Abstract
Background
Accurate accelerometer-based methods are required for assessment of 24-h physical behavior in young children. We aimed to summarize evidence on measurement properties of accelerometer-based methods for assessing 24-h physical behavior in young children.
Methods
We searched PubMed (MEDLINE) up to June 2021 for studies evaluating reliability or validity of accelerometer-based methods for assessing physical activity (PA), sedentary behavior (SB), or sleep in 0–5-year-olds. Studies using a subjective comparison measure or an accelerometer-based device that did not directly output time series data were excluded. We developed a Checklist for Assessing the Methodological Quality of studies using Accelerometer-based Methods (CAMQAM) inspired by COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN).
Results
Sixty-two studies were included, examining conventional cut-point-based methods or multi-parameter methods. For infants (0—12 months), several multi-parameter methods proved valid for classifying SB and PA. From three months of age, methods were valid for identifying sleep. In toddlers (1—3 years), cut-points appeared valid for distinguishing SB and light PA (LPA) from moderate-to-vigorous PA (MVPA). One multi-parameter method distinguished toddler specific SB. For sleep, no studies were found in toddlers. In preschoolers (3—5 years), valid hip and wrist cut-points for assessing SB, LPA, MVPA, and wrist cut-points for sleep were identified. Several multi-parameter methods proved valid for identifying SB, LPA, and MVPA, and sleep.
Despite promising results of multi-parameter methods, few models were open-source. While most studies used a single device or axis to measure physical behavior, more promising results were found when combining data derived from different sensor placements or multiple axes.
Conclusions
Up to age three, valid cut-points to assess 24-h physical behavior were lacking, while multi-parameter methods proved valid for distinguishing some waking behaviors. For preschoolers, valid cut-points and algorithms were identified for all physical behaviors. Overall, we recommend more high-quality studies evaluating 24-h accelerometer data from multiple sensor placements and axes for physical behavior assessment. Standardized protocols focusing on including well-defined physical behaviors in different settings representative for children’s developmental stage are required. Using our CAMQAM checklist may further improve methodological study quality.
PROSPERO Registration number
CRD42020184751.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12966-022-01296-y.
Keywords: 24-h physical behavior, Physical activity, Sedentary behavior, Sleep, Infants, Toddlers, Preschoolers, Accelerometer, Cut-points, Machine learning, Measurement properties, Validity, Reliability
Introduction
Accurate assessment of 24-h physical behavior in young children is crucial as it provides the basis for examining the health benefits of these behaviors and thereby evidence for establishing 24-h movement guidelines. Recent studies indicated the importance of an integrated approach to all 24-h physical behaviors for health, encompassing sleep, sedentary behavior (SB), and physical activity (PA) [1–5]. These behaviors are distributed along an intensity continuum ranging from low energy expenditure, such as sleep, to vigorous PA requiring high energy expenditure [6, 7].
Currently, a wide variety of direct measurement instruments are used to assess physical behaviors of children, such as doubly labelled water, (in)direct calorimetry, polysomnography, direct (video) observation, and accelerometry [8]. Polysomnography is considered a “gold standard” for sleep, however, this can only be applied in a laboratory setting. Doubly labelled water is considered a “gold standard” for total energy expenditure, however, it cannot distinguish frequency, type, and intensity of specific physical behaviors [9, 10]. Direct calorimetry accurately measures metabolic rate in confinement, and indirect calorimetry allows for this assessment in free-living situations, however, both methods come with relatively high costs and are also not distinctive for frequency, type, and intensity of specific physical behaviors [11]. While direct (video) observation is considered a suitable comparator measure for assessing different types of physical behaviors, it is less suitable for assessing activity intensity because this can only be derived by assigning a metabolic equivalent to represent energy cost, which is unknown for the youngest age groups (i.e., infants and toddlers) [6, 7]. In addition, direct observation is very time consuming and requires trained observers scoring a specified protocol [9]. Given these limitations, these methods might not be feasible for measuring young children’s 24-h physical behaviors in free-living situations. Accelerometers can capture data on body movement, or lack thereof, continuously over extended periods of time, and are therefore widely considered the most promising method for physical behavior assessment.
Current reviews on reliability and validity of accelerometer-based methods for measuring physical behaviors in young children were limited to evaluation of only one measurement property [12] or one physical behavior [13]. Lynch and colleagues (2019) reviewed studies that evaluated criterion validity of accelerometers against indirect calorimetry, concluding that accelerometers can accurately assess SB and PA in children 3 to 18 years old [12]. De Vries and colleagues (2006) reviewed criterion-, convergent validity, test–retest- and inter-device reliability of accelerometers. They found that accelerometers provide reasonable estimates for assessing PA, however, no evidence on reliability was found in 2- to 4-years-old children [13]. Moreover, evidence on these measurement properties for infants (0—12 months) and toddlers (1—3 years) is lacking [14, 15]. Bruijns and colleagues (2020) reviewed estimates of PA and SB derived from accelerometer data in infants and toddlers and found that PA estimates were inconclusive and largely heterogeneous [14]. Additionally, no studies under three years old were found in a review on the evidence for methodological accelerometer decisions (e.g., epoch length, wear location, data analysis approach) for assessing PA in children aged 0—5 years [15].
While accelerometer-based methods provide reasonable estimates of time spent in SB, PA, and sleep in school-aged children [12, 13, 16–19], this cannot be generalized to young children due to major differences in types and intensity of their physical behaviors [20]. Physical activity types are different for children, depending on their developmental stage, e.g., daytime naps, crawling, and being carried in the youngest age groups [15, 21]. Moreover, the intensity of activities might differ between children depending on the efficiency of motor skills. For instance, toddlers start walking around one year of age, increase locomotor (e.g., running, jumping, hopping), stability (e.g., balancing, climbing), and develop object-control skills (e.g., kicking, catching, rolling) [22]. Preschoolers (3–5 years) further develop these skills and often participate in modified sports [23]. These differences in physical behaviors and motor development require age group specific studies on the validity and reliability of measurement instruments and analysis techniques, adapted to the child’s developmental stage.
For assessment of 24-h physical behavior in young children a complete overview of measurement properties of accelerometer-based methods is unavailable and there is no consensus about the optimal measurement protocol (e.g., epoch length, wear location) and accelerometer processing (e.g., cut-points, algorithms, machine learning methods) decisions for the use of accelerometer-based methods in young children [15]. To be able to select the most appropriate method for the child’s developmental stage, an overview of current accelerometer processing and study designs, and measurement properties of the available accelerometer-based methods is warranted. Therefore, we aimed to comprehensively review all studies examining the measurement properties test–retest, inter-device reliability, criterion- and convergent validity of accelerometer-based methods assessing 24-h physical behavior in young children aged 0–5 years, including an evaluation of the quality of evidence.
Methods
We registered this review on PROSPERO (international prospective register of ongoing systematic reviews; registration number: CRD42020184751) and followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [24].
Search strategy
We systematically searched the electronic database PubMed (MEDLINE) up until 26th June 2021. The search strategy focused on terms related to young children (e.g., infant, toddler, preschooler), accelerometer-based methods (e.g., accelerometry/methods, actigraphy), and measurement properties (e.g., validity, reliability). These terms were used in AND-combination with terms related to physical behavior: SB (e.g., inactive behavior, stationary behavior, sitting), PA (e.g., motor activity, tummy time, cycling), OR sleep (e.g., nap, bedtime, night rest). Articles related to animals, a variety of disorders (e.g., autism, attention deficit disorder), and diseases were excluded using the NOT-combination. Medical Subject Heading (MeSH), title and abstract (TIAB), and free-text search terms were used, and a variety of publication types were excluded (e.g., book sections, thesis). The full search strategy can be found in Additional File 1.
Eligibility criteria
Studies were eligible for inclusion when the study: 1) used an accelerometer-based method to monitor at least one physical behavior: SB, PA, or sleep; 2) evaluated at least one measurement property of an accelerometer-based method: test–retest or inter-device reliability, criterion- or convergent validity; 3) included a (sub)sample of apparently healthy children, born term (> 37 weeks), with a mean age < 5 years or a wider range with the results for 0–5-year-olds reported separately; 4) was published in English in a peer-reviewed journal; and 5) full-text was available.
Studies were excluded when the study: 1) used a diary, parent- or proxy-report, or relied on parents for direct observation as comparison measure; 2) evaluated measurement properties in a clinical population, e.g., focused on only children with overweight or obesity; or 3) relied on accelerometer-based devices that do not directly output data on acceleration time series data or magnitude of acceleration, e.g., Fitbit.
Selection procedures
We imported articles into reference manager software (EndNote X 9.1), and subsequently removed duplicate articles. Two researchers (AL and TA) independently screened titles and abstracts for eligibility using Rayyan and subsequently screened full-text articles. For four publications, the mean age of the study population was missing. To resolve this missing information, we contacted the authors. In addition, the reference lists of all relevant full-text articles were screened for possible inclusion of additional studies. A third researcher (MC) was consulted to resolve discrepancies.
Data extraction
For all eligible studies, two researchers (AL and JA) extracted data using a structured form. Disagreements were resolved through discussion. Extracted data included the evaluated measurement properties, study and target population, accelerometer specifications (i.e., device and model, placement location and site, epoch length, axis), accelerometer data analysis approach used, outcome(s) and setting, comparison method (in case of validity), time interval (in case of test–retest reliability), and results of the evaluated measurement properties. The variety of accelerometer-based methods was described using code combinations of the following four elements: accelerometer brand, analysis approach, axis, and epoch length (see Additional File 3).
Methodological quality assessment
Two researchers (AL and either TA or MC) rated the methodological quality of the included studies independently using a newly developed checklist to assess risk of bias. Risk of bias refers to whether the results for evaluating a measurement property are trustworthy based on the methodological study quality. In case of disagreement, all three researchers discussed the rating until consensus was reached.
Checklist development
We newly developed a Checklist for Assessing the Methodological Quality of studies using Accelerometer-based Methods (CAMQAM), as there was no standardized checklist available. The CAMQAM was inspired by quality assessment of patient reported outcomes, the standardized COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) risk of bias checklist [25–27], and by a previous review by Terwee and colleagues [28]. To fit accelerometer-based methods, we used the following relevant parts and, made minimal adjustments (e.g., wordings): ‘Box 6 Reliability’ for test–retest- and inter-device reliability,’Box 8 Criterion Validity’ for criterion validity, and ‘Box 9 Hypothesis testing for construct validity’ part ‘9a Comparison with other outcome measurement instruments’ for convergent validity. Moreover, we developed two boxes with additional items to rate methodological quality of studies assessing the criterion- or convergent validity of a specific accelerometer data analysis approach to categorize physical behavior: 1) conventional cut-points based method using a single value, or 2) multi-parameter method using more than one parameter, e.g., sleep algorithm, machine learning method. Two of the authors (TA and MC) independently rated the most diverse included studies for each measurement property. Thereafter, we added examples or explanations to clarify the items and ensure studies were scored using the correct box. The CAMQAM was used as a modular tool; only those boxes were completed for the measurement properties evaluated in the study.
For each examined measurement property, the study design requirements were rated as either very good, adequate, doubtful, or inadequate quality [25]. To rate the final methodological study quality, a worst score method was adopted, i.e., using the lowest rating of any item in a box. Additional File 2 presents the complete checklist and scoring manual.
In the appraisal of methodological study quality, the following study aspects were considered: study design (e.g., sample, epoch length, measurement duration, comparison instrument and their measurement properties in the study population) and the performed statistical analysis to evaluate the measurement property of the accelerometer-based method (see Table 1 in Additional File 2 for a summary of the definitions).
Rating study results
The result of each study on a measurement property was rated against the criteria for good measurement properties proposed in the COSMIN guideline, i.e., sufficient (+), insufficient (-), inconsistent (±) or intermediate (?) [26]. Below is indicated for each measurement property which outcomes were considered sufficient (+). Outcomes were considered insufficient (-) when these criteria were not met, and intermediate (?) when not all necessary information was reported. Due to the great variety of accelerometer-based methods adopted in the studies, quantitative pooling or quantitatively summarizing of the results was not feasible.
Reliability
Reliability results were considered acceptable under the following conditions: 1) Intraclass Correlation Coefficients (ICC) or Kappa values (κ) were ≥ 0.70 [28]; or Pearson (rp), Spearman rank (rsp) or unknown (r) correlation coefficients were ≥ 0.80 [25]. Some studies reported multiple correlations per accelerometer-based method for reliability, e.g., separate correlations for different physical intensities. Therefore, we applied a rating per physical behavior (i.e., incorporating correlations separately for PA, SB, and/or sleep), and an overall rating (i.e., incorporating all correlations) to obtain final reliability rating for each study. When ≥ 75% of reliability outcomes were acceptable, a sufficient rating was received, when ≥ 50% and < 75% of reliability outcomes were acceptable an inconsistent rating was received, and an insufficient evidence rating was received when < 50% of reliability outcomes were acceptable.
Validity
Criterion validity was considered acceptable when: 1) correlations or κ with the ‘gold standard’ were ≥ 0.70 (Table 1, e.g., comparison measure was polysomnography for accelerometer-based methods aiming to assess sleep, or indirect calorimetry to score energy expenditure); or diagnostic test results (i.e., area under the receiver operating curve, accuracy, sensitivity, or specificity) were ≥ 0.80.
Table 1.
Physical behavior assessed by accelerometer-based methods evaluating validity, subdivided by level of evidencea, and criteria for acceptable outcome values
| Physical behavior | Level of Evidence | ||
| Level 1 | Level 2 | Level 3 | |
| Physical activity | Indirect calorimetry to score energy expenditure, e.g., DLW, AEE | Direct observation to score activity type | Pedometer (daily) step counts |
| Direct video observation to score activity type | Accelerometer-based magnitude of acceleration (different brand/type) | ||
| Sedentary behavior (primarily defined as an activity type, and secondarily as an intensity) | Direct video observation to score activity type | Direct observation to score activity type | Accelerometer-based magnitude of acceleration (different brand/type) |
| Indirect calorimetry to score energy expenditure | Accelerometer-based orientation classification (thigh data), e.g., activPAL | ||
| Sleep | Polysomnography | Videosomnography or direct video observation to classify sleep–wake states | Direct observation to classify sleep–wake states |
| Indirect calorimetry, e.g., SMR | Accelerometer-based magnitude of acceleration (different brand/type) | ||
| Outcome value | Acceptable results | ||
| Level 1 | Level 2 | Level 3 | |
| rp, rsp, r, R2 | ≥ .70 | ≥ .60 | ≥ .60 |
| AUC-ROC, accuracy, Se, Sp | ≥ .80 | ≥ .80 | ≥ .80 |
| ICC, CCC κ, κw, κqw | ≥ .70 | ≥ .70 | ≥ .70 |
Abbreviations: AEE activity energy expenditure, AUC-ROC area under the receiver operating curve, CCC concordance correlation coefficient, DLW doubly labelled water, ICC intraclass correlation coefficient, κ Kappa, κw weighted Kappa, κqw quadratic weighted Kappa, rp Pearson correlation coefficient, rsp Spearman’s rank-order correlation coefficient, r unknown correlation coefficient, R2 R-squared value, Se sensitivity, SMR sleeping metabolic rate, Sp specificity
a Level of evidence: level 1 indicating strong evidence, level 2 indicating moderate evidence, and level 3 indicating weak evidence
To rate the results of studies that evaluated convergent validity, we formulated criteria for acceptable results regarding the confidence in the comparison instrument to accurately measure the relevant physical behavior (i.e., level of evidence) (Table 1). We first assessed the level of evidence using these criteria, where level 1 indicated strong evidence, level 2 indicated moderate evidence, and level 3 indicated weak evidence. Thereafter, subdivided by the level of evidence, we rated study results as acceptable when: 1a) correlations (i.e., rp, rsp, r) with the comparison measure were ≥ 0.70 (level 1); or 1b) correlations with the comparison measure were ≥ 0.60 (level 2 or level 3) [13]; 1c) ICC, Concordance Correlation Coefficients (CCC), or κ with the comparison measure were ≥ 0.70; 2) or diagnostic test results were ≥ 0.80. As most studies reported multiple results, we applied a rating per physical behavior (i.e., incorporating results separately for SB, PA, and/or sleep), and an overall rating for each study. When ≥ 75% of the validity outcomes were rated as acceptable, a sufficient rating was received, when ≥ 50% and < 75% of validity outcomes were rated as acceptable an inconsistent rating was received, and an insufficient evidence rating was received when < 50% of validity outcomes were acceptable.
Quality of evidence grading
Quality of evidence was graded using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach as proposed in the COSMIN guideline, i.e., high, moderate, low, or very low [26], to indicate trustworthiness of the measurement property results. To derive the grading, the methodological study quality (i.e., risk of bias) was weighted with relevant risk factors: 1) inconsistency, i.e., unexplained inconsistency of results across studies, 2) imprecision, i.e., total sample size of the available studies, and 3) indirectness, i.e., evidence from different populations than the population of interest in this review [26]. The evidence grading was subsequently downgraded with one, two, or three levels for each risk factor, to moderate, low, or very low quality of evidence. The quality of evidence grading was performed for each measurement property and each accelerometer-based method separately.
Results
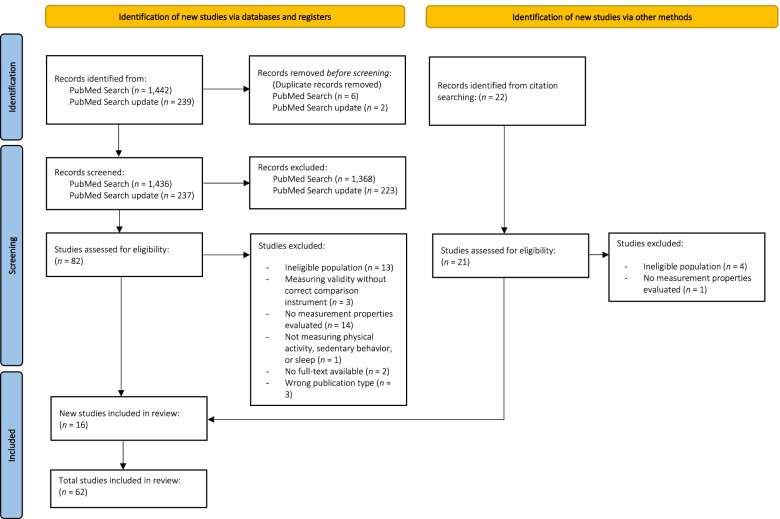
The systematic literature search yielded a total of 1,673 unique articles. After title and abstract screening, 82 full-texts were screened. Additionally, 16 articles were found through cross-reference searches. Therefore, a total of 98 full-text articles were assessed for eligibility, of which 62 were included (see Fig. 1 for the full selection process). Thirteen of the included studies evaluated the measurement properties of accelerometer-based methods for assessing SB, PA, and/or sleep in infants [29–41], nine in toddlers [42–50], and forty in preschoolers [51–90].
Fig. 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagram of study inclusion
The included studies evaluated measurement properties for time series data or magnitude of acceleration directly [42, 45, 51–60, 62, 63, 70] or applied one of the following data analysis approaches to categorize physical behavior: a conventional cut-points based method using a single value [29–34, 42–47, 51–53, 56, 61, 64–81, 89], or a multi-parameter method (e.g., algorithm, machine learning) [30, 35–41, 48–50, 55, 66, 75, 82–90].
Reliability
Table 2 summarizes the results for reliability, of which two studies examined test–retest reliability [29, 65], and one study examined inter-device reliability [42]. Test–retest reliability of an accelerometer-based method using a cut-points based method was evaluated by measuring SB and PA in preschool aged children [65]. Total PA, SB, light PA (LPA) and moderate-to-vigorous PA (MVPA) were considered reliable across all wear time criteria, except for absolute values of SB. For absolute values of SB, results were sufficient if data was collected for ≥ 5 days/week of ≥ 10 h. Despite adequate methodological study quality, these results received low quality of evidence as they were retrieved in a sample of 91 preschoolers. Inter-device reliability for epoch level activity counts (60 s) was rated as sufficient for activity counts in toddlers wearing two Actical devices side-by-side on the non-dominant ankle [42]. Despite adequate methodological study quality, these results received low quality of evidence as they were retrieved in a limited sample of 24 toddlers.
Table 2.
Reliability of accelerometer-based methods, sorted by methodological study quality, study result rating and quality of evidence
| Study | Study populationa | Outcome(s) & Setting | Time interval | Methodological study qualityb | Placement | Device-based methodc | Results | Study result ratingd | Quality of evidencee |
|---|---|---|---|---|---|---|---|---|---|
| Hager et al. (2016) [42] |
Toddlers n = 24 * 2 Ac Age = 24.5 ± 5.2 (14.7 to 35.5) months Sex = 41.7% girls |
Activity counts Laboratory (structured activities) |
n.a | A | Non-dominant ankle; side-by-side | Ac-cts-omni-60 | ICC? = .98 | + | Low |
| Aadland & Johannessen (2015) [65] |
Preschoolers n = 91 Age = 4.07 ± 0.5 (3 to 5) years Sex = 51% girls |
Total PA, SB, LPA and MVPA in min/day and % of valid wear time Free-living |
14 days | A | Not reported | AG-Ev-VA-10 |
ICC−(1,1) ≥ .75 for all outcomes across all wear criteria (≥ 6, 8 and 10 h/day and ≥ 3 and 5 days/week) Except for SB (min/day): ICC−(1,1) .61 to .81 Higher ICC−(1,1) for percentages than absolute values ICC−(1,1) ≥ .80 (≥ 6 and ≥ 8 h/day) > 7 days required ICC−(1,1) ≥ .80 (≥ 10 h/day) within 7 days: 3.9 to 7.1 days |
+ (SB + ; PA +) |
Low |
| Greenspan, Cunha, & Lobo (2021) [29] |
Infants n = 16 Age = 3.1 ± 1.1 (1.8 to 5) months Sex = 51% girls |
Body position: supine, reclined, upright, inclined, and prone Free-living (structured play) |
0 days | I | Trunk | GG-Gr-HA/VA/DA-1 |
κw = .89, 95% CI (.87 to .91) Supine: agreement = 89.2% Reclined: agreement = 72.6% Upright: agreement = 90.9% Inclined: agreement = 84.6% Prone: agreement = 91.1% |
+ | Very low |
Abbreviations: Ac Actical, AG ActiGraph, cpm counts per minute, cts counts, DA diagonal axis (z-axis), Ev Evenson’s cut-points (2008) [91], GG get around garment with ADXL335, Gr Greenspan’s cut-points (2021) [29], HA horizontal axis (x-axis), ICC? intraclass correlation coefficient analysis decision was unclear, ICC−(1,1) intraclass correlation coefficient inappropriate analysis decision one-way random effects model, κwweighted Kappa, LPA light physical activity, MVPA moderate-to-vigorous physical activity, n.a. not applicable, omni omnidirectional, PA physical activity, r unknown correlation coefficient, SB sedentary behavior, VA vertical axis (y-axis), 1 1 s epoch, 10 10 s epoch, 60 60 s epoch
aAge presented as mean ± SD (range)
bMethodological study quality based on newly developed checklist: VG very good, A adequate, D doubtful, I inadequate
cDevice-based method described using code combinations of four elements resulting in the following format: brand-axis-approach-epoch length
dStudy result rating based on COSMIN guideline: + sufficient, ± inconsistent, - insufficient, ? intermediate
eQuality of evidence based on GRADE approach
Validity
The following subsections present the results for validity by age group. Notably, most studies used the vertical axis (VA). In studies among infants the accelerometer was predominantly worn on the ankle, while for studies among toddlers or preschoolers the devices were mainly placed on the hip. Unless otherwise specified, we report study results based on this majority placement and axis.
Infants
Table 3 summarizes the results for validity, of which four studies examined criterion validity [30–32, 35], and nine studies examined convergent validity [29, 33, 34, 36–41] in infants.
Table 3.
Criterion and convergent validity of accelerometer-based methods for infants, sorted by methodological study quality, quality of evidence (level of evidence), and study result rating
| Study | Study populationa | Outcome(s) & Setting | Comparison measure(s) | Methodological study qualityb | Placement | Device-based methodc | Results | Study result ratingd | Quality of evidencee (level of evidence) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Criterion validity | Galland et al. (2012) [30] |
n = 31 Age = 13.0 ± 3.1 (10.0 to 22.3) weeks Sex = 27.3% girls |
Sleep quality: sleep latency, TST, sleep efficiency, and WASO (duration and number) Laboratory (daytime nap) |
Polysomnography to score sleep stages as sleep (active, quiet, intermediate) and wake | VG | Shin | Ac-CS-omni-15 | accuracy = 86.3%, Se = 85.7%, Sp = 84.3%, κ = .66, PABAK = .72; Sleep latency rp = .79*** (underestimated by 3 min*), TST rp = .83***, Sleep efficiency rp = .87***, WASO (duration) rp = .48** (overestimated by 6.5 min***), WASO (number) rp = .35 (overestimated by 3***) | + | Low |
| Ac-CS-omni-30 | accuracy = 86.1%, Se = 84.7%, Sp = 87.4%, κ = .66, PABAK = .72 | + | ||||||||
| Ac-CS-omni-60 | accuracy = 84.5%, Se = 79.8%, Sp = 90.2%, κ = .63, PABAK = .69 | - | ||||||||
| Ac-S0-omni-15 | accuracy = 82.3%, Se = 94.8%, Sp = 57.8%, κ = .55, PABAK = .65; Sleep latency rp = .80*** (underestimated by 5 min***), TST rp = .76*** (overestimated by 11 min*), Sleep efficiency rp = .76*** (overestimated by 16.5%***), WASO (duration) rp = .48** (overestimated by 7 min***), WASO (number) rp = .38* (overestimated by 3***) | ± | ||||||||
| Ac-S0-omni-30 | accuracy = 86.3%, Se = 91.0%, Sp = 77.7%, κ = .65, PABAK = .72 | ± | ||||||||
| Ac-S0-omni-60 | accuracy = 84.5%, Se = 80.0%, Sp = 89.9%, κ = .63, PABAK = .69 | ± | ||||||||
| Ac-PS-omni-15 | accuracy = 84.3%, Se = 95.1%, Sp = 63.1%, κ = .59, PABAK = .69; Sleep latency rp = .93***, TST rp = .80*** (overestimated by 11 min*), Sleep efficiency rp = .81*** (overestimated by 13.6%*), WASO (duration) rp = .50** (overestimated by 3.5 min***), WASO (number) rp = .13 (overestimated by 3***) | ± | ||||||||
| Ac-PS-omni-30 | accuracy = 86.8%, Se = 90.8%, Sp = 79.0%, κ = .66, PABAK = .74 | ± | ||||||||
| Ac-PS-omni-60 | accuracy = 84.6%, Se = 79.9%, Sp = 90.3%, κ = .63, PABAK = .69 | ± | ||||||||
| Ac-WSC-omni-15 | accuracy = 83.2%, Se = 94.6%, Sp = 60.2%, κ = .57, PABAK = .66; Sleep latency rp = .78*** (underestimated by 4 min*), TST rp = .78*** (overestimated by 10 min*), Sleep efficiency rp = .79*** (overestimated by 15.2%*), WASO (duration) rp = .41* (overestimated by 7 min***), WASO (number) rp = .29 (overestimated by 3***) | ± | ||||||||
| Ac-WSC-omni-30 | accuracy = 86.5%, Se = 90.9%, Sp = 78.2%, κ = .66, PABAK = .73 | ± | ||||||||
| Ac-WSC-omni-60 | accuracy = 84.5%, Se = 80.0%, Sp = 89.9%, κ = .63, PABAK = .69 | ± | ||||||||
| Insana, Gozal, & Montgomery-Downs (2010) [31] |
n = 22 Age = 14.1 ± 0.6 (13.0 to 15.0) months Sex = 45.5% girls |
Sleep quality: TST and WASO (duration) Laboratory (in the hospital) |
Polysomnography to score sleep stages as sleep and wake | VG | Ankle | Aw-ACT40-uni-15 |
accuracy = 89.6%, Se (89.0 to 96.3%), Sp = 58.9% TST: rp = .83***, ICC = .80, MD = -72.3 (SD = 61.5) min***, d = .70 WASO: rp = .52*, ICC = .65, MD = 13.9 (SD = 30.9) min*, d = .44 |
± | Low | |
| Aw-ACT80-uni-15 |
TST: rp = .84***, ICC = .86, MD = 52.1 (SD = 60.4) min**, d = .50 WASO: rp = .52*, ICC = .65, MD = 6.4 (SD = 26.8) min |
± | ||||||||
| Rioualen et al. (2015) [32] |
n = 24 Age = 2.5 ± 0.7 days Sex = 50.0% girls |
Sleep stage: wake, active sleep, and quiet sleep Laboratory (in the hospital) |
Polysomnography to score sleep stages as sleep (active, quiet) and wake | VG | Wrist | Aw-ASA40-uni-60 |
Se = 93%, 95% CI (89 to 96) Sp = 20%, 95% CI (14 to 27) |
± | Low | |
| Ankle | Aw-ASA40-uni-60 | accuracy = 58.5%, Se = 87%, 95% CI (81 to 93), Sp = 31%, 95% CI (24 to 39) | - | |||||||
| Lewicke, Sazonov, & Schuckers (2004) [35] |
n = 25 Age = n.r Sex = n.r |
Sleep stage: wake, active sleep, and quiet sleep Laboratory |
Polysomnography to score sleep stages as sleep (active, quiet, indeterminate) and wake | I | Left hip | mSCA-LVQ-uni-30 |
Training: accuracy = 80.7%, Se = 94.6%, Sp = 48.2% Validation: accuracy = 75.3%, Se = 92.3%, Sp = 42.4% |
± | Very low | |
| Convergent validity | Camerota et al. (2018) [33] |
n = 82 Age = 3.6 ± 0.6 (2.7 to 5.2) months Sex = 43% girls |
Sleep quality: sleep onset time, rise time, sleep period, WASO (number and duration), TST, and longest sleep period Free-living (at home) |
Videosomnography to score sleep stages as sleep and wake | VG | Left ankle | Aw-ACTdef-uni-15 |
κ = .47, Se = 52%, Sp = 95% Sleep onset time: r = .79*, underestimated by 29 min***, d = .43 Rise time: r = .76* Sleep period: r = .78*, overestimated by 23.6 min*, d = .28 WASO: (number) r = .47*, underestimated by 1.1***, d = .54; (duration): r = .59*, overestimated by 58.4 min***, d = 72 TST: r = .54* Longest sleep period: r = .38*, overestimated by 35.5 min*, d = .28 |
- |
Moderate (level 2) |
| Greenspan et al. (2021) [29] |
n = 16 Age = 3.1 ± 1.1 (1.8 to 5) months Sex = 51% girls |
Body position: supine (parallel to floor stomach facing up), reclined (trunk tilted about 45° posteriorly from upright), upright (90°), inclined (trunk tilted about 45° anteriorly from upright), and prone (parallel to floor stomach facing down) Free-living (structured and free play) |
DVO to score body position by two independent raters using outlined definitions | VG | Trunk | GG-Gr-HA/VA/DA-1 |
κw = .84, 95% CI (.83 to .84) Supine: accuracy = 90.7%, rsp = .97*** Reclined: accuracy = 73.5%, rsp = .89*** Upright: accuracy = 83.1%, rsp = .97*** Inclined: accuracy = 41.4%, rsp = .67** Prone: accuracy = 78.4%, rsp = .96*** |
± |
Low (level 1) |
|
| Jun & Choi (2020) [40] |
n = 9 Age = 144 ± 284.5 (2 to 720) days Sex = 59.1% girls |
Activity type: sleeping (without substantial movement), strong movement (struggling with crying or in agony), weak movement (moving in comfy state), and movement by external force (from nurse or caregiver) Laboratory (at the hospital) |
DVO to score activity type by two independent raters using a 3-stage classification scheme | A | Chest | ICM-DNN-HA/VA/DA-4 |
accuracy = .96, F-score = .95, precision = .98, recall = .93, Sp = .98 Sleep: accuracy = .97, F-score = .99, precision = .99, recall = 1.0, Sp = .94 Strong movement: accuracy = .97, F-score = .95, precision = .96, recall = .94, Sp = .99 Weak movement: accuracy = .95, F-score = .93, precision = .97, recall = .90, Sp = .99 External force: accuracy = .95, F-score = .95, precision = 1.0, recall = .89, Sp = 1.0 |
+ |
Very low (level 1) |
|
| Airaksinen et al. (2020) [39] |
n = 22 Age = 6.7 ± 0.8 (4.5 to 7.7) months Sex = 59.1% girls |
Body position: prone (navel on floor), supine (lower back on floor), side left/right, crawl posture (supported by hands, and knees or feet); Movement: macro still (no movement), turn left/right (change of posture along prone-side-supine axis), pivot left/right (change of facing whole body direction, without movement), crawl proto (practice crawl without moving during prone/side posture and move multiple limbs during supine posture), crawl commando (crawl with forward movement) Laboratory (semi-structured) |
DVO to score body position and movement by three independent raters using a developed annotation scheme | A | Arms + legs; proximally | SM-CNN-VM-2 |
Movement track: F-score = 80% Full agreement: posture: accuracy = 99.1%, movement: accuracy = 90.7%; All frames: posture: accuracy = 98.2%, movement: accuracy = 81.7% Most frequent confusions in prone-side-supine axis as well as between crawl posture and prone Individual sensors lower performance (left arm posture: accuracy = 71%, movement: accuracy = 70%, left leg posture: accuracy = 90%, movement: accuracy = 68%) compared to four-sensor setup (posture: accuracy = 95%, movement: accuracy = 80%), and two-sensor setup (right leg + arm posture: accuracy = 94%, movement: accuracy = 78%; left leg + arm posture: accuracy = 95%, movement: accuracy = 79%; left + right arm posture: accuracy = 85%, movement: accuracy = 72%; left + right leg posture: accuracy = 93%, movement: accuracy = 72%) |
+ Arm: - Arms: ± Leg: ± Legs: ± Combined 2-sensor: ± ; 4-sensor: + |
Very low (level 1) |
|
| SM-SVM-VM-2 |
Movement track: F-score consistently 5–10% lower performance in prone positions (crawl proto*, turn right***; pivot left*) Posture classification comparable between CNN and SVM |
± | ||||||||
| Smith et al. (2015) [41] |
n = 12 Age = 6.8 ± 2.9 (1 to 12) months Sex = 66.7% girls |
Activity type: leg movement (change of limb position) Laboratory |
DVO to score activity type by one rater | D | Legs | Op-AAV-VM-n.r | accuracy = 92.7%, Se = 92.0% | + |
Very low (level 1) |
|
| Hewitt et al. (2019) [34] |
n = 32 Age = 15.2 ± 6.4 (4.7 to 24.9) weeks Sex = 40.6% girls |
Body position: prone on floor (tummy with both hips touching the floor), prone supported (held in prone, on parent’s chest), and non-prone (supine, left/right side lying, reclined in car seat/pram, upright, supported sitting, cradle hold) Laboratory (structured positions) |
DVO to score body position by one rater (one randomly chosen video was scored by four independent raters) using outlined definitions | D | Right hip | AG-He-VA/HA-1 |
Prone: accuracy = 90%, MD = -18.3 s, LoA (-97.0 to 60.3) Non-prone: accuracy = 99.9%, MD = -0.2 s, LoA (-1.2 to 0.9) Prone supported: accuracy = 63.6%, MD = -127.3 s, LoA (-324.7 to 70.2) |
± |
Very low (level 1) |
|
| GA-Ai-VA/HA-1 |
Prone: accuracy = 95.4%, MD = -8.4 s, LoA (-78.2—61.3) Non-prone: accuracy = 98%, MD = 31.2 s, LoA (-154.9 to 92.4) Prone supported: accuracy = 52.2%, MD = -166.9 s, LoA (-390.7 to 56.8) |
± | ||||||||
| Ankle | AG-He-VA/DA-1 |
Prone: accuracy = 87.9%, MD = -22.1 s, LoA (-124.0 to 79.7) Non-prone: accuracy = 96.3%, MD = -56.6 s, LoA (-209.5 to 96.3) Prone supported: accuracy = 53.3%, MD = -163.1 s, LoA (-431.7 to 105.6) |
± | |||||||
| Chest | MB-He-VA/HA/DA-1 |
Prone: accuracy = 79.2%, MD = -38 s, LoA (-194.5 to 118.5) Non-prone: accuracy = 99.9%, MD = 2.0 s, LoA (-14.0 to 10.8) Prone supported: accuracy = 66.1%, MD = -113 s, LoA (-355.6 to 129.6) |
- | |||||||
| Horger et al. (2021) [37] |
n = 9 Agestart = 7.96 ± 2.51 (0.89 to 8.19) months Ageend = 10.89 ± 1.14 (9.5 to 13.08) months Sex = 44.0% girls |
Sleep quality: sleep onset, morning wake time, WASO, sleep efficiency, and sleep duration Free-living (at home) |
Videosomnography to score sleep quality | D | Left ankle | MM-PSinf-uni-60 |
Sleep onset: rp= .94**, MD = 0.76 min, SD = 34.5 min Morning wake: rp= .74, MD = -14.1 min, SD = 40.4 min WASO: rp= .20, MD = 1.2, SD = 3.9 Sleep efficiency: rp= .30 Sleep duration: rp= .36 |
- |
Very low (level 2) |
|
| MM-PS-uni-60 |
Sleep onset: rp= .86** Morning wake: rp= .55 WASO: rp= .27 Sleep efficiency: rp= .51 Sleep duration: rp= .12 |
- | ||||||||
| Sadeh et al. (1995) [38] |
n = 41 (10 newborns; 11 3-month-olds; 10 6-month-olds; 10 12-month-olds) Age = 0 to 12 months Sex = 46.4% girls |
Sleep stage: sleep (active and quiet) and wake Free-living (newborns at hospital; others at home) |
DO using Thoman’s observation scheme (1975, 1995) to score sleep stage as sleep (active and quiet), wake, sleep–wake transition and uncertain | D | Left ankle | AMA-PS-uni-60 |
All infants: accuracy = 83.4% (sleep–wake = 95.6%; wake = 93.5%; active sleep = 74.9% and quiet sleep = 78.0%) (excl. 12-month-olds) Newborns: accuracy = 74.9% (wake = 82.8%; active sleep = 74.4.1%, quiet sleep = 54.9%) 3-month-olds: accuracy = 87.3% (wake = 92.5%, active sleep = 78.3%, quiet sleep = 87.2%; sleep–wake = 93.8%); 6-month-olds: accuracy = 83.2% (wake = 97.8%, active sleep = 66.4%, quiet sleep = 76.7%; sleep–wake = 97.9%); 12-month-olds: wake = 99.3%; sleep–wake = 97.2% Wake time: r (.85 to .99), % active sleep time: r (.78 to .98), % quiet sleep time: r (.36 to .85) (lowest correlations in newborns) Wake: MD (0.2 to 3.5%), sleep: MD (0.4 to 11.3%) |
± < 3 months: - > 3 months: + |
Very low (level 3) |
|
| Gnidovec, Neubauer, & Zidar (2002) [36] |
n = 10 Age = 1 to 6 months Sex = 40% girls |
Sleep stage: Sleep (active and quiet) and wake (active and quiet) Free-living (at home) |
DO using Thoman’s observation scheme (1990) to score sleep stage as sleep (active and quiet), wake (active and quiet), sleep–wake transition and uncertain | I | Left ankle | Gw-ASW-uni-10 |
1-month: accuracy = 72.0% (sleep = 88.7%, wake = 57.5%); 3-months: accuracy = 90.1% (sleep = 97.0%, wake = 84.5%); 6-months: accuracy = 95.0% (sleep = 88.4%, wake = 98.0%) After 3rd month 88.9% and 6th month 94.4% accuracy (calibration sample n = 5) Invalid discrimination between active- and quiet sleep all age groups < 75%, best for 3-month-olds (accuracy = 74.3%; active sleep: accuracy = 49.3%, quiet sleep: accuracy = 88.3%), as compared to 1-month (accuracy = 58.5%; active sleep: accuracy = 35.9%, quiet sleep: accuracy = 90.5%) and 6-months (accuracy = 66.5%; active sleep: accuracy = 39.9%, quiet sleep: accuracy = 87.1%) |
± 1 month: - > 3 months: + |
Very low (level 3) |
Abbreviations: AAV acceleration and angular velocity algorithm [41], Ac Actical, ACTdef Actiware software with default wake threshold value of .888 * mean acceleration, ACT40 Actiware software with wake threshold value of 40, ACT80 Actiware software with wake threshold value of 80, ASA40 Actiwatch activity and sleep analysis software with wake threshold value = 40, AG ActiGraph, Ai Activinsights software, AMA AMA-32, ASW automatic sleep wake scoring algorithm, Aw Actiwatch, CI confidence interval, CNN convolutional neural network, CS count-scaled algorithm [30], d Cohen’s d, DA diagonal axis (z-axis), DNN deep neural network, DO direct observation, DVO direct video observation, GA GENEActiv, GG get around garment with ADXL335, Gr Greenspan’s cut-points (2021) [29], Gw Gaewiler, HA horizontal axis (x-axis), He Hewitt’s cut-points (2019) [34], ICC intraclass correlation coefficient, ICM ICM20600 chip, κ Kappa, κw weighted Kappa, LoA limits of agreement, LVQ neural network learning vector quantization, MB MonBaby, MD mean difference,MM MicroMini sleep watch, mSCA miniature semiconductor chip accelerometer, n.r. not reported, omni omnidirectional, Op Opal APDM, PABAK prevalence- and bias-adjusted Kappa, PS probability scaled algorithm [38], PSinf probability scaled algorithm for infants [92], r correlation coefficient (unknown), rp correlation coefficient (Pearson), rsp correlation coefficient (Spearman rank), SD standard deviation, Se sensitivity, SM Suunto Movesense sensor, Sp specificity, SVM support vector machine, S0 zero-threshold computation [93], TST total sleep time, uni uniaxial (axis was not specified), VA vertical axis (y-axis), VM vector magnitude, WASO wake after sleep onset, WSC weighted sum activity algorithm [30], 1 1 s epoch, 2 2 s epoch, 4 4 s epoch, 10 10 s epoch, 15 15 s epoch, 30 30 s epoch, 60 60 s epoch
aAge presented as mean ± SD (range)
bMethodological study quality based on newly developed checklist: VG very good, A adequate, D doubtful, I inadequate
cDevice-based method described using code combinations of four elements resulting in the following format: brand-axis-approach-epoch length
dStudy result rating based on COSMIN guideline: + sufficient, ± inconsistent, - insufficient, ? intermediate
eQuality of evidence based on GRADE approach
*p < .05
**p < .01
***p < .001
No studies assessed validity of cut-points for SB, LPA and MVPA in infants, while for sleep no cut-points (i.e., wake thresholds) were evaluated as valid [30–33]. Quality of evidence was low for studies evaluating criterion validity, as results were retrieved in limited samples of 22 to 31 infants, despite very good methodological quality [30–32]. The results of the study that evaluated convergent validity, were insufficient, despite moderate quality of evidence [33].
In contrast, multi-parameter methods were more suitable for assessing the physical behavior of infants than a conventional cut-points based method. Infant leg movements could sufficiently be distinguished from non-infant produced movement using an algorithm describing velocity and acceleration magnitude for this activity [41]. However, these results received very low quality of evidence as methodological study quality was doubtful and the results were retrieved in a sample of only 12 infants.
For posture and movement classification, using arm and leg data, validity of convolutional neural networks was rated as sufficient [39]. The performance of convolutional neural networks and supported vector machines were comparable for classification of infant specific postures, e.g., tummy time and crawl posture. However, for movement in prone positions (e.g., crawl, turn and pivot) the performance of the convolutional neural networks was consistently 5 to 10% higher than the performance of support vector machines, resulting in a sufficient study result rating for the former and an inconsistent rating for the latter. Despite adequate methodological study quality, these results received low quality of evidence as the results were retrieved in a sample of 22 infants. Another neural network using chest data was rated as sufficient for sleep and movement classification [40]. Despite adequate methodological study quality, the results received very low quality of evidence as the results were retrieved in a sample of only nine infants.
Sleep could be distinguished from wake from 3-months of age using different multi-parameter methods [30, 36, 38]. Convergent validity of the Sadeh algorithm that calculates the probability of sleep, was rated as sufficient in free-living situations for infants [38]. However, it was less suitable to distinguish active and quiet sleep. These results received very low quality of evidence as the results were retrieved in a limited sample of 41 infants and methodological study quality was doubtful. Similarly, convergent validity of the automatic sleep–wake scoring algorithm developed for raw data was rated as sufficient to distinguish sleep from wake, despite low accuracy for distinguishing active from quiet sleep [36]. However, these results received very low quality of evidence as they were retrieved in a sample of only 10 infants and methodological study quality was inadequate. Galland and colleagues (2012) determined the accuracy of three algorithms for distinguishing sleep from wake states using 15-, 30- and 60 s epochs in infants with a mean age around 3-months [30]. In line with previous results, criterion validity of the Sadeh and the Cole-Kripke (computing the weighted sum activity) algorithm was rated as insufficient. However, criterion validity of an algorithm similar to the Cole-Kripke algorithm that uses count-scaled data (leg placement) was rated as sufficient in infants of around 3-months of age using 15 s or 30 s epochs. The best performing algorithm used a sampling epoch of 15 s. Sleep agreement of the other algorithms was highest using the 15- or 30 s epoch, however, at the expense of wake agreement. Notably, correspondence with polysomnography was poorest for the number of wake time after sleep onset using 60 s epochs. Despite very good methodological study quality, these results received low quality of evidence due to the limited sample size of 31 infants.
Toddlers
Table 4 summarizes the results of nine studies in toddlers that examined convergent validity [42–50]. No studies evaluated methods to distinguish sleep from wake.
Table 4.
Convergent validity of accelerometer-based methods for toddlers, sorted by methodological study quality, quality of evidence (level of evidence), and study result rating
| Study | Study populationa | Outcome(s) & Setting | Comparison measure(s) |
Method ological study qualityb |
Placement | Device-based methodc | Results | Study result ratingd |
Quality of evidencee (level of evidence) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Convergent validity | Kwon et al. (2019) [49] |
n = 21 Age = 25 ± 2.5 (13 to 35) months Sex = 50% girls |
Activity type: running (forward from one place to another), walking (forward from one place to another), climbing up/down (the stairs/foam climber), crawling (moving forward on two hands and two knees), riding a ride on toy (sitting on toy, moving forward using two feet), standing (without lifting a foot), sitting (on the ground), stroller (sit on stroller/wagon pushed by adult), and being carried (by adult while adult is walking) Free-living (free play in commercial indoor playroom) |
DVO using a developed coding scheme to score activity type by two independent raters | VG | Hip | AG-RF-VA/HA/DA/VM-5 |
Best differentiating features: DA FFT SD (d' = 0.64), DA FFT max (d' = 0.61), HA FFT SD (d' = 0.47). Feature importance all 78 features < 0.1 (highest: SD of VM 0.039). Top 10 ranked features: basic quantiles (e.g., min, median, max) of single axis direct values and FFT values RF: accuracy = 89%, precision = 88%, recall = 89%, F-score = .88 58% of carried labels were correctly (SB) classified, whereas 89% of ambulation was correctly classified |
+ |
Low (level 1) |
| Costa et al. (2014) [46] |
n = 20 Age = 2.99 ± 0.48 (2 to 3) years Sex = 60% girls |
Activity intensity: Total time in SB, LPA, and MVPA Laboratory (semi-structured activity sessions) |
DVO using CARS (modified) to score activity type and determine activity intensity (SB: stationary with no movement, and with movement of the limbs; LPA: slow/easy translocation; MVPA: translocation fast, and with moderate effort) by one rater (repeated after one month for random minute of each child) | VG | Right hip | AG-C-VM-5 |
Total PA: CCC = .80, MD = 48.0 s*, LoA (-217.9 to 121.9) SB: CCC = .74, MD = 48.0 s*, LoA (-121.9 to 217.9) LPA: CCC = .34, MD = -163.5 s***, LoA (-343.0 to 16.0) MVPA: CCC = .40, MD = 117.8 s***, LoA (-51.4 to 286.9) |
± (SB + ; PA -) |
Low (level 1) |
|
| AG-C-VA-5 |
Total PA: CCC = .84, MD = 5.3 s, LoA (-171.1 to 181.6) SB: CCC = .77, MD = -5.3 s, LoA (-181.6 to 171.1) LPA: CCC = .45***, MD = -112.5 s, LoA (-320.5 to 95.5) MVPA: CCC = .42, MD = 115.5 s***, LoA (-49.3 to 280.3) |
± (SB + ; PA -) |
||||||||
| AG-Pa-VA-15 |
Total PA: CCC = .71, MD = 50.5 s, LoA (-183.0 to 284.0) SB: CCC = .75, MD = -22.0 s, LoA (-209.7 to 165.7) LPA: CCC = .38, MD = -115.3 s**, LoA (-397.27 to 166.8) MVPA: CCC = .30, MD = 165.8 s***, LoA (-71.2 to 402.73) |
± (SB + ; PA -) |
||||||||
| AG-T12-VA-15 |
Total PA: CCC = .85, MD = 15.3 s, LoA (-152.4 to 182.9) SB: CCC = .79, MD = -15.3 s, LoA (-182.9 to 152.4) LPA: CCC = .36, MD = -150.5 s***, LoA (-391.1 to 90.1) MVPA: CCC = .30, MD = 165.8 s***, LoA (-71.2 to 402.7) |
± (SB + ; PA -) |
||||||||
| van Cauwenberghe et al. (2011) [45] |
n = 31 Age = 20 ± 4 (12 to 30) months Sex = 45.2% girls |
Activity intensity: SB, LPA and MVPA Free-living (out- & indoor free play at childcare) |
DVO using OSRAC-P to score activity type and derive activity intensity (SB: stationary and motionless, and stationary with limb/trunk movement; LPA: slow, easy movement; MVPA: moderate, and fast movement) by two independent raters | VG | Right hip | AG-cts-VA-15 |
mean rsp = .66*** epoch-by-epoch intensity level rsp = .52*** |
- |
Low (level 1) |
|
| AG-Pa-VA-15 |
accuracy = 58.3% SB: AUC-ROC = .71, Se = 67.0%, Sp = 75.4% LPA: AUC-ROC = .62, Se = 60.0%, Sp = 63.2% MVPA: AUC-ROC = .57, Se = 21.5%, Sp = 91.3% |
- (SB -; PA -) |
||||||||
| AG-Si3-VA-15 |
accuracy = 52.7% SB: AUC-ROC = .58, Se = 91.8%, Sp = 23.9% LPA: AUC-ROC = .52, Se = 14.6%, Sp = 89.0% MVPA: AUC-ROC = .53, Se = 8.9%, Sp = 97.1% |
- (SB -; PA -) |
||||||||
| AG-vC-VA-15 |
accuracy = 52.2% SB: AUC-ROC = .56, Se = 94.4%, Sp = 17.2% LPA: AUC-ROC = .51, Se = 9.0%, Sp = 93.7% MVPA: AUC-ROC = .53, Se = 10.0%, Sp = 96.9% |
- (SB -; PA -) |
||||||||
| Trost et al. (2012) [44] |
n = 18 Age = 2.3 ± 0.4 years Sex = 55.6% girls |
Activity intensity: SB, LPA and MVPA Free-living (regularly scheduled play) |
DVO using CARS (modified) to score activity type and determine activity intensity (SB: lying down or sitting; LPA: standing; MVPA: walking and running) by two raters | VG | Right hip | AG-T12-VA-15 |
SB: MD = -7.6***, LoA (-17.6to 2.3) LPA: MD = 7.2***, LoA (-2.0 to 16.3) MVPA: MD = 0.5, LoA (-2.6 to 3.5) |
? |
Low (level 1) |
|
| Pre-school cut-points: AG-Si/vC/Re/Pa/N-VA-15 | VG | Preschool and toddler cut-points overestimated SB*** and underestimated LPA***; Si** and vC ** underestimated MVPA; Pa (≥ 420) same trend as the toddler cut-point T12: MD = 0.5, 95% LoA (-2.5 to 3.5) | ? |
Low (level 2) |
||||||
| Albert et al. (2020) [48] |
n = 22 Age = 1.5 ± 0.5 (1.1 to 2) years Sex = 54.6% girls |
Activity type: Run/walk, crawl, climb, stand, sit, lie down, carried, and stroller as defined by Kwon et al. (2019)[49] Free-living (guided play) |
DVO using a developed coding scheme to score activity type by three independent raters | A | Waist | AG-RF-HA/VA/DA-2 |
accuracy = 63.8% RF + HMM: accuracy = 64.8% Run/walk: recall = 80.0%, precision = 88.2% Crawl: recall = 81.2%, precision = 68.3% Climb: recall = 56.0%, precision = 29.0% Stand: recall = 45.4%, precision = 49.2% Sit: recall = 66.6%, precision = 66.9% Lie down: recall = 61.7%, precision = 76.0% Carried: recall = 58.8%, precision = 43.5% Stroller: recall = 28.2%, precision = 41.0% Sit, stand and stroller collapsed: accuracy = 79.3% |
- |
Very low (level 1) |
|
| AG-SVM-HA/VA/DA-2 |
accuracy = 58.6% SVM + HMM: accuracy = 60.1% |
- | ||||||||
| AG-LR-HA/VA/DA-2 |
accuracy = 57.0% LR + HMM: accuracy = 59.1% |
- | ||||||||
| AG-J48-HA/VA/DA-2 |
accuracy = 57.3% J48 + HMM: accuracy = 57.5% |
- | ||||||||
| AG-kNN-HA/VA/DA-2 |
accuracy = 52.6% kNN + HMM: accuracy = 54.1% |
- | ||||||||
| Pulakka et al. (2013) [43] |
Validation n = 40 Age = 16.9 ± 5.8 (16.0 to 18.3) months Sex = 60% girls Cross-validation n = 30 Age = 17.0 ± 0.6 (16 to 18.5) months Sex = 60% girls |
Activity intensity: SB, LPA, MPA, and VPA Free-living (free play sessions |
DVO using CPAF to score activity type and derive activity intensity (SB: stationary, no movement; LPA: stationary, limb movement, MPA: slow trunk movement; VPA: rapid trunk movement) by one rater (and 19.5% of the videos by a second rater) | D | Right hip | AG-Pul-VM-15 |
Validation SB vs. LPA: AUC-ROC = .73, CI (.67 to .80) VPA vs. MPA: AUC-ROC = .67, CI (.56 to .78) SB vs LPA and MVPA: AUC-ROC = .98, CI (.97 to .99) LPA vs. MPA: AUC-ROC = .94, CI (.91 to .97) Cross-validation SB and LPA vs. MVPA: accuracy = 92%, Se = 94.2%, Sp = 90.9%, κ = .83 |
+ (SB + ; PA ±) |
Very low (level 1) |
|
| AG-Pul-VA-15 |
Validation SB vs. LPA: AUC-ROC = .62, CI (.56 to .67) VPA vs. MPA: AUC-ROC = .59, CI (.47 to .72) SB vs. LPA and MVPA: AUC-ROC = .95, CI (.93 to .96) LPA vs. MPA: AUC-ROC = . 90, CI (.87 to .94) Cross-validation SB and LPA vs. MVPA: accuracy = 84%, Se = 84.1%, Sp = 84.6%, κ = .67 |
± (SB + ; PA ±) |
||||||||
| Hager et al. (2016) [42] |
n = 24 Age = 24.5 ± 5.2 (14.7 to 35.5) months Sex = 41.7% girls |
Activity intensity: SB, LPA, and MVPA Laboratory (structured activities) |
DO using CARS to score activity type and derive activity intensity (SB: stationary with no movement; LPA: stationary with movement of the limbs, and slow/easy translocation; MVPA: translocation fast, and with moderate effort) by one rater | D | Left ankle | Ac-Ha-omni-30 |
rsp = .75 SB: Se = 81.8%, Sp = 77.5%; LPA: Se = 61.7%, Sp = 84.7%; MVPA: Se = 85.7%, Sp = 88.4% |
± (SB ± ; PA +) |
Very low (level 2) |
|
| Oftedal et al. (2014) [47] |
n = 10 Age = 29 ± 6 months Sex = 50% girls |
Activity intensity: SB and non-SB Laboratory (semi-structured activity sessions) |
DVO using DO software Behavioral Evaluation Strategy and Taxonomy to score activity type and determine activity intensity (SB: lying/sitting with(out) limb movement, and standing still) by one rater | I | Waist | AG–O-VM-5 |
Se = 82%, Sp = 83% bias = -5.1%, LoA (-27.5 to 16.1%) |
SB: + |
Very low (level 1) |
|
| AG–O-VA-5 | Se = 76%, Sp = 93%, bias = -17.3%, LoA (-44.3 to 8.3%)* | SB: ± | ||||||||
| Nam & Park (2013) [50] |
n = 10 Age = 22.4 ± 3.3 (16 to 29) months Sex = 50% girls |
Activity type: Wiggling, rolling, standing still, standing up, sitting down, walking, toddling, crawling, climbing up/down, and stopping (precise definitions not indicated) Laboratory (simulated real home environment) |
DVO to score activity type by one rater | I | Hip | mSCA-DT- VA/HA/DA/VM-n.r | accuracy = 74.0% (39.5 to 97.2%) | ± |
Very low (level 1) |
|
| mSCA-NB- VA/HA/DA/VM-n.r | accuracy = 73.0% (28.0 to 90.9%) | - | ||||||||
| mSCA-BN-VA/HA/DA/VM-n.r | accuracy = 84.8% (57.8 to 98.9%) | + | ||||||||
| mSCA-SVM-VA/HA/DA/VM-n.r | accuracy = 86.2% (39.8 to 99.9%) | + | ||||||||
| mSCA-kNN-VA/HA/DA/VM-n.r | accuracy = 84.1% (67.8 to 94.6%) | + | ||||||||
| mSCA-J48-VA/HA/DA/VM-n.r | accuracy = 88.3% (71.7 to 98.7%) | + | ||||||||
| mSCA-MLP-VA/HA/DA/VM-n.r | accuracy = 84.8% (52.5 to 99.5%) | ± | ||||||||
| mSCA-MLR-VA/HA/DA/VM-n.r | accuracy = 86.9% (72.1 to 98.7%) | + |
Abbreviations: Ac Actical, AUC-ROC area under the receiver operating curve, AG ActiGraph, cts counts, BN Bayes net, C Costa’s cut-points (2014) [46], CARS children’s activity rating system, CCC concordance correlation coefficient, CI confidence interval, CPAF children’s physical activity form, d’ discriminability index, DA diagonal axis (z-axis), DO direct observation, DVO direct video observation, FFT fast Fourier transform, Ha Hager’s cut-points (2014) [42], HMM hidden Markov model, J48 decision tree (pruned), κ Kappa, kNN k-nearest neighbors, LoA limits of agreement, LPA light physical activity, LR logistic regression, MD mean difference, MLP multi-layer perceptron network, MLR multinomial logistic regression, MPA moderate physical activity, mSCA miniature semiconductor chip accelerometer, MVPA moderate-to-vigorous physical activity, N NHANES cut-points [88], NB naïve Bayes, n.r. not reported, O Oftedal’s cut-points (2014) [47], omni omnidirectional, OSRAC-P observational system for recording physical activity in children preschool, Pa Pate’s cut-points (2006) [52], PA physical activity, Pul Pulakka’s cut-points (2013) [43], Re Reilly’s cut-points (2003)[80], RF random forests, rsp correlation coefficient (Spearman rank), SB sedentary behavior, SD standard deviation, Se sensitivity, Si Sirard’s age-specific cut-points (2005) [81], Si3 Sirard’s cut-points (2005) for 3-year-olds [81], Sp specificity, SVM support vector machine, T12 Trost’s cut-points (2012) [44], VA vertical axis (y-axis), vC van Cauwenberghe’s cut-points (2011) [45], VM vector magnitude, VPA vigorous physical activity, 5 5 s epoch, 15 15 s epoch, 30 30 s epoch
aAge presented as mean ± SD (range)
bMethodological study quality based on newly developed checklist: VG very good, A adequate, D doubtful, I inadequate
cDevice-based method described using code combinations of four elements resulting in the following format: brand-axis-approach-epoch length
dStudy result rating based on COSMIN guideline: + sufficient, ± inconsistent, - insufficient, ? intermediate
eQuality of evidence based on GRADE approach
* p < .05
** p < .01
*** p < .001
For the assessment of SB, LPA and MVPA no valid cut-point sets were found. Four studies evaluated the convergent validity of cut-points based methods for accelerometers using direct (video) observation as comparison measure [43, 44, 46, 47]. These studies suggested that cut-points can be used to distinguish SB [46, 47] or low intensity [43, 44] from high intensity PA. Cut-points to distinguish SB and LPA from MVPA were rated as sufficient, with MVPA for the vector magnitude (VM) ≥ 208 counts/15 s (Mage = 1.42 ± 0.05 years) [43], or for the VA ≥ 418 counts/15 s (Mage = 2.30 ± 0.40 years) [44]. In contrast, cut-points to distinguish SB from total PA were rated as sufficient, for the VM with SB < 6 counts/5 s (Mage = 2.99 ± 0.48 years) [46], or < 40 counts/5 s [47]. These results seemed promising as high agreement and low bias were found, but the results of these studies received low [44, 46] to very low [43, 47] quality of evidence due to small sample sizes (10 ≥ n ≤ 40), despite very good methodological quality of two studies [44, 46].
Using a multi-parameter method, SB (e.g., carrying) could be sufficiently distinguished from ambulation PA (e.g., running, crawling, and climbing) using time-domain and frequency acceleration signal features. Convergent validity of this random forests was rated as sufficient [49]. However, these results received low quality of evidence as the results were retrieved in a sample of only 21 toddlers, despite very good methodological study quality. In another study, compared to other multi-parameter methods, random forests provided the best classification of activity type (i.e., running/walking, crawling, climbing, standing, sitting, lying down, carried and stroller) [48]. To improve accuracy, the models were augmented by a hidden Markov model by providing the predictions of the models as observations. Despite small improvements, study results were rated as insufficient.
Preschoolers
Table 5 summarizes the results for validity, of which ten studies examined criterion validity [51–55, 66, 67, 75, 84, 88] and thirty studies examined convergent validity [51, 56–64, 68–74, 76–83, 85–87, 89, 90] in preschoolers.
Table 5.
Criterion and convergent validity of accelerometer-based methods for preschoolers, sorted by methodological study quality, quality of evidence (level of evidence), and study result rating
| Study | Study populationa | Outcome(s) & Setting | Comparison measure(s) |
Method ological study qualityb |
Placement | Device-based methodc | Results | Study result ratingd |
Quality of evidencee (level of evidence) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Criterion validity | Adolph et al. (2012) [51] |
n = 64 Age = 4.5 ± 0.8 (3 to 5) years Sex = 42.2% girls |
cpm Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 method to determine AEE | VG | Chest | Ah-cts-uni-60 | r = .72*** | + | Moderate |
| Right hip | RT-cts-VM-60 | r = .80** | + | |||||||
| RT-cts-VA-60 | r = .80** | + | ||||||||
| RT-cts-HA-60 | r = .78** | + | ||||||||
| RT-cts-DA-60 | r = .74** | + | ||||||||
| Zakeri et al. (2013) [55] |
n = 69 Age = 4.6 ± 1.0 (3 to 5) years Sex = 50.7% girls |
Minute-by-minute EE Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine EE | VG | Right hip | AG-cts-VA-60 | r = .76*** | + | Moderate | |
| AG-cts-HA-60 | r = .74*** | + | ||||||||
| AG-cts-DA-60 | r = .76*** | + | ||||||||
| AG-CSTS-VA/HA/DA/VM-60 | MAPE = 0.3 ± 6.9%, CCC = .93 | + | ||||||||
| AG-MARS-VA/HA/DA/VM-60 | MAPE = 0.3 ± 4.8%, CCC = .95 | + | ||||||||
| Bélanger et al. (2013) [66] |
n = 12 Age = 3.1 ± 1.0 (2 to 5) years Sex = 66.7% girls |
Sleep quality: sleep latency, TST, WASO (number), and sleep efficiency Free-living (at home) |
Polysomnography to score sleep stages as sleep and wake | VG |
Non-dominant wrist (raw data) |
Aw-AS-VA-30 |
Sleep latency: ICC = .96** TST: ICC = .94**, overestimated by 13 min** WASO: ICC = .28, underestimated by 20** Sleep efficiency: ICC = .76**, overestimated by 2 min* Se = 98.7%, Sp = 58.7%, accuracy = 95.6%, NVP = 81.0% |
+ | Low | |
| Aw-ACT40-VA-30 |
Sleep latency: ICC = .92** TST: ICC = .94**, underestimated by 25 min** WASO: ICC = .42, overestimated by 37** Sleep efficiency: ICC = .73**, underestimated by 4 min** Se = 92.7%, Sp = 69.9%, accuracy = 90.7%, NVP = 47.4% |
± | ||||||||
| Aw-ACT80-VA-30 |
Sleep latency: ICC = .92** TST: ICC = .95* WASO: ICC = .32, overestimated by 25** Sleep efficiency: ICC = .70** Se = 95.8%, Sp = 56.7%, accuracy = 92.4%, NVP = 55.0% |
± | ||||||||
|
Non-dominant wrist (adjusted data) |
Aw-ACT40-VA-30 |
Sleep latency: ICC = .96** TST: ICC = .94**, underestimated by 58 min** WASO: ICC = .28, overestimated by 35** Sleep efficiency: ICC = .76**, underestimated by 9.4 min** Se = 87.9%, Sp = 81.0%, accuracy = 87.5%, NVP = 39.4% |
+ | |||||||
| Aw-ACT80-VA-30 |
Sleep latency: ICC = .96** TST: ICC = .97**, underestimated by 21.5 min** WASO: ICC = .36, overestimated by 34** Sleep efficiency: ICC = .82**, underestimated by 3.5 min** Se = 93.4%, Sp = 70.9%, accuracy = 91.4%, NVP = 49.6% |
+ | ||||||||
| Aw-AS-VA-30 |
Sleep latency: ICC = .93** TST: ICC = .98** WASO: ICC = .36, underestimated by 20** Sleep efficiency: ICC = .90** Se = 97.7%, Sp = 61.2%, accuracy = 95.0%, NVP = 72.1% |
± | ||||||||
| Left ankle | Aw-ACT40-VA-30 |
Sleep latency: ICC = .83** TST: ICC = .94**, underestimated by > 25 min** WASO: ICC = .01, overestimated by 36** Sleep efficiency: ICC = .80**, underestimated by 6.5 min** Se = 90.5%, Sp = 75.1%, accuracy = 89.3%, NVP = 41.7% |
± | |||||||
| Aw-ACT80-VA-30 |
Sleep latency: ICC = .85** TST: ICC = .95** WASO: ICC = .09, overestimated by 28** Sleep efficiency: ICC = .81** Se = 95.0%, Sp = 65.0%, accuracy = 92.1%, NVP = 53.7% |
± | ||||||||
| Aw-AS-VA-30 |
Sleep latency: ICC = .81** TST: ICC = .91** WASO: ICC = .14, underestimated by 20** Sleep efficiency: ICC = .77** Se = 97.6%, Sp = 57.7%, accuracy = 94.6%, NVP = 76.8% |
± | ||||||||
| Roscoe, James, & Duncan (2017) [67] |
n = 21 Age = 4.7 ± 0.5 (4 to 5) years Sex = 38.1% girls |
Activity intensity: SB (< 2 METs), LPA (2–2.99 METs), and MPA (3–5.99 METs) Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine EE | VG | Non-dominant wrist | GA-Ro-VM-60 |
SB: AUC-ROC = .99, 95% CI (.98 to 1.0), Se = 90%, Sp = 90% LPA: AUC-ROC = .75, 95% CI (.65 to .85), Se = 40%, Sp = 20% MPA: AUC-ROC = .92, 95% CI (.86 to .98), Se = 86%, Sp = 40% |
± (SB + ; PA -) |
Low | |
| Dominant wrist | GA-Ro-VM-60 |
SB: AUC-ROC = .99, 95% CI (.97 to 1.0), Se = 100%, Sp = 10% LPA: AUC-ROC = .76, 95% CI (.60 to .86), Se = 10%, Sp = 85% MPA: AUC-ROC = .90, 95% CI (.83 to .96), Se = 76%, Sp = 40% |
- (SB ± ; PA -) |
|||||||
| Pfeiffer et al. (2006) [53] |
n = 18 Age = 4.4 ± 0.7 (3 to 5) years Sex = 61.0% girls |
cpm Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 | VG | Right hip | Ac-cts-omni-60 |
Validation r = .89, rsp = .90, R2 = .96, SE = 3.02, AIC = 435.9, ICC = .59, rsp = .80*** |
+ | Very low | |
|
Activity intensity: MPA and VPA Free-living (in- and outdoor activities at preschool) |
D | Ac-Pf-omni-60 |
Cross-validation MPA: accuracy = 73%, κ = .40, modified κ = .46 VPA: accuracy = 85%, κ = .26, modified κ = .71 |
PA: ± | ||||||
| Pate et al. (2006) [52] |
n = 29 Age = 4.4 ± 0.8 (3.3 to 5.9) years Sex = 46.2% girls |
cpm Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine EE | VG | Right hip | AG-cts-VA-60 |
Validation rp = .82, R2 = .90, SE = 4.70, AIC = 735.8, ICC = .57, rsp = .66*** |
± | Very low | |
|
Activity intensity: MVPA and VPA Free-living (in- and outdoor activities at preschool) |
D | AG-Pa-VA-60 |
Cross-validation MVPA: accuracy = 69%, Se = 96.6%, Sp = 86.2% κ = .36, modified κ = .38 VPA: accuracy = 81%, Se = 65.5%, Sp = 95.4%, κ = .13, modified κ = .62 |
PA: - | ||||||
| Sijtsma et al. (2013) [54] |
n = 30 Age = 3.4 ± 0.3 (3.1 to 4.4) years Sex = 60.0% girls |
Mean activity cpm (ACM) and mean total activity counts per day (ACD) Free-living (at home for 5 days) |
Indirect calorimetry using DLW to determine TEE; breath-by-breath VO2 and VCO2 to determine SMR to calculate PAL and AEE |
D | Middle lower back | TD-cts-tri-60 |
PAL: ACM rp = .61**, ACD rp = 46* - ACM, gender & weight, R2 = .50*; ACD, height, gender & sleep duration, R2 = .48* AEE: ACM rp = .56*, ACD rp = .38 - ACM, R2 = .31*; ACD, gender & sleep duration, R2 = .39* TEE: ACM rp = .34, ACD rp = .21 - Multivariate models with ACM & SMR or ACM, ACD & sleep duration not significant Using 5 or 3 days of data did not provide different results for PAL estimation, MD = -0.02 ± 0.07, LoA (-0.16 to 0.11) |
- | Very low | |
| Ahmadi et al. (2020) [84] |
n = 31 Age = 4.1 ± 1.0 (3 to 5) years Sex = 20% girls |
EE Free-living (free play) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine EE | A | Non-dominant wrist | AG-RF-VM-10 |
Free-living (FL) model: RMSE = 0.63 (SD = 0.47) kcal/min, RMSE = 0.96 (SD = 0.67) METs, MAPE = 27.4% (SD = 14.0) Retrained lab (RL) model: RMSE = 0.66 (SD = 0.47) kcal/min, RMSE = 1.01 (SD = 0.67) METs, MAPE = 28.3% (SD = 15.0) Existing lab, FL and RL models: mean bias not different from zero, predicted EE within ± 6% of measured EE |
? | Very low | |
| AG-SVM-VM-10 |
Free-living (FL) model: RMSE = 0.64 (SD = 0.51) kcal/min, RMSE = 0.99 (SD = 0.73) METs, MAPE = 25.4% (SD = 12.2) Retrained lab (RL) model: RMSE = 0.65 (SD = 0.54) kcal/min, RMSE = 0.99 (SD = 0.77) METs, MAPE = 26.0% (SD = 12.6) Existing lab, FL and RL models: mean bias not different from zero, predicted EE within ± 6% of measured EE |
? | ||||||||
| Right hip | AG-RF-VM-10 |
Free-living (FL) model: RMSE = 0.63 (SD = 0.42) kcal/min, RMSE = 0.96 (SD = 0.59) METs, MAPE = 28.1% (SD = 12.0) Retrained lab (RL) model: RMSE = 0.67 (SD = 0.41) kcal/min, RMSE = 1.02 (SD = 0.57) METs, MAPE = 28.3% (SD = 12.7) FL and RL models: EE overestimated during play sessions with low total EE and underestimated during sessions with high total EE Existing lab models: mean bias not different from zero, predicted EE within ± 6% of measured EE |
? | |||||||
| AG-ANN-VM-10 |
Free-living (FL) model: RMSE = 0.63 (SD = 0.43) kcal/min, RMSE = 0.96 (SD = 0.61) METs, MAPE = 27.1% (SD = 11.1) Retrained lab (RL) model: RMSE = 0.65 (SD = 0.44) kcal/min, RMSE = 0.99 (SD = 0.62) METs, MAPE = 28.4% (SD = 11.8) Existing lab, FL and RL models: EE overestimated during play sessions with low total EE and underestimated during sessions with high total EE |
? | ||||||||
| Steenbock et al. (2019) [88] |
n = 41 Age = 4.8 ± 0.8 (3 to 6) years Sex = 46% girls |
Absolute (kJ/min) and relative (kg/min/J) EE Free-living (in- and outdoor semi-structured activities at school) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine EE | A | Right hip | AG-LM- HA/VA/DA-30 | RMSE = 2.91 (SD = 0.95) kJ/min, RMSE = 124.91 (SD = 30.58) J/min/kg, RMSE = 1.70 (SD = 0.39) METs | ? | Very low | |
| AG-MLM- HA/VA/DA-30 | RMSE = 2.91 (SD = 0.99) kJ/min, RMSE = 125.40 (SD = 31.50) J/min/kg, RMSE = 1.70 (SD = 0.40) METs | ? | ||||||||
| AG-RF- HA/VA/DA-30 | RMSE = 2.74 (SD = 0.96) kJ/min, RMSE = 115.56 (SD = 27.35) J/min/kg, RMSE = 1.56 (SD = 0.36) METs | ? | ||||||||
| AG-ANN- HA/VA/DA-30 | RMSE = 2.86 (SD = 0.95) kJ/min, RMSE = 121.51 (SD = 29.57) J/min/kg, RMSE = 1.66 (SD = 0.39) METs | ? | ||||||||
| GA-LM- HA/VA/DA-30 | RMSE = 2.89 (SD = 0.95) kJ/min, RMSE = 123.79 (SD = 31.28) J/min/kg, RMSE = 1.68 (SD = 0.39) METs | ? | ||||||||
| GA-MLM- HA/VA/DA-30 | RMSE = 2.90 (SD = 0.98) kJ/min, RMSE = 124.70 (SD = 32.95) J/min/kg, RMSE = 1.69 (SD = 0.42) METs | ? | ||||||||
| GA-RF- HA/VA/DA-30 | RMSE = 2.73 (SD = 1.00) kJ/min, RMSE = 112.57 (SD = 28.83) J/min/kg, RMSE = 1.53 (SD = 0.38) METs | ? | ||||||||
| GA-ANN- HA/VA/DA-30 | RMSE = 2.83 (SD = 0.98) kJ/min, RMSE = 118.04 (SD = 29.80) J/min/kg, RMSE = 1.66 (SD = 0.43) METs | ? | ||||||||
| Left hip | AG-LM- HA/VA/DA-30 | RMSE = 2.84 (SD = 0.94) kJ/min, RMSE = 123.64 (SD = 31.82) J/min/kg, RMSE = 1.67 (SD = 0.41) METs | ? | |||||||
| AG-MLM- HA/VA/DA-30 | RMSE = 2.81 (SD = 0.99) kJ/min, RMSE = 123.58 (SD = 31.94) J/min/kg, RMSE = 1.67 (SD = 0.41) METs | ? | ||||||||
| AG-RF- HA/VA/DA-30 | RMSE = 2.60 (SD = 0.97) kJ/min, RMSE = 112.32 (SD = 28.40) J/min/kg, RMSE = 1.52 (SD = 0.38) METs | ? | ||||||||
| AG-ANN- HA/VA/DA-30 | RMSE = 2.78 (SD = 1.01) kJ/min, RMSE = 116.89 (SD = 28.41) J/min/kg, RMSE = 1.63 (SD = 0.42) METs | ? | ||||||||
| Right wrist | GA-LM- HA/VA/DA-30 | RMSE = 2.85 (SD = 0.83) kJ/min, RMSE = 125.60 (SD = 28.52) J/min/kg, RMSE = 1.69 (SD = 0.38) METs | ? | |||||||
| GA-MLM- HA/VA/DA-30 | RMSE = 2.83 (SD = 0.87) kJ/min, RMSE = 125.42 (SD = 28.74) J/min/kg, RMSE = 1.69 (SD = 0.38) METs | ? | ||||||||
| GA-RF- HA/VA/DA-30 | RMSE = 2.56 (SD = 0.83) kJ/min, RMSE = 109.34 (SD = 26.98) J/min/kg, RMSE = 1.48 (SD = 0.37) METs | ? | ||||||||
| GA-ANN- HA/VA/DA-30 | RMSE = 2.74 (SD = 0.88) kJ/min, RMSE = 115.91 (SD = 28.55) J/min/kg, RMSE = 1.62 (SD = 0.40) METs | ? | ||||||||
| Non-dominant wrist | GA-LM- HA/VA/DA-30 | RMSE = 2.83 (SD = 0.86) kJ/min, RMSE = 125.21 (SD = 27.38) J/min/kg, RMSE = 1.70 (SD = 0.37) METs | ? | |||||||
| GA-MLM- HA/VA/DA-30 |
RMSE = 2.83 (SD = 0.89) kJ/min, RMSE = 124.91 (SD = 27.58) J/min/kg, RMSE = 1.69 (SD = 0.38) METs |
? | ||||||||
| GA-RF- HA/VA/DA-30 | RMSE = 2.56 (SD = 0.83) kJ/min, RMSE = 108.64 (SD = 26.33) J/min/kg, RMSE = 1.47 (SD = 0.36) METs | ? | ||||||||
| GA-ANN- HA/VA/DA-30 | RMSE = 2.72 (SD = 0.91) kJ/min, RMSE = 114.01 (SD = 27.88) J/min/kg, RMSE = 1.61 (SD = 0.44) METs | ? | ||||||||
| Right thigh | aP-LM- HA/VA/DA-30 | RMSE = 2.94 (SD = 0.91) kJ/min, RMSE = 126.22 (SD = 29.46) J/min/kg, RMSE = 1.69 (SD = 0.38) METs | ? | |||||||
| aP-MLM- HA/VA/DA-30 | RMSE = 2.92 (SD = 0.95) kJ/min, RMSE = 125.96 (SD = 29.86) J/min/kg, RMSE = 1.69 (SD = 0.39) METs | ? | ||||||||
| aP-RF- HA/VA/DA-30 | RMSE = 2.76 (SD = 0.94) kJ/min, RMSE = 115.61 (SD = 27.93) J/min/kg, RMSE = 1.56 (SD = 0.38) METs | ? | ||||||||
| aP-ANN- HA/VA/DA-30 | RMSE = 3.08 (SD = 1.00) kJ/min, RMSE = 125.98 (SD = 31.50) J/min/kg, RMSE = 1.81 (SD = 0.40) METs | ? | ||||||||
| Butte et al. (2014) [75] |
n = 50 Age = 4.5 ± 0.8 (3 to 5) years Sex = 50.0% girls |
cpm Laboratory (structured activities) |
Indirect calorimetry using breath-by-breath VO2 and VCO2 to determine minute-by-minute EE | I | Right hip | AG-CSTS-VA/HA/DA/VM-60 | MAPE = -0.2 ± 6.7%, MAE = -0.005 ± 0.07 kcal/min, RMSE = 0.07 kcal/min, R2 = .88 | + | Very low | |
| AG-MARS-VA/HA/DA/VM-60 | MAPE = 1.1 ± 6.6%, MAE = 0.009 ± 0.07 kcal/min, RMSE = 0.07 kcal/min | ? | ||||||||
|
n = 105 Age = 4.6 ± 0.9 years Sex = 66.7% girls |
Activity intensity: SB, LPA, MPA, and VPA Free-living |
Indirect calorimetry using DLW to determine AEE | I | AG-B-VM-60 |
accuracy = 70% SB: Sp = 83% LPA: Sp = 64% MPA: Sp = 35% VPA: Sp = 38% MVPA collapsed: accuracy = 74% |
- (SB + ; PA -) |
||||
| AG-B-HA-60 |
accuracy = 68% SB: Sp = 82% LPA: Sp = 58% MPA: Sp = 37% VPA: Sp = 27% MVPA collapsed: accuracy = 71% |
- (SB + ; PA -) |
||||||||
| Chest | Ah-B-HA-60 |
accuracy = 70%; Sp: SB: Sp = 81% LPA: Sp = 64% MPA: Sp = 48% VPA: Sp = 39% MVPA collapsed: accuracy = 74% |
- (SB + ; PA -) |
|||||||
| Convergent validity | Sirard et al. (2005) [81] |
n = 269 (n = 69 3-, n = 125 4-, n = 75 5-year-olds) Sex = 58% 3-, 52% 4-, 52% 5-year-old girls |
Activity intensity: SB, LPA, MPA and VPA Free-living (at preschool) |
DVO using CARS to score activity type and derive activity intensity (SB: stationary, motionless or with trunk/limb movements; LPA: slow/easy movement; MPA: moderate movement; VPA: fast movement) by a single rater (beginning and end of video by four additional raters) | VG | Right hip | AG-Si-VA-15 |
Total counts: rp = .58*** SB: rp = .70***, Se (94.4 to 100%), Sp (91.7 to 100%) LPA: rp = .59*** VPA: rp = .61***, Se (95.8 to 100%), Sp (80.0 to 83.3%) MPA: rp = .50***, Se (86.7 to 94.4%), Sp (66.7 to 100%) MVPA: rp = .46*** |
+ (SB + ; PA +) |
High (level 1) |
| Peirera et al. (2020) [74] |
n = 60 Age = 2.7 ± 0.4 (1.8 to 3.5) years Sex = 50% girls |
% time spent in SB Free-living (at childcare) |
aP-PRE-uni-n.r. at right thigh (SB: sitting/lying) |
VG | Hip | All outside the ± 10% equivalent interval of (-4.05 to 4.05) |
Moderate (level 2) |
|||
| AG-C-VA-5 | bias = -5.11, 90% CI (-7.90 to -2.32) | ? | ||||||||
| AG-Ev-VA-15 | bias = 8.15, 90% CI (5.44 to 10.86) | ? | ||||||||
| AG-T12-VA-15 | bias = 4.46, 90% CI (1.65 to 7.28) | ? | ||||||||
| AG-K-VA-15 | bias = -7.95, 90% CI (-11.01 to -4.89) | ? | ||||||||
| AG-Pa-VA-15 | bias = 6.17, 90% CI (3.40 to 8.93) | ? | ||||||||
| AG-Pa2-VA-15 | bias = -9.26, 90% CI (-12.32 to -6.21) | ? | ||||||||
| AG-Re-VA-60 | bias = -40.52, 90% CI (-43.82 to -37.22) | ? | ||||||||
| AG-Si-VA-15 | bias = -15.07, 90% CI (-18.16 to -11.97) | ? | ||||||||
| AG-vC-VA-15 | bias = -18.71, 90% CI (-21.89 to -15.54) | ? | ||||||||
| Dobell et al. (2019) [58] |
n = 62 Age = 3.5 ± 0.5 (3 to 5) years Sex = 45.5% girls |
Activity intensity: SB, LPA, and MVPA Free-living (free-play in nursery) |
DO using OSRAC-P (modified) to score activity type and derive activity intensity (SB: stationary/ motionless; LPA: stationary torso with limb and slow/easy movement; MVPA: moderate and fast movement) by two independent raters | VG | Non-dominant wrist | AG-cts-VM-5/10/15/30 |
rsp = .34, R2 = .11* (5 s) to rsp = .48, R2 = .23* (30 s) SB: AUC-ROC (.71 to .78), Se (.64 to .68), Sp (.64 to .78) LPA: AUC-ROC (.55 to .56), Se (.74 to .80), Sp (.33 to .43) MVPA: AUC-ROC (.67 to .78), Se (.63 to .80), Sp (.80 to .82) |
- (SB -; PA -) |
Moderate (level 2) |
|
| Right hip | AG-cts-VA-5/10/15/30 |
rsp = .38, R2 = .16* (5 s) to rsp = .52, R2 = .27* (10 s) SB: AUC-ROC (.69 to .77), Se (.61 to .72), Sp (.69 to .72) LPA: AUC-ROC (.53 to .54), Se (.59 to .76), Sp (.39 to .50) MVPA: AUC-ROC (.71 to .81), Se (.55 to .70), Sp (.77 to .79) |
- (SB -; PA -) |
|||||||
| AG-cts-VM-5/10/15/30 |
rsp = .40, R2 = .16* (5 s) to rsp = .55, R2 = .30* (30 s) SB: AUC-ROC (.73 to .79), Se (.69 to .72), Sp (.67 to .75) LPA: AUC-ROC = .55, Se (.78 to .82), Sp (.35 to .36) MVPA: AUC-ROC (.72 to .82), Se (.68 to .78), Sp (.62 to .79) |
- (SB -; PA -) |
||||||||
| Ahmadi, Pavey, & Trost (2020) [85] |
n = 31 Age = 4.0 ± 0.9 (3 to 5) years Sex = 29.0% girls |
Activity intensity: SB, LPA, MVPA, run and walk Free-living (20 min active play session) |
DVO using customized scheme to score activity type and derive activity intensity (SB: sitting/lying down, and stationary, motionless; LPA: standing, stationary, movement of the limbs/trunk, easy translocation, MPA: moderate and fast translocation; walk: translocation, medium speed; run: translocation (very) fast) | VG | Right hip | AG-RF-VM-1 |
Time and frequency features: F-score = 70.6%, + temporal features: F-score = 75.8% SB: F-score = 73.3%, + temporal: F-score = 80.0% LPA: F-score = 76.0%, + temporal: F-score = 80.4% MVPA: F-score = 61.0%, + temporal: F-score = 65.2% Walk: F-score = 55.7%, + temporal: F-score = 62.9% Run: F-score = 53.1%, + temporal: F-score = 67.2% |
- |
Low (level 1) |
|
| AG-RF-VM-5 |
Time and frequency features: F-score = 79.5%, + temporal features: F-score = 82.2% SB: F-score = 80.6%, + temporal: F-score = 85.7% LPA: F-score = 82.7%, + temporal: F-score = 85.6% MVPA: F-score = 75.5%, + temporal: F-score = 76.3% Walk: F-score = 69.8%, + temporal: F-score = 68.8% Run: F-score = 71.2%, + temporal: F-score = 72.8% |
- (incl. temp oral ±) |
||||||||
| AG-RF-VM-10 |
Time and frequency features: F-score = 83.1%, + temporal features: F-score = 85.3% SB: F-score = 82.3%, + temporal: F-score = 87.6% LPA: F-score = 85.7%, + temporal: F-score = 87.9% MVPA: F-score = 77.6%, + temporal: F-score = 76.4% Walk: F-score = 80.7%, + temporal: F-score = 81.0% Run: F-score = 74.4%, + temporal: F-score = 73.6% |
± | ||||||||
| AG-RF-VM-15 |
Time and frequency features: F-score = 84.0%, + temporal features: F-score = 85.9% SB: F-score = 85.0%, + temporal: F-score = 87.7% LPA: F-score = 86.8%, + temporal: F-score = 88.2% MVPA: F-score = 75.3%, + temporal: F-score = 78.5% Walk: F-score = 78.4%, + temporal: F-score = 79.4% Run: F-score = 80.0%, + temporal: F-score = 82.6% |
± | ||||||||
| Non-dominant wrist | AG-RF-VM-1 |
Time and frequency features: F-score = 62.6%, + temporal features: F-score = 68.8% SB: F-score = 63.3%, + temporal: F-score = 69.2% LPA: F-score = 71.4%, + temporal: F-score = 75.5% MVPA: F-score = 45.7%, + temporal: F-score = 57.5% Walk: F-score = 45.9%, + temporal: F-score = 54.8% Run: F-score = 55.1%, + temporal: F-score = 61.6% |
- | |||||||
| AG-RF-VM-5 |
Time and frequency features: F-score = 70.8%, + temporal features: F-score = 75.5% SB: F-score = 69.3%, + temporal: F-score = 78.% LPA: F-score = 76.5%, + temporal: F-score = 80.1% MVPA: F-score = 60.9%, + temporal: F-score = 66.9% Walk: F-score = 60.7%, + temporal: F-score = 60.3% Run: F-score = 68.5%, + temporal: F-score = 68.8% |
- | ||||||||
| AG-RF-VM-10 |
Time and frequency features: F-score = 74.5%, + temporal features: F-score = 80.0% SB: F-score = 73.7%, + temporal: F-score = 82.4% LPA: F-score = 79.1%, + temporal: F-score = 82.9% MVPA: F-score = 62.0%, + temporal: F-score = 70.3% Walk: F-score = 68.8%, + temporal: F-score = 70.8% Run: F-score = 73.4%, + temporal: F-score = 71.5% |
- (incl. temp oral ±) |
||||||||
| AG-RF-VM-15 |
Time and frequency features: F-score = 77.3%, + temporal features: F-score = 80.6% SB: F-score = 78.2%, + temporal: F-score = 83.3% LPA: F-score = 81.2%, + temporal: F-score = 83.7% MVPA: F-score = 62.1%, + temporal: F-score = 70.7% Walk: F-score = 70.5%, + temporal: F-score = 69.0% Run: F-score = 82.4%, + temporal: F-score = 82.4% |
- (incl. temp oral ±) |
||||||||
| Right hip + Non-dominant wrist | AG-RF-VM-1 |
Time and frequency features: F-score = 72.5%, + temporal features: F-score = 76.8% SB: F-score = 75.8%, + temporal: F-score = 80.8% LPA: F-score = 77.7%, + temporal: F-score = 81.0% MVPA: F-score = 62.1%, + temporal: F-score = 66.7% Walk: F-score = 58.4%, + temporal: F-score = 64.9% Run: F-score = 64.5%, + temporal: F-score = 67.9% |
- | |||||||
| AG-RF-VM-5 |
Time and frequency features: F-score = 79.6%, + temporal features: F-score = 82.1% SB: F-score = 81.6%, + temporal: F-score = 86.0% LPA: F-score = 82.8%, + temporal: F-score = 85.6% MVPA: F-score = 74.3%, + temporal: F-score = 74.5% Walk: F-score = 70.1%, + temporal: F-score = 69.5% Run: F-score = 71.7%, + temporal: F-score = 72.5% |
- (incl. temp oral ±) |
||||||||
| AG-RF-VM-10 |
Time and frequency features: F-score = 83.2%, + temporal features: F-score = 85.3% SB: F-score = 83.9%, + temporal: F-score = 87.5% LPA: F-score = 85.8%, + temporal: F-score = 87.9% MVPA: F-score = 75.6%, + temporal: F-score = 77.2% Walk: F-score = 79.5%, + temporal: F-score = 80.7% Run: F-score = 74.9%, + temporal: F-score = 73.0% |
- (incl. temp oral ±) |
||||||||
| AG-RF-VM-15 |
Time and frequency features: F-score = 84.3%, + temporal features: F-score = 86.4% SB: F-score = 85.5%, + temporal: F-score = 88.7% LPA: F-score = 86.4%, + temporal: F-score = 88.4% MVPA: F-score = 77.1%, + temporal: F-score = 78.0% Walk: F-score = 78.1%, + temporal: F-score = 79.8% Run: F-score = 86.6%, + temporal: F-score = 86.8% |
± | ||||||||
| Hislop et al. (2012) [70] |
n = 31 Age = 4.4 ± 0.8 years Sex = 51.6% girls |
cpm and % time spent in MVPA Free-living (unstructured outdoor free play during preschool) |
DVO using CARS (modified) to score activity type and derive activity intensity (MVPA: moderate/fast translocation) by one rater | VG | Right hip | AG-cts-VA-15 | rsp = .39* | - |
Low (level 1) |
|
| RT-cts-VM-15 | rsp = .56** | - | ||||||||
| AG-Si-VA-15 | MD = 0.8 min* | ? | ||||||||
| RT-Swr-VM-15 | MD = -12.2 min* | ? | ||||||||
| RT-Slj-VM-15 | MD = 0 min | ? | ||||||||
| Hislop et al. (2012) [61] |
n = 31 Age = 4.4 ± 0.8 years Sex = 51.6% girls |
Activity intensity: SB, LPA, and MVPA Free-living (unstructured outdoor free play during preschool) |
DVO using CARS to score activity type and derive activity intensity (SB: stationary, motionless or with movement of limbs/trunk; LPA: easy translocation; MVPA: moderate/fast translocation) by one rater | VG | Right hip | AG-Ev-VA-15 | SB: MD = 13.2, LoA (-2.2 to 28.6)** | ? |
Low (level 1) |
|
| AG-Si-VA-15 |
SB: MD = -7.2, LoA (-20.2 to 5.7)**; LPA: MD = 6.3, LoA (-6.0 to 18.6)** MVPA: MD = 0.8, LoA (-6.2 to 7.8) |
? | ||||||||
| AG-Puy-VA-15 |
SB: MD = 0.4, LoA (-13.25 to 13.99); LPA: MD = -2.2, LoA (-15.0 to 10.5) MVPA: MD = 1.7, LoA (-8.0 to 11.5) |
? | ||||||||
| AG-vC-VA-15 |
SB: MD = -8.2, LoA (-22.7 to 6.2)**; LPA: MD = 11.4, LoA (-1.4 to 24.2)** MVPA: MD = -3.3, LoA (-11.8 to 5.3)** |
? | ||||||||
| AG-Pa-VA-15 | MVPA: MD = -8.7, LoA (-19.9 to 2.5)** | ? | ||||||||
| AG-Re-VA-15 | SB: MD = -3.6, LoA (-17.6 to 10.4)** | ? | ||||||||
| Hislop et al. (2016) [76] |
n = 32 Age = 4.20 ± 0.5 (3 to 5) years Sex = 34.4% girls |
Activity intensity: SB, LPA, MVPA and total PA Free-living (free-play in nursery) |
DVO using CARS (modified) to score activity type and derive activity intensity (SB: stationary, motionless; LPA: stationary, movement of the trunk/limbs and easy translocation; MVPA: moderate and fast translocation) | VG | Non-dominant wrist | AG-J13-VM-5 |
Total PA: MD = 1.1, LoA (-9.9 to 12.1) Locomotion CARS vs. high intensity: MD = -2.0, LoA (-9.4 to 5.4) No clear agreement MVPA: MD = -9.3, LoA (-20.0 to 1.5); Locomotion vs. high wrist estimate: MD = 3.4, LoA (-3.1 to 10.0); Standing vs. low wrist estimate: MD = 2.8, LoA (-10.3 to 16.4) |
? |
Low (level 1) |
|
| Waist | AG-Ev-VA-5 | No clear agreement: Total PA: MD = 6.3, LoA (-8.8 to 21.4); MVPA: MD = -3.8, LoA (-10.7 to 3.1); Locomotion: MD = 3.4, LoA (-3.1 to 10.0); Standing: MD = 2.8, LoA (-10.3 to 16.4) | ? | |||||||
| Martin et al. (2011) [72] |
n = 23 Age = 4.5 ± 0.7 years Sex = 60.9% girls |
SB and total PA Free-living |
aP-PRE-uni-n.r. at right thigh (SB: sitting/lying, and quiet standing) | VG | Right hip | AG-Re-VA-60 |
rsp = .66***, MD = -2.1 ± 4.6%, LoA (-11.4 to 7.2%)* Corrected (counts increased by 9%): rsp = .68***, MD = -4.3 ± 4.8%, LoA (-14.0 to 5.4%)*** |
+ |
Low (level 2) |
|
| van Cauwenberghe et al. (2012) [64] |
n = 49 Age = 4.0 ± 0.5 (3 to 4) years Sex = 55.1% girls |
SB and total PA Free-living (at childcare) |
aP-PRE-uni-n.r. at right thigh (SB: sitting/lying) |
VG | Right hip | Ac-Ev-omni-15 |
accuracy = 73.0%, κ = .46, 95% CI (.45 to .47) MD = 1.3 min; 0.1%, LoA (-59.4 to 61.9); 39.2% |
- |
Low (level 2) |
|
| Kahan, Nicaise, & Reuben (2013) [71] |
n = 12 Age = 4.7 ± 0.3 years Sex = 75.0% girls |
Activity intensity: SB and MVPA Free-living (unstructured outdoor free play) |
DO using OSRAC-P to score activity type and derive activity intensity (SB: stationary, motionless or with limb/trunk movement, light activity; MVPA: moderate/ vigorous activity) scored by one rater | VG | Right hip | AG-Si-VA-5 |
accuracy = 81.2, 95% CI (79.2 to 83.1), κ = .48 SB: Se = 81.4%, Sp = 50.7%, bias = -8.1% MVPA: Se = 35.8%, Sp = 87.6%, bias = 4.7% |
± (SB ± ; PA ±) |
Low (level 2) |
|
| AG-vC-VA-5 |
accuracy = 78.5, 95% CI (76.4 to 80.3), κ = .48 SB: Se = 80.0%, Sp = 52.4%, bias = -8.6% MVPA: Se = 53.9%, Sp = 79.1%, bias = -5.3% |
- (SB ± ; PA -) |
||||||||
| AG-Ev-VA-5 |
accuracy = 79.9, 95% CI (77.5 to 82.1), κ = .58 SB: Se = 75.2%, Sp = 66.4%, bias = 36.3%*** MVPA: Se = 54.8%, Sp = 78.9%, bias = -5.9% |
- (SB -; PA -) |
||||||||
| AG-Pa-VA-5 |
accuracy = 77.2, 95% CI (74.9 to 79.4), κ = .53 SB: Se = 50.0%, Sp = 58.7%, bias = 33.2%*** MVPA: Se = 62.7%, Sp = 72.2%, bias = -15.8%*** |
- (SB -; PA -) |
||||||||
| Alhassan et al. (2017) [56] |
n = 33 Age = 4.4 ± 0.8 (2.9 to 5) years Sex = 36.4% girls |
Counts Free-living (at preschool) |
Aw-cts-uni-15 at non-dominant wrist | VG | Waist | AG-cts-VA-15 | rsp = .41*** | - |
Low (level 2) |
|
|
Activity intensity: SB, LPA, MPA, and VPA Free-living (at preschool) |
DO using OSRAC-P (modified) to score activity type and derive activity intensity (SB: stationary, motionless or with trunk/limb movement; LPA: easy translocation; MPA: moderate translocation; VPA: vigorous translocation) by one rater |
A VG (for MVPA) |
AG-cts-VA-15 | rsp = .47*** | - |
Low (MVPA) Very low (rest) (level 2) |
||||
| AG-Si-VA-15 |
accuracy = 50.3%, κ = .13, κw = .19 SB: accuracy = 62.7%, κ = .26, Se = 87.4%, Sp = 38.2% LPA: accuracy = 65.0%, κ = .01, Se = 18.5%, Sp = 82.2% MPA: accuracy = 86.3%, κ = .06, Se = 10.0%, Sp = 95.1% VPA: accuracy = 86.5%, κ = .06, Se = 5.3%, Sp = 98.5% MVPA: accuracy = 76.9%, κ = .15, Se = 16.2%, Sp = 95.2% |
- (SB -; PA -) |
||||||||
| AG-Pa-VA-15 |
accuracy = 44.1%, κ = .21, κw = .32 SB: accuracy = 61.5%, κ = 0.40, Se = 60.1%, Sp = 79.7% LPA: accuracy = 60.7%, κ = .13, Se = 51.1%, Sp = 64.3% MPA: accuracy = 80.3%, κ = .09, Se = 24.0%, Sp = 86.8% VPA: accuracy = 86.1%, κ = .19, Se = 18.0%, Sp = 96.2% MVPA: accuracy = 75.3%, κ = .27, Se = 39.8%, Sp = 86.0% |
- (SB -; PA -) |
||||||||
| Non-dominant wrist | Aw-cts-uni-15 | rsp = .47*** | - | |||||||
| Aw-Ek-uni-15 |
accuracy = 50.3%, κ = .13, κw = .19 SB: accuracy = 65.47%, κ = 0.31, Se = 41.5%, Sp = 89.1% LPA: accuracy = 53.8%, κ = .10, Se = 62.3%, Sp = 50.7% MPA: accuracy = 82.8%, κ = .11, Se = 22.0%, Sp = 89.7% VPA: accuracy = 86.3%, κ = .31, Se = 33.9%, Sp = 94.0% MVPA: accuracy = 77.5%, κ = .35, Se = 46.9%, Sp = 86.8% |
- (SB -; PA -) |
||||||||
| Ahmadi et al. (2020) [83] |
n = 31 Age = 4.0 ± 0.9 (3 to 5) years Sex = 29% girls |
Activity intensity: SB, LPA, MVPA, run, and walk Free-living (play session) |
DVO using customized scheme to score activity type and derive activity intensity (SB: sitting/lying down, and stationary, motionless; LPA: standing, stationary, movement of the limbs/trunk, easy translocation, MPA: moderate and fast translocation; walk: translocation, medium speed; run: translocation (very) fast) | A | Non-dominant wrist | AG-RF-VM-15 |
accuracy = 59.1%, 95% CI (57.1 to 61.1%), κ = .37 SB: accuracy = 76.8% LPA: accuracy = 57.5% MVPA: accuracy = 83.6% Walk: accuracy = 14.8% Run: accuracy = 68.7% Excl. multiple activities: walk accuracy (14.8 to 43.8%) and run accuracy (68.7 to 100%) |
- (SB -; PA -) |
Very low (level 1) |
|
| AG-SVM-VM-15 |
accuracy = 59.3%, 95% CI (57.3 to 61.3%), κ = .37 SB: accuracy = 76.8% LPA: accuracy = 58.3% MVPA: accuracy = 82.6% Walk: accuracy = 12.3% Run: accuracy = 70.1% Excl. multiple activities: walk accuracy (12.3 to 45.8%) and run accuracy (70.1 to 100%) |
- (SB -; PA -) |
||||||||
| Right hip | AG-RF-VM-15 |
accuracy = 69.4%, 95% CI (67.4 to 71.2%), κ = .48 SB: accuracy = 71.7% LPA: accuracy = 79.3% MVPA: accuracy = 71.3% Walk: accuracy = 10.4% Run: accuracy = 74.5% Excl. multiple activities: walk accuracy (10.4 to 29.2%) and run accuracy (74.5 to 100%) |
- (SB -; PA -) |
|||||||
| AG-SVM-VM-15 |
accuracy = 66.4%, 95% CI (64.4 to 68.3%), κ = .45 SB: accuracy = 77.7% LPA: accuracy = 71.1% MVPA: accuracy = 73.0% Walk: accuracy = 8.9% Run: accuracy = 65.8% Excl. multiple activities: walk accuracy (8.9 to 33.3%) and run accuracy (65.8 to 100%) |
- (SB -; PA -) |
||||||||
| Trost et al. (2018) [89] |
n = 11 Age = 4.8 ± 0.87 (3 to 6) years Sex = 55% girls |
Activity intensity: SB, LPA, MVPA, run, and walk Laboratory (semi-standardized activities |
DO to score activity type and determine activity intensity based on preschool-specific MET thresholds (SB < 1.5 METs, LPA 1.5–2.7, MPA 2.8–3.4 VPA ≥ 3.5) | A | Non-dominant wrist | AG-SVM-VM-15 |
accuracy = 80.4%, 95% CI (78.9 to 81.9%), κw = .73, CV κw = .78 SB: accuracy = 90.0% LPA: accuracy = 73.7% MVPA: accuracy = 78.6% Walk: accuracy = 70.6% Run: accuracy = 71.2% |
+ (SB + ; PA -) |
Very low (level 2) |
|
| AG-RF-VM-15 |
accuracy = 78.1%, 95% CI (76.6 to 79.9%), κw = .70, CV κw = .76 SB: accuracy = 89.1% LPA: accuracy = 68.7% MVPA: accuracy = 79.1% Walk: accuracy = 61.1% Run: accuracy = 68.8% |
± (SB + ; PA -) |
||||||||
| AG-T18-VA-15 | κw = .64 | - | ||||||||
| AG-T18-VM-15 | κw = .49 | - | ||||||||
| Right hip | AG-SVM-VM-15 |
accuracy = 81.3%, 95% CI (79.9 to 82.8%), κw = .74, CV κw = .82 SB: accuracy = 94.0% LPA: accuracy = 76.8% MVPA: accuracy = 76.0% Walk: accuracy = 63.5% Run: accuracy = 69.8% |
+ (SB + ; PA -) |
|||||||
| AG-RF-VM-15 |
accuracy = 80.2%, 95% CI (79.9 to 81.6%), κw = .72, CV κw = .81 SB: accuracy = 93.2% LPA: accuracy = 72.1% MVPA: accuracy = 76.7% Walk: accuracy = 61.1% Run: accuracy = 73.0% |
± (SB + ; PA -) |
||||||||
| AG-T18-VA-15 | κw = .65 | - | ||||||||
| AG-T18-VM-15 | κw = .61 | - | ||||||||
| Non-dominant wrist + hip | AG-SVM-VM-15 |
accuracy = 85.2%, 95% CI (83.8 to 86.5%), κw = .80, CV κw = .84 SB: accuracy = 94.7% LPA: accuracy = 80.2% MVPA: accuracy = 81.7% Walk: accuracy = 69.7% Run: accuracy = 82.3% |
+ (SB + ; PA +) |
|||||||
| AG-RF-VM-15 |
accuracy = 81.8%, 95% CI (80.4 to 83.2%), κw = .75, CV κw = .81 SB: accuracy = 93.0% LPA: accuracy = 73.9% MVPA: accuracy = 80.7% Walk: accuracy = 63.0% Run: accuracy = 75.3% |
+ (SB + ; PA +) |
||||||||
| Finn & Specker (2000) [60] |
n = 40 Age = (3 to 4) years Sex = 60% girls |
Mean activity counts (3-min) Free-living |
DVO using CARS (3-min average) to score activity type and derive activity intensity (SB: stationary, motionless or with movement of limbs/trunk; LPA: easy translocation; MVPA: moderate/fast translocation) by two independent raters | D | Waist | Aw-cts-uni-60 |
r = .03 to r = .92 (median = .74) More active children higher association between CARS and counts: within-child correlation coefficients vs. CARS r = .37* or counts r = .31 |
PA: - |
Very low (level 1) |
|
| Brønd et al. (2020) [86] |
n = 29 Age = 4.4 (3 to 6) years Sex = n.r. % girls |
Activity type: Sit, stand, run, walk, and bike Free-living (structured activities at school) |
DO to score activity type (sit: on floor/chair playing; stand: stand close to table playing; run: run together with instructor; walk: walks together with instructor; bike: on running bike) by one rater | D | Thigh | AX-DT-HA/VA/DA-2 |
Sit: Se = 100%, Sp = 100% Stand: Se = 100%, Sp = 99.8% Bike (sitting bike): Se = 64.8%, Sp = 100% Walk: Se = 82.6%, Sp = 98.1% Run: Se = 92.4%, Sp = 95.0% |
+ |
Very low (level 2) |
|
| Zhao et al. (2013) [90] |
n = 69 Age = (3 to 5) years Sex = 55% girls |
Activity type: Sleep, rest, quiet play, low active play, moderately active play, and very active play Laboratory (structured activities) |
DO to score activity type (sleep: lying and sleeping; rest: watching tv, quiet play: sitting while coloring, puzzle, video game; low active play: stand and play; moderately active play: standing while ball toss, active video game, dance; very active play: running in place) | D | Right hip | AG-SVM -VA/HA/DA/VM-60 |
accuracy = 75.3% Sleep: accuracy = 91.44% Rest: accuracy = 65.66% Quiet play: accuracy = 74.07% Low active play: accuracy = 68.49% Moderately active play: accuracy = 93.73% Very active play: accuracy = 98.73% Misclassification highest for sleep (31.6%) and quiet play (33.0%) |
± |
Very low (level 2) |
|
| AG-MLR—VA/HA/DA/VM-60 | accuracy (67.2 to 73.2%) | - | ||||||||
| Hagenbuchner et al. (2015) [87] |
n = 11 Age = 4.8 ± 0.87 (3 to 6) years Sex = 55% girls |
Activity intensity: SB, LPA, MVPA, run, and walk Laboratory (activity trials) |
DO to score activity type and derive activity intensity (SB: watching tv, tablet/computer, reading, quiet play; LPA: clean up toys, standing art, treasure hunt; MVPA: bicycle riding, obstacle course, active game; walk: walk at self-selected pace; run: run at self-selected speed) | D | Right hip | AG-MLP-VM-60 |
accuracy = 69.7% SB: accuracy = 81.8% LPA: accuracy = 78.8% MVPA: accuracy = 63.6% Walk: accuracy = 36.4% Run: accuracy = 45.5% |
- (SB + ; PA -) |
Very low (level 2) |
|
| AG-SOM-VM-60 |
accuracy = 53.8% SB: accuracy = 59.1% LPA: accuracy = 57.6% MVPA: accuracy = 66.7% Walk: accuracy = 36.4% Run: accuracy = 0.0% |
- (SB -; PA -) |
||||||||
| AG-DLEN-VM-60 |
accuracy = 82.6% SB: accuracy = 84.1% LPA: accuracy = 90.9% MVPA: accuracy = 78.8% Walk: accuracy = 72.7% Run: accuracy = 72.7% |
± (SB + ; PA -) |
||||||||
| de Bock et al. (2010) [68] |
n = 33 Age = 3.5 ± 0.8 (boys); 4.3 ± 1.1 (girls) years Sex = 36.36% girls |
Activity intensity: SB and MVPA Free-living (at preschool) |
DO using CARS to score activity type and derive activity intensity (SB: stationary, motionless or with trunk/limb movement; MVPA: easy, moderate, and fast translocation) by five independent raters | D | Chest | Ah-dB-VA-15 |
Calibration MVPA: AUC-ROC = .86 SB: AUC-ROC = .79 Cross-validation SB: accuracy 67% (boys), 69% (girls); Sp = 52% (boys), 61% (girls); Se = 78% (boys), 75% (girls) MVPA: accuracy = 84% (boys), 87% (girls) |
- (SB -; PA +) |
Very low (level 2) |
|
| Fairweather et al. (1999) [59] |
n = 11 Age = 3.7 ± 0.5 years Sex = 72.7% girls |
Mean cpm Free-living (exercise class) |
DO using 1-min average CPAF score (ranging from 1 to 4) scored by one rater | D | Right hip | CSA-cts-uni-60 | r = .87***, rsp = .79** | PA: + |
Very low (level 2) |
|
|
n = 10 Age = 4.0 ± 0.4 years Sex = 90% girls |
CSA at left hip |
r = .92**, MD = 31 (SD = 64, 95% CI (1 to 61)*, rsp = .97** Relative PA assessment largely unaffected by location |
PA: + | |||||||
| Klesges & Klesges (1987) [62] |
n = 28 Age = 33.9 ± 8.0 months Sex = 43.3% girls |
Total PA (all-day) and hourly PA Free-living (unstructured activities) |
DO using FATS to score behavior and intensity | D | Left hip | CPAC-cts-uni-n.r |
r = .54*** (total PA); r = .62** to .95*** (hourly PA) Behavior: lying rsp = -.37; sitting rsp = -.26; standing rsp = .60**; walking rsp = .50**; running rsp = .37 Intensity: minimal rsp = -.51**; moderate rsp = .51**; extreme rsp = .40* Summary: correlations higher for older children (< 32.5 months rsp = .39; > 32.5 months rsp = .80***), girls (rsp = ,67*, boys rsp = .43), and obese children (rsp = .75*, normal weight rsp = .46*) |
PA: ± |
Very low (level 2) |
|
| Klesges et al. (1985) [63] |
n = 30 Age = 47.7 ± 12.5 months Sex = 40% girls |
Total PA Free living (free play) |
DO using FATS to score behavior and intensity | D | Left hip | CPAC-cts-uni-n.r |
Behavior: r = .38*, rsp = .28: lying r = .17, rsp = -.18; sitting r = -.31*, rsp = -.32*; crawling r = -.22, rsp = -.20; climbing r = -.06, rsp = .02; standing r = .35*, rsp = .37*; walking r = -.11, rsp = -.03; running r = .32*, rsp = .22 Intensity: r = .32*, rsp = .29: minimal r = -.27, rsp = -.23; moderate r = .05, rsp = .07; extreme r = .44**, rsp = .43** Summary: r = .40**, rsp = .36* |
PA: - |
Very low (level 2) |
|
| Right hip | LSI-cts-uni-n.r |
Behavior: r = .38*, rsp = .28: lying r = .17, rsp = -.18; sitting r = -.31*, rsp = -.32*; crawling r = -.22, rsp = -.20; climbing r = -.06, rsp = .02; standing r = .35*, rsp = .37*; walking r = -.11, rsp = -.03; running r = .32*, rsp = .22 Intensity: r = .32*, rsp = .29: minimal r = -.27, rsp = -.23; moderate r = .05, rsp = .07; extreme r = .44**, rsp = .43** Summary: r = .40**, rsp = .36* |
PA: - | |||||||
| Ettienne et al. (2016) [69] |
n = 30 Age = 3.5 ± 0.6 years Sex = 43% girls |
Activity intensity: SB, LPA, and MVPA Free-living (during preschool) |
DO using (modified) SOFIT to score activity type and derive activity intensity (SB: lying; LPA: sitting, standing; MVPA: walking, very active) | D | Non-dominant wrist | Ac-Sc-omni-60 |
accuracy = 74%, κw = .17*** 391 min classified as MVPA, whereas DO class was LPA; 406 min DO classified as MVPA and accelerometer as LPA |
- |
Very low (level 2) |
|
| Djafarian et al. (2013) [57] |
n = 42 Age = 4.1 ± 0.8 (3 to 5) years Sex = 47.6% girls |
cpm 1–10-min periods Free-living (structured & unstructured) |
DO using 1-min average CARS score | D | Non-dominant wrist | Aw-cts-uni-300 |
r = .52** (n = 21 cross-validation sample) Measured (DO) vs. predicted (log accelerometry) CARS score MD = 0.025 (± 0.38), CI 95% with 0.74 CARS unit |
PA: - |
Very low (level 2) |
|
| Davies et al. (2012) [82] |
n = 30 Age = 4.1 ± 0.5 (3.1 to 4.9) years Sex = 60% girls |
Activity type: Sit/lie, stand, and walk Free-living (usual nursery setting) |
DVO using to score activity type (walk, sit, stand, lie, other (crouching down, kneeling up, crawling) by one rater | I | Right thigh | aP-PRE-uni-1 |
Time spent: sitting MD = -4.4%**, standing MD = 7.1%** Sit/lie: Se = 86.7%, Sp = 97.1%, PPV = 96.3% Stand: Se = 91.8%, Sp = 84.3%, PPV = 75.4% Walk: Se = 80.3%, Sp = 95.9%, PPV = 78.4% |
+ |
Very low (level 1) |
|
| Johansson et al. (2015) [77] |
Calibration n = 26 Age = 26 ± 6.0 months Sex = 38% girls Cross-validation n = 12 Age = 25 ± 5.6 (15 to 36) months Sex = 50% girls |
Activity intensity: SB, LPA, and MVPA Free-living (structured activities and free play at preschool) |
DVO using CARS to score activity type and derive activity intensity (SB: stationary, motionless; LPA: stationary, movement of the limbs/trunk, easy translocation; MVPA: moderate and fast translocation) | I | Non-dominant wrist | AG-J13-VM-5 |
Calibration SB: AUC-ROC = .98, CI (.95 to 1.0) MVPA: AUC-ROC = .90, CI (.81 to .98) Cross-validation SB: rsp = .91 LPA: rsp = .77* MVPA: rsp = .69* |
+ (SB + ; PA ±) |
Very low (level 1) |
|
| AG-J13-VA-5 |
Calibration SB: AUC-ROC = .98, CI (.95 to 1.0) MVPA: AUC-ROC = .88, CI (.78 to .97) Cross-validation SB: rsp = .91 LPA: rsp = .89* MVPA: rsp = .77* |
+ (SB + ; PA +) |
||||||||
| Johansson et al. (2016) [78] |
n = 30 Age = 49.0 ± 3.7 months Sex = 53% girls |
Activity intensity: SB, LPA, and MVPA Free-living (structured indoor activities and free play at preschool) |
DO using CARS to score activity type and derive activity intensity (SB: stationary, motionless; LPA: stationary, movement of the limbs/trunk, easy translocation; MVPA: moderate and fast translocation) by one rater | I | Left hip | AG-J16-VM-5 |
κqw = .86, 95% CI (.85 to .87), accuracy = 75% SB: Se = 100%, Sp = 60%, AUC-ROC = .95 MVPA: Se = 70%, Sp = 93%, AUC-ROC = .91 |
+ (SB ± ; PA ±) |
Very low (level 2) |
|
| AG-J16-VA-5 |
κqw = .76, 95% CI (.74 to .77), accuracy = 68% SB: Se = 100%, Sp = 60%, AUC-ROC = .93 MVPA: Se = 70%, Sp = 100%, AUC-ROC = .95 |
± (SB ± ; PA ±) |
||||||||
| Non-dominant wrist | AG-J16-VM-5 |
κqw = .95, 95% CI (.94 to .96), accuracy = 82% SB: Se = 100%, Sp = 60%, AUC-ROC = .99 MVPA: Se = 70%, Sp = 100%, AUC-ROC = .96 |
+ (SB ± ; PA ±) |
|||||||
| AG-J16-VA-5 |
κqw = .92, 95% CI (.91 to .93), accuracy = 82% SB: Se = 100%, Sp = 60%, AUC-ROC = .99 MVPA: Se = 70%, Sp = 100%, AUC-ROC = .95 |
+ (SB ± ; PA ±) |
||||||||
| Reilly et al. (2003) [80] |
n = 52 Age = 3.5 ± 0.5 (3 to 4) years Sex = 59.62% girls |
Activity intensity: SB Free-living |
DO using CPAF to score activity type and derive activity intensity (SB: stationary, motionless or with limb movement) by one rater |
I | Right hip | CSA-Re-uni-60 |
Se = 83%, 95% CI (78 to 86%) Sp = 82%, 95% CI (89 to 86%) |
SB: + |
Very low (level 2) |
|
| Adolph et al. (2012) [51] |
n = 64 Age = 4.5 ± 0.8 (3 to 5) years Sex = 42.2% girls |
Activity intensity: SB, LPA, and MVPA Laboratory |
DO using CARS to score activity type and derive CARS levels (1 to 5) | I | Chest | Ah-A-uni-60 |
accuracy = 72%, TPR = 82% SB: accuracy = 75% LPA: accuracy = 61% MVPA: accuracy = 82% |
- (SB -; PA ±) |
Very low (level 2) |
|
| Right hip | Ac-A-omni-60 |
accuracy = 71%, TPR = 69% SB: accuracy = 77% LPA: accuracy = 63% MVPA: accuracy = 69% |
- (SB -; PA -) |
|||||||
| RT-A-VM-60 |
accuracy = 73%, TPR = 79% SB: accuracy = 76% LPA: accuracy = 65% MVPA: accuracy = 79% |
- (SB -; PA ±) |
||||||||
| Li et al. (2020) [79] |
n = 34 Age = 4.0 ± 0.5 (3 to 5) years Sex = 58.8% girls |
Activity intensity: SB, LPA, MPA, and VPA Free-living (during preschool) |
AG-B-VM-60 | I | Right hip | AG-LiROC-VM-60 |
κ = .30, accuracy = 59.5% SB: Se = 77.8%, Sp = 77.8%, FPR = 22.2%, FNR = 22.2%, κ = .54 LPA: Se = 26.8%, Sp = 87.5%, FPR = 12.5%, FNR = 73.2%, κ = .16 MPA: Se = 4.5%, Sp = 69.8%, FPR = 3.2%, FNR = 95.5%, κ = .02 VPA: = Se = 79.0%, Sp = 79.0%, FPR = 21.0%, FNR = 21.0%, κ = .11 MVPA collapsed: κ = .35, accuracy = 63.6%, Se = 78.9%, Sp = 78.9%, FPR = 20.1%, FNR = 21.1%, κ = .28 |
- (SB -; PA -) |
Very low (level 2) |
|
| AG-LiOLR-VM-60 |
κ = .37, accuracy = 71.5% SB: Se = 91.0%, Sp = 52.8%, FPR = 47.2%, FNR = 9.1%, κ = .47 LPA: Se = 43.3%, Sp = 86.5%, FPR = 56.7%, FNR = 13.5%, κ = .32 MPA: Se = 8.8%, Sp = 99.1%, FPR = 1.0%, FNR = 76.1%, κ = .12 VPA: Se = 23.9%, Sp = 99.0%, FPR = 1.0%, FNR = 76.1%, κ = .28 MVPA collapsed: κ = .39, accuracy = 72.4%, Se = 24.3%, Sp = 99.0%, FPR = 1.0%, FNR = 75.7%, κ = .33 |
- (SB -; PA -) |
||||||||
| AG-J13-VM-60 | Non-dominant wrist | AG-Li4k-VM-60 |
κ = .37, accuracy = 63.7% SB: Se = 71.6%, Sp = 85.1%, FPR = 14.9%, FNR = 28.4%, κ = .53 LPA: Se = 50.9%, Sp = 76.8%, FPR = 23.2%, FNR = 49.1%, κ = .27 MPA: Se = 48.4%, Sp = 86.8%, FPR = 13.2%, FNR = 51.6%, κ = .19 VPA: Se = 33.9%, Sp = 98.2%, FPR = 1.8%, FNR = 66.1%, κ = .31 MVPA collapsed: κ = .40, accuracy = 65.6%, Se = 68.4%, Sp = 86.6%, FPR = 13.4%, FNR = 31.6%, κ = .35 |
- (SB -; PA -) |
||||||
| Pagels, Boldemann, & Raustorp (2011) [73] |
n = 55 Age = 4.5 ± 0.6 (3.4 to 5.7) years Sex = 49.1% girls |
Activity intensity: LPA and MVPA Free-living (at preschool) |
Pedometer (Yamax SW200) to measure daily steps | I | Waist | AG-Si-VA-15 |
r = .67***, R2adj = 45%: (3-year-olds: r = .37, 4-year-olds: r = .52**, 5-year-olds: r = .84***) LPA: r = .76***, R2adj = 52% MVPA: 3-year-olds (r = .19, R2adj = 4%); 4-to-5-year-olds (r = .50***, R2adj = 23%) |
PA: - |
Very low (level 3) |
Abbreviations: A Adolph’s cut-points (2012) [51], Ac Actical, ACT40 Actiware software with wake threshold value of 40, ACT80 Actiware software with wake threshold value of 80, AEE activity energy expenditure, AIC Akaike information criterion, AG ActiGraph, Ah Actiheart, ANN artificial neural network, aP activPAL, AS AlgoSmooth [94], AUC-ROC area under the receiver operating curve, Aw Actiwatch, AX Axivity, B Butte’s cut-points (2014) [75], C Costa’s cut-points (2014) [46], CARS children’s activity rating system, CCC concordance correlation coefficient, CI confidence interval, CPAC Caltrac personal activity computer, CPAF children’s physical activity form, cpm counts per minute, cts counts, CSA computer science and applications activity monitor, CSTS cross-sectional time series, CV cross-validation, DA diagonal axis (z-axis), dB de Bock’s cut-points (2010) [68], DLEN deep learning ensemble network, DLW doubly labelled water, DO direct observation, DT decision table, DVO direct video observation, EE energy expenditure, Ek Ekblom’s cut-points (2012) [95], Ev Evenson’s cut-points (2008) [91], FATS Fargo activity time-sampling survey, FNR false negative rate, FPR false positive rate, GA GENEActiv, HA horizontal axis (x-axis), ICC intraclass correlation coefficient, J13 Johansson’s cut-points (2015) [77], J16 Johansson’s cut-points (2016) [78], κ Kappa, K Kelly’s cut-points (2016) [96], κw weighted Kappa, κqw quadratic weighted Kappa, LiROC Li’s cut-points (2020) [79], LiORL Li’s cut-points (2020) [79], Li4k Li’s cut-points (2020) [79], LoA limits of agreement, LM linear model, LPA light physical activity, LSI LSI moving activity monitor, MAE mean absolute error, MAPE mean absolute percentage error, MARS multivariate adaptive regression splines, MD mean difference, METs metabolic equivalents, MLM mixed linear model, MLP multi-layer perceptron network, MLR multinomial logistic regression, MPA moderate physical activity, MVPA moderate-to-vigorous physical activity, n.r. not reported, NVP negative predictive value, omni omnidirectional, OSRAC-P observational system for recording physical activity in children preschool, Pa Pate’s cut-points (2006) [52], PA physical activity, Pa2 Pate’s cut-points (2006) [52], PAL physical activity level, Pf Pfeiffer’s cut-points (2006) [53], PPV positive predictive value, PRE activPAL professional research edition software, Puy Puyau’s cut-points (2002) [97], r correlation coefficient (unknown), Re Reilly’s cut-points (2003) [80], RF random forests, Ro Roscoe’s cut-points (2017) [67], rp correlation coefficient (Pearson), rsp correlation coefficient (Spearman rank), R2 R-squared value, R.2adj adjusted R-squared value, RMSE root mean square error, RT Research Tracker 3, SB sedentary behavior, Sc Schaefer’s cut-points (2014) [98], SD standard deviation, Se sensitivity, SE standard error, Si Sirard’s age-specific cut-points (2005) [81], Slj Sun’s cut point (2008) [99], SMR sleeping metabolic rate, SOFIT system for observing fitness instruction time, SOM self-organizing map, Sp specificity, SVM support vector machine, Swr Sun’s cut point (2008) [99], TD TracmorD, TEE total energy expenditure, tri mean of the three axes, TPR true positive rate, TST total sleep time, T12 Trost’s cut-points (2012) [44], T18 Trost’s cut-points (2018) [89], uni uniaxial (axis not specified), VA vertical axis (y-axis), vC van Cauwenberghe’s cut-points (2011) [45], VPA vigorous physical activity, VCO2 carbon dioxide, VM vector magnitude, VO2 oxygen consumption, WASO wake after sleep onset, 1 1 s epoch, 2 2 s epoch, 5 5 s epoch, 10 10 s epoch, 15 15 s epoch, 30 30 s epoch, 60 60 s epoch, 300 5 min epochs
aAge presented as mean ± SD (range)
bMethodological study quality based on newly developed checklist: VG very good, A adequate, D doubtful, I inadequate
cDevice-based method described using code combinations of four elements resulting in the following format: brand-axis-approach-epoch length
dStudy result rating based on COSMIN guideline: + sufficient, ± inconsistent, - insufficient, ? intermediate
eQuality of evidence based on GRADE approach
* p < .05
** p < .01
*** p < .001
For the assessment of SB, LPA and MVPA, hip [81] and wrist [78] cut-points were evaluated as valid. Sirard and colleagues (2005) evaluated convergent validity of age specific cut-points [81]. Compared to observational scores using the Children’s Activity Rating Scale (CARS) agreement was high. Highest correlation between predicted and observed scores was found for SB, whereas lowest correlation between predicted and observed scores was found for MVPA. These results received high quality of evidence as the methodological study quality was very good and results were retrieved in a sample of 269 preschoolers. Similar results for convergent validity of Sirard’s SB and MVPA cut-points were found, using the Observational System for Recording physical Activity in Children-Preschool (OSRAC-P) as comparison measure [71]. Highest sensitivity was found for SB, while sensitivity was lowest for VPA. However, specificity was lowest for SB and highest for MVPA. Compared to other cut-points based methods, Sirard’s cut-points were most sensitive in detecting SB and converged best with direct observation [45, 52, 71, 91]. However, convergent validity of Sirard’s cut-points was rated as inconsistent with moderate quality of evidence, as these results were retrieved in a sample of 56 preschoolers. Another study evaluated convergent validity of the Sirard MVPA cut-point compared to the same direct observation scheme, i.e., CARS [61]. Bias was lowest when applying the Sirard MVPA cut-point versus other cut-points based methods in a sample of only 32 preschoolers [45, 52, 97]. When applied to accelerometer-derived data in toddlers, results of Sirard’s cut-points were rated as insufficient [45].
Johansson and colleagues (2016) evaluated convergent validity of wrist cut-points (both VA and VM) [78]. Agreement with direct observation (i.e., CARS) was high [78]. However, these results received very low quality of evidence, as the methodological study quality was inadequate, and results were retrieved in a limited sample of 30 preschoolers.
Some multi-parameter methods were also suitable for assessing SB, LPA and MVPA. Convergent validity of a support vector machine was evaluated as sufficient for distinguishing SB, LPA and MVPA, walking and running in laboratory setting [89] but not in free-living settings [83, 85]. Trost and colleagues (2018) developed random forest and support vector machine models to categorize SB, light activities and games (i.e., LPA), moderate-to-vigorous activities and games (i.e., MVPA), walking and running [89]. Almost perfect agreement with direct observation was found (hip and combination hip and wrist), while cut-points for this sample resulted in only moderate to substantial agreement. Using hip or wrist only data, convergent validity of support vector machines was rated as sufficient, while both random forests and support vector machines were rated as sufficient when hip and wrist data were combined. In free-living settings accuracy of these models decreased by 11 to 15% [85]. Hip classifiers had moderate agreement with direct video observation, while agreement of wrist classifiers was lower in free-living. In free-living settings, accuracy of random forests combining hip and wrist data was comparable. However, study results were rated as insufficient. In addition, support vector machine models have not been tested while combining hip and wrist data. Despite very good [85] and adequate [83, 89] methodological study quality, these results received low quality of evidence as the results were retrieved in limited samples of 11 [89] and 31 [83, 85] preschoolers. Convergent validity of a simple decision table was evaluated as sufficient for distinguishing comparable activity types (i.e., sit, stand, run, walk and bike) in a free-living setting [86]. These study results received very low quality of evidence as methodological study quality was doubtful and the results were retrieved in a sample of only 29 preschoolers.
Criterion validity of support vector machine models, random forests, and artificial neural networks was evaluated [84, 88]. Despite intermediate study results, random forests and artificial neural networks seemed to result in equal prediction accuracy of energy expenditure [88]. Results of the other study indicated that predicted energy expenditure of existing lab, free-living and retrained random forests (wrist and hip) and support vector machines (wrist) were within ± 6% of measured energy expenditure, but not for artificial neural networks (hip) [84]. Despite adequate methodological study quality, these study results received very low quality of evidence as they were retrieved in limited samples of 31 [84] and 41 [88] preschoolers. Criterion validity of cross-sectional time series models [55, 75] and multivariate adaptive regression splines [55] was evaluated as sufficient for predicting minute-by-minute energy expenditure. Results indicated a lack of bias and acceptable limits of agreement for these models, however, bias was slightly lower for multivariate adaptive regression splines. These results received moderate [55] and very low [75] quality of evidence.
For sleep assessment, different cut-points based methods (i.e., wake threshold values) were evaluated to distinguish sleep from wake. Moreover, the multi-parameter method AlgoSmooth was evaluated, which smooths data derived from the wake threshold value of 40 before scoring sleep or wake [100]. Criterion validity of wake threshold values of 40 and 80 applied to adjusted wrist data (i.e., regressed using lower activity counts of the ankle device) was rated as sufficient for wake time but poor for wake time after onset, but results were rated as inconsistent when applied to raw data [66]. In contrast, when the raw wrist data was smoothed using the AlgoSmooth algorithm, criterion validity was evaluated as sufficient [66]. Correlations between an Actiwatch and polysomnography were high, except for wake time after onset. Results were worse for ankle data. Despite very good methodological study quality, these results received low quality of evidence as the results were retrieved in a limited sample of 12 preschoolers [66].
Convergence between devices
Few studies examined the convergence between different accelerometers [56, 64, 72, 74]. No studies evaluated convergence between accelerometer-based methods in infants and toddlers. Convergence of both time spent in SB derived by ActiGraph and activPAL (hip vs. thigh) [72, 74], Actical and activPAL (wrist vs. thigh) [64], and ActiGraph and Actiwatch (waist vs. wrist) count data [56] was rated as insufficient as low to moderate agreement was found. Despite very good methodological study quality of all studies, these results received moderate [74] to low [56, 64, 72] quality of evidence due to sample sizes of 23 to 60 preschoolers.
Combining data
Combining data derived from multiple sensors [39, 85, 89] or multiple axes [34, 43, 47, 49, 77, 78] resulted in more valid predictions. Single placed sensors resulted in lower performance and insufficient data for posture and movement classification, compared to combining data from two or four different locations [39]. In line with these results, the combination of hip and wrist data in models for activity intensity prediction resulted in higher performance compared to using hip or wrist data only [85, 89]. Despite very good [85] and adequate [39, 89] methodological study quality, these results received (very) low quality of evidence due to limited sample sizes of 31 [85], 22 [39], and 11 [89] children.
Generally, using data from the VM to categorize activity intensity provided better results (higher agreement between accelerometry and comparison measure) than the VA (y-axis) [43, 47, 77, 78]. In line with these results, for activity type classification (i.e., running walking climbing up/down, crawling, riding on a ride on toy, standing, sitting, stroller, being carried) feature importance was highest for the VM standard deviation versus features of the different axes or other VM features [49]. In addition, combined cut-points for the VA (y-axis) and horizontal axis (x-axis) were used to classify the postures of infants as prone and non-prone [34]. Despite the inconsistent results, the study indicated that combining data from these axes is required to accurately assess horizontal movement behaviors such as tummy time (time spent prone on floor). The combination of the acceleration signal time-domain and frequency features also resulted in better activity type classification [49, 50]. When comparing feature sets, accuracy was higher when frequency-domain features were included in addition to time-domain features. Moreover, activity intensity classification improved when adding temporal features to this base set (i.e., time domain and frequency features) [85].
Discussion
This review summarizes studies that evaluated the measurement properties of accelerometer-based methods for assessing physical behavior in young children (< 5 years old). To assess the methodological quality of the 62 included studies, we developed a new checklist inspired by COSMIN [25–27]. Despite very good to adequate methodological study quality of 58% of the studies, only ten percent of the study results received high or moderate quality of evidence, due to limited samples sizes.
Validated cut-points for the youngest age group (i.e., infants) are still lacking, while multi-parameter methods were evaluated as sufficient to distinguish posture, SB and PA using multiple sensors [39], movement and sleep [40], leg movements [41], and sleep–wake [30, 36, 38]. Despite very good [30] or adequate [39, 40] methodological study quality of some of these studies, quality of evidence was rated as low [30] to very low [36, 38–41].
In toddlers, hip cut-points were considered valid for distinguishing SB and LPA [46, 47] from high intensity PA [43, 44], despite large differences between cut-points based methods. No studies were found for identifying sleep in toddlers using cut-points based or multi-parameter methods. For SB, VM cut-points varied between < 40 counts/5 s [47] and < 97 counts/5 s [46]. For MVPA, cut-points were VM ≥ 208 counts/15 s [43] and VA ≥ 418 counts/15 s [44]. The difference between the SB cut-points is probably due to inconsistency in the definition of SB adopted by the different observational schemes used. Specifically, in the study by Costa and colleagues, SB was defined as “stationary with no movement and stationary with movement of the limbs”, resulting in a higher cut-point [46] than Oftedal and colleagues who did not include limb movement [47]. Notably, the MVPA cut-points were derived in study samples with divergent characteristics. Trost and colleagues included children from an urban area that were around one year older than the children from a rural area included by Pulakka and colleagues [43, 44]. Conversely, cut-points could not identify toddler specific behaviors such as “being carried” as SB. A random forest model was considered valid to distinguish SB (including this toddler specific behavior) from PA [49]. Despite very good methodological study quality of some studies [44, 46, 49], quality of evidence for these cut-points based and multi-parameter methods was low.
For distinguishing different physical intensities (i.e., SB, LPA, and MVPA), we found strongest evidence in preschoolers. Next to age-specific hip cut-points [81], wrist cut-points were also evaluated as valid [78]. For assessing sleep, adjusted wrist [66] cut-points were evaluated as valid. Quality of evidence for hip cut-points was high [81], and these cut-points were also positively evaluated in cross-validation studies [61, 71], but not when applied in toddlers [45]. The wrist cut-points, however, have not been cross-validated and despite very good methodological study quality of the study assessing sleep cut-points [66], quality of evidence was low [66, 78]. Conversely, for identifying SB, LPA, and MVPA, using multi-parameter methods resulted in more promising results compared to cut-points based methods [83, 85, 89]. Although random forest and support vector machine models were rated as sufficient in laboratory setting [89], these were rated as insufficient in a free-living setting [83, 85]. Activity type could be distinguished using a decision table in a free-living setting [86]. In addition, sleep could be distinguished from wake using the AlgoSmooth algorithm applied to (raw) wrist data [66]. Despite very good [66, 85] and adequate [83, 86, 89] methodological study quality, quality of evidence was low [66, 85] or very low [83, 86, 89].
Despite the promising results of multi-parameter methods, only few models were accessible as open-source software [84–86, 88]. This hampers the replication of study results as closed source models cannot be reused. In case software is available, be aware to use the same version, configuration, and implementation (e.g., brand, axis, placement, parameters, target group). It is not recommended to reuse cut-points based methods when deviating from accelerometer specifications (i.e., brand, axis, and placement) or target population (age group), as cut-points need to be re-evaluated. Moreover, the inconvenience of cut-points based methods is related to the derivation of the magnitude of acceleration (count data), which is kept close source by most manufacturers.
Most studies used a single device or axis to measure physical behavior, while more promising results were found when combining data derived from different sensor placements [39, 85, 89] or multiple axes [34, 43, 47, 49, 50, 90]. Movement patterns of young children are sporadic, omnidirectional, and unique per developmental stage (e.g., lying on back or tummy, crawling or walking), and accelerometers capture only the movement of the body segment it is attached to [15, 20, 23]. This requires accelerometers that can capture movement in multiple planes, and placement of accelerometers on different sites (e.g., wrist and hip, legs, and arms).
There are a few reasons that contributed to the (very) low quality of evidence of the studies. Firstly, the quality of evidence was mostly downgraded due to limited sample sizes of < 100 children included in studies, i.e., imprecision [26]. If more studies would have used the same measurement and analyses protocol (i.e., accelerometer brand, accelerometer data analysis approach, axis, and epoch length), this sample size issue could have been resolved by pooling the results. Besides sample size, another important aspect for the generalizability is that the variation of the performed physical behaviors in the target population is captured. Secondly, the doubtful methodological study quality contributed to the downgrading of the quality of evidence, i.e., risk of bias [26]. Common methodological limitations varied per measurement property. Regarding convergent validity, both the unknown or insufficient measurement properties of the comparison instrument and the too long epoch lengths [101] resulted in low methodological study quality. For most studies that used direct observation as comparison measure, interrater agreement was insufficient, or a non-validated observation scheme was adopted. In some studies, physical behavior of toddlers was assessed using observation schemes developed and validated in preschoolers, thereby disregarding developmental specific physical behavior. Thus, physical activities and their intensities may have been misinterpreted. In addition, an epoch length < 60 s is preferred to measure the sporadic and intermittent nature of physical behavior in young children. However, some studies reintegrated the epochs up to three minutes without providing a valid reason, e.g., to align the epochs with the comparison instrument. For studies evaluating validity of cut-points based methods, low methodological study quality was mostly due to validation using data derived under the same circumstances as for the cut-point calibration, e.g., using the same sample instead of an independent sample. Studies that assessed validity of multi-parameter methods, mainly received low methodological study quality due to not reporting statistics suitable for comparing the performance of prediction models.
Next to the low quality of evidence, there were some general study limitations. For instance, in the reliability studies, differences between accelerometer recordings might be due to slightly different placement of the accelerometer, or actual different physical behaviors during the repeated measurements. Differences based on mechanical shaker experiments, on the other hand, are purely device related. Regarding validity studies using observation as comparison measure, it is difficult to estimate what observation time would be sufficient for validation of the targeted physical intensities and representative for physical behavior. This is also dependent on the observed activities and setting. Observation durations of included studies varied from 8 to 180 min. For instance, if observation took place in the childcare setting, this might not be representative for daily life physical behavior. Another general limitation is that activity types were not described in detail, resulting in different activity intensity ranges between studies.
Strengths and limitations
A strength of this review is that the methodological study quality was systematically assessed using the newly developed CAMQAM checklist. Another strength is that our search had no publication date limit. Although this resulted in including studies on devices that are no longer available on the market, this review includes all available studies examining measurement properties of accelerometer-based methods in 0—5-year-olds. A limitation of this review is that due to the great variability of accelerometer-based methods, it was not feasible to pool the study results, resulting in low quality of evidence ratings due to small sample sizes. Appropriate sample sizes are important for precision but also in order to capture adequate variation in physical activities. Another limitation is that we were unable to rate study results of measurement errors, as the minimal important difference or minimal important change is needed to conclude on the magnitude of measurement error. Since this information was not available for 0—5-year-olds, we only described these results. A limitation of the study result rating is that, the ratings were not weighted for the number of reported results. Lastly, our focus was limited to the evaluation and quality of measurement properties and did not include feasibility. Feasibility is context-specific because studies differ in available expertise and computational resources to perform the data analysis. Further, feasibility may change over time as software is subject to ongoing development and maintenance, or lack thereof, and accelerometers may change in price or dimensions as newer models enter the market.
Recommendations for future studies
High quality studies and standardized protocols are required to assess measurement properties (including feasibility) of these accelerometer-based methods and enable pooling of data. To improve methodological study quality of future studies, we recommend using our developed CAMQAM Checklist for Assessing the Methodological Quality of studies using Accelerometer-based Methods. Future studies should incorporate more precise definitions for physical activity types, adapted to the child’s developmental stage. For example, activity types such as crawling can be more precisely defined using inclination angles in video observation or derived from accelerometer-based methods. Additionally, for accelerometer-based methods to be generalizable to young children, ideally in a free-living setting, validation studies should include a variety of physical activity types representative for the target population. Moreover, we recommend that future studies transparently share methods by making these open-source available. Making methods accessible supports the sustained impact of research investments. Given the lack of reliable and/or valid of accelerometer-based methods and the lack of 24-h studies on physical behavior, especially in the youngest age groups (i.e., infants and toddlers), future studies should develop and evaluate methods targeted at these young age groups, including all 24-h physical behaviors, and exploring different sensor placements and axes using raw acceleration data of modern accelerometers.
Conclusions
Validated cut-points are lacking in infants and toddlers, while multi-parameter methods proved valid to distinguish SB and LPA from more vigorous activities. For preschoolers, both valid cut-points based and valid multi-parameter methods were identified, where multi-parameter methods appeared to have better measurement properties. Large heterogeneity and methodological limitations, impedes our ability to draw definitive conclusions about the best available accelerometer-based methods assessing all 24-h physical behaviors combined in young children.
Supplementary Information
Additional file 1. Search strategy using MEDLINE for studies evaluating accelerometer-based methods.
Additional file 2. CAMQAM: Checklist for Assessing the Methodological Quality of studies using Accelerometer-based Methods.
Additional file 3. Description of the elements and the corresponding codes to describe accelerometer-based methods.
Acknowledgements
Not applicable.
Authors’ contributions
AL, MC, TA, and VH conceived the study. AL and TA screened all articles for eligibility. AL and JA extracted the data. AL, MC and TA rated the methodological study quality. AL completed data analysis. AL drafted the manuscript. MC, TA, and VH revised and edited significant sections of the manuscript. All authors reviewed and approved the manuscript.
Funding
This review is part of the “My Little Moves” project that is funded by ZonMw (546003008) and the Bernard van Leer foundation. The funding bodies had no role in the design of the study; in the collection, analysis, and interpretation of the data; or in the writing of the manuscript.
Availability of data and materials
The data that support the findings of this review are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Annelinde Lettink, Teatske M. Altenburg, Jelle Arts, Vincent T. van Hees, and Mai J. M. Chinapaw declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chaput JP, Carson V, Gray CE, Tremblay MS. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health. 2014;11(12):12575–81. doi: 10.3390/ijerph111212575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuzik N, Poitras VJ, Tremblay MS, Lee EY, Hunter S, Carson V. Systematic review of the relationships between combinations of movement behaviours and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(5):849. doi: 10.1186/s12889-017-4851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rollo S, Antsygina O, Tremblay MS. The whole day matters: understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci. 2020;9(6):493–510. doi: 10.1016/j.jshs.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tremblay MS, Carson V, Chaput J-P, Connor Gorber S, Dinh T, Duggan M, et al. Canadian 24-hour movement guidelines for children and youth: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2016;41(6):S311–S27. doi: 10.1139/apnm-2016-0151. [DOI] [PubMed] [Google Scholar]
- 5.Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-hour movement guidelines for the early years (0–4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17(5):874. doi: 10.1186/s12889-017-4859-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8):1575–81. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 7.Butte NF, Watson KB, Ridley K, Zakeri IF, McMurray RG, Pfeiffer KA, et al. A youth compendium of physical activities: activity codes and metabolic intensities. Med Sci Sports Exerc. 2018;50(2):246–56. doi: 10.1249/mss.0000000000001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr. 2014;1:5. doi: 10.3389/fnut.2014.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loprinzi PD, Cardinal BJ. Measuring children's physical activity and sedentary behaviors. J Exerc Sci Fit. 2011;9(1):15–23. doi: 10.1016/s1728-869x(11)60002-6. [DOI] [Google Scholar]
- 10.Park J, Kazuko IT, Kim E, Kim J, Yoon J. Estimating free-living human energy expenditure: practical aspects of the doubly labeled water method and its applications. Nutr Res Pract. 2014;8(3):241–8. doi: 10.4162/nrp.2014.8.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ndahimana D, Kim EK. Measurement methods for physical activity and energy expenditure: a review. Clin Nutr Res. 2017;6(2):68–80. doi: 10.7762/cnr.2017.6.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lynch BA, Kaufman TK, Rajjo TI, Mohammed K, Kumar S, Murad MH, et al. Accuracy of accelerometers for measuring physical activity and levels of sedentary behavior in children: a systematic review. J Prim Care Community Health. 2019;10:1–8. doi: 10.1177/2150132719874252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Vries SI, Bakker I, Hopman-Rock M, Hirasing RA, van Mechelen W. Clinimetric review of motion sensors in children and adolescents. J Clin Epidemiol. 2006;59(7):670–80. doi: 10.1016/j.jclinepi.2005.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Bruijns BA, Truelove S, Johnson AM, Gilliland J, Tucker P. Infants’ and toddlers’ physical activity and sedentary time as measured by accelerometry: a systematic review and meta-analysis. Int J Behav Nutrition Physical Act. 2020;17(1):14. doi: 10.1186/s12966-020-0912-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cliff DP, Reilly JJ, Okely AD. Methodological considerations in using accelerometers to assess habitual physical activity in children aged 0–5 years. J Sci Med Sport. 2009;12(5):557–67. doi: 10.1016/j.jsams.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Sarker H, Anderson LN, Borkhoff CM, Abreo K, Tremblay MS, Lebovic G, et al. Validation of parent-reported physical activity and sedentary time by accelerometry in young children. BMC Research Notes. 2015;8(1):735. doi: 10.1186/s13104-015-1648-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sasaki JE, John D, Freedson PS. Validation and comparison of ActiGraph activity monitors. J Sci Med Sport. 2011;14(5):411–6. doi: 10.1016/j.jsams.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 18.Weiss AR, Johnson NL, Berger NA, Redline S. Validity of activity-based devices to estimate sleep. J Clin Sleep Med. 2010;6(4):336–342. doi: 10.5664/jcsm.27874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welk GJ, Schaben JA, Morrow JR. Reliability of accelerometry-based activity monitors: a generalizability study. Med Sci Sports Exerc. 2004;36(9):1637–1645. [PubMed] [Google Scholar]
- 20.Oliver M, Schofield GM, Kolt GS. Physical activity in preschoolers. Sports Med. 2007;37(12):1045–70. doi: 10.2165/00007256-200737120-00004. [DOI] [PubMed] [Google Scholar]
- 21.Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infant and children: a systematic review of observational studies. Sleep Med Rev. 2012;16(3):213–22. doi: 10.1016/j.smrv.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Adolph KE, Franchak JM. The development of motor behavior. Wiley Interdiscip Rev Cog Sci. 2017;8(1–2):e1430. doi: 10.1002/wcs.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gerber RJ, Wilks T, Erdie-Lalena C. Developmental milestones: motor development. Pediatr Rev. 2010;31(7):267–77. doi: 10.1542/pir.31-7-267. [DOI] [PubMed] [Google Scholar]
- 24.Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med. 2021;18(3):e1003583. doi: 10.1371/journal.pmed.1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mokkink LB, De Vet HC, Prinsen CA, Patrick DL, Alonso J, Bouter LM, et al. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1171–9. doi: 10.1007/s11136-017-1765-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prinsen CA, Mokkink LB, Bouter LM, Alonso J, Patrick DL, De Vet HC, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57. doi: 10.1007/s11136-018-1798-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Terwee CB, Prinsen CA, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27(5):1159–70. doi: 10.1007/s11136-018-1829-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Terwee CB, Mokkink LB, van Poppel MN, Chinapaw MJ, van Mechelen W, de Vet HC. Qualitative attributes and measurement properties of physical activity questionnaires. Sports Med. 2010;40(7):525–37. doi: 10.2165/11531370-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 29.Greenspan B, Cunha AB, Lobo MA. Design and validation of a smart garment to measure positioning practices of parents with young infants. Infant Behav Dev. 2021;62:101530. doi: 10.1016/j.infbeh.2021.101530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Galland BC, Kennedy GJ, Mitchell EA, Taylor BJ. Algorithms for using an activity-based accelerometer for identification of infant sleep-wake states during nap studies. Sleep Med. 2012;13(6):743–51. doi: 10.1016/j.sleep.2012.01.018. [DOI] [PubMed] [Google Scholar]
- 31.Insana SP, Gozal D, Montgomery-Downs HE. Invalidity of one actigraphy brand for identifying sleep and wake among infants. Sleep Med. 2010;11(2):191–6. doi: 10.1016/j.sleep.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rioualen S, Roué JM, Lefranc J, Gouillou M, Nowak E, Alavi Z, et al. Actigraphy is not a reliable method for measuring sleep patterns in neonates. Acta Paediatr. 2015;104(11):e478–82. doi: 10.1111/apa.13088. [DOI] [PubMed] [Google Scholar]
- 33.Camerota M, Tully KP, Grimes M, Gueron-Sela N, Propper CB. Assessment of infant sleep: how well do multiple methods compare? Sleep. 2018;41(10):zsy146. doi: 10.1093/sleep/zsy146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hewitt L, Stanley RM, Cliff D, Okely AD. Objective measurement of tummy time in infants (0–6 months): a validation study. PLoS One. 2019;14(2):e0210977. doi: 10.1371/journal.pone.0210977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lewicke AT, Sazonov ES, Schuckers SA. Sleep-wake identification in infants : heart rate variability compared to actigraphy. Conf Proc IEEE Eng Med Biol Soc. 2004;1:442–5. doi: 10.1109/IEMBS.2004.1403189. [DOI] [PubMed] [Google Scholar]
- 36.Gnidovec B, Neubauer D, Zidar J. Actigraphic assessment of sleep-wake rhythm during the first 6 months of life. Clin Neurophysiol. 2002;113(11):1815–21. doi: 10.1016/s1388-2457(02)00287-0. [DOI] [PubMed] [Google Scholar]
- 37.Horger MN, Marsiliani R, DeMasi A, Allia A, Berger SE. Researcher choices for infant sleep assessment: parent report, actigraphy, and a novel video system. J Genet Psychol. 2021;182(4):218–35. doi: 10.1080/00221325.2021.1905600. [DOI] [PubMed] [Google Scholar]
- 38.Sadeh A, Acebo C, Seifer R, Aytur S, Carskadon MA. Activity-based assessment of sleep-wake patterns during 1st year of life. Infant Behav Dev. 1995;18(3):329–37. doi: 10.1016/0163-6383(95)90021-7. [DOI] [Google Scholar]
- 39.Airaksinen M, Räsänen O, Ilén E, Häyrinen T, Kivi A, Marchi V, et al. Automatic posture and movement tracking of infants with wearable movement sensors. Sci Rep. 2020;10(1):169. doi: 10.1038/s41598-019-56862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jun K, Choi S. Unsupervised end-to-end deep model for newborn and infant activity recognition. Sensors (Basel) 2020;20(22):6467. doi: 10.3390/s20226467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith BA, Trujillo-Priego IA, Lane CJ, Finley JM, Horak FB. Daily quantity of infant leg movement: wearable sensor algorithm and relationship to walking onset. Sensors (Basel) 2015;15(8):19006–20. doi: 10.3390/s150819006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hager ER, Gormley CE, Latta LW, Treuth MS, Caulfield LE, Black MM. Toddler physical activity study: laboratory and community studies to evaluate accelerometer validity and correlates. BMC Public Health. 2016;16(6):936. doi: 10.1186/s12889-016-3569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pulakka A, Cheung YB, Ashorn U, Penpraze V, Maleta K, Phuka JC, et al. Feasibility and validity of the ActiGraph GT3X accelerometer in measuring physical activity of Malawian toddlers. Acta Paediatr. 2013;102(12):1192–8. doi: 10.1111/apa.12412. [DOI] [PubMed] [Google Scholar]
- 44.Trost SG, Fees BS, Haar SJ, Murray AD, Crowe LK. Identification and validity of accelerometer cut-points for toddlers. Obesity (Silver Spring) 2012;20(11):2317–9. doi: 10.1038/oby.2011.364. [DOI] [PubMed] [Google Scholar]
- 45.van Cauwenberghe E, Gubbels J, De Bourdeaudhuij I, Cardon G. Feasibility and validity of accelerometer measurements to assess physical activity in toddlers. Int J Behav Nutr Phys Act. 2011;8:67. doi: 10.1186/1479-5868-8-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Costa S, Barber SE, Cameron N, Clemes SA. Calibration and validation of the ActiGraph GT3X+ in 2–3 year olds. J Sci Med Sport. 2014;17(6):617–22. doi: 10.1016/j.jsams.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 47.Oftedal S, Bell KL, Davies PS, Ware RS, Boyd RN. Validation of accelerometer cut points in todlers with and without cerebral palsy. Med Sci Sports Exerc. 2014;46(9):1808–15. doi: 10.1249/MSS.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 48.Albert MV, Sugianto A, Nickele K, Zavos P, Sindu P, Ali M, et al. Hidden Markov model-based activity recognition for toddlers. Physiol Meas. 2020;41(2):025003. doi: 10.1088/1361-6579/ab6ebb. [DOI] [PubMed] [Google Scholar]
- 49.Kwon S, Zavos P, Nickele K, Sugianto A, Albert MV. Hip and wrist-worn accelerometer data analysis for toddler activities. Int J Environ Res Public Health. 2019;16(14). 10.3390/ijerph16142598 [DOI] [PMC free article] [PubMed]
- 50.Nam Y, Park JW. Child activity recognition based on cooperative fusion model of a triaxial accelerometer and a barometric pressure sensor. IEEE J Biomed Health Inform. 2013;17(2):420–6. doi: 10.1109/JBHI.2012.2235075. [DOI] [PubMed] [Google Scholar]
- 51.Adolph AL, Puyau MR, Vohra FA, Nicklas TA, Zakeri IF, Butte NF. Validation of uniaxial and triaxial accelerometers for the assessment of physical activity in preschool children. J Phys Act Health. 2012;9(7):944–53. doi: 10.1123/jpah.9.7.944. [DOI] [PubMed] [Google Scholar]
- 52.Pate RR, Almeida MJ, McIver KL, Pfeiffer KA, Dowda M. Validation and calibration of an accelerometer in preschool children. Obesity (Silver Spring) 2006;14(11):2000–6. doi: 10.1038/oby.2006.234. [DOI] [PubMed] [Google Scholar]
- 53.Pfeiffer KA, McIver KL, Dowda M, Almeida MJ, Pate RR. Validation and calibration of the Actical accelerometer in preschool children. Med Sci Sports Exerc. 2006;38(1):152–7. doi: 10.1249/01.mss.0000183219.44127.e7. [DOI] [PubMed] [Google Scholar]
- 54.Sijtsma A, Schierbeek H, Goris AH, Joosten KF, van Kessel I, Corpeleijn E, et al. Validation of the TracmorD triaxial accelerometer to assess physical activity in preschool children. Obesity (Silver Spring) 2013;21(9):1877–83. doi: 10.1002/oby.20401. [DOI] [PubMed] [Google Scholar]
- 55.Zakeri IF, Adolph AL, Puyau MR, Vohra FA, Butte NF. Cross-sectional time series and multivariate adaptive regression splines models using accelerometry and heart rate predict energy expenditure of preschoolers. J Nutr. 2013;143(1):114–22. doi: 10.3945/jn.112.168542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alhassan S, Sirard JR, Kurdziel LBF, Merrigan S, Greever C, Spencer RMC. Cross-validation of two accelerometers for assessment of physical pctivity and sedentary time in preschool children. Pediatr Exerc Sci. 2017;29(2):268–77. doi: 10.1123/pes.2016-0074. [DOI] [PubMed] [Google Scholar]
- 57.Djafarian K, Speakman JR, Stewart J, Jackson DM. Comparison of activity levels measured by a wrist worn accelerometer and direct observation in young children. Open J Pediatr. 2013;3(04):422–7. doi: 10.4236/ojped.2013.34076. [DOI] [Google Scholar]
- 58.Dobell AP, Eyre ELJ, Tallis J, Chinapaw MJM, Altenburg TM, Duncan MJ. Examining accelerometer validity for estimating physical activity in pre-schoolers during free-living activity. Scand J Med Sci Sports. 2019;29(10):1618–28. doi: 10.1111/sms.13496. [DOI] [PubMed] [Google Scholar]
- 59.Fairweather SC, Reilly J, Grant S, Whittaker A, Paton JY. Using the Computer Science and Applications (CSA) activity monitor in preschool children. Pediatr Exerc Sci. 1999;11(4):413–20. doi: 10.1123/pes.11.4.413. [DOI] [Google Scholar]
- 60.Finn KJ, Specker B. Comparison of Actiwatch activity and Children's Activity Rating scale in children. Med Sci Sports Exerc. 2000;32(10):1794–7. doi: 10.1097/00005768-200010000-00021. [DOI] [PubMed] [Google Scholar]
- 61.Hislop JF, Bulley C, Mercer TH, Reilly JJ. Comparison of accelerometry cut points for physical activity and sedentary behavior in preschool children: a validation study. Pediatr Exerc Sci. 2012;24(4):563–76. doi: 10.1123/pes.24.4.563. [DOI] [PubMed] [Google Scholar]
- 62.Klesges LM, Klesges RC. The assessment of children's physical activity: a comparison of methods. Med Sci Sports Exerc. 1987;19(5):511–517. doi: 10.1249/00005768-198710000-00015. [DOI] [PubMed] [Google Scholar]
- 63.Klesges RC, Klesges LM, Swenson AM, Pheley AM. A validation of two motion sensors in the prediction of child and adult physical activity levels. Am J Epidemiol. 1985;122(3):400–10. doi: 10.1093/oxfordjournals.aje.a114121. [DOI] [PubMed] [Google Scholar]
- 64.van Cauwenberghe E, Wooller L, Mackay L, Cardon G, Oliver M. Comparison of Actical and activPAL measures of sedentary behaviour in preschool children. J Sci Med Sport. 2012;15(6):526–31. doi: 10.1016/j.jsams.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 65.Aadland E, Johannessen K. Agreement of objectively measured physical activity and sedentary time in preschool children. Prev Med Rep. 2015;2:635–9. doi: 10.1016/j.pmedr.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bélanger ME, Bernier A, Paquet J, Simard V, Carrier J. Validating actigraphy as a measure of sleep for preschool children. J Clin Sleep Med. 2013;9(7):701–6. doi: 10.5664/jcsm.2844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Roscoe CMP, James RS, Duncan MJ. Calibration of GENEActiv accelerometer wrist cut-points for the assessment of physical activity intensity of preschool aged children. Eur J Pediatr. 2017;176(8):1093–8. doi: 10.1007/s00431-017-2948-2. [DOI] [PubMed] [Google Scholar]
- 68.de Bock F, Menze J, Becker S, Litaker D, Fischer J, Seidel I. Combining accelerometry and HR for assessing preschoolers' physical activity. Med Sci Sports Exerc. 2010;42(12):2237–43. doi: 10.1249/MSS.0b013e3181e27b5d. [DOI] [PubMed] [Google Scholar]
- 69.Ettienne R, Nigg CR, Li F, Su Y, McGlone K, Luick B, et al. Validation of the Actical accelerometer in multiethnic preschoolers: The Children's Healthy Living (CHL) program. Hawai'i J Med Public Health. 2016;75(4):95–100. [PMC free article] [PubMed] [Google Scholar]
- 70.Hislop JF, Bulley C, Mercer TH, Reilly JJ. Comparison of epoch and uniaxial versus triaxial accelerometers in the measurement of physical activity in preschool children: a validation study. Pediatr Exerc Sci. 2012;24(3):450–60. doi: 10.1123/pes.24.3.450. [DOI] [PubMed] [Google Scholar]
- 71.Kahan D, Nicaise V, Reuben K. Convergent validity of four accelerometer cutpoints with direct observation of preschool children's outdoor physical activity. Res Q Exerc Sport. 2013;84(1):59–67. doi: 10.1080/02701367.2013.762294. [DOI] [PubMed] [Google Scholar]
- 72.Martin A, Mcneil M, Penpraze V, Dall P, Granat M, Paton JY, et al. Objective measurement of habitual sedentary behavior in pre-school children: comparison of activPAL with Actigraph monitors. Pediatr Exerc Sci. 2011;23(4):468–76. doi: 10.1123/pes.23.4.468. [DOI] [PubMed] [Google Scholar]
- 73.Pagels P, Boldemann C, Raustorp A. Comparison of pedometer and accelerometer measures of physical activity during preschool time on 3- to 5-year-old children. Acta Paediatr. 2011;100(1):116–20. doi: 10.1111/j.1651-2227.2010.01962.x. [DOI] [PubMed] [Google Scholar]
- 74.Pereira JR, Sousa-Sá E, Zhang Z, Cliff DP, Santos R. Concurrent validity of the ActiGraph GT3X+ and activPAL for assessing sedentary behaviour in 2–3-year-old children under free-living conditions. J Sci Med Sport. 2020;23(2):151–6. doi: 10.1016/j.jsams.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 75.Butte NF, Wong WW, Lee JS, Adolph AL, Puyau MR, Zakeri IF. Prediction of energy expenditure and physical activity in preschoolers. Med Sci Sports Exerc. 2014;46(6):1216–26. doi: 10.1249/mss.0000000000000209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hislop J, Palmer N, Anand P, Aldin T. Validity of wrist worn accelerometers and comparability between hip and wrist placement sites in estimating physical activity behaviour in preschool children. Physiol Meas. 2016;37(10):1701–14. doi: 10.1088/0967-3334/37/10/1701. [DOI] [PubMed] [Google Scholar]
- 77.Johansson E, Ekelund U, Nero H, Marcus C, Hagströmer M. Calibration and cross-validation of a wrist-worn Actigraph in young preschoolers. Pediatr Obes. 2015;10(1):1–6. doi: 10.1111/j.2047-6310.2013.00213.x. [DOI] [PubMed] [Google Scholar]
- 78.Johansson E, Larisch LM, Marcus C, Hagströmer M. Calibration and validation of a wrist- and hip-worn Actigraph accelerometer in 4-year-old children. PLoS One. 2016;11(9):e0162436. doi: 10.1371/journal.pone.0162436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li S, Howard JT, Sosa ET, Cordova A, Parra-Medina D, Yin Z. Calibrating wrist-worn accelerometers for physical activity assessment in prechoolers : machine learning approaches. JMIR Form Res. 2020;4(8):e16727. doi: 10.2196/16727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Reilly JJ, Coyle J, Kelly L, Burke G, Grant S, Paton JY. An objective method for measurement of sedentary behavior in 3- to 4-year olds. Obes Res. 2003;11(10):1155–8. doi: 10.1038/oby.2003.158. [DOI] [PubMed] [Google Scholar]
- 81.Sirard J, Trost S, Pfeiffer K, Dowda M, Pate R. Calibration and evaluation of an objective measure of physical activity in preschool children. J Phys Act Health. 2005;2(3):345–57. doi: 10.1123/jpah.2.3.345. [DOI] [Google Scholar]
- 82.Davies G, Reilly J, McGowan AJ, Dall P, Granat M, Paton JY. Validity, practical utility, and reliability of the Activpal in preschool children. Med Sci Sports Exerc. 2012;44(4):761–8. doi: 10.1249/MSS.0b013e31823b1dc7. [DOI] [PubMed] [Google Scholar]
- 83.Ahmadi MN, Brookes D, Chowdhury A, Pavey T, Trost SG. Free-living evaluation of laboratory-based activity classifiers in preschoolers. Med Sci Sports Exerc. 2020;52(5):1227–34. doi: 10.1249/mss.0000000000002221. [DOI] [PubMed] [Google Scholar]
- 84.Ahmadi MN, Chowdhury A, Pavey T, Trost SG. Laboratory-based and free-living algorithms for energy expenditure estimation in preschool children: a free-living evaluation. PLoS One. 2020;15(5):e0233229. doi: 10.1371/journal.pone.0233229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ahmadi MN, Pavey TG, Trost SG. Machine learning models for classifying physical activity in free-living preschool children. Sensors (Basel). 2020;20(16). 10.3390/s20164364 [DOI] [PMC free article] [PubMed]
- 86.Brønd JC, Grøntved A, Andersen LB, Arvidsson D, Olesen LG. Simple method for the objective activity type assessment with preschoolers, children and adolescents. Children (Basel). 2020;7(7). 10.3390/children7070072 [DOI] [PMC free article] [PubMed]
- 87.Hagenbuchner M, Cliff DP, Trost SG, Van Tuc N, Peoples GE. Prediction of activity type in preschool children using machine learning techniques. J Sci Med Sport. 2015;18(4):426–31. doi: 10.1016/j.jsams.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 88.Steenbock B, Wright MN, Wirsik N, Brandes M. Accelerometry-based prediction of energy expenditure in preschoolers. J Meas Phys Behav. 2019;2(2):94–102. doi: 10.1123/jmpb.2018-0032. [DOI] [Google Scholar]
- 89.Trost SG, Cliff DP, Ahmadi MN, Tuc NV, Hagenbuchner M. Sensor-enabled activity class recognition in prechoolers: hip versus wrist Data. Med Sci Sports Exerc. 2018;50(3):634–41. doi: 10.1249/MSS.0000000000001460. [DOI] [PubMed] [Google Scholar]
- 90.Zhao W, Adolph AL, Puyau MR, Vohra FA, Butte NF, Zakeri IF. Support vector machines classifiers of physical activities in preschoolers. Physiol Rep. 2013;1(1):e00006. doi: 10.1002/phy2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 92.Sadeh A, Lavie P, Scher A, Tirosh E, Epstein R. Actigraphic home-monitoring sleep-disturbed and control infants and young children: a new method for pediatric assessment of sleep-wake patterns. Pediatrics. 1991;87(4):494–499. [PubMed] [Google Scholar]
- 93.Redmond DP, Hegge FW. Observations on the design and specification of a wrist-worn human activity monitoring system. Behav Res Methods Instrum Comput. 1985;17(6):659–69. doi: 10.3758/BF03200979. [DOI] [Google Scholar]
- 94.Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31(3):395–401. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ekblom O, Nyberg G, Bak EE, Ekelund U, Marcus C. Validity and comparability of a wrist-worn accelerometer in children. J Phys Act Health. 2012;9(3):389–93. doi: 10.1123/jpah.9.3.389. [DOI] [PubMed] [Google Scholar]
- 96.Kelly LA, Villalpando J, Carney B, Wendt S, Haas R, Ranieri BJ, et al. Development of Actigraph GT1M accelerometer cut-points for young children aged 12–36 months. J Athl Enhanc. 2016;5(4):1–4. doi: 10.4172/2324-9080.1000235. [DOI] [Google Scholar]
- 97.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–7. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 98.Schaefer CA, Nigg CR, Hill JO, Brink LA, Browning RC. Establishing and evaluating wrist cutpoints for the GENEActiv accelerometer in youth. Med Sci Sports Exerc. 2014;46(4):826–33. doi: 10.1249/MSS.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sun DX, Schmidt G, Teo-Koh SM. Validation of the RT3 accelerometer for measuring physical activity of children in simulated free-living conditions. Pediatr Exerc Sci. 2008;20(2):181–97. doi: 10.1123/pes.20.2.181. [DOI] [PubMed] [Google Scholar]
- 100.Sitnick SL, Goodlin-Jones BL, Anders TF. The use of actigraphy to study sleep disorders in preschoolers: some concerns about detection of nighttime awakenings. Sleep. 2008;31(3):395. doi: 10.1093/sleep/31.3.395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Altenburg TM, Wang X, van Ekris E, Andersen LB, Møller NC, Wedderkopp N, et al. The consequences of using different epoch lengths on the classification of accelerometer based sedentary behaviour and physical activity. PLOS ONE. 2021;16(7):e0254721. doi: 10.1371/journal.pone.0254721. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy using MEDLINE for studies evaluating accelerometer-based methods.
Additional file 2. CAMQAM: Checklist for Assessing the Methodological Quality of studies using Accelerometer-based Methods.
Additional file 3. Description of the elements and the corresponding codes to describe accelerometer-based methods.
Data Availability Statement
The data that support the findings of this review are available from the corresponding author upon reasonable request.