Abstract
Background
There is scattered evidence of the impact of workplace interventions in improving employees' physical activity. This systematic review was performed to evaluate the strategies of workplace interventions and their effectiveness, as reported in primary studies.
Method
Primary experimental trials, both randomized controlled trials (RCTs) and non‐RCTs, which examined interventions to increase healthy adult employees' physical activity were included in this review. Studies in English or Persian published between 2009 and 2019 with access to full text of resources were considered. Google Scholar, PubMed, Web of Science, Scopus and Cochrane Library, ProQuest (Thesis) and World Health Organization Clinical Trial Registration Databases and Persian databases such as SID, Magiran, IranMedex, Irandoc were searched. All the stages of review were conducted based on PRISMA. RoB and ROBINS‐I were used to assess the risk of bias of the primary studies.
Results
Thirty‐nine studies, with a total of 18 494 participants, met the inclusion criteria. Of these, 22 were RCTs, 17 were non‐RCTs. Effective interventions were reported in 15 RCTs and 14 non‐RCTs. Four main strategies of interventions were identified, consisting of motivation and support; monitoring and feedback; information and education; and activity. Thirteen different behavior change techniques (BCT) were identified with self‐determination theory (SDT) being the most frequent behavior change theory used.
Conclusion
It seems that a multi‐strategy intervention that one of the strategies of which is physical activity in the workplace (Activity), the use of behavioral change theories, especially SDT, may be indicative of a more effective intervention. It is recommended that BCTs be considered when designing physical activity interventions.
Keywords: behavior change models and theories, behavior change techniques (BCTs), effectiveness, employee, physical activity, systematic review
1. BACKGROUND
Physical inactivity is recognized as a major risk factor in non‐communicable diseases and premature deaths worldwide. Insufficient physical activity can increase the risk of cardiovascular diseases, type 2 diabetes, colon and breast cancers, and depression. 1 , 2
Based on the World Health Organization report, 25% of the world adults do not get adequate physical activity. The Americas and the Eastern Mediterranean regions have the highest prevalence of physical inactivity in adults. 3 Between 1 and 4 percent of direct health‐care costs are related to physical inactivity. 4 Estimates of disability‐adjusted life years (DALYs) for risk factors of non‐communicable diseases in the world showed that low physical activity led to 169.09 DALYs per 100 000 in 2000, increasing to 203.53 DALYs per 100 000 in 2019. 5
As many inactive adults spend many hours in the workplace, several intervention studies have been conducted to attempt to increase employee physical activity within the workplace. 6 , 7 Workplace interventions include health education, motivational training sessions, holding sports classes, using pedometers, and riding a bicycle to work. The outcomes of studies have been measured by multiple indicators such as changes in weight, body mass index (BMI), blood pressure, lipids and mental health conditions such as anxiety and depression. 8 , 9
There is scattered evidence of the impact of workplace physical activity interventions; Primary studies are often heterogeneous, with some having poorly designed methodology and ambiguous results. Furthermore, few secondary studies have been able to determine the most effective methods to increase employees' physical activity in different organizations. 10
Different studies have conducted to measure the levels of physical activity in different worksites, such as universities and health organizations. They have confirmed low average levels of employees' physical activity. 11 Also, the relationship between worksite physical activity and different physical and mental health outcomes have been assessed. Secondary studies have revealed individual, environmental and organizational determinants of physical activity in the workplace but there is no summary of the effectiveness of worksite interventions. 12
This study aimed to evaluate and categorize the strategies of workplace interventions in increasing employees' physical activity as effective and non‐effective, as reported in primary studies at the international and national levels.
2. METHODS
2.1. Criteria for considering studies for this review
Inclusion criteria included randomized controlled trials (RCTs) or non‐randomized controlled trials (non‐RCTs) based in the workplace with a study population of full‐time or part‐time employees aged 18 years or older and in a self‐reported healthy state and without contraindications to perform the physical activity interventions. Studies in English and Persian, published between 2009 and 2019, and with access to the full text were considered.
2.2. Search
Google Scholar, PubMed, Web of Science, Scopus and Cochrane Library, ProQuest (Thesis) and World Health Organization Clinical Trial Registration Databases were searched for studies on workplace interventions to increase physical activity.
As it was important to be able to apply the results of this review to Iran, Persian databases such as SID, Magiran, IranMedex, and Irandoc were also searched. We used the PICOS research tool which focuses on the Population, Intervention, Comparison and Outcomes and Study design. The key words used are shown in Table 1.
TABLE 1.
Key words used in the PICOS search
| Key word used |
|---|
|
(((physical* [Title] OR exercis* [Title] OR sport* [Title] OR movem*[Title] OR sit*[Title]))) AND (employe* [Title] OR work* [Title] OR job* [Title] OR staff* [Title] OR office*[Title]) AND (interven* [Title] OR trial* [Title] OR program* [Title] OR plan* [Title] OR barrier*[Title]) |
2.3. Data collection
2.3.1. Selection of studies
By using the inclusion criteria, titles and abstracts of studies were examined by two reviewers independently. The full texts of eligible studies were retrieved. All stages of the study were done based on the agreement between the two reviewers with a third reviewer making decisions when there was disagreement.
2.3.2. Data collection and management
Data from eligible primary studies were extracted, including the name of the first author; location of study (country and organization); sample size; sex and mean age of participants; duration of interventions and follow‐up; risk of bias in the study (low risk, some concern and high risk); measuring instruments (subjective measuring instruments such as self‐reported questionnaires to determine the level of physical activity and objective measuring instruments such as pedometer); indicators to measure the effect size; effectiveness of study; type of study (RCT or non‐RCT) and type of interventions.
Regarding the variety of the extracted interventions from the included studies, the authors decided to provide an applicable and simplified classification. So, they categorized them into four main strategies: (1) Information and education; (2) Activity; (3) Motivation and support; (4) Monitoring and feedback by the consensus.
2.3.3. Assessment of risk of bias
The risk of bias tool for randomized trials (RoB) and risk of bias in non‐randomized studies of interventions (ROBINS‐I) were used to assess the risk of bias. 13 , 14 Studies at high risk of bias were excluded from this systematic review.
The Cochrane Collaboration Risk of Bias (RoB) checklist was used for the quality assessment of included randomized trial studies, which consists of two parts and six domains. Risk of selection, reporting, and other bias are assessed in the part I and performance, detection, and attrition bias are assessed in part II. The domains were assessed based on “high”, “low”, and “unclear” risk levels.
For non‐ randomized trial studies the ROBINS‐I tool was used. It contains seven domains as follows: confounding, selection of participants into the study as pre‐intervention bias, classification of interventions as At‐ intervention bias, bias due to deviations from intended interventions, missing data, measurement of outcomes, selection of the reported result as Post‐intervention ones. Overall judgment about risk of bias response options are: low, moderate, serious, critical, no information level of bias which the three last ones were considered as poor quality. Two reviewers (P.M.K.H. and S.H.) performed the quality assessment of RCTs and two other researchers (N.K.H. and N.S.) assessed the Non‐RCTs risk of bias independently. Any disagreements in this process was resolved by the third independent reviewer (B.T).
2.3.4. Measures of effect and study effectiveness
As any included study in this review used different intervention to increase physical activity at workplace, the various outcomes were measured by different tools. Therefore the indicators which measured the effect size of physical activity interventions, were in various types; such as mean difference, mean (SD) in repeated measures analysis, adjusted mean change within and between groups, estimate of GLM repeated measures, relative risk (RR), odds ratio (OR), geometric mean ratio, Beta coefficient of regression, percentage change before and after intervention. These indicators have been shown separately for each study (Table 2).
TABLE 2.
Characteristics of the 39 articles
| Code | Studies (Author, Year of publication) | Study Setting (Location, Environment) | Sample [Number: Total/Female/Male Age: Mean (SD) or Range] | Intervention/Comparison description | Duration intervention follow up | The physical Activity Measurement tool (self‐report/objective) | Unit of measurement | Indicator | Result of quality assessment (risk of bias) |
|---|---|---|---|---|---|---|---|---|---|
| Effective/RCT | |||||||||
| 1 | Nicholas D Gilson et al. 2009 | Major regional universities (UK, Australia and Spain) |
179/141/38 41.3 (10) |
‐ Control group (n = 60; maintain normal behavior) route‐based ‐ Walking group (n = 60; at least 10 minutes sustained walking each workday) ‐ An incidental walking group (n = 59; walking in workday tasks) |
10 weeks | Objective: Pedometer | Step counts | Mean difference | Some concern |
| 2 | Holly Blake et al. 2015 | UK hospital workplace |
296/41/255 19–67 years |
I1:2 messages per week to increase physical activity by SMS I2: 2 messages per week to increase physical activity by e‐mail |
12 weeks F: 0‐6‐12‐16 weeks |
Self‐report: Global Physical Activity Questionnaire |
Frequency, d/week Duration, h/d |
Mean (SD) in Repeated measures analysis | Some concern |
| 3 | Charlotte L Brakenridge et al. 2016 | Organization in different cities in Australia (Sydney & Brisbane) |
153/72/81 40.0 (8.0) 37.6 (7.8) |
The organizational‐level intervention for both groups with additional support from a wearable activity tracker for intervention group |
I:3 months F:12 months |
Thigh‐worn activPAL3 monitor |
Work Hours and overall hours standing, stepping and step count Min/10 h Min/16 h |
Adjusted mean change (95% CI) within groups Adjusted mean difference (95% CI) between groups |
Some concern |
| 4 | M Fournier et al. 2016 | Service company in the south of France |
49/28/21 47.5 (8.29) |
I1: a group attending supervised PA sessions (PA condition) I2: a group attending the same sessions plus receiving text messages before each session (PA + SMS condition) |
28 weeks | Self‐report: IPAQ | MET/week | Estimate of repeated measures GLM | Some concern |
| 5 | Julie A Gazmararian et al. 2012 | Main campus of Emory University in Atlanta, Georgia |
410/252/158 21–73 years |
Control Gym Gym+Edu Gym+Time Gym+Edu + Time |
9 months | 7 Day Physical Activity Recall (PAR) | Percent of more days per week of adequate PA | RR | Low risk |
| 6 | Florence‐Emilie Kinnafick et al. 2016 | A large UK University |
65/61/4 18–66 years |
C: neutral SMS I: need supportive SMS two text messages per week |
I: 10 weeks F: 4 months |
7‐Day PAR | Time of Moderate Vigorous Physical activity (min) | Mean difference | Some concern |
| 7 | Minna Aittasalo et al. 2012 | 20 office‐based worksites in Southern Finland |
241/165/76 44.1 (9.4) 45.3 (9.1) |
C: COMP: only data collection I: STEP: (1) A 1‐hour preliminary meeting (2) Self‐monitoring of PA (3) Monthly e‐mail |
I:6 months F:6 months |
IPAQ |
Walking at work Walking for transportation Walking stairs Total walking (Weekly minutes) |
Odds ratio Geometric mean ratio |
Some concern |
| 8 | Naomi Burn et al. 2017 | Flinders University of South Australia |
71/66/5 44.4 (9.3) 48.3 (11.2) 46.8 (7.9) |
C:control I1:an after‐work group that had 3 × 60 min instructor‐led PA sessions each week of the six‐week program I2: an in‐work group that had 2 × 15 min instructor‐led PA periods 3 days/wk at mid‐morning and mid‐afternoon. |
6 weeks (40 days) | Self‐reported AAS (Active Australia Survey) | Total, Vigorous PA (Min/Week) | Mean difference | Some concern |
| 9 | Marcos Ausenka Riberio et al. 2014 |
Large University Hospital In Sao Paulo, Brazil |
195/195/0 40–50 years |
MTC (Minimal treatment Comparator) PedIC (Pedometer‐based individual counseling) PedGC (Pedometer‐based group counseling) AT (Aerobic training) |
I:3 months F:3 months |
Objective: Pedometer Self‐report: IPAQ |
Step count | Mean difference | Low risk |
| 10 | C Pedersen et al. 2018 | Norwegian Post delivering mail and logistic services |
202/48/154 42.5 (11.65) |
I: The intervention group was offered six sessions of group‐based intervention elements: Two workshops and four PA support group meetings, a total of 7.5 h C: The control group were not offered any employer initiated group‐sessions between baseline and post‐test assessments |
I:16 weeks F: 5 mounts |
Self‐report [the three‐item questionnaire International Physical Activity Index (IPAI)] |
Habitual PA in terms of the average frequency, duration, and intensity per week |
Mean difference | Some concern |
| 11 | Rod K Dishman et al. 2010 | Home Depot Inc. in the USA |
1442/995/447 36.2 (10) 19–64 |
I: ‐ Goal setting (personal goals and team goals) ‐ Organizational action / C: Monthly newsletters describing the health benefits of physical activity |
I: 12 weeks | Self‐report with handbook logs/Objective with pedometer |
Daily pedometer steps ‐ Weekly number of 10‐min blocks of MVPA ‐Biweekly self‐ratings indicators of their satisfaction with current physical activity levels, their confidence (i.e. self‐efficacy), commitment and intention to carry out the new goal |
Mean difference | Some concern |
| 12 | Karen Van Hoye et al. 2018 | Flemish employees (Belgium) |
227/124/103 41 (10) 19–67 |
Four intervention groups regarding 4 types of feedback: 1. Minimal Intervention Group (MIG; no feedback) 2. Pedometer Group (PG; feedback on daily steps only) 3. Display Group (DG; feedback on daily steps, on daily moderate to‐vigorous physical activity [MVPA] and on total energy expenditure [EE]) 4. Coaching Group (CoachG; same as DG with need supportive coaching) |
I: 4 weeks F: 12 months |
Self‐ report with FPACQ*/Objective with SWE** and Pedometer *The Flemish Physical Activity Computerized Questionnaire **The Sense Wear Armband |
‐ Daily physical activity level (PAL) ‐ Metabolic Equivalent of Task [MET] ‐ Number of daily Steps ‐ Daily minutes of moderate to vigorous physical activity (MVPA) ‐ Active daily EE (EE >3 METs) ‐ Total daily EE |
Mean difference | Low risk |
| 13 | Nirjhar Dutta et al. 2014 | Office workers at Caldrea, Inc., a company located in the Twin Cities Metro Area, MN, USA |
28/19/9 Mean Age: 40.4 |
I: Sit‐Stand Desks (SSDs) C: Usual sitting desks |
I: (cross‐over design) − 4 weeks ‐2 weeks washout − 4 weeks F: the same time, except washout period |
Self‐reported Occupational Sitting and PA questionnaire (OSPAQ)/accelerometers |
(OSPAQ) score/Steps/PA intensity | Mean difference | Some concerns |
| 14 | Wendell C Taylor et al. 2016 | 4 worksites in Texas, USA |
175/145/30 Mean Age: 43 |
1. Booster Break arm: 15 minutes break with a structured series of stretching, strengthening and aerobic movements, followed by a 60‐second meditation 2. Computer‐prompt arm: an interrupted sedentary time by 3‐minute breaks at five hourly intervals daily 3.Control Group or Usual‐break arm |
6 months | Self‐report (long Version of IPAQ)/Pedometer | METs/Total steps per week/Average steps per day | B of regression | Some concerns |
| 15 | Kazuhiro Watanabe et al. 2018 |
Different types of worksites in the Kanto area in Tokyo, Japan For white‐color employees |
190/66/123 48.14 (11.4) 43.11 (10.0) |
I: Selected interventions from a list of 13 interventions, feed backs (baseline,3 months, and 6 months), baseline occupational health services C: Feed backs (baseline,3 months, and 6 months), baseline occupational health services |
I: 3 months F: 6 months |
The Japanese version of Global Physical Activity Questionnaire | MET/week | B of regression | Some concerns |
| Effective/Non‐RCT | |||||||||
| 16 |
Charles Sounan et al. 2013 A pretest posttest study design |
University‐affiliated multi‐site healthcare center in Canada comprised of six hospitals and one administrative site |
310/286/24 47.6 (9.1) 24–70 years |
I: “Wellness Challenge”: 1 h lecture, 30 min evaluation, 8 week pedometer activity challenge |
I: 8 weeks |
Pedometer Self‐administered questionnaire IPAQ short form |
Mean (SD) of: ‐ Vigorous activity MET ‐ Moderate activity MET ‐ Walking MET ‐ Total MET score ‐ Days walking 10 min |
Mean difference & Activity classification based on step counting | Some concern |
| 17 |
M H Baghianimoghaddam et al. 2016 Pretest posttest design with comparison group |
Tabriz University located in Azerbaijan province at North‐West of Iran |
154/154/0 36.5 (6.7) 37.2 (7.3) |
(1) Increase step counts (try to increase 500 steps a day this week); (2) providing solutions to overcome barriers; (3) Recommending strategies to help perceived benefits of PA; (4) Suggestions for increasing social support and encouragement to promote PA as team work and worksite step competition; (5) Recommendation to promote staircase instead of the elevator, using their break times to walk and to park their cars further away from building. | 16 weeks |
Pedometer IPAQ |
‐ METs from IPAQ ‐ Step counts |
‐ Mean difference | Some concern |
| 18 | Minna Aittasalo et al. 2017 | 12 small or medium‐size workplaces (Finland) |
296/222/74 42.6 (10.9) |
Moving To Business (MTB) with 3 phases: starting, active, closing A list of multilevel interventions |
1 year |
Questionnaire Accelerometer |
PA and sitting during working and leisure times |
‐ Change in mean minutes ‐ Change in % wear‐time |
Some concern |
| 19 |
Pauline Manon Genin et al. 2017 Non‐RCT 3‐arms (Pilot study) |
Tertiary sector workers in a manufacture |
95/33/62 44 (9.9) |
(i) Control group (CON) engaged in less than 150 minutes moderate physical activity per week for at least 1 year, according to the IPAQ short‐form questionnaire and not motivated to start the worksite physical activity program (ii) Novice group (NOV) participants unsupported by physical activity and who started the worksite physical activity program at the beginning of the study, (iii) participants engaged in the worksite physical activity program for the last 2 years at least (minimum of two 45 minutes sessions per week) (EXP) |
5 months | IPAQ‐SF | MET/week | Mean Difference | Some concern |
| 20 | Jan Keller et al. 2016 | German pharmaceutical company |
1063/610/453 39.0 (10.1) 16–62 years |
Workplace health promotion (WHP) The WHP for intenders and changing actors consisted of an intervention that predominantly addressed self‐efficacy (participants' responses on their successful past activities& verbal persuasion), action planning, and coping planning (barrier) and contained up to 44 partly interactive pages on the study website | 12 weeks | Godin Leisure Time‐Questionnaire | Min/week | p‐value of Linear slope estimate | Low risk |
| 21 |
Isabel Hess et al. 2014 Pre and post‐test design |
Liverpool Hospital, UK |
389/361/28 20–67 years Mean Age: 39.1 |
TEAM Challenge (TEAM = Take steps, Eat well, And Measure up). |
12 weeks | Active Australia (AA) questionnaire | Frequency |
Before and after challenge median (IQR) |
Low risk |
| 22 |
Yun‐Ping Lin et al. 2017 Pretest posttest comparison group design |
Two aerospace industrial workplaces in Taiwan |
99/52/47 52.1 (6.57) 46.8 (9.75) |
I: Sit Less Walk More composed of 5 components C: a newsletter monthly |
12 weeks |
7‐item International Physical Activity Questionnaire (Taiwan) short‐form (IPAQ‐SF) |
Walking, MET‐min/wk Moderate, MET‐min/wk Vigorous, MET‐min/wk Total, MET‐min/wk |
Coefficient (SE) for Group*Time Mean Difference for each group |
Low risk |
| 23 | Gabriel A Koepp et al. 2013 |
Educational Credit Management Corporation (ECMC), a financial services corporation; in Oakdale, MN, USA |
36/25/11 42 (9.9) |
(access to) treadmill desk intervention | 1 year | belt‐worn accelerometer |
activity units (AU)/day min/day |
Mean diff | Low risk |
| 24 | S Hazaveei et al. 2018 | Hamadan University of Medical Sciences, Iran |
80/44/36 41–50 years |
4 class sessions, group walking with training program, 2 pool sessions, call and weekly SMS |
I: Not mentioned F: 1,2 months |
IPAQ |
Prevalence | Percent |
Some concern |
| 25 | Anass Arrogi et al. 2017 | A large pharmaceutical company in Flanders, Belgium |
300/234/66 42 (9) |
I: Two one‐hour in‐person counseling sessions, and three virtual counseling through e‐mail or telephone at weeks three, 6 and 9. Moreover, there were 2 other behavioral change techniques including identification barriers and self‐monitoring F: Only monitoring |
I: 3 months F: 9 months |
The 7‐item short version of the IPAQ/the Sense Wear Pro3 Armband |
Questionnaire Score/Steps/PA intensity in MET/Time of activity and intensity | Mean difference |
Some concern |
| 26 | M Vahedian‐Shahroodi et al. 2016 | Mashhad Factories Industrial, Iran |
76/76/0 Mean Age: 27.91 |
I: Four 15‐minute counseling sessions with intervals of one week in the first month then in weeks 6, 10, 14 and 18, by examining stage of the behavior change and using the five‐step counseling process C: Health, sport and physical activity pamphlet |
20 weeks | IPAQ (short form) | Score | Mean difference |
Some concern |
| 27 | Anna Puig‐Ribera et al. 2015 | Six campuses in four Spanish Universities in Galicia, the Basque Country and Catalonia |
264/179/93 42 (10) |
I: Workplace web‐based intervention (Walk@WorkSpain, W@WS) C: Maintained normal behavior |
3 phases: 1.Ramping:8 weeks 2. Maintenance:9–19 3. follow up: 2 months |
Pedometer |
Steps |
Mean difference |
Low Risk |
| 28 | Carling E. Butler et al. 2015 | The employees at Washington University in St. Louis, MO, USA |
121/103/18 46 (11) |
I: 1. The web‐based Activity Tracker with 8 weeks of pedometer‐based walking and tracking activities 2. Individualized walking plans based on a 10‐Question Walking Plan Quiz 3. Weekly wellness education sessions 4. Consultation opportunities 5. Participation rewards 6. Goal setting |
I: 8 weeks F: immediately after 8 weeks |
Pedometer |
Average Daily Steps (LSM) Least Squares Means/Odds Ratio |
Mean difference/Odds Ratio |
Low Risk |
| 29 | M. Ryan Mason et al. 2017 | A Large southeastern university, Kentucky, USA | 2206 |
A PA intervention with tiered incentives (value: $10.50–$29.00), based on their pre‐intervention PA level in 4 groups: 1. <6000 2. 6000 to 7999 3. 8000 to 9999 4. ≥10 000 steps/d |
I:6 weeks Pre: 1 week Post:1 week |
Accelerometer |
Step/d | Mean difference |
Some concern |
| Non‐effective/RCTs | |||||||||
| 30 | Mika Liukkonen et al. 2017 | Medium‐sized enterprise in recycling in Finland |
121 42 (10) |
Group A received only the separate test results (not the Body Age index). Group B received the Body Age results (index in years) Group C received both Body Age and separate test results, as well as a training computer (FT60; Polar Electro Inc.) |
1 year | IPAQ‐SF | MET/min/week | Mean difference | Some concern |
| 31 | Rosemary RC McEachan et al. 2011 | 44 UK worksites (based within 5 organizations: Bus Company; Hospital; Local Government Council; National Government Organization; University) |
1260/690/570 42.46 (10.77) 43.13 (10.41) |
The intervention consisted of a 3‐month toolkit of activities consisted of 8 key components |
I:3 months F:3,9 months |
IPAQ‐SF | B of Regression model | Beta and CI | Some concern |
| 32 | Anne N. Thorndike et al. 2012 | Massachusetts General Hospital (MGH), a teaching hospital in Boston, Massachusetts, USA |
330/285/45 44.2 (11.8) 41.6 (13.6) |
I: Internet and personal contacts C: No intervention |
I: 9 months F: 1 year |
Self‐report with web‐based logs/Objective with pedometer | Average time spent per week in physical activities, such as walking or running, bicycling, or other aerobic exercise/steps | Mean difference | Some concern |
| 33 | Jennifer L. Reed et al. 2018 | Nurses working in a cardiovascular setting, Canada |
76/74/2 46 (11) |
Three intervention groups: 1.Individual 2.Friends 3.Team An intervention providing participants with feedback from an activity monitor coupled with a web‐based individual, friend or team PA challenge, on their physical activity |
I: 6 weeks F: the same |
Accelerometer |
‐ Steps ‐ Minutes of MVPA |
F | Some concern |
| 34 | Nancy M. Gell et al. 2015 | Female employees at a public university in the Southeastern USA |
87/87/0 48.9 (10.6) 45.4 (10.7) |
I: sending 3 text messages per week to their personal cell phone via SMS which were motivational, informational, and specific to performing physical activity C: All participants received the maps display walking routs in the area. Furthermore, they had access to the web sites links which show guidelines and educational materials for physical activity |
I: 24 weeks F: the same |
Pedometer | Steps | Mean steps | Some concern |
| 35 | Rodriguez‐Hernandez MG. et al. 2019 | Sedentary office employees at Auburn University, USA |
68/51/17 48 (9) 46 (9) 42 (10) |
I: ‐ Intervention group 1: continues walking, ‐ Intervention group 2: intermittent walking C: All participant received move bands and recommendation to walk 10 000 steps per day |
I:10 weeks F:1 week |
RPE (Rating of Perceived Exertion) as a self‐report tool for physical activity intensity/ ‐Move band for 10 weeks ‐waist worn accelerometer for baseline, weeks 6 and 11, as objective tools to count steps |
RPE mean score/Steps | Mean difference/F | Some concern |
| 36 | Suzan JW Robroek et al. 2012 |
Six companies in the Netherlands From health care organizations (n = 2), commercial services (n = 2) and an executive branch of government (n = 2) |
924/472/454 Mean Age: 42 20–63 years |
I: A standard worksite health promotion program, plus access to an individual Health Portal with four main parts: 1. a personal coach, 2. a monitoring activity, 3. a computer‐based advice, and 4. opportunities to contact health professionals C: The standard worksite health promotion program (Access to a limited Health Portal, consisting of: ‐ General information on health topics) |
I: 12 months full intervention and 12 months partial intervention (without 4th part) F: 24 months |
IPAQ (short form) | MET‐minutes per week | Odds Ratio | Some concern |
| Non‐effective/Non‐RCTs | |||||||||
| 37 | Emma J Adams et al. 2017 | Non‐RCT – Field trial | 5512 | A menu of options was provided with suggestions for activities which could be delivered | About 1–2 years |
Self‐reported physical activity was assessed using a single item measure of physical activity Work‐related physical activity was assessed using a question taken from the European Prospective Investigation in Cancer and Nutrition questionnaire (EPIC) |
‐ Mode of transport to and from work ‐ Time spent walking ‐ Incidental walking ‐ Mediators of behavior change ‐ Colleague support |
Percent of each variable | Some concern |
| 38 |
Katrien A De Cocker et al. 2010 Quasi‐experimental controlled pretest posttest study |
A social service Belgian company with 3main selection criteria ‐ White‐collar workers with a sedentary job ‐ At least 500 eligible employees ‐ No earlier participation in a pedometer‐based program |
298 |
A PA intervention based on ‘10 000 Steps Ghent’, a whole‐community intervention The underlying idea is that interventions should include multilevel strategies focusing on behavioral and (social) environmental factors |
20 weeks | Pedometer | Step count | Mean difference | Low risk |
| 39 | RF Hunter et al. 2013 | An office‐based workplace setting in Belfast, Northern Ireland, UK |
406/272/134 43.32 (9.37) |
I: Getting a financial incentive for their times of physical activity based on the PAL (Physical Activity Loyalty) card C: No financial incentive. Only monitoring by the PAL |
I: 12 weeks F: 6 months |
The Global Physical Activity Questionnaire (GPAQ)/Objective records based on the PAL (Physical Activity Loyalty) card | Questionnaire Score/time of PA | Mean difference | Some concerns |
It was considered an effective intervention to improve workplace physical activity, based on the positive significant change reported at least in one of the measured indicators of any intervention in each included study.
2.3.5. Analysis
Due to the different participants' characteristics and the type of work, the diversity in intervention duration and the different kinds of settings as well as the different methods of measurement of physical activity, a meta‐analysis was not feasible, we conducted a narrative synthesis for this review. The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) statement was used for reporting this systematic review. 15
3. RESULTS
3.1. Study selection
A total of 5026 relevant articles were retrieved, of which 4872 were from the databases mentioned in the method part and 154 articles were found by a manual search of the reference list of the primary studies. Following removal of duplicates and screening by the title and abstract, 357 full‐text articles were quality assessed. Of these, 39 articles were selected for systematic review. The exclusion criteria included poor quality studies, irrelevant outcomes, non‐workplace interventions, non‐interventional studies, and the articles that were not in English or Persian. The process is shown in Figure 1.
FIGURE 1.
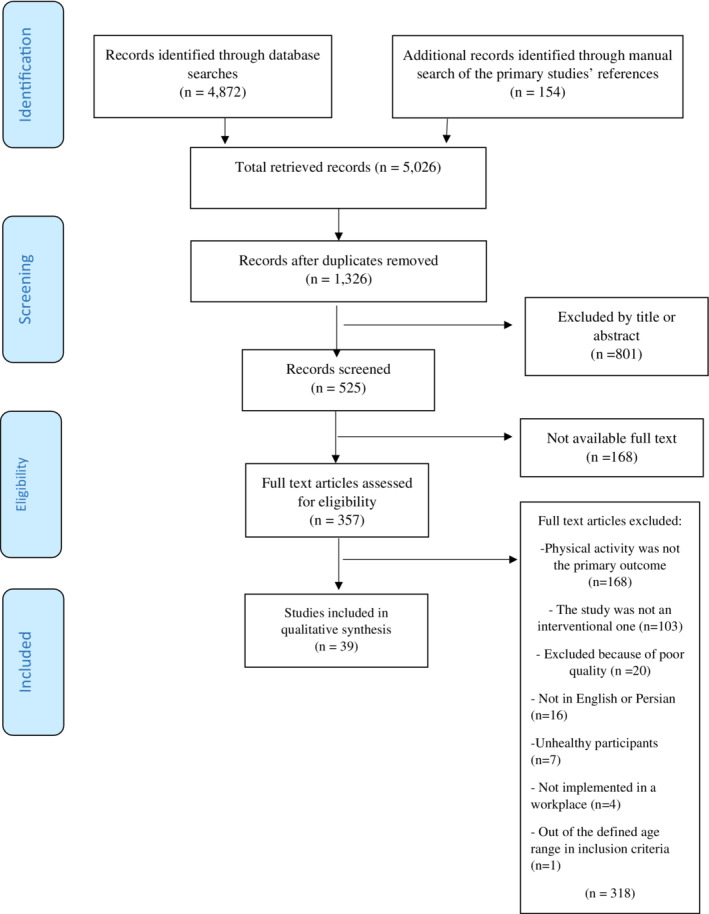
PRISMA flow diagram.
3.2. Description of studies
Thirty‐nine studies with a total of 18 494 participants met the inclusion criteria. Of these, 22 were RCTS and 17 were non‐RCT.
Table 2 displays the characteristics of the 39 articles. 15 RCTs and 14 Non‐RCT revealed effective interventions; the studies 1 to 15 were effective RCTs, 16 to 29 were effective non‐RCTs, 30 to 36 were non‐effective RCTs and the last 3 (37 to 39) were non‐effective non‐RCTs. The sample size of studies ranged from 28 to 5512 participants. The durations of the interventions were reported from 1 month to 1 year and the majority of the studies did not have a follow‐up phase. The majority of participants were women and in the fifth and sixth decades of life. The interventions were conducted either as uni‐centric or multi‐centric trials. Three studies were located in Iran and the rest of the studies were in the United States, Europe, and East Asia.
3.3. Quality assessment of studies
From the 39 studies included in this review, 10 were classified as low risk of bias and 29 were considered some concerns of risk of bias based on RoB and ROBINS‐I.
3.4. Worksite physical activity interventions
3.4.1. Strategies of interventions
Four main strategies of interventions were extracted from included studies. The average number of strategies used per study was 2.6 in the 29 effective studies, and 2.4 strategies in the 10 non‐effective studies. The majority of studies used three strategies of physical interventions. Table 3 shows the frequencies of use of the four main strategies in effective and non‐effective studies.
TABLE 3.
The frequencies of use of the four strategies of interventions
| Type of study | |||
|---|---|---|---|
| Strategy of intervention | Effective (29 studies) | Non‐effective (10 studies) | |
| 1 | Motivation & Support | 29 | 9 |
| 2 | Monitoring & Feedback | 20 | 8 |
| 3 | Information & Education | 19 | 6 |
| 4 | Activity | 9 | 1 |
3.4.2. Behavior change techniques (BCTs)
Abraham et al. structured a list of 40 behavior change techniques (BCTs). 16 BCTs are techniques that help an individual change their behavior to promote better health. 17 We reviewed the application of BCTs in the evaluation of the interventions' effectiveness. In 39 studies, 247 BCTs were extracted, with 187 BCTs used in effective studies, and 60 BCTs in the non‐effective studies. Effective studies reported 13 types of BCTs, while the non‐effective studies reported 10 BCTs types shown in Table 4. The average number of BCTs used per effective study was 6.4, while the average for non‐effective studies was six. Of the 40 BCTs, only 13 were used in the included studies, regardless of their effectiveness; 27 BCTs were not mentioned in the reviewed studies.
TABLE 4.
Behavior change techniques (BCTs) in studies based on effectiveness
| BCTs | Frequency of studies that used BCTs in effective studies | Frequency of studies that used BCTs in non‐effective studies |
|---|---|---|
| Provide information on consequences of behavior in general | 19 | 7 |
| Goal setting (outcome) | 18 | 5 |
| Prompt self‐monitoring of behavioral outcome | 18 | 5 |
| Plan social support/social change | 18 | 4 |
| Provide feedback on performance | 16 | 6 |
| Teach to use prompts/cues | 12 | 4 |
| Provide information on consequences of behavior to the individual | 10 | 5 |
| Environmental restructuring | 9 | 4 |
| Goal setting (behavior) | 8 | — |
| Provide instruction on how to perform the behavior | 7 | 2 |
| Provide information on where and when to perform the behavior | 6 | — |
| Model/Demonstrate the behavior | 5 | — |
| Prompt self‐monitoring of behavior | 3 | 6 |
3.4.3. Behavior change theories
Behavior change theories are about altering habits and behaviors in long term. The theories that were reported in the reviewed studies included ecological approach, 18 theory of planned behavior, 19 , 20 social cognitive theory, 21 , 22 self‐determination theory (SDT), 23 , 24 , 25 , 26 health action process approach (HAPA), 27 social‐ecological approach, 28 , 29 goal setting theory, 26 the attributes of the diffusion of innovations model, theories of self‐efficacy and self‐regulation, 30 BASNEF model, 31 Trans theoretical Model (TTM), 5A model, 32 health belief model, 33 self‐presentation theory, 34 behavioral choice theory. 35
The behavior change theories were used in 48% (14 studies) of effective and 40% (4 studies) of non‐effective studies. Self‐determination theory (SDT) was the most frequent theory that has been used in 5 effective studies, and was not reported in any non‐effective study.
4. DISCUSSION
This systematic review was carried out to assess the workplace interventions that were designed to increase the employees' physical activity. From 39 included studies, 29 reported the effectiveness of interventions in terms of at least one outcome measure.
Four main strategies of interventions were extracted and classified as motivation and support, monitoring and feedback, information and education, and activity. Thirteen behavior change techniques were identified. Self‐determination theory (SDT) was the most frequent behavior change theory used.
In a systematic review conducted by Dugdill et al., the reviewed studies were reported in terms of the interventions' effectiveness. 36 However, in this review, strategies of interventions, behavior change techniques, and behavior change theories were also considered.
Similar to the current review, a systematic review by To et al., considered the effect of increased physical activity interventions on the improvement of outcomes such as physical activity level, steps, or BMI. The number of non‐RCTs (interventions with pre‐posttest and quasi‐experimental controlled design) that reported improvement in physical activity was higher than RCTs. In comparison, the crude number of effective RCTs reported in our study, was higher than non‐RCTs. 37
The meta‐analysis conducted by Taylor et al. evaluated the impact of theories on the effectiveness of worksite physical activity interventions, indicating that only 26% of the studies used theories and 46% used at least one behavior change theory. Furthermore, they pointed out the possible relationship between the lower use of theories and the lack of effectiveness of physical activity interventions. Theory‐based interventions were more effective, but only produced small‐sized effects on physical activity. 38 Similarly, in our study, the use of behavior change theories was more frequent in effective studies than the ineffective ones.
The findings of this review are inconsistent with evidence from earlier studies, which argued that the theoretical underpinning of interventions does not enhance intervention effectiveness. Power et al., found no difference in effectiveness between theory‐based interventions and interventions not reporting a theory usage for physical activity‐related outcomes. 39
Brennan et al. (2021) in the systematic review studied the characteristics of mother‐daughter physical activity improvement interventions, reported the BCTs separately based on the studies' effectiveness, similar to our review. In the list of BCTs reported in both reviews, “Goal setting”, “Provide instruction on how to perform the behavior”, and “Prompt self‐monitoring of behavior” were held in common. In Brennan et al., 37 different behavior change techniques were reported across the studies. Brennan et al., also mentioned that many studies use a social cognitive theory as a theoretical foundation. 40
“Provide information on consequences of behavior in general” was the most common BCT in both effective and non‐effective RCTs and non‐RCTs. In a systematic review, Malik et al., reported that the most used BCTs in workplace physical activity interventions included “Goal setting” and “Provide instruction on how to perform the behavior”. 10 In the current review, 11 of the 40 BCTs were not used at all. These unused BCTs could be considered as a potential area for research in future studies.
4.1. Strengths of this systematic review
According to our knowledge, very few systematic reviews have examined and categorized the strategies of interventions, BCTs, and behavior change theories simultaneously.
As such, this review makes a valuable contribution to this area of research. We used explicit methods to code all interventions into effective RCTs/non‐RCTs and non‐effective RCTs/non‐RCTs. To minimize reviewer errors and bias at the title and abstract screening, quality assessment, and data extraction stages, two reviewers performed these tasks and were supervised by the third researcher to solve the inconsistencies.
4.2. Limitations of this systematic review
Limitations to this review should be taken into account when interpreting the findings.
First, this review was limited to peer reviewed studies published in English and Persian. Therefore, relevant studies published in other languages or in gray literature sources may have been missed. Second, due to the nature of a systematic review, there remains a risk of publication bias, as interventions yielding a negative or non‐significant outcome are less likely to be published. Finally, due to the heterogeneity among the studies, such as the variety of workplace and participants characteristics and the type of works, studies' small sample sizes, the diversity in intervention duration and the different kinds of settings as well the different methods of measurement of physical activity, a meta‐analysis was not feasible.
5. CONCLUSION
In summary, this systematic review provides a comprehensive overview of studies related to workplace physical activity interventions. Our review indicates workplace‐based physical interventions may be potentially effective in increasing physical activity behaviors. In this review, the interventions of primary studies were categorized into four main strategies: information and education, activity, motivation and support, and monitoring and feedback. BCTs were extracted from the studies. Behavior change models and theories were also considered. It seems a multi‐strategy intervention increases physical activity in the workplace; “Activity” has to be one of these strategies. Behavioral change theories, especially self‐determination theory (SDT), increase the likelihood of a more effective intervention. It is also recommended that BCTs be considered in designing physical activity interventions. Finally, the number of RCTs reporting effectiveness was lower than the non‐effectiveness reporting ones. Therefore, conducting well‐designed RCTs to evaluate the effectiveness of worksite interventions to increase physical activity is recommended. While the studies included in this review indicate some evidence that workplace physical activity interventions can be effective, overall, the results are inconclusive, and more research is needed to ascertain which components of workplace physical activity interventions are most likely to increase effectiveness within the workplace setting.
AUTHOR CONTRIBUTIONS
Mozhdeh Ramezani, Zahra Rampisheh and Batool Tayefi had equal contribution in designing the paper. Elham Zandian and Narjes Khalili had contribution in writing search syntax and searching in databases for eligible studies. Parissa Massahikhaleghi, and Soodabeh Hoveidamanesh extracted the data, Zahra Rampisheh and Mozhdeh Ramezani re‐checked the extracted data. Zahra Rampisheh and Batool Tayefi performed the data analysis, Elham Zandian, and Neda SoleimanvandiAzar had cooperation in drafting of the manuscript, Zahra Rampisheh and Mozhdeh Ramezani provided critically important intellectual content during manuscript revisions. All authors read and approved the final manuscript and take public responsibility for their contributions to the manuscript.
FUNDING INFORMATION
This work was supported by Preventive Medicine and Public Health Research Center of the Iran University of Medical Sciences (Grant number: 1397‐2‐62‐12398).
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest. The authors alone are responsible for the content and writing of the article.
CONSENT TO PARTICIPATE
Not applicable.
INFORMATION CONSENT
Not applicable.
REGISTRY AND THE REGISTRATION NUMBER OF THE STUDY/TRIAL
Not applicable.
ANIMAL STUDIES
Not applicable.
Ramezani M, Tayefi B, Zandian E, et al. Workplace interventions for increasing physical activity in employees: A systematic review. J Occup Health. 2022;64:e12358. doi: 10.1002/1348-9585.12358
DATA AVAILABILITY STATEMENT
All data generated or analyzed during the current study are available from the corresponding author on reasonable request.
REFERENCES
- 1. Lee I‐M, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non‐communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet. 2012;380(9838):219‐229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization Physical activity [Online]; 2020. Accessed November 21, 2021. https://www.who.int/en/news‐room/fact‐sheets/detail/physical‐activity
- 3. World Health Organization Prevalence of insufficient physical activity among adults aged 18+ years (age‐standardized estimate) [Online]; 2021. Accessed November 21, 2021. https://www.who.int/data/gho/data/indicators/indicator‐details/GHO/prevalence‐of‐insufficient‐physical‐activity‐among‐adults‐aged‐18‐years‐(age‐standardized‐estimate)‐(‐)
- 4. Ding D, Lawson KD, Kolbe‐Alexander TL, et al. The economic burden of physical inactivity: a global analysis of major non‐communicable diseases. The Lancet. 2016;388(10051):1311‐1324. [DOI] [PubMed] [Google Scholar]
- 5. (IHME), I.f.H.M.a.E GBD Compare [Online]; 2019. Accessed November 21, 2021. http://ihmeuw.org/5mr1
- 6. Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta‐analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330‐339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Proper KI, Koning M, Van der Beek AJ, Hildebrandt VH, Bosscher RJ, van Mechelen W. The effectiveness of worksite physical activity programs on physical activity, physical fitness, and health. Clin J Sport Med. 2003;13(2):106‐117. [DOI] [PubMed] [Google Scholar]
- 8. Ojo SO, Bailey DP, Chater AM, Hewson DJ. The impact of active workstations on workplace productivity and performance: a systematic review. Int J Environ Res Public Health. 2018;15(3):417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oakman J, Neupane S, Proper KI, Kinsman N, Nygård C‐H. Workplace interventions to improve work ability: a systematic review and meta‐analysis of their effectiveness. Scand J Work Environ Health. 2018;44(2):134‐146. [DOI] [PubMed] [Google Scholar]
- 10. Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19(1):149‐180. [DOI] [PubMed] [Google Scholar]
- 11. Sadeghpour A, Sadeghpour M, Hosseini M. The relationship of physical activity levels and mental health: a case study at Isfahan University of Medical Sciences, Iran. J Isfahan Med Sch. 2014;32(274):90‐101. [Google Scholar]
- 12. Ramezankhani A, Haghdoost AA, Okhovati M, Sahamkhadam N. Determinants of physical activity in the workplace: A systematic review. Razi J Med Sci. 2016;22(141):19‐29. [Google Scholar]
- 13. Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- 14. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS‐I: a tool for assessing risk of bias in non‐randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;10:1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27(3):379‐387. [DOI] [PubMed] [Google Scholar]
- 17. Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO‐RE taxonomy. Psychol Health. 2011;26(11):1479‐1498. [DOI] [PubMed] [Google Scholar]
- 18. Gilson ND, Puig‐Ribera A, McKenna J, Brown WJ, Burton NW, Cooke CB. Do walking strategies to increase physical activity reduce reported sitting in workplaces: a randomized control trial. Int J Behav Nutr Phys Act. 2009;6(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Blake H, Suggs LS, Coman E, Aguirre L, Batt ME. Active8! Technology‐based intervention to promote physical activity in hospital employees. Am J Health Promot. 2017;31(2):109‐118. [DOI] [PubMed] [Google Scholar]
- 20. McEachan RR, Lawton RJ, Jackson C, Conner M, Meads DM, West RM. Testing a workplace physical activity intervention: a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2011;8(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gazmararian JA, Elon L, Newsome K, Schild L, Jacobson KL. A randomized prospective trial of a worksite intervention program to increase physical activity. Am J Health Promot. 2013;28(1):32‐40. [DOI] [PubMed] [Google Scholar]
- 22. Keller J, Gellert P, Knoll N, Schneider M, Ernsting A. Self‐efficacy and planning as predictors of physical activity in the context of workplace health promotion. Appl Psychol Health Well Being. 2016;8(3):301‐321. [DOI] [PubMed] [Google Scholar]
- 23. Kinnafick F‐E, Thøgersen‐Ntoumani C, Duda J. The effect of need supportive text messages on motivation and physical activity behaviour. J Behav Med. 2016;39(4):574‐586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Van Hoye K, Wijtzes AI, Lefevre J, De Baere S, Boen F. Year‐round effects of a four‐week randomized controlled trial using different types of feedback on employees' physical activity. BMC Public Health. 2018;18(1):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arrogi A, Schotte A, Bogaerts A, Boen F, Seghers J. Short‐and long‐term effectiveness of a three‐month individualized need‐supportive physical activity counseling intervention at the workplace. BMC Public Health. 2017;17(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pedersen C, Halvari H, Williams GC. Worksite intervention effects on motivation, physical activity, and health: a cluster randomized controlled trial. Psychol Sport Exerc. 2018;35:171‐180. [Google Scholar]
- 27. Aittasalo M, Rinne M, Pasanen M, Kukkonen‐Harjula K, Vasankari T. Promoting walking among office employees – evaluation of a randomized controlled intervention with pedometers and e‐mail messages. BMC Public Health. 2012;12(1):403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Burn N, Norton LH, Drummond C, Norton KI. Changes in physical activity behaviour and health risk factors following a randomised controlled pilot workplace exercise intervention. Aims Public Health. 2017;4(2):189‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. De Cocker KA, De Bourdeaudhuij IM, Cardon GM. The effect of a multi‐strategy workplace physical activity intervention promoting pedometer use and step count increase. Health Educ Res. 2010;25(4):608‐619. [DOI] [PubMed] [Google Scholar]
- 30. Lin Y‐P, Lin C‐C, Chen M‐M, Lee K‐C. Short‐term efficacy of a “Sit Less, Walk More” workplace intervention on improving cardiometabolic health and work productivity in office workers. J Occup Environ Med. 2017;59(3):327‐334. [DOI] [PubMed] [Google Scholar]
- 31. Hazaveei S, Moeini B, Atogara M, Roshanaei G. The effect of educational program based on BASNEF Model on performing regular physical activity among employees women in Hamadan University of Medical Sciences. J Ilam Univ Med Sci. 2018;25(5):67‐78. [Google Scholar]
- 32. Vahedian‐Shahroodi M, Sedghi F, Lael‐monfared E. Effect of intervention counseling 5A step method based on the structure on stage of change to promote physical activity female employees in mashhad factories industrial. J Sch Public Health Inst Public Health Res. 2016;14(1):59‐70. [Google Scholar]
- 33. Butler CE, Clark BR, Burlis TL, Castillo JC, Racette SB. Physical activity for campus employees: a university worksite wellness program. J Phys Act Health. 2015;12(4):470‐476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reed JL, Cole CA, Ziss MC, et al. The impact of web‐based feedback on physical activity and cardiovascular health of nurses working in a cardiovascular setting: a randomized trial. Front Physiol. 2018;9:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gell NM, Wadsworth DD. The use of text messaging to promote physical activity in working women: a randomized controlled trial. J Phys Act Health. 2015;12(6):756‐763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dugdill L, Brettle A, Hulme C, McCluskey S, Long A. Workplace physical activity interventions: a systematic review. Int J Workplace Health Manag. 2008;1:20‐40. [Google Scholar]
- 37. To QG, Chen TT, Magnussen CG, To KG. Workplace physical activity interventions: a systematic review. Am J Health Promot. 2013;27(6):e113‐e123. [DOI] [PubMed] [Google Scholar]
- 38. Taylor N, Conner M, Lawton R. The impact of theory on the effectiveness of worksite physical activity interventions: a meta‐analysis and meta‐regression. Health Psychol Rev. 2012;6(1):33‐73. [Google Scholar]
- 39. Power BT, Kiezebrink K, Allan JL, Campbell MK. Effects of workplace‐based dietary and/or physical activity interventions for weight management targeting healthcare professionals: a systematic review of randomised controlled trials. BMC Obes. 2014;1(1):1‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Brennan C, O'Donoghue G, Hall AM, Keogh A, Matthews J. A systematic review of the intervention characteristics, and behavior change theory and techniques used in mother‐daughter interventions targeting physical activity. Prev Med. 2021;153:106764. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during the current study are available from the corresponding author on reasonable request.


