Abstract
Background and Aims
Fluid loss due to diarrhea remains a significant cause of mortality among children under the age of 5.
Methods
Oral rehydration therapy (ORT) is a first‐line therapeutic measure to compensate the volume loss due to diarrhea and vomiting among gastroenteritis patients. Despite adequate knowledge, the practice of ORT is limited, particularly in developing countries.
Results
Several recommendations are provided regarding the use of ORT to treat hypovolemia, however, the information regarding its adequate usage is restricted within the healthcare centers and professionals.
Conclusion
This review highlights the importance of providing recommendations regarding the use of ORT. We also discuss the barriers and alternatives that might limit its use.
Keywords: children, diarrhea, fluid loss, gastroenteritis, hypovolemia, oral rehydration therapy (ORT)
1. INTRODUCTION
Diarrhea is responsible for 7,600,000 deaths, worldwide, among children aged <5 years. 1 Survival of children suffering from hypovolemic shock depends greatly on the promptness of the treatment. Poorly managed cases have been reported with organ damage, acidosis, kidney failure, and death. Diarrhea‐associated hypovolemia is the second leading cause of death among the children aged below 5 years. Volume loss is characterized by reduction in the volume of intracellular fluid and is mainly associated with loss of sodium and water. 2 , 3 , 4
The words volume depletion (i.e., hypovolemia) and dehydration are often used interchangeably. However, these terms vary in terms of the physiological conditions resulting from different types of fluid loss. Similar to other research practice, 5 we throughout the text these terms will be used interchangeably (Figure 1).
Figure 1.
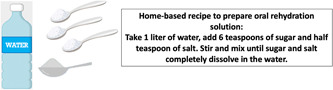
Describes the recipe of home‐made oral rehydration solution
Oral rehydration therapy (ORT), first introduced in 1960s, 6 is a gold standard for treating fluid loss as a result of acute diarrhea. 7 Oral rehydration solution (ORS) is composed of iso‐osmolar glucose electrolyte solution with base and citrate that is administered to treat dehydration and metabolic acidosis. 8 , 9 The use of ORS has reduced the incidence of associated morbidities and mortalities, however, over the period of past 30 years, its use remains low or unchanged in many regions of the world. 9 , 10 According to the monography by UNICEF in 2009, the overall use of ORS was reported to be 33% in developing countries, which could also indicate the possibility of increased child mortality due to diarrhea. 1 , 11 , 12 , 13
Three significant scientific observation contributed chiefly to the development of ORS: (1) requirement of sodium for the absorption of glucose in small intestine and increase in the absorption of sodium following the presence of luminal glucose, (2) enterotoxin of cholera does not decrease fluid and sodium absorption by the action of intracellular cyclic AMP (adenosine monophosphate), and (3) treatment of acute diarrhea in the field during Bangladesh war in 1970. 8 Additionally, later outbreaks of cholera in Peru and Rwanda proved its efficacy. 14
The following variations of ORS are declared by the World Health Organization (WHO).
1.1. Carrier organic solute
In ORS formula suggested by WHO, glucose is used as an organic solvent carrier for sodium transport (Table 1). Although some promising solutions (e.g., zinc, probiotics, glucose polymers, l‐isoleucine, dextrose) have shown effective results, 15 , 16 there are no definitive data for more routine use. 17 , 18
Table 1.
Oral rehydration solutions (ORS) that are commonly used
| Osmolality |
mEq/l Sodium |
Potassium | Open (bicarbonate) | Carbohydrate (g/l) | |
|---|---|---|---|---|---|
| ORS | |||||
| 235 | 10 | 20 | 70 | 40 | Serilate |
| 200 | 30 | 25 | 50 | 30 | Inhalation |
| 250 | 30 | 20 | 45 | 25 | Pediality |
| 310 | 30 | 20 | 75 | 25 | Leadership |
| 310 | 30 | 30 | 90 | 20 | WHO 1975 |
| 245 | 30 | 20 | 75 | 13.5 | WHO 2002 |
| Commonly used drinks (not suitable for supplemental treatment) | |||||
| 700 | 0 | 20 | 3 | 150−100 | Apple juice |
| 450 | 0 | 5 | 250 | 0 | chicken soup |
| 550 | 13 | 0.1 | 2 | 150−100 | Cola |
| 330 | 3 | 3 | 20 | 45 | Processed herbal extracts |
| 565 | 3.6 | 0.1 | 3.5 | 90 | Ginger juice |
| 5 | 0 | 0 | 0 | 0 | Tea |
1.2. Polymer‐based formulas
In polymer‐based ORS, rice, wheat, and corn are used as starch sources for glucose. Starch is slowly broken down into glucose molecules by amylase in the small intestine. A systematic review showed that polymer‐based ORS was more effective in reducing fecal volume and duration of diarrhea in patients with acute cholera‐induced diarrhea or other causes than ORS with glucose‐based ORs. 19 However, there is insufficient data to show that the polymer‐based ORS is superior to the lower osmolality glucose‐based ORS.
2. CLINICAL MANAGEMENT OF DEHYDRATION
ORT is the preferred treatment for fluid and electrolyte loss due to diarrhea caused by gastroenteritis in children with mild to moderate dehydration. ORT is used to treat gastroenteritis‐induced hypovolemia independent of age, causative agent, or initial sodium content. 20 ORS with reduced osmolarity 250 mOsm/L or less, WHO approved, decreases episodes of diarrhea, vomiting, and need for intravenous (IV) rehydration therapy. 21 However, there were early concerns that decreased osmolality of the ORS may cause hyponatremia in patients with cholera who often have high levels of sodium diarrhea. A large descriptive study was conducted in Bangladesh that reported incidence of symptomatic hyponatremia in both the pediatric and adult groups in the study population where only 20% of cholera patients were reported. 22 The findings suggested that ORS with reduced osmolality is also effective to treat patients with acute diarrhea.
ORT can be used at home or under medically supervised conditions.
2.1. Home
If patients' caregivers have adequate knowledge to diagnose the clinical symptoms of volume loss, ORT can be used at home, leading to less frequent visits to the office or emergency room for hypovolemia. A ready‐made commercial standard of prepared ORS (in powdered form) is recommended for use in nonmedical facilities as serious hazards may occur when using home‐based instructions with sugar and sodium (Table 1). 23 , 24
2.2. Medical supervised conditions
Before initiating an ORT, a child being brought to a health, or emergency care center with diarrhea should be evaluated for the cause of the diarrhea and whether further diagnostic tests or interventions are necessary. If there is evidence that resuscitation is appropriate, ORT should be started using standard commercial formula, if there is mild to moderate hypovolemia. ORT is generally based on the degree of dehydration of the body.
2.3. Evaluation of dehydration
After deciding to initiate fluid therapy, clinical evaluation of the patient's hydration status is necessary, as it determines clinical decisions on the use of ORT in individuals with the following characteristics:
Identify patients who are not dehydrated and can be transferred home using ORT.
Identify patients with moderate to low dehydration, where ORT is the preferred treatment for resuscitation.
Identify patients with severe dehydration who need fluid replacement.
Although attempts have been made to distinguish between mild to moderate dehydration (Table 2), it is still difficult to distinguish clinically between the two degrees of dehydration. 25 As a result, experts in the field group these patients and use a similar management approach when symptoms are overlapped, involving a wide range of dehydration (3%–9% volume reduction).
Table 2.
Clinical symptoms of dehydration in infants and children
| Findings | Mild (3%–5%) | Moderate (6%–9%) | Severe (10%) |
|---|---|---|---|
| In case of 3%–9% water loss, ORT is required. Rehydration phase: administration of 50–100 ml/kg ORS every 4 h. | Volume loss ≥10% | ||
| Maintenance phase: nutrition and fluids should be resumed, and ORT is continued | Rehydration phase: administration of 20 ml/kg body weight isotonic saline. When the patient is stable, ORS to be administered 25–100 ml/kg ORS every 4 h. | ||
| Maintenance phase: nutrition and fluids along with ORS | |||
| Pulse | Fill, normal number | Fast | Fast and weak or absent |
| Systolic pressure | Normal | Normal or low | Down |
| Breathing | Normal | Deep, the respiratory rate may increase | Deep, rapid, or decreased breathing or lack of breathing |
| Oral mucosa | Sticky or slightly dry | Dry | Fragile |
| Anterior Fontanel | Normal | Submerged | Significantly sunk |
| Eyes | Normal | Goodbye | Significantly reduced |
| Skin turgor | Normal | Decreased | Clad |
| Skin | Normal | Cold | Cold, lattice, edges black |
| The amount of urine | Normal or mildly reduced | Dropped significantly | No urine |
| Systemic symptoms | Increased thirst | Inattention, irritability | Breathable, loose breaths, coma |
Abbreviations: ORS, oral rehydration solution; ORT, oral rehydration therapy.
3. PRACTICES TO TREAT DEHYDRATION AT DIFFERENT STAGES OF WATER LOSS
3.1. Lack of water
For patients with diarrhea but without evidence of water deficiency, ORT is used to maintain hydration by replacing stools, as mentioned above. If stool output is minimal, ORS may not be required. Regardless of the stool removal, age‐appropriate nutrition (including breastfeeding) should be continued with supplemental fluids.
3.2. Mild to moderate water loss
Several specialists use the same management approach for patients with mild to moderate dehydration (3%–9% volume reduction). While some patients with relatively less intense water loss can be provided with home‐based care. When required, oral fluid replacement techniques are taught. However, care for patients with higher degree of dehydration is better monitored in a medical setting.
3.2.1. Rehydration phase
Liquid therapy should be administered with ORS of 50 to 100 ml/kg every 4 h. Extra ORS is given to replace ongoing loss of digestive system (stool or vomiting). The patient should be rechecked for hydration and regular replacement.
3.2.2. Maintenance phase
After the completion of replacement phase, nutrition and fluids should be started, and the ORT is continued for continuous gastrointestinal excretion. The patient's hydration status, diarrhea, and vomiting should be assessed, as well as the amount of fluid excreted per hour added to the amount required the next hour.
3.3. Severe dehydration
Severe dehydration is defined as a volume loss of more than 10% which is treated as follows.
3.3.1. Rehydration phase
Very severe dehydration is a medical emergency and requires IV treatment with a rapid administration of 20 ml/kg body weight with isotonic saline.
As the patient's clinical status stabilizes and his or her level of consciousness returns to normal, treatment can be switched to ORS. The nasal tube can be used in patients with a normal mental state, who may not be able to consume enough fluid. ORS is given with a volume of 100 ml/kg body weight at 4 h or 25ml/kg. Additional ORS is prescribed to replace continuous gastrointestinal excretion. At the end of each hour, the patient's hydration status and diarrhea and vomiting should be assessed, and the amount of excretion per hour should be added to the amount required the next hour.
3.4. Maintenance phase
After repletion is completed, nutrition and fluids should be started, and ORT is continued to replace gastrointestinal excretion.
4. LIMITATIONS IN THE USE ORT
Knowledge concerning the importance and usage of ORT and associated practice are missing factors that might have contributed to the limited use of ORT. 26 , 27
A recent study by Misgna et al. 1 concerning the awareness regarding the use of ORT in Ethiopia reported that 51% of the total children suffering from diarrhea, were receiving ORT whereas, 43.8% of the mothers were fully aware of the purpose of ORT. A number of previous studies have shown that unawareness regarding the use of ORT, lack of knowledge of diarrhea and fluid loss and associated sign and symptoms, and unavailability of ORT products delay the treatment and worsen the clinical condition. 28 A study conducted in Gambia by Sillah et al. 29 reported that maternal knowledge‐attitude‐practice score for the use of ORS among children suffering from diarrhea, under the age of 5 was 33.9. The use of ORT in practice was seen to be 4%. Additionally, higher socioeconomic status and increased age are associated with the greater use of ORT. Similarly, Agbolade et al. 30 study based on Nigerian military camp reported that the awareness of the use of ORS or sugar‐salt solution was greater than its use, 98% versus 49.5%.
Previous experience of using ORT, seeking medical advice, and knowledge of ORT are common factors associated with the increased use of ORT. 31 A study conducted in Kenya concerning the use of ORT in diarrhea among children stated that caregivers who did not use ORS for rehydration were not much aware of these, had no access to the facility, children disliked the taste, lack of confidence to treat diarrhea at home and had greater inclination towards the use of western medicine. 32
5. COMMERCIAL AND STANDARD ORS
For ORT, the WHO standard or marketable ORS that has a concentration of equimolar 1 glucose and sodium with osmolality should be used. ORS available in the market differs in osmolality and sodium concentration (Table 1). All commercial ORS contain 2%–3% carbohydrates, such as glucose, rice, or other grains; this is sufficient to maintain nutritional status in the short term (24–48 h) until osmol overload in the gut is avoided. 33
6. OTHER REMEDIES FOR DEHYDRATION
6.1. Household drinks and liquids
Common household fluids for children with hypovolemia include gelatin, tea, fruit juice, sports drinks, and nonalcoholic beverages. These liquids are low in sodium and almost all of them have a higher carbohydrate content and osmolality than standard ORS (Table 1). As a result, they are not recommended as a standard ORS alternative for resuscitation in children with gastroenteritis, because there are concerns that may cause hyponatremia‐induced osmotic diarrhea. However, a Canadian clinical trial in 6‐ to 60‐month‐old children with mild gastroenteritis without clinical signs of dehydration showed that apple juice (diluted 1: 1 with apple juice and water) compared to standard commercial ORS flavored apples are less susceptible to treatment failure (17%–25%). 34 Zinc supplementation should be prescribed for children with diarrhea in developing countries, due to the prevalence of zinc deficiency. 35 , 36 , 37 Additionally, usage of zinc‐based formula is also effective in reducing diarrhea. 38
6.2. IV rehydration
Alternatively, IV fluid therapy, composed of 0.9% sodium chloride (NaCl) is also used extensively for the compensation of fluid loss following gastroenteritis and diarrhea, particularly. 39 A number of studies have compared the effects of ORT and IV rehydration therapy for the following purpose. In 2002, Atherly‐John et al. 40 compared the effects of these two among the acute gastroenteritis children and reported that the use of ORT was associated with shorter hospital stay and increased patient satisfaction. However, out of 18 patients receiving ORT, four failed to respond well and were moved to IV therapy.
Similarly, in a systemic review Freedman et al. 41 demonstrated that use of ORT was characterized by shorter stay at the hospital nonetheless, had greater risk of developing paralytic ileus, as compared to IV therapy. Phlebitis was more prevalent in IV group. Simplicity and noninvasiveness of ORT make it the first choice for the treatment mild to moderate diarrhea.
Advancement in the management of gastroenteritis has purposed the use of rapid ORT, that is, administered for 4 h. 42 , 43 In cases where rapid ORT fails, IV or rapid IV therapy containing 0.9% NaCl 20 ml/kg/h for 2–4 h is considered. 44 To it, ORT is also continued. The WHO recommends the use IV rehydration therapy for 3–6 h in the cases of severe dehydration. 45 Nonetheless, ORT is a cost‐effective method for non‐severe diarrhea emergencies. 46 A recent study conducted on calves stated that ORT is a gold standard for treating moderate dehydration, supported from the outcomes based on blood pH, changes in plasma volume, levels of electrolytes, and physical examination. The study concluded that ORT is likely to more effective than small volume of lactated Ringer's solution (IV) or subcutaneous therapy. 47
7. CONTRAINDICATION AND ADVERSE EFFECTS OF ORT
In patients with volume loss greater than 10%, those who are unable to drink liquid (respiratory problems or unconsciousness), patients under shock, unable to maintain ORS in body due to vomiting, and those with ileus, ORS is contraindicated. 48 A recent study stated that it might not be suitable among children with mixed/cardioinhibitory vasovagal syncope. 49
Among children in whom fluid loss is undervalued, ORT can lead to acute kidney injury, acidosis, and death. 4 A recent study also reported 11 cases of facial edema following rehydration therapy in 23 patients. They reported that it was associated with a greater volume of rehydration solution and faster infusion speed. Furthermore, cardiovascular adverse events, epilepticus, pulmonary edema, and convulsions are also reported in these patients. 50
Despite the knowledge and known positive outcomes of ORT, its usage remains to be 30%–40% to the date. Inadequate supplies, lack of healthcare knowledge, and faulty government policies have added to the cause of stagnancy in these numbers. 51
8. CONCLUSION
A number of modifications have been made to the therapy, nonetheless, it is still first choice for the treatment of volume depletion, following diarrhea. In cases where ORT fails, IV rehydration is recommended. These are cost‐effective and easily available options that can save several lives, which are foregone due to incorrect understanding regarding the treatment of diarrhea. Clear and simple set of guidelines is required to fill the void between the knowledge and the practice of using ORT.
AUTHOR CONTRIBUTIONS
Ziba Aghsaeifard: Conceptualization; Writing – original draft. Ghobad Heidari: Formal Analysis. Reza Alizadeh: Writing – review and editing. All authors have read and approved the final version of the manuscript. Ziba Aghsaeifard had full access to all of the data in this study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Written consent was signed for all the patients aged 18 years or above. For patients under 18, a legal guardian or parent signed the consent form.
TRANSPARENCY STATEMENT
Ziba Aghsaeifard affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Aghsaeifard Z, Heidari G, Alizadeh R. Understanding the use of oral rehydration therapy: a narrative review from clinical practice to main recommendations. Health Sci Rep 2022;5:e827. 10.1002/hsr2.827
DATA AVAILABILITY STATEMENT
The authors confirm that the data supporting the findings of this study are available within the article.
REFERENCES
- 1. Misgna HG, Ebessa B, Kassa M. Prevalence of oral rehydration therapy use and associated factors among under‐five children with diarrhea in Dangure, Benishangul Gumuz Region, Ethiopia/2018. BMC Res Notes. 2019;12(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maleki‐Sadeghi N, Rahmani P, Aghsaeifard Z, Heidari G. Effects of aminophylline on the levels of neutrophil gelatinase‐associated lipocalin (NGAL) in asphyxiated term neonates. Arch Physiol Biochem. 2020;128(4):1105‐1110. [DOI] [PubMed] [Google Scholar]
- 3. Rahmani P, Farahmand F, Heidari G, Sayarifard A. Noninvasive markers for esophageal varices in children with cirrhosis. Clin Exp Pediatr. 2021;64(1):31‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anigilaje EA. Management of diarrhoeal dehydration in childhood: a review for clinicians in developing countries. Front Pediatr. 2018;6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bhave G, Neilson EG. Volume depletion versus dehydration: how understanding the difference can guide therapy. Am J Kidney Dis. 2011;58(2):302‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sack RB. History of the development of oral rehydration fluids. J Indian Med Assoc. 2003;101(6):360‐364. [PubMed] [Google Scholar]
- 7. Schenkman N, Spencer E. Is oral rehydration in pediatric patients with gastroenteritis more effective than parenteral rehydration? Evid Based Pract. 2019;22(8):1‐2. [Google Scholar]
- 8. Binder HJ, Brown I, Ramakrishna BS, Young GP. Oral rehydration therapy in the second decade of the twenty‐first century. Curr Gastroenterol Rep. 2014;16(3):376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aghsaeifard Z, Zendehdel A, Alizadeh R, Salehnasab A. Chronic hemodialysis: evaluation of dialysis adequacy and mortality. Ann Med Surg. 2022;76:103541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Santosham M, Chandran A, Fitzwater S, Fischer‐Walker C, Baqui AH, Black R. Progress and barriers for the control of diarrhoeal disease. The Lancet. 2010;376(9734):63‐67. [DOI] [PubMed] [Google Scholar]
- 11. Aghsaeifard Z, Firouzi R, Alizadeh R. Predisposing factors and uremic pericardial effusion among ESRD patients undergoing dialysis. Ann Med Surg. 2022;77:103579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Olson CK, Blum LS, Patel KN, et al. Community case management of childhood diarrhea in a setting with declining use of oral rehydration therapy: findings from cross‐sectional studies among primary household caregivers, Kenya, 2007. Am J Trop Med Hyg. 2011;85(6):1134‐1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. WHO U. Diarrhoea: why children are still dying and what can be done. UNICEF/WHO; 2009. [Google Scholar]
- 14. Milner SM, Greenough WB 3rd, Asuku ME, et al. From cholera to burns: a role for oral rehydration therapy. J Health Popul Nutr. 2011;29(6):648‐651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ahmadipour S, Mohsenzadeh A, Alimadadi H, Salehnia M, Fallahi A. Treating viral diarrhea in children by probiotic and zinc supplements. Pediatr Gastroenterol Hepatol Nutr. 2019;22(2):162‐170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alam NH, Raqib R, Ashraf H, et al. L‐isoleucine‐supplemented oral rehydration solution in the treatment of acute diarrhoea in children: a randomized controlled trial. J Health Popul Nutr. 2011;29(3):183‐190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grigsby A, Herron J, Hunter BR. Does the addition of dextrose to iv crystalloid therapy provide clinical benefit in acute dehydration? A systematic review and meta‐analysis. Can J Emerg Med. 2019;21(5):638‐645. [DOI] [PubMed] [Google Scholar]
- 18. Ofei SY, Fuchs GJ. Principles and practice of oral rehydration. Curr Gastroenterol Rep. 2019;21(12):67. [DOI] [PubMed] [Google Scholar]
- 19. Gregorio GV, Gonzales MLM, Dans LF, Martinez EG. Polymer‐based oral rehydration solution for treating acute watery diarrhoea. Cochrane Database Syst Rev. 2016;12(12):CD006519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koletzko S, Osterrieder S. Acute infectious diarrhea in children. Dtsch Arztebl Int. 2009;106(33):539‐548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Barr W, Smith A. Acute diarrhea in adults. Am Fam Physician. 2014;89(3):180‐189. [PubMed] [Google Scholar]
- 22. Alam NH, Yunus M, Faruque ASG, et al. Symptomatic hyponatremia during treatment of dehydrating diarrheal disease with reduced osmolarity oral rehydration solution. JAMA. 2006;296(5):567‐573. [DOI] [PubMed] [Google Scholar]
- 23. Mosites E, Hackleman R, Weum KL, Pintye J, Manhart LE, Hawes SE. Bangladesh ORS case study. University of Washington; 2012. [Google Scholar]
- 24. Pantenburg B, Ochoa TJ, Ecker L, Ruiz J. Use of commercially available oral rehydration solutions in Lima, Peru. Am J Trop Med Hyg. 2012;86(6):922‐924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Freedman SB, Vandermeer B, Milne A, Hartling L, Pediatric Emergency Research Canada Gastroenteritis Study Group . Diagnosing clinically significant dehydration in children with acute gastroenteritis using noninvasive methods: a meta‐analysis. J Pediatr. 2015;166(4):908‐916. [DOI] [PubMed] [Google Scholar]
- 26. Abadi MFKA, Hujail SAAR. Assessment of mothers' knowledge, attitude, and practice about oral rehydration solution in treatment of diarrhea in Karbala. Karbala J Med. 2019;12(2):2203‐2211. [Google Scholar]
- 27. Haricharan KR, Punith S, Harsha P, Gowtham R. Knowledge, attitude and practices of oral rehydration therapy among mothers coming to tertiary care centre. Int J Contemp Pediatr. 2019;6(1):127. [Google Scholar]
- 28. Hall‐Clifford R, Amerson R. From guidelines to local realities: evaluation of oral rehydration therapy and zinc supplementation in Guatemala. Rev Panam Salud Publica. 2017;41:e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sillah F, Ho H‐J, Chao JC. The use of oral rehydration salt in managing children under 5 y old with diarrhea in the Gambia: knowledge, attitude, and practice. Nutrition. 2013;29(11‐12):1368‐1373. [DOI] [PubMed] [Google Scholar]
- 30. Agbolade MO, Dipeolu I, Ajuwon A. Knowledge and use of oral rehydration therapy among mothers of under‐five children in a military barrack in Ibadan, Nigeria. Afr J Biomed Res. 2015;18:7‐15. [Google Scholar]
- 31. Mengistie B, Berhane Y, Worku A. Predictors of oral rehydration therapy use among under‐five children with diarrhea in eastern Ethiopia: a community based case control study. BMC Public Health. 2012;12:1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Blum LS, Oria PA, Olson CK, Breiman RF, Ram PK. Examining the use of oral rehydration salts and other oral rehydration therapy for childhood diarrhea in Kenya. Am J Trop Med Hyg. 2011;85(6):1126‐1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Freedman S, Ali S, Michas M, Gouin S, Hartling L. Treatment of acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries. Evid Based Child Health. 2013;8:1123‐1137. [DOI] [PubMed] [Google Scholar]
- 34. Freedman S, Willan A, Boutis K, Schuh S. Effect of dilute apple juice and preferred fluids vs electrolyte maintenance solution on treatment failure among children with mild gastroenteritis: a randomized clinical trial. JAMA. 2016;315:1966‐1974. [DOI] [PubMed] [Google Scholar]
- 35. Suh J‐S, Hahn W‐H, Cho B‐S. Recent advances of oral rehydration therapy (ORT). Electrolyte Blood Press. 2010;8(2):82‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tran CD, Hawkes J, Graham RD, et al. Zinc‐fortified oral rehydration solution improved intestinal permeability and small intestinal mucosal recovery. Clin Pediatr (Phila). 2015;54(7):676‐682. [DOI] [PubMed] [Google Scholar]
- 37. Trehan I, Grabowsky M, Schenker I . Oral rehydration therapy and zinc: looking back and looking ahead. J Trop Pediatr. 2019;65(5):417‐420. [DOI] [PubMed] [Google Scholar]
- 38. Porrostami K, Arjmand R, Asayesh H, Noroozi M, Safari O, Qorbani M. Effectiveness of gastrofix on duration of diarrhea and length of hospitalization in children with acute gastroenteritis: a randomized controlled trial. Int J Pediatr. 2018;6(6):7723‐7731. [Google Scholar]
- 39. Moritz ML, Ayus JC. Improving intravenous fluid therapy in children with gastroenteritis. Pediatr Nephrol. 2010;25(8):1383‐1384. [DOI] [PubMed] [Google Scholar]
- 40. Atherly‐John YC, Cunningham SJ, Crain EF. A randomized trial of oral vs intravenous rehydration in a pediatric emergency department. Arch Pediatr Adolesc Med. 2002;156(12):1240‐1243. [DOI] [PubMed] [Google Scholar]
- 41. Freedman SB, Ali S, Oleszczuk M, Gouin S, Hartling L. Treatment of acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries. Evid Based Child Health. 2013;8(4):1123‐1137. [DOI] [PubMed] [Google Scholar]
- 42. National Collaborating Centre for Women's and Children's Health (UK). Diarrhoea and vomiting caused by gastroenteritis: diagnosis, assessment and management in children younger than 5 years. NICE Clinical Guidelines, No. 84. RCOG Press; 2009. [PubMed]
- 43. Alam NH, Ashraf H, Ahmed T, Jahan N, Gyr N. Randomised trial showed that rapid rehydration of severely malnourished children with dehydrating diarrhoea was as safe and effective as slow rehydration. Acta Paediatr (Stockholm). 2019;109:1473‐1484. [DOI] [PubMed] [Google Scholar]
- 44. Azarfar A, Ravanshad Y, Keykhosravi A, Bagheri S, Gharashi Z, Esmaeeli M. Rapid intravenous rehydration to correct dehydration and resolve vomiting in children with acute gastroenteritis. Turk J Emerg Med. 2016;14(3):111‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Toaimah FHS, Mohammad HMF. Rapid intravenous rehydration therapy in children with acute gastroenteritis: a systematic review. Pediatr Emerg Care. 2016;32(2):131‐135. [DOI] [PubMed] [Google Scholar]
- 46. Mosegui GG, Vianna CM, Rodrigues MS, Valle PM, Silva FV. Cost‐effectiveness analysis of oral rehydration therapy compared to intravenous rehydration for acute gastroenteritis without severe dehydration treatment. J Infect Public Health. 2019;12(6):816‐821. [DOI] [PubMed] [Google Scholar]
- 47. Doré V, Foster DM, Ru H, Smith GW. Comparison of oral, intravenous, and subcutaneous fluid therapy for resuscitation of calves with diarrhea. J Dairy Sci. 2019;102(12):11337‐11348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ulrickson M. Oral rehydration therapy in children with acute gastroenteritis. J Am Acad PAs. 2005;18(1):24‐29. [DOI] [PubMed] [Google Scholar]
- 49. Li W, Wang S, Liu X, Zou R, Tan C, Wang C. Assessment of efficacy of oral rehydration salts in children with neurally mediated syncope of different hemodynamic patterns. J Child Neurol. 2019;34(1):5‐10. [DOI] [PubMed] [Google Scholar]
- 50. Houston KA, Gibb J, Olupot‐Olupot P, et al. Gastroenteritis aggressive versus slow treatment for rehydration (gastro): a phase ii rehydration trial for severe dehydration: who plan c versus slow rehydration. BMC Med. 2019;17(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Khan AM, Wright JE, Bhutta ZA. A half century of oral rehydration therapy in childhood gastroenteritis: toward increasing uptake and improving coverage. Dig Dis Sci. 2020;65(2):355‐360. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article.


