Abstract
Background
Angong Niuhuang Pill (ANP), a renowned precious traditional Chinese medicine prescription, is extensively utilized for the clinical treatment of stroke, meningitis and encephalorrhagia in China. As a classic resuscitation-inducing aromatic prescription, ANP has been investigated for its pharmacological effects in recent years, while the volatile composition in ANP still lacks comprehensive elucidation.
Method
To better explore the volatile constituents in ANP, a qualitative analysis method was developed based on gas chromatography coupled with mass spectrometry. Furthermore, a validated quantitative method was established to determine 21 main compounds in 8 batches of commercially available ANP samples by gas chromatography-tandem mass spectrometry. The quantitative data were successively subjected to Pearson correlation coefficient analysis. Additionally, the absorbed volatile constituents in rat plasma after single oral administration of ANP have also been characterized.
Results
A total of 93 volatile constituents including 29 sesquiterpenoids, 28 monoterpenoids, 13 fatty acids and their esters, 7 alkanes, 6 ketones, 3 phenols, 3 aldehydes, 2 benzoate esters, and 2 other types, were preliminarily characterized, which primarily originated from Borneolum, Moschus, Curcumae Radix, and Gardeniae Fructus. d-Borneol, isoborneol and muscone were the top three abundant ingredients (> 600 μg/g) in 8 batches of ANP samples. Subsequently, the average Pearson correlation coefficient of the contents of 21 analytes was 0.993, inferring the high batch-to-batch similarity among 8 batches. After oral administration of ANP, d-borneol, isoborneol, muscone and camphor were the main volatile constituents absorbed in the rat plasma.
Conclusion
This research may be helpful for the comprehensive quality control study of ANP, and provide for guarantee the clinical efficacy of ANP.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13020-022-00659-8.
Keywords: Angong Niuhuang Pill, Volatile constituents, GC–MS, Pearson correlation coefficient
Introduction
Angong Niuhuang Pill (ANP), one of the most famous first-aid traditional Chinese medicines (TCMs), contains 11 crude drugs, including Bovis Calculus, Buffalo Horn, Moschus, Margarita, Cinnabaris, Realgar, Coptidis Rhizoma, Scutellariae Radix, Gardeniae Fructus, Curcumae Radix and Borneolum. ANP was first recorded in Treatise on Differentiation and Treatment of Epidemic Febrile Diseases in the Qing Dynasty and has a history of over 200 years of application in China. According to the TCM theory and clinical practice, ANP has been proved to be beneficial to the treatment of various central nervous system diseases, such as stroke coma, meningitis and intracerebral hemorrhage [1]. A recent meta-analysis of 18 trials involving 1601 patients reported that adjuvant treatment with ANP could significantly improve the total response rate and reduce the neurologic deficit score in patients with acute cerebral infarction and acute intracerebral hemorrhage [2].
Generally, ANP contains volatile and non-volatile constituents, contributing to an integral part of the overall efficacy of ANP. The volatile substances of aromatic drugs are mainly deemed to process the important properties of resuscitation and awakening in traditional Chinese medicines. Since ANP is a typical resuscitation-inducing aromatic prescription, its therapeutic effect on cerebrovascular diseases may be closely related to the volatile components. For instance, muscone, d-borneol, and isoborneol, the representative components from Moschus, Borneolum, respectively, showed various biological activities in vitro and in vivo. Muscone might treat myocardial infarction and protect cardiovascular and cerebrovascular system [3, 4], regulate neuroprotective system [5] and improve osteoarticular injuries [6]. Isoborneol and d-borneol had the characteristics of anti-inflammatory [7], anti-atherosclerosis [8] and promoting penetration [9], and played significant roles in the treatment of cerebrovascular diseases [12]. However, there are few researches on systematical characterization the volatile chemical composition in ANP.
In this study, the volatile constituents in ANP were comprehensively characterized based on the sensitive gas chromatography coupled with mass spectrometry (GC–MS) in vitro and in vivo. The GC–MS method was complemented for the volatile compounds identification based on database matching, retention indices and standard references confirmation. Then, 21 compounds were quantified in 8 batches of ANP by gas chromatography-tandem mass spectrometry (GC–MS/MS), and the batch-to-batch similarity was evaluated by Pearson correlation coefficient (PCC) analysis. Furthermore, the volatile constituent of ANP in vivo were characterized in the plasma of rats which was single oral administrated. To our knowledge, the determination of main volatile compounds in ANP was reported for the first time. It is hoped that the results can provide a valuable reference for quality control and clinical efficacy research of ANP.
Methods
Reagents and materials
Eight batches of ANP (No. S1–S8) were purchased from Beijing TongRenTang Technologies Co., Ltd and their information was listed in Additional file 1: Table S1. All the ANP samples used artificial Moschus and in vitro cultured Bovis Calculus in their prescription. The reference standards of muscone, α-pinene, limonene, eucalyptol, isoborneol, and d-borneol were obtained from National Institutes for Food and Drug Control (Beijing, China). Acetophenone, fenchol and β-caryophyllene were bought from Shanghai Yuanye Bio-Technology Co., Ltd (Shanghai, China). Camphene, benzaldehyde, α-terpinene, benzeneacetaldehyde, terpinolene, camphor, tridecane, 4-methyl-4-phenyl-2-pentanone, and humulene were acquired from Chengdu Push Bio-Technology Co., Ltd (Chengdu, China). ar-Tumerone was purchased from BioBioPha Co., Ltd. (Kunming, China). The standard mix of n-alkanes (C7–C40) was obtained from Sigma-Aldrich (St. Louis, MO, USA). (+)-3-Carene was bought from Toronto Research Chemicals (Toronto, ON, Canada). β-Pinene was acquired from Dr. Ehrensdorfer GmbH (Augsburg, Germany). α-Curcumene was purchased from Extrasynthese (Lyon Nord, France). The purities of all used reference standards were higher than 95%.
Anhydrous ethanol and ethyl acetate (HPLC grade) were purchased from Yonghua Chemical Technology Co., Ltd (Suzhou, China). Distilled water was prepared using a Milli-Q Integral water purification system (Millipore, Bedford, MA, USA). Other reagents were analytical grade.
Preparation of standard and sample solutions
The 21 reference standards were dissolved with anhydrous ethanol respectively to prepare the corresponding stock solutions at the concentration of 1 mg/mL. An appropriate amount of individual standard stock solutions was mixed into a 10 mL volumetric flask to prepare a mixed standard stock solution, which was diluted with anhydrous ethanol to obtain a series of working solutions at proper concentrations for calibration curves. All working solutions were stored at − 20 °C until analysis.
After ground into fine powder, 1.5 g ANP was accurately weighed and extracted using steam distillation for 4 h with 100 mL distilled water. The volatile oils were collected and residual water was removed with anhydrous sodium sulfate, finally were dissolved in 2 mL ethyl acetate. The solution was directly analyzed after adding n-tridecane as an internal standard (IS). Since some compounds of high contents such as isoborneol, d-borneol, β-caryophyllene, ar-turmerone and muscone were overloaded, the solution was also analyzed after diluted by 40 times with ethyl acetate and added with IS. The n-tridecane in all injection samples was at the final concentration of 14.20 μg/mL.
Collection and precipitation procedure of plasma samples
Male Wistar rats (Animal certificate number: SCXK [HU]-2018-0016) were purchased from Shanghai Lab. Animal Research Center (Shanghai, China). All rats were housed at 24 ± 2 °C on a 12 h light/dark cycle, and fed a standard diet and water for 1 week before the experiment. Then all rats (200 ± 20 g) were randomly divided into two groups: ANP group and control group. The rats were fasted for 12 h prior to experiments but water was provided ad libitum. ANP suspension dissolved in physiological saline was orally administrated to nine rats (ANP group) at a dosage of 8.1 g/kg, and the rest two rats (control group) were orally administered with the same dose of saline respectively. All procedures were carried out in accordance with Guide for the Care and Use of Laboratory Animals (National Institutes of Health).
The blood samples were collected in heparinized 1.5-mL polythene tubes at 0, 0.25, 0.5, 0.75, 1, 1.5, 2 and 4 h after oral administration. At each time point, the blood samples of 3 rats (ANP group) or 2 rats (control group) were mixed into one sample, and were centrifuged immediately at 4500 rpm for 10 min at 4 °C to collect the plasma, which were stored at − 80 °C before analysis. For GC–MS analysis, a 100 μL aliquot of plasma sample was added with 100 μL of ethyl acetate, followed by vortex-mixing for 1 min and centrifugation for 10 min at 13,000 rpm. An aliquot of supernatant was transferred into an injection vial for analysis.
Chromatographic and mass spectrometric conditions
The qualitative analysis was performed on an Agilent 7890B gas chromatography system coupled to an Agilent 5977A quadrupole mass spectrometer (GC–MS, Agilent Technologies, USA). The GC separation was achieved on an Agilent DB-5 MS capillary column (60 m × 0.25 mm i.d.) coated with a 0.25 μm film of 5% phenyl polymethyl siloxane. High-purity helium gas was used as carrier gas, with a flow rate of 1.0 mL/min. The injection and interface temperatures were set to 280 °C and 250 °C, respectively. The column temperature was programmed as follows: the oven was initially maintained at 60 °C for 3 min, sequentially increased to 100 °C at 10 °C/min, increased to 135 °C at 2 °C/min, then increased to 165 °C at 5 °C/min, increased to 168 °C at 1 °C/min, increased to 200 °C at 5 °C/min, held for 2 min, and then increased to 295 °C at 10 °C/min, held constant for 5 min. The split ratio was set to 10:1. The injection volume was 1 μL. The electron energy was set to 70 eV. The source temperature was 230 °C and the quadrupole temperature was 150 °C. The mass data was acquired using full scan mode with a mass range of m/z 50–600 after a solvent delay of 9.1 min. Data acquisition was obtained by Agilent MassHunter GC–MS Acquisition Software Version B.07.03.2129.
For quantitative analysis, the Agilent 7890B GC system equipped with an Agilent 7000D triple quadrupole mass spectrometer (GC–MS/MS, Agilent Technologies, USA) was performed. The Agilent DB-5 MS UI capillary column (30 m × 0.25 mm i.d., 0.25 μm) were used for separation, the initial oven temperature was 60 °C, and raised to 76 °C with 8 °C/min, then increased to 82 °C at the rate of 2 °C/min, and ramped with 15 °C/min to 130 °C, further rose at 20 °C/min to 230 °C and held for 2 min. The injection and interface temperatures were both kept at 250 °C. The carrier gas (helium, > 99.999%) flow rate was set at 1.0 mL/min. The electron energy and source temperature were set to 70 eV and 230 °C, respectively. The flow rate of quenching gas (helium, > 99.999%) and collision gas (nitrogen, > 99.999%) was 2.25 mL/min and 1.5 mL/min, separately. Data acquisition was achieved on Agilent MassHunter Workstation GC/MS Data Acquisition Software Version 10.0.368.
Validation of quantitative method
Calibration curves, LODs and LOQs
After added with an equal amount of internal standard (IS) n-tridecane (final concentration: 14.20 μg/mL), a series of working solutions at multiple concentrations were analyzed. The calibration curves were constructed by plotting the relationships between peak area and concentration of the analytes and IS.
The mixed standard stock solution was further diluted with anhydrous ethanol and analyzed by GC–MS/MS. The concentration of the analyte with signal-to-noise ratio (S/N) of 10 was defined as the limit of quantification (LOQ), and the concentration of the analyte with S/N of 3 was assigned as the limit of detection (LOD).
Precision, repeatability, stability and recovery
The precision was evaluated by the determination of intra- and inter-day variances. The mixed standard solutions at three different concentration levels (low, medium, high) were analyzed for consecutive 3 days and continuous six times per day, and the peak area ratio of each compound and IS was recorded to calculate the relative standard deviation (RSD) value, respectively. Six parallel ANP samples from the same batch were prepared and analyzed for the repeatability test. To confirm the stability, a single sample solution was stored in sample chamber and analyzed at 0, 2, 4, 8, 12 and 24 h, respectively. Recovery test was used to verify the accuracy of the established method. A known amount of mixed reference solution at middle concentration was added in the same sample for six parallel extraction and analysis.
Data analysis
The qualitative analysis was realized on Agilent MassHunter Workstation Qualitative Analysis Software 10.0. The retention indices of all chromatographic peaks were calculated based on the data of C7–C40 n-alkanes acquired with the same GC–MS method. The acquired components were tentatively identified by comparison with mass spectra and retention indices in the National Institute of Standards and Technology (NIST) 2017 library, and some were unambiguously determined by direct comparison with reference standards. Agilent MassHunter Workstation Quantitative Analysis Software Version 10.0 was used for quantitative analysis. Related graphical analysis was conducted on Graphpad Prism 8.02 (San Diego, USA).
The pairwise PCC between batches was based on the vectors of concentrations from each batch as Formula (1).
| 1 |
Here, B1 and B2 represented the vectors of ingredients’ concentration of the first and second batches respectively. Finally, the PCCs were displayed through the correlation heat map, the batch-to-batch similarity was evaluated according to the average value of PCCs among all pairs from batches.
Results and discussion
Characterization of volatile constituents in ANP
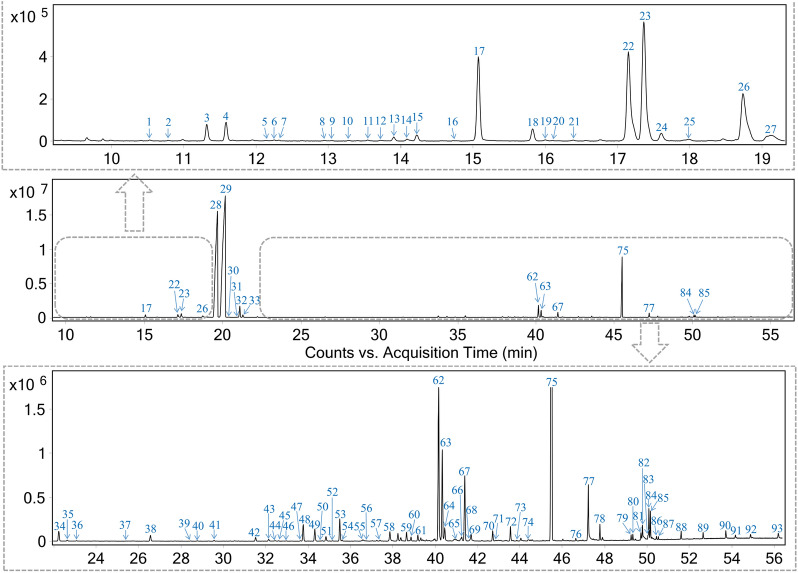
For the qualitative analysis, the temperature-programmed conditions of GC–MS were optimized in terms of resolution, symmetricity and capacity of chromatographic peaks. Then, the mixed reference standard solution and ANP sample solution were analyzed by the optimized GC–MS method, and the total ion chromatogram of the essential oil from ANP is shown in Fig. 1. The volatile constituents of ANP were identified by comparing their mass spectra and retention indices with those of NIST library, and accurately identified by matching with authentic standards. As illustrated in Fig. 1 and Table 1, a total of 93 components, including 29 sesquiterpenoids, 28 monoterpeneoids, 13 fatty acids and their esters, 7 alkanes, 6 ketones, 3 phenols, 3 aldehydes, 2 benzoate esters and 2 other type components, were preliminarily characterized. Among them, 21 compounds were determined by comparison with reference standards. The essential oil was dominated by d-borneol, isoborneol and muscone, making up 90.69% of the identified oil composition.
Fig. 1.
The total ion chromatogram of the essential oil from Angong Niuhuang Pill based on GC–MS
Table 1.
Identification of the chemical constituents in the essential oil of ANP by GC–MS
| No. | tR (min) | Compound | Formula | CAS | RI (measured) | RI (NIST) | Match | Structure type | Source |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 10.53 | Tricyclene | C10H16 | 508-32-7 | 930.02 | 925 | 853 | Monoterpeneoids | B |
| 2 | 10.79 | α-Pinenea | C10H16 | 80-56-8 | 939.35 | 937 | 872 | Monoterpeneoids | GF, CR |
| 3 | 11.32 | Camphenea | C10H16 | 79-92-5 | 958.17 | 952 | 954 | Monoterpeneoids | B, CR |
| 4 | 11.59 | Benzaldehydea | C7H6O | 100-52-7 | 967.74 | 962 | 951 | Aldehydes | GF |
| 5 | 12.13 | β-Pinenea | C10H16 | 127-91-3 | 987.29 | 979 | 847 | Monoterpeneoids | CR |
| 6 | 12.25 | 2-Pentylfuran | C9H14O | 3777-69-3 | 991.45 | 993 | 839 | Furans | GF |
| 7 | 12.32 | 2,2,4,6,6-Pentamethylheptane | C12H26 | 13475-82-6 | 993.74 | 991 | 897 | Alkanes | B |
| 8 | 12.95 | α-Phellandrene | C10H16 | 99-83-2 | 1012.46 | 1005 | 906 | Monoterpeneoids | CR |
| 9 | 13.05 | (+)-3-Carenea | C10H16 | 498-15-7 | 1015.16 | 1010 | 740 | Monoterpeneoids | CR |
| 10 | 13.29 | α-Terpinenea | C10H16 | 99-86-5 | 1021.92 | 1017 | 825 | Monoterpeneoids | CR |
| 11 | 13.54 | p-Cymene | C10H14 | 99-87-6 | 1028.7 | 1025 | 900 | Monoterpeneoids | GF, CR |
| 12 | 13.72 | Limonenea | C10H16 | 138-86-3 | 1033.6 | 1030 | 836 | Monoterpeneoids | GF, CR |
| 13 | 13.9 | Eucalyptola | C10H18O | 470-82-6 | 1038.53 | 1032 | 934 | Monoterpeneoids | GF, CR |
| 14 | 14.09 | β-Isophorone | C9H14O | 471-01-2 | 1043.5 | 1044 | 843 | Ketones | GF |
| 15 | 14.22 | Benzeneacetaldehydea | C8H8O | 122-78-1 | 1047.2 | 1045 | 935 | Aldehydes | GF |
| 16 | 14.73 | r-Terpinene | C10H16 | 99-85-4 | 1061.04 | 1060 | 733 | Monoterpeneoids | CR |
| 17 | 15.07 | Acetophenonea | C8H8O | 98-86-2 | 1070.44 | 1065 | 965 | Ketones | GF |
| 18 | 15.83 | Terpinolenea | C10H16 | 586-62-9 | 1090.9 | 1088 | 935 | Monoterpeneoids | CR |
| 19 | 16.01 | p-Cymenene | C10H12 | 1195-32-0 | 1095.82 | 1090 | 843 | Monoterpeneoids | CR |
| 20 | 16.1 | Fenchone | C10H16O | 1195-79-5 | 1098.36 | 1096 | 810 | Monoterpeneoids | B |
| 21 | 16.39 | Nonanal | C9H18O | 124-19-6 | 1105.11 | 1104 | 872 | Aldehydes | GF |
| 22 | 17.15 | Isofenchol | C10H18O | 6168-62-3 | 1121.75 | – | 918 | Monoterpeneoids | B |
| 23 | 17.37 | Fenchola | C10H18O | 1632-73-1 | 1126.45 | 1113 | 904 | Monoterpeneoids | B |
| 24 | 17.61 | β-Fenchol | C10H18O | 22627-95-8 | 1131.74 | 1116 | 848 | Monoterpeneoids | B |
| 25 | 17.98 | α-Campholenal | C10H16O | 4501-58-0 | 1140.03 | 1125 | 828 | Monoterpeneoids | B |
| 26 | 18.74 | Camphora | C10H16O | 76-22-2 | 1156.5 | 1145 | 930 | Monoterpeneoids | B |
| 27 | 19.12 | Camphene hydrate | C10H18O | 465-31-6 | 1164.88 | 1148 | 925 | Monoterpeneoids | B |
| 28 | 19.67 | Isoborneola | C10H18O | 124-76-5 | 1177.11 | 1157 | 976 | Monoterpeneoids | B |
| 29 | 20.17 | d-Borneola | C10H18O | 464-43-7 | 1188.07 | 1167 | 963 | Monoterpeneoids | B |
| 30 | 20.39 | α,α,3-Trimethylbenzenemethanol | C10H14O | 5208-37-7 | 1192.7 | 1180 | 845 | Alcohols | CR |
| 31 | 20.83 | l-α-Terpineol | C10H18O | 10482-56-1 | 1202.58 | 1190 | 819 | Monoterpeneoids | GF, CR |
| 32 | 21.11 | 2-Bornanol | C10H18O | 10,385-78-1 | 1207.45 | – | 811 | Monoterpeneoids | B |
| 33 | 21.3 | Neoisopulegol | C10H18O | 29141-10-4 | 1211.19 | – | 813 | Monoterpeneoids | B |
| 34 | 22.22 | 4-Methyleneisophorone | C10H14O | 20548-00-9 | 1229.01 | 1242 | 952 | Ketones | GF |
| 35 | 22.64 | Bornyl formate | C11H18O2 | 7492-41-3 | 1236.94 | 1226 | 908 | Monoterpeneoids | B |
| 36 | 23.08 | Isobornyl formate | C11H18O2 | 1200-67-5 | 1245.47 | 1232 | 818 | Monoterpeneoids | B |
| 37 | 25.41 | l-Bornyl acetate | C12H20O2 | 5655-61-8 | 1290.31 | 1284 | 640 | Monoterpeneoids | B |
| 38 | 26.55 | 4-Vinylguaiacol | C9H10O2 | 7786-61-0 | 1314.47 | 1317 | 932 | Phenols | CR |
| 39 | 28.45 | Eugenol | C10H12O2 | 97-53-0 | 1357.5 | 1357 | 819 | Phenols | GF |
| 40 | 28.76 | Benzalacetone | C10H10O | 122-57-6 | 1364.59 | – | 865 | Ketones | GF |
| 41 | 29.56 | 4-Methyl-4-phenyl-2-pentanonea | C12H16O | 7403-42-1 | 1382.7 | – | 769 | Ketones | CR |
| 42 | 31.52 | β-Caryophyllenea | C15H24 | 87-44-5 | 1429.53 | 1419 | 932 | Sesquiterpenoids | CR |
| 43 | 32.13 | Paeonol | C9H10O3 | 552-41-0 | 1444.74 | 1438 | 914 | Phenols | GF |
| 44 | 32.44 | trans-β-Farnesene | C15H24 | 18794-84-8 | 1452.39 | 1457 | 796 | Sesquiterpenoids | CR |
| 45 | 32.61 | Sesquisabinene | C15H24 | 58319-04-3 | 1456.51 | 1464 | 811 | Sesquiterpenoids | CR |
| 46 | 32.98 | Humulenea | C15H24 | 6753-98-6 | 1465.58 | 1454 | 804 | Sesquiterpenoids | CR |
| 47 | 33.65 | 1,3-Cyclohexadiene, 1-(1,5-dimethyl-4-hexenyl)-4-methyl- | C15H24 | 451-55-8 | 1482.09 | 1480 | 876 | Sesquiterpenoids | CR |
| 48 | 33.77 | α-Curcumenea | C15H22 | 644-30-4 | 1485.18 | 1483 | 957 | Sesquiterpenoids | CR |
| 49 | 34.32 | α-Zingiberene | C15H24 | 495-60-3 | 1498.67 | 1495 | 891 | Sesquiterpenoids | CR |
| 50 | 34.57 | α-Farnesene | C15H24 | 502-61-4 | 1505.36 | 1508 | 672 | Sesquiterpenoids | CR |
| 51 | 34.84 | β-Bisabolene | C15H24 | 495-61-4 | 1513.02 | 1509 | 919 | Sesquiterpenoids | CR |
| 52 | 35.15 | Ethylparaben | C9H10O3 | 120–47-8 | 1521.51 | – | 910 | Benzoate esters | M |
| 53 | 35.49 | β-Sesquiphellandrene | C15H24 | 20307-83-9 | 1530.9 | 1524 | 929 | Sesquiterpenoids | CR |
| 54 | 35.61 | trans-γ-Bisabolene | C15H24 | 53585-13-0 | 1534.09 | 1533 | 833 | Sesquiterpenoids | CR |
| 55 | 36.59 | cis-Sesquisabinene hydrate | C15H26O | 58319-05-4 | 1561.06 | 1543 | 857 | Sesquiterpenoids | CR |
| 56 | 36.72 | trans-Nerolidol | C15H26O | 40716-66-3 | 1564.79 | 1564 | 750 | Sesquiterpenoids | CR |
| 57 | 37.39 | ar-Tumerol | C15H22O | 38142-57-3 | 1583.26 | 1583 | 792 | Sesquiterpenoids | CR |
| 58 | 37.86 | trans-Sesquisabinene hydrate | C15H26O | 145,512–84-1 | 1596.08 | 1581 | 900 | Sesquiterpenoids | CR |
| 59 | 38.64 | Zingiberenol | C15H26O | 58334-55-7 | 1620.64 | 1616 | 923 | Sesquiterpenoids | CR |
| 60 | 38.85 | trans-Nuciferol | C15H22O | 39599-18-3 | 1627.39 | – | 712 | Sesquiterpenoids | CR |
| 61 | 39.18 | β-Acorenol | C15H26O | 28400-11-5 | 1637.839241 | 1649 | 808 | Sesquiterpenoids | CR |
| 62 | 40.16 | ar-Tumeronea | C15H20O | 532-65-0 | 1669.3 | 1664 | 949 | Sesquiterpenoids | CR |
| 63 | 40.33 | Tumerone | C15H22O | 180315-67-7 | 1674.84 | 1632 | 935 | Sesquiterpenoids | CR |
| 64 | 40.44 | (Z)-γ-Atlantone | C15H22O | 108549-48-0 | 1678.45 | 1699 | 836 | Sesquiterpenoids | CR |
| 65 | 41 | 4-(1,5-Dimethylhex-4-enyl)cyclohex-2-enone | C14H22O | 1723-80-4 | 1696.24 | 1698 | 848 | Sesquiterpenoids | CR |
| 66 | 41.24 | Bisacurol | C15H24O | 120681-80-3 | 1704.32 | – | 910 | Sesquiterpenoids | CR |
| 67 | 41.4 | Curlone | C15H22O | 82508-14-3 | 1709.55 | – | 948 | Sesquiterpenoids | CR |
| 68 | 41.61 | Curcuphenol | C15H22O | 69301-27-5 | 1716.86 | 1717 | 814 | Sesquiterpenoids | CR |
| 69 | 41.7 | (Z)-α-Atlantone | C15H22O | 56192-70-2 | 1719.91 | 1717 | 915 | Sesquiterpenoids | CR |
| 70 | 42.71 | (6R,7R)-Bisabolone | C15H24O | 72441-71-5 | 1754.45 | 1747 | 936 | Sesquiterpenoids | CR |
| 71 | 42.82 | Tetradecanoic acid | C14H28O2 | 544-63-8 | 1758.18 | 1768 | 780 | Fatty acids and their esters | GF |
| 72 | 43.55 | (−)-(E)-α-Atlantone | C15H22O | 108645-54-1 | 1783.13 | 1773 | 927 | Sesquiterpenoids | CR |
| 73 | 43.85 | Ethyl myristate | C16H32O2 | 124-06-1 | 1793.15 | 1794 | 665 | Fatty acids and their esters | GF |
| 74 | 44.39 | Turmeronol B | C15H20O2 | 131651-38-2 | 1815.66 | – | 763 | Sesquiterpenoids | CR |
| 75 | 45.5 | Musconea | C16H30O | 541-91-3 | 1867.53 | – | 929 | Ketones | M |
| 76 | 46.64 | Methyl palmitate | C17H34O2 | 112-39-0 | 1925.78 | 1926 | 868 | Fatty acids and their esters | M, GF |
| 77 | 47.23 | Palmitic acid | C16H32O2 | 10/3/1957 | 1960.36 | 1968 | 957 | Fatty acids and their esters | M, GF |
| 78 | 47.78 | Ethyl palmitate | C18H36O2 | 628-97-7 | 1992.48 | 1993 | 915 | Fatty acids and their esters | B, M, GF, CR |
| 79 | 49.25 | Methyl linoleate | C19H34O2 | 112-63-0 | 2094.97 | 2092 | 904 | Fatty acids and their esters | GF |
| 80 | 49.33 | Methyl oleate | C19H36O2 | 112-62-9 | 2100.76 | 2091 | 846 | Fatty acids and their esters | M, GF |
| 81 | 49.72 | Linoleic acid | C18H32O2 | 60-33-3 | 2132.12 | 2133 | 900 | Fatty acids and their esters | M, GF |
| 82 | 49.79 | Oleic acid | C18H34O2 | 112–80-1 | 2138.03 | 2141 | 887 | Fatty acids and their esters | M, GF |
| 83 | 50.05 | Stearic acid | C18H36O2 | 11/4/1957 | 2159.94 | 2172 | 842 | Fatty acids and their esters | M, GF |
| 84 | 50.09 | Ethyl linoleate | C20H36O2 | 544-35-4 | 2163.23 | 2162 | 937 | Fatty acids and their esters | M |
| 85 | 50.17 | Ethyl oleate | C20H38O2 | 111-62-6 | 2169.06 | 2173 | 905 | Fatty acids and their esters | M |
| 86 | 50.45 | Ethyl stearate | C20H40O2 | 111-61-5 | 2192.34 | 2195 | 811 | Fatty acids and their esters | B |
| 87 | 50.54 | Docosane | C22H46 | 629-97-0 | 2199.89 | 2200 | 855 | Alkanes | GF |
| 88 | 51.62 | Tricosane | C23H48 | 638-67-5 | 2299.86 | 2300 | 880 | Alkanes | GF |
| 89 | 52.65 | Tetracosane | C24H50 | 646-31-1 | 2399.86 | 2400 | 886 | Alkanes | GF |
| 90 | 53.72 | Pentacosane | C25H52 | 629-99-2 | 2499.78 | 2500 | 878 | Alkanes | GF |
| 91 | 54.17 | Di(2-propylpentyl) phthalate | C24H38O4 | 70910-37-1 | 2538.21 | 2527 | 911 | Benzoate esters | GF |
| 92 | 54.89 | Hexacocane | C26H54 | 630-01-3 | 2599.7 | 2600 | 873 | Alkanes | GF |
| 93 | 56.2 | Heptacosane | C27H56 | 593-49-7 | 2699.46 | 2700 | 851 | Alkanes | GF |
The batch of ANP used for qualification was S7
Sources: B Borneolum, M Moschus, CR Curcumae Radix, GF Gardeniae Fructus
–: The RI was not found in NIST library
aThe identification was confirmed with reference standards
Among the 93 preliminarily identified volatile compounds, 11 components might be derived from Moschus, including 1 ketone, 1 benzoate ester and 9 fatty acids and their esters. The most abundant composition in Moschus was muscone (Peak 75) [13], which was also one of the principal constituents in ANP. Furthermore, 19 compounds comprising 16 monoterpeneoids, 2 fatty acid esters and 1 alkane, were tentatively assigned to Borneolum, of which the highest were d-borneol (Peak 29) and isoborneol (Peak 28) [7]. Additionally, 46 components were originated from Curcumae Radix, consisting of 29 sesquiterpenoids, 13 monoterpeneoids, 1 phenol, 1 ketone, 1 fatty acid ester, and 1 alcohol. Chinese Pharmacopoeia recorded its four botanical origins, including Curcuma wenyujin Y. H. Chen et C. Ling, Curcuma longa L., Curcuma phaeocaulis Val. and Curcuma kwangsiensis S. G. Lee et C. F. Liang. Sesquiterpenoid was one of the most abundant types in Curcumae Radix. Baesd on the characteristic constituents including ar-Tumerone (Peak 62), β-caryophyllene (Peak 42) and α-curcumene (Peak 48), the Curcumae Radix in those ANP could be traced to Curcuma longa L. [14–16]. Furthermore, 32 volatile components in ANP could be sourced from Gardeniae Fructus, containing 10 fatty acids and their esters, 6 alkanes, 5 monoterpeneoids, 4 ketones, 3 aldehydes, 2 phenols, and 1 furan and 1 benzoate ester. The constituents containing “-cyclohexane-trimethyl-” group represented by 4-methyleneisophorone (Peak 34) and β-Isophorone (Peak 14) might be the characteristic aromatic compounds in Gardeniae Fructus [17], which were detected in ANP. The detailed sources of volatile constituents in ANP are shown in Table 1 and Additional file 2: Fig. S1.
Quantitative analysis of representative volatile constituents in ANP
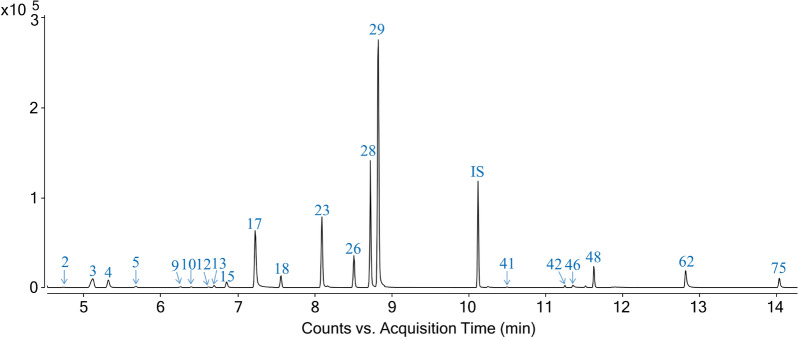
For the quantitative analysis, a temperature-programmed process of GC–MS/MS for 21 volatile constituents was developed within 15 min. A dynamic multiple reaction monitoring (dMRM) pattern was selected for quantification. As an alternative for multiple reaction monitoring, dMRM can monitor analytes automatically around the expected retention time, without defining a specific time period for the selected transitions, thereby decreasing concurrent transitions and improving the sensitivity [18, 19]. The segmented dMRM chromatogram of 21 target compounds is shown in Fig. 2. The dMRM parameters for all analytes and IS are presented in Additional file 1: Table S2.
Fig. 2.
The segmented dMRM chromatogram of 21 target compounds and internal standard based on GC–MS/MS
Method validation
The results of methodological study are shown in Additional file 1: Tables S3, S4. For the calibration curve established, all analytes showed good linearity within their linear ranges and their correlation coefficient R2 values varied from 0.9918 to 0.9997. The LODs and LOQs ranged from 0.60 to 150.40 ng/mL and from 6.00 to 451.20 ng/mL, respectively, indicating this method was sensitive enough for the quantitative analysis of the major volatile constituents of ANP. The RSD values of the intra- and inter-day were in the ranges of 0.04–5.84% and 0.48–6.83%, respectively. The RSD values for repeatability of all compounds ranged from 1.13 to 9.00%, which showed that the repeatability of tested samples was good. The RSD values for stability of all analytes were with the range of 1.39–6.70%, indicating that the samples in sample chamber were relatively stable within 24 h. The overall recoveries of 21 compounds were in a range of 90.80–109.83% with RSD values less than 8.68%, which indicated the verified method was accurate for quantification. The results demonstrated that the developed quantitative method was sensitive, rapid, accurate and reproducible for determination of representative volatile constituents in ANP.
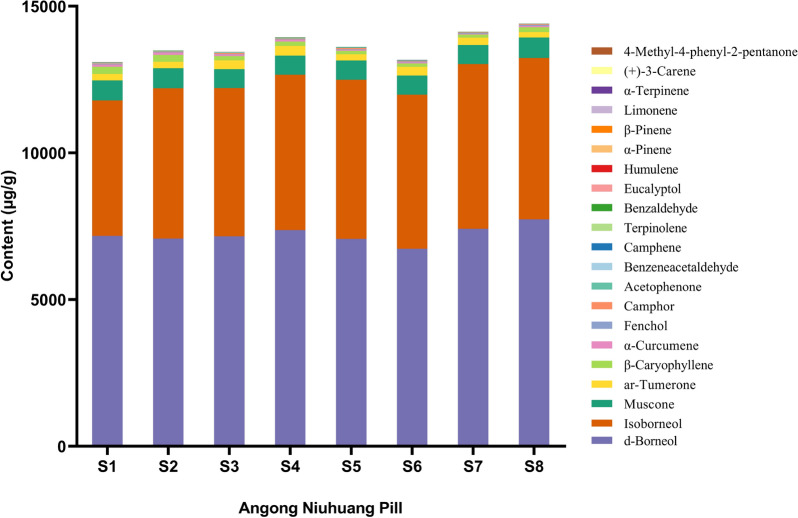
Contents of representative volatile constituents in ANP
In total, eight batches of ANP were analyzed by the developed and verified GC–MS/MS method, and the quantitative results are presented in Fig. 3 and Additional file 1: Table S5. It was found that d-borneol (6727.63–7734.92 μg/g), isoborneol (4614.45–5620.61 μg/g) and muscone (637.90–694.74 μg/g) were the top three abundant ingredients in all batches of ANP samples, making up 95% of the total contents at least. Notably, the characteristic ar-tumerone (186.33–324.22 μg/g), β-caryophyllene (106.81–244.95 μg/g), and α-curcumene (20.16–80.29 μg/g) were of high content level. The content of each component varied greatly, while the content distribution of each component in the eight batches was relatively consistent.
Fig. 3.
The content of 21 volatile compounds in 19 batches of ANP samples
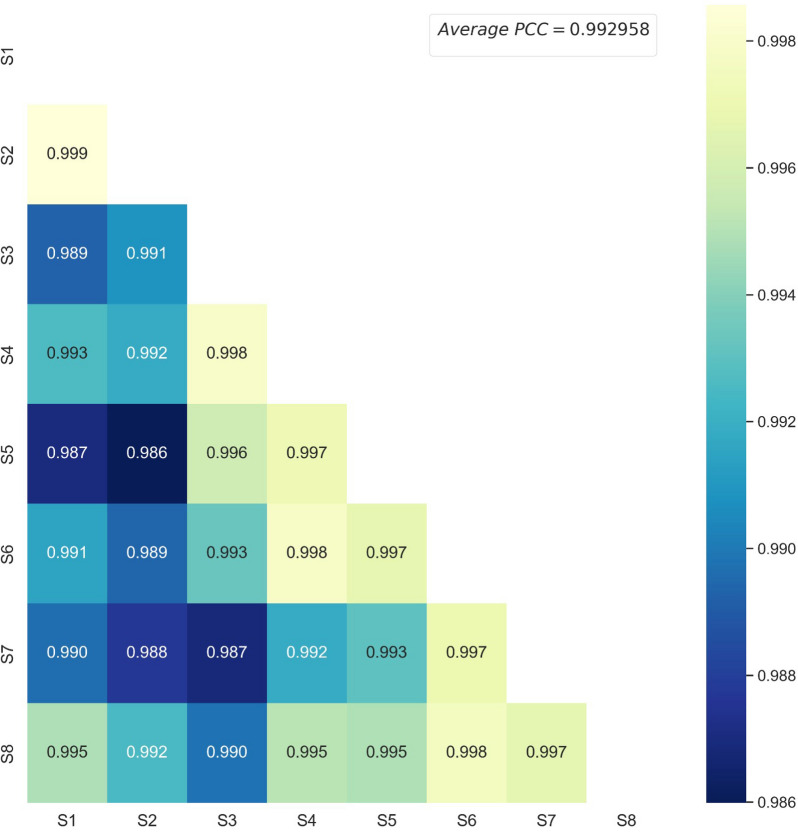
Batch-to-batch similarity evaluation of ANP samples
In order to evaluate the batch-to-batch similarity of multiple ANP samples, the quantitative data of 8 batches were subjected to PCC analysis. For the sake of reducing the concentration distribution difference of different components, the concentrations were processed with logarithm first. Furthermore, the concentration heat map of eight batches was displayed in Additional file 2: Fig. S2, indicating that the concentration distribution of these batches are generally similar. Subsequently, the batch-to-batch similarity was quantified by constructing the correlation coefficient matrix, and the heat map of it was shown in Fig. 4. It could be found that the average PCC was 0.993, and even the lowest PCC between S2 and S5 was also more than 0.986, further revealing the high similarity among the eight batches.
Fig. 4.
The heat map of Pearson correlation coefficients between 8 batches
Characterization of volatile constituents of ANP in vivo
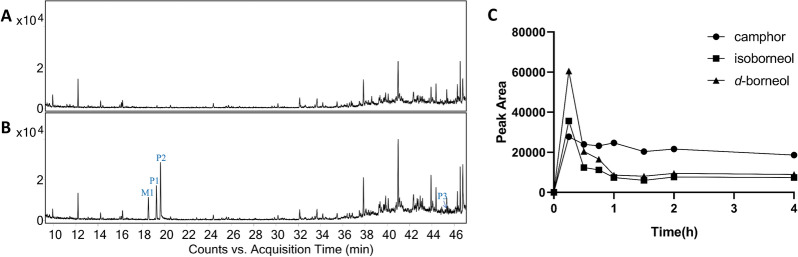
To clarify the absorbed volatile component in vivo, the rat plasma after oral administration of ANP were analyzed by the developed GC–MS method. Since ANP was a classic first-aid Chinese patent medicine, single administration was performed. As shown in Fig. 5A, B, four absorbed components from ANP were characterized in 0.25 h, including three prototypes (P1–P3) and one metabolite (M1). By comparison with the retention time and mass spectral data of the reference standards, M1, P1, P2, and P3 were assigned to camphor, isoborneol (28), d-borneol (29) and muscone (75), respectively (Table 2), and their relative plasma concentration profiling in 0.25 to 4 h were depicted in Fig. 5C. The relative plasma concentration profiling of muscone could not be displayed because the content of muscone was extremely low at 0.25–4 h. The volatile constituents of most two high content in ANP were quickly absorbed after oral administration, and then decreased rapidly. While the content of camphor, the 2-position oxide of isoborneol and borneol [20, 21], remained relatively stable within 4 h, suggesting that isoborneol and borneol may be gradually metabolized into camphor. Curiously, no metabolites of muscone were detected, which were consistent with previously reports [22, 23]. Additionally, few metabolites were characterized partly because that single administration not accumulated the drug in vivo.
Fig. 5.
The total ion chromatograms of blank plasma sample (A) and administered plasma sample (B) at 0.25 h; C mean peak area-time curves for camphor, isoborneol and d-borneol in rats after oral administration of Angong Niuhuang Pill (n = 3)
Table 2.
Identification of the absorbed constituents in rat plasma after oral administration of ANP by GC–MS
| No | tR (min) | Compound | Formula | CAS | Structure type | Source |
|---|---|---|---|---|---|---|
| M1 | 18.54 | Camphora | C10H16O | 76-22-2 | Monoterpenes | B |
| P1 | 19.27 | Isoborneola | C10H18O | 124-76-5 | Monoterpenes | B |
| P2 | 19.63 | d-Borneola | C10H18O | 464-43-7 | Monoterpenes | B |
| P3 | 45.32 | Musconea | C16H30O | 541-91-3 | Ketones | M |
Sources: B Borneolum, M Moschus
aThe identification was confirmed with reference standards
Most notably, isoborneol, d-borneol and muscone played significant roles in the treatment of cerebrovascular diseases, corresponding to the main efficacy of ANP. Dong et al. [12] found that isoborneol and d-borneol may improve the function of neurovascular units through anti-apoptotic and anti-inflammatory properties so as to exert their protective effects against cerebral ischemia injury. Moreover, borneol and muscone acted as absorption enhancers in the blood–brain barrier by increasing paracellular and transcellular transport [11, 24, 25]. Muscone have been reported that could mediate neuroprotective effects against cerebral ischemia by preventing oxidative stress and Ca2+ influx [10]. When combined with other drugs, they can effectively promote the penetration of drugs through the blood–brain barrier, which is of great significance for the development of treating cerebrovascular diseases.
Conclusion
In this study, GC–MS and GC–MS/MS were used to conduct a comprehensive qualitative and quantitative analysis of the representative volatile constituents in commercial ANP. Combined with retention indices and reference standards, the chemical characteristics of volatile constituents in ANP were described comprehensively and systematically for the first time. A total of 93 volatile components, assigned to four aromatic Chinese medicine, were preliminarily identified in ANP. Among them, 21 volatile components were selected and accurately quantified within 15 min based on the established GC–MS/MS method, in which d-borneol, isoborneol and muscone were the top three abundant ingredients in the ANP. According to the contents of 21 determined constituents, 8 batches of ANP were generally chemical similar based on PCC analysis. In addition, d-borneol, isoborneol and muscone and one metabolite (camphor) were found in rat plasma after single oral administration, suggesting that these prototypes and their metabolites could be potential bioactive substances of ANP. Collectively, this study provides a comprehensive information of volatile component of ANP in vitro and in vivo, which may helpful for the quality evaluation and pharmacological research of ANP. Meanwhile, the non-volatile constituents were also important for its holistic efficacy, which need further investigated using the appropriate analytical method.
Supplementary Information
Additional file 1: Table S1. The information on eight batches of commercially available ANP samples. Table S2. Dynamic multiple reaction monitoring parameters of all analytes and internal standard. Table S3. Calibration curves, LODs and LOQs of 21 volatile analytes in ANP samples. Table S4. Intra-day precision, inter-day precision, repeatability, stability and recovery of 21 volatile analytes in ANP samples. Table S5. Contents of 21 volatile analytes in ANP samples (μg/g, mean ± SD, n = 4).
Additional file 2: Figure S1. The sources of volatile constituents in ANP samples. Figure S2. The concentration heat map of 21 volatile analytes in ANP samples from eight batches.
Acknowledgements
The authors thank Hui-Ying Wang (State Key Laboratory of Natural Medicines, China) for the technical assistance.
Abbreviations
- ANP
Angong Niuhuang Pill
- TCM
Traditional Chinese medicine
- GC–MS
Gas chromatography coupled with mass spectrometry
- GC–MS/MS
Gas chromatography coupled with tandem mass spectrometry
- IS
Internal standard
- S/N
Signal-to-noise ratio
- LOQ
Limit of quantification
- LOD
Limit of detection
- RSD
Relative standard deviation
- NIST
National Institute of Standards and Technology
- PCC
Pearson correlation coefficient
- dMRM
Dynamic multiple reaction monitoring
Author contributions
PL and WG conceived and designed the study; YJ, JL and MD performed the experiment; YJ prepared the manuscript; ZFG analyzed the data; HY and HJL revised the manuscript; WG finalized the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81730104).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with the ethical guidelines and approved by the Ethics Committee on Laboratory Animal Management of China Pharmaceutical University.
Consent for publication
Not applicable.
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Wen Gao, Email: gw_cpu@126.com.
Ping Li, Email: liping2004@126.com.
References
- 1.Guo Y, Yan SH, Xu LP, Zhu GX, Yu XT, Tong XL. Use of Angong Niuhuang in treating central nervous system diseases and related research. Evid Based Complement Alternat Med. 2014;2014:346918. doi: 10.1155/2014/346918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu HW, Yan Y, Pang PF, Mao JJ, Hu XJ, Li D, Zhou B, Shan H. Angong Niuhuang Pill as adjuvant therapy for treating acute cerebral infarction and intracerebral hemorrhage: a meta-analysis of randomized controlled trials. J Ethnopharmacol. 2019;237:307–313. doi: 10.1016/j.jep.2019.03.043. [DOI] [PubMed] [Google Scholar]
- 3.Wu QB, Li HT, Wu Y, Shen WX, Zeng L, Cheng HB, He L. Protective effects of muscone on ischemia–reperfusion injury in cardiac myocytes. J Ethnopharmacol. 2011;138:34–39. doi: 10.1016/j.jep.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 4.Du YQ, Gu X, Meng HY, Nan A, Liu SY, Peng CY, Ge YB, Yang ZJ. Muscone improves cardiac function in mice after myocardial infarction by alleviating cardiac macrophage-mediated chronic inflammation through inhibition of NF-κB and NLRP3 inflammasome. Am J Transl Res. 2018;10:4235–4246. [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou LY, Yao M, Tian ZR, Liu SF, Song YJ, Ye J, Li G, Sun YL, Cui XJ, Wang YJ. Muscone suppresses inflammatory responses and neuronal damage in a rat model of cervical spondylotic myelopathy by regulating Drp1-dependent mitochondrial fission. J Neurochem. 2020;155:154–176. doi: 10.1111/jnc.15011. [DOI] [PubMed] [Google Scholar]
- 6.Zhai X, Yan ZJ, Zhao J, Chen K, Yang YL, Cai MX, He C, Huang CY, Li B, Yang MY, Zhou XY, Zhao YC, Wei XZ, Bai YS, Li M. Muscone ameliorates ovariectomy-induced bone loss and receptor activator of nuclear factor-κb ligand-induced osteoclastogenesis by suppressing TNF receptor–associated factor 6-mediated signaling pathways. Front Pharmacol. 2020;11:348. doi: 10.3389/fphar.2020.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou L, Zhang Y, Li W, Zhang JM, Wang D, Fu J, Wang P. Comparison of chemical profiles, anti-inflammatory activity, and UPLC-Q-TOF/MS-based metabolomics in endotoxic fever rats between synthetic borneol and natural borneol. Molecules. 2017;22:1446. doi: 10.3390/molecules22091446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang YF, Li ZR, Liu BX, Wu RM, Gong HF, Su ZH, Zhang SD. Isoborneol attenuates low-density lipoprotein accumulation and foam cell formation in macrophages. Drug Des Devel Ther. 2020;14:167–173. doi: 10.2147/DDDT.S233013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang C, Guo SJ, Wu XW, Yang PS, Han L, Dai XX, Shi XY. Multiscale study on the enhancing effect and mechanism of borneolum on transdermal permeation of drugs with different log P values and molecular sizes. Int J Pharm. 2020;580:119225. doi: 10.1016/j.ijpharm.2020.119225. [DOI] [PubMed] [Google Scholar]
- 10.Yu LC, Wang N, Zhang YF, Wang Y, Li J, Wu Q, Liu YF. Neuroprotective effect of muscone on glutamate-induced apoptosis in PC12 cells via antioxidant and Ca2+ antagonism. Neurochem Int. 2014;70:10–21. doi: 10.1016/j.neuint.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Wang GY, Wang N, Liao HN. Effects of muscone on the expression of P-gp, MMP-9 on blood–brain barrier model in vitro. Cell Mol Neurobiol. 2015;35:1105–1115. doi: 10.1007/s10571-015-0204-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong TW, Chen N, Ma X, Wang J, Wen J, Xie Q, Ma R. The protective roles of l-borneolum, d-borneolum and synthetic borneol in cerebral ischaemia via modulation of the neurovascular unit. Biomed Pharmacother. 2018;102:874–883. doi: 10.1016/j.biopha.2018.03.087. [DOI] [PubMed] [Google Scholar]
- 13.Jiang QY, Luo Y, Tan T, Yang M, Liao ZG. Comparison of volatile chemical compositions of Moschus from different species and producing areas by GC–MS and chemometric analysis. Chin J Exp Tradit Med Form. 2018;24:49–55. [Google Scholar]
- 14.Hu YC, Kong WJ, Yang XH, Xie LW, Wen J, Yang MH. GC–MS combined with chemometric techniques for the quality control and original discrimination of Curcumae longae rhizome: analysis of essential oils. J Sep Sci. 2014;37:404–411. doi: 10.1002/jssc.201301102. [DOI] [PubMed] [Google Scholar]
- 15.Wang L, Li X, Wang Y, Ren XY, Liu XY, Dong Y, Ma JM, Song RL, Wei J, Yu AX, Fan QQ, Shan DJ, Yao JL, She GM. Rapid discrimination and screening of volatile markers for varietal recognition of Curcumae radix using ATR-FTIR and HS-GC-MS combined with chemometrics. J Ethnopharmacol. 2021;280:114422. doi: 10.1016/j.jep.2021.114422. [DOI] [PubMed] [Google Scholar]
- 16.Zhang LY, Yang ZW, Chen DK, Huang ZB, Li YL, Lan XZ, Su P, Pan WY, Zhou W, Zheng X, Du ZY. Variation on composition and bioactivity of essential oils of four common Curcuma herbs. Chem Biodivers. 2017;14:e1700280. doi: 10.1002/cbdv.201700280. [DOI] [PubMed] [Google Scholar]
- 17.Fang JY, Yang B, Ge ZW, Bai X, Yan BJ. Single standard substance for the determination of nine volatile components in the distillate of Fructus Gardeniae and Radix Curcumae (an intermediate of Xingnaojing injection) J Sep Sci. 2017;40:3946–3957. doi: 10.1002/jssc.201700593. [DOI] [PubMed] [Google Scholar]
- 18.Liang J, Wu WY, Sun GX, Wang DD, Hou JJ, Yang WZ, Jiang BH, Liu X, Guo DA. A dynamic multiple reaction monitoring method for the multiple components quantification of complex traditional Chinese medicine preparations: Niuhuang Shangqing pill as an example. J Chromatogr A. 2013;1294:58–69. doi: 10.1016/j.chroma.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 19.Andrade GCRM, Monteiro SH, Francisco JG, Figueiredo LA, Botelho RG, Tornisielo VL. Liquid chromatography–electrospray ionization tandem mass spectrometry and dynamic multiple reaction monitoring method for determining multiple pesticide residues in tomato. Food Chem. 2015;175:57–65. doi: 10.1016/j.foodchem.2014.11.105. [DOI] [PubMed] [Google Scholar]
- 20.Cheng C, Liu XW, Du FF, Li MJ, Xu F, Wang FQ, Liu Y, Li C, Sun Y. Sensitive assay for measurement of volatile borneol, isoborneol, and the metabolite camphor in rat pharmacokinetic study of Borneolum (Bingpian) and Borneolum syntheticum (synthetic Bingpian) Acta Pharmacol Sin. 2013;34:1337–1348. doi: 10.1038/aps.2013.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mu JQ, Gao X, Li Q, Yang XM, Yang WL, Sun X, Bi KS, Zhang HF. Vortex-ultrasound-assisted dispersive liquid–liquid microextraction coupled with gas chromatography–mass spectrometry for the analysis of volatile bioactive components and comparative pharmacokinetic study of the herb–herb interactions in Guanxin Shutong capsule. J Sep Sci. 2017;40:3267–3278. doi: 10.1002/jssc.201700500. [DOI] [PubMed] [Google Scholar]
- 22.Chang WL, Han L, Huang HM, Wen B, Peng CC, Lv C, Zhang WD, Liu RH. Simultaneous determination of four volatile compounds in rat plasma after oral administration of Shexiang Baoxin pill (SBP) by HS-SPDE-GC–MS/MS and its application to pharmacokinetic studies. J Chromatogr B. 2014;963:47–53. doi: 10.1016/j.jchromb.2014.05.047. [DOI] [PubMed] [Google Scholar]
- 23.Xu W, Zhang YP, Zhou CJ, Tai YN, Zhang XQ, Liu J, Sha M, Huang MQ, Zhu YL, Peng J, Lu JJ. Simultaneous quantification six active compounds in rat plasma by UPLC–MS/MS and its application to a pharmacokinetic study of Pien-Tze-Huang. J Chromatogr B. 2017;1061–1062:314–321. doi: 10.1016/j.jchromb.2017.07.033. [DOI] [PubMed] [Google Scholar]
- 24.Chen ZZ, Lu Y, Du SY, Shang KX, Cai CB. Influence of borneol and muscone on geniposide transport through MDCK and MDCK-MDR1 cells as blood–brain barrier in vitro model. Int J Pharm. 2013;456:73–79. doi: 10.1016/j.ijpharm.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 25.Wu JY, Li YJ, Yang L, Hu YY, Hu XB, Tang TT, Wang JM, Liu XY, Xiang DX. Borneol and Α-asarone as adjuvant agents for improving blood–brain barrier permeability of puerarin and tetramethylpyrazine by activating adenosine receptors. Drug Delivery. 2018;25:1858–1864. doi: 10.1080/10717544.2018.1516005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. The information on eight batches of commercially available ANP samples. Table S2. Dynamic multiple reaction monitoring parameters of all analytes and internal standard. Table S3. Calibration curves, LODs and LOQs of 21 volatile analytes in ANP samples. Table S4. Intra-day precision, inter-day precision, repeatability, stability and recovery of 21 volatile analytes in ANP samples. Table S5. Contents of 21 volatile analytes in ANP samples (μg/g, mean ± SD, n = 4).
Additional file 2: Figure S1. The sources of volatile constituents in ANP samples. Figure S2. The concentration heat map of 21 volatile analytes in ANP samples from eight batches.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.