Abstract
Xanthogranulomatous pyelonephritis is a rare and aggressive form of chronic pyelonephritis, it can occur at all age groups but is more common in women than in men, supposedly relating to the increased incidence of urinary tract infections and chronic nephrolithiasis in woman. Computed tomography (CT) findings are very helpful in making the correct diagnosis, but the definitive diagnosis is still based on histology, as there are many differential diagnoses such as renal cell carcinoma and renal tuberculosis. The complications of this type of pyelonephritis are due to the involvement of adjacent organs. The most frequent ones are Psoas abscess, perinephric abscess, and sepsis. Nephrocutaneous and renocolic fistulas are less common. We report a case of a 61-year-old male, who presented to emergency for left-sided lumbar pain for whom radiological investigations confirmed a renocolic fistula complicating xanthogranulomatous pyelonephritis. The diagnosis of XGP was proven by histopathological examination of the nephrectomy specimen slides, but there was also association with an underlying malignant squamous differentiation consistent with urothelial carcinoma, which was not evident on CT. XGP is a rare variant of chronic pyelonephritis with known imaging features. The treatment of choice is nephrectomy and histopathological examination is required for final diagnosis, as there may be associated renal malignancy.
Keywords: Xanthogranulomatous pyelonephritis, Urothelial carcinoma, Nephrectomy, Renocolic fistula
Abbreviations: CT, computerized tomography; XGP, xanthogranulomatous pyelonephritis; WCC, white count cell; RCC, renal cell carcinoma
Introduction
Xanthogranulomatous pyelonephritis (XGP) is a rare and aggressive variant of chronic pyelonephritis leading to a non-functioning kidney. XGP occurs most frequently in middle-aged to elderly patients, with a predilection for females, probably due to an increased incidence of urinary tract infections (UTIs) and consequently struvite stones. There is also an increased incidence in patients with diabetes [1].
XGP is also known as pseudotumor due to the tumor-like enlargement of the kidney and locally destructive behavior [2]. The disease is typically characterized by the destruction and replacement of renal and peri-renal tissue by granulomatous tissue containing lipid-laden macrophages [1,2]. As it can cause several complications such as sepsis, perinephric/psoas abscess, and involve adjacent structures leading in some rare cases to nephrocutaneous or renal-colonic fistulas, no conservative or medical therapy is possible. Nephrectomy remains the treatment of choice and has an excellent prognosis, especially in single-sided cases, also it enables a diagnosis of certainty by eliminating associated malignancy [3].
Case presentation
A 61-year-old man with a history of chronic nephrolithiasis for which he received medical treatment only, was admitted to the emergency department for left flank pain for the past 5 days.
On Physical examination, hemodynamic and respiratory values were normal: 122/76 mmHg of blood pressure, pulse rate of 85, and respiratory rate of 16, with a low fever of 38,1°C (oral). Abdominal palpation revealed a soft abdomen with localized tenderness on the left lumbar fossa. At the time of his admission, the initial blood count cell showed a WCC of 20 × 109/L [reference range: 4.5-11.000], a hemoglobin level of 77 g/L [reference range: 10-15.5 g/dl], and a normal platelet count of 385 × 109 /L. C-reactive protein was elevated to 254 mg/L. Urea, creatinine, and electrolytes were in normal values. Cytobacteriological urinalysis had shown a positive culture of a multi-drug resistant Enterobacter Cloacae sensitive to carbapenem.
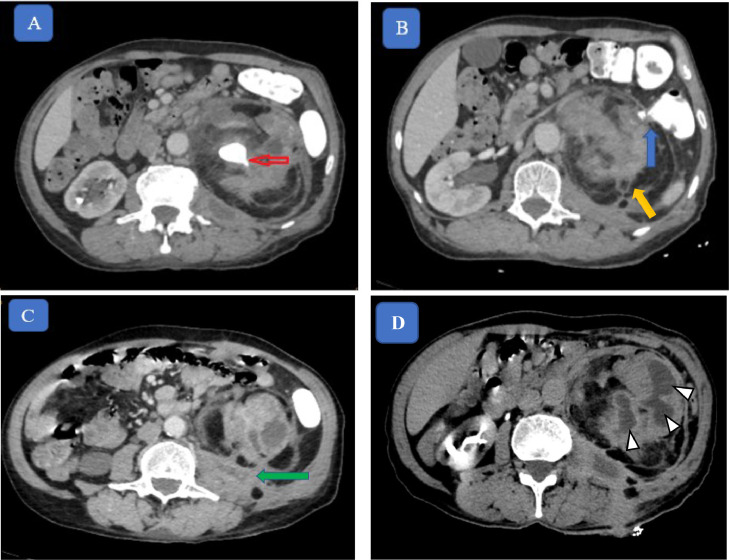
A contrast-enhanced abdominal CT scan was performed, which revealed left kidney severe hydronephrosis caused by an obstructive 28 mm coral calculus (also known as Staghorn Calculi) with thinning of the renal parenchyma and locules of air in the dilated calyces. It also revealed a 7 cm diameter perinephric loculated fluid collection that extends to the left psoas muscle. We noted as well a thin fistula between the proximal descending colon and the damaged left kidney through the kidney capsule (Gerota's fascia) (Fig. 1).
Fig. 1.
Abdominal CT scan oral and intravenous contrast material (A, B, C) showing: Staghorn calculi (red arrow) obstructing renal pelvis with associated hydronephrosis. Thin fistulae between the descending colon and left kidney (blue arrow). Infiltration and enlargement of the left psoas muscle, with abscess within it (green arrow). Extensive peri-nephric fat stranding and fibro-fat accumulation (yellow arrow). Calyceal dilatation giving a multiloculated appearance: “Bear's paw sign.”
The patient started symptomatic treatment and intravenous antibiotic therapy with ceftriaxone, and he was transferred to the urology department, where he underwent a total left-sided nephrectomy and repair of renocolic fistula, no postoperative complications were noted so far.
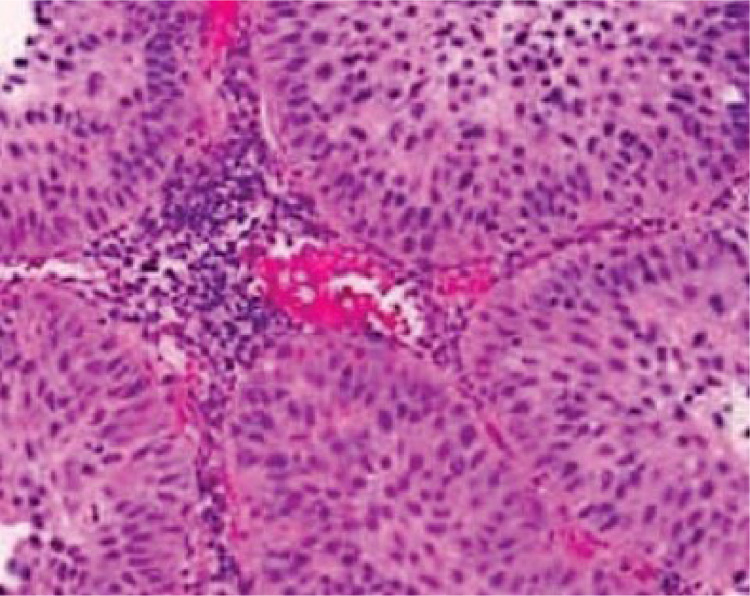
The diagnosis of XGP was proven by histopathological examination of the nephrectomy specimen slides, but there was also association with an underlying malignant squamous differentiation consistent with urothelial carcinoma, which was not evident on CT (Fig. 2).
Fig. 2.
Microscopic histological section showing tumor cells with marked nuclear atypia and indistinct cell borders, and a dense lymphocytic infiltrate.
Discussion
Xanthogranulomatous pyelonephritis (XGP) is an atypical long-term pyelonephritis with destruction of renal parenchyma and a long-term inflammatory infiltrate of macrophages.
XGP can be staged based on the extension of the disease. The First Stage of the form is localized to the renal parenchyma. The second stage involves the perinephric fat, the third Stage: involves the perinephric fat and/or abdominal wall, and the Advanced stage involves the adjacent gastrointestinal tract [4]. Our patient was staged as advanced disease as he presented a renocolic fistula. In XGP, growing inflammation results in necrosis of the thinning cortex and abscess formation. This abscess continues to grow, perforating neighboring structures, and leading to renocolic fistulas. However, Reno-cutaneous and reno-bronchial fistulas have also been described in some rare cases before [4]. Other than infectious loco-regional complications due to the aggressive features of XGP, it is reported in the published literature that it can be associated with transitional cell carcinoma of the renal pelvis and RCC [5].
Although partial nephrectomy can be performed for focal disease, most cases require total nephrectomy to resolve symptoms and exclude any malignancy risk [6].
The upper urinary tract urothelial carcinoma is uncommon, accounting for about 5%-10% of all urothelial carcinomas. The most common clinical symptom is painless hematuria and the usual radiological signs are an enhanced soft tissue lesion, collecting system filling defect, and phantom calyx [8]. They were all absent in our case.
There are only a few reports of coexisting CCT and XGP involving the kidney [8]. Obstruction, long-term inflammation, and mechanical irritation by stones have been postulated to be responsible for the pathogenesis of TCC in the presence of XGP [7].
Conclusion
To our knowledge, only a few similar cases of urothelial carcinoma associated with xanthogranulomatous pyelonephritis were reported so far. The clinical and radiological presentation of XGP may mimic urothelial carcinoma since the symptoms are not specific and the radiographic findings may be those of XGP. For this reason, radiologists and surgeons should be aware of the possibility of underlying carcinoma while diagnosing a case of XPT on clinical or radiological findings, since only histology can confirm the correct diagnosis.
Patient consent
I, the author of the article: “Unusual case of urothelial carcinoma disguised as xanthogranulomatous pyelonephritis and causing reno-colic fistula: Case report and review of literature” approve that the patient gives her consent for information be to published in Radiology Case Reports.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests.
References
- 1.Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28(1):255–276. doi: 10.1148/rg.281075171. [DOI] [PubMed] [Google Scholar]
- 2.Jha SK, Aeddula NR. Pyelonephritis Xanthogranulomatous. 2020. europepmc.org (2-5).
- 3.Parsons MA, Harris SC, Longstaff AJ, Grainger RG. Xanthogranulomatous pyelonephritis: a pathological, clinical and aetiological analysis of 87 cases. Diagn Histopathol. 1983;6(3–4):203–219. [PubMed] [Google Scholar]
- 4.Flood HD, Jones B, Grainger R. Ureterocolic fistula: a unique complication of extracorporeal shock wave lithotripsy. J Urol. 1992;147(1):122–124. doi: 10.1016/s0022-5347(17)37154-9. [DOI] [PubMed] [Google Scholar]
- 5.Dyer RB, Chen MY, Zagoria RJ. Classic signs in uroradiology. Radiographics. 2004;24(suppl 1):S247–S280. doi: 10.1148/rg.24si045509. [DOI] [PubMed] [Google Scholar]
- 6.Vikram R, Sandler CM, Ng CS. Imaging and staging of transitional cell carcinoma: part 2, upper urinary tract. Am J Roentgenol. 2009;192(6):1488–1493. doi: 10.2214/AJR.09.2577. [DOI] [PubMed] [Google Scholar]
- 7.Begum T, Huq ME, Ahmed M. Xanthogranulomatous pyelonephritis. Case Rep. 2016;2016 doi: 10.1136/bcr-2016-216025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ordones FV, Das K, Prowse S, Cohen P, Brook NR. High-grade transitional cell carcinoma masquerading as a xanthogranulomatous pyelonephritis and perinephric abscess. Radiol Case Rep. 2017;12(2):281–284. doi: 10.1016/j.radcr.2016.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]