability in single leg drop landing. J Ilam Univ Med Sci. 2017;25:42-54. [Google Scholar]
- 39. Myer GD, Ford KR, Hewett TE. New method to identify athletes at high risk of ACL injury using clinic-based measurements and freeware computer analysis. Br J Sports Med. 2011;45:238-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39:352-364. [PMC free article] [PubMed] [Google Scholar]
- 41. Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025-2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445-455. [DOI] [PubMed] [Google Scholar]
- 43. Myklebust G, Maehlum S, Engebretsen L, Strand T, Solheim E. Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. Scand J Med Sci Sports. 2007;7:289-292. [DOI] [PubMed] [Google Scholar]
- 44. Nagano Y, Ida H, Akai M, Fukubayashi T. Effects of jump and balance training on knee kinematics and electromyography of female basketball athletes during a single limb drop landing: pre-post intervention study. Sport Med Arthrosc Rehabil Ther Technol. 2011;3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Noor R, Olyaei G, Hadian MR, Talebian S, Bashir MS. A reliable and accurate system of joint position sense measurement. Biomed Res. 2018;29:2528-2531. [Google Scholar]
- 46. Onate J, Cortes N, Welch C, Van Lunen B. Expert versus novice interrater reliability and criterion validity of the landing error scoring system. J Sport Rehabil. 2010;19:41-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ozer D, Senbursa G, Baltaci G, Hayran M. The effect on neuromuscular stability, performance, multi-joint coordination and proprioception of barefoot, taping or preventative bracing. Foot. 2009;19:205-210. [DOI] [PubMed] [Google Scholar]
- 48. Padua DA, Boling MC, DiStefano LJ, Onate JA, Beutler AI, Marshall SW. Reliability of the landing error scoring system–real time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehabil. 2011;20:145-156. [DOI] [PubMed] [Google Scholar]
- 49. Padua DA, DiStefano LJ, Beutler AI, De La Motte SJ, DiStefano MJ, Marshall SW. The landing error scoring system as a screening tool for an anterior cruciate ligament injury-prevention program in elite-youth soccer athletes. J Athl Train. 2015;50:589-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the Jump-ACL study. Am J Sports Med. 2009;37:1996-2002. [DOI] [PubMed] [Google Scholar]
- 51. Palmieri-Smith RM, Wojtys EM, Ashton-Miller JA. Association between preparatory muscle activation and peak valgus knee angle. J Electromyogr Kinesiol. 2008;18:973-979. [DOI] [PubMed] [Google Scholar]
- 52. Pinto BL, Beaudette SM, Brown SHM. Tactile cues can change movement: an example using tape to redistribute flexion from the lumbar spine to the hips and knees during lifting. Hum Mov Sci. 2018;60:32-39. [DOI] [PubMed] [Google Scholar]
- 53. Pollard CD, Sigward SM, Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech (Bristol, Avon). 2010;25:142-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pols MA, Peeters PHM, Bueno-De-Mesquita HB, et al. Validity and repeatability of a modified Baecke questionnaire on physical activity. Int J Epidemiol. 1995;24:381-388. [DOI] [PubMed] [Google Scholar]
- 55. Renstrom P, Ljungqvist A, Arendt E, et al. Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement. Br J Sports Med. 2008;42:394-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rodacki AL, Fowler NE, Bennett SJ. Multi-segment coordination: fatigue effects. Med Sci Sports Exerc. 2001;33:1157-1167. [DOI] [PubMed] [Google Scholar]
- 57. Rostami A, Letafatkar A, Gokeler A, Khaleghi M. The effects of external focus instruction exercise on performance and kinetics in landing after volleyball blocks of female athletes. J Sport Rehabil. 2018;29:1-37. [DOI] [PubMed] [Google Scholar]
- 58. Sheikhi B, Letafatkar A, Hogg J, Naseri-Mobaraki E. The influence of kinesio taping on trunk and lower extremity motions during different landing tasks: implications for anterior cruciate ligament injury. J Exp Orthop. 2021;8:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Simoneau GG, Degner RM, Kramper CA, Kittleson KH. Changes in ankle joint proprioception resulting from strips of athletic tape applied over the skin. J Athl Train. 1997;32:141-147. [PMC free article] [PubMed] [Google Scholar]
- 60. Smith HC, Johnson RJ, Shultz SJ, et al. A prospective evaluation of the Landing Error Scoring System (LESS) as a screening tool for anterior cruciate ligament injury risk. Am J Sports Med. 2012;40:521-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Stillman BC, McMeeken JM. The role of weightbearing in the clinical assessment of knee joint position sense. Aust J Physiother. 2001;47:247-253. [DOI] [PubMed] [Google Scholar]
- 62. Struminger AH, Lewek MD, Goto S, Hibberd E, Blackburn JT. Comparison of gluteal and hamstring activation during five commonly used plyometric exercises. Clin Biomech (Bristol, Avon). 2013;28:783-789. [DOI] [PubMed] [Google Scholar]
- 63. Swanik KA, Lephart SM, Swanik CB, Lephart SP, Stone DA, Fu FH. The effects of shoulder plyometric training on proprioception and selected muscle performance characteristics. J Shoulder Elbow Surg. 2002;11:579-586. [DOI] [PubMed] [Google Scholar]
- 64. Tang SFT, Chen C-K, Hsu R, Chou S-W, Hong W-H, Lew HL. Vastus medialis obliquus and vastus lateralis activity in open and closed kinetic chain exercises in patients with patellofemoral pain syndrome: an electromyographic study. Arch Phys Med Rehabil. 2001;82:1441-1445. [DOI] [PubMed] [Google Scholar]
- 65. Tegnander A, Olsen OE, Moholdt TT, Engebretsen L, Bahr R. Injuries in Norwegian female elite soccer: a prospective one-season cohort study. Knee Surg Sports Traumatol Arthrosc. 2008;16:194-198. [DOI] [PubMed] [Google Scholar]
- 66. Williams GN, Chmielewski T, Rudolph KS, Buchanan TS, Snyder-Mackler L. Dynamic knee stability: current theory and implications for clinicians and scientists. J Orthop Sport Phys Ther. 2001;31:546-566. [DOI] [PubMed] [Google Scholar]
- 67. Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol, Avon). 2012;27:1045-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Yu B, Herman D, Preston J, Lu W, Kirkendall DT, Garrett WE. Immediate effects of a knee brace with a constraint to knee extension on knee kinematics and ground reaction forces in a stop-jump task. Am J Sports Med. 2004;32:1136-1143. [DOI] [PubMed] [Google Scholar]