Abstract
Purpose
Based on the diagnosis-related groups payment, China developed an innovative episode-based payment scheme, called “payment method by disease types with point counting”, to control health expenditures inflation. This study aimed to investigate the impacts of this new payment method on volume, expenditures, and efficiency in Chinese public hospitals.
Methods
The study sample consisted of 7 tertiary hospitals and 14 secondary hospitals in Jinhua (intervention group) and 4 tertiary hospitals and 14 secondary hospitals in Taizhou (control group). Monthly data points were collected for each sampled hospital from June 2016 to June 2019 using a self-administered questionnaire with impact evaluation indicators. Controlled interrupted time-series analysis was employed to estimate the effect of the new payment method.
Results
The significant slowing trends in inpatient expenditures per visit (tertiary hospitals: β7=−123.16, p=0.042; secondary hospitals: β7=−89.24, p=0.021) and out-of-pocket payments (tertiary hospitals: β7=−4.18, p=0.027; secondary hospitals: β7=−4.87, p=0.019) were observed after policy intervention. However, outpatient expenditures per visit in tertiary (β7=1.67, p=0.018) and secondary hospitals (β7=1.24, p=0.003) rose faster with the new payment method. Additionally, payment reform also caused an increase in the number of inpatient visits (β7=100.01, p=0.038) and reduced the length of stay (β7=−0.10, p=0.036) in tertiary hospitals.
Conclusion
The introduction of payment method by disease types with point counting causes the cost containment for inpatient care, whereas the increase in outpatient expenditures. The findings suggest this new payment scheme has the potential for rollout in other areas, but the cost-shifting from the inpatient to outpatient setting should be prevented.
Keywords: episode-based payment, expenditures, public hospitals, controlled interrupted time series, China
Introduction
Rapid growth in health care expenditures in high-income and lower-middle-income countries has become a significant concern for policymakers and the public.1 China is not exceptional. Total health expenditures in China increased from 1,9980.4 billion RMB in 2010 to 65,195.9 billion RMB in 2019 and are growing at a rate of more than 10% per year.2 Soaring health expenditures threw a great challenge on China’s health system. Fee-for-service (FFS) payment drives the rising medical expenditure by incentivizing overtreatment.3 In recent years, the Chinese government has been determined to explore alternative payment approaches.
Although several payment methods (eg, global budgets, capitation) have been adopted since the new reform of China’s health system in 2009, one of the payment methods called diagnosis-related groups (DRGs) attracted widespread attention. Under the DRG-based payment system, hospitals are remunerated with a fixed predefined amount according to the characteristics and disease complexity of patients regardless of the actual costs that hospitals incur for treatments.4,5 In comparison with FFS, DRG-based payment transfers the financial risk to healthcare providers and therefore encourages them to increase efficiency and avoid overtreatment. Some cities in China (eg, Beijing, Zhongshan) have already piloted a DRG-based payment ten years ago.5,6 Concerning the effectiveness of this payment scheme, existing studies proved that it reduced health expenditures and out-of-pocket (OOP) payments.6–8 However, some unintended consequences were reported as well. For example, hospitals provided inadequate services, discharged patients prematurely, and decreased the quality of care.7,9 Moreover, previous studies also found unnecessary admissions, patient cream-skimming, and upcoding under the DRGs system.8,10
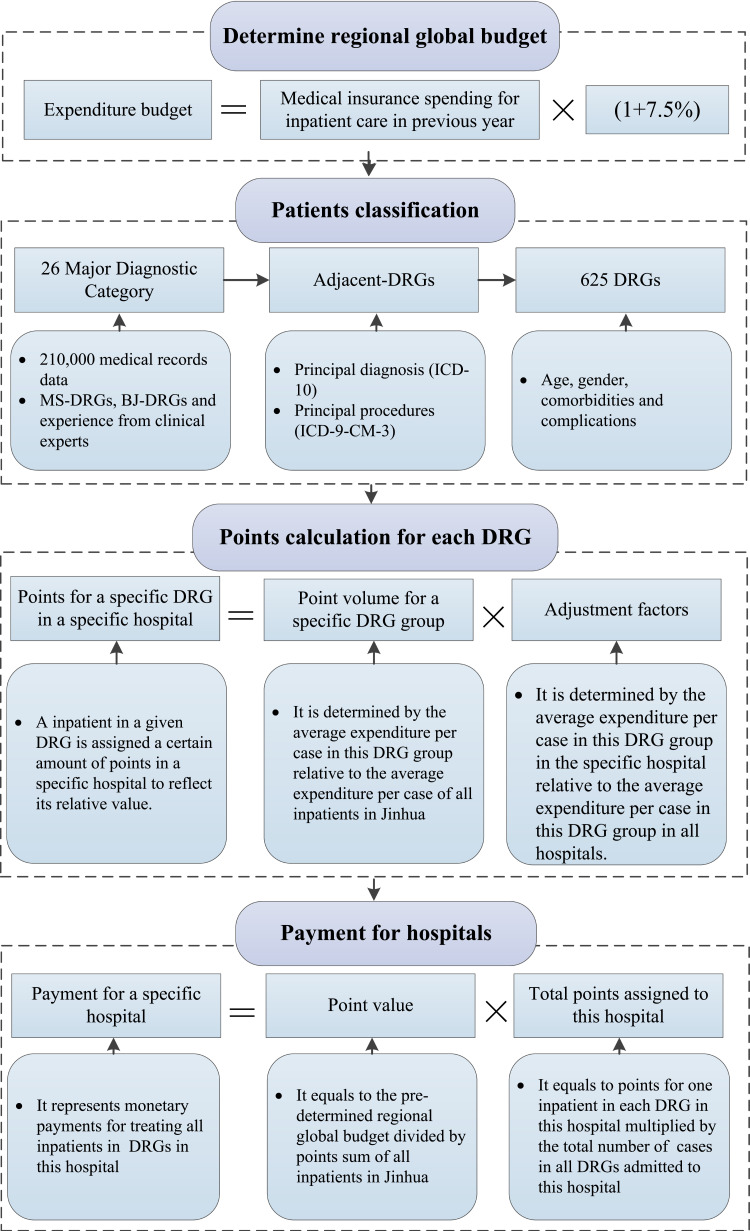
To overcome these shortcomings, Jinhua, an economically developed city in Zhejiang province, redesigned the rules of DRGs payment to develop an innovative payment method, called “payment method by disease types with point counting”.11,12 Under this new payment system, a certain number of points reflecting the relative usage of resources are assigned to each DRG group. The monetary value for each point is calculated according to the predetermined regional budget and the point sum of all inpatient cases for a whole year in Jinhua. As a result, the amount of payment for each inpatient is not fixed, and the annual reimbursement for each hospital is affected by the service volume and its cost relative to other hospitals.11,12 Figure 1 sketches the core design components of the payment method by disease types with point counting method in Jinhua. A detailed introduction is provided in the Institutional background section.
Figure 1.
Core components of payment method by disease types with point counting.
With the implementation of Jinhua’s payment scheme, this new payment method has caught nationwide attention. In 2021, National Healthcare Security Administration selected Jinhua as a national demonstration city for DRGs payment, and approximately 60 cities learned from Jinhua’s experience and started implementing this new payment method. Predictably, this new episode-based payment scheme will create promising effects. Before the broad rollout of this payment system, policymakers need to be informed of its potential consequences. Despite findings from the published literature providing evidence to understand the impact of provider payment on healthcare outcomes,7,9,13,14 the effectiveness of this innovative episode-based payment scheme in addressing the unintended consequences has not been reported. Additionally, whether negative performances will be created accordingly under this payment system with the regional global budget is unknown.
Using hospital-level data from Jinhua, this study aimed to evaluate the impacts of payment method by disease types with point counting compared with a neighboring city by employing a controlled interrupted time-series analysis (ITSA). This study will add to the literature in several ways. First, we provided the first empirical evidence on understanding hospitals´ response to this innovative payment scheme in China. Second, ITSA with an independent control, a useful quasi-experimental design, was used to accurately estimate the longitudinal effects of policy intervention. Third, our results yield important policy implications for addressing the unintended consequences caused by the DRGs payment.
Methods
Institutional Background
To control the rapid increase in health expenditures, Jinhua started payment reform since 2016. Based on DRG-based patient classification rules, Jinhua designed the payment method by disease types with point counting and selected seven public hospitals from urban areas to pilot from July 2016 to June 2017. After a year of the pilot, Jinhua started to fully promote this new payment method in all 42 hospitals in urban areas on July 1, 2017. Except for expenditures on mental diseases and some specific cancers, this payment method covers almost all inpatient expenditures. This payment method works in the following four steps (Figure 1).
The first step is to determine the regional global budget. It was calculated based on a 7.5% increase in total medical insurance spending for inpatient care in the previous year. The second step is the classification of inpatient cases. Following the classification system from Beijing-DRGs (BJ-DRGs), Medicare Severity DRGs (MS-DRGs), as well as experience from specialist physicians, Jinhua used 210,000 medical records from all hospitals and classified them into 26 major diagnostic categories (MDCs).15,16 Then, the International Classification of Diseases, 10th Revision and International Classification of Diseases, 9th Revision, Clinical Modification were used to identify the principal diagnosis and principal procedure (surgical, diagnostic, or therapeutic procedure), respectively. Lastly, demographic and administrative variables (such as age, gender, comorbidities, and complications) were used to further divide each principal diagnosis and principal procedure into different DRG groups. Accordingly, a total of 625 DRGs were generated. The third step is to calculate the points for each DRG group. Firstly, the specific point volume for each DRG group is determined by the average expenditure per case in this DRG group relative to the average expenditure per case of all inpatients in Jinhua. Then, the adjustment factor is calculated to reflect the differences in the cost of treating patients from the same DRG group in different hospitals. It is determined by the average expenditure per case in this DRG group in the specific hospital relative to the average expenditure per case in this DRG group in all hospitals. Finally, the points for a specific DRG group in a specific hospital are equal to the product of the above two-step estimation results. Consequently, different hospitals are assigned different point volumes for the same DRG group.11,12 The fourth step is payment for each hospital. The monetary value for one point is calculated according to the quotient of the predetermined regional global budget and the point sum of all inpatients rendered by all hospitals in Jinhua. As a result, the actual reimbursements for each hospital are equal to the sum of the monetary value of the total points.
Study Design and Setting
This study employed an ecologically controlled ITSA design with pre-intervention and post-intervention periods. As a quasi-experimental study design for strong causal inference, ITSA allows us to discern the effects of the payment method from that of secular time trends by testing a trend difference before and after policy implementation.17 In addition, a comparison group not exposed to the intervention was utilized to reduce time-varying confounding.18 Therefore, Jinhua was set as the intervention group and compared with the control group.
Concerning comparability with Jinhua, neighboring Taizhou city in Zhejiang province was regarded as the control group owing to its similar characteristics in terms of economic development and health resource allocation. In 2019, Jinhua, with a 5.62 million population, and Taizhou, with a 6.15 million population, created ¥455.991 billion and ¥ 513.405 billion in the gross domestic product (GDP), respectively.19 In comparison with the situation of Jinhua, with 145 hospitals, 30,305 beds, and 18,938 doctors, Taizhou has 133 hospitals equipped with 27,762 beds and 19,258 doctors. Annual discharges from hospitals in Jinhua and Taizhou range from 850,000 to 870,000.19 In addition to the similarity to Jinhua, another reason for choosing Taizhou as the control group is that no great payment reform was implemented during the observation period of this study. It helps us estimate intervention effects more accurately.
Data Source
About 50% of public hospitals in the study cities were extracted with the adoption of a random sampling strategy using hospital code. Twenty-one public hospitals in Jinhua (7 tertiary hospitals and 14 secondary hospitals) and 18 public hospitals in Taizhou (4 tertiary hospitals and 14 secondary hospitals) were selected. For each hospital, monthly data points were collected for 37 consecutive months (13 months pre-intervention and 24 months post-intervention) starting in June 2016 and ending in June 2019. We used the self-administered questionnaire, including impact evaluation indicators, for data collection. The questionnaire was distributed to managers in each hospital via e-mail in June 2021, and all questionnaires were returned. All returned questionnaires were checked for completeness and credibility to ensure high data quality.
Outcome Variables
Based on existing literature and availability of data,7,14 this study evaluated the impact of payment method reform on public hospitals from three aspects: service volume, expenditures, and efficiency. Hospital volume was measured by the number of outpatient visits and inpatient visits. Medical expenditures were measured by outpatient expenditures per visit, inpatient expenditures per visit, and OOP payments per visit. Outpatient/inpatient expenditures consist of expenditures for drugs, consumables, examinations, laboratory tests, and medical consultation services in outpatient/inpatient sites. The average length of stay (LOS) was used to measure hospital efficiency. Before a model was established with these variables, all expenditure data were adjusted by the consumer price index for their comparable monetary value during 2016 and 2019.20
Data Analysis
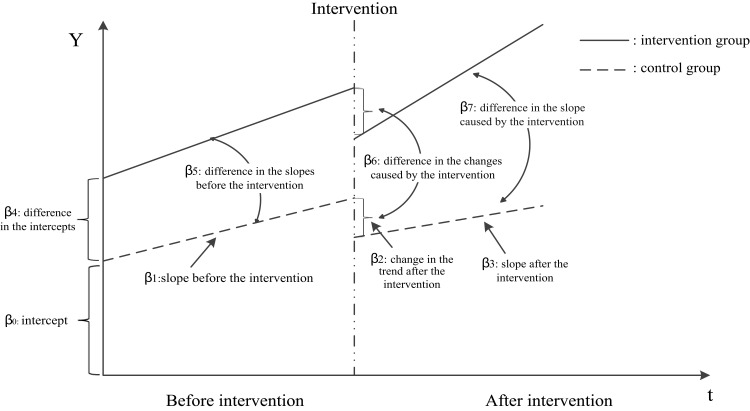
We used a multiple-group ITSA comparing the outcome variables between the intervention and control city and between the pre-intervention (June 2016 until June 2017) and post-intervention (July 2017 until June 2019) period. Figure 2 shows the visual description of multiple-group ITSA, and the model employs the following equation:
 |
Figure 2.
Visual description of multiple group ITSA.
Where  is the outcome variable measured at each monthly time point t;
is the outcome variable measured at each monthly time point t;  represents the months since the observation started;
represents the months since the observation started;  is a dummy variable with an assignment of 0 and 1, representing before and after the intervention respectively; Z is also a dummy variable indicating the treatment and control group (0=Taizhou, 1=Jinhua);
is a dummy variable with an assignment of 0 and 1, representing before and after the intervention respectively; Z is also a dummy variable indicating the treatment and control group (0=Taizhou, 1=Jinhua);  ,
,  and
and  represent all interaction terms among the variables explained above.21,22 The meanings of
represent all interaction terms among the variables explained above.21,22 The meanings of  to
to  are displayed in Figure 2, in which
are displayed in Figure 2, in which  to
to  represent trends in the control group;
represent trends in the control group;  and
and  are differences in the intercepts and slopes between the intervention and control groups prior to the intervention; and
are differences in the intercepts and slopes between the intervention and control groups prior to the intervention; and  and
and  indicate the differences in level and slope changes after intervention between the intervention and control groups. Thus, the impact of the payment reform was estimated by observing whether the intervention hospitals deviated from baseline levels (
indicate the differences in level and slope changes after intervention between the intervention and control groups. Thus, the impact of the payment reform was estimated by observing whether the intervention hospitals deviated from baseline levels ( ) and trends (
) and trends ( ) to a greater extent than the control hospitals.
) to a greater extent than the control hospitals.
An ITSA dataset was generated by calculating the average of sampled hospital data by month, differentiating control from intervention hospitals. Secondary and tertiary hospitals were subjected to ITSA separately to observe the impact of the intervention on hospitals at different levels. Data autocorrelation must be taken into account. Hence, ordinary least squares regression using Newey–West standard errors was adopted to handle autocorrelation and potential heteroskedasticity.22 All statistical analyses were performed using Stata 14.0.
Results
Overall Characteristics of Outcome Variables
Table 1 shows the monthly mean and standard deviation (SD) of outcome variables by tertiary and secondary hospitals in the intervention (Jinhua) and control groups (Taizhou). In both cities, the number of outpatients and inpatients in tertiary and secondary hospitals showed a growing trend from pre-intervention to post-intervention.
Table 1.
Monthly Mean (SD) of Outcome Variables in Intervention and Control Groups
| Indicators | Regions | Tertiary Hospitals | Secondary Hospitals | ||
|---|---|---|---|---|---|
| Pre-Intervention | Post-Intervention | Pre-Intervention | Post-Intervention | ||
| Number of outpatients (n) | Jinhua | 151,314.46 (9786.14) | 174,558.08 (14,096.53) | 19,156.77 (1384.25) | 21,357.71 (3476.00) |
| Taizhou | 102,945.31 (6653.38) | 120,252.71 (15,711.47) | 24,096.08 (2506.77) | 28,182.46 (3156.74) | |
| Number of inpatients (n) | Jinhua | 8713.69 (578.77) | 10,554.799 (1148.52) | 357.38 (25.48) | 446.13 (132.52) |
| Taizhou | 3628.85 (229.76) | 4273.63 (550.40) | 1333.69 (108.51) | 1535.08 (165.57) | |
| Expenditures per outpatient visit (CNY) | Jinhua | 238.81 (4.97) | 250.99 (12.47) | 162.47 (4.11) | 178.88 (20.31) |
| Taizhou | 240.69 (7.36) | 251.31 (12.61) | 217.80 (6.38) | 226.24 (8.41) | |
| Expenditures per inpatient visit (CNY) | Jinhua | 11,294.78 (528.24) | 11,290.55 (715.61) | 7585.44 (585.09) | 8003.99 (682.25) |
| Taizhou | 9497.53 (628.57) | 9676.68 (612.47) | 5837.87 (289.42) | 6196.62 (379.41) | |
| OOP payments per visit (CNY) | Jinhua | 222.67 (26.33) | 215.03 (49.73) | 374.71 (39.56) | 350.86 (38.09) |
| Taizhou | 438.41 (58.16) | 363.86 (29.54) | 151.37 (7.91) | 163.96 (24.55) | |
| LOS (day) | Jinhua | 9.34 (0.32) | 7.82 (0.71) | 12.26 (0.51) | 10.34 (0.72) |
| Taizhou | 8.82 (0.54) | 7.74 (0.69) | 11.83 (0.45) | 9.94 (0.73) | |
Unlike the control city, average inpatient expenditures in tertiary hospitals from the intervention ones decreased from 11,294.78 CNY to 11,290.55 CNY, whereas outpatient expenditures increased across the study period. Data also showed a reduction in OOP payments per visit, except for secondary hospitals in Taizhou (151.37 CNY vs 163.96 CNY). In comparison with the control group, LOS in the intervention ones showed a greater decline, especially in tertiary hospitals.
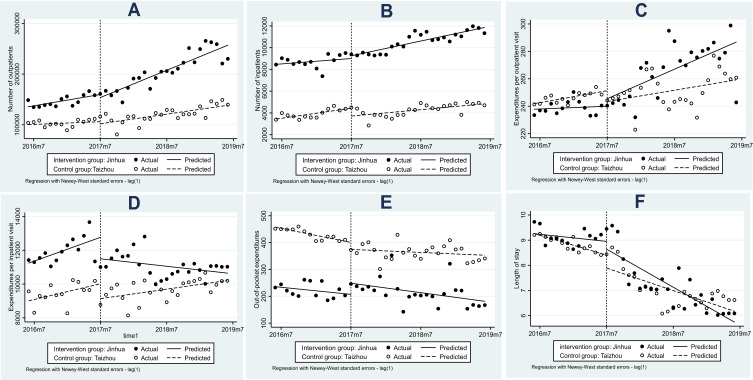
Impacts of the New Payment Method on Tertiary Hospitals
Table 2 and Figure 3 display the controlled ITSA results for tertiary hospitals. In terms of service volume, the pre-trend difference between the intervention and control groups was not significant, despite the intervention group starting with a numerically higher outpatient (β4=35,264.23, p<0.001) and inpatient (pre-level difference: β4=5469.15, p<0.001) visits. Therefore, the two groups are sufficiently comparable prior to the policy intervention. After the implementation of the new payment method, a steeper increase (β7=100.01, p=0.038) in inpatient visits was observed, indicating that the payment reform caused the growth of the number of inpatient visits in tertiary hospitals. However, the intervention effect on the number of outpatient visits was not remarkable, owing to the statistically non-significant differences in level and trend change.
Table 2.
Impact of Payment Method Reform in Tertiary Hospitals Based on Controlled ITSA
| Number of Outpatients | Number of Inpatients | Expenditures Per Outpatient Visit | Expenditures Per Inpatient Visit | OOP Payments Per Visit | LOS | |
|---|---|---|---|---|---|---|
| Before intervention | ||||||
| Level (control group, β0) | 100,242.80** | 3435.60** | 241.87** | 9009.28** | 457.59** | 9.26** |
| Trend (control group, β1) | 450.42 | 76.83** | 0.73** | 77.71* | −4.39** | −0.07** |
| Difference in level (β4) | 35,264.23** | 5031.79** | −4.05 | 2235.96** | −221.74** | −0.01 |
| Difference in trend (β5) | 1414.92 | 35.78 | −0.56 | 39.52 | 2.19 | 0.04 |
| After intervention | ||||||
| Level change (control group, β2) | −4042.05 | −723.70* | −7.90 | −879.88* | −25.86 | −0.52 |
| Change in trend (control group, β3) | 1131.88 | −27.89 | −0.04 | −31.01 | 3.45 | −0.01 |
| Difference in level change (β6) | −2032.88 | 976.08 | 13.39 | −390.73 | 67.26* | 0.21 |
| Difference in change in trend (β7) | 1499.28 | 100.01* | 1.67* | −123.16* | −4.18* | −0.10* |
| F | 98.36** | 437.66** | 14.53** | 41.61** | 168.79** | 182.71** |
Note: *p<0.05; **p<0.001.
Figure 3.
Time trend of volume, expenditure and efficiency by months and group in tertiary hospitals. (A) and (B) are number of outpatients and inpatients in tertiary hospitals; (C) and (D) are outpatient and inpatient expenditures per visit in tertiary hospitals; (E) is OOP payments per visit in tertiary hospitals; (F) is LOS in tertiary hospitals.
With regard to expenditures, the intervention and control groups had similar trends in spite of differences in their baseline levels in the pre-intervention period. After the payment method reform, we found a growing trend in inpatient expenditures per visit (post-trend difference: β7=−123.16, p=0.042) and OOP payments per visit (post-trend difference: β7=−4.18, p=0.027) was slowing, even though OOP payments instantly increased by ¥67.26 (p=0.003). However, outpatient expenditures per visit in the intervention group displayed a significantly sharper increase (post-trend difference: β7=1.67, p=0.018) than that in the control ones. The data also showed remarkably decreased LOS (post-trend difference: β7=−0.10, p=0.036) in the intervention group after the reform.
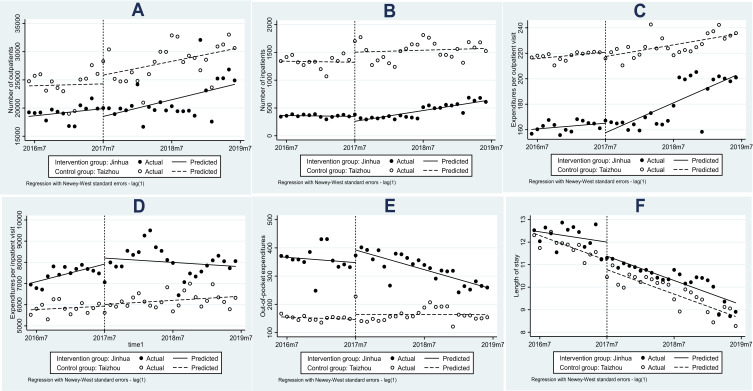
Impacts of the New Payment Method on Secondary Hospitals
Table 3 and Figure 4 show the controlled ITSA results for secondary hospitals. Similar to tertiary hospitals, no remarkable differences were observed in the pre-intervention trends for the six outcome variables in spite of the substantial difference in the intercepts between the intervention and control groups before the intervention. Overall, the payment scheme reform created significant effects on medical expenditures in secondary hospitals, but it did not involve efficiency and service volume. Specifically, introducing the new payment method was followed by a reduction of ¥89.24 (p=0.021) per month in inpatient expenditures and ¥4.87 (p=0.019) per month in OOP payments. However, outpatient expenditures (post-trend difference: β7=1.24, p=0.003) in the intervention group showed faster growth than that in the control group.
Table 3.
Impact of Payment Method Reform in Secondary Hospitals Based on Controlled ITSA
| Number of Outpatients | Number of Inpatients | Expenditures Per Outpatient Visit | Expenditures Per Inpatient Visit | OOP Expenditures Per Visit | LOS | |
|---|---|---|---|---|---|---|
| Before intervention | ||||||
| Level (control group, β0) | 23,932.00** | 1342.85** | 215.46 | 5757.89** | 155.43** | 12.38** |
| Trend (control group, β1) | 27.34 | −1.52 | 0.41* | 13.32 | −0.68 | −0.09** |
| Difference in level (β4) | −5410.54** | −977.85** | −55.21** | 1257.67** | 212.66** | 0.11 |
| Difference in trend (β5) | 78.54 | 0.25 | −0.04 | 56.01 | −0.88 | 0.05 |
| After intervention | ||||||
| Level change (control group, β2) | 1551.07 | 181.34 | −3.41 | 78.54 | 17.82 | −0.41* |
| Change in trend (control group, β3) | 176.47 | 4.46 | 0.35 | 2.92 | 0.63 | 0.01 |
| Difference in level change (β6) | −2935.27 | −269.07 | −4.08 | 203.76 | 26.64 | −0.22 |
| Difference in change in trend (β7) | −35.05 | 12.92 | 1.24* | −89.24* | −4.87* | −0.05 |
| F | 27.33** | 279.20** | 317.60** | 45.86** | 186.19 | 90.85** |
Note: *p<0.05; **p<0.001.
Figure 4.
Time trend of volume, expenditure and efficiency by months and group in secondary hospitals. (A) and (B) are number of outpatients and inpatients in secondary hospitals; (C) and (D) are outpatient and inpatient expenditures per visit in secondary hospitals; (E) is OOP payments per visit in secondary hospitals; (F) is LOS in secondary hospitals.
Discussion
This study focused on the impacts of payment method by disease types with point counting using the controlled ITSA design. We found that public hospitals responded sensitively to this new payment scheme and adjusted their behaviors accordingly, resulting in remarkable changes in volume, expenditures, and efficiency.
The reduction in inpatient expenditures in tertiary and secondary hospitals was great after the payment reform. Health providers are incentivized to actively control costs and avoid potential revenue loss, because shifting from FFS to this new case-based payment scheme with a regional global budget generated significantly increased financial risks.6,23 However, the hospital expenditure in the Chinese health insurance system consists of insurance payments and OOP payments. When the case-based payment method was only applied to insurance payments but not to the total hospital expenditures or OOP payments, the risk of cost-shifting to OOP payments may occur.24,25 For example, providers might induce patients to use some drugs and tests that are not covered by health insurance, which may increase the financial burden of individual patients.
Encouragingly, a decline in OOP payments following the implementation of the new payment method was observed in this study. Under this new episode-based payment system, on the one hand, the hospital is reimbursed for each admission depending on the relative level of its cost to the regional average cost. Hospitals are highly incentivized to make the total cost (including OOP payments) lower than the expected payment per case to maximize surplus. On the other hand, strict supervision from Jinhua’s medical insurance bureau also prevents the behavior of shifting cost containment pressure to patients.
Notably, the expenditures per outpatient visit increased largely after policy intervention. A potential explanation is that the current payment method is designed for inpatient care, but does not involve an outpatient setting. Additionally, FFS for outpatient care was implemented in most Chinese public hospitals.26 Lack of incentives and restraints similar to that in inpatient sites, the cost-shift from inpatient to outpatient setting might occur in order to minimize costs of inpatient care. For example, specialists require patients to finish examinations and laboratory tests in outpatient setting before admission. In this case, however, the financial burden of outpatients might increase because of the lower reimbursement rate for outpatient expenditures in China’s insurance system.27 It informs policymakers that careful monitoring is critical to avoid strategic behaviors of compensating for lost income, and an appropriate payment method for outpatient care should be designed and implemented.
Our results also found that this new payment method caused an increase in inpatients in tertiary hospitals. In prior studies, DRG-based payment was found to provide incentives to admit more patients who only need outpatient care, further resulting in increased inpatients.10,28 However, the explanation for our finding is different. According to the rules of this payment method, the monetary value for each point is reduced when an unnecessary admission rate increases largely. It is not beneficial for hospitals to increase inpatients by admitting patients who only need outpatient care. We assume the new payment scheme motivates tertiary hospitals to utilize their competitive advantage to attract more patients from secondary hospitals for earning more points, although an unremarkable reduction in service volume for secondary hospitals was observed in this study. Moreover, tertiary hospitals, based on point assignment rules, might be given more points when they admit patients from the same DRG group as the secondary hospitals. Under such an incentive mechanism, inpatients could be distributed unreasonably between secondary and tertiary hospitals. The finding reminds policymakers to design payment method components, including appropriate point value weight with reasonable adjustment, considering the hospital level.
Consistent with most previous studies,29,30 our results demonstrated that LOS in tertiary hospitals decreased at a faster speed in the post-reform as well. A widely accepted explanation is that motivation for cost reductions and gaining surplus under per case payment system drive providers to reduce inefficient or unnecessary procedures in care provision.31 However, early discharge is also considered to make a contribution to the shortened hospital stay.32 In addition, the cost shift from inpatient to outpatient settings mentioned above could be used to explain the decreased LOS as well. Thus, the impact mechanism of this episode-based payment method on LOS needs to be further examined in the future.
Overall, the payment method by disease types with point counting showed its unique advantages in addressing the unwanted consequences of DRGs system, such as avoiding deficit for medical insurance funds and unnecessary admissions. However, no provider payment method is perfect. This new episode-based payment method is not exceptional. The unintended consequences of cost-shifting provide the policy implication of implementing multiple payment methods (eg, pay-for-performance, capitation) to compensate for the shortcomings of a single payment scheme. Simultaneously, designing an adjustment system for point counting to regulate the behaviors of tertiary hospitals in admitting patients should be taken into account as well.
Several limitations should be acknowledged. First, caution should be exercised in generalizing the empirical findings of this study, because data from only one pilot city was used. Results may be different when implementing this new episode-based payment scheme in other cities. Second, outcome variables related to healthcare quality were not included in this study because of limitations in data availability. Thus, a study that analyzes the effects of this payment reform on healthcare quality needs to be conducted in the future. Third, the longer-term effect of this new payment method needs to be investigated, although a 24-month post-intervention period was observed in our study. Fourth, the impact mechanism of this payment reform on providers’ behaviors should be further investigated to understand changes in the outcomes deeply.
Conclusion
The introduction of the payment method by disease types with point counting created a positive effect on slowing down the growth of inpatient expenditures. Still, it contributed to the increase in outpatient expenditures in China. Additionally, remarkably increased inpatients and reduced LOS in tertiary hospitals were observed with the implementation of the payment reform. The findings remind policymakers of implementing a supervision system preventing cost-shifting from inpatient to outpatient setting and incentives and restraint mechanisms regulating the behaviors of tertiary hospitals in admitting patients when expanding this innovative episode-based payment scheme to more regions.
Acknowledgments
We thank the managers in sample hospitals for their help in collecting the data.
Funding Statement
This study was supported by the Scientific Research Foundation for Scholars of HZNU (NO. 4265C50221204120), Research Fund of Hainan Medical University (NO. HYPY2020025), High-level Talents Project of Hainan Natural Science Foundation (NO. 821RC578), and Research Fund Hainan Province Clinical Medical Center (NO. QWYH202175).
Abbreviations
DRGs, diagnosis-related groups; FFS, fee-for-service; OOP, out-of-pocket; ITSA, interrupted time-series analysis; LOS, average length of stay; SD, standard deviation; GDP, gross domestic product.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of Hangzhou Normal University, and managers in sample hospitals gave their written informed consent before participating in the questionnaires.
Disclosure
The authors declare that they have no competing interests in this work.
References
- 1.Pejcic AV. Growth of global health spending share in low and middle income countries. Front Public Health. 2017;5:1–3. doi: 10.3389/fpubh.2017.00052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.China NBoSo. China Statistical Yearbook. Beijing: China Statistics Press; 2019. [Google Scholar]
- 3.Gao C, Xu F, Liu GG Payment reform and changes in health care in China. Soc Sci Med. 2014;111:10–16. doi: 10.1016/j.socscimed.2014.03.035 [DOI] [PubMed] [Google Scholar]
- 4.Zeng JQ The pilot results of 47148 cases of BJ-DRGs-based payment in China. Int J Health Plann Manage. 2019;34:1386–1398. doi: 10.1002/hpm.2818 [DOI] [PubMed] [Google Scholar]
- 5.Jian W, Lu M, Chan KY, et al. Payment reform pilot in Beijing hospitals reduced expenditures and out-of-pocket payments per admission. Health Aff. 2015;34(10):1745–1752. doi: 10.1377/hlthaff.2015.0074 [DOI] [PubMed] [Google Scholar]
- 6.Yuan S, Liu W, Wei F, et al. Impacts of hospital payment based on diagnosis related groups (DRGs) with global budget on resource use and quality of care: a case study in China. Iran J Public Health. 2019;48(2):238–246. [PMC free article] [PubMed] [Google Scholar]
- 7.Zou K, Li HY, Zhou D, Liao ZJ The effects of diagnosis-related groups payment on hospital healthcare in China: a systematic review. BMC Health Serv Res. 2020;20(1):1–11. doi: 10.1186/s12913-020-4957-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jian W, Lu M, Liu G, Chan KY, Poon AN Beijing’s diagnosis-related group payment reform pilot: impact on quality of acute myocardial infarction care. Soc Sci Med. 2019;243:112590. doi: 10.1016/j.socscimed.2019.112590 [DOI] [PubMed] [Google Scholar]
- 9.Ghazaryan E, Delarmente BA, Garber K, Gross M, Sriudomporn S, Rao KD Effectiveness of hospital payment reforms in low- and middle-income countries: a systematic review. Health Policy Plan. 2021;36:1344–1356. doi: 10.1093/heapol/czab050 [DOI] [PubMed] [Google Scholar]
- 10.Kroneman M, Nagy J. Introducing DRG-based financing in Hungary: a study into the relationship between supply of hospital beds and use of these beds under changing institutional circumstances. Health Policy. 2001;55(1):19–36. doi: 10.1016/S0168-8510(00)00118-4 [DOI] [PubMed] [Google Scholar]
- 11.Xiaozhou J. Exploration and practice of DRGs payment method in Jinhua. China Health Insur. 2021;6:42–45. [Google Scholar]
- 12.Shao N, Evaluation XY and Analysis on the DRGs payment reform in Jinhua. China Health Insur. 2018;4:41–43. [Google Scholar]
- 13.Lai Y, Fu H, Li L, Yip W Hospital response to a case-based payment scheme under regional global budget: the case of Guangzhou in China. Soc Sci Med. 2021;292:114601. doi: 10.1016/j.socscimed.2021.114601 [DOI] [PubMed] [Google Scholar]
- 14.Qian M, Zhang X, Chen Y, Xu S, Ying X. The pilot of a new patient classification-based payment system in China: the impact on costs, length of stay and quality. Soc Sci Med. 2021;289:114415. doi: 10.1016/j.socscimed.2021.114415 [DOI] [PubMed] [Google Scholar]
- 15.Mitchell KC. Understanding the financial impact of MS-DRGs. Healthc Financ Manage. 2007;61(11):56. [PubMed] [Google Scholar]
- 16.Jian WY, Lu M, Cui T, Hu M. Evaluating performance of local case-mix system by international comparison: a case study in Beijing, China. Int J Health Plann Manage. 2012;26(4):471–481. doi: 10.1002/hpm.1111 [DOI] [PubMed] [Google Scholar]
- 17.Fretheim A, Zhang F, Ross-Degnan D, et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. J Clin Epidemiol. 2015;68(3):324–333. doi: 10.1016/j.jclinepi.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 18.Shadish W, Cook T, Campbell D. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin Company; 2002. [Google Scholar]
- 19.Bureau ZS. Zhejiang Statistical Yearbook-2020. Beijing: China Statistics Press; 2020. [Google Scholar]
- 20.Lu G, Ls B, Qmc D, Xk E, Mg F, Feng LF. Effect of healthcare system reforms on public hospitals’ revenue structures: evidence from Beijing, China. Soc Sci Med. 2021;283:114210. doi: 10.1016/j.socscimed.2021.114210 [DOI] [PubMed] [Google Scholar]
- 21.Linden A, Adams JL. Applying a propensity score‐based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231–1238. doi: 10.1111/j.1365-2753.2010.01504.x [DOI] [PubMed] [Google Scholar]
- 22.Linden A. Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J. 2015;15:480–500. doi: 10.1177/1536867X1501500208 [DOI] [Google Scholar]
- 23.Zhang L, Sun L. Impacts of diagnosis-related groups payment on the healthcare providers’ behavior in China: a cross-sectional study among physicians. Risk Manag Healthc Policy. 2021;14:2263–2276. doi: 10.2147/RMHP.S308183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang J. The impact of a diagnosis-related group-based prospective payment experiment: the experience of Shanghai. Appl Econ Lett. 2010;17(18):1797–1803. doi: 10.1080/13504850903317347 [DOI] [Google Scholar]
- 25.Xu J, Jian W, Zhu K, Kwon S, Fang H. Reforming public hospital financing in China: progress and challenges. BMJ. 2019;365:l4015. doi: 10.1136/bmj.l4015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yuan B, He L, Meng Q, Jia L. Payment methods for outpatient care facilities. Cochrane Database Syst Rev. 2017;3:CD011153. doi: 10.1002/14651858.CD011153.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei Y. Catastrophic outpatient health payments and health payment-induced poverty under china’s new rural cooperative medical scheme. Appl Econ Perspect Policy. 2014;37(1):64–85. [Google Scholar]
- 28.Lang HC, Chi C, Liu CM. Impact of the case payment reimbursement method on the utilization and costs of laparoscopic cholecystectomy. Health Policy. 2004;67(2):195–206. doi: 10.1016/S0168-8510(03)00119-2 [DOI] [PubMed] [Google Scholar]
- 29.Kutz A, Gut L, Ebrahimi F, Wagner U, Schuetz P, Mueller B. Association of the Swiss diagnosis-related group reimbursement system with length of stay, mortality, and readmission rates in hospitalized adult patients. JAMA Network Open. 2019;2(2):e188332. doi: 10.1001/jamanetworkopen.2018.8332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi JW, Kim SJ, Park HK, Jang SI, Park EC. Effects of a mandatory DRG payment system in South Korea: analysis of multi-year nationwide hospital claims data. BMC Health Serv Res. 2019;19(1):776. doi: 10.1186/s12913-019-4650-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan SY, Melendez-Torres GJ. Do prospective payment systems (PPSs) lead to desirable providers’ incentives and patients’ outcomes? A systematic review of evidence from developing countries. Health Policy Plan. 2018;33(1):137–153. doi: 10.1093/heapol/czx151 [DOI] [PubMed] [Google Scholar]
- 32.Ellis RP. Creaming, skimping and dumping: provider competition on the intensive and extensive margins. J Health Econ. 1998;17(5):537–555. doi: 10.1016/S0167-6296(97)00042-8 [DOI] [PubMed] [Google Scholar]