Abstract
Purpose of Review
Femoracetabular impingement (FAI) is a common source of hip pain in children and adolescents. While nonoperative therapies and open surgical procedures can be effective, hip arthroscopy is a minimally invasive treatment option with substantial benefit. The purpose of this paper is to evaluate the current role of hip arthroscopy in treating FAI within the pediatric population. This article examines its efficacy through a review of hip arthroscopy outcomes in the contemporary orthopaedic literature.
Recent Findings
Morphologic changes in the acetabulum and proximal femur seen in FAI can be attributed to a multitude of etiologies—including idiopathic FAI, Legg-Calve-Perthes, and slipped capital femoral epiphysis. In general, arthroscopic treatment of FAI secondary to these conditions leads to statistically significant improvements in pain and patient-reported outcomes in the short and long term. In the pediatric athlete, repetitive stress on the hip perpetuates FAI and can drastically hinder performance. Hip arthroscopy allows for a high rate of return to sport with minimal morbidity in this population.
Summary
Overall, pediatric hip arthroscopy is effective in treating FAI secondary to a wide variety of conditions. Despite its clinical benefits, patients and their families should be counseled regarding alternative treatments, potential complications, and return to play.
Keywords: Hip arthroscopy, Femoroacetabular impingement, Pediatrics, Legg-Calve-Perthes, SCFE
Introduction
Femoroacetabular impingement (FAI) is a common source of hip pain in the pediatric population. Family history, secondary pediatric hip pathologies, and athletics are among the multiple etiologies for FAI in skeletally immature individuals [1–5]. Between 2000 to 2016, the incidence of FAI has risen among adolescent patients [6]. Diagnosis and treatment type are routinely made using a combination of clinical and radiographic findings. While nonoperative treatment—including activity modification, analgesics, physical therapy, corticosteroid injections—can be effective for first-line management [7–10], select patients fail these conservative measures and continue to have debilitating pain. Multiple surgical options have proven to be effective for FAI [6, 11, 12]. Among these, hip arthroscopy is a minimally invasive procedure used for reshaping the proximal femur/acetabulum as well as debridement and repair of the surrounding soft tissue. Initially described by Gross in 1977 [13], hip arthroscopy can decrease pain and preserve hip function by restoring physiologic hip morphology [2, 14, 15]. Understanding the etiology of FAI—whether idiopathic or due to secondary hip pathologies—helps provide evidence-based guidance for treatment. This paper aims to explore the contemporary understanding of pediatric patient outcomes after hip arthroscopy in the treatment of FAI.
Primary FAI
While FAI can often be attributed to a variety of conditions, primary FAI is idiopathic in nature. Repetitive flexion, internal rotation, and adduction promotes impingement and subsequent hip morphologic changes [14, 16]. These alterations manifest as CAM, pincer, or mixed lesions which lead to hip pain and limited range of motion (Fig. 1) [17]. However, hip arthroscopy is an efficacious treatment option in the short, intermediate, and long term for primary FAI.
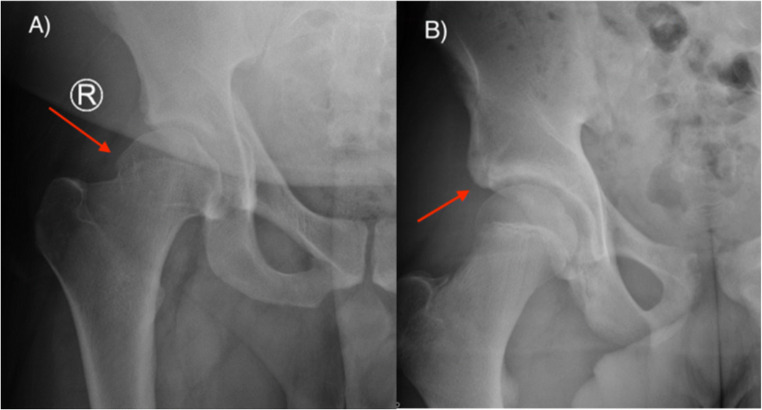
Fig. 1.
FAI radiographic findings show a CAM lesion (Photo A), Pincer lesion (Photo B), or both
Overall, post-operative short-term functional outcomes found in the literature support hip arthroscopy in the treatment of FAI. Nwachukwu et al. conducted a prospective, single-center registry study to evaluate post-arthroscopic outcomes after treating primary FAI. Of the 47 children enrolled, 91% reported greater function at one year. Also, a higher proportion of children obtained substantial clinical benefit compared to their adult countertops in the registry (53% vs 40%) [18].
Midterm outcomes suggest hip arthroscopy is a reliable tool for pain relief. Beck et al evaluated 5-year clinical outcomes and failure rates in 139 patients (age 13–21) who underwent arthroscopic treatment for FAI. Patients with previous hip surgery, acetabular dysplasia, and FAI secondary to pediatric hip disorders were excluded. Mean post-operative outcome scores were significantly higher across all metric tools (p < 0.001), and meaningful outcome thresholds were observed in 89.2% of participants. Of these patients, only 2.4% required revision arthroscopic surgery. None underwent conversion to total hip arthroplasty [19•].
With the increase in popularity of hip arthroscopy, there is growing evidence to support the long-term efficacy of this procedure. Menge et al examined 10-year hip arthroscopy outcomes in adolescent patients (mean age = 16 ± 1.2 years) with symptomatic FAI and labral tears. Again, exclusion criteria included history of hip surgery, history of hip fracture/dislocation, acetabular dysplasia, or Legg-Calve-Perthes disease (LCPD). Revision surgery was observed in 10% of patients, all of whom were female. In the non-revision cohort (mean follow-up = 12 years), statistically significant increases were observed in HOS-ADL, HOS–Sport, mHHS, and SF-12 PCS [20•].
Hip arthroscopic surgery involves eliminating points of femoral-acetabular abutment, but post-operative bone regrowth has been speculated. Perets et al followed 11 pediatric hips (10 females) after arthroscopic femoroplasty to determine if cam lesions returned. At 2 years, no radiographic evidence of bone regrowth was documented in the entire cohort.[21]
Hip arthroscopy is an effective treatment option in the sustained management of primary FAI. Future investigations into optimal timing of arthroscopic surgery to decrease conversion rates to hip osteotomy or arthroplasty may be valuable.
Legg-Calve-Perthes
LCPD is defined as aseptic necrosis of the femoral epiphysis in young children and is a common hip pain generator. Perthes commonly affects children between the ages of 4–8 years old with a five times higher incidence in males [22]. While the exact etiology is unclear, genetics, birth history, vascular disruption, and socioeconomic status are known risk factors. LCPD disease exists along a spectrum ranging from minimal femoral head involvement to total head destruction with associated acetabular changes (Fig. 2) [23–26]. Open hip osteotomy has been the favored treatment for advanced LCPD, but there is significant morbidity following these procedures [27–29]. Growing evidence supports the role of hip arthroscopy as an effective alternative treatment of FAI.
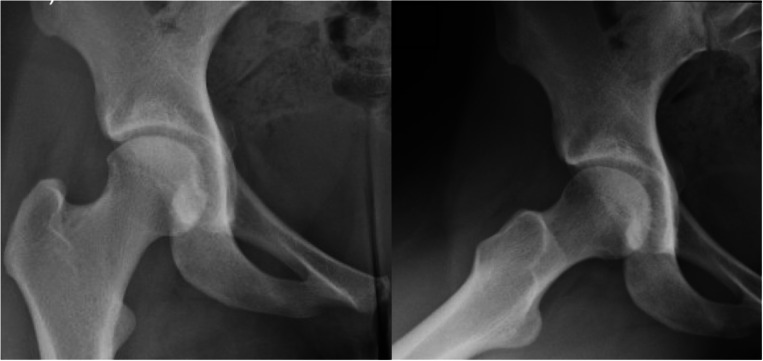
Fig. 2.
Fourteen-year-old male h/o bilateral SCFE pinning (Photos A and B) complicated by left FAI who underwent left hip arthroscopy, labral repair, and femoral osteoplasty (Photo C)
Lim et al. performed a retrospective review of functional outcomes after hip arthroscopy in 34 pediatric patients with various hip pathologies. In the LCPD subgroup, all patients reported decreased symptoms and greater function at an average follow-up of 5.2 years [30•].
One retrospective study evaluated modified Harris Hip Scores in ten patients (mean age = 12.7 years old) who underwent hip arthroscopic debridement for LCPD. Patients with advanced disease stages—as determined by the Stulberg and Waldenström classification—were not excluded. Interestingly, no significant association was demonstrated between successful outcomes and age, laterality of surgery, or stage of disease. However, a significant difference was observed between pre- and post-operative mHHS after arthroscopic treatment [31•].
Lastly, hip arthroscopy has diagnostic utility in the setting of LCPD. Current imaging modalities—such as X-ray and MRI—are useful for evaluating intaarticular pathology but can underestimate the disease process. Tiwari et al. compared the diagnostic efficacy of MRI to hip arthroscopy in LCPD. MRI was shown to have poor sensitivity with respect to labral tears (25%) and loose bodies (20%) and a low negative predictive value for synovial effusions (12%) [32]. While MRI is clinically useful in the diagnostic workup, hip arthroscopy provides optimal visualization of LCPD pathology.
Slipped Capital Femoral Epiphysis (SCFE)
SCFE is a condition which involves posteroinferior displacement of the capital femoral epiphysis on the metaphysis through the physis. Patients typically present with pain in the groin, thigh or knee and may also demonstrate a notable limp. Incidence in the USA is around 10 per 100,000, with greater risk in males, adolescents, and overweight individuals [33, 34]. As the clinical course of SCFE progresses, modification is made to the anatomy of the proximal femur which can lead to development of FAI (Fig. 3). Pediatric patients with FAI are at increased risk of hip pain, early arthrosis, and subsequent decreased range of motion through the hip joint [35]. Operative techniques used in preventing development of FAI in SCFE patients are beyond the scope of this review. The focus will be on surgical outcomes following three surgical interventions for pediatric patients with FAI secondary to SCFE: arthroscopic osteochondroplasty, open osteochondroplasty with surgical hip dislocation, and open osteotomy.
Fig. 3.
Legg-Calve-Perthes radiographic findings demonstrate femoral epiphyseal flattening and associated acetabular dysplasia
Arthroscopic osteochondroplasty has historically been successful in managing FAI in patients with mild to moderate SCFE. Chen et al. performed a retrospective study of 37 patients with FAI secondary to SCFE. Patients with mild or moderate slippage (Southwick angle <30 or 30–60 respectively) had better outcomes after arthroscopy [36]. Tscholl investigated 14 patients with mild epiphysiolysis who underwent arthroscopic osteochondroplasty with results demonstrating an overall decrease in the alpha angle postoperatively [37]. A recent study demonstrated improved hip function and decreased pain following arthroscopy even in patients with severe SCFE (Southwick angle >60) [38]. Saito performed a systematic review of 6 studies on arthroscopy for FAI secondary to SCFE showing significant improvement on Modified Harris Hip Score, improved internal rotation, and only 1 major complication out of 90 hips [39•].
Open osteochondroplasty may be necessary in cases with a greater degree of slippage as it provides a 360-degree view and facilitates surgical hip dislocation. Valenza studied 17 hips treated with open osteochondroplasty with surgical hip dislocation resulting in subjective improvement of FAI symptoms and an increase in hip mobility [40]. Two recent studies have directly compared surgical approaches for FAI secondary to SCFE. Oduwole performed a systematic review and meta-analysis of 15 studies totaling 266 hips treated with either arthroscopic osteochondroplasty, open surgical hip dislocation or open osteotomy. Hip dislocation resulted in the greatest mean alpha angle reduction followed closely by arthroscopy (41% vs 32% respectively) while arthroscopy had a significantly lower rate of complication compared to dislocation or open osteotomy (1.6% vs 10.7% vs 6.7%) [41]. A retrospective review comparing hip arthroscopy versus open surgical hip dislocation in 86 patients did not detect a difference in postoperative improvement between groups. Preoperatively, the open group had greater degree of deformity and higher rate of full thickness cartilage defects [42].
There are several areas for future research regarding secondary FAI following SCFE. Future studies may focus on long-term outcomes following the various surgical approaches as current literature investigates outcomes at less than 5 years postop. Additionally, further research to determine standardized indications for arthroscopy vs open approaches with respect to Southwick angle or other preoperative criteria may be beneficial.
Adolescent Athletes
In the USA, upwards of 60 million children are involved in recreational or competitive organized sports [43, 44]. Pediatric athletes are susceptible to developing intraarticular hip pathologies due to a multitude of factors. Type of sport can propagate changes in proximal femur and acetabular anatomy due to increased forces across the hip (Fig. 4) [4, 5]. Additionally, intensity and duration of training are known contributors to FAI development [45]. A cross-sectional study examining 214 male pediatric soccer players revealed a 30% prevalence of FAI. In this cohort, a two-fold higher rate of FAI was seen in individuals training 12.5 h or more of per wee [4]. A meta-analysis performed by Nepple et al. investigated the association between adolescent athletic participation and CAM lesion development. Compared to the control group, male athletes were found to have 1.8–8 times higher rate of CAM deformity and greater pooled prevalence rate (41% vs 17%) [46]. Lastly, early single sport specialization is associated with a higher likelihood of intraarticular pathology development in adolescent athletes [47].
Fig. 4.
Eighteen-year-old female collegiate fencer with a 6-month history of right groin pain. Right hip X-rays demonstrates a right CAM lesion with crossover sign
In adolescent athletes, hip pain attributed to FAI creates significant challenges for orthopedic surgeons. Maximizing post-operative hip function, minimizing time to return to play, and sustaining long-term hip preservation are the primary goals of treatment in this population. For these reasons, correct surgical indications are critical in returning patients to their pre-operative levels. Understanding how patients perform after hip arthroscopy will help clarify the utility of these procedures.
A single-center, retrospective review evaluated 2-year outcomes in 69 pediatric athletes (mean age 15.9) who underwent hip arthroscopy for symptomatic FAI. The most common sports included track and field, soccer, dance, baseball, and basketball. At the final timepoint, 84% had resumed competitive activity, and all patient-reported outcomes were improved compared to pre-surgical levels. However, 7.4% of patients required revision arthroscopy at roughly 3 years after index procedure [48•].
Byrd et al. investigated post-arthroscopic outcomes in adolescent athletes with symptomatic FAI. Follow-up ranged from 24 to 120 months. Using the mHHS outcome measure, 97% of patients reported improvement, and 86% returned to sport. Failure to return to play was observed in patients with comparatively lower mHHS numbers preoperatively.
Memon et al performed a systematic review that evaluated the rate of return to sport after hip arthroscopy in athletes—including pediatric, professional, collegiate, and recreational. Pediatric patients showed a 95% pooled rate of return, the highest among any group in the study [49•].
FAI can be detrimental to athletic performance and sustained participation in sport. Hip arthroscopy consistently affords pediatric athletes expedited return to play at pre-injury levels without the morbidity observed after open hip surgery. However, mild CAM deformity and lack of participation in sports are independently associated with poorer outcomes [50].
Complications
Hip arthroscopy provides a less invasive alternative with reduced morbidity compared to open hip surgery. Despite its usefulness in the treatment of FAI, there are risks associated with hip arthroscopy. These complications are likely similar to those observed in adults, but there is a paucity of studies in the pediatric population. The overall complication rate within the literature ranges from 1.3 to 4.2% [51–54]. A commonly described complication associated with hip arthroscopy is neuropraxia which can be observed in the sciatic, femoral, and obturator nerve distributions. Shelton et al. evaluated the expected neuromonitoring changes observed during pediatric hip arthroscopy and reported intraoperative SSEPs changes > 50% in approximately 80% of patients. However, clinical findings of neuropraxia or nerve injury were only observed in 19% and resolved within 1–2 days for all patients [55]. Of note, the amount of skeletal traction was not quantified in this study.
Iatrogenic femoral neck fracture is a potential consequence of hip arthroscopy. Femoral head resection involves a delicate balance between adequate lesion debridement and sufficient bone stock preservation. Excessive bone removal can perpetuate femoral neck fractures. Historically, fracture risk can be minimized by removing less than 30% of neck diameter, 5–7mm of depth, and 8–12mm of width [56]. To our knowledge, there are no recent pediatric studies that examine hip fractures secondary to hip arthroscopy, but this phenomenon is described in the adult literature. Truntzer et al. evaluated 1-year outcomes after 2,581 hip arthroscopies and determined a major and minor complication rate of 1.74% and 4.22%, respectively. In terms of proximal femur fractures, the authors reported an incidence rate of 1.08% [57]. Proposed factors that may mitigate this risk include strict adherence to post-operative weight bearing restrictions, early return to high-intensity running, and falls [58].
Lastly, while comparatively less invasive than other hip surgical treatments, hip arthroscopy for the treatment of FAI requires limitations in the post-operative period. Counseling patients and their families about expected recovery—particularly return to school—is critical. Willimon et al. investigated missed classroom time in a cohort of 206 elementary, middle, and high school children after common pediatric orthopaedic surgeries. On average, treatment of FAI with hip arthroscopy resulted in 4.8 days of missed school days which was found to be more than supracondylar fixation and isolated ACL reconstruction [59].
Hip arthroscopy is a technically challenging procedure that requires ample case volume to perform at a proficient level. Additional challenges in the pediatric population—including stage of skeletal maturity and existing hip disorders—have the potential to increase case complexity. The learning curve has been studied in the adult population [60], but there is no literature that identifies the minimum number of pediatric hip arthroscopy cases needed to attain a statistically significant decrease in complications. Future studies investigating this topic may reduce iatrogenic injury and improve outcomes.
Conclusion
FAI—both idiopathic and secondary—exists as a challenging musculoskeletal condition within the pediatric population. Hip arthroscopy is a useful, minimally invasive treatment option for patients who have exhausted nonoperative modalities. However, appropriate patient selection and discussions with families are crucial for optimizing patient outcomes in children and adolescents.
Declarations
Conflict of Interest
Bejan Alvandi, Steven Dayton, Matthew Hartwell, Erik Gerlach, Peter Swiatek, John Carney, and Vehniah Tjong declare that they have no relevant conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on HIP/FAI
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bejan A. Alvandi, Email: bejan.alvandi@northwestern.edu
Steven R. Dayton, Email: steven.dayton@northwestern.edu
Matthew J. Hartwell, Email: matthew.hartwell@northwestern.edu
Erik B. Gerlach, Email: erik.gerlach@gmail.com
Peter R. Swiatek, Email: peter.swiatek@northwestern.edu
John J. Carney, Email: john.carney@northwestern.edu
Vehniah K. Tjong, Email: vtjong@gmail.com
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Sheppard ED, Read CR, Wills BW, Reed Estes A. Femoroacetabular impingement in pediatric patients. Pediatr Rev. Published Online First: 2019. 10.1542/pir.2017-0137. [DOI] [PubMed]
- 2.Pathy R, Sink EL. Femoroacetabular impingement in children and adolescents. Curr Opin Pediatr. 2016. 10.1097/MOP.0000000000000301. [DOI] [PubMed]
- 3.Pollard TCB, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, Carr AJ. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Jt Surg Ser B. Published Online First: 2010. 10.1302/0301-620X.92B2.22850. [DOI] [PubMed]
- 4.Polat G, Arzu U, Dinç E, Bayraktar B. Prevalence of femoroacetabular impingement and effect of training frequency on aetiology in paediatric football players. HIP Int. Published Online First: 2019. 10.1177/1120700018781939. [DOI] [PubMed]
- 5.Polat G, Arzu U, Dinç E, Bayraktar B. Etiological importance of training frequency, age and prevalance of Femoroacetabular İmpingement(FAİ) in pediatric male athletes. Orthop J Sport Med. Published Online First: 2017. 10.1177/2325967117s00067.
- 6.Hale RF, Melugin HP, Zhou J, LaPrade M, Bernard C, Leland D, Levy BA, Krych AJ. Incidence of femoroacetabular impingement and surgical management trends over time. Am J Sports Med. Published Online First: 2021. 10.1177/0363546520970914. [DOI] [PMC free article] [PubMed]
- 7.Pennock AT, Bomar JD, Johnson KP, Randich K, Upasani VV. Nonoperative Management of femoroacetabular impingement: a prospective study. Am J Sports Med. Published Online First: 2018. 10.1177/0363546518804805. [DOI] [PubMed]
- 8.Wright AA, Hegedus EJ, Taylor JB, Dischiavi SL, Stubbs AJ. Non-operative management of femoroacetabular impingement: a prospective, randomized controlled clinical trial pilot study. J Sci Med Sport. Published Online First: 2016. 10.1016/j.jsams.2015.11.008. [DOI] [PubMed]
- 9.Egger AC, Frangiamore S, Rosneck J. Femoroacetabular impingement: a review. Sports Med Arthrosc. 2016. 10.1097/JSA.0000000000000126. [DOI] [PubMed]
- 10.Byrd JWT. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med. Published Online First: 2014. 10.1177/0363546513499136. [DOI] [PubMed]
- 11.Kuhns BD, Weber AE, Levy DM, Wuerz TH. The natural history of femoroacetabular impingement. Front Surg. 2015. 10.3389/fsurg.2015.00058. [DOI] [PMC free article] [PubMed]
- 12.Clohisy JC, Nepple JJ, Ross JR, Pashos G, Schoenecker PL. Does surgical hip dislocation and periacetabular osteotomy improve pain in patients with perthes-like deformities and acetabular dysplasia? Clin Orthop Relat Res. Published Online First: 2015. 10.1007/s11999-014-4115-7. [DOI] [PMC free article] [PubMed]
- 13.Gross R. Arthroscopy in hip disorders in children. Ortho Rev. 1977;6:43–49. [Google Scholar]
- 14.Hanke MS, Schmaranzer F, Steppacher SD, Lerch TD, Siebenrock KA. Hip preservation. EFORT Open Rev. Published Online First: 2020. 10.1302/2058-5241.5.190074. [DOI] [PMC free article] [PubMed]
- 15.Carsen S, Tourn D, Marien M, Smit K. Arthroscopy of the pediatric hip. Ann Jt. Published Online First: 2018. 10.21037/aoj.2018.06.01.
- 16.Trigg SD, Schroeder JD, Hulsopple C. Femoroacetabular impingement syndrome. Curr Sports Med Rep. Published Online First: 2020. 10.1249/JSR.0000000000000748. [DOI] [PubMed]
- 17.Fernquest S, Arnold C, Palmer A, Broomfield J, Denton J, Taylor A, Glyn-Jones S. Osseous impingement occurs early in flexion in cam-type femoroacetabular impingement. Bone Jt J. Published Online First: 2017. 10.1302/0301-620X.99B4.BJJ-2016-1274.R1. [DOI] [PubMed]
- 18.Nwachukwu BU, Chang B, Kahlenberg CA, Fields KG, Nawabi DH, Kelly BT, Ranawat AS. Does hip arthroscopy provide meaningful outcome improvement for adolescent femoroacetabular impingement. Orthop J Sport Med. Published Online First: 2017. 10.1177/2325967117s00112. [DOI] [PubMed]
- 19.• Beck EC, Nwachuckwu BU, Jan K, Nho SJ. Hip arthroscopy for femoroacetabular impingement syndrome in adolescents provides clinically significant outcome benefit at minimum 5-year follow-up. Arthrosc J Arthrosc Relat Surg. Published Online First: 2021. 10.1016/j.arthro.2020.12.188. Evaluates 5-year patient reported outcomes after hip arthroscopy for FAI with clinically significant improvement achieved in 89.2% of patients. [DOI] [PubMed]
- 20.• Menge TJ, Briggs KK, Rahl MD, Philippon MJ. Hip arthroscopy for femoroacetabular impingement in adolescents: 10-year patient-reported outcomes. Am J Sports Med. Published Online First: 2021. 10.1177/0363546520973977. Prospective study showing successfull 10-year outcomes in adolescents after hip arthroscopy with only a 10% revision rate. [DOI] [PubMed]
- 21.Perets I, Gupta A, Chaharbakhshi EO, Ashberg L, Hartigan DE, Close MR, Domb BG. Does bony regrowth occur after arthroscopic femoroplasty in a group of young adolescents? Arthrosc - J Arthrosc Relat Surg. Published Online First: 2017. 10.1016/j.arthro.2017.01.023. [DOI] [PubMed]
- 22.Pavone V, Chisari E, Vescio A, Lizzio C, Sessa G, Testa G. Aetiology of Legg-Calvé-Perthes disease: a systematic review. World J. Orthop. 2019. 10.5312/wjo.v10.i3.145. [DOI] [PMC free article] [PubMed]
- 23.Rampal V, Clément JL, Solla F. Legg-Calvé-Perthes disease: classifications and prognostic factors. Clin Cases Miner Bone Metab. 2017. 10.11138/ccmbm/2017.14.1.074. [DOI] [PMC free article] [PubMed]
- 24.Shah H. Perthes disease. Evaluation and management. Orthop Clin North Am. 2014. 10.1016/j.ocl.2013.08.005. [DOI] [PubMed]
- 25.Ibrahim T, Little DG. The pathogenesis and treatment of Legg-Calvé-Perthes disease. JBJS Rev. 2016;4. 10.2106/JBJS.RVW.15.00063. [DOI] [PubMed]
- 26.Divi SN, Bielski RJ. Legg-Calvé-Perthes disease. Pediatr Ann. Published Online First: 2016. 10.3928/00904481-20160310-03. [DOI] [PubMed]
- 27.Sucato DJ. Role of femoral head surgery in skeletally mature perthes disease. J Pediatr Orthop. Published Online First: 2013. 10.1097/BPO.0b013e318295e86b. [DOI] [PubMed]
- 28.Matsubayashi S, Chiba K, Tsujimoto R, Osaki M, Wada A. Femoral osteotomy to improve range of motion in residual deformity of perthes disease: a case report. Ann Med Surg. Published Online First: 2020. 10.1016/j.amsu.2020.04.031. [DOI] [PMC free article] [PubMed]
- 29.Citlak A. Long-term follow-up results of femoral varus osteotomy in the treatment of Perthes disease, and comparison of open-wedge and closed-wedge osteotomy techniques: A retrospective observational study. Med (United States). Published Online First: 2020. 10.1097/MD.0000000000019041. [DOI] [PMC free article] [PubMed]
- 30.• Lim C, Cho TJ, Shin CH, Choi IH, Yoo WJ. Functional outcomes of hip arthroscopy for pediatric and adolescent hip disorders. CiOS Clin Orthop Surg. Published Online First: 2020. 10.4055/cios.2020.12.1.94. Highlights the efficacy and saftey profile of hip arthroscopy in the treatment of multiple pediatric hip conditions. [DOI] [PMC free article] [PubMed]
- 31.• Kanatli U, Ayanoglu T, Ozer M, Ataoglu MB, Cetinkaya M. Hip arthroscopy for Legg-Calvè-Perthes disease in paediatric population. Acta Orthop Traumatol Turc. Published Online First: 2019. 10.1016/j.aott.2019.03.005*. Retrospective study showing improved pre- to post-operative outcomes after arthroscopic treatment of LCP (no difference with age, side, and the stage of the disease). [DOI] [PMC free article] [PubMed]
- 32.Tiwari V, Gamanagatti S, Mittal R, Nag H, Khan SA. Correlation between MRI and hip arthroscopy in children with Legg–Calve–Perthes disease. Musculoskelet Surg. Published Online First: 2018. 10.1007/s12306-017-0513-9. [DOI] [PubMed]
- 33.Aronsson DD, Loder RT, Breur GJ, Weinstein SL. Slipped capital femoral epiphysis: Current concepts. J Am Acad Orthop Surg. 2006. 10.5435/00124635-200611000-00010. [DOI] [PubMed]
- 34.Soni JF, Valenza WR, Uliana CS. Surgical treatment of femoroacetabular impingement after slipped capital femoral epiphysis. Curr Opin Pediatr. 2018. 10.1097/MOP.0000000000000565. [DOI] [PubMed]
- 35.Moretti B, Notarnicola A, Garofalo R, Moretti L, Patella S, Marlinghaus E, Patella V. Shock waves in the treatment of stress fractures. Ultrasound Med Biol. Published Online First: 2009. 10.1016/j.ultrasmedbio.2008.12.002. [DOI] [PubMed]
- 36.Chen A, Youderian A, Watkins S, Gourineni P. Arthroscopic femoral neck osteoplasty in slipped capital femoral epiphysis. Arthrosc J Arthrosc Relat Surg. Published Online First: 2014. 10.1016/j.arthro.2014.05.024. [DOI] [PubMed]
- 37.Tscholl PM, Zingg PO, Dora C, Frey E, Dierauer S, Ramseier LE. Arthroscopic osteochondroplasty in patients with mild slipped capital femoral epiphysis after in situ fixation. J Child Orthop. Published Online First: 2016. 10.1007/s11832-015-0707-3. [DOI] [PMC free article] [PubMed]
- 38.Basheer SZ, Cooper AP, Maheshwari R, Balakumar B, Madan S. Arthroscopic treatment of femoroacetabular impingement following slipped capital femoral epiphysis. Bone Jt J. Published Online First: 2016. 10.1302/0301-620X.98B1.35831. [DOI] [PubMed]
- 39.• Saito M, Kuroda Y, Sunil Kumar KH, Khanduja V. Outcomes after arthroscopic osteochondroplasty for femoroacetabular impingement secondary to slipped capital femoral epiphysis: a systematic review. Arthrosc J Arthrosc Relat Surg. 2021. 10.1016/j.arthro.2020.12.213. Systematic review examining six studies that evaluated short- and medium-term SCFE outcomes after arthroscopy. [DOI] [PubMed]
- 40.Valenza WR, Soni JF, Uliana CS, Faria FF, Schelle GC, Sugisawa DS. Surgical treatment of femoroacetabular impingement using controlled hip dislocation after occurrence of slipped capital femoral epiphysis. Rev Bras Ortop (English Ed. Published Online First: 2016. 10.1016/j.rboe.2015.10.013. [DOI] [PMC free article] [PubMed]
- 41.Oduwole KO, De Sa D, Kay J, et al. Surgical treatment of femoroacetabular impingement following slipped capital femoral epiphysis: a systematic review. Bone Jt Res. Published Online First: 2017. 10.1302/2046-3758.68.BJR-2017-0018.R1. [DOI] [PMC free article] [PubMed]
- 42.Wylie JD, McClincy MP, Uppal N, et al. Surgical treatment of symptomatic post-slipped capital femoral epiphysis deformity: a comparative study between hip arthroscopy and surgical hip dislocation with or without intertrochanteric osteotomy. J Child Orthop. Published Online First: 2020. 10.1302/1863-2548.14.190194. [DOI] [PMC free article] [PubMed]
- 43.Popkin CA, Bayomy AF, Ahmad CS. Early sport specialization. J Am Acad Orthop Surg. 2019. 10.5435/JAAOS-D-18-00187. [DOI] [PubMed]
- 44.Matzkin E, Garvey K. Youth sports specialization: does practice make perfect? NASN Sch Nurse. Published Online First: 2019. 10.1177/1942602X18814619. [DOI] [PubMed]
- 45.de Silva V, Swain M, Broderick C, McKay D. Does high level youth sports participation increase the risk of femoroacetabular impingement? A review of the current literature. Pediatr Rheumatol. 2016. 10.1186/s12969-016-0077-5. [DOI] [PMC free article] [PubMed]
- 46.Nepple JJ, Vigdorchik JM, Clohisy JC. What is the association between sports participation and the development of proximal femoral cam deformity? Am J Sports Med. Published Online First: 2015. 10.1177/0363546514563909. [DOI] [PubMed]
- 47.McGovern RP, Kivlan BR, Christoforetti JJ, et al. Risk of intra-articular hip injury in adolescent athletes: a five-year multicentre cohort study. Int Orthop. Published Online First: 2020. 10.1007/s00264-020-04598-7. [DOI] [PubMed]
- 48.• Litrenta J, Mu BH, Ortiz-Declet V, Chen AW, Perets I, Wojnowski NM, Domb BG. Hip arthroscopy successfully treats femoroacetabular impingement in adolescent athletes. J Pediatr Orthop. Published Online First: 2020. 10.1097/BPO.0000000000001411. Retrospective review showing acceptable complication, limited reoperation, and faster return to sport rates in adolescent athletes treated with hip arthroscopy at two-year follow-up.
- 49.• Memon M, Kay J, Hache P, Simunovic N, Harris JD, O’Donnell J, Ayeni OR. Athletes experience a high rate of return to sport following hip arthroscopy. Knee Surg Sport Traumatol Arthrosc 2019. 10.1007/s00167-018-4929-z. Systematic review showing high return to play rates and improved pain/functional outcomes in athletes post-FAI arthroscopic surgery. [DOI] [PubMed]
- 50.Nepple JJ, Yen Y-M, Zaltz I, et al. FAI surgery in the adolescent population: mild deformities and lack of sports participation are associated with an increased risk of treatment failure. Orthop J Sport Med. Published Online First: 2019. 10.1177/2325967119s00019.
- 51.Nwachukwu BU, McFeely ED, Nasreddine AY, Krcik JA, Frank J, Kocher MS. Complications of hip arthroscopy in children and adolescents. J Pediatr Orthop. Published Online First: 2011. 10.1097/BPO.0b013e31820cadc5. [DOI] [PubMed]
- 52.Cvetanovich GL, Chalmers PN, Levy DM, Mather RC, Harris JD, Bush-Joseph CA, Nho SJ. Hip arthroscopy surgical volume trends and 30-day postoperative complications. arthrosc J Arthrosc Relat Surg. Published Online First: 2016. 10.1016/j.arthro.2016.01.042. [DOI] [PubMed]
- 53.Niroopan G, De Sa D, MacDonald A, Burrow S, Larson CM, Ayeni OR. Hip Arthroscopy in trauma: a systematic review of indications, efficacy, and complications. Arthrosc J Arthrosc Relat Surg. 2016. 10.1016/j.arthro.2015.12.029. [DOI] [PubMed]
- 54.De Sa D, Stephens K, Parmar D, Simunovic N, Philippon MJ, Karlsson J, Ayeni OR. A comparison of supine and lateral decubitus Positions for hip arthroscopy: a systematic review of outcomes and complications. Arthrosc J Arthrosc Relat Surg. 2016. 10.1016/j.arthro.2015.12.028. [DOI] [PubMed]
- 55.Shelton TJ, Patel A, Agatstein L, Haus BM. What neuromonitoring changes can be expected during hip arthroscopy in the pediatric population? Am J Sports Med. Published Online First: 2020. 10.1177/0363546519889038. [DOI] [PubMed]
- 56.Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. J Bone Jt Surg Ser A. Published Online First: 2005. 10.2106/JBJS.D.01793. [DOI] [PubMed]
- 57.Truntzer JN, Hoppe DJ, Shapiro LM, Abrams GD, Safran M. Complication rates for hip arthroscopy are underestimated: a population-based study. Arthrosc J Arthrosc Relat Surg. Published Online First: 2017. 10.1016/j.arthro.2017.01.021. [DOI] [PubMed]
- 58.Horner NS, Vikas K, MacDonald AE, Naendrup J-H, Simunovic N, Ayeni OR. Femoral neck fractures as a complication of hip arthroscopy: a systematic review. J Hip Preserv Surg. Published Online First: 2017. 10.1093/jhps/hnw048. [DOI] [PMC free article] [PubMed]
- 59.Willimon SC, Johnson MM, Herzog MM, Busch MT. Time to return to school after 10 common orthopaedic surgeries among children and adolescents. J Pediatr Orthop. Published Online First: 2019. 10.1097/BPO.0000000000000947. [DOI] [PubMed]
- 60.Schüttler KF, Schramm R, El-Zayat BF, Schofer MD, Efe T, Heyse TJ. The effect of surgeon’s learning curve: complications and outcome after hip arthroscopy. Arch Orthop Trauma Surg. Published Online First: 2018. 10.1007/s00402-018-2960-7. [DOI] [PubMed]