Abstract
Introduction
Nonsurgical aesthetic treatments of the lower face are increasing in demand. In particular, they aim to restore facial youth following the changes due to progressive resorption of facial skeleton and atrophy of facial fat compartments which give the perception of a descent face.
Objectives
The aim of this research is to describe the nonsurgical reshaping of the aged lower jaw by means of hyaluronic acid fillers.
Methods
A retrospective analysis of data from adult female patients undergoing treatment with hyaluronic acid injections in the lower third of the face was performed. Injection techniques, relevant anatomy of the anatomical area and rheological properties of the fillers to be used are highlighted.
Results
Thirty-six consecutive patients were enrolled (100% female; mean age: 45.7 years). A minimum of 4 up to 7 vials of hyaluronic acid filler was injected to achieve the desired results. The visual analogue scale was used to assess patient satisfaction. Thirty-two patients (88.8%) rated their appearance post-treatment with a satisfaction score ranging between 85% and 100%. A total absence of ecchymosis and/or swelling in the early postoperative days has been highlighted. There were no cases of infection, paresthesia, hematoma or necrosis.
Conclusions
For those patients not willing to undergo surgery, the jawline remodelling with hyaluronic acid fillers seems to be a viable option for ameliorating the definition of the lower third of the face. Nonetheless, it is mandatory to perform multilayer injections using fillers with different rheological properties.
Keywords: filler injection, lower jaw, nonsurgical, multilayer injection, hyaluronic acid
Introduction
Facial aging is a complex multifactorial phenomenon that embraces both hard and soft tissues. Over the years, there is a progressive resorption of the facial skeleton characterized by the posterior displacement of the maxilla, and the lateral-inferior shifting of the lateral and inferior orbital rim creating a larger orbital aperture. In the aging process, there is a sort of contraction of the lower jaw in a vertical and a horizontal plane induced by the resorption of the gonial angle, chin symphysis, body and ramus of the jaw. Moreover, we should also consider a possible tooth loss that causes the resorption of the alveolar process contributing thus to an aged appearance [1]. The loss of hard tissue support is accompanied by the overlying soft tissue slipping. Although there are no fat compartments along the lower jaw, but only subcutaneous fat tissue, the deflation of midfacial fat compartments induces soft tissue falling that, associated with the loss of bony projection, contributes to the loss of definition of the jawline [2,3].
Progressive atrophy of facial fat compartments is recorded. Moreover, the attenuation of the zygomatic-cutaneous, orbito-malar, and mandibular retaining ligaments gives the appearance of facial soft tissues descent. As some anatomical studies have confirmed, it acts as a hammock between the atrophied fat compartments and the soft tissues of the face, contributing to the morphological appearance of the tear through deformity, malar bags, and jowling [4].
A deep plane facelift is the surgical gold standard to restore a youthful and natural appearance of the face. Over the last years, an increasing interest in deep plane face lifting techniques has been rising, highlighting the role of facial retaining ligament release and facial fat compartments repositioning [5,6].
However, during the last 20 years, nonsurgical anti-aging facial procedures have gained more and more popularity. Patients have been aiming for natural results with no need for surgical interventions; for this reason, the use of hyaluronic acid (HA) fillers has shown to be a mainstay among nonsurgical facial aesthetic procedures [7].
Since their first introduction at the end of the 20th century, the role of HA fillers has dramatically changed, shifting from purely dermatologic treatments, such as fine lines filling, to a total facial reshaping tool [8,9]. Nowadays, facial fillers are used for a wide range of procedures such as nonsurgical nose job, temple volumization, eyebrow repositioning, etc. Moreover, HA fillers are even used to restore post-surgical facial deformities, showing a good profile of safety with long term stability [10–13]. The aforementioned issues paved the way for the treatment of certain areas, such as the jawline, that were previously considered nonsuitable for HA filler injections [14].
Objectives
This research aims to describe nonsurgical reshaping of the aged lower jaw by means of hyaluronic acid fillers, highlighting the specifics of fillers and the technique with respect to facial anatomy.
Methods
This retrospective case series includes 36 consecutive patients, seeking nonsurgical lower jaw sculpting, treated by the senior author (RR) from January, 2014 to January, 2020. The study was conformed to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement for cohort studies. Every patient signed an informed consent for the procedure and scientific purposes. Only HA-based fillers were used, different brands with different cross-linking agents (1,4-butanediol diglycidyl ether [BDDE] or polyethene glycol [PEG]) were employed (Nyuma Pharma; Neauvia; Teoxane; Stylage, Laboratoires Vivacy). For each brand, different fillers with different rheological properties were chosen according to the anatomical layer to be injected.
Every procedure was performed at least 21 days after the first consultation in an office setting and was not followed by or combined with any other aesthetic treatment. No antibiotic, corticosteroid, painkillers, or other drugs were prescribed to the patients at the end of the procedure. After the injections, an HA-based topical gel was applied on the skin in the treated area, and a HA patch was placed over for 20 minutes to reduce post-injection redness and swelling. Due to the complexity of the injections, it is always recommended to have the patients stay in the waiting room for at least 20–30 minutes after the procedure in order to exclude vascular impairments or any other early adverse event. The patients were evaluated 21 days after the procedure. At this time, the visual analogue scale (VAS) was used to assess patient satisfaction from 100 (the best aesthetic outcome possible) to 0 (the worst). In 3 cases a touch-up was performed after VAS evaluation, under the physician’s suggestion to address minor asymmetries. Less than 1 mL was required per touch-up.
Filler Rheology
To inject over the periosteum, a filler with a G’ over 400 Pa was chosen. While, to inject subcutaneously, a filler with lower G’ between 200 and 300 Pa was chosen. As a general rule, the deeper the injections are (over/under the periosteum) the higher the G’ (storage/elastic modulus) and the G* (hardness) should be:. This is the ratio between G’ (storage/elastic modulus) and G” (loss/viscous modulus). On the other hand, the more superficial the injection has to be (dermal layer), the higher the G” and the tan delta (G” and G’ ratio) should be [15].
Pre-operative Plan and Injection Technique
After face cleansing with 80% isopropyl alcohol, the symphysis midline was identified on the lower edge of the mandible where the first deep bolus was released with a high G’ filler: about 1.5 cm apart in each side. One more point was marked where the second bolus was released. If 3 points were not enough and jowling was still observed, 1 more point would be marked and injected at about 1.5 cm apart per side, paying careful attention not to go laterally to the mandibular septum. In order to achieve a straight jaw-line, the amount to inject over the periosteum should be higher in the midline compared to the laterally marked points in an ideal pyramid shape (eg if 0.2 mL are injected into the midline, 0.1 mL about 1.5 cm apart on each side has to be injected). Deep perpendicular injections were carried out with a 25 G, 4 cm long needle.
Once deep injections were performed, an over-protruded chin could be identified. In such a case, the labio-mental crease was marked, then 1 triangle per side with the apex pointing towards the labio-mental crease was marked and injected subcutaneously. Using a filler with a lower G’ compared to the deep injections already performed, the injections were carried out with a cannula, filling the labio-mental crease and the 2 triangles previously marked to erase the overprotruded aspect of the chin by pushing forward the soft tissues of the surrounding area. During these injections, the cannula usually encounters some resistance due to the fatty fibrotic tissue represented under the skin of this anatomical area. A 4-cm cannula was used for these 27G injections.
On the gonial angle, a perpendicular injection was performed over the periosteum with the same high G’ filler previously used for the chin. The injection was performed in the most lateral part of the gonial angle to straighten the mandible posteriorly. Then, a lower G’ filler was used to restore the mandible body and ramus. The low G’ filler was the same as the one previously injected into the subcutaneous tissue. To fill the subcutaneous tissue over the body of the jaw, the cannula entry point was performed with a needle, 1 cm ahead of the anterior margin of the masseter, over the lower border of the mandible. Once the cannula is inserted, one or more passages were performed to fill the area with retrograde releasing.
Over the parotid, the ramus area was filled with the same low G’ filler. The entry point was performed ahead of the tragus. The cannula should not be inserted in the superficial subcutaneous layer. The HA was retrogradely released, with one or more passages, over the parotid fascia. In this area, some resistance can be felt in the cannula movements due to the presence of the parotid fascia (Figure 1). Excessively superficial injections in this area usually make the filler visible, leading to unpleasant results. The area between the masseteric cutaneous ligament and the mandibular septum was never injected in order to prevent a worsening of the jowling (Table 1).
Figure 1.
The black dot indicates the area to be filled with deep injections over the periosteum, with a high G’ filler. The blue lines indicate the area to be filled subcutaneously with an hyaluronic acid filler with a G’ ranging between 200 and 300 Pa.
Table 1.
Features of injection sites, hyaluronic acid dose, type of injection, the anatomical layer to be injected, and the needle/cannula use
| Injection Site | Hyaluronic Acid Injection (Range) | Type of Injection | Anatomical Layer | Needle/Cannula |
|---|---|---|---|---|
| Symphysis | 0.2–0.3 mL | Bolus release | Over the periosteum | Needle |
| Para-symphysis | 0.1–0.2 mL | Bolus release | Over the periosteum | Needle |
| Supplementary injections lateral to the para-symphisis (before mandibular septum) | 0.1 mL | Bolus release | Over the periosteum | Needle |
| Gonial angle | 0.3–0.5 mL | Bolus release | Over the periosteum | Needle |
| Mandibular ramus | 0.5–1 mL | Retrograde release | Subcutaneous tissue (between the SMAS and the parotid fascia) | Cannula |
| Mandibular body | 0.5–1 mL | Retrograde release | Subcutaneous tissue (under the platysma) | Cannula |
| Cutaneous part of the lower lip | 1–1.5 mL | Retrograde release | Subcutaneous tissue (fatty fibrotic perioral tissue) | Cannula |
SMAS = superficial musculoaponeurotic system.
Results
Thirty-six consecutive patients seeking nonsurgical reshaping of the jaw-line were examined and treated. Every patient was female, age ranging from 42 to 71 years (mean 45.7 years). Minimum follow-up was 3 months, maximum 2 years. A minimum of 4 and up to 7 vials of HA filler was injected to achieve the desired results. Early or tardive adverse events were not reported. A moderate reduction of lower teeth display was recorded in all the patients. However, this issue was clearly explained to the patients before the injections (Figure 2). Patient satisfaction assessment results reported no scores lower than 75. Twelve patients gave a score of 100, 8 patients rated 90, 12 patients indicated a score of 85, 4 patients rated 80, and 2 indicated 75 (Table 2). Whenever the procedure was carried out with fillers not containing a local anesthetic, patients reported more pain and discomfort than patients who received fillers premixed with a local anesthetic.
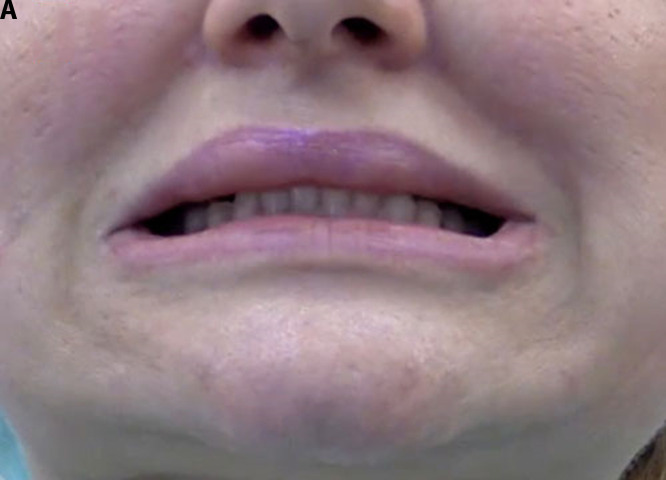
Figure 2.

(A) Pre-injection teeth display in a 46-year-old patient. (B) Reduction of teeth display due to the myomodulation induced by filler injections in the areas of the depressor angulis oris and in the depressor of the lower lip muscles.
Table 2.
Patient satisfaction with hyaluronic acid filler procedure*.
| VAS Score | 100 | 90 | 85 | 80 | 75 |
|---|---|---|---|---|---|
| Number of patients | 12 | 8 | 12 | 4 | 2 |
Patients were asked to rate their satisfaction from 0 to 100, with 0 representing the worst possible aesthetic outcome, and 100 representing the best possible aesthetic outcome.
Conclusions
A well-defined jawline is an important aesthetic and anatomical landmark to have a clear demarcation between the face and the neck [14]. To achieve natural and pleasant results, it is mandatory for the injector to have a deep knowledge of the facial anatomy and the HA fillers rheology. Using different HA fillers for each facial anatomical layer is required to avoid unnatural results, especially the “detection” of the filler during facial dynamics [9].
Several case series of lower jaw nonsurgical reshaping with the use of fillers are published in medical literature, even though most of them are not focused on the treatment of the aging mandible [14,16–18]. In a recent paper, Bertossi et al described their experience in the nonsurgical definition of the chin and jawline in younger adults, using a grid system approach.
In 2020, also Mastroluca et al focused on the lower third definition in male patients to achieve a more masculine identity; even in this paper, the focus was not on the reversal of the facial aging process of the lower third [18]. Most published articles about nonsurgical chin and jawline definition are focused on the use of a single filler, usually with a high G’ [17,19]. Nonetheless, it is a demanding treatment that should be approached only by experienced injectors with suitable training. If compared to other face areas there is not so much research focused on it.
The results on our patients show neither early nor tardive adverse events. This is explained by the injection pattern that focuses on relevant anatomical landmarks. Indeed, every deep injection is performed along the anterior edge of the mandible. Consequently, the knowledge of vascular pedicles and nerves of this area is of paramount importance to avoid vascular impairments as well as sensorial and/or motor paresis. As regards the facial artery and mandibular marginal nerve, the use of a cannula is recommended when the body of the mandible has to be injected. The needle “entry point” should be performed superficially above the platysma [20]. Perpendicular injections above the lower edge of the mandible allow to easily avoid ascendant mental artery or mental nerve injuries.
In order to achieve natural results, we approached the lower third using different fillers, with different rheological properties. A similar approach was suggested by Salti, despite he focused on facial mid-third restoration [9]. The use of fillers with different rheological properties in different anatomical facial layers can be considered an anatomical concept that supports the golden rule “like with like” of facial reconstruction [21]. When a filler is implanted deeply over the bone to give projection, it needs to have enough strength to support the overlying tissue (muscles, fat, etc.), avoiding deformation in the facial dynamics. In turn, if soft tissues have to be filled in or pushed forward to avoid the filler visibility in facial animations (in smiling, speaking, etc.), it is suggested that the same deeply injected filler not be used but one with a lower G’ so as not to detect it in facial muscle contractions. The role of deep injections with high G’ over the chin could be compared to the role of chin implants: as shown in literature, alloplastic chin implantation can help strengthen and further define a retrusive chin and a weak jawline [22].
Furthermore, an interesting role of this kind of filler is the myomodulation detected at the site of depressor angulis oris and depressor of the lower lip muscles. De Maio firstly identified the role of HA fillers in modifying facial muscles contractions in the peri-oral region to achieve natural and pleasing results and solve aesthetical problems such as gummy smiles or asymmetrical smiling [23]. In the present case series, we identified a reduction of lower teeth displays in all the injected patients; this was easily understood thanks to De Maio findings [24,25]. When HA is injected with a cannula in the triangles marked between the chin and the lower lip, the filler thus reduces the capability of contractions in the depressor angulis oris and in the depressor of the lower lip muscles. This “secondary” effect mimics the mouth corner lift, usually achieved with botulinum toxin injections into the aforementioned muscles [26].
The VAS scale evaluation revealed a high mean of patient satisfaction, also related to the absence of required days off after the procedure and/or swelling in the early postoperative days (Figures 3–8).
Figure 3.
Lateral view of a 68-year-old patient before (above), and 1 month after injections (below).
Figure 4.
Three-quarter view of a 68-year-old patient before (above) and 1 month after the injections (below).
Figure 5.
Three-quarter view of a 44-year-old patient before (upper) and 2 years after the injections (below).
Figure 6.
Three-quarter view of a 44-year-old patient before (above) and 2 years after the injections (below).
Figure 7.
Three-quarter view of a 46-year-old patient before (above) and 3 months after the injections (below).
Figure 8.
Three-quarter view of a 46 year old patient before (upper part) and 3 months after the injections (lower part).
Consultation plays a key to achieve high patient satisfaction, especially with naive patients [18]. Usually, patients consider HA fillers as just an “injection” due to information found on the internet or in ads. It is mandatory during the first consultation to let them understand the type of injections performed, potential risks such as vascular impairments, and eventually secondary effects such as lower teeth display reduction that can be detected postoperatively [27].
After advanced filling procedures, it should be mandatory to have the patients waiting in the office for at least 30 minutes following the injections. This has already been described for others areas rich in vascular networks such as the nose [10]. In the present case series, after the injection, an HA-based topical gel was applied over the skin in the treated area, and an HA patch was placed over it for 20 minutes. This care is performed to calm the patient and to have time to detect early complications, such as vascular impairments that may require early hyaluroindase (HYAL) injections [28–30]. However, the application of early HYAL injections always needs to be discussed with patients prior to proceeding with the treatment because if the patient opts out of them, then it would be best not to perform the procedure.
Some papers regarding the use of a single filler or a single brand of fillers to reshape the mandible have been published [14,16–18]. However, in the present paper, we focused on the meaning of knowing the rheological properties of the filler independently from the brand. Almost all facial filler brands have different types of fillers, a correct knowledge of the rheological properties of the filler based on the anatomical layer to be injected allows the physician not to focus only on a certain brand.
Published papers on the same topic mainly address “young adults.” Indeed, Braz et al. concluded that this technique is for patients around 40–45 years old with a beginning of sagging of the lower face (small jowl and visibility the mandibular ligament fixed point and a little retrogenia) or young patients with retrogenia who do not want to undergo surgery [31]. During this case series, we also evaluated older patients (Figure 3 shows a treated 72-year-old patient) reporting a high score in patient satisfaction. Naturally, not all older patients can benefit from these tridimensional injections. When a patient complains about facial aging, the first suggested option should be a surgical facelift. However, if the patient does not want to undergo surgery but desires to ameliorate the appearance of the jawline, then multilayer HA injections represent a viable option.
The present case series is limited by the evaluation of the results done comparing pre and post-treatment photos and a VAS scale filled out by the patients. Clinical photographs are useful for scientific records and research, despite in standardization and systematization of the photographic positions for the clinical evaluations reliability and reproducibility, the variability is still a matter of fact [32]. Regarding the results of patients’ evaluation, self-perceived aesthetical improvement is one of the most debated issues in aesthetic surgery [33]. The VAS evaluation is widely used in literature and clinical practice. It was used in this work thanks to its simplicity, quickness, smartness, and adaptability. However, seeking measurement bias is crucial, principally when patient satisfaction is taken as an outcome [34].
Multilayer HA injection treatment for lower jaw aging represents a viable option for ameliorating the jaw-line definition in those patients not willing to undergo surgery. Deep knowledge of the relevant anatomy and rheological features of each filler properly used in each anatomical layer is required.
Footnotes
Authorship: All authors have contributed significantly to this publication.
Competing interests: None.
Conflicts of Interest: R.R. is a payed speaker for Neauvia International and works as a consultant for Nyuma Pharma; N.Z. works as scientific coordinator for Neauvia International and consultant for Merz Pharma. P.B. is a paid speaker for Teoxane. Other authors declare no conflict of interest.
Funding: None.
References
- 1.Kloss FR, Gassner R. Bone and aging: effects on the maxillofacial skeleton. Exp Gerontol. 2006;41(2):123–129. doi: 10.1016/j.exger.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Rohrich RJ, Avashia YJ, Savetsky IL. Prediction of Facial Aging Using the Facial Fat Compartments. Plast Reconstr Surg. 2021;147(1S-2):38S–42S. doi: 10.1097/PRS.0000000000007624. [DOI] [PubMed] [Google Scholar]
- 3.Sarigul Guduk S, Cevik Cenkeri H, Derin Cicek E, Kus S. Evaluation of aging changes of the superficial fat compartments of the midface over time: A computed tomography study. J Cosmet Dermatol. 2021;21(4):1430–1435. doi: 10.1111/jocd.14292. [DOI] [PubMed] [Google Scholar]
- 4.Farkas JP, Pessa JE, Hubbard B, Rohrich RJ. The Science and Theory behind Facial Aging. Plast Reconstr Surg Glob Open. 2013;1(1):e8–e15. doi: 10.1097/GOX.0b013e31828ed1da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacono AA. A Novel Volumizing Extended Deep-Plane Facelift: Using Composite Flap Shifts to Volumize the Midface and Jawline. Facial Plast Surg Clin North Am. 2020;28(3):331–368. doi: 10.1016/j.fsc.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Jacono AA, Bryant LM, Ahmedli NN. A Novel Extended Deep Plane Facelift Technique for Jawline Rejuvenation and Volumization. Aesthet Surg J. 2019;39(12):1265–1281. doi: 10.1093/asj/sjy292. [DOI] [PubMed] [Google Scholar]
- 7.ASAPS. [Accessed 2nd of September, 2021]. Available from:. https://www.surgery.org/sites/default/files/ASAPS-Stats2016-11-12.pdf.
- 8.Andre P. Hyaluronic acid and its use as a “rejuvenation” agent in cosmetic dermatology. Semin Cutan Med Surg. 2004;23(4):218–222. doi: 10.1016/j.sder.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 9.Salti G, Rauso R. Facial Rejuvenation with Fillers: The Dual Plane Technique. J Cutan Aesthet Surg. 2015;8(3):127–133. doi: 10.4103/0974-2077.167264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rauso R, Tartaro G, Chirico F, Zerbinati N, Albani G, Rugge L. Rhinofilling with hyaluronic acid thought as a cartilage graft. J Craniomaxillofac Surg. 2020;48(3):223–228. doi: 10.1016/j.jcms.2020.01.008. [DOI] [PubMed] [Google Scholar]
- 11.Rauso R, Federico F, Zerbinati N, De Cicco D, Nicoletti GF, Tartaro G. Hyaluronic Acid Injections to Correct Lips Deformity Following Surgical Removal of Permanent Implant. J Craniofac Surg. 2020;31(6):e604–e606. doi: 10.1097/SCS.0000000000006689. [DOI] [PubMed] [Google Scholar]
- 12.Mashiko T, Mori H, Kato H, et al. Semipermanent volumization by an absorbable filler: onlay injection technique to the bone. Plast Reconstr Surg Glob Open. 2013;1(1):e4–e14. doi: 10.1097/GOX.0b013e31828c66b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rauso R, Nicoletti GF, Sesenna E, et al. Superficial Temporal Artery Perforator Flap: Indications, Surgical Outcomes, and Donor Site Morbidity. Dent J (Basel) 2020;8(4):117. doi: 10.3390/dj8040117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bertossi D, Robiony M, Lazzarotto A, Giampaoli G, Nocini R, Nocini PF. Nonsurgical Redefinition of the Chin and Jawline of Younger Adults With a Hyaluronic Acid Filler: Results Evaluated With a Grid System Approach. Aesthet Surg J. 2021;41(9):1068–1076. doi: 10.1093/asj/sjaa179. [DOI] [PubMed] [Google Scholar]
- 15.Borrell M, Leslie DB, Tezel A. Lift capabilities of hyaluronic acid fillers. J Cosmet Laser Ther. 2011;13(1):21–27. doi: 10.3109/14764172.2011.552609. [DOI] [PubMed] [Google Scholar]
- 16.Beer K, Kaufman-Janette J, Bank D, et al. Safe and Effective Chin Augmentation With the Hyaluronic Acid Injectable Filler, VYC-20L. Dermatol Surg. 2021;47(1):80–85. doi: 10.1097/DSS.0000000000002795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogilvie P, Sattler G, Gaymans F, et al. Safe, Effective Chin and Jaw Restoration With VYC-25L Hyaluronic Acid Injectable Gel. Dermatol Surg. 2019;45(10):1294–1303. doi: 10.1097/DSS.0000000000001960. [DOI] [PubMed] [Google Scholar]
- 18.Mastroluca E, Patalano M, Bertossi D. Minimally invasive aesthetic treatment of male patients: The importance of consultation and the lower third of the face. J Cosmet Dermatol. 2021;20(7):2086–2092. doi: 10.1111/jocd.14231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moradi A, Shirazi A, David R. Nonsurgical Chin and Jawline Augmentation Using Calcium Hydroxylapatite and Hyaluronic Acid Fillers. Facial Plast Surg. 2019;35(2):140–148. doi: 10.1055/s-0039-1683854. [DOI] [PubMed] [Google Scholar]
- 20.Huettner F, Rueda S, Ozturk CN, et al. The relationship of the marginal mandibular nerve to the mandibular osseocutaneous ligament and lesser ligaments of the lower face. Aesthet Surg J. 2015;35(2):111–120. doi: 10.1093/asj/sju054. [DOI] [PubMed] [Google Scholar]
- 21.Yano T, Karakawa R, Shibata T, et al. Ideal esthetic and functional full-thickness lower eyelid “like with like” reconstruction using a combined Hughes flap and swing skin flap technique. J Plast Reconstr Aesthet Surg. 2021;74(11):3015–3021. doi: 10.1016/j.bjps.2021.03.119. [DOI] [PubMed] [Google Scholar]
- 22.Kridel RWH, Patel S. Cheek and Chin Implants to Enhance Facelift Results. Facial Plast Surg. 2017;33(3):279–284. doi: 10.1055/s-0037-1598055. [DOI] [PubMed] [Google Scholar]
- 23.de Maio M. Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aesthetic Plast Surg. 2018;42(3):798–814. doi: 10.1007/s00266-018-1116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Maio M. Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aesthetic Plast Surg. 2020;44(4):1300–1316. doi: 10.1007/s00266-02001825-9. [DOI] [PubMed] [Google Scholar]
- 25.de Maio M. Myomodulation with Injectable Fillers: An Update. Aesthetic Plast Surg. 2020;44(4):1317–1319. doi: 10.1007/s00266-020-01768-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wollina U, Goldman A. Lip enhancement and mouth corner lift with fillers and botulinum toxin A. Dermatol Ther. 2020;33(6):e14231. doi: 10.1111/dth.14231. [DOI] [PubMed] [Google Scholar]
- 27.Rauso R, Sesenna E, Fragola R, Zerbinati N, Nicoletti GF, Tartaro G. Skin Necrosis and Vision Loss or Impairment After Facial Filler Injection. J Craniofac Surg. 2020;31(8):2289–2293. doi: 10.1097/SCS.0000000000007047. [DOI] [PubMed] [Google Scholar]
- 28.Rauso R, Zerbinati N, Franco R, et al. Cross-linked hyaluronic acid filler hydrolysis with hyaluronidase: Different settings to reproduce different clinical scenarios. Dermatol Ther. 2020;33(2):e13269. doi: 10.1111/dth.13269. [DOI] [PubMed] [Google Scholar]
- 29.Rauso R, Zerbinati N, Fragola R, Nicoletti GF, Tartaro G. Transvascular Hydrolysis of Hyaluronic Acid Filler With Hyaluronidase: An Ex Vivo Study. Dermatol Surg. 2021;47(3):370–372. doi: 10.1097/DSS.0000000000002773. [DOI] [PubMed] [Google Scholar]
- 30.Rauso R, Colella G, Franco R, et al. Is hyaluronidase able to reverse embolism associated with hyaluronic acid filler? An anatomical case study. J Biol Regul Homeost Agents. 2019;33(6):1927–1930. doi: 10.23812/19-397-L. [DOI] [PubMed] [Google Scholar]
- 31.Braz A, Humphrey S, Weinkle S, et al. Lower Face: Clinical Anatomy and Regional Approaches with Injectable Fillers. Plast Reconstr Surg. 2015;136(5 Suppl):235S–257S. doi: 10.1097/PRS.0000000000001836. [DOI] [PubMed] [Google Scholar]
- 32.Henderson JL, Larrabee WF, Jr, Krieger BD. Photographic standards for facial plastic surgery. Arch Facial Plast Surg. 2005;7(5):331–333. doi: 10.1001/archfaci.7.5.331. [DOI] [PubMed] [Google Scholar]
- 33.Baser E, Kocagoz GD, Calim OF, Verim A, Yilmaz F, Ozturan O. Assessment of Patient Satisfaction With Evaluation Methods in Open Technique Septorhinoplasty. J Craniofac Surg. 2016;27(2):420–424. doi: 10.1097/SCS.0000000000002321. [DOI] [PubMed] [Google Scholar]
- 34.Svensson E. Different ranking approaches defining association and agreement measures of paired ordinal data. Stat Med. 2012;31(26):3104–3117. doi: 10.1002/sim.5382. [DOI] [PubMed] [Google Scholar]