Abstract
Background
People with sleep problems are more likely to have mental disorders. This study aimed to assess the effect of insomnia on the prognosis of patients with major depressive disorder (MDD).
Methods
We divided the patients into three groups according to the Insomnia Severity Index (ISI) scores. In addition, we compared the results of the Hamilton Depression Scale (HAMD) and Symptom Checklist-90 (SCL-90) scores. We evaluated the effect of insomnia at the 2nd, 4th, and 8th-week follow-up on the prognosis of MDD.
Results
Fifty-five patients between 19 and 58 years old, with a diagnosis of MDD via the Structured Clinical Interview for the Diagnostic and Statistical Manual-5 (DSM-5). The ISI scores of the moderate and severe group decreased significantly (P < 0.05) in the 2nd week compared to the baseline. The HAMD scores in all groups improved significantly in the 2nd week.
Conclusions
This study was inspired to assess insomnia as a comorbid disorder for patients with MDD, which may bring poor treatment consequences.
Keywords: Sleep disturbance, Insomnia, Major depressive disorder
Introduction
Sleep disorders afflict nearly a quarter of the global population. People with sleep problems are more likely to have mental disorders, such as bipolar disorder, generalized anxiety disorder, and especially major depressive disorder (MDD) [1]. MDD is a common mental disorder affecting more than 4% of the global population [2]. MDD is one of the most commonly diagnosed mental disorders, with a lifetime prevalence of approximately 16% [3, 4]. In many cases, sleep disorder is the main complaint of MDD [5].
Sleep disturbance is one of the most consistent symptoms associated with MDD [6]. These sleep regulation problems are not secondary to the disorders; instead, they precede depressive episodes and persist during remission. Furthermore, it has been found that depressed patients with sleep disturbance may have more severe symptoms and treatment difficulties [7]. In addition, improving sleep in patients with MDD can improve outcomes [8]. These observations suggest that it is essential for sleep medicine practitioners to realize patients with MDD and solve their sleep problems.
It is generally agreed that sleep disturbance is a symptom that can be alleviated related to the treatment of MDD. Moreover, insomnia is an important predictor of MDD recurrence and may lead to unpleasant clinical outcomes [7, 9]. It is well known that insomnia is an independent diagnostic entity, which may lead to the development of MDD [10]. Insomnia in people indicates a greater risk for MDD that persists for at least 30 years [11]. A study has confirmed the importance of insomnia as a risk factor for MDD and the necessity of early treatment of insomnia [12]. So, it is crucial to examine the role of insomnia in evaluating the prognosis of MDD.
The aim of this study was to assess the effect of insomnia on the prognosis of patients with MDD. First, we evaluated the Insomnia Severity Index (ISI), Hamilton Depression Scale (HAMD), and Symptom Checklist-90 (SCL-90) as a predictor of the effect of insomnia on MDD. ISI scale yields a total score ranging from 0 to 28. The total score is interpreted: (0–7: absence of insomnia; 8–14: slight insomnia; 15–21: moderate insomnia; and 22–28: severe insomnia [13]. The patients were divided into three groups according to the ISI scores: (8–14: slight insomnia; 15–21: moderate insomnia; 22–28: severe insomnia). In addition, we compared the results of HAMD and SCL-90 scores and evaluated the effect of insomnia at the 2nd, 4th, and 8th-week follow-up.
Method
Study design and participants
Participants were recruited from the department of psychiatry, the third people’s hospital in Foshan, China. Fifty-five patients between 19 and 58 years old with a diagnosis of MDD via the Structured Clinical Interview for the Diagnostic and Statistical Manual-5 (DSM-5). Patients under the age of 18 were excluded. The exclusion criteria of this study were active drug abuse, excessive use of sleep drugs, and other brain diseases, such as severe developmental disorder, Parkinson’s disease, and acquired brain injury.
The ISI is a self-report questionnaire used to assess the nature and severity of insomnia. The total score is divided into three grades: (8–14: slight insomnia; 15–21: moderate insomnia; 22–28: severe insomnia) [13]. HAMD is considered the standard measure of severity for MDD. Furthermore, many psychometric properties of the HAMD are reliable and consistently meet the established criteria. SCL-90 is widely used in mental health screening and the diagnosis of mental diseases. According to the ISI scores, we divided the MDD patients with insomnia into three groups: slight, moderate, and severe group.
Outcomes
All patients were assessed using ISI, HAMD, and SCL-90 scores at baseline, 2nd week, 4th week, and 8th week. We used HAMD to evaluate response and remission. The remission of depressive symptoms was defined as a final HAMD score ≤ 7. A response to treatment was defined as a 50% reduction in the scale scores between the baseline and 2nd week, 4th week, and 8th-week assessments. We assessed insomnia states using ISI scores.
Statistical analysis
For comparisons among the baseline of the slight, moderate, and severe group: age, HAMD, SCL 90, and ISI scores, one-way ANOVA was used. Categorical variables (gender, education, smoking, and educational level) were performed using χ2 tests. Regarding the predictive effect of insomnia on MDD recovery, we performed two-way ANOVA using the difference among baseline and 2nd week, 4th week, and 8th-week scores as ISI, HAMD, and SCL-90 scores. Bonferroni post hoc tests were performed to determine differences between groups. Frequency analysis χ2 was performed to assess the occurrence of remission and response. P < 0.05 was considered statistically significant, and the data are presented as mean ± standard deviation (SD). All data were analyzed with the SPSS Statistics, version 21.0 for Windows (IBM Corporation, Armonk, USA).
Patient and public involvement
No patients or the public participated in the study protocol design, specific objectives or study questions, and the design or implementation of the current study. No patients or the public participated in the interpretation of the study results or the preparation of the manuscript. There are no plans to disseminate the results of the study to participants.
Results
Participant characteristics
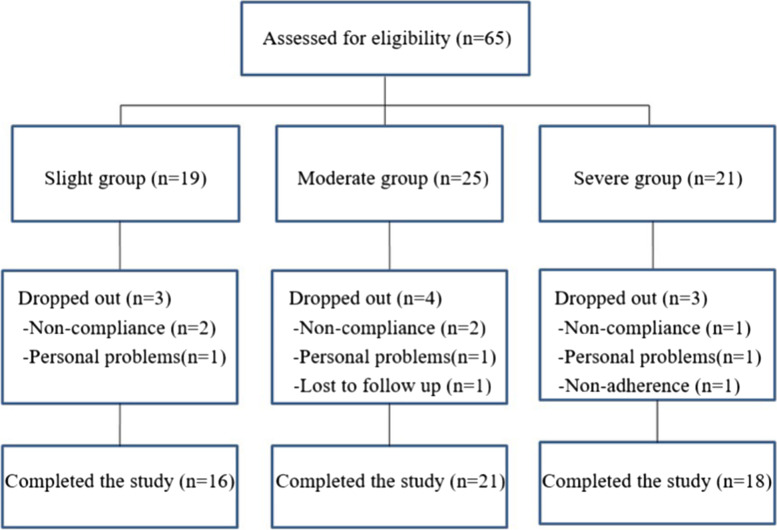
We screened 65 subjects, including slight group (n = 19), Moderate group (n = 25), and Severe group (n = 21). However, ten subjects dropped out due to non-compliance, personal problems, lack of follow up, and non-adherence to drug therapy. Ultimately, 21 men and 34 women (mean age 38.27 ± 11.47 years) were enrolled (Fig. 1).
Fig. 1.
The flow diagram of included and excluded patients
There were no significant differences among the three groups regard to age or duration of illness on HAMD. According to the patient’s condition, the medication prescription of the patients was recorded. Furthermore, there is no difference in the educational experience and smoking status. In addition, the baseline characteristics of all groups are summarized in Table 1.
Table 1.
Baseline characteristics of the participants
| Slight | Moderate | Severe | P-value | |
|---|---|---|---|---|
| Participants | 16 | 21 | 18 | |
| Age (years) | 35.16 ± 11.81 | 39.33 ± 10.95 | 39.83 ± 11.85 | 0.43 |
| Gender (M/F) | 7/9 | 8/13 | 6/12 | 0.82 |
| Education | 0.96 | |||
| Below 9 years, n (%) | 1 (6.25) | 2 (9.5) | 1 (5.5) | |
| Up to 9 years, n (%) | 5 (31.3) | 7 (33.3) | 8 (44.4) | |
| 10–12 years, n (%) | 3 (18.8) | 2 (9.5) | 2 (11.1) | |
| 13–17 years, n (%) | 7 (43.8) | 10 (47.6) | 7 (38.9) | |
| Smoking, n (%) | 2 (12.5) | 3 (14.3) | 3 (16.7) | 0.94 |
| First-episode, n (%) | 10 (62.5) | 13 (61.9) | 9 (50) | 0.69 |
| Baseline HAMD score | 21.94 ± 4.60 | 22.09 ± 5.04 | 22.94 ± 8.16 | 0.88 |
| Baseline SCL 90 score | 200.31 ± 53.69 | 205.38 ± 70.08 | 219.56 ± 67.57 | 0.72 |
| Baseline ISI score | 10.31 ± 2.94 | 16.81 ± 1.50 | 23.56 ± 1.62 | |
| Current treatment | 0.78 | |||
| Sertraline | 5 | 7 | 5 | |
| Fluvoxamine | 6 | 4 | 4 | |
| Escitalopram | 2 | 5 | 6 | |
| Fluoxetine | 3 | 5 | 3 |
HAMD Hamilton Depression Scale, ISI Insomnia Severity Index, SCL-90 Symptom Checklist-90
Outcomes
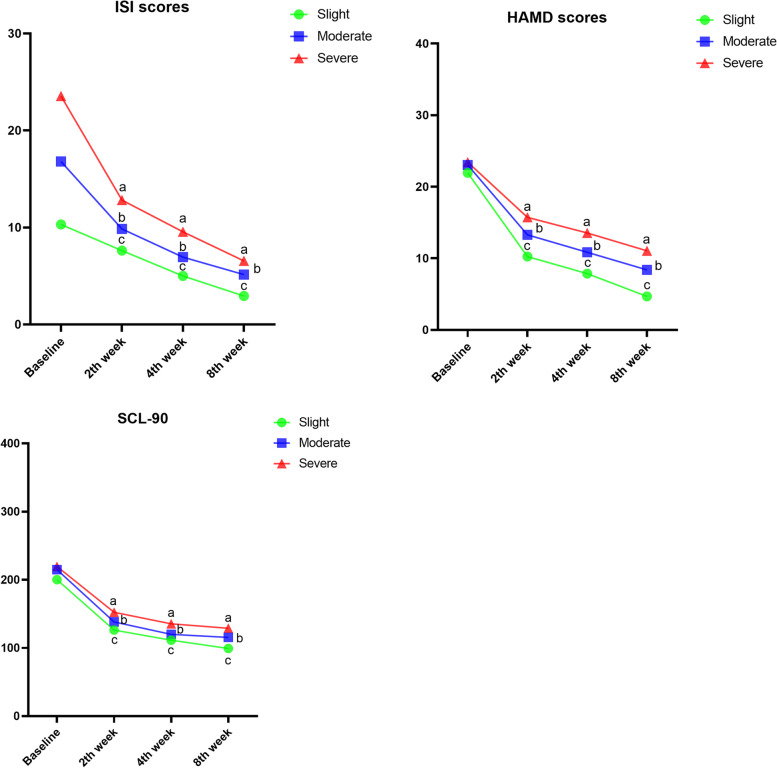
The effects of insomnia on the prognosis of patients with MDD are shown in Fig. 1. The sleep quality of MDD patients improved beginning in the 2nd week and gradually improved with the increase of prognosis time. The ISI scores of the moderate and severe group decreased significantly (P < 0.05) in the 2nd week compared to the baseline. The scores of all groups improved significantly at 8 weeks (Fig. 2).
Fig. 2.
Scores on the ISI, HAMD and SCL-90 in time of 2nd, 4th, and 8th-week follow-up. a indicate P < 0.05 versus the baseline of the severe group; b indicate P < 0.05 versus the baseline of the moderate group; c indicate P < 0.05 versus the baseline of the slight group. HAMD, Hamilton Depression Scale; ISI, Insomnia Severity Index; SCL-90, Symptom Checklist-90
The HAMD scores in all groups improved significantly in the second week. In the 4th and 8th weeks, the change from baseline in HAMD score of the slight group was higher than that of the severe group (Table 2). In the 8th week, significant differences were observed between the moderate and severe groups in comparison to the slight group by the response HAMD (χ2 = 6.13; P<0.05) and remission HAMD (χ2 = 13.32; P<0.05). As shown in Table 3, we observed the change from baseline in SCL-90 score of the slight group (100.93 ± 48.85) was higher than that of the severe group (90.66 ± 58.54) in the 8th week. Furthermore, the trends of ISI, HAMD, and SCL-90 are similar.
Table 2.
Change from baseline in HAMD score. Remission: final HAMD score ≤ 7. Response: 50% reduction in the pre-post-intervention
| Slight | Moderate | Severe | χ2 | P-value | |
|---|---|---|---|---|---|
| 2nd week follow-up | 10.25 ± 4.31 | 7.88 ± 2.55 | 4.69 ± 2.77 | ||
| Change from baseline in HAMD score | 11.69 ± 4.46 | 9.76 ± 4.83 | 7.72 ± 6.22 | ||
| Response HAMD, n | 8 | 5 | 3 | 5.02 | P = 0.081 |
| Remission HAMD, n | 5 | 1 | 1 | 6.98 | P<0.05 |
| 4th week follow-up | 13.29 ± 4.11 | 10.85 ± 4.30 | 8.38 ± 3.71 | ||
| Change from baseline in HAMD score | 14.07 ± 3.99 | 12.2 ± 4.89 | 9.88 ± 6.65 | ||
| Response HAMD, n | 13 | 11 | 10 | 3.65 | P = 0.16 |
| Remission HAMD, n | 6 | 5 | 5 | 0.85 | P = 0.66 |
| 8th week follow-up | 15.72 ± 5.02 | 13.56 ± 6.29 | 11.06 ± 6.99 | ||
| Change from baseline in HAMD score | 17.25 ± 4.01 | 14.67 ± 4.72 | 12.38 ± 6.97 | ||
| Response HAMD, n | 15 | 14 | 12 | 6.13 | P<0.05 |
| Remission HAMD, n | 14 | 7 | 6 | 13.32 | P<0.05 |
Table 3.
Change from baseline in SCL-90 score
| Slight | Moderate | Severe | |
|---|---|---|---|
| 2nd week follow-up | 126.4 ± 31.08 | 138.2 ± 44.23 | 152.3 ± 54.03 |
| Change from baseline in SCL-90 score | 73.91 ± 46.69 | 67.18 ± 61.38 | 67.26 ± 61.92 |
| 4th week follow-up | 111.4 ± 24.45 | 120.1 ± 30.63 | 135.6 ± 46.02 |
| Change from baseline in SCL-90 score | 88.91 ± 46.56 | 85.28 ± 60.85 | 83.96 ± 59.78 |
| 8th week follow-up | 99.38 ± 11.88 | 115.5 ± 21.48 | 128.9 ± 35.27 |
| Change from baseline in SCL-90 score | 100.93 ± 48.85 | 89.88 ± 62.19 | 90.66 ± 58.54 |
Discussion
This study demonstrates the effect of insomnia on patients with MDD. According to ISI, HAMD, and SCL-90 scores, the sleep quality of MDD patients improved beginning in the 2nd week and gradually improved with the increase of prognosis time. In addition, there is a recovery consistency between insomnia and MDD. It is a study to demonstrate that there is a clear correlation between insomnia and MDD.
Insomnia is a syndrome defined as difficulty in falling asleep, maintaining sleep, or non-restorative sleep [14]. There is a bidirectional relationship between insomnia and mood symptoms, poor sleep may precede the episode of MDD, and depressed mood disrupt standard sleep patterns [15]. In addition, people with insomnia are three times more likely to suffer from MDD than those without insomnia [16]. Insomnia is a condition caused by other disorders that are completely independent and can lead to coexisting disorders. Mental disorders, circadian rhythm disorders, or other sleep disorders may be the disorders [17, 18]. In this study, 55 MDD patients with insomnia were enrolled. According to the ISI scores, they were divided into three groups. The results showed no significant differences among the three groups regarding HAMD scores. In the prognosis of MDD, insomnia may be of great significance in preventing the recovery of the disorder.
In routine practice, clinicians have a wide choice of individual drugs, and need good evidence to make the best choice for each patient as Selective serotonin reuptake inhibitors (SSRIs), sertraline, fluvoxamine, escitalopram, and fluoxetine have been indicated to be effective for MDD [19]. In addition, evidence has suggested that sertraline and fluoxetine have similar insomnia efficacy [20]. From a clinical trial, fluvoxamine appears to be beneficial for treating insomnia in MDD [21]. In addition, previous studies have shown that escitalopram could improve subjective sleep experience [22, 23]. In terms of drug selection, we selected these four drugs according to the best choice for each patient. These SSRIs have beneficial effects on sleep disorders. It indicates that insomnia coexists with MDD.
Insomnia is the main symptom of several common sleep disorders, but it often coexists with mental illnesses. In addition, insomnia can affect the trajectory of MDD and increase the severity and duration of this disorder [14]. The poor subjective sleep quality before the treatment of MDD may indicate a reduced treatment response. It has been reported that MDD patients with interpersonal therapy have higher sleep quality scores than that with no remission and significantly improved mood [24]. Furthermore, poor sleep quality is related to poor response to depressed therapy [25]. In addition, it has been reported that the severity of insomnia is one of the clinical features predicting suicide within 1 year, and this connection has been reported in adolescence [26]. Adolescents with insomnia have the most severe MDD, and those with insomnia have more severe MDD than those without sleep disturbance [27]. Sleep disturbances are also associated with an increased risk of suicide in adolescents [28, 29]. Therefore, we can recognize the depth impact of insomnia on MDD. Our results showed that the sleep quality improved beginning in the 2nd week and gradually improved with the increase of time. The HAMD scores in all groups improved significantly in the second week. Moreover, the slight group performed best. It can see that insomnia is closely related to the prognosis of MDD. In the recovery process of depression, better sleep quality is beneficial to the recovery of MDD.
It has been indicated that insomnia is closely connected to depressive symptoms, resulting in poor prognosis conditions. Insomnia-related symptoms are essential and modifiable risk factors for achieving and maintaining MDD remission. Based on the above results, clinicians need to evaluate the sleep symptoms of MDD patients carefully. Insomnia commonly coexists with MDD rather than following MDD. We believe that insomnia and MDD need require specific treatment. The evidence confirms that we should pay more attention to insomnia while treating MDD.
Conclusions
This study was inspired to assess insomnia as a comorbid disorder for patients with MDD, which may bring poor treatment consequences. This study suggests that severe sleep disorders may have poor implications on the prognosis of MDD.
Acknowledgments
Not applicable.
Authors’ contributions
Guohong Xu and Jiaquan Liang made contributions to the conception or design of the work, Xiaoling Li and Caixia Xu analyzed the data; Guohong Xu aided in drafting the manuscript; Guojun Xie and Jiaquan Liang agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The author(s) read and approved the final manuscript.
Funding
This research was supported by the project of Foshan Science and Technology Bureau (1920001001018) and the High-level Hospital Development Program for Foshan “Climbing” Project (DF-04-02-002).
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
We obtained written informed consent from all patients. This study was approved by the ethics committee of the Third People’s Hospital of Foshan (No. FSSY-LS201903), China, and the experiments were conducted following the declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors have no potential or actual conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guohong Xu, Email: xug1@163.com.
Xiaoling Li, Email: 37348176@qq.com.
Caixia Xu, Email: 13827799842@139.com.
Guojun Xie, Email: xiegjfs@126.com.
Jiaquan Liang, Email: Liangjiaquan@muc.edu.cn.
References
- 1.Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23(4):2324–2332. doi: 10.1111/jcmm.14170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou L, Zhu Y, Chen W, Tang Y. Emerging role of microRNAs in major depressive disorder and its implication on diagnosis and therapeutic response. J Affect Disord. 2021;286:80–86. doi: 10.1016/j.jad.2021.02.063. [DOI] [PubMed] [Google Scholar]
- 3.Gutiérrez-Rojas L, Porras-Segovia A, Dunne H, Andrade-González N, Cervilla JA. Prevalence and correlates of major depressive disorder: a systematic review. Braz J Psychiatry. 2020;42(6):657–672. doi: 10.1590/1516-4446-2020-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao YJ, Jin Y, Rao WW, Zhang QE, Zhang L, Jackson T, et al. Prevalence of major depressive disorder among adults in China: a systematic review and Meta-analysis. Front Psychiatry. 2021;12:659470. doi: 10.3389/fpsyt.2021.659470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, et al. Clarifying the role of sleep in depression: a narrative review. Psychiatry Res. 2020;291:113239. doi: 10.1016/j.psychres.2020.113239. [DOI] [PubMed] [Google Scholar]
- 6.Melhuish Beaupre L, Brown GM, Kennedy JL. Circadian genes in major depressive disorder. World J Biol Psychiatry. 2020;21(2):80–90. doi: 10.1080/15622975.2018.1500028. [DOI] [PubMed] [Google Scholar]
- 7.Knechtle B, Economou NT, Nikolaidis PT, Velentza L, Kallianos A, Steiropoulos P, et al. Clinical characteristics of obstructive sleep apnea in psychiatric disease. J Clin Med. 2019;8:4. doi: 10.3390/jcm8040534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boland EM, Vittengl JR, Clark LA, Thase ME, Jarrett RB. Is sleep disturbance linked to short- and long-term outcomes following treatments for recurrent depression? J Affect Disord. 2020;262:323–332. doi: 10.1016/j.jad.2019.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mason BL, Davidov A, Minhajuddin A, Trivedi MH. Focusing on insomnia symptoms to better understand depression: a STAR*D report. J Affect Disord. 2020;260:183–186. doi: 10.1016/j.jad.2019.08.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McIntyre RS, Lee Y, Mansur RB. A pragmatic approach to the diagnosis and treatment of mixed features in adults with mood disorders. CNS Spectr. 2016;21(S1):25–33. doi: 10.1017/s109285291600078x. [DOI] [PubMed] [Google Scholar]
- 11.Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liberman JN, Davis T, Pesa J, Chow W, Verbanac J, Heverly-Fitt S, et al. Predicting incident treatment-resistant depression: a model designed for health Systems of Care. J Manag Care Spec Pharm. 2020;26(8):987–995. doi: 10.18553/jmcp.2020.26.8.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. 2021;18:3. doi: 10.3390/ijerph18031082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sutton EL. Insomnia. Ann Intern Med. 2021;174(3):Itc33–itc48. doi: 10.7326/aitc202103160. [DOI] [PubMed] [Google Scholar]
- 15.Brietzke E, Vazquez GH, Kang MJY, Soares CN. Pharmacological treatment for insomnia in patients with major depressive disorder. Expert Opin Pharmacother. 2019;20(11):1341–1349. doi: 10.1080/14656566.2019.1614562. [DOI] [PubMed] [Google Scholar]
- 16.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 17.Crouse JJ, Carpenter JS, Song YJC, Hockey SJ, Naismith SL, Grunstein RR, et al. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention. Lancet Psychiatry. 2021;8(9):813–823. doi: 10.1016/s2215-0366(21)00034-1. [DOI] [PubMed] [Google Scholar]
- 18.K Pavlova M, Latreille V. Sleep Disorders. Am J Med. 2019;132(3):292–299. doi: 10.1016/j.amjmed.2018.09.021. [DOI] [PubMed] [Google Scholar]
- 19.Yuan Z, Chen Z, Xue M, Zhang J, Leng L. Application of antidepressants in depression: a systematic review and meta-analysis. J Clin Neurosci. 2020;80:169–181. doi: 10.1016/j.jocn.2020.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Thaler KJ, Morgan LC, Van Noord M, Gaynes BN, Hansen RA, Lux LJ, et al. Comparative effectiveness of second-generation antidepressants for accompanying anxiety, insomnia, and pain in depressed patients: a systematic review. Depress Anxiety. 2012;29(6):495–505. doi: 10.1002/da.21951. [DOI] [PubMed] [Google Scholar]
- 21.Hao Y, Hu Y, Wang H, Paudel D, Xu Y, Zhang B. The effect of fluvoxamine on sleep architecture of depressed patients with insomnia: an 8-week, open-label, baseline-controlled study. Nat Sci Sleep. 2019;11:291–300. doi: 10.2147/nss.S220947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stein DJ, Lopez AG. Effects of escitalopram on sleep problems in patients with major depression or generalized anxiety disorder. Adv Ther. 2011;28(11):1021–1037. doi: 10.1007/s12325-011-0071-8. [DOI] [PubMed] [Google Scholar]
- 23.Stein DJ, Khoo JP, Ahokas A, Jarema M, Van Ameringen M, Vavrusova L, et al. 12-week double-blind randomized multicenter study of efficacy and safety of agomelatine (25-50 mg/day) versus escitalopram (10-20 mg/day) in out-patients with severe generalized anxiety disorder. Eur Neuropsychopharmacol. 2018;28(8):970–979. doi: 10.1016/j.euroneuro.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Tubaki BR, Chandake S, Sarhyal A. Ayurveda management of major depressive disorder: a case study. J Ayurveda Integr Med. 2021;12(2):378–383. doi: 10.1016/j.jaim.2021.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gebara MA, Siripong N, DiNapoli EA, Maree RD, Germain A, Reynolds CF, et al. Effect of insomnia treatments on depression: a systematic review and meta-analysis. Depress Anxiety. 2018;35(8):717–731. doi: 10.1002/da.22776. [DOI] [PubMed] [Google Scholar]
- 26.Asarnow LD, Mirchandaney R. Sleep and mood disorders among youth. Child Adolesc Psychiatr Clin N Am. 2021;30(1):251–268. doi: 10.1016/j.chc.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsieh YP, Lu WH, Yen CF. Psychosocial determinants of insomnia in adolescents: roles of mental health, behavioral health, and social environment. Front Neurosci. 2019;13:848. doi: 10.3389/fnins.2019.00848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan NY, Zhang J, Tsang CC, Li AM, Chan JWY, Wing YK, et al. The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents. Sleep Med. 2020;74:124–131. doi: 10.1016/j.sleep.2020.05.035. [DOI] [PubMed] [Google Scholar]
- 29.Chen SJ, Zhang JH, Li SX, Tsang CC, Chan KCC, Au CT, et al. The trajectories and associations of eveningness and insomnia with daytime sleepiness, depression and suicidal ideation in adolescents: a 3-year longitudinal study. J Affect Disord. 2021;294:533–542. doi: 10.1016/j.jad.2021.07.033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.