Abstract
Objective
To examine the effects of online antenatal education on worries about labour, fear of childbirth, preparedness for labour and fear of COVID-19 during the COVID-19 pandemic.
Design
A single-blind randomised controlled trial comparing two groups: an antenatal education group and a control group.
Participants
The sample consisted of 44 pregnant women.
Measurements
A demographic data form, The Oxford Worries on Labour Scale, The Fear of Birth Scale, The Prenatal Self Evaluation Questionnaire and The Fear of COVID-19 Scale were used for data collection.
Findings
Online antenatal education decreased worries about labour, fear of childbirth and fear of COVID-19 and improved preparedness for labour.
Key conclusions
Online antenatal education offered during the COVID-19 pandemic is effective in preparedness for labour.
Implications for practice
As an alternative, online antenatal education should be offered to pregnant women unable to attend face to face education programs due to fear of transmission of infection.
Keywords: Pregnancy, COVID-19, Antenatal education, Fear of childbirth, Worry, Preparedness for labour
Introduction
It is stated in the literature that the effect of COVID-19 on women's labour experiences is important (Mayopoulos et al., 2021). It is also reported that during the COVID-19 pandemic, women have had a higher level of fear of childbirth (Ravaldi et al., 2021) and a higher rate of traumatic labour (Mayopoulos et al., 2021). Traumatic labour experiences increase rates of postpartum depression, posttraumatic stress disorder and caesarean section, decrease rates of breastfeeding and lead to negligence of babies, and fear and worries about breastfeeding in the future (Fenaroli, 2019; Hosseini et al., 2018; Ternström et al., 2015; Modarres et al., 2012; Goodman et al., 2004). Besides, it has been noted in the literature that depression symptoms increased in the third trimester during the pandemic (H. Wu et al., 2020). Depression symptoms were shown to occur in 29.6% of the women in a study in China and 35.4% of the women in a study in Turkey (Durankuş and Aksu, 2022; H. Wu et al., 2020). In addition, the prevalence of anxiety (34%) and depression (30%) was reported to increase in the women becoming pregnant and giving birth during the pandemic (Sun et al., 2020). Therefore, pregnant women should be provided with stronger support during the pandemic (Ravaldi et al., 2021; Brooks et al., 2020).
Lack of knowledge and fear of the unknown during pregnancy and labour cause women to feel worried (Pınar, et al., 2018). Pregnant women were observed to be more worried about their own health (Corbett et al., 2020) and the labour process during the COVID-19 pandemic (Ravaldi et al., 2021; Brooks et al., 2020). It was stated in the literature that women had more positive feelings about labour before the pandemic but more negative feelings about labour during the pandemic (Ravaldi et al., 2021). It is important to eliminate fears and worries of pregnant women so that they can have positive labour experiences (Fenaroli et al., 2019; Ghanbari-Homayi et al., 2019). It is known that antenatal education is effective in removing worries and fears of women about labour (İsbir et al., 2016; Serçekuş and Başkale, 2016) and increases positive labour experiences (Hassanzadeh et al., 2020). Antenatal education is important in that it improves women's awareness of their needs and helps them to understand the labour process better (Pınar, et al., 2018).
It is stated in the literature that although pregnant women need antenatal education, they are likely to face the risk of a potential cross infection when they go to health centres to receive healthcare during pandemics (Ho, 2003). They were afraid of antenatal visits and even cancelled their appointments due to the fear of COVID-19 transmission during the COVID-19 pandemic (Y. Wu et al., 2020). However, they need more care and counselling during the antenatal period (Ravaldi et al., 2021; Brooks et al., 2020). Therefore, it is important and preferable to offer online antenatal education (Du et al., 2020). Although there is sufficient evidence about effectiveness of face to face antenatal education in preparedness for labour and elimination of birth-related fears (Mete et al., 2017; İsbir et al., 2016; Serçekuş and Başkale, 2016; Serçekuş and Mete, 2010a), there have been few studies about the effects of online antenatal education (Pasadino et al., 2020). The effects of online education offered during the pandemic are not clear yet. Therefore, the aim of the present study was to examine the effects of online antenatal education given during the COVID-19 pandemic on pregnant women's worries about labour, fear of childbirth, preparedness for labour and fear of COVID-19.
Methods
Study design
This was a single blind, randomised controlled trial with a pre-post-test. The study was conducted in accordance with CONSORT guidelines (2010) (Shulz et al., 2010). The identification code of this clinical trial is NCT05115071.
Participants
The study was performed with pregnant women presenting to an obstetrics and gynaecology outpatient clinic of a university hospital in the western part of Turkey. The inclusion criteria were the age of 18 years or more, gestation of 24–34 weeks, graduation at least from primary school, nulliparity, not being at high risk in pregnancy, ability to use the application of Microsoft Teams, not having a psychiatric disease and not having attended any other antenatal programmes in the antenatal period.
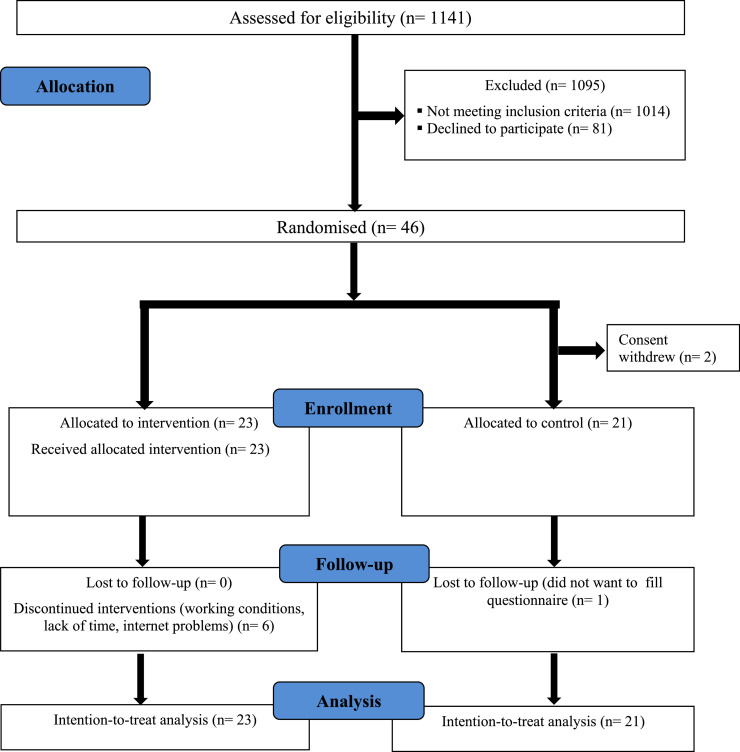
Between October 2021 and December 2021, 1141 pregnant women were evaluated in terms of the inclusion criteria. Out of 1141 pregnant women, 1014 did not fulfil the inclusion criteria (not being nulliparous and not having 24–34 weeks gestation) and 81 declined to participate in the study. A total of 1095 women were excluded from the study. Out of the remaining 46 pregnant women who accepted to take part in the study and satisfied the inclusion criteria, 23 were randomly assigned into the intervention group and 23 into the control group. Two pregnant women assigned into the control group wanted to drop out of the study before initiation of the study and the study was continued with 21 women in the control group and 23 in the intervention group. Seventeen women in the intervention group attended all sessions of the eight-hour online education, but eight pregnant women could not attend the education program regularly due to inappropriate working conditions, inadequate time and problems with access to the Internet. Six women in the intervention group and one pregnant woman in the control group did not fill in the post-test. The study was completed with 23 women in the intervention group and 21 in the control group by using intention-to-treat analysis (Fig. 1 ). There were no significant differences likely to affect attending the education program except for working and technical conditions between the pregnant women completing the program and those not completing the program.
Fig. 1.
CONSORT flow diagram of the study.
Sample size calculation
The sample size was calculated with the statistics program of G*Power based on the results of a study using antenatal education (Serçekuş and Başkale 2016). It was found to be 32, of whom 16 were assigned into the intervention group and 16 were assigned into the control group, based on α =0.05, effect size (d)= 1.05 and study power of 80%. Taking account of possible losses, the sample size was planned to be higher. To prevent losses and bias, intention-to-treat analysis was performed.
Randomization and blinding
Following an initial evaluation, the pregnant women meeting the inclusion criteria were randomly assigned into the intervention and control groups. Block randomization was utilised to ensure that each group had an equal number of participants. In block randomization, participants who will be assigned into experimental and control groups are divided into blocks and the blocks are selected by using simple random sampling (Kanık et al., 2011). In the present study, 23 blocks were randomly selected, and each block included two women (AB=1, BA=2). Random selection of the blocks was performed by using numbers from a website producing randomization numbers (randomizer.org). The women had an equal chance of being in the experimental and control groups. They were blinded to their groups. However, it was not possible to blind the researchers to the intervention and control groups due to the nature of the randomization.
Intervention
The intervention group was provided with online antenatal childbirth preparation education through Microsoft Teams. The education was offered to groups of 7–8 participants and lasted 4 h weekly for 2 weeks. A total of 8 sessions were conducted. Two sessions were held on Monday and two sessions were held on Thursday each week. Each session lasted 50 min and 10-minutes breaks were given between the sessions. The education was offered by two lecturers having a trainer certificate for and experienced in labour preparation (XX, YY). Content of the education was created in accordance with the guides updated for the pandemic. It included childbirth (discussion of feelings about childbirth, discussion of strategies to deal with fear of childbirth, mechanisms of labour, discussion of enhancement of women's self-confidence about childbirth), improvement of skills to cope with stress and pain in labour (breathing and relaxation exercises) and COVID-19 (the effects of the COVID-19 pandemic on the individual, prevention and treatment of COVID-19 and vaccines). During the education sessions, the trainers’ and participants’ cameras were turned on and the pregnant women could ask questions whenever they wanted and got actively involved. The women were encouraged to interact with each other more during break times. They performed breathing exercises together and relaxation exercises at the end of each session.
Unlike the women in the intervention group, the women in the control group received routine prenatal care and were not offered any interventions during the study. The routine prenatal care offered to the control group included taking history, performing physical and ultrasound examinations and giving education. It lasted about 15–20 min. During the routine prenatal care, sufficient time cannot be allocated for antenatal education. At the end of the study, the women in the control group were provided with the same online antenatal education as the intervention group.
Instruments
Data were collected via a demographic data form, The Oxford Worries on Labour Scale (OWLS), The Fear of Birth Scale (FOBS), Preparation for Labour Subscale and Wellbeing of Self and Baby Subscale of The Prenatal Self Evaluation Questionnaire and The Fear of COVID-19 Scale (FCV-19S).
Demographic Data Form: This form consists of five questions about age, gestational week, education, employment and income.
The Oxford Worries on Labour Scale: The OWLS was developed by Redshaw et al. in 2009 to assess women's worries on labour. The scale can be utilised before, during and after labour. It is a ten-item, four-point Likert scale and one corresponds to very worried, two fairly worried, three not very worried and four never worried. None of the items are inversely scored. As scores on the scale increase, worries on labour decrease. The validity and reliability of the OWLS for the Turkish population were tested by Erkal Aksoy and Özentürk (2016). The scale has three subscales: pain and distress, pre-labour uncertainty and interventions. Cronbach's alpha for the scale was reported to be 0.83 (Erkal Aksoy and Özentürk, 2016). It was found to be 0.84 in the present study.
The Fear of Birth Scale: The FOBS was created by Haines et al. in 2011 to measure the fear of birth. Respondents are asked to rate their feelings in response to the question “How do you feel about the approaching birth now?” on a 100mm-line with one end corresponding to calm and the other end corresponding to worried and on another 100mm-line with one end corresponding to lack of fear and the other end corresponding to severe fear. The cut-off point for the scale was 50 and women and their partners receiving more than 50 are considered to experience fear of birth. The scale can be administered to both pregnant women and their partners. Psychometric analyses of the FOBS in the Turkish population were performed by Serçekuş et al. (2020). In a study by Serçekuş et al. on the validity and reliability of the scale in the Turkish language, its Cronbach's alpha was found to be 0.93 (Serçekuş et al., 2020). Cronbach's alpha for the scale in the present study was found to be 0.92.
The Prenatal Self Evaluation Questionnaire: The Prenatal Self Evaluation Questionnaire was developed by Lederman in 1979 to evaluate adaptation of the women to pregnancy and motherhood in the prenatal period. It is composed of 79 items. The validity and reliability of the questionnaire in the Turkish language were tested by Beydağ and Mete (2008). Low scores show high adaptation to pregnancy. The questionnaire has seven subscales and two of them were used in the present study: Preparation for Labour Subscale and Wellbeing of Self and Baby Subscale
Preparation for Labour Subscale: Items 7, 13, 24, 25, 26, 38, 47, 48, 56 and 72 in the Prenatal Self Evaluation Questionnaire belong to Preparation for Labour Subscale. These items are about the preparedness of women for labour. Preparation for Labour Subscale is a four-point Likert scale and four corresponds to describing well, three partly describing, two somewhat describing and one never describing. Some of the items are scored in the reverse order. Cronbach's alpha for the scale was reported to be 0.72 by Beydağ and Mete (2008) and was found to be 0.67 in the present study.
Wellbeing of Self and Baby Subscale: Items 12, 16, 17, 30, 41, 51, 57, 63, 68 and 71 in the Prenatal Self Evaluation Questionnaire belong to Wellbeing of Self and Baby Subscale. These items are related to worries of women about their health and their babies’ health. Similar to Preparation for Labour Subscale, some items of Wellbeing of Self and Baby Subscale are scored in the reverse order. Cronbach's alpha for the subscale was reported to be 0.85 by Beydağ and Mete (2008) and was found to be 0.83 in the present study.
The Fear of COVID-19 Scale: The FCV-19S was developed by Ahorsu et al. in 2020. The scale has a single-factor structure and seven items. It is a five-point Likert scale and one corresponds to completely disagree and five corresponds to completely agree. None of the items are scored in the reverse order. High scores show a high level of fear about COVID-19. The validity and reliability of the scale in the Turkish population were tested by Ladikli et al. (2020) and Cronbach's alpha was reported to be 0.86. Cronbach's alpha for the scale was found to be 0.81 in the current study.
Data collection
Data were collected through online forms between October and December in 2021. The demographic data form, the OWLS, the FOBS, Preparation for Labour and Wellbeing of Self and Baby subscales of the Prenatal Self Evaluation Questionnaire and the FCV-19S were administered as pre-tests before the education. The intervention group received eight-hour online antenatal education. At the end of this education, the patients were given the OWLS, the FOBS, Preparation for Labour and Wellbeing of Self and Baby subscales and the FCV-19S as post-tests. Administration of the post-tests was completed in 24 h after completion of the education. The control group filled in the same data collection tools at the same time as the intervention group.
Data analysis
Data were analysed by using the Statistical Package Program for Social Sciences 22.0. Skewness and Kurtosis were utilised to test normality of the data. Since they showed values ranging from +1.5 to −1.5, the data were considered to have a normal distribution (Tabachnick and Fidell, 2013). Data about demographic features of the women were analysed with numbers, percentages and mean values. Differences in demographic features between the groups were examined by using independent samples t-test and Chi-square test. Pre-test and post-test scores of the groups were examined by adopting independent groups t-test. Prevention of bias and management of missing data in all the analyses were based on the intention-to-treat analysis. The most common method of filling in missing data was using the measures of the last observation (EMA 2011; Partlak Günüşen and Üstün 2009). In this study, the missing data were also compensated using the last‐observation‐carried forward method.
Ethical considerations
Ethical approval for the study was obtained from the ethical committee of non-interventional research of a university (approval date: 19 January 2021; approval number: E-60,116,787–020–10,516). The pregnant women were given information about the study. They were assured that participation in the study had a voluntary basis and that obtained data would not be shared with anyone and any institutions. Oral and written informed consent was obtained from all the participants.
Results
Sociodemographic features of the pregnant women are presented in Table 1 . There was no significant difference in sociodemographic features between the intervention and control groups (Table 1).
Table 1.
Demographic characteristics of the participants in the intervention and control groups.
| Variable | Intervention group (n = 23) | Control group (n = 21) | Statistics | p |
|---|---|---|---|---|
| Agea | 26.69±4.93 | 25.66±4.58 | t = 0.714 | 0.479 |
| Gestational weeka | 29.13±4.90 | 27.38±3.16 | t = 1391 | 0.172 |
| Educationb | ||||
| Primary or high school | 10 (43.5) | 11 (52.4) | x2=0.349 | 0.555 |
| University | 13 (56.5) | 10 (47.6) | ||
| Employmentb | ||||
| Employed | 14 (60.9) | 9 (42.9) | x2=1.428 | 0. 232 |
| Unemployed | 9 (39.1) | 12 (57.1) | ||
| Incomeb | ||||
| Moderate | 18 (78.3) | 15 (71.4) | x2=0.273 | 0.601 |
| High | 5 (21.7) | 6 (28.6) |
Mean ± standard deviation.
Frequencies.
There was no significant difference in the mean scores on the OWLS, the FOBS, the FCV-19S and Preparation for Labour and Well-being of Self and Baby subscales between the intervention and control groups before the intervention group received the online antenatal education (Table 2 ). After the intervention group received the online antenatal education, a significant difference was found in the scores on the OWLS, the FOBS, the FCV-19S and Preparation for Labour and Well-being of Self and Baby subscales between the intervention and control groups. The pregnant women in the intervention group were significantly less worried about labour (p<0.05), significantly less afraid of birth (p<0.05) and significantly less afraid of COVID-19 (p<0.05), significantly more prepared for labour (p<0.01) and had significantly more positive feelings about their wellbeing and their babies’ wellbeing (p<0.05) (Table 2).
Table 2.
Scores on The Oxford Worries on Labour Scale, The Fear of Birth Scale, Preparation for Labour Subscale, Wellbeing of Self and Baby Subscale, The Fear of COVID-19 Scale before and after education.
| Scales | Pre-test Intervention group (n = 23) Mean (SD) | Control group (n = 21)Mean (SD) | P | Post-test Intervention group (n = 23) Mean (SD) | Control group (n = 21)Mean (SD) | p |
|---|---|---|---|---|---|---|
| OWLSa | 23.21±5.60 | 21.23±6.12 | 0.269 | 27.26±7.37 | 21.23±5.91 | 0.005 |
| FOBSa | 5.41±2.57 | 6.28±2.15 | 0.232 | 4.45±2.58 | 6.50±2.41 | 0.010 |
| Preparation for laboura | 22.04±4.73 | 24.47±4.87 | 0.101 | 16.86±4.55 | 23.95±5.44 | <0.000 |
| Wellbeing of self and babya | 22.39±6.54 | 23.76±6.68 | 0.496 | 17.73±6.79 | 23.09±6.70 | 0.012 |
| FCV-19Sa | 18.34±3.41 | 21.23±6.42 | 0.076 | 16.34±4.74 | 20.00±4.12 | 0.010 |
Mean (Standard Deviation)
OWLS: The Oxford Worries on Labour Scale, FOBS: The Fear of Birth Scale, FCV-19S: The Fear of COVID-19 Scale.
Discussion
In the present study, the women receiving online antenatal education had significantly lower scores on the OWLS and FOBS. Therefore, online antenatal education can be considered as effective in reducing worries about labour and fear of birth. Several studies have shown that pregnant women's fear of birth (İsbir et al., 2016; Serçekuş and Başkale, 2016; Toohill et al., 2014), worries about labour (Uslu Yuvacı et al., 2021) and worries about their health and their babies’ health decreased after face to face antenatal education (Serçekuş and Mete, 2010a). A qualitative study by Miquelutti et al. also revealed that antenatal education was effective in reducing anxiety experienced by women during their labour (Miquelutti et al., 2013). Considering that pregnant women's fear of birth (Ravaldi et al., 2021) and worries about their health and their babies’ health increase during pandemics (Corbett et al., 2020; Ravaldi et al., 2021; Mırzak Şahin and Kabakçı, 2021), the finding that online education reduced this fear and worries is of great importance. It has been previously shown that provision of antenatal education in groups is more preferable since it allows pregnant women to share their experiences and receive support from each other (Serçekuş and Mete, 2010a, 2010b). In the present study, the women were offered antenatal education in groups and their cameras were turned on throughout the education sessions. This might have increased interactions between the women.
It has been stated in the literature that pregnant women experience intense fear of COVID-19 (Eroğlu et al., 2021; Durmuş et al., 2021). This great fear of COVID-19 may increase fear and worries felt during pregnancy (Salehi et al., 2020). In the current study, online antenatal education was found to be effective in reduction of the fear of COVID-19. This effect might have been due to transmitting information about COVID-19, allowing the women to express their opinions and feelings about the pandemic, supplying answers to all their questions about the issue and interactions between them throughout the education sessions.
Antenatal education plays an important role in physical and psychological preparations of pregnant women for birth (Pınar et al., 2018; Afshar et al., 2017). It strengthens their ability to make information-based decisions (Fraser and Cooper, 2009) and enables them to have realistic expectations about birth (Miquelutti et al., 2013; Ip et al., 2009; Goodman et al., 2004). This may increase self-control of pregnant women during labour (Miquelutti et al., 2013; Ip et al., 2009; Goodman et al., 2004). Increased self-control and self-efficacy during labour improve coping strategies and have a positive effect on labour (Dahlberg and Aune, 2013). It is very likely that pregnant women having a chance to practise relaxation techniques and breathing exercises during antenatal education have self-confidence and a positive attitude towards labour (Ho and Holroyd, 2002; Miquelutti et al., 2013). Several prior studies have shown that face to face antenatal education increases preparedness for labour (Mete et al., 2017; Serçekuş and Mete, 2010a) and maternal self-efficacy (Serçekuş and Başkale, 2016). In present study, the women receiving online education had significantly lower scores on the Preparation for Labour Subscale. This suggests that online antenatal education improved preparedness for labour in the pregnant women. Provision of information about the process of labour and strategies to cope with labour pain and performing relaxation and breathing exercises in groups in each education session might have enhanced preparedness for labour in the women.
Conclusion
The online antenatal education offered in this randomised, controlled study during the pandemic was shown to be effective in reduction of fear and worries about labour and in improvement of preparedness for labour in the pregnant women. The online antenatal education also decreased the fear of COVID-19. When the increased likelihood for experiencing fear of birth and a traumatic birth during the pandemic is taken into account, it becomes important to continue delivering antenatal education. However, the pandemic has caused the fear of exposure to cross infections and created difficulty in receiving face to face antenatal education. Online antenatal education can be a better alternative to face to face antenatal education throughout critical periods like pandemics since it is easily accessible and poses fewer health risks. However, further studies can elucidate the effects of online antenatal education better.
Limitations and strengths
One important strength of this study is its randomised, controlled design. Besides, the study was performed with primiparous women to understand the effect of the online antenatal education clearly. However, inclusion of only the women who could access and use technology (Internet and computer etc.) can be considered as a limitation of the study.
Ethical approval
Ethical approval was obtained from Covid-19 Research Evaluation Committee of the Turkish Ministry of Health and the medical ethics committee of a university in the western part of Turkey (E-60,116,787–020–113,991).
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit author statement
Elif Uludağ: Conceptualization, Methodology, Formal analysis, Writing-Review & Editing. Pınar Serçekuş: Methodology, Formal analysis, Writing-Review & Editing. Okan Vardar: Investigation, Writing- Original Draft, Visualization. Sevgi Özkan: Writing-Review & Editing, Süleyman Erkan Alataş: Writing-Review & Editing.
Conflict of Interest
None.
Acknowledgement
The authors would like to thank all of the women who accept to participate in the study.
References
- Afshar Y, Wang ET, Mei J, Esakoff TF, Pisarska MD, Gregory KD. Childbirth education class and birth plans are associated with a vaginal delivery. Birth. 2017;44(1):29–34. doi: 10.1111/birt.12263. [DOI] [PubMed] [Google Scholar]
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydağ KT, Mete S. Validity and Reliability Study of the Prenatal Self Evaluation Questionnaire. J. Anatolia Nurs. Health Sci. 2008;11(1):16–24. [Google Scholar]
- Brooks SK, Weston D, Greenberg N. Psychological impact of infectious disease outbreaks on pregnant women: rapid evidence review. Public Health. 2020;189:26–36. doi: 10.1101/2020.04.16.20068031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbett GA, Milne SJ, Hehir MP, Lindow SW, O'connell MP. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;249:96. doi: 10.1016/j.ejogrb.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlberg U, Aune I. The woman's birth experience—The effect of interpersonal relationships and continuity of care. Midwifery. 2013;29(4):407–415. doi: 10.1016/j.midw.2012.09.006. [DOI] [PubMed] [Google Scholar]
- Du L, Gu YB, Cui MQ, Li WX, Wang J, Zhu LP, Xu B. Investigation on demands for antenatal care services among 2 002 pregnant women during the epidemic of COVID-19 in Shanghai. Zhonghua Fu Chan Ke Za Zhi. 2020;55(3):160–165. doi: 10.3760/cma.j.cn112141-20200218-00112. Doi: [DOI] [PubMed] [Google Scholar]
- Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J. Matern. Fetal Neonatal Med. 2022;35(2):205–211. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- Erkal Aksoy Y, Özentürk MG. Turkish validity and reliability of the oxford worries about labour scale. Turkiye Klinikleri J. Health Sci. 2016;1(3):170–183. [Google Scholar]
- European Medicines Agency (EMA). 2011. Guideline on missing data in confirmatory clinical trials. 1–12. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-missing-data-confirmatory-clinical-trials_en.pdf.
- Fenaroli V, Molgora S, Dodaro S, Svelato A, Gesi L, Molidoro G.…Ragusa A. The childbirth experience: obstetric and psychological predictors in Italian primiparous women. BMC Pregnancy Childbirth. 2019;19(1):1–7. doi: 10.1186/s12884-019-2561-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraser D, Cooper M. 15th ed. Churchill Livingstone; Edinburgh: 2009. Myles’ Textbook for Midwives. [Google Scholar]
- Ghanbari-Homayi S, Fardiazar Z, Meedya S, Mohammad-Alizadeh-Charandabi S, Asghari-Jafarabadi M, Mohammadi E, Mirghafourvand M. Predictors of traumatic birth experience among a group of Iranian primipara women: a cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):1–9. doi: 10.1186/s12884-019-2333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J. Adv. Nurs. 2004;46(2):212–219. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- Haines H, Pallant JF, Karlström A, Hildingsson I. Cross-cultural comparison of levels of childbirth-related fear in an Australian and Swedish sample. Midwifery. 2011;27(4):560–567. doi: 10.1016/j.midw.2010.05.004. [DOI] [PubMed] [Google Scholar]
- Hassanzadeh R, Abbas-Alizadeh F, Meedya S, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M. Fear of childbirth, anxiety and depression in three groups of primiparous pregnant women not attending, irregularly attending and regularly attending childbirth preparation classes. BMC Womens Health. 2020;20(180):1–8. doi: 10.1186/s12905-020-01048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho I, Holroyd E. Chinese women's perceptions of the effectiveness of antenatal education in the preparation for motherhood. J. Adv. Nurs. 2002;38(1):74–85. doi: 10.1046/j.1365-2648.2002.02148.x. [DOI] [PubMed] [Google Scholar]
- Hosseini VM, Nazarzadeh M, Jahanfar S. Interventions for reducing fear of childbirth: a systematic review and meta-analysis of clinical trials. Women Birth. 2018;31(4):254–262. doi: 10.1016/j.wombi.2017.10.007. [DOI] [PubMed] [Google Scholar]
- Ip WY, Tang CS, Goggins WB. An educational intervention to improve women's ability to cope with childbirth. J. Clin. Nurs. 2009;18(15):2125–2135. doi: 10.1111/j.1365-2702.2008.02720.x. [DOI] [PubMed] [Google Scholar]
- İsbir GG, Inci F, Önal H, Yıldız PD. The effects of antenatal education on fear of childbirth, maternal self-efficacy and post-traumatic stress disorder (PTSD) symptoms following childbirth: an experimental study. Appl. Nurs. Res. 2016;32:227–232. doi: 10.1016/j.apnr.2016.07.013. [DOI] [PubMed] [Google Scholar]
- Kanik EA, Taşdelen B, Erdoğan S. Randomization in clinical trials. Marmara Med. J. 2011;24(3):149–155. [Google Scholar]
- Ladikli N, Bahadır E, Yumuşak FN, Akkuzu H, Karaman G, Türkkan Z. The reliability and validity of Turkish version of coronavirus anxiety scale. Int. J. Soc. Sci. 2020;3(2):71–80. [Google Scholar]
- Lederman RP, Lederman E, Work BA, McCann DS. Relationship of psychological factors in pregnancy to progress in labor. Nurs. Res. 1979;28(2):94–97. doi: 10.1097/00006199-197903000-00012. [DOI] [PubMed] [Google Scholar]
- Mayopoulos GA, Ein-Dor T, Dishy GA, Nandru R, Chan SJ, Hanley LE.…Dekel S. COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J. Affect. Disord. 2021;282:122–125. doi: 10.1016/j.jad.2020.12.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mete S, Çiçek Ö, Aluş Tokat M, Çamlıbel U, Uludağ E. Doğuma Hazırlık Sınıflarının Doğum Korkusu, Doğum Tercihi ve Doğuma Hazır Oluşluğa Etkisi. Turkiye Klinikleri Hemsirelik Bilimleri. 2017;9(3):201–206. doi: 10.5336/nurses.2016-53977. Doi: [DOI] [Google Scholar]
- Miquelutti MA, Cecatti JG, Makuch MY. Antenatal education and the birthing experience of Brazilian women: a qualitative study. BMC Pregnancy Childbirth. 2013;13(1):1–8. doi: 10.1186/1471-2393-13-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modarres M, Afrasiabi S, Rahnama P, Montazeri A. Prevalence and risk factors of childbirth-related post-traumatic stress symptoms. BMC Pregnancy Childbirth. 2012;12(1):1–6. doi: 10.1186/1471-2393-12-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partlak Günüşen N, Üstün B. Intention to treat analysis: a statistical analysis necessary when sample loss occur in randomized-controlled trial. E-Journal of Dokuz Eylul University Nursing Faculty. 2009;1(1):46–56. [Google Scholar]
- Pasadino F, DeMarco K, Lampert E. Connecting with families through virtual perinatal education during the covid-19 pandemic. MCN Am. J. Matern. Child Nurs. 2020;45(6):364–370. doi: 10.1097/NMC.0000000000000665. Doi: [DOI] [PubMed] [Google Scholar]
- Pinar G, Avsar F, Aslantekin F. Evaluation of the impact of childbirth education classes in Turkey on adaptation to pregnancy process, concerns about birth, rate of vaginal birth, and adaptation to maternity: a case-control study. Nurs. Res. 2018;27(3):315–342. doi: 10.1177/105477381668233. [DOI] [PubMed] [Google Scholar]
- Ravaldi C, Wilson A, Ricca V, Homer C, Vannacci A. Pregnant women voice their concerns and birth expectations during the COVID-19 pandemic in Italy. Women Birth. 2021;34(4):335–343. doi: 10.1016/j.wombi.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redshaw M, Martin C, Rowe R, Hockley C. The Oxford worries about labour scale: women's experience and measurement characteristics of a measure of maternal concern about labour and birth. Psychol. Health Med. 2009;14(3):354–366. doi: 10.1080/13548500802707159. [DOI] [PubMed] [Google Scholar]
- Salehi L, Rahimzadeh M, Molaei E, Zaheri H, Esmaelzadeh-Saeieh S. The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: a structural equation model. Brain Behav. 2020;10(11):e01835. doi: 10.1002/brb3.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serçekuş P, Başkale H. Effects of antenatal education on fear of childbirth, maternal self-efficacy and parental attachment. Midwifery. 2016;34:166–172. doi: 10.1016/j.midw.2015.11.016. [DOI] [PubMed] [Google Scholar]
- Serçekuş P, Mete S. Effects of antenatal education on maternal prenatal and postpartum adaptation. J. Adv. Nurs. 2010;66(5):999–1010. doi: 10.1111/j.1365-2648.2009.05253.x. [DOI] [PubMed] [Google Scholar]
- Serçekuş P, Mete S. Turkish women's perceptions of antenatal education. Int. Nurs. Rev. 2010;57(3):395–401. doi: 10.1111/j.1466-7657.2009.00799.x. [DOI] [PubMed] [Google Scholar]
- Serçekuş P, Vardar O, Özkan S. Fear of childbirth among pregnant women and their partners in Turkey. Sexual Reproductive Healthcare. 2020;24 doi: 10.1016/j.srhc.2020.100501. [DOI] [PubMed] [Google Scholar]
- Sun F, Zhu J, Tao H, Ma Y, Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J. Psychosom. Obstet. Gynaecol. 2020;42(2):91–99. doi: 10.1080/0167482X.2020.1857360. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. 6th ed. Pearson; Boston: 2013. Using Multivariate Statistics. [Google Scholar]
- Ternström E, Hildingsson I, Haines H, Rubertsson C. Higher prevalence of childbirth related fear in foreign born pregnant women–findings from a community sample in Sweden. Midwifery. 2015;31(4):445–450. doi: 10.1016/j.midw.2014.11.011. [DOI] [PubMed] [Google Scholar]
- Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, Ryding EL. A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women. Birth. 2014;41(4):384–394. doi: 10.1111/birt.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uslu Yuvaci H, Cinar N, Yalnizoglu Caka S, Topal S, Peksen S, Saglam N, Cevrioglu AS. Effects of antepartum education on worries about labor and mode of delivery. J. Psychosomatic Obstetrics Gynecol. 2021;42(3):228–234. doi: 10.1080/0167482X.2020.1725465. [DOI] [PubMed] [Google Scholar]
- Wu H, Sun W, Huang X, Yu S, Wang H, Bi X.…Ming WK. Online antenatal care during the COVID-19 pandemic: opportunities and challenges. J. Med. Internet Res. 2020;22(7):e19916. doi: 10.2196/19916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J.…Huang HF. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am. J. Obstet. Gynecol. 2020;223(2):240. doi: 10.1016/j.ajog.2020.05.009. -e1. [DOI] [PMC free article] [PubMed] [Google Scholar]