Abstract
Background/Aim: Non-medical practitioners (NMPs) are an ill-defined group of professionals offering patient diagnostic and therapeutic methods mostly in the field of complementary and alternative medicine (CAM). Despite a lack of quality-assessed structured professional formation, many patients with cancer visit NMPs for advice. This study aimed to learn more on patients’ motives and expectations for consulting an NMP.
Patients and Methods: A standardized questionnaire was distributed to adult cancer patients addressing attitudes towards NMPs, motives and expectations for consulting an NMP.
Results: A total of 279 patients took part in the survey. Of the included patients 44.8% had already visited an NMP and 16.5% planned to do so. Reasons to visit an NMP were seeking for a supplementary treatment (72.0%) or control of side-effects (68.0%). While the oncologist ranked higher than the NMP in all aspects of physician-patient interaction and patients more often trusted in the oncologist, those patients rating their oncologist rather low in any of these questions significantly more often consulted an NMP. The methods applied or recommended by the NMPs were highly heterogenous ranging from biologically-based methods to mind-body-techniques. Most often used methods were homeopathy (72.0%) vitamin D (62.7%), selenium (42.7%), acupuncture (38.7%).
Conclusion: There is a high proportion of cancer patients visiting NMPs mostly for additional treatment. Biologically-based treatments may induce side-effects and interactions, especially as NMPs are not trained on medically accepted cancer treatment and medications. Offering information on CAM and improving the physician-patient relationship are important means to answer unmet needs from the side of the patient.
Keywords: Non-medical-practitioner, complementary and alternative medicine (CAM), communication, cancer, patientphysician-relationship
Approximately half of all cancer patients use complementary and alternative medicine (CAM) (1). The main reasons for using CAM are to reduce side-effects or to boost the immune-system. Some patients use CAM to have better control of the cancer or/and not to leave out a chance (2,3). No uniform definition on CAM exists, yet the term comprises methods beyond conventional or academic medicine which are used instead of or along with conventional medicine.
The WHO defines CAM as “a broad set of health care practices that are not part of that country’s own tradition or conventional medicine and are not fully integrated into the dominant health-care system. They are used interchangeably with traditional medicine in some countries” (4). The range of CAM procedures is wide and includes movement and exercise therapy, mental and cognitive methods, nutrition, diet, and supplements, as well as biologically-based methods, such as phytotherapy. Moreover, holistic methods, which comprise a whole medical system as homeopathy or Traditional Chinese Medicine, are part of CAM. Patients can gain access to CAM in various ways, e.g., through attending physicians, their own research or by visiting an alternative non-medical practitioners (NMPs). In several surveys on cancer patients, we found that 17% to 24% of patients visited an NMP for CAM (2,3).
Twenty-one percent of patients consent to the argument, that they “prefer a non-medical practitioner or naturopath because they have a deeper understanding of my illness” and even 33% report that NMPs, in contrast to physicians, spend more time for the individual patient during the consultation (2).
While in many countries, NMPs are not regulated, in Germany they are based on a law published in 1939 (5). The “Bund Deutscher Heilpraktiker” (Association of German Non-medical Practitioners), one of many professional associations in Germany, describes the procedures of NMPs as naturopathic, and are based on a holistic medical approach, as well as experience, and are independent of the current scientific state of orthodox medicine (6).
Prerequisites for NMPs in Germany. The prerequisites which must be fulfilled in order for one to be able to practice as a non-medical practitioner in Germany repeatedly lead to controversial discussions (7,8). Candidates for the profession of alternative practitioner may prepare for an examination (Heilpraktikerprüfung) held by the regional health office either by attending courses offered by different private institutes or by self-study. Prerequisites for participation are a lower secondary school certificate and 25 years of age. The examination aims to test the candidate’s knowledge of allowed medical activities, which are limited in contrast to studied physicians. For example, NMPs are not allowed to perform blood transfusions. Furthermore, any patient with a serious, life-threatening disease must be sent to a physician. This shall protect patients from the risk of treatment by an unsuitable alternative practice.
Contrary to what one would expect, the examination does not include testing of knowledge or ability to carry out procedures later in professional practice. In a sixty-minute exam and a multiple-choice test of 60 questions, all clinical subjects of the four central medical exams for physicians are included. At the end of 2017, the Federal Ministry of Health in Germany published a new guideline for the exam of candidates, which came into force in March 2018. Now candidates shall additionally show their ability to adequately examine patients (9).
Diagnostic and therapeutic methods of NMPs in Germany. In a former survey, we addressed NMPs and asked them on the diagnostic and therapeutic methods they used for cancer patients (10). We found a broad range of different methods most not belonging to evidence-based procedures. Moreover, there was no association between diagnostic methods, goals of treatment and therapeutic methods so that the concepts of treatment remain dubious. Furthermore, a part of the NMPs used alternative methods, such as homeopathy, to cure cancer or applied toxic substances as amygdaline which releases hydrocyanic acid (10).
In fact, NMPs with potentially health-endangering methods repeatedly appear in the headlines of newspapers (11,12). Their status is criticized not only regarding the therapeutic approaches they use, but also for the lack of medical training. In 2019, a non-medical practitioner from a so-called biological cancer center had to testify in court because he had overdosed his oncological patients with 3-bromopyruvate. Three patients died due to this treatment (13).
Nevertheless, for many patients the NMP is an important person during and after their cancer treatment. As a consequence, a discussion is ongoing, whether the education of NMPs in Germany should be improved by a structured evidence-based curriculum under the supervision of physicians and scientists. The alternative discussed is that the state recognition could be revoked in order to clarify that offers of NMPs are not part of a scientifically based health system.
In order to better understand the patients’ perspective, we set out to learn more on their attitudes, motives and expectations with respect to NMPs.
Patients and Methods
We conducted an anonymous cross-sectional study using a standardized questionnaire.
Patients. A group of patients was included from the oncological outpatient clinic of a German University Hospital for pilot testing a print version of the questionnaire. For the main study, the online questionnaire was distributed via the self-help group Melanoma Forum to its members and visitors of its website, which is also frequently visited by patients with other types of cancers and by relatives and other caregivers.
Questionnaire. The questionnaire was developed in two steps. Experts from the working group Prevention and Integrative Oncology (AG PRIO) of the German Cancer Society developed a first version of a standardized questionnaire addressing the patients’ perspectives on NMPs. This questionnaire was handed to eight individuals to test its comprehensibility and determine the time needed to complete it. Then, the pilot version was tested on outpatients with different types of cancers and completed forms were analyzed for missing answers and inconsistencies. Furthermore, patients filling in the questionnaire were asked to mark any phrase hard to understand. After revisions, the questionnaire was put online and distributed via the above-mentioned website.
The questionnaire consisted of five parts with 16 questions:
1. Demographic data (age, sex, highest level of education, job, type of tumor disease, year of initial diagnosis);
2. Questions on the patients’ relationship to the oncologist (e.g., feeling adequately informed, trusting the physician, empathy and guidance provided by the physician);
3. Questions on visit to an NMP, reasons for this visit, features influencing the choice of an NMP;
4. Questions on the relationship to the NMP (same questions as with respect to the oncologist);
5. Questions on interest in CAM and application of CAM methods by the NMP (for the latter we provided a list of 49 often used CAM methods in Germany which we derived from our former surveys with patients and NMPs) (2,3,10).
The questionnaire comprises closed questions, in part using a 4-part Likert scale (I fully consent, I consent a little bit, I mostly consent, I do not consent). From the pilot study, we learnt that the questionnaire was easy to answer without any help and no changes were necessary. It took about 10 minutes to complete it.
Statistics. The data from the survey were transferred to the SPSS version 28 for statistical evaluation calculating frequencies. For correlations we used the Chi-square test. A p-value under 0.05 was considered significant.
Ethical approval. The study was approved by the Ethics Committee of the University Hospital at Jena (No. 2017-1547). Informed consent was obtained from all individual participants included in the study by answering the questionnaire.
Results
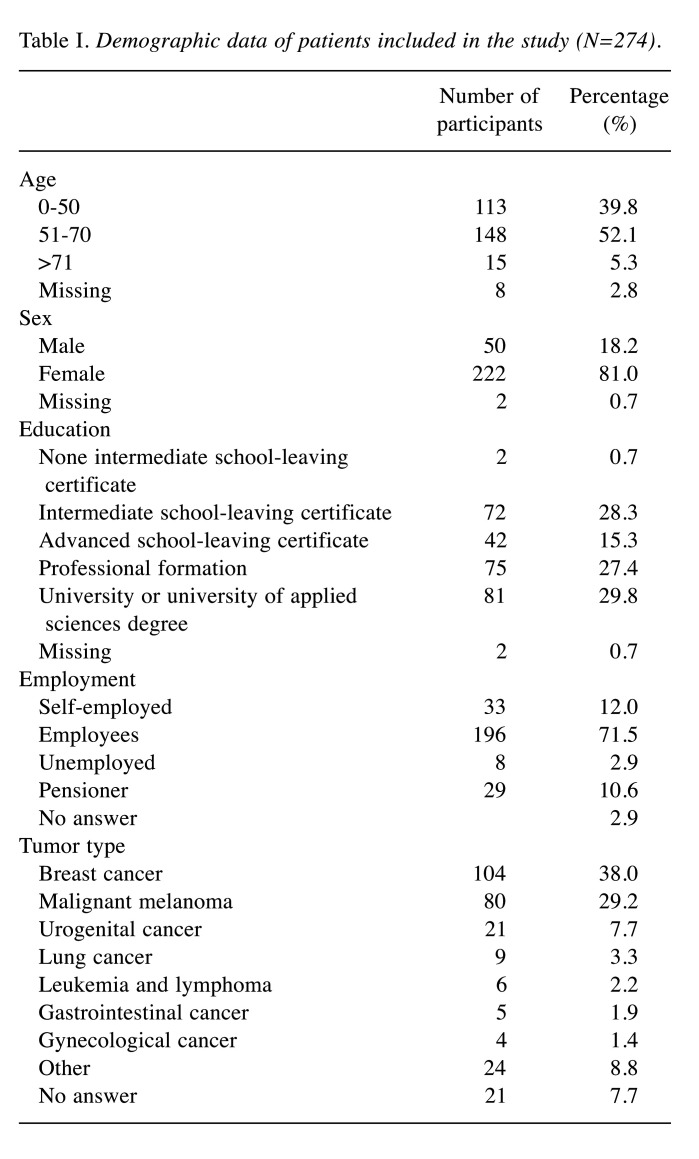
Demographic data. Two hundred seventy-four patients participated in the survey. The demographic data are summarized in Table I. A total of 222 participants were females (81.0%) and 50 males (18.2%). The largest group were patients with breast cancer (N=104, 37.3%) or melanoma (N=80, 28.7%).
Table I. Demographic data of patients included in the study (N=274).
Visit to a non-medical practitioner (NMP). This question was answered by 230 patients (83.9%). Twenty-eight patients (12.2%) had visited an NMP only before cancer diagnosis, 41 (17.8%) before and after cancer diagnosis and 34 (14.8%) only after the cancer diagnosis. Thirty-eight patients (16.5%) planned to visit an NMP and 89 (38.7%) stated that they would not do so.
The NMP was mostly found due to recommendations of friends or family (N=168; 61.3%), followed by the Internet (N=79; 28.8%), newspapers (N=11; 4.0%), a flyer from the practitioner (N=8; 2.9%) or by recommendation from a physician (N=6; 2.2%).
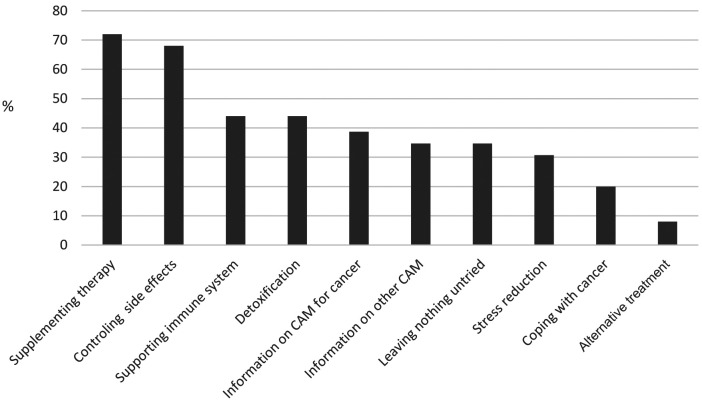
Most often named reasons to visit an NMP (Figure 1) were seeking for a supplemental treatment (N=54, 72.0%) or control of side-effects (N=51; 68%). Yet six patients (8%) reported that they were looking for an alternative treatment method. Strengthening the immune system was stated significantly more frequently by women (p=0.008) and people with higher education (p=0.017). Moreover, higher education was positively associated with aiming at stress reduction (p=0.021).
Figure 1. Reasons to visit a non-medical practitioner in case of cancer (N=75).
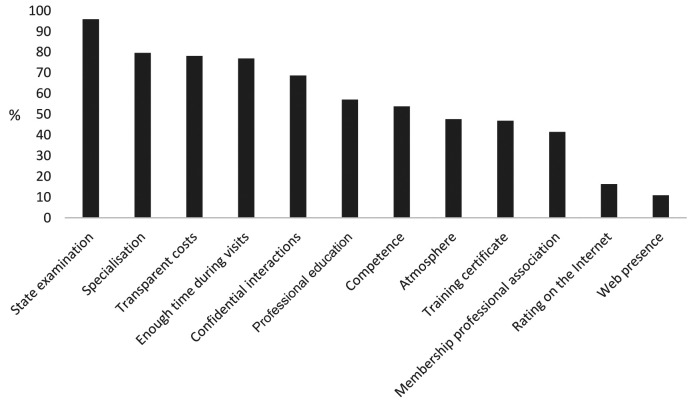
Regarding the features that are important to decide which NMP to consult (Figure 2), most important were the state examination (N=141; 95.9%), the specialization (N=117; 79.6%), transparent costs (N=115; 78.2%), enough time during visits (N=113; 76.9%) and confidential interactions (N=101; 68.7%). Younger people more often named the atmosphere at the NMP being a reason to visit him/her (p=0.018).
Figure 2. Features influencing the patient decision to consult a non-medical practitioner (N=147).
Interest in complementary and alternative methods (CAM). The question on interest in CAM was answered by 236 participants (83.1%). From these 125 (53.0%) had already used CAM before cancer diagnosis, while 64 (27.1%) became interested after the diagnosis and 37 (15.6%) answered that they were not interested at all. There was no correlation between interest in CAM and age, sex, or education.
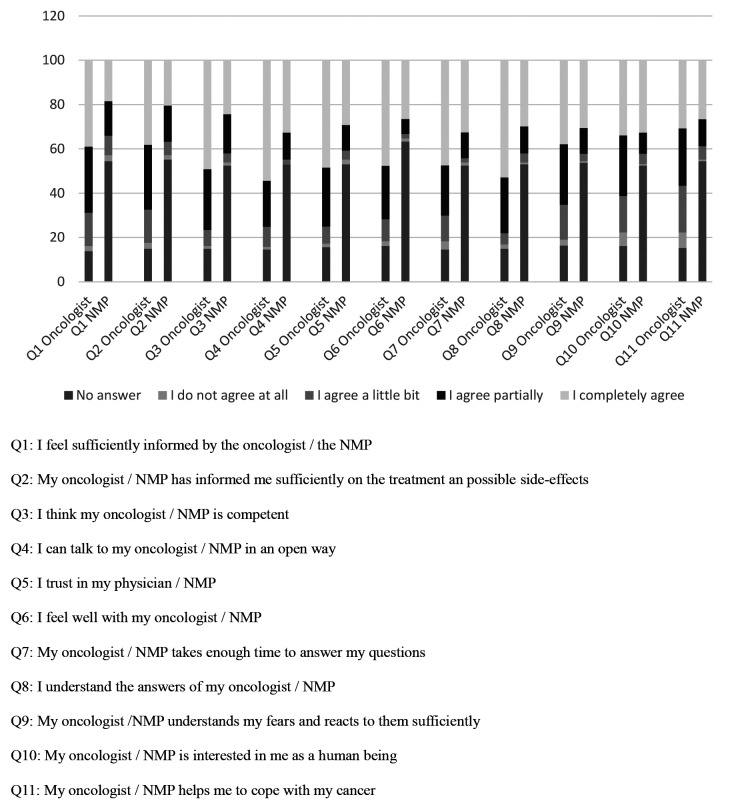
Relationship to the oncologist and the NMP. A majority of the patients agreed partially or completely that there is a high competence on the side of the oncologist that they were sufficiently informed and could talk openly to the oncologist, trusted in him and felt supported. In contrast, the same questions were not answered by patients who visited an NMP. Considering complete and partial agreement, in all questions, the oncologist ranked higher than the NMP (Figure 3).
Figure 3. Opinion of patients for oncologists and non-medical practitioners (NMPs) (N=274 for the questions on the oncologist and N=147 for the questions on the NMPs).
Older people more often agreed to their oncologist being competent (p=0.001) and being able to talk openly to him/her (p<0.001) and receiving well understandable explanations (p<0.001). They also more often trusted in the oncologist (p<0.001). With respect to the NMP, no such correlation with age could be demonstrated. For sex and education, we did not find any correlations neither with respect to the oncologist nor the NMP. Patients rating their oncologist rather low in any of these questions significantly more often consulted an NMP (all p<0.001).
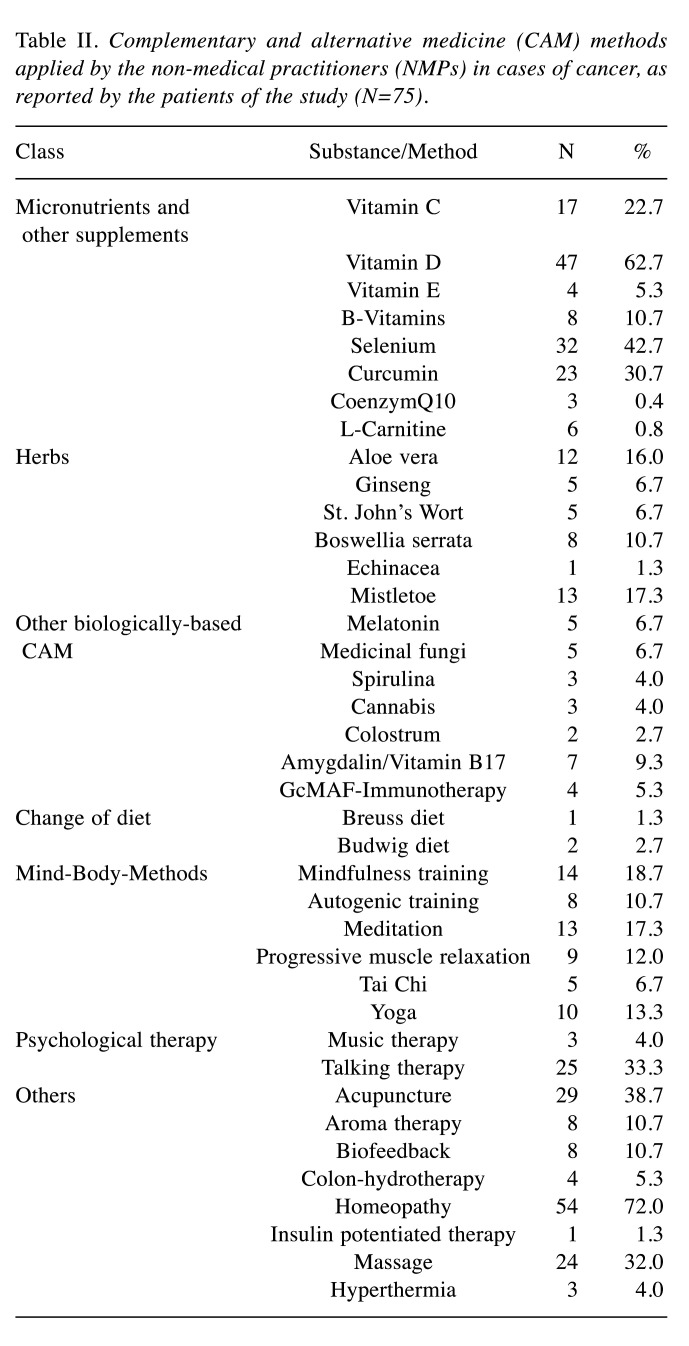
CAM methods applied by the NMPs. The methods applied or recommended by the NMPs were highly heterogenous ranging from biologically-based methods (mostly micronutrients and herbs) to mind-body-techniques (Table II). Most often used methods were homeopathy (N=54; 72.0%), vitamin D (N=47; 62.7%), selenium (N=32; 42.7%), acupuncture (N=29; 38.7%), talking therapy (N=25; 33.3%) and curcumin (N=23; 30.7%).
Table II. Complementary and alternative medicine (CAM) methods applied by the non-medical practitioners (NMPs) in cases of cancer, as reported by the patients of the study (N=75).
Only women reported that the NMP offered them mindfulness exercises (p=0.004) and more women than man reported received talking therapy (p=0.024). With respect to education there was a positive correlation between the level of education and being offered talking therapy (p=0.022).
Discussion
In our patient population, nearly two thirds had already visited an NMP and one third has been already treated by an NMP with respect to their cancer.
While in several studies, female age and higher education have been associated with more interest in and usage of CAM (14-18) and in a survey by Munstedt et al., trust in NMPs was higher in female patients (19), we did not find any such association with respect to NMPs.
A higher educational level could be associated with doubts about the conventional medical system and therefore could lead to more interest on CAM (20). On the other hand, a review regarding CAM usage in Scandinavia by Nilsson et al. revealed that education levels varied among CAM user in the included studies, and no trend towards high or low education was observed (21). Insofar, the level of education does not necessarily seem to be the most important reason for using CAM. It appears to be more related to satisfaction with medical care, as our study showed.
Most importantly, the satisfaction of patients with the oncologists is rather high and with respect to most questions we put higher than with the NMPs. This at first glance seems contradictory, but points to unmet needs which seem to be accepted by the patients without disturbing the physician-patient relationship. Yet, patients rating the relationship to their oncologist rather low significantly more often consulted an NMP.
To understand the motives to contact an NMP, we looked at the aims. In this section the answers are in line with motifs to use CAM (2,22,23). The most frequent aims for consulting an NMP were additional treatments (supplementation of the medical therapy, control of side-effects, stress reduction) which may be achieved by evidence-based complementary methods as already described in guidelines (24). Also, the aim not to leave anything untried points to a strong need for psychosocial support. An important issue is that about two thirds of patients name control of side-effects as the motif to contact an NMP. While also for supportive treatment, there has been huge progress in the last decades, information on side-effects and treatment of those still seems to be insufficient. Moreover, the longer duration of modern treatments and a remaining number of side-effects, for which no sufficient evidence-based treatment exists (for example polyneuropathy, fatigue, cognitive dysfunction), have a strong impact on quality of life. Also, this demands for more empathy, caring and support. On the other hand, a part of the patients is less compliant with supportive treatments in part as for example exercising is strenuous. Yet, there seems to be a number of patients who do “not want to take more drugs” and who try to reduce antiemetics or pain medication. For all this, better information, repeated screening for problems and repeated (short) discussions with physicians are essential. Nevertheless, for most methods offered by the NMPs as homeopathy (72%) or acupuncture (40%), there is no evidence of effectiveness beyond a placebo effect.
In our study, less than one tenth of the participants looked for a replacement of the cancer treatment, which is the most dangerous form of alternative medicine as it is well-documented to lead to a worse prognosis (25-27) and some may even induce death as for example amygdalin which was offered by about 10% of the NMPs.
Trust in an NMP is mostly based on the approval according to the “Heilpraktikergesetz” (NMP-law) which is understood as a sign for competence. Also, specialization on certain methods adds to trustworthiness. The vast majority of the population does not know about the exam of the NMPs and the lack of education. In our analyses of the course offers of German private schools for NMPs, we were able to show that they do not include any education on scientifically based medical issues but only include methods with low or missing evidence (28). Moreover, as NMPs do not have to learn anything on scientific diagnostics and treatments, they may strongly overvalue their own methods and underestimate the risks of interactions. Accordingly, in a survey in cooperation with associations of NMPs, we have shown that there is no relationship between the diagnostic and therapeutic methods applied by NMPs (10). In our study, the methods applied or recommended by the NMPs were highly heterogenous including many biologically-based methods (mostly micronutrients and herbs). In several studies, it was shown that about one third of cancer patients using CAM are at risk of interactions (29-32), which were not detected by the physician as disclosure of CAM usage is low. Most probably, CAM usage recommended by the NMP is even less often discussed with the physician, as most physicians are rather skeptical with respect to NMPs, and the patient does not want to get into a troublesome controversy. Moreover, most probably, the trust of patients in the NMP is rather high as most often the NMP was chosen on the recommendations next ones.
Limitations. There are some limitations in our study. First of all, details on how many patients were addressed and how many of those participated are unclear. Moreover, the survey may not be representative as at least the online part only addressed patients familiar with the internet.
Conclusion
Within the modern health care system, reduced access to physicians and nurses leads to an increasing gap between what patients want in terms of care and how the medical care is currently being provided by physicians. Lack of time on the side of the physician is the prominent motif to address an NMP or naturopath (2). Considering the dangers of unqualified NMPs two options seem valuable: either improving the training of NMPs or abolishing this profession (33). Many people and politicians argue for the first option. Considering the huge amount of money spend on alternative medicine, it might a better investment to transfer this money into training, time to communicate and support for well-trained professions as physicians and nurses. Moreover, physicians should have some training on CAM to provide evidence-based recommendations.
Conflicts of Interest
The Authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Authors’ Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jutta Hübner and Emadaldin Ahmadi. The first draft of the manuscript was written by Jutta Hübner and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The Authors thank Leonie Sibold for supporting in material preparation, data collection and parts of the introduction.
References
- 1.Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11(3):187–203. doi: 10.1177/1534735411423920. [DOI] [PubMed] [Google Scholar]
- 2.Huebner J, Micke O, Muecke R, Buentzel J, Prott FJ, Kleeberg U, Senf B, Muenstedt K, PRIO (Working Group Prevention and Integrative Oncology of the German Cancer Society) User rate of complementary and alternative medicine (CAM) of patients visiting a counseling facility for CAM of a German comprehensive cancer center. Anticancer Res. 2014;34(2):943–948. [PubMed] [Google Scholar]
- 3.Huebner J, Prott FJ, Micke O, Muecke R, Senf B, Dennert G, Muenstedt K, PRIO (Working Group Prevention and Integrative Oncology - German Cancer Society) Online survey of cancer patients on complementary and alternative medicine. Oncol Res Treat. 2014;37(6):304–308. doi: 10.1159/000362616. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Traditional Medicine Strategy. Available at: https://apps.who.int/iris/bitstream/handle/10665/92455/9789241506090_eng.pdf. [Last accessed on July 29, 2022]
- 5.Heilpraktikergesetz in der im Bundesgesetzblatt Teil III, Gliederungsnummer 2122-2, veröffentlichten bereinigten Fassung, das zuletzt durch Artikel 17e des Gesetzes vom 23. Dezember 2016 (BGBl. I S. 3191) geändert worden ist [Heilpraktikergesetz in the revised version published in the Federal Law Gazette Part III, structure number 2122-2, which was last amended by Article 17e of the law of 23 December 2016 (Federal Law Gazette I p. 3191)] [Google Scholar]
- 6.Bund Deutscher Heilpraktiker e.V.: Berufsbild des Heilpraktikers [Professional profile of the non-medical practitioner] Available at: https://www.bdh-online.de/wp-content/uploads/2015/08/Berufsbild-Heilpraktiker_2015_210x297_20150814.pdf. [Last accessed on December 3, 2021]
- 7.Anlauf M, Aust N, Bertelsen H-W, Boscheinen J, Ernst E, Friedrich DR, Grams N, Hoyningen-Huene P, Hübner J, Hucklenbroich P, Raspe H, Reichardt J-O, Schmacke N, SchöneSeifert B, Scholz OR, Taupitz J, Weymayr C. Münsteraner Kreis: Münsteraner Memorandum Heilpraktiker [Münsteraner Kreis: Münsteraner Memorandum non-medical practitioner] Available at: http://daebl.de/BB36. [Last accessed on July 29, 2022]
- 8.Schöne-Seifert B. Weg mit der staatlichen Lizenz für Heilpraktiker! MMW Fortschr Med. 2017;159(16):35. doi: 10.1007/s15006-017-0057-9. [DOI] [PubMed] [Google Scholar]
- 9.Bundesministerium für Gesundheit: Bekanntmachung von Leitlinien zur Überprüfung von Heilpraktikeranwärterinnen und -anwärtern nach § 2 des Heilpraktikergesetzes in Verbindung mit § 2 Absatz 1 Buchstabe i der Ersten Durchführungsverordnung zum Heilpraktikergesetz [Announcement of guidelines for the examination of alternative practitioners according to § 2 of the Heilpraktikergesetz in connection with § 2 paragraph 1 letter i of the First Implementation Ordinance to the Heilpraktikergesetz] 2017 [Google Scholar]
- 10.Koehl B, Muenstedt K, Micke O, Muecke R, Buentzel J, Stoll C, Prott FJ, Dennert G, Senf B, Huebner J. Survey of German non-medical practitioners regarding complementary and alternative medicine in oncology. Oncol Res Treat. 2014;37(1-2):49–53. doi: 10.1159/000358158. [DOI] [PubMed] [Google Scholar]
- 11.So gefährlich sind Heilpraktiker in Deutschland. Available at: https://www.stern.de/gesundheit/heilpraktiker-in-deutschland—so-gefaehrlich-sind-sie—-der-grosse-stern-report-7434370.html. [Last accessed on December 1, 2021]
- 12.Grabar E. Alternative Krebstherapie: Wenn Heilpraktiker aus Versehen töten [Alternative cancer therapy: when non-medical practitioners accidentally kill]. Die Zeit, 2016. Available at: https://www.zeit.de/wissen/gesundheit/2016-08/heilpraktikerermittlungen-tote-alternative-krebstherapie-klaus-ross-brueggen. [Last accessed on July 29, 2022]
- 13.Röse M. Brüggen/Krefeld: Heilpraktiker-Prozess endet früher [Brüggen/Krefeld: Heilpraktiker process ends earlier]. Rp Online, 2019. Available at: https://rp-online.de/nrw/staedte/viersen/heilpraktiker-prozess-gegen-klaus-r-vom-biologischenkrebszentrum-in-brueggen-bracht-endet-vorzeitig_aid-42897075. [Last accessed on December 3, 2021]
- 14.Rakovitch E, Pignol JP, Chartier C, Ezer M, Verma S, Dranitsaris G, Clemons M. Complementary and alternative medicine use is associated with an increased perception of breast cancer risk and death. Breast Cancer Res Treat. 2005;90(2):139–148. doi: 10.1007/s10549-004-3779-1. [DOI] [PubMed] [Google Scholar]
- 15.Chang KH, Brodie R, Choong MA, Sweeney KJ, Kerin MJ. Complementary and alternative medicine use in oncology: a questionnaire survey of patients and health care professionals. BMC Cancer. 2011;11:196. doi: 10.1186/1471-2407-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Molassiotis A, Fernández-Ortega P, Pud D, Ozden G, Scott JA, Panteli V, Margulies A, Browall M, Magri M, Selvekerova S, Madsen E, Milovics L, Bruyns I, Gudmundsdottir G, Hummerston S, Ahmad AM, Platin N, Kearney N, Patiraki E. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16(4):655–663. doi: 10.1093/annonc/mdi110. [DOI] [PubMed] [Google Scholar]
- 17.Eisfeld H, Bauer F, Dubois C, Schmidt T, Kastrati K, Hochhaus A, Hübner J. Importance of and satisfaction with information about their disease in cancer patients. J Cancer Educ. 2020;35(2):403–411. doi: 10.1007/s13187-019-1480-7. [DOI] [PubMed] [Google Scholar]
- 18.Dufter SA, Hübner J, Ahmadi E, Zomorodbakhsch B. Traits of cancer patients and CAM usage. J Cancer Res Clin Oncol. 2021;147(12):3685–3692. doi: 10.1007/s00432-021-03605-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Münstedt K, Funk D, Riepen T, Berkes E, Hübner J. Perceptions of German patients consulting a general practitioner or a gynaecologist on conventional medicine, naturopathy and holistic/alternative medicine. Eur J Integr Med. 2019;27:45–51. doi: 10.1016/j.eujim.2019.02.011. [DOI] [Google Scholar]
- 20.Verhoef MJ, Balneaves LG, Boon HS, Vroegindewey A. Reasons for and characteristics associated with complementary and alternative medicine use among adult cancer patients: a systematic review. Integr Cancer Ther. 2005;4(4):274–286. doi: 10.1177/1534735405282361. [DOI] [PubMed] [Google Scholar]
- 21.Nilsson J, Källman M, Östlund U, Holgersson G, Bergqvist M, Bergström S. The use of complementary and alternative medicine in Scandinavia. Anticancer Res. 2016;36(7):3243–3251. [PubMed] [Google Scholar]
- 22.Loquai C, Dechent D, Garzarolli M, Kaatz M, Kaehler KC, Kurschat P, Meiss F, Micke O, Muecke R, Muenstedt K, Stein A, Nashan D, Stoll C, Schmidtmann I, Huebner J. Use of complementary and alternative medicine: A multicenter cross-sectional study in 1089 melanoma patients. Eur J Cancer. 2017;71:70–79. doi: 10.1016/j.ejca.2016.10.029. [DOI] [PubMed] [Google Scholar]
- 23.Bauer F, Schmidt T, Eisfeld H, Dubois C, Kastrati K, Hochhaus A, Huebner J. Information needs and usage of complementary and alternative medicine in members of a German self-help group for gastrointestinal stroma tumours, sarcoma, and renal cancer. Complement Ther Med. 2018;41:105–110. doi: 10.1016/j.ctim.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF): Komplementärmedizin in der Behandlung von onkologischen PatientInnen, Langversion 1.1, 2021, AWMF Registernummer: 032/055OL. Available at: https://www.leitlinienprogramm-onkologie.de/leitlinien/komplementaermedizin/ [Last accessed on December 3, 2021]
- 25.Risberg T, Vickers A, Bremnes RM, Wist EA, Kaasa S, Cassileth BR. Does use of alternative medicine predict survival from cancer. Eur J Cancer. 2003;39(3):372–377. doi: 10.1016/s0959-8049(02)00701-3. [DOI] [PubMed] [Google Scholar]
- 26.Joseph K, Vrouwe S, Kamruzzaman A, Balbaid A, Fenton D, Berendt R, Yu E, Tai P. Outcome analysis of breast cancer patients who declined evidence-based treatment. World J Surg Oncol. 2012;10:118. doi: 10.1186/1477-7819-10-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson SB, Park HS, Gross CP, Yu JB. Use of alternative medicine for cancer and its impact on survival. J Natl Cancer Inst. 2018;110(1) doi: 10.1093/jnci/djx145. [DOI] [PubMed] [Google Scholar]
- 28.Hoffmeister L, Muenstedt K, Huebner J, Keinki C. Erratum to: Education of non-medical practitioners in Germany-an analysis of course subjects of specialized schools. Wien Med Wochenschr. 2022 doi: 10.1007/s10354-021-00909-8. [DOI] [PubMed] [Google Scholar]
- 29.Zeller T, Muenstedt K, Stoll C, Schweder J, Senf B, Ruckhaeberle E, Becker S, Serve H, Huebner J. Potential interactions of complementary and alternative medicine with cancer therapy in outpatients with gynecological cancer in a comprehensive cancer center. J Cancer Res Clin Oncol. 2013;139(3):357–365. doi: 10.1007/s00432-012-1336-6. [DOI] [PubMed] [Google Scholar]
- 30.Loquai C, Dechent D, Garzarolli M, Kaatz M, Kaehler KC, Kurschat P, Meiss F, Stein A, Nashan D, Micke O, Muecke R, Muenstedt K, Stoll C, Schmidtmann I, Huebner J. Risk of interactions between complementary and alternative medicine and medication for comorbidities in patients with melanoma. Med Oncol. 2016;33(5):52. doi: 10.1007/s12032-016-0764-6. [DOI] [PubMed] [Google Scholar]
- 31.Firkins R, Eisfeld H, Keinki C, Buentzel J, Hochhaus A, Schmidt T, Huebner J. The use of complementary and alternative medicine by patients in routine care and the risk of interactions. J Cancer Res Clin Oncol. 2018;144(3):551–557. doi: 10.1007/s00432-018-2587-7. [DOI] [PubMed] [Google Scholar]
- 32.Wolf CPJG, Rachow T, Ernst T, Hochhaus A, Zomorodbakhsch B, Foller S, Rengsberger M, Hartmann M, Huebner J. Complementary and alternative medicine (CAM) supplements in cancer outpatients: analyses of usage and of interaction risks with cancer treatment. J Cancer Res Clin Oncol. 2022;148(5):1123–1135. doi: 10.1007/s00432-021-03675-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anlauf M, Aust N, Bertelsen H-W, Boscheinen J, Ernst E, Friedrich DR, Grams N, Hoyningen-Huene P, Hübner J, Hucklenbroich P, Raspe H, Reichardt J-O, Schmacke N, Schöne-Seifert B, Scholz OR, Taupitz J, Weymayr C. Münsteraner Memorandum Heilpraktiker. Die Thesen des “Münsteraner Kreises” zu einer Neuregelung des Heilpraktikerwesens. Ethik Med. 2017;29:334–342. doi: 10.1007/s00481-017-0461-9. [DOI] [Google Scholar]