Abstract
Background
Chronic cough (CC) is a common condition, but the burden of CC in general populations remains largely unknown. This study aims to investigate the disease prevalence and burden among community-based CC patients in South Korea and Taiwan, using structured tools.
Methods
A population-based cross-sectional study uses data from the 2020 South Korea and Taiwan National Health and Wellness Survey (NHWS) as well as a CC survey conducted between January–February 2020 and March–April 2020, respectively. Health outcome measures included health-related quality of life (HRQoL), health state utilities, work productivity and activity impairment (WPAI), and measurement of depression, anxiety, and insomnia among CC patients.
Results
The weighted lifetime and 12-month prevalence of CC was 6.20% and 4.34% in South Korea, and 8.27% and 5.55% in Taiwan. Compared to matched non-CC controls, CC patients reported poorer HRQoL (SF-12v2) in terms of physical component summary (PCS) score (South Korea: 47.69 ± 7.68 vs. 50.08 ± 7.29; Taiwan: 48.58 ± 7.15 vs. 50.50 ± 7.30) and mental component summary (MCS) score (44.15 ± 8.85 vs. 46.28 ± 8.50; 42.44 ± 7.78 vs. 44.60 ± 8.08), health state utilities EQ-5D index (0.73 ± 0.23 vs. 0.82 ± 0.16; 0.82 ± 0.13 vs. 0.86 ± 0.14), and more visits to healthcare professionals (7.80 vs. 4.61; 6.09 vs. 4.20) (p < 0.05). In terms of WPAI, CC patients reported higher impairments in presenteeism (32.8% vs. 21.0%; 25.9% vs. 19.4%), total work productivity (36.2% vs. 22.3%; 27.7% vs. 20.6%), and total activity (34.2% vs. 23.2%; 27.7% vs. 20.3%) than non-CC controls (p < 0.001). CC patients in South Korea and Taiwan experienced anxiety, depression, and insomnia more than non-CC controls. Poorer health outcomes were associated with the severity of CC. Patients with severe CC (visual analogue scale [VAS]>4) in both nations reported lower PCS score (45.80 vs. 49.48; 47.41 vs. 49.22) and higher absenteeism (8.5% vs. 3.6%; 5.5% vs. 1.8%) than patients with mild CC (VAS≤4) (p < 0.05).
Conclusions
The findings revealed that the disease burden of CC in general populations of South Korea and Taiwan is considerable with a negative impact on the overall quality of life, social and work life, and psychological comorbidities and is significantly associated with increased severity of the CC. There is an unmet need for further treatment interventions for CC patients to relieve the burden of CC in both nations.
Keywords: Chronic cough, Prevalence, HRQoL, Work productivity and activity impairment, Cough severity
Introduction
Cough is a physiological reflex and is a prevalent condition presented in patients seeking care from primary care globally.1 Chronic cough (CC) is typically defined as a cough persisting for a duration of at least 8 weeks.1, 2, 3
Meta-analysis of prior studies estimated the global prevalence of CC at 9.6%, with higher regional prevalence observed in Oceania (18.1%), Europe (12.7%), and United States (11.0%).4 On the other hand, CC prevalence in Asia and Africa were gauged at 4.4% and 2.3% respectively.4 According to epidemiological studies, the prevalence of CC in East Asia was 2–5%.5 A nationwide study in South Korea showed that the point prevalence of CC was approximately 2.6% among adults aged 18 years and older.6 Another study found that the prevalence of CC among Korean elderly (≥65 years) was 4.6%.7 In Taiwan, a nationwide survey conducted in 2001 in paid employees aged 25–65 years revealed that the prevalence of CC with phlegm during the past 12 months was 3.1%.8
Studies have shown the negative impact of CC on patients’ quality of life.9, 10, 11, 12 The Korean National Health and Nutrition Examination Survey (KNHANES) 2010–2016 revealed that Korean adults (≥40 years) who have CC experienced reduced health-related quality of life (HRQoL) as compared to non-CC adults.13 Another study assessing the impact of cough among Korean patients reported that CC disrupted their daily lives and relationships with family and friends.14 Also, CC is significantly associated with depression.15 In Taiwan, there have been indirect associations of CC with the quality of life.16,17 The Asia-Pacific Burden of Respiratory Disease (APBORD) study showed that cough associated with chronic respiratory diseases such as asthma, allergic rhinitis, chronic obstructive pulmonary disease and rhinosinusitis demonstrated a greater burden on work productivity and activity impairment.17
However, there is scarcity of data on the impact and disease burden of CC. Given the high prevalence, there is a need to better understand the epidemiology of CC as well as the estimated disease burden among CC patients in South Korea and Taiwan. Herein, the study aims to investigate the prevalence of CC and examine the impact of CC on the HRQoL, work productivity and activity impairment (WPAI), healthcare resource utilization (HRU) in large community-based populations of South Korea and Taiwan at a national level. In addition, a secondary objective is to compare the impact of cough severity on the health outcomes among patients with CC.
Methods
This is a population-based cross-sectional study, including the 2020 South Korea and Taiwan National Health and Wellness Survey (NHWS) as well as a CC survey. Both the NHWS surveys and the CC survey were approved by the Pearl Pathways Institutional Review Board (IN, US; #19-KANT-211). The NHWS survey was conducted from January to February 2020, while the CC survey was conducted from March to April 2020. All respondents provided informed consent prior to participating.
Study population
The 2020 South Korea and Taiwan NHWS were cross-sectional surveys collecting self-reported patient characteristics, disease status, and patient reported outcomes from adult respondents. In South Korea and Taiwan, potential respondents to the NHWS were recruited through an existing, general-purpose (ie, not health care-specific) web-based consumer panel. All panelists explicitly agreed to be a panel member. While recruiting respondents for the NHWS, a stratified random sampling procedure, with strata by sex and age, was implemented to ensure that the demographic composition of the NHWS respondents is representative of the respective adult population in South Korea and Taiwan.
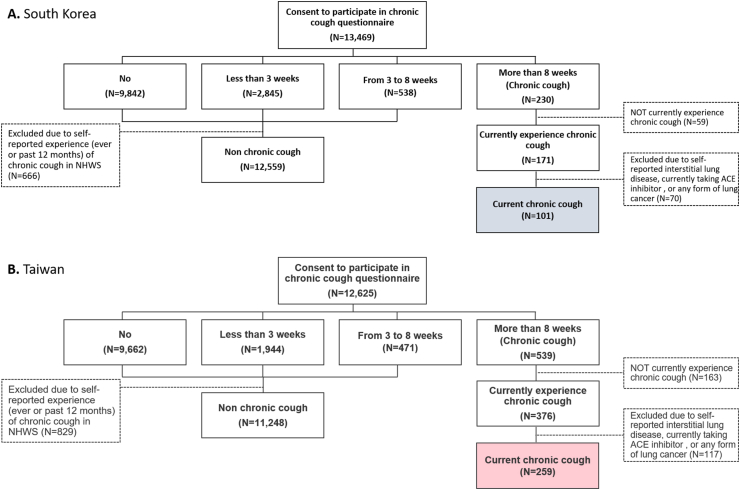
All respondents who completed the NHWS 2020 in South Korea and Taiwan were invited to participate in a CC survey to further understand their experience with CC if they fulfill the inclusion and exclusion criteria. The distribution of the respondents is detailed in Fig. 1. The inclusion criterion for participation: self-reporting coughing daily for ≥8 weeks in the past 12 months and is currently coughing at the time of survey. Respondents were excluded if they self-reported any form of lung cancer, having interstitial lung disease, and currently taking an angiotensin converting enzyme (ACE) inhibitor.
Fig. 1.
Respondent flow chart in (A) South Korea and (B) Taiwan.
Based on responses to the CC survey, current CC patients who were coughing at the time of the survey were further identified from respondents self-reporting CC in the past 12 months (hereafter, CC patients). Non-CC controls were defined as subjects who reported not coughing for ≥8 weeks in the past 12 months in the CC survey and not reported experiencing CC in the NHWS. CC patients were further divided into subgroups based on their cough severity as measured by a 0–10 visual analogue scale (VAS), ie, 0 is indicative of no cough to 10 being indicative of extremely severe cough. Individuals with VAS>4 are considered to have more severe CC.18
Outcomes and covariates collected from NHWS
Demographic measures included age, gender, employment status, household income, marital status, and level of education of all respondents.
General health characteristics included body mass index (BMI), smoking status, alcohol use, and exercise behavior and Charlson Comorbidity Index (CCI). The CCI weights the presence and seriousness of chronic comorbid diseases. An adapted version of the CCI was created excluding chronic pulmonary disease from the index score,19 as chronic cough can be frequently caused or the burden can be confounded by chronic pulmonary disease.1 Higher index indicates greater comorbid burden.19, 20, 21
Health outcomes including HRQoL, health state utilities, and WPAI were determined among current CC patients (ie, respondents with self-reported experiencing CC at the time of the study).
HRQoL was assessed by 12-Item Short Form Survey Instrument (SF-12v2). SF-12v2 is a multipurpose, generic HRQoL validated instrument comprising of 12 questions.22 The instrument reports 2 summary scores: physical component summary (PCS) and mental component summary (MCS) scores. The PCS and MCS scores are norm-based scores with higher scores indicate better quality of life. Health state utilities was generated from SF-12v2 through application of the SF-6D algorithm which takes 6 domains from the SF-12v2 22. The SF-6D is a single index measure for health using general population values. The SF-6D health utilities score is on a theoretical 0–1 scale. EQ-5D-5L instrument is a standardized measure of health status to provide a simple, generic measure of health.23 It provides a single summary index with higher scores indicate better health status. Market-specific norms were used to generate health state utilities in South Korea and Taiwan.24 Higher scores indicate better HRQoL.
The WPAI questionnaire was used to measure the impact of health on employment-related and general activities. It is a six-item validated instrument that consists of 4 metrics: absenteeism (the percentage of work time missed because of one's health in the past 7 days), presenteeism (the percentage of impairment experienced because of one's health while at work in the past 7 days), total work productivity loss (an overall impairment estimate that is a combination of absenteeism and presenteeism), and activity impairment (the percentage of impairment in daily activities because of one's health in the past 7 days).25 These 4 subscales are generated in the form of percentages, with higher values indicating greater impairment. Only respondents who reported being full-time, part-time, or self-employed provided data for absenteeism, presenteeism, and total work impairment. All respondents provided data for activity impairment.
HRU was quantified by the total number of visits to healthcare providers visits in the past 6 months (including but not limited to general practitioner, nurse practitioner/physician assistant, other traditional healthcare provider, pulmonologist, or allergist). Psychological comorbidities measured in this study included self-reported experience of anxiety, depression, and insomnia in the past 12 months.
Statistical analysis
Prevalence of CC in South Korea and Taiwan was analyzed and reported descriptively, using the responses from the NHWS, with the total number of respondents to the NHWS used as the denominator. The numerators for the respective prevalence are defined as:
-
-
Lifetime prevalence: total number of respondents who self-reported ever experienced CC
-
-
12-month prevalence: total number of respondents who self-reported experienced CC in the past 12 months
-
-
Prevalence of respondents being previously diagnosed by a physician: total number of respondents who self-reported receiving a diagnosis from a physician to have CC.
Prevalence was also calculated using the same methodology for the subgroups: i) gender: male and female; ii) age group: 18–29, 30–39, 40–49, 50–64, and ≥65, and iii) smoking status: never, former, and current. Using responses from the NHWS, the weighted prevalence was generated after weighting using gender and age to project to the entire adult population in the respective nations.
Bivariate comparison of demographic and health characteristics, as well as health outcomes between non-CC controls and CC patients were performed using chi-square tests for categorical variables and one-way analysis of variance (ANOVA) for continuous variables, to understand the baseline differences between the two groups.
Propensity score matching using a greedy matching algorithm was conducted to address baseline differences in patient characteristics as well as unequal sample sizes between non-CC controls and CC patients. Patients with CC were 1:3 propensity score matched to respondents without CC. Covariates included in the matching were: age, gender, employment status, household income, marital status, level of education, adapted CCI, BMI, smoking status, use of alcohol, and exercise behavior. Post-matching bivariate analyses were conducted to assess the balance of matching.
Among CC patients, multivariate comparisons of HRQoL, WPAI, HRU and comorbidities were conducted between mild and severe CC patients using generalized linear models (GLMs). Regression models were conducted between the subgroups controlling for covariates. Age, gender, and adapted CCI were included as covariates. GLMs specifying normal distributions and identity link functions were used for predicting normally distributed outcomes (eg, HRQoL metrics) and GLMs specifying negative binomial distributions with log link functions were used for predicting discrete, count-like outcomes with skewed distribution (eg, WPAI and HRU). GLMs specifying binomial distribution with logit link functions were used for predicting binary outcomes (eg, experience of comorbidities).
Results
Participants
The 2020 NHWS survey was completed by 20 108 respondents in South Korea and 20 050 in Taiwan. Among the 20 108 respondents who completed NHWS in South Korea, 13 469 consented to participate in the CC questionnaire and were screened. There were 230 respondents in South Korea with self-reported coughing of ≥8 weeks; among them, 59 were excluded due to not currently experiencing CC, while 70 were excluded due to self-reported interstitial lung disease or any form of lung cancer, or currently taking ACE inhibitor. A total of 101 eligible current CC patients were identified and completed the CC questionnaire, while 12 559 respondents were identified as non-CC controls (Fig. 1A).
Among the 20 050 respondents who completed NHWS in Taiwan, 12 625 consented to participate in the CC questionnaire and were screened. Among 539 respondents in Taiwan with self-reported coughing of ≥8 weeks, 163 were excluded due to not currently experiencing CC, while 117 were excluded due to self-reported interstitial lung disease or any form of lung cancer, or currently taking ACE inhibitor. A total of 259 eligible current CC patients were identified and completed the CC questionnaire, while 11 248 respondents were identified as non-CC controls (Fig. 1B).
Among CC patients in South Korea, 58 patients were considered mild CC patients while 43 were considered severe based on their cough severity VAS. Among CC patients in Taiwan, 153 were considered mild and 106 severe.
Prevalence
The weighted lifetime prevalence of CC was found to be 6.20% and 8.27% in South Korea and Taiwan, respectively. The weighted 12-month prevalence of CC was found to be 4.34% and 5.55% in South Korea and Taiwan, respectively (Table 1).
Table 1.
Weighted prevalence estimates for CC in South Korea and Taiwan.
| Weighted lifetime prevalence |
Weighted 12-month prevalence |
Weighted diagnosed by physiciana |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | Total | Prevalence | Count | Total | Prevalence | Count | Total | Prevalence | |||
| South Korea | All respondents | 2,699,149 | 43,525,439 | 6.20% | 1,888,430 | 43,525,439 | 4.34% | 805,399 | 43,525,439 | 1.85% | |
| Gender | Male | 1,168,960 | 21,694,290 | 5.39% | 820,054 | 21,694,290 | 3.78% | 320,031 | 21,694,290 | 1.48% | |
| Female | 1,530,189 | 21,831,149 | 7.01% | 1,068,376 | 21,831,149 | 4.89% | 485,368 | 21,831,149 | 2.22% | ||
| Age group | 18–29 | 419,408 | 8,126,032 | 5.16% | 308,924 | 8,126,032 | 3.80% | 136,784 | 8,126,032 | 1.68% | |
| 30–39 | 518,128 | 7,461,814 | 6.94% | 358,050 | 7,461,814 | 4.80% | 144,907 | 7,461,814 | 1.94% | ||
| 40–49 | 427,757 | 8,103,835 | 5.28% | 306,466 | 8,103,835 | 3.78% | 109,961 | 8,103,835 | 1.36% | ||
| 50–64 | 534,578 | 12,013,068 | 4.45% | 370,710 | 12,013,068 | 3.09% | 167,949 | 12,013,068 | 1.40% | ||
| 65+ | 799,278 | 7,820,690 | 10.22% | 544,280 | 7,820,690 | 6.96% | 245,798 | 7,820,690 | 3.14% | ||
| Smoking status | Never | 1,552,470 | 27,333,551 | 5.68% | 1,057,423 | 27,333,551 | 3.87% | 487,175 | 27,333,551 | 1.78% | |
| Former | 363,692 | 6,630,833 | 5.48% | 246,088 | 6,630,833 | 3.71% | 106,170 | 6,630,833 | 1.60% | ||
| Current | 782,987 | 9,561,055 | 8.19% | 584,919 | 9,561,055 | 6.12% | 212,054 | 9,561,055 | 2.22% | ||
| Taiwan | All respondents | 1,645,458 | 19,904,827 | 8.27% | 1,105,221 | 19,904,827 | 5.55% | 547,145 | 19,904,827 | 2.75% | |
| Gender | Male | 795,134 | 9,757,795 | 8.15% | 510,727 | 9,757,795 | 5.23% | 242,987 | 9,757,795 | 2.49% | |
| Female | 850,324 | 10,147,032 | 8.38% | 594,494 | 10,147,032 | 5.86% | 304,158 | 10,147,032 | 3.00% | ||
| Age group | 18–29 | 220,260 | 3,740,236 | 5.89% | 139,468 | 3,740,236 | 3.73% | 69,516 | 3,740,236 | 1.86% | |
| 30–39 | 296,656 | 3,655,120 | 8.12% | 225,378 | 3,655,120 | 6.17% | 99,492 | 3,655,120 | 2.72% | ||
| 40–49 | 269,134 | 3,704,665 | 7.26% | 175,401 | 3,704,665 | 4.73% | 87,932 | 3,704,665 | 2.37% | ||
| 50–64 | 397,178 | 5,262,420 | 7.55% | 255,348 | 5,262,420 | 4.85% | 121,916 | 5,262,420 | 2.32% | ||
| 65+ | 462,230 | 3,542,386 | 13.05% | 309,626 | 3,542,386 | 8.74% | 168,289 | 3,542,386 | 4.75% | ||
| Smoking status | Never | 1,190,853 | 15,884,437 | 7.50% | 795,340 | 15,884,437 | 5.01% | 418,720 | 15,884,437 | 2.64% | |
| Former | 194,156 | 1,995,627 | 9.73% | 132,606 | 1,995,627 | 6.64% | 55,291 | 1,995,627 | 2.77% | ||
| Current | 260,449 | 2,024,763 | 12.86% | 177,275 | 2,024,763 | 8.76% | 73,134 | 2,024,763 | 3.61% | ||
CC, chronic cough.
Weighted diagnosed by physician is defined as the weighted prevalence of CC patients who had been diagnosed by a physician for their CC condition
Based on the responses from the NWHS, 1.85% and 2.75% of respondents in South Korea and Taiwan, respectively, had self-reported to have received a physician diagnosis of having CC (Table 1). In both nations, CC was found most prevalent in age ≥65 group (weighted 12-month prevalence: 6.96% in South Korea; 8.74% in Taiwan), and among current smokers (6.12% in South Korea; 8.76% in Taiwan).
Demographic and health characteristics in non-CC controls versus CC patients
Comparisons between non-CC controls and CC patients showed that CC patients had significantly higher comorbid burden measured by the adapted CCI (0.31 vs. 0.16) and were more often currently smoking (31.7% vs. 22.6%) than non-CC controls in South Korea (Table 2). However, in Taiwan, CC patients were found to be older (48.69 vs. 44.71), more often male (54.8% vs. 48.0%), currently smoking (17.0% vs. 9.0%), and had higher adapted CCI (0.39 vs. 0.23), compared to non-CC controls (Table 2).
Table 2.
Demographics and health characteristics of non-CC controls and CC patients in South Korea and Taiwan.
| South Korea |
Taiwan |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-CC (N = 12,559) |
CC patients (N = 101) |
Non-CC vs. CC P-value |
Non-CC (N = 11,248) |
CC patients (N = 259) |
Non-CC vs. CC P-value |
||||||
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||||||||
| Age | 45.21 ± 14.31 | 43.93 ± 13.99 | 0.372 | 44.71 ± 14.38 | 48.69 ± 14.35 | <0.001 | |||||
| Charlson Comorbidity index | 0.17 ± 0.49 | 0.42 ± 0.86 | <0.001 | 0.25 ± 0.62 | 0.52 ± 0.77 | <0.001 | |||||
| Adapted Charlson Comorbidity index | 0.16 ± 0.47 | 0.31 ± 0.78 | 0.002 | 0.23 ± 0.61 | 0.39 ± 0.70 | <0.001 | |||||
| % | Count | % | Count | P-value | % | Count | % | Count | P-value | ||
| Gender | Male | 49.9% | 6268 | 44.6% | 45 | 0.284 | 48.0% | 5398 | 54.8% | 142 | 0.030 |
| Female | 50.1% | 6291 | 55.4% | 56 | 52.0% | 5850 | 45.2% | 117 | |||
| Currently employed | No | 30.5% | 3828 | 25.7% | 26 | 0.303 | 24.4% | 2740 | 24.3% | 63 | 0.989 |
| Yes | 69.5% | 8731 | 74.3% | 75 | 75.6% | 8508 | 75.7% | 196 | |||
| Level of education | University degree | 61.4% | 7708 | 62.4% | 63 | 0.837 | 61.2% | 6887 | 58.3% | 151 | 0.339 |
| Not/Decline to answer | 38.6% | 4851 | 37.6% | 38 | 38.8% | 4361 | 41.7% | 108 | |||
| BMI category | Underweight (BMI<18.5) | 6.6% | 833 | 5.9% | 6 | 0.675 | 6.8% | 766 | 3.1% | 8 | 0.025 |
| Normal weight (18.5 ≤ BMI<23) | 42.5% | 5342 | 49.5% | 50 | 38.6% | 4347 | 37.1% | 96 | |||
| Overweight (23 ≤ BMI<25) | 21.1% | 2655 | 16.8% | 17 | 19.0% | 2139 | 22.0% | 57 | |||
| Obese (BMI≥25) | 24.8% | 3109 | 23.8% | 24 | 30.5% | 3430 | 35.1% | 91 | |||
| Decline to answer | 4.9% | 620 | 4.0% | 4 | 5.0% | 566 | 2.7% | 7 | |||
| Smoking status | Never | 60.6% | 7615 | 53.5% | 54 | 0.093 | 81.0% | 9114 | 69.9% | 181 | <0.001 |
| Former | 16.8% | 2109 | 14.9% | 15 | 10.0% | 1124 | 13.1% | 34 | |||
| Current | 22.6% | 2835 | 31.7% | 32 | 9.0% | 1010 | 17.0% | 44 | |||
| Use of alcohol | Abstain | 28.5% | 3576 | 27.7% | 28 | 0.868 | 55.5% | 6246 | 50.6% | 131 | 0.113 |
| Currently consume alcohol | 71.5% | 8983 | 72.3% | 73 | 44.5% | 5002 | 49.4% | 128 | |||
| Vigorous exercise in past 30 days | No | 33.4% | 4198 | 42.6% | 43 | 0.052 | 36.5% | 4102 | 37.1% | 96 | 0.844 |
| Yes | 66.6% | 8361 | 57.4% | 58 | 63.5% | 7146 | 62.9% | 163 | |||
CC, chronic cough; SD, standard deviation
Outcome assessment in matched non-CC controls versus CC patients
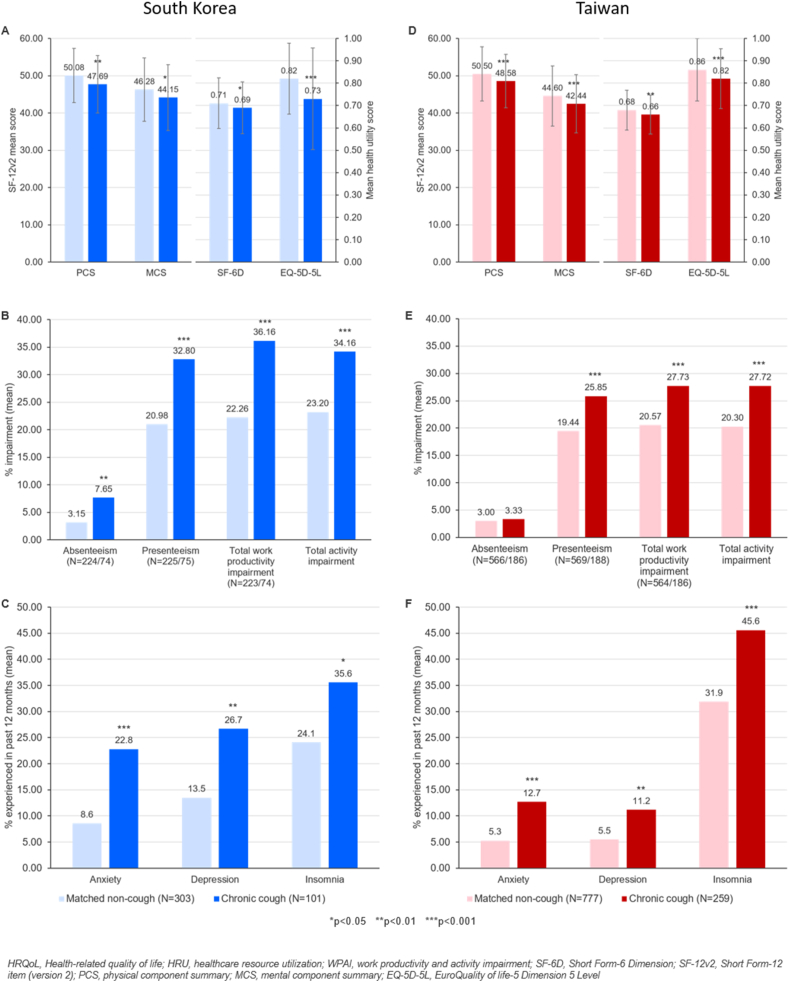
After 1:3 propensity score matching, a total of 303 and 777 matched non-CC controls in South Korea and Taiwan, respectively, were identified (Supplementary Table 1). Patients with CC reported significantly poorer HRQoL relative to matched non-CC controls, in terms of PCS score (47.69 ± 7.68 vs. 50.08 ± 7.29, mean ± standard deviation, p < 0.01), MCS score (44.15 ± 8.85 vs. 46.28 ± 8.50, p < 0.05) of SF-12v2, SF-6D (0.69 ± 0.12 vs. 0.71 ± 0.11, p < 0.05) and EQ-5D-5L (0.73 ± 0.23 vs. 0.82 ± 0.16, p < 0.001) scores in South Korea (Fig. 2A).
Fig. 2.
Comparison of HRQoL, WPAI, HRU and other symptoms experienced in matched non-CC controls and CC patients in South Korea (left panel – (A-C)) and Taiwan (right panel – (D-F)). Health-related quality of life (HRQoL) experienced in matched CC controls and CC patients in (A) South Korea and (D) Taiwan; Work productivity and activity impairment (WPAI) experienced by non-CC controls and CC patients in (B) South Korea and (E) Taiwan; Proportion of non-CC controls and CC patients experiencing anxiety, depression, insomnia in (C) South Korea and (F) Taiwan.
CC patients in South Korea reported significantly greater impairment in absenteeism (7.7% vs. 3.2%, p < 0.01), presenteeism (32.8% vs. 21.0%, p < 0.001), total work productivity (36.2% vs. 22.3%, p < 0.001) and total activity (34.2% vs. 23.2%, p < 0.001), compared to matched non-CC controls (Fig. 2B). Compared to matched non-CC controls, CC patients had significantly more visits to the healthcare professional (HCP) (7.80 vs. 4.61, p < 0.01) and reported higher proportion of experience anxiety (22.8% vs. 8.6%, p < 0.001), depression (26.7% vs. 13.5%, p < 0.01), and insomnia (35.6% vs. 24.1%, p < 0.05) in South Korea (Fig. 2C).
In Taiwan, similarly, CC patients experienced significantly poorer HRQoL in terms of PCS score (48.58 ± 7.15 vs. 50.50 ± 7.30, p < 0.001), MCS score (42.44 ± 7.78 vs. 44.60 ± 8.08, p < 0.001), SF-6D (0.66 ± 0.09 vs. 0.68 ± 0.09, p < 0.01) and EQ-5D-5L (0.82 ± 0.13 vs. 0.86 ± 0.14, p < 0.001) health utilities, compared to matched non-CC controls (Fig. 2D). CC patients in Taiwan reported significantly greater impairment in presenteeism (25.9% vs. 19.4%, p < 0.001), total work productivity impairment (27.7% vs. 20.6%, p < 0.001) and total activity impairment (27.7% vs. 20.3%, p < 0.001) than matched non-CC controls (Fig. 2E). CC patients also had significantly more visits to the HCP (6.09 vs. 4.20, p < 0.001) and reported significantly higher proportion of experience anxiety (12.7% vs. 5.3%, p < 0.001), depression (11.2% vs. 5.5%, p < 0.01) and insomnia (45.6% vs. 31.9%, p < 0.001), compared to matched non-CC controls in Taiwan (Fig. 2F).
Outcome assessment in mild vs. severe CC patients
Among CC patients in South Korea, patients with severe CC (VAS>4) reported significantly poorer PCS score (45.80 vs 49.48, p < 0.01) and EQ-5D-5L scores (0.67 vs 0.77, p < 0.05), significantly higher impairment in terms of absenteeism (8.5% vs 3.6%, p < 0.05), and significantly greater number of visits to the HCPs (10.13 vs 4.96, p < 0.01), compared to mild CC (VAS≤4) patients. Additionally, severe CC patients also reported significantly more depression (39.8% vs 16.5%, p < 0.05) compared to mild CC patients (Table 3).
Table 3.
HRQoL, WPAI, HRU and comorbidities among mild and severe CC patients in South Korea and Taiwan.
| South Korea (N = 101) |
|||||
|---|---|---|---|---|---|
| Mild CC (VAS≤4) (N = 58) |
Severe CC (VAS>4) (N = 43) |
P-value | |||
| Mean | 95% LCL–95% UCL | Mean | 95% LCL–95% UCL | ||
| HRQoL | |||||
| Physical Component Summary Score | 49.48 | 47.77–51.19 | 45.80 | 43.82–47.78 | 0.006 |
| Mental Component Summary Score | 44.95 | 42.70–47.20 | 43.15 | 40.55–45.75 | 0.303 |
| SF-6D Health Utilities Score | 0.69 | 0.67–0.72 | 0.68 | 0.65–0.71 | 0.500 |
| EQ-5D-5L Health Utilities Score | 0.77 | 0.71–0.82 | 0.67 | 0.61–0.74 | 0.030 |
| WPAI | |||||
| Absenteeism (N = 42/32) | 3.6% | 2.1%–6.2% | 8.5% | 4.7%–15.5% | 0.047 |
| Presenteeism (N = 42/33) | 29.8% | 23.0%–38.8% | 33.7% | 25.1%–45.4% | 0.550 |
| Total work productivity impairment (N = 42/32) | 31.8% | 24.6%–41.1% | 37.9% | 28.2%–50.9% | 0.392 |
| Total activity Impairment | 30.0% | 24.3%–37.1% | 37.3% | 29.4%–47.4% | 0.184 |
| HRU | |||||
| No. of HCP visits in past 6 months | 4.96 | 3.56–6.91 | 10.13 | 7.04–14.57 | 0.004 |
| Psychological comorbidities | |||||
| Anxiety in past 12 months | 14.1% | 6.7%–27.2% | 28.0% | 15.5%–45.0% | 0.115 |
| Depression in past 12 months | 16.5% | 8.4%–29.9% | 39.8% | 25.2%–56.5% | 0.020 |
| Insomnia in past 12 months | 29.6% | 18.6%–43.6% | 41.0% | 26.7%–57.0% | 0.264 |
| Taiwan (N=259) | |||||
| Mild CC (VAS≤4) (N=153) | Severe CC (VAS>4) (N=106) | P-value | |||
|
Mean SE |
95% LCL–95% UCL |
Mean SE |
95% LCL–95% UCL | ||
| HRQoL | |||||
| Physical Component Summary Score | 49.22 | 48.17–50.26 | 47.41 | 46.17–48.65 | 0.029 |
| Mental Component Summary Score | 42.73 | 41.50–43.96 | 41.80 | 40.34–43.26 | 0.341 |
| SF-6D Health Utilities Score | 0.66 | 0.65–0.68 | 0.65 | 0.63–0.66 | 0.061 |
| EQ-5D-5L Health Utilities Score | 0.83 | 0.81–0.85 | 0.80 | 0.77–0.82 | 0.103 |
| WPAI | |||||
| Absenteeism (N = 108/78) | 1.8% | 1.1%–3.2% | 5.5% | 2.9%–10.5% | 0.016 |
| Presenteeism (N = 109/79) | 23.8% | 20.1%–28.2% | 29.1% | 24.0%–35.3% | 0.129 |
| Total work productivity impairment (N = 108/78) | 25.4% | 21.6%–30.0% | 31.5% | 26.0%–38.1% | 0.097 |
| Total activity Impairment | 24.1% | 21.0%–27.7% | 32.7% | 27.7%–38.5% | 0.006 |
| HRU | |||||
| No. of HCP visits in past 6 months | 5.33 | 4.48–6.34 | 6.83 | 5.57–8.37 | 0.071 |
| Psychological comorbidities | |||||
| Anxiety in past 12 months | 9.4% | 5.7%–15.1% | 15.5% | 9.7%–23.7% | 0.134 |
| Depression in past 12 months | 8.8% | 5.0%–15.0% | 13.7% | 8.0%–22.3% | 0.242 |
| Insomnia in past 12 months | 44.8% | 36.8%–53.1% | 48.9% | 39.1%–58.7% | 0.537 |
CC, chronic cough; EQ-5D-5L, EuroQuality of life-5 Dimension 5 Level; HCP, healthcare professions; HRQoL, health-related quality of life; HRU, healthcare resource utilization; LCI, lower confidence interval; SE, standard error; SF-6D, Short-Form Six-Dimension; UCI, upper confidence interval; VAS, visual analog scale; WPAI, work productivity and activity impairment
Among CC patients in Taiwan, after adjusting for potential confounders, severe CC patients reported significantly poorer PCS score (47.41 vs. 49.22, p < 0.05), significantly higher impairment in terms of absenteeism (5.5% vs. 1.8%, p < 0.05) and total activity impairment (32.7% vs. 24.1%, p < 0.01) (Table 3).
Discussion
To our knowledge, this is the first study to determine the 12-month period prevalence of CC as well as the disease burden, using various structured tools including WPAI, in relation to cough severity in South Korea and Taiwan. Results of the study showed that the prevalence of CC was 4.34%–5.55% and CC have a substantial impact on the quality of life in both nations. The CC prevalence reported in this study was comparable to the previously estimated regional CC prevalence in Asia (4.4%).4
Interestingly, the lifetime and 12-month prevalence of CC in Taiwan (8.27%, 5.55%) are higher than in South Korea (6.20%, 4.34%). While reasons for the difference are not clear, obesity might be one of candidate factors, as the prevalence of obesity (BMI≥25) was higher in Taiwanese (Table 2). Meanwhile, consistent with previous studies on CC prevalence, CC was observed to be most prevalent in elderly (≥65 years)26 and among current smokers5,27 in both nations.
The poorer HRQoL among CC patients is generally in accordance with previous studies.13,14,17,28, 29, 30 However, WPAI scores and healthcare use have not been previously reported. In both nations, CC patients had higher comorbid burden, poorer physical and mental summary scores (PCS and MCS), poorer general health scores (SF-6D and EQ-5D-5L), higher WPAI and more visits to HCPs. The WPAI scores in the present study indicated that most of the patients still attended work with their illness but had severely impacted work productivity and activity. In both nations, adults with CC experienced greater presenteeism and impairment of total work productivity and total activity. Interestingly, CC patients in South Korea experienced greater absenteeism than CC patients in Taiwan. This could be related to the increased HCP visits reported by the Korean CC patients.
Increased visitations to HCPs or emergency departments were found to be associated with CC.17,31 Patients with chronic respiratory diseases in the Asia-Pacific region, including Korea and Taiwan, indicated cough as a key symptom for frequently seeking medical care.16,32 It is also plausible with the implementation of an algorithmic approach to diagnose and manage CC1 might result in increased visits to HCPs for treatment and follow-up. Reasons for HCP visitations were not explored in this study.
Furthermore, CC patients in both nations more frequently reported anxiety, depression, and insomnia than non-CC controls. Similar to our findings, previous studies also identified that the prevalence of insomnia or sleep disturbances was significantly associated with persistent cough and other respiratory symptoms.33, 34, 35, 36 About 33% of patients with sleep-disordered breathing reportedly had chronic cough36 Disturbed sleep, anxiety and depression were also reported in more than half of the CC patients in a UK study.37 A Korean study reported that the lower overall EQ-5D-3L score among individuals with CC were more associated with anxiety or depression.13
Individuals with severe CC were found to have significantly poorer health outcomes than those with mild CC. Severe CC patients (VAS>4) had significantly lower PCS and EQ-5D scores, higher absenteeism and more visits to the HCPs as compared to patients with mild CC (VAS≤4) in Korea. Significantly higher proportion of severe CC patients in Korea also reported experiencing symptoms of depression. On the other hand, increased severity of CC resulted in significantly poorer PCS score and higher absenteeism and total activity impairment among Taiwanese CC patients than matched non-CC controls. This dose response supports the notion that cough impairs HRQoL and cough severity is a clinically important outcome to be measured in clinical practice and trials.
Overall, CC patients from South Korea had poorer health utilities score, greater WPAI, and more HCP visits than patients from Taiwan. These findings are supposedly related to different patient preferences between the two nations when seeking treatment but requires future studies.
This study provided novel insights to the prevalence and burden of CC in South Korea and Taiwan. Previously, the point prevalence of CC was only reported in a study of Koreans in 2012,6,38 but not in Taiwan. The study has another strength that it is the first study to address the associations between CC and health-related outcomes using structured measurement tools, particularly the work and activity impairment, in a large general adult population (aged ≥18 years). Cough severity and its associations with health outcomes have not been reported in general population studies of both nations.
However, there are limitations of this study. Although the NHWS is a broad representative of the Korean and Taiwanese national adult population, individuals without internet access or comfort with online administration including those with severe comorbidities and disabilities could be likely to be under-represented in this study. Moreover, the NHWS being a cross-sectional and self-reported data survey, verification of responses could not be performed to exclude recall bias; hence, no causal relationships could be conducted.
Another limitation is that sensitivity analysis in both nations could not be performed as the health outcomes of CC patients who were excluded from this study, ie, with self-reported diagnosis of lung cancer or interstitial lung diseases, or ACE inhibitor use was not explicitly explored in this study. Further investigation is warranted.
The proportion of respondents who had received a diagnosis from a physician for having CC in both nations (1.85%–2.75%) was lower than the reported 12-month prevalence (4.34%–5.55%). This highlighted a possible under-diagnosis or under-recognition of CC as a disease entity by physicians in both nations. Coughing or CC has been long associated with comorbidities such as asthma, chronic obstructive pulmonary disease, allergic rhinitis, rhinosinusitis, and gastroesophageal reflux disease (GERD). As such, diagnoses of CC could become obscured or confounded by the presence of such underlying health issues or comorbidities. There has been a paradigm change during the last decade, which views CC as a distinct clinical syndrome mainly characterized by persistent coughing and hypersensitivity, termed as cough hypersensitivity syndrome by the European Respiratory Society Task Force.1 However, there is a controversy among physicians whether CC should be considered as a disease entity (or to what extent), and the new disease concept has not been fully implemented into the healthcare system.12,39
The prevalence of comorbidities such as asthma, chronic obstructive pulmonary disease, allergic rhinitis, rhinosinusitis, and GERD, environmental factors such as pollution levels in the respondents' neighborhood or working environment as well as seasonal factors (eg, pollen season in the region) could also explain for the differences in the prevalence and patient burden observed between the 2 nations.5,40 However, associations of underlying health conditions as well as environmental factors and disease specific HRQoL were not explored in this study and the differences between nations warrant further investigation. Additionally, future studies with larger population of eligible CC patients would be needed to understand the association of respondents’ specific health characteristics (eg, BMI) and lifestyle (eg, smoking, alcohol consumption) with CC severity, as well as the overall impact on the quality of life among patients with CC.
Conclusion
This study provided up-to-date weighted prevalence estimates of CC in large community-based populations of South Korea and Taiwan. Furthermore, the study showed that CC patients in both South Korea and Taiwan experience a considerable degree of burden which has a negative impact on patients overall QoL, social and work life, or psychological comorbidities. Increased burden was found to be related to the severity of CC; whereby severe cough was significantly associated with worse QoL. These findings highlighted an unmet need for better interventions and treatment to relieve the burden of CC.
Abbreviations
ACE, angiotensin-converting enzyme; ANOVA, one-way analysis of variance; APBORD, Asia-Pacific Burden of Respiratory Disease; BMI, body mass index; CC, chronic cough; CCI, Charlson Comorbidity Index; EQ-5D, EuroQol-5 Dimension; GLMs, generalized linear models; HCP, healthcare professional; HRQoL, health-related quality of life; HRU, healthcare resource utilization; KNHANES, Korean National Health and Nutrition Examination Survey; MCS, mental component summary; NHWS, National Health and Wellness Survey; PCS, physical component summary; SF-12v2, 12-Item Short Form Survey Instrument; VAS, visual analogue scale; WPAI, work productivity and activity impairment.
Funding and acknowledgements
Cerner Enviza received funding from Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc, to conduct the study and develop the manuscript. The authors acknowledge Dr. Yirong Chen of Cerner Enviza for the support in the statistical analysis, and Dr. Amanda Woo of Cerner Enviza for providing medical writing and editorial support.
Availability of data and materials
Study data to support our findings are available from Cerner Enviza, but availability of the data is restricted and was used under license for this study and are not publicly available. Data are however available from the authors upon reasonable request and with permission of Cerner Enviza.
Statement of contribution
SH Kang contributed to the concept or design of the study. SH Kang, W-J Song, and C-J Yu contributed to the analysis or interpretation of the data, drafting of the article, and critical revision for important intellectual content. All authors had full access to the data, contributed to the study, approved the final version for publication, and take responsibility for its accuracy and integrity.
Agreement to publish
The authors confirm and provide consent for the contents in this article to be published.
Ethics statement
The 2020 National Health and Wellness Survey (NHWS) (protocol # 19-KANT-211) and CC Survey (protocol #20-KANT-215) were approved by the Pearl Pathways Institutional Review Board (Indianapolis, Indiana, USA). All respondents provided informed online consent prior to participating.
Declaration of competing interest
SH Kang is an employee of MSD, Korea. WJ Song has received research grants from MSD and AstraZeneca, consulting fees from MSD and AstraZeneca, and lecture fees from MSD, AstraZeneca, GSK, and Novartis. CJ Yu declares no conflict of interest.
Footnotes
Full list of author information is available at the end of the article
Supplementary data to this article can be found online at https://doi.org/10.1016/j.waojou.2022.100681.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Morice A.H., Millqvist E., Bieksiene K., et al. ERS guidelines on the diagnosis and treatment of chronic cough in adults and children. Eur Respir J. 2020;55(1):20. doi: 10.1183/13993003.01136-2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irwin R.S., French C.L., Chang A.B., et al. Classification of cough as a symptom in adults and management algorithms. Chest. 2018;153(1):196–209. doi: 10.1016/j.chest.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song D.J., Song W.J., Kwon J.W., et al. KAAACI evidence-based clinical practice guidelines for chronic cough in adults and children in Korea. Allergy Asthma Immunol Res. 2018;10(6):591–613. doi: 10.4168/aair.2018.10.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song W.J., Chang Y.S., Faruqi S., et al. The global epidemiology of chronic cough in adults: a systematic review and meta-analysis. Eur Respir J. 2015;45(5):1479–1481. doi: 10.1183/09031936.00218714. [DOI] [PubMed] [Google Scholar]
- 5.Song W.J., Faruqi S., Klaewsongkram J., Lee S.E., Chang Y.S. Chronic cough: an Asian perspective. Part 1: epidemiology. Asia Pac Allergy. 2015;5(3):136–144. doi: 10.5415/apallergy.2015.5.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kang M.G., Song W.J., Kim H.J., et al. Point prevalence and epidemiological characteristics of chronic cough in the general adult population: the Korean National Health and Nutrition Examination Survey 2010-2012. Medicine (Baltimore) 2017;96(13) doi: 10.1097/MD.0000000000006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song W.J., Morice A.H., Kim M.H., et al. Cough in the elderly population: relationships with multiple comorbidity. PLoS One. 2013;8(10) doi: 10.1371/journal.pone.0078081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng Y., Guo Y.L., Yeh W.Y. A national survey of psychosocial job stressors and their implications for health among working people in Taiwan. Int Arch Occup Environ Health. 2001;74(7):495–504. doi: 10.1007/s004200100254. [DOI] [PubMed] [Google Scholar]
- 9.Chamberlain S.A.F., Garrod R., Douiri A., et al. The impact of chronic cough: a cross-sectional European survey. Lung. 2015;193(3):401–408. doi: 10.1007/s00408-015-9701-2. [DOI] [PubMed] [Google Scholar]
- 10.Young E.C., Smith J.A. Quality of life in patients with chronic cough. Ther Adv Respir Dis. 2010;4(1):49–55. doi: 10.1177/1753465809358249. [DOI] [PubMed] [Google Scholar]
- 11.Bishwajit G., Tang S., Yaya S., Feng Z. Burden of asthma, dyspnea, and chronic cough in South Asia. Int J Chronic Obstr Pulm Dis. 2017;12:1093–1099. doi: 10.2147/COPD.S133148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Won H.K., Song W.J. Impact and disease burden of chronic cough. Asia Pac Allergy. 2021;11(2):e22. doi: 10.5415/apallergy.2021.11.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Won H.K., Lee J.H., An J., et al. Impact of chronic cough on health-related quality of life in the Korean adult general population: the Korean national health and nutrition examination survey 2010–2016. Allergy Asthma Immunol Res. 2020;12(6):964–979. doi: 10.4168/aair.2020.12.6.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kang S.Y., Won H.K., Lee S.M., et al. Impact of cough and unmet needs in chronic cough: a survey of patients in Korea. Lung. 2019;197(5):635–639. doi: 10.1007/s00408-019-00258-9. [DOI] [PubMed] [Google Scholar]
- 15.Sohn K.H., Song W.J., Kim S.H., Jang H.C., Kim K.W., Chang Y.S. Chronic cough, not asthma, is associated with depression in the elderly: a community-based population analysis in South Korea. Korean J Intern Med. 2019;34(6):1363–1371. doi: 10.3904/kjim.2018.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho S.H., Lin H.C., Ghoshal A.G., et al. Respiratory disease in the Asia-Pacific region: cough as a key symptom. Allergy Asthma Proc. 2016;37(2):131–140. doi: 10.2500/aap.2016.37.3925. [DOI] [PubMed] [Google Scholar]
- 17.Lin H.C., Cho S.H., Ghoshal A.G., et al. Respiratory diseases and the impact of cough in Taiwan: results from the APBORD observational study. Medicine (Baltimore) 2016;95(27) doi: 10.1097/MD.0000000000003854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kubo T., Tobe K., Okuyama K., et al. Disease burden and quality of life of patients with chronic cough in Japan: a population-based cross-sectional survey. BMJ Open Respir Res. 2021;8(1) doi: 10.1136/bmjresp-2020-000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Charlson M.E., Charlson R.E., Peterson J.C., Marinopoulos S.S., Briggs W.M., Hollenberg J.P. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol. 2008;61(12):1234–1240. doi: 10.1016/j.jclinepi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 20.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Quan H., Li B., Couris C.M., et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 22.Brazier J.E., Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42(9):851–859. doi: 10.1097/01.mlr.0000135827.18610.0d. [DOI] [PubMed] [Google Scholar]
- 23.EuroQol Group EuroQol - a new facility for the measurement of health-related quality of life. Health Pol. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 24.Shiroiwa T., Fukuda T., Ikeda S., et al. Japanese population norms for preference-based measures: EQ-5D-3L, EQ-5D-5L, and SF-6D. Qual Life Res. 2016;25:707–719. doi: 10.1007/s11136-015-1108-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Reilly M.C., Gooch K.L., Wong R.L., Kupper H., van der Heijde D. Validity, reliability and responsiveness of the work productivity and activity impairment questionnaire in ankylosing spondylitis. Rheumatol Oxf Engl. 2010;49(4):812–819. doi: 10.1093/rheumatology/kep457. [DOI] [PubMed] [Google Scholar]
- 26.Song W.J., Won H.K., An J., et al. Chronic cough in the elderly. Pulm Pharmacol Ther. 2019;56:63–68. doi: 10.1016/j.pupt.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Chung K.F., Pavord I.D. Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371(9621):1364–1374. doi: 10.1016/S0140-6736(08)60595-4. [DOI] [PubMed] [Google Scholar]
- 28.Ma W., Yu L., Wang Y., Li X., Lü H., Qiu Z. Changes in health-related quality of life and clinical implications in Chinese patients with chronic cough. Cough. 2009;5(1):7. doi: 10.1186/1745-9974-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fujimura M. Frequency of persistent cough and trends in seeking medical care and treatment-results of an internet survey. Allergol Int. 2012;61(4):573–581. doi: 10.2332/allergolint.11-OA-0368. [DOI] [PubMed] [Google Scholar]
- 30.Zeiger R.S., Schatz M., Butler R.K., Weaver J.P., Bali V., Chen W. Burden of specialist-diagnosed chronic cough in adults. J Allergy Clin Immunol Pract. 2020;8(5):1645–1657. doi: 10.1016/j.jaip.2020.01.054. e7. [DOI] [PubMed] [Google Scholar]
- 31.Wang D.Y., Ghoshal A.G., Bin Abdul Muttalif A.R., et al. Quality of life and economic burden of respiratory disease in Asia-Pacific—Asia-Pacific burden of respiratory diseases study. Value Health Reg Issues. 2016;9:72–77. doi: 10.1016/j.vhri.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Wang D.Y., Ghoshal A.G., Razak Bin Abdul M.A., Lin H.C.L., Thanaviratananich S., Bagga S., et al. Cough as a key symptom in asthma, allergic rhinitis, COPD and rhinosinusitis and its impact in Asia. Value Health. 2014;17(7):A776–A777. doi: 10.1016/j.jval.2014.08.351. [DOI] [PubMed] [Google Scholar]
- 33.Dodge R., Cline M.G., Quan S.F. The natural history of insomnia and its relationship to respiratory symptoms. Arch Intern Med. 1995;155(16):1797–1800. doi: 10.1001/archinte.1995.00430160145014. [DOI] [PubMed] [Google Scholar]
- 34.McCallion P., De Soyza A. Cough and bronchiectasis. Pulm Pharmacol Ther. 2017;47:77–83. doi: 10.1016/j.pupt.2017.04.010. [DOI] [PubMed] [Google Scholar]
- 35.Kuzniar T.J., Morgenthaler T.I., Afessa B., Lim K.G. Chronic cough from the patient's perspective. Mayo Clin Proc. 2007;82(1):56–60. doi: 10.4065/82.1.56. [DOI] [PubMed] [Google Scholar]
- 36.Chan K.K.Y., Ing A.J., Laks L., Cossa G., Rogers P., Birring S.S. Chronic cough in patients with sleep-disordered breathing. Eur Respir J. 2010;35(2):368–372. doi: 10.1183/09031936.00110409. [DOI] [PubMed] [Google Scholar]
- 37.Everett C.F., Kastelik J.A., Thompson R.H., Morice A.H. Chronic persistent cough in the community: a questionnaire survey. Cough Lond Engl. 2007;3:5. doi: 10.1186/1745-9974-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song W.J., Chang Y.S., Faruqi S., et al. Defining chronic cough: a systematic review of the epidemiological literature. Allergy Asthma Immunol Res. 2016;8(2):146–155. doi: 10.4168/aair.2016.8.2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGarvey L., Gibson P.G. What is chronic cough? Terminology. J Allergy Clin Immunol Pract. 2019;7(6):1711–1714. doi: 10.1016/j.jaip.2019.04.012. [DOI] [PubMed] [Google Scholar]
- 40.Jo E.J., Song W.J. Environmental triggers for chronic cough. Asia Pac Allergy. 2019;9(2):e16. doi: 10.5415/apallergy.2019.9.e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Study data to support our findings are available from Cerner Enviza, but availability of the data is restricted and was used under license for this study and are not publicly available. Data are however available from the authors upon reasonable request and with permission of Cerner Enviza.