Abstract
Nascent and rapidly growing research into defining the concept of “food addiction” (FA) in relation to obesity is currently underway. Food addiction is present in a subset of patients who are overweight or have obesity, and its presence is associated with other psychosocial disorders such as depression, anxiety, eating disorders, impulse control disorders, and lower quality of life. Food addiction is associated with higher intake of and preference for highly processed foods that have addictive-like properties such as cravings, reward sensitivity, and impaired control. Food addiction is associated with less weight loss in patients with obesity utilizing diet and lifestyle-related interventions. In clinical practice, identifying the subset of patients with obesity with FA-related psychosocial constraints and continued emphasis on avoiding highly processed foods may improve obesity and weight management outcomes.
Food addiction is thought to be an addictive-like phenotype.
Food addiction is noted to have significant overlap with substance use disorder (SUD) and other eating disorders, but is currently not classified a diagnosis by DSM-IV and DSM-V criteria.
Food addiction has similarities to SUD, such as cravings, reduced control over intake, increased impulsivity and altered reward-sensitivity.
The Yale Food Addiction Scale, which is a clinical scale modeled by the DSM-IV and DSM-V criteria for SUD, has been used to quantify and study FA.
Introduction
In the United States (U.S.), about 39% of the population is considered overweight or obese, and that number is expected to trend higher.1 Obesity, now considered a chronic disease, is clinically challenging to manage as it involves lifelong lifestyle changes. Development of obesity is multifactorial and involves environmental influences, genetic influences, and complex brain and gastrointestinal signaling that mediate hunger, satiety, and reward pathways.2–7 Nascent and rapidly-growing research into FA and its role in obesity is currently underway. The purpose of this clinical review is to focus on the clinically applicable outcomes of FA related research in respect to clinical obesity management.
Defining Food Addiction
Food addiction has similarities to substance use disorder (SUD) that help us understand and research the concept, although it is not recognized as a SUD, eating disorder, or as a behavioral disorder in the DSM-IV and DSM-V.2 Similarities between FA and SUD include cravings, reduced control over intake, increased impulsivity and altered reward-sensitivity.6 To quantify and study FA, researchers developed the Yale Food Addiction Scale (YFAS), which is a clinical scale modeled by the DSM-IV and DSM-V criteria for SUD.7,8 Similar to DSM-IV and DSM-V criteria for SUD and behavioral disorders, the “diagnosis” of FA is not retained if clinical impairment or distress is not present, even if other symptoms are present.8
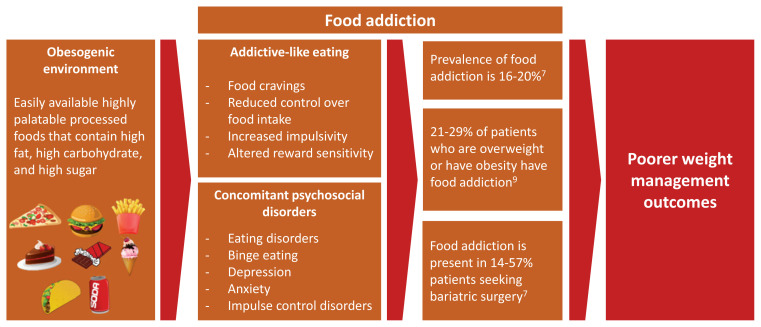
The prevalence of FA has been reported by Penzenstadler et al. and varies between 16.2% and 19.9%.7 Food addiction was higher in overweight patients, patients seeking weight loss, and in patients with an eating disorder (ED) such as binge eating and bulimia nervosa, depression, and anxiety.7 In patients seeking bariatric surgery, the prevalence of FA ranged from 14% to 57.8%, and was not to associated with pre-surgical weight or postsurgical weight outcomes.7
Metabolic and Psychosocial Characteristics of Patients with Obesity and Food Addiction
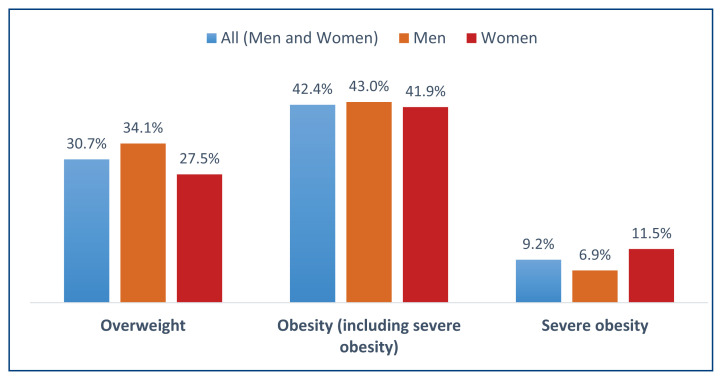
Food addiction itself may not lead to obesity or metabolic syndrome related risk factors. Kiyici et al. found that there was no statistically significant difference between patients with and without FA in terms of metabolic syndrome-related measures such as body mass index (BMI), fat percentage, waist circumference, serum insulin, insulin resistance, hemoglobin A1c, lipid parameters, and vascular adiposity index (n=224 patients).5 Fasting plasma glucose was found to be lower in FA patients.5 In contrast, in a larger cohort of older (age 55–75) patients with obesity undergoing a randomized six-year intensive lifestyle intervention study (n=448), FA was associated with higher BMI and waist circumference.9 However, similar to Kiyici et al. FA was not associated with lipid profile, insulin resistance, and total energy expenditure.5,9 Other studies have also found equivocal associations between FA, BMI, and metabolic syndrome-related measures (Figure 1).2,4
Figure 1.
Overweight is defined as BMI 25–29.9. Class I obesity is BMI 30–34.9. Class II obesity is BMI 35–39.9. Class III obesity (severe obesity) is BMI >40.
Data from: Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. NCHS Health EStats, Centers for Disease Control and Prevention. 2020. Updated February 8, 2021. Accessed January 29, 2021. www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm
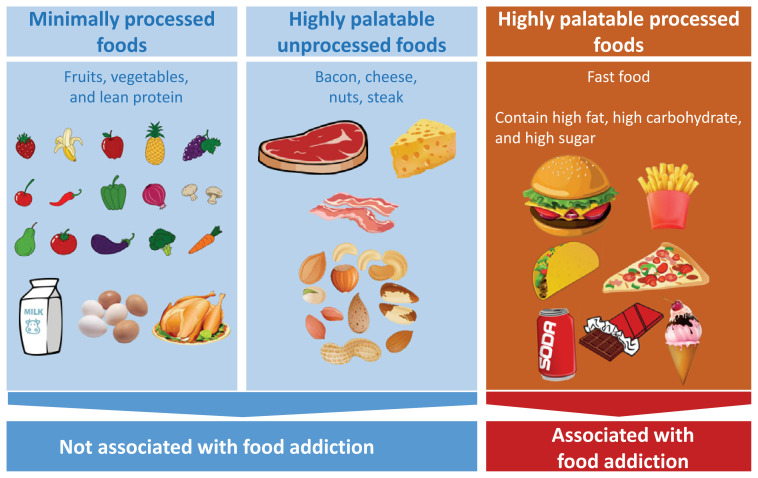
Although FA itself may not directly lead to obesity and metabolic syndrome-like risk factors, it may modulate factors that either contribute to obesity or poor outcomes in weight loss management such as depression, impaired impulse control, eating disorders, and preference for highly palatable foods (Figure 2). For example, patients with obesity and FA were more likely to have depression.5,9,10 Depression was found to be higher in women who are obese, and depression itself was related to a significantly higher daily caloric intake and lower physical activity.11 In a double blind study, women with obesity (n=61) with known emotional eating who were induced into a sad state had significantly greater preference for a sweeter carbohydrate rich beverage compared to a protein rich beverage.12
Figure 2.
With the associations of FA and eating and impulse control disorders such as binge ED and bulimia nervosa, perhaps there is subset of patients with obesity and FA who may benefit from interventions that target such disorders. Munguia et al. studied outcomes of 16 weeks of cognitive behavioral therapy (CBT) in patients separated by subtypes and severity of EDs and food addiction.13 Cognitive behavioral therapy included cognitive restructuring, problem-solving, emotion management techniques, and normalization of eating behavior.13 Patients with EDs had higher FA than those with obesity alone or those with obesity and milder forms of EDs. 13 The patients with both an ED and FA had the poorest outcomes after 16 weeks of CBT compared to patients with obesity and FA.13 In the subset of patients with obesity and FA, incorporating therapies that target addiction like behaviors may be warranted. The review by Adams et al., describes ongoing early phase studies of behavioral interventions that modulate addiction-like behaviors such as impulsivity, self-control, response inhibition, and attention bias towards highly palatable foods.6 Perhaps in the subset of patients with obesity and psychosocial risk factors such as depression, emotional eating, and eating disorders, FA may hamper the ability to manage their weight with diet and lifestyle changes. The following section will explore this concept further by highlighting studies that found associations between FA and preference for highly palatable foods.
Highly Processed and Highly Palatable Foods Are Associated with Food Addiction
The association of FA to SUD-like addiction has been explored in animal and human studies, and includes addiction-like behaviors such as cravings, inability to cut down or stop eating, reward sensitivity, impaired impulse control, and reduced response inhibition.6 These addictive-like behavioral changes are associated with preference for highly palatable foods with addictive properties. An animal study by Lenoir et al. demonstrated that rats preferred the non-nutritive sweetener saccharin (sweet taste without calories) and sucrose (sweet taste with calories) to cocaine, an effect also seen in rats who were already made to be addicted to cocaine.14 Human studies, on the other hand, have not shown that sweet taste and highly palatable foods produce tolerance and withdrawal effects that would define a DSM-V SUD.3 The most common FA-associated symptom was the inability to cut down or stop eating.7 Joyner et al. found that FA was significantly associated with higher ratings of food craving and higher BMI. Food craving itself was associated with higher BMI and binge episodes.15 Craving for fats was significantly associated with addictive-like eating and higher BMI.15 Cravings for sweets significantly mediated the relationship between addictive-like eating and binge eating episodes, but not BMI.15 Cravings for foods high in non-sugar carbohydrates also significantly mediated the relationships between FA and binge eating episodes, but not BMI.15
Food addiction is associated with preference towards highly processed and highly palatable foods (Figure 3). Schulte et al. sought to examine whether highly processed foods were more closely associated with SUD, such as greater loss of control, liking, pleasure, and craving compared to highly palatable but unprocessed foods such as bacon, cheese, nuts, and steak, or minimally processed foods such as fruits, vegetables, and lean protein.16 Highly processed foods were significantly associated with loss of control, liking, pleasure, and craving, indicating greater abuse liability when compared to unprocessed foods (n=501 participants).16 In another study, women who were overweight or had obesity (n=44) were asked to rate subjective food craving during a taste test of ad libitum foods.17 Highly processed, relative to minimally processed, foods were more associated with indicators of abuse liability in those with FA (38.6% of the study population). The question remains on whether FA is associated with an increase in intake of highly palatable foods.
Figure 3.
Studies in humans have shown that FA is associated with higher intake of highly palatable and highly processed foods.18 In a prospective cohort study comprising data collected from 127,000 female nurses, FA was positively associated with consumption of highly palatable foods and processed foods with a combination of carbohydrates and fats such as “fast foods” (hamburgers, fries, pizza), candy bars, and low fat or low-calorie snacks and beverages.19 Interestingly, FA was inversely or not associated with consumption of more non-processed and non-artificial types of foods such as certain sweet foods (cakes), refined grains (pasta, potatoes, white rice), homemade cookies, dark chocolate, full-fat cheese, and sugar-sweetened beverage intake.19 Similarly, university students with FA (n=120) significantly rated preference for highly processed foods with added amounts of fat and refined carbohydrates/sugar (for example: chocolate, pizza, cake), whereas unprocessed foods were least associated with YFAS scores.20 Highly processed foods with higher fat and glycemic index had a stronger association towards problematic and addictive like behaviors compared to unprocessed foods.20 Similarly, in a larger cohort of Turkish university students (n=851), highly palatable foods were significantly correlated with FA, however this study did not compare processed vs. unprocessed foods specifically.21
Food addiction is also associated with higher intake of highly processed foods in patients with obesity. In patients who were overweight or had obesity with FA, significant differences were found in patients without FA (n=29) to those with FA (n=29) with the FA group having significantly higher caloric intake per kg of body weight, higher carbohydrate intake, higher fat intake, and significantly higher amounts of dietary sugar, sodium, potassium, calcium, fat, saturated fat, trans fat, and monounsaturated fat.22
There are several limitations to the studies showing associations between FA and intake of highly palatable and processed foods. Recall bias is an evident limitation as patients were asked to provide subjective estimates of types and amounts of foods and micronutrients eaten over the past 12 months.18,22 Self-report and subjective scoring of food preference may have a recruitment bias from participants who have an interest in answering questions about eating behavior. As noted by Schulte et al., it is difficult to conclude that the magnitude of the subjective experience towards highly palatable foods are as addictive as DSM-V SUD substances.17 Future studies may benefit from examining patients with identified DSM-V SUD and their subjective propensities towards highly palatable foods.
From these studies, it seems that highly palatable and processed foods that contain both carbohydrates and fats are associated with FA compared to unprocessed foods or to sugars alone or carbohydrates alone. Highly processed foods appear to be more reinforcing, have greater abuse liability, addictive properties, and may lead to a greater risk for obesity in those with concurrent FA. The following section will explore FA and outcomes in weight loss management.
Food Addiction and Weight Loss Outcomes
The frequency of FA is high in patients with obesity seeking weight loss through dietary intervention or bariatric surgery.5,23 In patients seeking diet and lifestyle intervention, FA is associated with poorer weight loss management outcomes. Camacho-Barcia et al. examined the role of FA on patients with obesity (n=448) in a randomized parallel-group intervention study that included an intensive lifestyle intervention with an energy-reduced Mediterranean diet, physical activity promotion, and behavioral support on primary prevention of cardiovascular disease (CVD) events.9 FA at baseline resulted in a significantly higher weight regain after three years.9 Gordon et al. examined whether patients with obesity ( n=182) enrolled in a 22-month behavioral weight loss program had changes to FA and subsequent weight loss.24 Reductions in consumption of “problem foods” as identified in the YFAS were significantly associated with reductions in FA symptoms at four months and 10 months, however, were also associated with a sharper rebound of FA symptoms over the 22-month period.24 The initial reduction in problem food consumption were not associated with long-term reductions in weight.24 Month-to-month changes in FA were not associated with month-to-month changes in weight, however higher overall FA scores were associated with less weight loss over 22 months.24 In patients who were overweight or who had obesity enrolled in a 12-month healthy low-fat or healthy low-carbohydrate diet intervention (n=609), FA was significantly associated with increased odds of gaining weight at 12 months and higher attrition rates.25
Similarly, in patients with obesity undergoing a pre-bariatric surgery dietary intervention (n=110), FA was associated with significantly less weight loss.23 These studies support an association between FA and less weight loss in patients with obesity utilizing diet and lifestyle related interventions for weight management.
The current research on bariatric surgery-related weight loss outcomes lacks sufficient data and long term follow up studies to draw conclusions regarding associations with FAA systematic review by Ivezaj et al. found only two out of 19 studies that included FA scores and post-bariatric surgery outcomes.26 Pre-bariatric FA was 32–57%, with significant reductions in FA to 7.2% at six months, 2% at nine months, and 13.7% at 12 months post-operatively. 26 FA was not associated with weight regain and post-surgical weight loss outcomes.26 The caveat of these studies were a high attrition rate post-surgically, which may have skewed the results, and no data of post-bariatric outcomes longer than 12 months.
Currently, there is only one pilot study examining post-bariatric surgery outcomes longer than 12 months, however it was limited by a low number of post-bariatric patients who also met criteria for FA. Cassin et al., examined the outcomes associated with FA within post-bariatric surgery patients (n=100) who received telephone cognitive behavioral therapy (Tele-CBT) sessions (total of six sessions of one hour each) at one-year post-surgery and were followed for an additional 1.25- and 1.5-years post-surgery.27 At one-year post-bariatric surgery, 13% of patients had scored for FA.27 Those with FA had significantly higher scores for binge eating disorder, depression, anxiety, however a statistically insignificant 8% less total weight loss.27 Compared to the control group (no Tele-CBT), patients who completed the Tele-CBT had significantly lower FA symptoms scores at 1.25 years, but not at 1.5 years. Only one patient in the Tele-CBT group met full diagnostic criteria for FA at 1.25 years and 1.5 years, and only two patients in the control group met the full criteria for FA at 1.25 years but not at 1.5yrs.27 Thus, although this pilot study showed Tele-CBT was associated with improved FA post-bariatric surgery outcomes, it was limited by a small sample size. Due to the limited size, length, and high drop-out rates in bariatric management studies, it is currently difficult to ascertain whether FA plays a role in modifying surgical weight management in patients with obesity.
The presence of food addiction may modify weight loss outcomes in patients with obesity in respect to consumption of problem foods, long-term weight goals, and existing psychosocial/ behavioral conditions such as binge eating, depression, and anxiety. A multifaceted approach to improve weight loss outcomes in patients with obesity and FA may be beneficial. A recent systematic review by Leary et al. of nine studies (total of n=812 patients) examined the efficacy of weight loss interventions targeted specifically to FA.28 Interventions included diet and lifestyle modification, behavioral modification, medications, and surgical modifications. Five out of eight studies that included both pre- and post-intervention FA scores reported a statistically significant reduction in FA post-intervention.28 Two of the five studies were medication interventions that used either naltrexone and bupropion or pexacerfont and reported a significant reduction in FA symptoms post-intervention.28 In three studies with lifestyle modification interventions and two surgical interventions, there was a significant reduction in FA symptom scores in the intervention group only.28 These few initial studies are very encouraging, however remain limited by small sample sizes and lack of long-term follow-up.
Conclusion
Obesity management is a challenging lifelong process. Food addiction is present in a subset of patients who are overweight or have obesity, and its presence is associated with other psychosocial disorders such as binge eating, depression, anxiety, eating disorders associated with poor impulse control, and lower quality of life. Food addiction is not recognized as a DSM-V defined SUD, however, there are similarities between FA and SUD such as cravings, reduced control over intake, increased impulsivity and altered reward-sensitivity. Studies in humans have shown that FA is associated with higher intake of and preference for highly processed and highly palatable foods. Thus far, studies have found equivocal associations between FA, BMI and metabolic syndrome-related measures. FA is associated with less weight loss in patients with obesity utilizing diet and lifestyle related interventions for weight loss. In bariatric weight loss management, there is insufficient data linking FA to weight loss outcomes and further studies with long-term follow-up are required.
As further research into food addiction continues, how can physicians apply this knowledge to guide obesity management? Food addiction is tied to complex underlying psychosocial factors and a preference for highly processed foods with addictive properties associated with lower success in weight loss strategies. Furthermore, higher intake of highly processed foods increases mortality.29 The increasingly “obesogenic environment” with easily available highly processed foods also contributes to the challenge of weight management.30 However addressing the availability of highly processed foods and ingredients is a complex problem with no clear short-term solutions. Early identification of the subset of patients with obesity who have FA in addition to psychosocial factors that modulate FA, such as depression, eating disorders, and impulse control disorders, may be an important step in the initial assessment of obesity management patients. This may allow for targeted or multifaceted therapies for improving weight loss outcomes. Incorporating behavioral interventions such as CBT that modulate addiction-like behaviors such as impulsivity, self-control, response inhibition, and attention bias towards highly palatable foods may help improve long term obesity and weight management outcomes.
Footnotes
Reuben De Almeida, MD, MSc, is an Internal Medicine Resident, University of Missouri-Kansas City-School of Medicine (UMKC-SOM). Peminda Cabandugama, MD, is an Assistant Professor of Medicine and Faculty Member of the Endocrinology Fellowship Program at the UMKC-SOM. Geetha Kamath, MD, (above), is an Assistant Professor, Department of Internal Medicine, University Health Weight Management Clinic, UMKCSOM. All are in Kansas City, Missouri.
Disclosure
None reported.
References
- 1.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief. 2020;360:1–8. [PubMed] [Google Scholar]
- 2.Zawertailo L, Attwells S, deRuiter WK, Le TL, Dawson D, Selby P. Food Addiction and Tobacco Use Disorder: Common Liability and Shared Mechanisms. Nutrients. 2020;12(12):3834. doi: 10.3390/nu12123834. Published 2020 Dec 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziauddeen H, Farooqi IS, Fletcher PC. Obesity and the brain: how convincing is the addiction model? Nat Rev Neurosci. 2012;13(4):279–286. doi: 10.1038/nrn3212. Published 2012 Mar 14. [DOI] [PubMed] [Google Scholar]
- 4.Constant A, Moirand R, Thibault R, Val-Laillet D. Meeting of Minds around Food Addiction: Insights from Addiction Medicine, Nutrition, Psychology, and Neurosciences. Nutrients. 2020;12(11):3564. doi: 10.3390/nu12113564. Published 2020 Nov 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiyici S, Koca N, Sigirli D, Aslan BB, Guclu M, Kisakol G. Food Addiction Correlates with Psychosocial Functioning More Than Metabolic Parameters in Patients with Obesity. Metab Syndr Relat Disord. 2020;18(3):161–167. doi: 10.1089/met.2019.0108. [DOI] [PubMed] [Google Scholar]
- 6.Adams RC, Sedgmond J, Maizey L, Chambers CD, Lawrence NS. Food Addiction: Implications for the Diagnosis and Treatment of Overeating. Nutrients. 2019;11(9):2086. doi: 10.3390/nu11092086. Published 2019 Sep 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Penzenstadler L, Soares C, Karila L, Khazaal Y. Systematic Review of Food Addiction as Measured with the Yale Food Addiction Scale: Implications for the Food Addiction Construct. Curr Neuropharmacol. 2019;17(6):526–538. doi: 10.2174/1570159X16666181108093520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gearhardt AN, Corbin WR, Brownell KD. Development of the Yale Food Addiction Scale Version 2.0. Psychol Addict Behav. 2016;30(1):113–121. doi: 10.1037/adb0000136. ] [DOI] [PubMed] [Google Scholar]
- 9.Camacho-Barcia L, Munguía L, Lucas I, et al. Metabolic, Affective and Neurocognitive Characterization of Metabolic Syndrome Patients with and without Food Addiction. Implications for Weight Progression Nutrients. 2021;13(8):2779. doi: 10.3390/nu13082779. Published 2021 Aug 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burmeister JM, Hinman N, Koball A, Hoffmann DA, Carels RA. Food addiction in adults seeking weight loss treatment. Implications for psychosocial health and weight loss. Appetite. 2013;60(1):103–110. doi: 10.1016/j.appet.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Simon GE, Ludman EJ, Linde JA, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30(1):32–39. doi: 10.1016/j.genhosppsych.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spring B, Schneider K, Smith M, et al. Abuse potential of carbohydrates for overweight carbohydrate cravers. Psychopharmacology (Berl) 2008;197(4):637–647. doi: 10.1007/s00213-008-1085-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munguía L, Gaspar-Pérez A, Jiménez-Murcia S, et al. Food Addiction in Eating Disorders: A Cluster Analysis Approach and Treatment Outcome. Nutrients. 2022;14(5):1084. doi: 10.3390/nu14051084. Published 2022 Mar 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenoir M, Serre F, Cantin L, Ahmed SH. Intense sweetness surpasses cocaine reward. PLoS One. 2007;2(8):e698. doi: 10.1371/journal.pone.0000698. Published 2007 Aug 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joyner MA, Gearhardt AN, White MA. Food craving as a mediator between addictive-like eating and problematic eating outcomes. Eat Behav. 2015;19:98–101. doi: 10.1016/j.eatbeh.2015.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulte EM, Smeal JK, Gearhardt AN. Foods are differentially associated with subjective effect report questions of abuse liability. PLoS One. 2017;12(8):e0184220. doi: 10.1371/journal.pone.0184220. Published 2017 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schulte EM, Sonneville KR, Gearhardt AN. Subjective experiences of highly processed food consumption in individuals with food addiction. Psychol Addict Behav. 2019;33(2):144–153. doi: 10.1037/adb0000441. [DOI] [PubMed] [Google Scholar]
- 18.Pursey KM, Skinner J, Leary M, Burrows T. The Relationship between Addictive Eating and Dietary Intake: A Systematic Review. Nutrients. 2021;14(1):164. doi: 10.3390/nu14010164. Published 2021 Dec 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lemeshow AR, Rimm EB, Hasin DS, et al. Food and beverage consumption and food addiction among women in the Nurses’ Health Studies. Appetite. 2018;121:186–197. doi: 10.1016/j.appet.2017.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulte EM, Avena NM, Gearhardt AN. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10(2):e0117959. doi: 10.1371/journal.pone.0117959. Published 2015 Feb 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayaz A, Nergiz-Unal R, Dedebayraktar D, et al. How does food addiction influence dietary intake profile? PLoS One. 2018;13(4):e0195541. doi: 10.1371/journal.pone.0195541. Published 2018 Apr 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pedram P, Sun G. Hormonal and dietary characteristics in obese human subjects with and without food addiction. Nutrients. 2014;7(1):223–238. doi: 10.3390/nu7010223. Published 2014 Dec 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guerrero Pérez F, Sánchez-González J, Sánchez I, et al. Food addiction and preoperative weight loss achievement in patients seeking bariatric surgery. Eur Eat Disord Rev. 2018;26(6):645–656. doi: 10.1002/erv.2649. [DOI] [PubMed] [Google Scholar]
- 24.Gordon EL, Merlo LJ, Durning PE, Perri MG. Longitudinal Changes in Food Addiction Symptoms and Body Weight among Adults in a Behavioral Weight-Loss Program. Nutrients. 2020;12(12):3687. doi: 10.3390/nu12123687. Published 2020 Nov 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fielding-Singh P, Patel ML, King AC, Gardner CD. Baseline Psychosocial and Demographic Factors Associated with Study Attrition and 12-Month Weight Gain in the DIETFITS Trial. Obesity (Silver Spring) 2019;27(12):1997–2004. doi: 10.1002/oby.22650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ivezaj V, Wiedemann AA, Grilo CM. Food addiction and bariatric surgery: a systematic review of the literature. Obes Rev. 2017;18(12):1386–1397. doi: 10.1111/obr.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cassin S, Leung S, Hawa R, Wnuk S, Jackson T, Sockalingam S. Food Addiction Is Associated with Binge Eating and Psychiatric Distress among Post-Operative Bariatric Surgery Patients and May Improve in Response to Cognitive Behavioural Therapy. Nutrients. 2020;12(10):2905. doi: 10.3390/nu12102905. Published 2020 Sep 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leary M, Pursey KM, Verdejo-Garcia A, Burrows TL. Current Intervention Treatments for Food Addiction: A Systematic Review. Behav Sci (Basel) 2021;11(6):80. doi: 10.3390/bs11060080. Published 2021 May 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suksatan W, Moradi S, Naeini F, et al. Ultra-Processed Food Consumption and Adult Mortality Risk: A Systematic Review and Dose-Response Meta-Analysis of 207,291 Participants. Nutrients. 2021;14(1):174. doi: 10.3390/nu14010174. Published 2021 Dec 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lustig RH. Ultraprocessed Food: Addictive, Toxic, and Ready for Regulation. Nutrients. 2020;12(11):3401. doi: 10.3390/nu12113401. Published 2020 Nov 5. [DOI] [PMC free article] [PubMed] [Google Scholar]