Abstract
Objective
Healthy Habits, Happy Homes (4H) is a home-based, pre-school childhood obesity prevention intervention which demonstrated efficacy in North America which we translated to Scotland (4HS) by considering contextual factors and adapting study design. RE-AIM Framework was used to assess 1) extent to which development of 4HS intervention (including recruitment) was participatory and inclusive; 2) feasibility of translating a complex public health intervention from one setting to another; 3) extent to which translation was pragmatic and 4) fidelity of intervention to the principles of Motivational Interviewing (MI).
Study design
Feasibility testing, process evaluation and measurements of intervention fidelity were undertaken to evaluate the translation of 4H to an economically deprived area of Scotland (4HS).
Methods
4HS study processes; participatory approach, recruitment methods, level of pragmatism were evaluated using the RE-AIM framework. Qualitative and quantitative measures identified key implementation features and functioning of 4HS intervention. Fidelity MI principles was determined through coding of audiotapes using Motivation Interviewing Treatment Integrity (MITI) code.
Results
Key facilitators for positive impact with families, included: inclusive recruitment methods, appropriate channels of communication and correspondence (Reach) with n = 126 enquiries and n = 26 (21%) families recruited. Positive links with local parents and community workers integral to the research process at n = 9 meetings (Effectiveness). 61.5% of families lived in the most deprived data zone in Scotland, 23% were one parent families, thus awareness and consideration of local contextual factors (Adoption) and locally relevant materials were important. 4HS was feasible to deliver, pragmatic in nature and intervention demonstrated good fidelity to MI (Implementation).
Conclusion
Translation of 4H from North America to Scotland was successful. Future studies should consider implementation of 4HS approach within routine practice within the UK (practice based evidence) or through thoughtful evaluation in a future trial (evidence based practice).
Keywords: Childhood obesity prevention, Translation, Process evaluation, RE-AIM
Highlights
-
•
Translated of a pre-school, home-based obesity prevention intervention in areas of economic deprivation.
-
•
Use of RE-AIM original and pragmatic forms for feasibility testing and process evaluation.
-
•
Key facilitators for positive impact: inclusive recruitment, appropriate communication, positive links with parents & workers.
-
•
Study was; feasible to deliver, pragmatic in nature, able to demonstrate good fidelity to MI.
1. Introduction
Worldwide too many children and young people live with a Body Mass Index (BMI) that is above the healthy range. Globally, at least 124 million school age children [1] and a further 38 million pre-school children [2] are now thought to live with obesity as defined by high BMI-for-age. In the UK, annual surveillance data determines the proportion of children within each BMI category, including overweight or obesity. Within Scotland, this data is currently collected and reported at one time point; when children enter the first year of primary school (aged 4 – 5years). Latest figures in 2017/18 highlighted that more than 1 in 5 (22.4%) children growing up in Scotland, have a BMI >85th percentile relative to UK1990 reference data [3].
Pre-school children and particularly those living in areas of disadvantage are especially vulnerable to obesity. Consistently, for more than 15 years, the proportion of children who have a BMI within the healthy range has reduced for those growing up in Scottish communities experiencing poverty. For example, Dundee City has consistently had rates of overweight and obesity that are higher than the national average, due in part, to the city’s higher than average level of economic deprivation [3].
Obesity in childhood is known to track into adolescence and adulthood, often leading to consequences associated with weight bias and stigma [4] and linked to physical and mental ill health [5,6]. Causes of childhood obesity are complex and multifactorial, and addressing the problem requires an understanding of the wider environment and the many other influencing elements that impact on energy balance related behaviours in children and their families. Although evidence is still emerging on the effectiveness of Whole Systems Approaches to tackling obesity [7], it is recognised that increasing the proportion of children who have a BMI within the healthiest range requires action in all areas within the complex and adaptive systems of the obesogenic environment [[8], [9], [10]].
Interventions that enable parents to support their children to be as healthy as possible, in the places where they live, can be one important action within a whole system approach to obesity prevention in that, the intervention is one, inter-connected event, within a system. For the pre-school age group, obesity prevention interventions that focus on household routines, use behavioural change techniques, involve parents and are culturally appropriate are most effective [11]. One such intervention that targets the most obesity-promoting behaviours, is relatively low cost, has evidence of efficacy [12] and is a valuable home-based intervention, is Healthy Habits Happy Homes (4H) [13].
Recently, the original 4H was adapted, piloted and rolled out in Canada. The original 4H and Canadian pilot study used Motivational Interviewing (MI), behaviour change approach within the home setting with pre-school children and their families [14,15]. Translating efficacious interventions from one setting to another might provide an efficient and rapid means of implementing obesity prevention research trials, and ultimately obesity prevention programmes as part of public health services.
In a previous paper [16] we described the rationale for translating the highly promising (efficacious and low-cost) 4H to Scotland (4HS), developed a study logic model and theory of change and outlined crucial information about the context in which the feasibility study would take place. Children living in the North East area within the city of Dundee are twice as likely to have obesity by the time they start primary school compared to their peers who grow up across the city in the wealthiest neighbourhoods [3]. Plans were outlined for assessing the extent to which the translation process of 4HS was participatory and inclusive, and the extent to which the Scottish version of the intervention was faithful to the principles of MI by means of relevant models that would allow process evaluation.
The RE-AIM planning and evaluation framework [17] provides a useful tool for appraisal of interventions across five dimensions (R-reach, E-effectiveness, A-adoption, I-implementation and M-maintenance). More recently, RE-AIM has evolved to offer pragmatic use of the 5 key dimensions to facilitate successful, wide-ranging and equitable population-based impact and is particularly suitable for translating interventions in public health [18].
The aims of the present study are therefore to utilise the RE-AIM framework, both in its original and pragmatic forms, to; 1) outline the processes involved in achieving a participative and inclusive approach to translation of 4HS, a complex public health intervention; 2) evaluate feasibility parameters of the translation process, highlighting pragmatic features; 3) assess fidelity of the delivered intervention to the principles of MI.
2. Methods
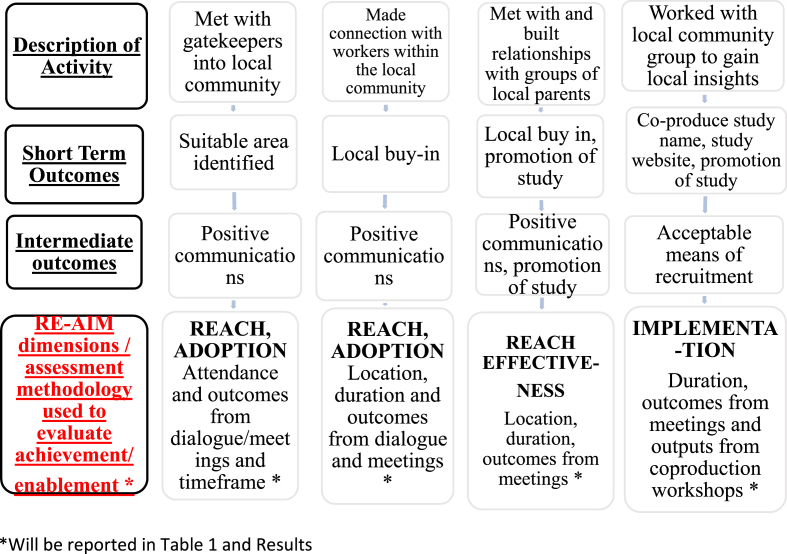
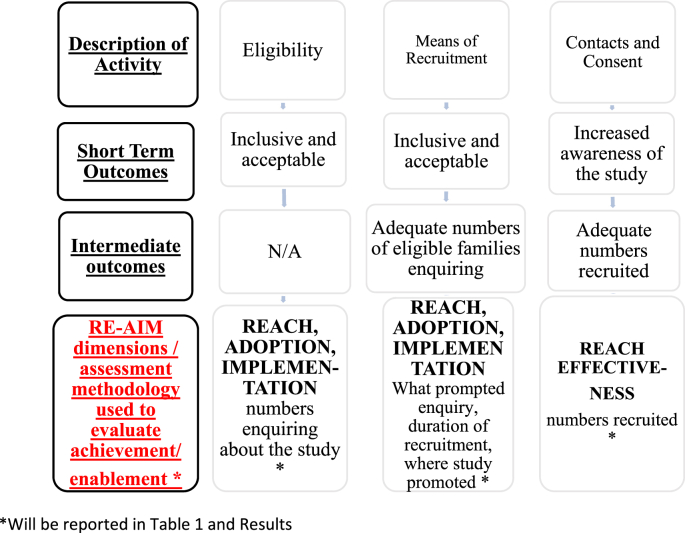
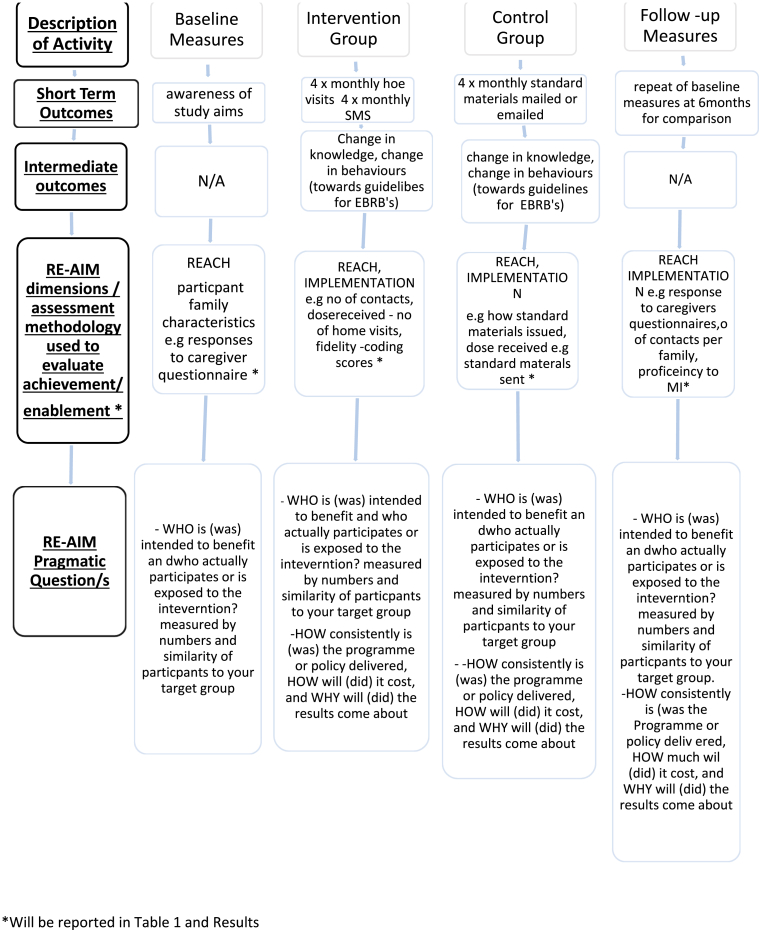
This methods section outlines 4HS research processes undertaken by JG, through an iterative process, between December 2016–May 2019 in order to address the 3 study aims. The original 5 dimensions of RE-AIM were matched with RE-AIM pragmatic questions to create an assessment methodology (summarised in Fig. 1, Fig. 2, Fig. 3) suitable to reflect the contextual factors within this community setting.
Fig. 1.
Participatory methods of 4HS
Fig. 2.
Inclusive recruitment Methods.
Fig. 3.
4HS intervention methods.
2.1. Summary of participatory methods of 4HS (linked to aim 1 & 2)
2.2. Summary of 4HS inclusive recruitment process (linked to aims 1 & 2)
The early stage of the 4HS study that are described in Fig. 1, Fig. 2, took approximately 12months and was considered important ‘groundwork’ for subsequent delivery of the 4HS intervention.
2.3. Summary of 4HS intervention and evaluation of the translation process (linked to aim 2)
Following successful participatory and inclusive recruitment approach, delivery of the 4HS intervention, was carried out by one researcher (JG) and took place over a period of 15 months. Fig. 3, below, summarises the intervention methods, with full details described elsewhere [16]. RE-AIM dimensions and pragmatic questions [18] are included in Fig. 3, creating an assessment methodology to determine pragmatic translation and feasibility of 4HS. In summary, the intervention component of 4HS randomised controlled feasibility trial involved monthly contact with n = 26 families over a 6month period. The intervention group experienced monthly visits to the home, using MI approach and fortnightly SMS to support positive lifestyle changes linked to four Energy Balance Related Behaviours (EBRB) of sleep, physical activity, screen time and family meal routine, measured at baseline and 6months using a range of objective and subjective measures. The control group received general healthy lifestyle information linked to sleep routine, family meals, physical activity and screen time each month mailed or emailed. The only eligibility criteria was that the family lived in the NE of Dundee and had at least one child aged 2–5years.
2.4. Measures of fidelity of the intervention to the principles of Motivational Interviewing (linked to aim 3)
Fidelity to the planned intervention and in particular adherence to an MI approach was measured using the Motivational Treatment Integrity (MITI 4) coding system [19,20]. A practitioner with expertise in MI (LS) who was independent of the research evaluated audio recordings of 5 (10%) of randomly selected home visits during the intervention trial. A similar proportion were evaluated in the Canadian pilot [15]. Full recordings from the whole visits (ranging from 25-65mins in length) were examined. A coding sheet was used for each recording to allow a global rating score of technical and relational elements and also a count for the coder to tally instances of 10 interview behaviours.
MITI 4 allows for a global ratings score to give an overall impression of the use of MI with behaviour counts also used in assessing competency. The MITI tool is the most commonly used to evaluate fidelity of MI and it has been used in a range of research settings [19]. In order to determine proficiency (basic – competent) to MI, summary scores serve as useful measures [20].
3. Results
Table 1 highlights the Reach, Effectiveness, Adoption, Implementation, Maintenance features of 4HS captured with both qualitative (e.g., themes from meetings/group discussions) and quantitative data (e.g, basic descriptive statistics of participant characteristics). Table 2 indicates the self-assessment score calculated for key features of 4HS translation processes using RE-AIM pragmatic questions [18].
Table 1.
Evaluation of Healthy Habits Happy Homes Scotland (4HS) Translational Processes using RE-AIM.
| Component of study | RE-AIM Dimensions & Features of 4HS Study | Process & Feasibility Results Demonstrating Achievement or Enablement of: Aim 1 (participatory and inclusive approach) and Aim 2 (feasibility of translated intervention) |
|---|---|---|
| Participatory Approach (aim 1) | Reach | R |
|
|
|
|
|
|
|
|
|
|
|
|
| Effectiveness | E | |
|
|
|
| Adoption (setting/context) | A | |
|
|
|
|
|
|
|
|
|
|
I | |
| Implementation |
|
|
|
M N/A – will be adressed in a later mixed methods outcome paper | |
| Maintenance | ||
|
||
| Inclusive recruitment (aim 1) | Reach | R |
|
|
|
|
|
|
| Effectiveness |
|
|
|
|
|
| Adoption | E N/A -will be addressed in a later mixed methods outcome paper | |
|
A | |
| Implementation |
|
|
|
I | |
| Maintenance |
|
|
|
M N/A – will be addressed in a later, mixed methods, outcomes paper | |
| Feasibility of translating 4HS (aim 2) | Reach | R |
|
|
|
| Effectiveness |
|
|
|
E N/A – will be addressed in a later, mixed methods, outcomes paper | |
| Adoption | A N/A - will be addressed in a later, mixed methods, outcomes paper | |
|
I | |
| Implementation |
|
|
|
|
|
| Maintenance |
|
|
|
M N/A– will be addressed in a later, mixed methods, outcomes paper |
As defined by Scottish Index Of Multiple Deprivation SIMD quintile 1, contains the 20% most deprived data zones in Scotland.
Table 2.
Pragmatic features of 4HS using RE-AIM; dimensions, pragmatic questions and self rating score.
| RE-AIM Dimensiona | Key Pragmatic Questions Consideredb | Features of 4HS that support pragmatic criteria | RE-AIM dimensional self ratingc |
|---|---|---|---|
| Reach At the level of patients, clients, or participants. Important to consider not only how many persons participate out of those intended or targeted, but also the characteristics of those who take part compared with those who do not. Given the impact of health disparities, participation levels of various key underserved and vulnerable subgroups are especially important. | WHO is (was) intended to benefit and who actually participates or is exposed to the intervention? Measured by number and similarity of participants to your target group. |
|
9 |
| Effectiveness at the patient, client, citizen, or participant level. Responses to this question include defining the key or desired outcomes and the impact on different subgroups (eg, men vs women; those at high risk vs those at low risk; those with high incomes or education vs those with low incomes or education). Additional outcomes include quality of life indicators and any negative effects or unintended consequences from the program. | WHAT are (were) the most important benefits you are trying to achieve and what is (was) the likelihood of negative outcomes? Measured by change on key outcome(s) and consistency across subgroups. |
|
8 |
| Adoption participation is critical to understand the number and types of organizations, clinics, or agencies that initiate a program or policy. This participation involves considering the characteristics of the settings that are approached or targeted to participate compared with those that actually do. It also involves understanding barriers to and facilitators of adoption as well as how the program or policy fits with organizational priorities and existing workflow. | WHERE is (was) the program or policy applied and WHO applied it? Measured by what settings and staff take up the intervention and which do not. |
|
8 |
| Implementation How questions also include the organizational resources that are required and how much the policy or program costs to implement. At minimum, it is important to report the time and staff resources required so that people in other settings can decide if they have the resources to adopt a program or policy. | HOW consistently is (was) the program or policy delivered, HOW will it be (was it) adapted, HOW much will (did) it cost, and WHY will (did) the results come about? |
|
8 |
| Maintenance This dimension can be operationalized as the sustainability of the policy or program and includes consideration of many factors, including but not limited to resource availability; alignment of the policy or program with organizational mission, objectives, and goals; and integration into job descriptions and performance evaluations. | WHEN will (was) the initiative become operational; how long will (was) it be sustained (setting level); and how long are the results sustained (individual level)? Measured by longevity of effects (individual level) and program sustainability (setting level). |
|
8 |
(9–10 = excellent, 7–8, good but could do with a little work, 5–6 = fair, need planning <5 needs serious attention).
3.1. Description of 4HS study translational processes in achieving a pragmatic and inclusive approach (aim 1)
3.1.1. Participatory approach
Estimated time invested by the researcher in activities associated with the participatory approach, outlined in Table 1 was approximately 8–10 h per week for 9 months. This involved an iterative process of making links with strategic workers at n = 4 meetings and local parents and community workers integral to the research process at n = 9 meetings. Information on ‘Adoption’is found in Table 1 highlighting the levels of deprivation and childhood obesity (at age 4–5years) within Dundee City. During the five co-production workshops, there was strong feeling that no limits should be set with regard eligibility criteria for recruitment of children with additonal support needs or physical disabilities. Details key points discussed and dates of co-production workshops are attached (supplementary file 1). A study website was co-created with group members with a focus on local imagery and simple language and the name of the intervention trial became the ‘Dundee Family Health Study’. The North East area of Dundee was purposively selected and no further setting exclusions were set, a defining characteristic of a pragmatic trial. 40% of households within the North East area sit within the 15% most deprived data zones in Scotland, and in two of the neighbourhoods this value is 65% and 96% respectively [21].
3.1.2. Inclusive recruitment
Approximately 5 h per week for 10 months was the time required by the researcher to ensure there was an inclusive recruitment strategy, as summarised in Table 1. The ‘Reach’ of the inclusive recruitment strategy is demonstrated by the number of enquiries and means of recruitment outline in Table 1. Two positive articles that were published in local newspapers, and on their social media site, proved a popular means by which people made contact and enquired about the study with n = 16 and n = 9 enquiries respectively. Supplementary File 2 shows one of the newspaper articles. Characteristics of the families who signed up to the intervention trial are shown under ‘Adoption’, in Table 1, demonstrating representativeness of the local population, an essential feature of a pragmatic trial. Here, there was a high proportion of one-parent families or lead parent not in employment. A total of n = 126 families made contact with the researcher to enquire about the study with 1 in 5 (n = 26) of them enrolling in the study.
3.2. Evaluation and feasibility of pragmatic features of 4HS translation process (aim 2)
Based on discussions during five workshops it was felt that overall the original 4H intervention materials were appropriate, with only small alterations required. For example, the words or language used were amended (simple non jargon, non ‘american’ e.g., remove soda), preferences for locally relevant photographs and images to be used within the materials and the use of colours that were not associated with either of the two city (Dundee) football teams. The number of contacts made with families involved in 4HS intervention are outlined in Table 1 under ‘implementation’. The 4HS intervention, required a mean of 15 correspondences (email/text/phone/letter) in order to complete a baseline visit with a family; with a mean of n = 56 contacts with an intervention family (total, n = 726) and a mean of n = 37 contacts with the control group (total, n = 371) over the 6 month study duration. These were mainly sms text message and email, thus costs were contained and suitable for a low resourced setting.
Table 2 highlights the pragmatic features of 4HS that were considered to demonstrate high level of application of external validity assessed using a recognised RE-AIM self-assessment tool.
3.3. Assessment of the fidelity of the delivered 4HS intervention to the principles of MI (aim 3)
Fidelity and proficiency in MI during intervention visits was assessed as fair-to-good or good based on 4 competency parameters applied to five randomly selected interviews as shown, in Table 3.
Table 3.
Assessment of Fidelity to MI: summary scores for five randomly selected interviews.
| MITI -4 outcome measure for determining competence in MI | MITI -4 basic competence (fair) Threshold Score |
MITI -4 proficiency (good) Threshold Score |
Researcher range scores | Researcher Average Score |
|---|---|---|---|---|
| Global Clinician Rating –technical (cultivating + sustaining/2) | Average of 3 | Average of 4 | (3–4) | 3.2 (fair to good) |
| Global Clinician Rating – Relational (partnership + empathy/2) | Average of 3.5 | Average of 4 | (3–4) | 4.2 (good) |
| Reflection to Question Ratio (total reflection/total questions) | 1:1 | 2:1 | 2.75:1 (good) | |
| Percent Complex Reflections (CR/(SR + CR) | 40% | 50% | 48.5% (fair to good) | |
| Total MI-Adherent (SC + A + EA) | NA | NA | 10–19 | 15.4 |
| Total MI – non adherent (confront + persuade) | NA | NA | 0–3 | 1.4 |
Complex reflections (CR) typically add substantial meaning or emphasis to what client has said.
Simple Reflections (SR) convey understanding or facilitate client-clinician exchange.
Seeking Collaboration (SC) clinician explicitly attempts to share power or acknowledge expertise of client.
Affirmation (A) clinican utterance that accentuates something positive about the client.
Emphasising Autonomy (EA) utterances that clearly focus the responsibility with the client for decisions about change.
4. Discussion
In an earlier paper, 4HS theory of change and causal pathway were outlined in a logic model [16]. This model postulated that time invested in building relationships and involving local people in the research process would lead to suitable ‘buy-in’ and creation of appropriate study materials (related to aim 1 here). Consequently, the study would be promoted in a manner that; was identified as being acceptable (social media, leaflets and face-to-face); offered equitable recruitment (eligible for all suitably aged children, living in the target area) and encouraged participant families to engage (supermarket gift vouchers as incentives). If the intervention was delivered in a pragmatic way, with consideration to local contextual factors and family circumstance through a non–judgemental, supportive approach participants would be more likely to elicit positive behavioural change of EBRB’s in line with study outcomes (related to aim 2 here) and become invested in study aims. The present paper examines the extent to which 4HS study processes enabled or achieved these intentions.
A useful systematic review [11] highlighted that very few high quality studies looked at interventions to prevent obesity or improve obesity related behaviours in children from socioeconomically disadvantaged families and that, amongst other things, future studies should assess how implementable they are. It is also recognised that, adapting an existing intervention for cultural relevance, requires consideration and understanding of context which is crucially importance for replication and generalisability [22].
The 4HS study took place in an area of high deprivation, indeed two of the neighbourhoods sit within the most income deprived data zones in Scotland [21]. This is an important contextual factor. Often the people who live in these communities are considered ‘hard to reach’or alternatively, ‘easy to forget’ linked to the social challenges that often coincide with disadvantage and high incidence of poverty. Dundee, for example has the highest number of drug related deaths per resident in Europe [23]. North East Dundee was purposively selected as location for 4HS feasibility trial by a group of multi-agency staff from local authority, health and social care and third sector. Selection of this geographical area was based on level of deprivation and childhood obesity rates and because no similar project or intervention was being delivered locally.
Participatory methods facilitated local ‘buy in’ to study aims leading to co-production of suitable intervention materials, positive communication and promotion of study, including a co-designed website leaflet and poster. It also enabled the researcher, community-based workers, and local people from the North East to engage in a reciprocal relationship. Key attributes thought to enable this: a non-judgemental and empathetic approach, the ability to put child and family needs at the centre and ‘come alongside’ the individual and enhanced, active listening skills. The investment of time required to make connections within the community was key to establish links with the parent group that became a vital element of the study’s progression. Further insights and a deeper understanding of local contextual factors such as life circumstances (both barriers and facilitators) was also achieved. Feasibility parameters including the time taken at each stage of translation was recorded to inform future studies.
The time invested in arranging and organising face to face meetings, building relationships, understanding local context and raising awareness of the 4HS study was thought essential for a successful recruitment process, subsequent delivery of the 4HS intervention and at the later stage with the MI approach within households. Interestingly, this approach supports the findings of a recent study that explored factors related to participant engagement in HENRY, a pre-school, obesity prevention programme delivered in children’s centres in the UK. The authors concluded that factors at a three levels of local implementation require to be tackled; strategic level, manager buy-in and participant experience in order to achieve successful delivery [24].
Similar participatory and co-production approaches would be recommended in the initial stages of any future studies involving development, adaptation or translation of interventions to new settings and there is increasing recognition of the benefits in involving people in the research process more generally. Indeed, the research team involved in the ‘Better Start Bradford’ programme have produced a helpful toolkit, including an operational guide and evaluation framework, that was created based on their learning of integrating this research approach into everyday practice [25].
The inclusive recruitment methods, advertising and promotion of 4HS study were informed by conversations and discussions during the participatory phase and co-prodcution workshops and are a key strength of this study. Only two inclusion criteria, based on the age (2.0–5.5years) and household location (postcode within North East area) of the child were set, based on discussions with parents during the co-prodcution workshops, ensuring that there was equitable opportunity for families to participate, regardless, for example, of child disability or additonal support need. This minimised the risk of bias and ensured high application of external validity and reflected the needs of the local community. Use of social media and face-to-face attendance at community events were felt the best way to reach families during the recruitment phase. Printing and travel costs were kept to a minimum, with co-creation of a suitable study website, sharing posts on social media and positive local press stories. Local community events offered an opportunity to interact directly with families, hand out leaflets (targetted) and display posters as detailsed in Table 1.
Much effort and a flexible approach was required by the investigator (JG) in the lead up to implementation of 4HS intervention It was felt that inclusive recruitment was a key facilitator for positive impact with local people became crucial, in ‘championing’ and promoting the study within networks and beyond (mainly through social media). In a full scale trial and/or public health practice with more than one researcher, over a longer period of time it is predicted that ongoing momentum and ‘word of mouth’ would boost recruitment numbers. In a qualitative study where parental focus groups were used to understand what might trigger parents/carers to enter childhood weight management service, word of mouth and a positive experience by others came through as very important [26]. Indeed a number of enquiries were made regarding the 4HS intervention after the recruitment period ended and as such it was necessary to close down the study website.
There was consistency in how the intervention was implemented due to only one researcher being involved in delivery and detailed notes were kept by the researcher to summarise each home visit session. In general, the researcher was as flexible as possible in scheduling times to suit families including offering visits to take place in evenings and/or weekends, and notes were written during or immediately following each intervention visit. Table 2 highlighted the pragmatic features of 4HS by using the self rating scoring tool, useful in ‘real –world’ settings which considers who, what, where, how, when, and why questions which are easy to understand and use [18].
The amount of correspondence required to keep in regular contact with the families (e.g., to arrange/re-schedule home visits) was high (a mean of 15 sms text or email was required to achieve baseline home visit) and required the use of technology such as smart phones or an electronic device that enabled communication which best suited the target audience. The administrative tasks associated with home visits with busy parents within active households was, at times challenging due to a number of reasons (e.g., last minute change of work schedule, illness (parent or child) children at childcare/nursery, competing priorities for time including other children and/or appointments) and these further reinforce the importance of understanding contextual factors such as poverty and one parent families.
In practice, cancellation and re-scheduling of home visits could be interpreted as a sign of poor motivation in engaging with support and a flexible approach by staff may not be practical or cost effective to implement due to pressures within services or lack of suitable resource. In the family nurse partnership pilot [27] it is of note that there was a higher than expected attrition rate and nurses often found it difficult to re-schedule clients if they cancelled. However, interestingly, new guidance from NHS Health Scotland highlights the need for flexible and person centred appointments and services that meet the needs of the family [28].
The present findings suggest that the intervention was fairly faithful to MI. The researcher who delivered the intervention (JG) has extensive previous experience of applying an MI approach with families, but the fair-good scores and researcher experience suggest that there are challenges in utilising MI skills within dynamic and hectic family home settings (e.g., there are many more distractions than there would be in a clinical setting such as one or more children and adults present, household interruptions such as phone, devices, televisions). This is an important consideration in the skills, experience and training that would be required of researchers in any future definitive trial or for practitioners within routine public health or clinical practice. It is recommended that a minimum of 3 days of behaviour change/MI training course (delivered interactive and balance of theory and practice) would be a required, with additional peer support/supervision in assessing proficiency in delivery within a home environment. Importantly, a MI approach was well accepted by both families and practitioners in 4H Canada [15].
Qualitative and quantitative data related to the RE-AIM dimensions demonstrate that continuing this intervention after completion of this study within routine practice within the UK in a relatively low resourced setting is realistic. Indeed there are plans in place for rapid research impact for 4HS which is soon to be implemented within routine public health practice within an NHS services’ child healthy weight pathway in Tayside, Scotland, providing a rare, yet valuable opportunity for practice based evidence to be generated.
The 4HS study processes were evaluated and reported in order to determine practicability of translating the existing 4H intervention to a new setting and context. Key facilitators for positive impact of 4HS methodology for successful delivery of 4HS intervention were the inclusive recruitment methods, appropriate channels of communication and correspondence, positive links with local people and community workers integral to the research process and awareness and consideration of local contextual factors. The insights generated in this study could prove useful for determining the contribution of 4HS and 4HS intervention to the wider systems linked to childhood obesity. Connecting these insights with study outcomes is an important next step in order to understand the nature of that contribution to the wider complex and adaptive systems.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Thank you to the people living and working in the North East End of Dundee, particularly to Christine and Carolyn and the members of the Health Inequalities Positive Action Group in Whitfield. A huge thanks also goes to Hazel who attended many community events. This research was undertaken as part of a PhD studentship, funded by the Hannah Dairy Research Foundation (SC007058).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhip.2020.100026.
Contributor Information
Jenny Gillespie, Email: jenny.gillespie@strath.ac.uk.
Adrienne R. Hughes, Email: adrienne.hughes@strath.ac.uk.
Ann-Marie Gibson, Email: annmarie.gibson@strath.ac.uk.
Jess Haines, Email: jhaines@uoguelph.ca.
Elsie M. Taveras, Email: elsie.taveras@mgh.harvard.edu.
Laura Stewart, Email: drlaura@appletreeconsultancy.com.
John J. Reilly, Email: john.j.reilly@strath.ac.uk.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;16:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. 390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNICEF/WHO/World Bank Group . Key findings of the 2019 edition; 2019. Levels and Trends in Child Malnutrition: Joint Child Malnutrition Estimates.https://www.who.int/nutgrowthdb/jme-2019-key-findings.pdf?ua=1 accessed 16/02/20. [Google Scholar]
- 3.Information Services Division (ISD). Scotland Body Mass Index of Primary 1 Children in School Year 2017/8 2018 https://www.isdscotland.org/Health-Topics/Child-Health/Publications/2018-12-11/2018-12-11-P1-BMI-Statistics-Publication-Report.pdf (accessed 16/02/2020).
- 4.Flint S. Weight stigma and discrimination: time for change! Nutr. Bull. 2019;44:249–253. [Google Scholar]
- 5.Reilly J.J.R., Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int. J. Obes. 2011;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 6.Rankin J., Matthews L., Cobley S., Han A., Sanders S., et al. Psychological consequences of childhood obesity: psychiatric comorbidity and prevention. Adolesc. Health Med. Therapeut. 2016;7:125–146. doi: 10.2147/AHMT.S101631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bagnell A.M., Radley D., Jones R., Gately P., Nobles J., et al. Whole systems approaches to obesity and other public health challenges: a systematic review. BMC Publ. Health. 2019;19:8. doi: 10.1186/s12889-018-6274-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.foresighthttps://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/296290/obesity-map-full-hi-res.pdf).
- 9.Londons Child Obesity Taskforce . Ten Ambitions for London; 2019. Every Child A Healthy Weight.https://www.london.gov.uk/sites/default/files/every_child_a_healthy_weight.pdf © Greater London Authority. accessed 16/02/2020. [Google Scholar]
- 10.Public Health England . © Crown copyright; 2019. Whole Systems Approach to Obesity: A Guide to Support Local Approaches to Promoting a Healthy Weight.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/820783/Whole_systems_approach_to_obesity_guide.pdf accessed 16/02/2020. [Google Scholar]
- 11.Laws R., Campbell K.J., van der Pligt P., et al. The impact of interventions to prevent obesity or improve obesity related behaviours in children (0–5 years) from socioeconomically disadvantaged and/or indigenous families: a systematic review. BMC Publ. Health. 2014;14(779) doi: 10.1186/1471-2458-14-779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haines J., McDonald J., O’Brian A., Sherry B., Bottino C., Schmidt M., Taveras E. Healthy Habits Happy homes: randomised trial to improve household routines for obesity prevention amongst pre-school-aged children. J. Am. Med. Assoc. Pediatr. 2013;167(11) doi: 10.1001/jamapediatrics.2013.2356. [DOI] [PubMed] [Google Scholar]
- 13.Taveras E., McDonald J., O’Brien A., et al. Healthy Habits, Happy Homes: methods and baseline data of a randomized controlled trial to improve household routines for obesity prevention. Preventative Med. 2012;55(5):418–426. doi: 10.1016/j.ypmed.2012.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Haines J., Douglas S., Mirotta J.A., et al. Guelph Family Health Study: pilot study of a home-based obesity prevention intervention. Can. J. Public Health. 2018;109(4) doi: 10.17269/s41997-018-0072-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Kane C., Irwin J.D., Morrow D., Tang L., Wong S., et al. Motivational Interviewing with families in the home environment. Patient Educ. Counsel. 2019;102(1):2072–2080. doi: 10.1016/j.pec.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Gillespie J., Hughes A., Gibson A.M., Haines J., Taveras E., Reilly J.J. Protocol for Healthy Habits Happy Homes (4H) Scotland: feasibility of a participatory approach to adaptation and implementation of a study aimed at early prevention of obesity. BMJopen. 2019;9:6. doi: 10.1136/bmjopen-2018-028038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow R.E., Vogt T.M., Boles S.M. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am. J. Publ. Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glasgow R., Estabrooks P.E. Pragmatic applications of RE-AIM for health care initiatives in community and clinical settings. Prev. Chron. Dis. 2018;15 doi: 10.5888/pcd15.170271. Public Health research, practice and policy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moyers T.B., Rowell L.N., Manuel J.K., Ernst D., Houck J.M. The motivational interviewing treatment integrity code (MITI 4): rationale, preliminary reliability and validity. J. Subst. Abuse Treat. 2016;65:36–42. doi: 10.1016/j.jsat.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moyers T.B., Manuel J.K., Ernst D. 2015. Motivational Interviewing Treatment Integrity Coding Manual 4.2.1. Unpublished manual. [Google Scholar]
- 21.Partnership Dundee. 2012. Dundee North East Census Profile.https://www.dundeecity.gov.uk/sites/default/files/publications/LCPP_NorthEast_Profile_0.pdf accessed 16/02/20. [Google Scholar]
- 22.Moore G.F., Evans R.E., Hawkins J., Littlecott H., Mendez-Torres G.J., et al. From complex social intervention to interventions in complex social systems: future directions and unresolved questions for intervention development and evaluation. Evaluation. 2019;25(1):23–45. doi: 10.1177/1356389018803219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Records of Scotland . 2019. Drug-related Deaths in Scotland in 2018.https://www.nrscotland.gov.uk/files//statistics/drug-related-deaths/2018/drug-related-deaths-18-pub.pdf National statistics © Crown Copyright. accessed 16/02/20. [Google Scholar]
- 24.Burton W., Twiddy M., Sahota P., Brown J., Bryant J. Participant engagement with a UK community-based pre-school childhood obesity prevention programme: a focused ethnography study. Publ. Health. 2019;19:1074. doi: 10.1186/s12889-019-7410-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dickerson J., Bird P.K., Bryant M., Dharni N., Bridges S., et al. Integrating research and system-wide practice in public health: lessons learnt from Better Start Bradford. BMC Publ. Health. 2019;19:260. doi: 10.1186/s12889-019-6554-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gillespie J., Midmore C., Hoeflich J., Ness C., Ballard P., et al. Parents as the start of the solution: a social marketing approach to understanding triggers and barriers to entering a childhood weight management service. J. Hum. Nutr. Diet. 2015;28(s1):83–92. doi: 10.1111/jhn.12237. [DOI] [PubMed] [Google Scholar]
- 27.Barnes J, Ball M, Meadows P, McLeish J, Belskey J et al. Nurse-family partnerhsip programme: first year pilot sites implementation in England: pregnancy and post-partum period. Institute for the Study of Children, Families and Social Issues. Birkbeck, university of London. Research Report No DCSF-RW051.
- 28.NHS Health Scotland Standards for the delivery of tier 2 and tier 3 weight management services for children and young people in Scotland. 2019. http://www.healthscotland.scot/media/2658/standards-for-the-delivery-of-tier-2-and-tier-3-weight-management-services-for-children-and-young-people-in-scotland-english-oct2019.pdf © NHS Health Scotland. accessed 16/02/20.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.