Abstract
Purpose of Review
Cross-discipline fitness, or CrossFit, has exploded in popularity during the last two decades. During this time, there have been a high volume of patients presenting to clinicians with a wide range of associated injuries. Given the high intensity, high repetition, and competitive nature of CrossFit training and competition, athletes are vulnerable to injury, particularly upper extremity injury. The rate of injury to the shoulder, elbow, and wrist in CrossFit is higher when compared to traditional weight-training and more comparable to elite-level gymnastics and Olympic-style lifting. Due to the growing popularity of CrossFit-style exercise and the relatively high rate of injury among its participants, clinicians are likely to encounter these athletes. The purpose of this review is to familiarize clinicians with CrossFit and the associated injuries they will likely encounter.
Recent Findings
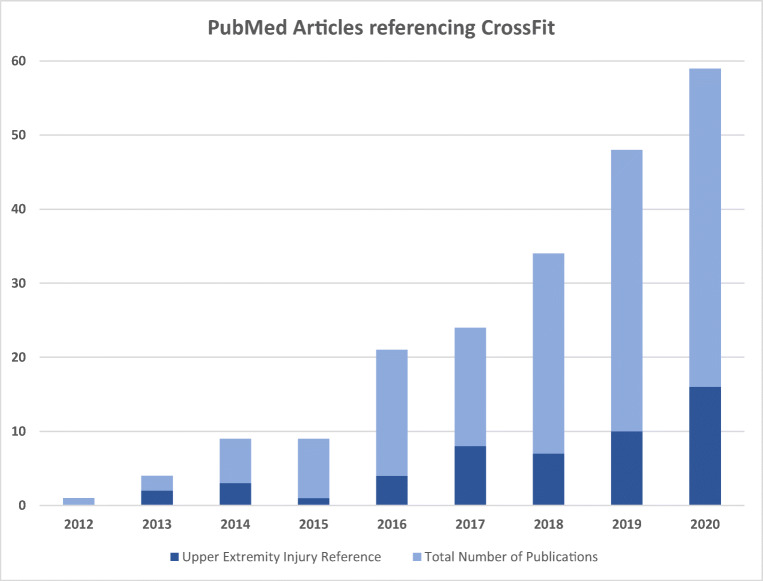
The medical literature focusing on CrossFit has demonstrated exponential growth, with the first article published in 2012 and 59 articles published in 2020. Although the body of literature is growing, there are no high-level studies focusing on CrossFit. The literature mainly consists of level IV and V studies, primarily consisting of case reports and case series. Recent studies have proven that CrossFit athletes are vulnerable to high rates of upper extremity injury and a few studies have identified risk factors for injury. Future high-level research is required to study modifiable risk factors, diagnostic criteria, and treatment options for these high-risk athletes in order to improve the safety of their sport.
Summary
The CrossFit body of research is limited to level IV and V studies; however, the literature is clear, CrossFit athletes face a high rate of upper extremity injury. For this reason, clinicians must be familiar with CrossFit and its associated pathology. The goal of this review is to familiarize clinicians with CrossFit and the associated pathologies they will likely encounter.
Keywords: CrossFit, Injury, Exercise, Shoulder, Elbow, Wrist
Introduction
Cross-discipline fitness, or CrossFit (XF), is a form of high-intensity interval training that includes functional exercises from various disciplines including Olympic-style weightlifting, powerlifting, and gymnastics, among others. CrossFit Inc. was founded as an incorporation for cross-discipline fitness in 2000. According to information from CrossFit Inc. and a 2016 CNBC report, XF grew from 13 affiliate gyms in 2005 to over 15,000 affiliate gyms in 158 countries worldwide today [1]. In 2018 the CrossFit Inc. Open Competition had over 415,000 participants. During this time, the medical literature focusing on XF has also demonstrated exponential growth, expanding from the first article in 2012 to 59 articles published in 2020 (Fig. 1). Some articles focus on nutrition, metabolic function, training physiology, or physical performance, but many of the articles focus on injuries. XF’s relationship to injury has been recognized by the mainstream press and media as well. Concerns regarding the high rate of injury in XF have been highlighted in “Is CrossFit Killing Us?” Outside Magazine, “Does CrossFit Have a Future?” The New Yorker, and “Lift, Squat, Repeat: Inside the CrossFit Cult” TIME [2–4]. Although case series and case reports have described many different injuries, the literature has consistently shown that XF athletes are at highest risk for upper extremity injury [5, 6, 7, 8, 9•, 10, 11, 12••, 13, 14•, 15, 16•, 17, 18, 19]. Due to XF’s worldwide popularity and propensity for injury, every clinician who provides musculoskeletal care should be familiar with XF and its associated patterns of pathology. The purpose of this article is to review the literature published on XF injuries and provide clinicians with an up-to-date discussion on associated upper extremity injuries.
Fig. 1.
Literature review of articles referencing XF and upper extremity XF injuries
Injury Overview
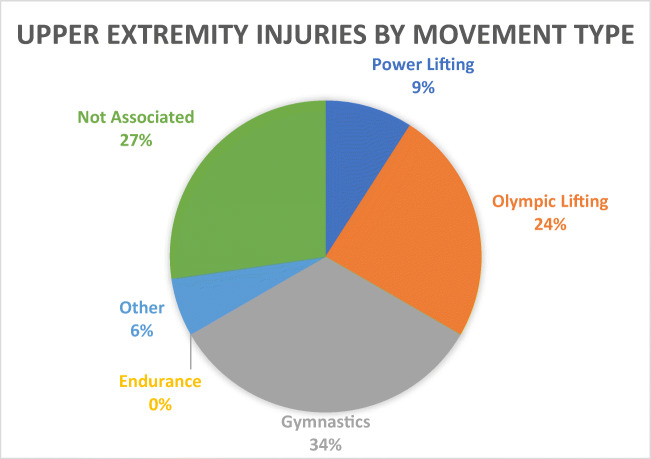
The overall injury rate of athletes participating in XF has been reported from 0.2 to 18.9 injuries per 1000 h of training [9•, 20]. When compared to traditional weightlifting, athletes participating in XF routines have been estimated to suffer 1.3 times more injuries and seek medical attention 1.86 times more often [14•]. Many of the athletes are diagnosed with conditions that can be managed non-operatively; however, approximately 2.6 to 7.0% of all presenting XF injuries require surgery [20, 21]. Risk factors for injury have been identified and include improper form, previous injury, beginner participants with less than 6 months of experience, advanced level participants with over 3 years of experience, over 11 h per week of training, and repetitive activities leading to overuse injuries [5, 13, 22] (Fig. 2). Alekseyev et al. studied all injury types and determined that squats, deadlifts, clean and jerk, and press were the exercises that accounted for the most injuries in their 885 participant cohort [13]. Weisenthal and colleagues surveyed 486 CrossFit participants and reported injuries according to body region and movement type. There were 84 reported injuries and 33 involved the upper extremity, of which most injuries were caused by gymnastic exercises and Olympic-style lifts [8] (Fig. 3).
Fig. 2.
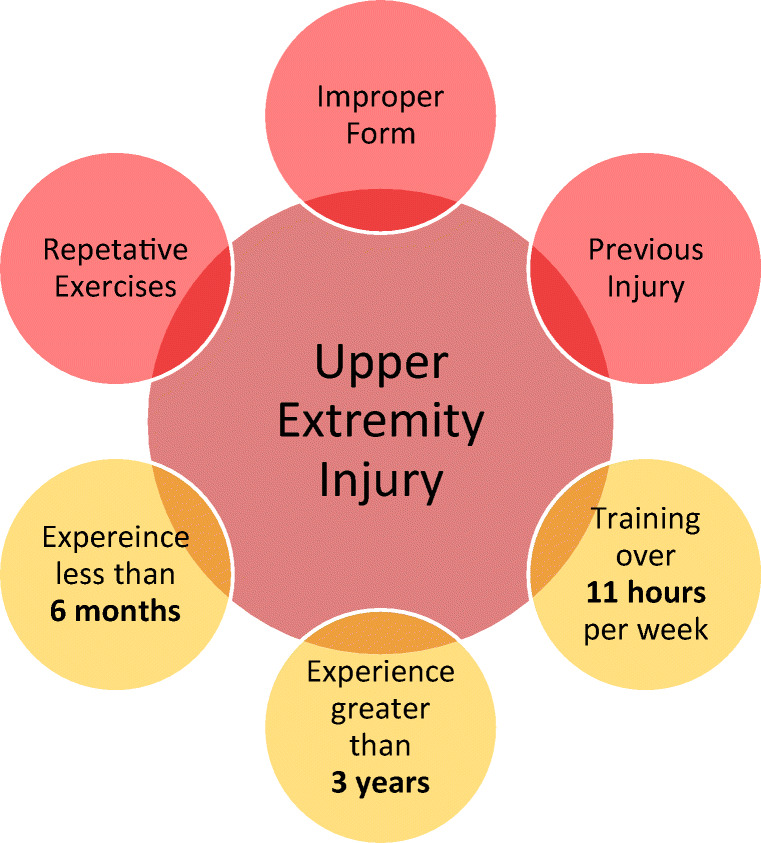
Diagram of risk factors proven to be associated with an increased risk for upper extremity injury
Fig. 3.
Weisenthal et al. surveyed 486 CrossFit participants and reported injuries according to body region and movement type. There were 84 reported injuries and 33 involved the upper extremity. This pie chart demonstrates the proportion of upper extremity injuries by movement type [8]
Shoulder Injuries
Demographics
Shoulder-specific injuries have been estimated to occur at a rate of 1.94 injuries per 1000 h of XF training [22]. Among all injury types, the shoulder has the largest body of literature and has been repeatedly shown to be the most vulnerable joint during XF training and competition, representing 19–39% of all reported injuries [5, 8, 9•, 12••, 13, 16•, 17, 20, 21]. Although the proportion of injuries involving the shoulder is high among XF athletes, the proportion is high for other related sports. Shoulder injuries make up 49% of gymnastics and 51% of traditional weightlifting injuries [22]. Male XF athletes have been shown to have a 2.8 times higher rate of shoulder injuries when compared to female athletes [23•]. Of the high-risk exercises that account for the most injuries during XF exercise, the Olympic-style lifts and gymnastic-style exercises place high loads on the shoulder through a wide range of motion. According to a survey of 187 XF athletes conducted by Summitt et al., 44 athletes (23.5%) reported 51 previous shoulder injuries. The most common exercises that lead to injury were overhead presses (n=13, 25%), snatches (n=10, 20%), and Kipping pull-ups (n=5, 10%) [22]. There is no granular data on the specific injury mechanism for each of these exercises; however, it is our authors’ opinion that these shoulder injuries are the result of three main conditions: eccentric loading, impingement, and extraphysiologic motion.
Eccentric Loading
Eccentric loading is a common cause for injury to muscle tendon units. The possibility of eccentrically loading a muscle to failure is possible during any exercise; however, many of the motions utilized in Olympic lifts such as clean and jerk, press and snatches, and the gymnastic moves including pull-ups and muscle-ups utilize momentum to generate enough force to complete the exercise. When combined with high repetitions, fatigue, and poor form, the high load, dynamic movement, and momentum generated in the glenohumeral joint during these exercises makes the muscle tendon units around the shoulder vulnerable to injury.
Impingement
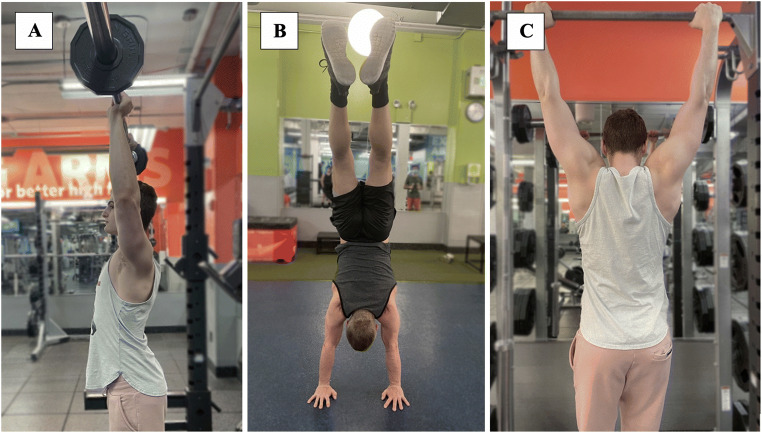
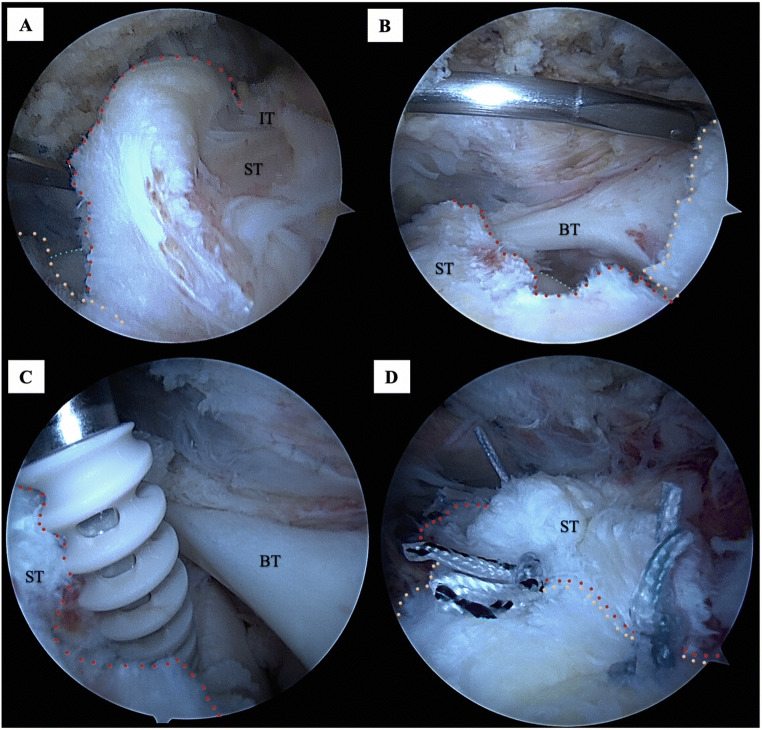
Both internal and external impingement of the shoulder are a concern in many XF exercises. Internal impingement of the shoulder in a position of maximum arm abduction and external rotation leads to pathologic contact between the posterior superior glenoid and the greater tuberosity at the articular side of the supraspinatus tendon insertion. This injury mechanism leads to partial articular-sided posterior rotator cuff tears, posterosuperior labral tears, and scarring of the posterior capsule. Historically this injury pattern was seen in the setting of throwing and overhead athletes. But certain gymnastic-type movements, especially the Kipping pull-up, put the athlete at high risk for this injury pattern by loading the shoulder in a high degree of abduction and external rotation (Fig. 4). The at-risk position for external impingement, specifically subacromial impingement, is more widespread in XF exercises. Olympic lifts such as jerk press, overhead press and snatch, and gymnastic moves including pull-ups, muscle-ups, handstands, handstand pushups, and handstand walks all load the shoulder in an arm overhead position (Fig. 5). Loading the arm in this position predisposes athletes to subacromial bursitis as well as rotator cuff tendinitis and tendinopathy including partial- and full-thickness tears. When these high-risk exercises are performed using proper technique, injury risk from impingement can be mitigated. Prinold et al. studied glenohumeral, scapulothoracic, and humerothoracic kinematics during pull-ups using various hand positions. In their observational study of eleven participants, wide hand grip and reversed hand grip (palms facing body) lead to kinematic patterns that increased the risk for impingement (Fig. 6). Their study suggested that a forward grip (palms away from body) at shoulder width provide the most favorable kinematics and decreased the potential for rotator cuff injury through subacromial impingement [24]. Anecdotally, the authors have recognized unusual rotator cuff tendon tear patterns associated with XF. Generally, attritional and traumatic rotator cuff tears occur laterally at the tendon’s insertion on the greater tuberosity. However, during XF when heavy loads are placed in the shoulder in an impingement position, more unusual tear patterns can develop. Millet et al. classified types of rotator cuff tears that occur near the muscle tendon junction as the result of either the failure of a previous repair or from acute trauma [25]. Figure 7 demonstrates the arthroscopic photos of a 49-year-old XF athlete who presented after developing pain after performing dip exercises in deep shoulder extension and abduction. She was diagnosed with a full-thickness rotator cuff tear based on physical exam and MRI, she failed conservative management, and she was ultimately indicated for an arthroscopic repair. This patient demonstrates an unusual tear pattern consistent with a Millet-type IA tear pattern [25] caused by the trauma from the repetitive impingement of her XF exercise regimen.
Fig. 4.

Kipping pull-up demonstrating shoulder abduction and external rotation
Fig. 5.
Sources of shoulder impingement: A finishing position for jerk press, overhead press, and snatch; B handstand position; C starting position for pull-ups and muscle-ups
Fig. 6.
Hand position variation during pull-ups: A forward hand grip (palms away from body); B wide hand grip; C reversed hand grip (palms facing body)
Fig. 7.
Arthroscopic photos of the subacromial space in the lateral decubitus position demonstrating full-thickness supraspinatus tendon (ST) and infraspinatus tendon (IT) tears with a large lateral intact tendon stump (yellow tracing) on the greater tuberosity footprint but an adequate amount of medial tendon (red tracing) at the muscle tendon junction for suture repair, consistent with a type IA tear pattern as classified by Millet et al. [25]. A View of the full-thickness ST and IT tears and the underlying articular cartilage of the humerus (blue tracing) through the anterior portal. B View of the full-thickness ST tear and the biceps tendon (BT) through the posterior portal. C Suture anchors placed in the great tuberosity for ST repair. D Repair of the tendon achieved with 3 suture anchors, demonstrating the large lateral tendon stump (yellow tracing) still intact on the tuberosity
Extraphysiologic Motion
Extraphysiologic motion is the third factor that contributes to XF’s high shoulder injury rate. The glenohumeral joint’s relatively incongruent architecture affords it a large range of motion, but also predisposes the shoulder joint to instability. The glenohumeral joint relies on the labrum, rotator cuff, and other surrounding musculature to keep the humeral head centered on the glenoid. Extraphysiologic motion in the shoulder joint ranges from microinstability which may lead to chondral and labral damage over time, to subluxations which can cause the same damage and lead to apprehension in the athletes, to dislocations which are the most extreme form. An acute shoulder dislocation can lead to glenoid fractures, tuberosity fractures, rotator cuff tears, and nerve palsies, and recurrent dislocations can lead to bone loss, chronic instability, chondral wear, and eventually dislocation arthropathy. Many of the gymnastic- and Olympic-style lifts in XF have the potential to cause extraphysiologic motion, but exercises with heavy load that use momentum to carry the arm into abduction and external rotation are the highest risk. The jerk press, snatches, pull-ups, muscle-ups, handstands, handstand pushups, and handstand walks all place the shoulder at risk for injury due to the high loads they place on the shoulder beyond the normal arc of motion.
Treatment
Few studies have focused on treatment for the common shoulder pathologies seen in XF athletes. Overall, most XF injuries can be managed non-operatively, with 93–97.4% not requiring surgery [20, 21]. For the athletes that do require surgery, rotator cuff tears are a common indication. Carbone et al. studied the return rate of XF athletes after arthroscopic rotator cuff repairs [26••]. At the time of arthroscopy, concomitant acromioplasty (79%), biceps tenodesis (64.7%), and acromioclavicular joint coplaning or resection (52%) were performed. At 2-year follow-up, their 22-patient cohort had a 100% return to sport rate, and they returned at a median 8.7 ± 3.4 months. The athletes’ average constant scores, American Shoulder and Elbow Surgeons score, and visual analog scale scores improved significantly from preoperatively to final follow-up. Ultrasound evaluation performed after 2 years demonstrated a 78% healing rate. Of the 5 patients with incomplete healing, two had lower patient-reported outcomes at follow-up. Of all the patients who underwent surgery, 59% reported they were able to return to a higher level of fitness and only 9% reported returning to a lower level a 2-year follow-up [26••]. Another study by Carbone and colleagues demonstrated a 100% rate of return to XF after an arthroscopic suprapectoral biceps tenodesis when it was performed in addition to a supraspinatus repair [27••]. These case series give clinicians some literature to cite when counseling patients on return to XF after rotator cuff repair. However, additional higher-level studies are needed to determine proper indications, surgical techniques, and postoperative rehab protocols for this unique group of athletes.
Prevention
In the survey conducted by Summitt et al., among the 44 shoulder injuries, the most common attributable causes were improper form (33.3% of all injuries) or an exacerbation of a previous injury (33.3% of all injuries) [22]. Participants should therefore ensure they take the time to learn the proper technique for each exercise and take the time to fully recover from injuries. Athletes must focus on maintaining good form as they become fatigued. Given the high intensity, high repetition, and competitive nature of XF training and competition, fatigue leaves athletes vulnerable to shoulder injuries through improper form. Athletes and trainers are encouraged to stop an exercise set once fatigue leads to compromised form, and athletes are always encouraged to seek an evaluation by a medical professional if they are unable to tolerate return to exercise.
Elbow Injuries
Elbow injuries are estimated to be the 3rd to 5th most common injury sustained during XF, representing 1.3 to 12% of all injuries sustained [5, 8, 16•, 20, 21, 28]. The overall rate of injury is similar when compared to other weight training disciplines, including Olympic lifting (3–10%), power lifting (8–28%), strongman (6%), and the highland games (14%) [19]. The most commonly reported elbow injuries are tendinitis and epicondylitis; however, there are also reports of distal biceps ruptures, elbow dislocations, and rhabdomyolysis-induced upper extremity compartment syndrome [23•, 29].
Elbow injuries are typically sustained during Olympic-style lifting and gymnastics activities, which may be due to the high loads these exercises place on the elbow at the extremes of motion [18]. Exercises like the snatch, which is a central component of Olympic lifting and frequent XF element, places additional stress on the upper extremity due to the need for wide grip and elbow hyperextension [30]. Significant differences in elbow injury rates and patterns between genders and ages have not been detected; however, this may be due to low sample size [20, 23•].
Wrist Injuries
Wrist and hand injuries represent the 3rd to 7th most common site of injury sustained among XF participants [5, 6, 16•, 20, 28, 31, 32]. The overall percentages of injuries varied from 3.4 to 20.4%, depending on the definition of injury and whether they were diagnosed by a medical professional. According to a study by Tawfik and colleagues, the majority of distal upper extremity occurred at the wrist (76.4%), followed by the finger (14.5%), and hand (3.6%). Both male sex and XF participation for more than 5 years increased the likelihood of developing a hand or wrist injury (OR 2.10 male, OR 2.75 participation > 5 years). Although the vast majority of participants (72.7%) do not seek medical care for their hand/wrist injuries, those that did were diagnosed with a sprain, ligament rupture, or fracture [31]. This is consistent with MRI data on Olympic-level weightlifters and gymnasts, who sustained injuries to their extensor tendons (especially extensor carpi ulnaris), scapholunate and lunotriquetral ligaments, triangular fibrocartilage complex, and scaphoid and distal radial physis [33].
XF commonly utilizes movements from Olympic lifting and gymnastics, which report 2 of the 3 highest wrist injury rates among Olympic summer games athletes (1.56% weightlifting, 3.13% gymnastics, based on MRI) [33]. The overall rate of injury to the hand and wrist among XF participants (3.4–20.4%) is similar to that of other weight-training disciplines, including Olympic lifting (5–23%), body building (12–23%), and highland games (11%) [19]. Within XF participants, injuries to the hand and wrist were most commonly sustained during Olympic lifting and power lifting activities [8]. This is likely due to the high loads placed on the wrist, particularly in hyperextension, during many Olympic lifting, power lifting, and gymnastics movements [33, 34] (Fig. 8).
Fig. 8.

Wrist hyperextension during Olympic-style clean
Rhabdomyolysis
While injuries are common amongst XF athletes, a review of XF-induced upper extremity pathologies would not be complete without discussing rhabdomyolysis. Rhabdomyolysis is a potentially life-threatening condition often caused by vigorous physical activity leading to a cascade of muscle cell damage [35]. The condition occurs following damage to the skeletal muscular system causing toxic cellular material to enter the blood stream resulting in elevated creatine phosphokinase [36]. Serious cases of rhabdomyolysis may lead to renal failure, compartment syndrome, and dysrhythmias if left untreated [37]. As the popularity of extreme exercise regiments grows, there has been increased concern for compartment syndrome amongst otherwise healthy athletic individuals. Since rhabdomyolysis is a relatively uncommon condition, its true incidence in XF athletes is unknown and the condition is likely underreported. Two of the largest XF case series in the literature that report rhabdomyolysis followed 168 and 523 and reported 1 (0.5%) and 11 (2.1%) participants who developed rhabdomyolysis, respectively [28, 38].
Rhabdomyolysis can originate in any muscle group, making case reports of isolated upper extremity rhabdomyolysis uncommon. A case report by Meyer et al. discussed a healthy 31-year-old woman who developed two days of worsening bilateral biceps pain and soreness following a XF workout consisting of pushups, plyometrics, and weight training. She was eventually diagnosed with exercise-induced rhabdomyolysis of the biceps [39]. Another case report by Adhikari et al. reported a similar clinical scenario in a 22-year-old male who presented to the emergency department with generalized body aches and chest, upper back, shoulder, and arms pain 2 days after a high-intensity XF session and was diagnosed with bilateral upper extremity rhabdomyolysis [40]. One study by Routman et al. highlights a more specific and unusual form of upper extremity compartment syndrome in XF athletes; Routman and colleagues discussed two athletes who completed the “Sissy Test” which is a XF challenge consisting of 336 kettlebell swings and 336 squat thrust push-ups that were completed within 30 min. Both athletes in the case series experienced severe shoulder pain and an elevated creatine kinase. Magnetic resonances images of the shoulders demonstrated isolated infraspinatus myositis and marked edema in both cases, establishing the diagnosis of infraspinatus rhabdomyolysis in both athletes [41].
Although upper extremity rhabdomyolysis is an uncommon condition in XF athletes, the condition is severe and requires urgent hospitalization and rapid intravenous fluid administration to prevent serious and irreversible sequelae including renal failure and death. For this reason, XF participants, trainers, and clinicians should be educated on the prevention, treatment, and diagnosis of rhabdomyolysis.
Conclusions
The CrossFit body of research is limited to level IV and V studies; however, the literature is clear, CrossFit athletes face a high rate of upper extremity injury. For this reason, clinicians must be familiar with CrossFit and its associated pathology. There is limited evidence to guide athletes and trainers on injury prevention or to guide clinicians on treatment. However, athletes and trainers should focus on the development of proper form and avoiding exercise that elicit pain. Participants at the beginner or intermediate level and participants with a previous injury should be particularly careful in avoiding repetitive exercises, as well as the exercises which have been proven to be high-risk for upper extremity injury, including clean and jerk, snatch, press, and kipping pull-ups.
Declarations
Conflict of Interest
Richard W. Nicolay: declares that he has no conflict of interest.
Laura Moore: declares that she has no conflict of interest.
Tyler DeSena: declares that he has no conflict of interest.
Joshua Dines: declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Sports Injuries and Rehabilitation
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Richard W. Nicolay, Email: nicolayr@hss.edu
Laura K. Moore, Email: moorel@hss.edu
Tyler D. DeSena, Email: desenatyler@gmail.com
Joshua S. Dines, Email: dinesj@hss.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Clifford C. The founder of CrossFit credits his success to one simple secret. In: CNBC, editor. Iconic Tour. CNBC.com 2016.
- 2.Davis G. Is CrossFit killing us. In: Magazine O, editor. Training & Performance. Outsideonline.com 2013.
- 3.Hart M. Does CrossFit have a future. In: Yorker TN, editor. The Sporting Scene. NewYorker.com 2021.
- 4.Gregory S. Lift, Squat, Repeat: inside the CrossFit cult. In: Gregory S, editor. Time.com 2014.
- 5.Mehrab M, de Vos RJ, Kraan GA, Mathijssen NMC. Injury Incidence and Patterns Among Dutch CrossFit Athletes. Orthop J Sports Med. 2017;5(12):2325967117745263. doi: 10.1177/2325967117745263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paiva TMM, Kanas M, Astur N, Wajchenberg M, Martins Filho DE. Correlation between previous sedentary lifestyle and CrossFit-related injuries. Einstein (Sao Paulo). 2021;19:eAO5941. 10.31744/einstein_journal/2021AO5941. [DOI] [PMC free article] [PubMed]
- 7.Toledo R, Dias MR, Souza D, Soares R, Toledo R, Lacio M, et al. Joint and muscle injuries in men and women CrossFit(R) training participants. Phys Sportsmed. 2021;50:1–7. doi: 10.1080/00913847.2021.1892468. [DOI] [PubMed] [Google Scholar]
- 8.Weisenthal BM, Beck CA, Maloney MD, DeHaven KE, Giordano BD. Injury Rate and patterns among CrossFit athletes. Orthop J Sports Med. 2014;2(4):2325967114531177. doi: 10.1177/2325967114531177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.• Rodriguez MA, Garcia-Calleja P, Terrados N, Crespo I, Del Valle M, Olmedillas H. Injury in CrossFit(R): a systematic review of epidemiology and risk factors. Phys Sportsmed. 2021:1-8. 10.1080/00913847.2020.1864675. Recent systematic review of the incidence, nature, location and risk factors for injuries in over 12,000 CrossFit athletes.
- 10.Cheng TTJ, Mansor A, Lim YZ, Hossain Parash MT. Injury incidence, patterns, and risk factors in functional training athletes in an Asian population. Orthop J Sports Med. 2020;8(10):2325967120957412. doi: 10.1177/2325967120957412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barranco-Ruiz Y, Villa-Gonzalez E, Martinez-Amat A, Da Silva-Grigoletto ME. Prevalence of injuries in exercise programs based on CrossFit((R)), cross training and high-intensity functional training methodologies: a systematic review. J Hum Kinet. 2020;73:251–265. doi: 10.2478/hukin-2020-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.•• Szeles PRQ, da Costa TS, da Cunha RA, Hespanhol L, Pochini AC, Ramos LA, et al. CrossFit and the epidemiology of musculoskeletal injuries: a prospective 12-week cohort study. Orthop J Sports Med. 2020;8(3):2325967120908884. 10.1177/2325967120908884. A rare level II study which prospectively followed a cohort of 515 CrossFit athletes, reported the incidence of musculoskeletal injuries and quantified the odds ratios for associated risk factors for injury. [DOI] [PMC free article] [PubMed]
- 13.Alekseyev K, John A, Malek A, Lakdawala M, Verma N, Southall C, Nikolaidis A, Akella S, Erosa S, Islam R, Perez-Bravo E, Ross M. Identifying the most common crossfit injuries in a variety of athletes. Rehabil Process Outcome. 2020;9:1179572719897069. doi: 10.1177/1179572719897069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.• Elkin JL, Kammerman JS, Kunselman AR, Gallo RA. Likelihood of injury and medical care between CrossFit and traditional weightlifting participants. Orthop J Sports Med. 2019;7(5):2325967119843348. 10.1177/2325967119843348. This study demonstrated that athletes participating in CrossFit are more likely to be injured when compared to traditional weightlifting. [DOI] [PMC free article] [PubMed]
- 15.Tibana RA, de Sousa NMF. Are extreme conditioning programmes effective and safe? A narrative review of high-intensity functional training methods research paradigms and findings. BMJ Open Sport Exerc Med. 2018;4(1):e000435. doi: 10.1136/bmjsem-2018-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.• Feito Y, Burrows EK, Tabb LP. A 4-year analysis of the incidence of injuries among CrossFit-trained participants. Orthop J Sports Med. 2018;6(10):2325967118803100. 10.1177/2325967118803100. This study examined over 3,000 CrossFit athletes and found comparable injury rates to traditional weight lifting. The authors also identified, athlete inexperience and fewer workouts per week as risk factors for higher injury rates. [DOI] [PMC free article] [PubMed]
- 17.Montalvo AM, Shaefer H, Rodriguez B, Li T, Epnere K, Myer GD. Retrospective Injury Epidemiology and Risk Factors for Injury in CrossFit. J Sports Sci Med. 2017;16(1):53–59. [PMC free article] [PubMed] [Google Scholar]
- 18.Klimek C, Ashbeck C, Brook AJ, Durall C. Are injuries more common with CrossFit training than other forms of exercise? J Sport Rehabil. 2018;27(3):295–299. doi: 10.1123/jsr.2016-0040. [DOI] [PubMed] [Google Scholar]
- 19.Keogh JW, Winwood PW. The epidemiology of injuries across the weight-training sports. Sports Med. 2017;47(3):479–501. doi: 10.1007/s40279-016-0575-0. [DOI] [PubMed] [Google Scholar]
- 20.da Costa TS, Louzada CTN, Miyashita GK, da Silva PHJ, Sungaila HYF, Lara PHS, et al. CrossFit(R): Injury prevalence and main risk factors. Clinics (Sao Paulo). 2019;74:e1402. 10.6061/clinics/2019/e1402. [DOI] [PMC free article] [PubMed]
- 21.Hak PT, Hodzovic E, Hickey B. The nature and prevalence of injury during CrossFit training. J Strength Cond Res. 2013;Publish Ahead of Print. 10.1519/JSC.0000000000000318. [DOI] [PubMed]
- 22.Summitt RJ, Cotton RA, Kays AC, Slaven EJ. Shoulder injuries in individuals who participate in CrossFit training. Sports Health. 2016;8(6):541–546. doi: 10.1177/1941738116666073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.• Sugimoto D, Zwicker RL, Quinn BJ, Myer GD, Stracciolini A. Part II: Comparison of CrossFit-Related Injury Presenting to Sports Medicine Clinic by Sex and Age. Clin J Sport Med. 2020;30(3):251-6. 10.1097/JSM.0000000000000812. This study provides granular data on age and sex’s relationship with injury risk during CrossFit participation. It also gives insight into injury risk in pediatric and adolescent populations participating in CrossFit, which is rare in the current body of literature. [DOI] [PMC free article] [PubMed]
- 24.Prinold JA, Bull AM. Scapula kinematics of pull-up techniques: avoiding impingement risk with training changes. J Sci Med Sport. 2016;19(8):629–635. doi: 10.1016/j.jsams.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Millett PJ, Hussain ZB, Fritz EM, Warth RJ, Katthagen JC, Pogorzelski J. Rotator cuff tears at the musculotendinous junction: classification and surgical options for repair and reconstruction. Arthrosc Tech. 2017;6(4):e1075–e1e85. doi: 10.1016/j.eats.2017.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.•• Carbone S, Candela V, Gumina S. High rate of return to CrossFit Training after arthroscopic management of rotator cuff tear. Orthop J Sports Med. 2020;8(4):2325967120911039. 10.1177/2325967120911039. This case series demonstrates a high (100%) return to training rate nine months after an arthroscopic rotator cuff repair in a population of CrossFit athletes. This study provides important information to surgeons who are counseling CrossFit athletes with rotator cuff tears who are considering surgery. [DOI] [PMC free article] [PubMed]
- 27.•• Carbone S, Castagna V, Passaretti D, Candela V, Cerciello S, Delli Sante E, et al. Supraspinatus repair and biceps tenodesis in competitive CrossFit athletes allow for a 100% of return to sport. Knee Surg Sports Traumatol Arthrosc. 2020. 10.1007/s00167-020-06345-2. This case series demonstrates a high (100%) return to training and a high (90%) return to competition rate 24 months after an arthroscopic supraspinatus repair and biceps tenodesis in a population of CrossFit athletes. This study provides important information to surgeons who are counseling CrossFit athletes with rotator cuff tears and biceps pathology who are considering surgery.
- 28.Hopkins BS, Li D, Svet M, Kesavabhotla K, Dahdaleh NS. CrossFit and rhabdomyolysis: a case series of 11 patients presenting at a single academic institution. J Sci Med Sport. 2019;22(7):758–762. doi: 10.1016/j.jsams.2019.01.019. [DOI] [PubMed] [Google Scholar]
- 29.Doarn MC, Carlson MS. Exercise-induced bilateral upper-arm anterior and posterior compartment syndrome with rhabdomyolysis. J Shoulder Elbow Surg. 2021;30(3):e129–ee31. doi: 10.1016/j.jse.2020.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Lavallee ME, Balam T. An overview of strength training injuries: acute and chronic. Curr Sports Med Rep. 2010;9(5):307–313. doi: 10.1249/JSR.0b013e3181f3ed6d. [DOI] [PubMed] [Google Scholar]
- 31.Tawfik A, Katt BM, Sirch F, Simon ME, Padua F, Fletcher D, Beredjiklian P, Nakashian M. A Study on the incidence of hand or wrist injuries in CrossFit athletes. Cureus. 2021;13(3):e13818. doi: 10.7759/cureus.13818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams S, Booton T, Watson M, Rowland D, Altini M. Heart rate variability is a moderating factor in the workload-injury relationship of competitive CrossFit athletes. J Sports Sci Med. 2017;16(4):443–449. [PMC free article] [PubMed] [Google Scholar]
- 33.Alizai H, Engebretsen L, Jarraya M, Roemer FW, Guermazi A. Wrist injuries detected on magnetic resonance imaging in athletes participating in the Rio de Janeiro 2016 Summer Olympic Games. Quant Imaging Med Surg. 2021;11(7):3244-51. 10.21037/qims-20-1121. [DOI] [PMC free article] [PubMed]
- 34.Desai N, Vance DD, Rosenwasser MP, Ahmad CS. Artistic gymnastics injuries; epidemiology, evaluation, and treatment. J Am Acad Orthop Surg. 2019;27(13):459–467. doi: 10.5435/JAAOS-D-18-00147. [DOI] [PubMed] [Google Scholar]
- 35.Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: rhabdomyolysis -- an overview for clinicians. Crit Care. 2005;9(2):158–169. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giannoglou GD, Chatzizisis YS, Misirli G. The syndrome of rhabdomyolysis: pathophysiology and diagnosis. Eur J Intern Med. 2007;18(2):90–100. doi: 10.1016/j.ejim.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 37.Furman J. When exercise causes exertional rhabdomyolysis. JAAPA. 2015;28(4):38–43. doi: 10.1097/01.JAA.0000458861.78559.3b. [DOI] [PubMed] [Google Scholar]
- 38.Larsen C, Jensen MP. Rhabdomyolysis in a well-trained woman after unusually intense exercise. Ugeskr Laeger. 2014;176(25). [PubMed]
- 39.Meyer M, Sundaram S, Schafhalter-Zoppoth I. Exertional and CrossFit-induced rhabdomyolysis. Clin J Sport Med. 2018;28(6):e92–ee4. doi: 10.1097/JSM.0000000000000480. [DOI] [PubMed] [Google Scholar]
- 40.Adhikari P, Hari A, Morel L, Bueno Y. Exertional Rhabdomyolysis After CrossFit Exercise. Cureus. 2021;13(1):e12630. doi: 10.7759/cureus.12630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Routman HD, Triplet JJ, Kurowicki J, Singh N. Isolated rhabdomyolysis of the infraspinatus muscle following the CrossFit "Sissy Test": a report of two cases. JBJS Case Connect. 2018;8(1):e2. doi: 10.2106/JBJS.CC.17.00020. [DOI] [PubMed] [Google Scholar]