Abstract
Childhood maltreatment is a toxic stressor that occurs in the family context and is related to adverse outcomes including elevations in internalizing symptomology and externalizing symptomology. In the present study, we tested the role of threat and deprivation dimensions of child maltreatment in the etiology of comorbid psychopathology in emerging adulthood. Additionally, we investigated emotion regulation and emotion lability/negativity as mechanisms underlying the relationship between child maltreatment dimensions and emerging adult psychopathology. To address these aims, we used a longitudinal sample of emerging adults (N = 413, Mage = 19.67, 78.0% Black, 51.1% female) who had previously participated in research assessments at age 10–12. Using a person-centered approach with latent profile analysis, we identified three classes of emerging adulthood psychopathology characterized by different levels of symptom severity and comorbidity between internalizing and externalizing symptoms. Emerging adults who experienced deprivation only, compared to those who were not maltreated, were more likely to belong to a comorbid and severe psychopathology class versus the other identified psychopathology classes. There was also a significant indirect pathway from experiences of both threat and deprivation to a high externalizing class via emotion lability/negativity. Our results contribute to current models of childhood adversity and psychopathology and have implications for interventions to prevent psychopathology among emerging adults exposed to child maltreatment.
Keywords: Child maltreatment, adverse childhood experiences, emotion regulation, comorbidity, emerging adults
Introduction
Youth who experience child maltreatment endure toxic stress that is related to multiple adverse outcomes such as depression, anxiety, substance use, and related behavior problems (Cicchetti, 2016; Oshri et al., 2013). Studies have also identified child maltreatment as a risk factor for future comorbid elevations in internalizing (e.g., depression and anxiety) and externalizing (e.g., delinquency and substance use behaviors) symptomology (Dvir et al., 2014). Heightened internalizing symptoms that are comorbid with externalizing symptoms are particularly risky in emerging adulthood, a developmental period that occurs approximately between ages 18 to 25 and is characterized by the transition from adolescence to adulthood (Arnett, 2000). Notably, comorbid elevations in internalizing symptoms and externalizing symptoms are related to adverse and potentially life-threatening outcomes in emerging adulthood characterized by both negative affect and impulsiveness, including a heightened risk for suicidal thoughts and behaviors (Duprey et al., 2020; Goldston et al., 2009). Investigations that identify the salient characteristics of child maltreatment that contribute to risk for psychopathology comorbidity, and that identify the developmental processes between child maltreatment and comorbid internalizing and externalizing symptoms, can inform prevention and intervention approaches to promote mental health for emerging adults with histories of child maltreatment.
Child Maltreatment and Comorbid Psychopathology in Emerging Adulthood
Child maltreatment is a toxic stressor characterized by the absence of stable, safe, and nurturing care. According to the developmental psychopathology framework, exposure to child maltreatment disrupts normative child development processes and can interrupt the attainment of stage-salient developmental tasks such as the formation of attachment relationships and self-regulation abilities (Cicchetti & Banny, 2014). These developmental disruptions in turn can cascade into psychopathology, including symptomology and disorders on the internalizing and externalizing symptom spectrum. Indeed, research has demonstrated that exposure to child maltreatment increases the risk for both internalizing and externalizing psychopathology during childhood, adolescence, and emerging adulthood (Hagan et al., 2014; Rogosch et al., 2010).
Much of this literature, however, involves the operationalization of internalizing and externalizing psychopathology as separate, non-overlapping phenomena. Failure to examine comorbidity is a major limitation, as recent conceptualizations on the structure of psychopathology show that internalizing and externalizing symptoms show marked overlap through childhood and adulthood (Caspi et al., 2020; Willner et al., 2016). This comorbidity has been shown in adolescent and emerging adult samples, including samples of individuals in treatment for substance abuse (Chan et al., 2008), and with exposure to maltreatment (Dugré et al., 2020). Although the literature is sparse, there is some evidence that child maltreatment increases risk for comorbidity of various psychiatric diagnoses in samples of children (Ford et al., 2000) and adults (Pavlova et al., 2016). Additionally, a recent study showed that childhood physical and sexual abuse predicted a comorbid growth trajectory of internalizing and externalizing psychopathology from childhood to adolescence (Duprey et al., 2020). However, research is needed to examine maltreatment as a developmental antecedent of comorbid psychopathology in emerging adulthood, given that approximately three-quarters of lifetime diagnoses of psychopathology onset before age 24 (Kessler et al., 2005). Specifically, it is unknown whether maltreatment is a risk factor for comorbid internalizing and externalizing psychopathology among emerging adults, and what mechanisms underpin this association. Prospective and longitudinal studies are particularly needed, as these research designs minimize reporting and recall bias in relation to child maltreatment and have greater utility (compared with cross-sectional designs) for making causal inferences.
It is important to delineate the developmental precursors to comorbid internalizing and externalizing psychopathology for several reasons. Comorbid internalizing and externalizing psychopathology may constitute a qualitatively distinct type of psychopathology that has different etiological precursors than those for internalizing and externalizing psychopathology separately. Improved understanding of this distinct comorbid psychopathology can inform clinical and preventive interventions. Further, heightened internalizing and externalizing psychopathology poses a serious risk for adverse health and behavioral outcomes, including suicidal thoughts and behaviors (Duprey et al., 2020; Goldston et al., 2009). Thus, investigating the precursors to internalizing and externalizing comorbidity can drive research on the prevention of suicide and other associated risky behaviors. Last, there is some emerging evidence that comorbidity in psychopathology exists due to the existence of a latent general factor of psychopathology, named the p factor (Caspi et al., 2014). Additional insight on the developmental precursors to comorbidity and the mechanisms between them might help inform models of the structure of psychopathology. For instance, highlighting unique mechanisms linking childhood adversity with comorbid internalizing and externalizing psychopathology would support such comorbidity as being a phenotypically distinct type of psychopathology.
Mechanisms Between Dimensions of Child Maltreatment and Comorbid Psychopathology
We used the developmental psychopathology framework coupled with the dimensional model of psychopathology (McLaughlin & Sheridan, 2016) to inform our investigation of mechanisms linking child maltreatment and comorbid psychopathology in emerging adulthood. Child maltreatment is a multi-dimensional construct that includes different timing, severity, and various types of child abuse and neglect (i.e., physical abuse, sexual abuse, neglect, and emotional maltreatment). Much of the existing research on child maltreatment and comorbid psychopathology has operationalized maltreatment in ways that fail to account for the unique environmental experiences that characterize different types of maltreatment exposure (e.g., neglect versus physical abuse), and consequently may prevent researchers from uncovering key mechanisms linking unique experiences of childhood adversity with future psychopathology.
Alternatively, in the dimensional model of psychopathology, a key assumption is that different types of child maltreatment are characterized by unique aspects of the environment (McLaughlin & Sheridan, 2016). For instance, physical and sexual abuse are characterized by the experience of threat, defined as the experience or possibility of physical harm, while neglect and certain types of emotional maltreatment are characterized by deprivation, defined as the lack of environmental inputs that are typically expected (McLaughlin & Sheridan, 2016). Both exposure to threat and deprivation have been linked with internalizing and externalizing symptomology separately. In a recent prospective study, threat was directly associated with adolescent internalizing and externalizing symptoms, while deprivation was indirectly associated with internalizing and externalizing symptoms via language abilities (Miller et al., 2021). However, it is presently unknown whether these dimensions of child maltreatment (i.e., threat and deprivation) differentially relate to comorbid internalizing and externalizing psychopathology.
The dimensional model of adversity and psychopathology asserts that experiences of deprivation lead to future psychopathology in part due to deficits in cognitive systems, while experiences of threat lead to future psychopathology in part due to deficits in emotional processing (McLaughlin et al., 2021). Additionally, both experiences of threat and deprivation are expected to lead to psychopathology via alterations to physiological stress response systems (McLaughlin et al., 2021). However, it is presently unknown how these theoretical mechanisms may underlie the association between threat and deprivation exposures with comorbid internalizing and externalizing psychopathology.
Emotion Regulation and Lability/Negativity
The present study tests and extends the dimensional model of adversity and psychopathology by examining two distinct mechanisms, emotion regulation and emotion lability/negativity, in the association between child maltreatment and emerging adult comorbid psychopathology. Emotion regulation skills, defined as “the way individuals influence which emotions they have, when they have them, and how they experience and express them” (Lavi et al., 2019, p. 1503), are complex cognitive tasks that require top-down neural processing (Öner, 2018) and can be conceptualized within the cognitive systems mechanism of the dimensional model. Theoretically then, deprivation may lead to psychopathology via deficits in these cognitive emotion regulation skills. Alternatively, lability/negativity is an aspect of emotion reactivity that is defined as an “emotionally reactive response style” to emotional stimuli (Leaberry et al., 2017) and can be conceptualized within the emotional processing mechanism of the dimensional model. Thus, the experience of threat may lead to psychopathology via deficits in lability/negativity (an aspect of emotion processing).
Emotion regulation and lability/negativity are separate but associated processes relating to how individuals process and respond to emotions and emotional stimuli. Neurodevelopmental studies show that different neurocircuitry is recruited during tasks related to emotion reactivity (e.g., the amygdala and insula) and tasks relating to emotion regulation (e.g., the dorsolateral prefrontal cortex; Martin & Ochsner, 2016). There is additional evidence that childhood experiences characterized by threat impacts lower order neurocircuitry associated with emotion reactivity (e.g., altered amygdala activation; McCrory et al., 2011) while experiences of deprivation such as institutionalization impacts higher order neurocircuitry associated with cognitive emotion regulation skills (e.g., reductions in cortical thickness; McLaughlin et al., 2014). Thus, emotion lability/negativity and emotion regulation may represent two distinct pathways from child maltreatment to future psychopathology.
Research supports the association between child maltreatment with deficits in emotion regulation skills and heightened emotion lability/negativity throughout adolescence and adulthood (Kim-Spoon et al., 2013). Several recent meta-analyses have indeed shown that child maltreatment is significantly associated with deficits in emotion regulation and increased emotion dysregulation (Gruhn & Compas, 2020; Lavi et al., 2019). It has been further suggested that emotion regulation and reactivity serve as transdiagnostic mechanisms linking experiences of childhood adversity with various forms of future psychopathology (Aldao et al., 2016). For example, in a sample of children and adolescents, emotional reactivity mediated the association between child maltreatment severity and a general factor of psychopathology assessed two-years later (Weissman et al., 2019). Similar findings on the role of emotion regulation as a mediator between childhood maltreatment and depressive symptomology have been replicated in samples of emerging adults (e.g., Coates & Messman-Moore, 2014). However, missing are studies that investigate emotion regulation and lability/negativity as distinct mechanisms in the pathway from child maltreatment dimensions to comorbid internalizing and externalizing psychopathology.
The Emotion Regulation Checklist (ERC; Shields & Cicchetti, 1997) offers promise as a tool that can be used to investigate emotion regulation and lability/negativity as unique mechanisms in the pathway between child maltreatment and emerging adult comorbid psychopathology. The ERC has been used in prior studies to investigate associations between child maltreatment with emotion regulation and dysregulation. When conceptualized dichotomously (i.e., presence/absence), maltreatment predicts both poorer emotion regulation and greater lability/negativity (Kim-Spoon et al., 2013). Previous research has also demonstrated that the type of maltreatment may differentially influence emotion regulation and lability/negativity. For instance, children who had been neglected exhibited lower scores on emotion regulation compared to non-maltreated peers, although there were no group differences on lability/negativity (Shipman et al., 2005). Another recent study showed that a latent class of child maltreatment characterized by chronicity and multi-subtypes, and another class characterized by neglect, was associated with elevated scores on the ERC’s lability/negativity subscale, although emotion regulation was not considered in this study (Warmingham et al., 2019).
The ERC (Shields & Cicchetti, 1997) has also been used by investigators to test emotion regulation and lability/negativity as simultaneous, distinct mediators in the association between adversity exposure and psychopathology. For instance, using a multiple mediation framework, children’s emotion regulation scores mediated the association between mothers’ lack of awareness and youth internalizing, while lability/negativity mediated the association between mothers’ emotion regulation difficulties and youth internalizing (Crespo et al., 2017). Thus, while there have been no investigations specifically using threat and deprivation experiences as predictors of the ERC, there is support for the notion that the ERC subscales capture different processes and are predicted by unique childhood experiences.
Additionally, the ERC has been used to investigate relations between different aspects of emotion regulation with psychopathology. Some studies have investigated emotion regulation and lability/negativity as unique mechanisms towards a common psychopathology outcome (e.g., Crespo et al., 2017; Kim-Spoon et al., 2013; Shields & Cicchetti, 1998). For instance, lower emotion regulation and higher lability/negativity scores both uniquely predicted increases in internalizing symptoms (Kim-Spoon et al., 2013). In other studies, investigators have found that the ERC subscales predict diverse outcomes. In a longitudinal sample of maltreated and demographically- matched non-maltreated children, lability/negativity was a significant predictor of aggression while emotion regulation was not a significant predictor (Shields & Cicchetti, 1998). Another more recent study found that lability/negativity, but not emotion regulation, was associated with more externalizing psychopathology in a sample of maltreatment-exposed youth (Muller et al., 2013).
The Present Study
The present study examined the prospective associations among child maltreatment dimensions, childhood emotion regulation and lability/negativity, and emerging adult comorbid psychopathology (N = 413, age range 18–23; Wave 2, collected in years 2012–2016) among individuals who had participated in a week-long research camp when they were aged 10–12 (i.e., Wave 1, collected in years 2004–2007). We used a person-centered approach to characterize profiles of comorbid psychopathology in emerging adulthood, which enabled us to examine unique profiles, or classes, of naturally occurring comorbidity within our sample. We were specifically interested in characterizing profiles of psychopathology in our sample of maltreated and demographically matched non-maltreated emerging adults as it pertains to the unique constellation of specific symptomology and diagnoses that fall on both the internalizing symptomology spectrum (e.g., depression, suicidal ideation) and externalizing spectrum (e.g., antisocial personality disorder, substance use behaviors). This person-centered approach allowed us to uncover nuances in comorbidity that would be difficult or impossible to detect with traditional (e.g., factor analytic) approaches to modeling comorbidity.
The first aim of the present study was to investigate person-centered profiles of psychopathology in emerging adulthood. We hypothesized (H1) that several profiles of psychopathology would emerge, with at least one being characterized by comorbidity of heightened internalizing psychopathology with heightened externalizing psychopathology. Consistent with prior research (e.g., Olino et al., 2012), we also expected that there would be a class of emerging adults with low levels of psychopathology, a class of emerging adults with high levels of internalizing psychopathology and low levels of externalizing psychopathology, and a class of emerging adults with high levels of externalizing psychopathology and low levels of internalizing psychopathology. Our second aim was to investigate the role of child maltreatment dimensions as predictors of emerging adult psychopathology classes. We hypothesized (H2) that maltreatment characterized by threat, and maltreatment characterized by deprivation, would predict different classes of psychopathology in emerging adulthood. Given a lack of research that has delineated associations between threat and deprivation with profiles of comorbid psychopathology, we did not have formal hypotheses for this aim. Last, we aimed to investigate lability/negativity and regulation as mediators in the association between child maltreatment dimensions and emerging adult psychopathology classes. Consistent with the dimensional model of psychopathology, we hypothesized that lower levels of emotion regulation would mediate the association between maltreatment characterized by deprivation and emerging adult psychopathology (H3a), and that higher levels of lability/negativity (i.e., higher reactivity) would mediate the association between maltreatment characterized by threat and emerging adult psychopathology (H3b). We also expected that emerging adults who experienced both threat and deprivation would exhibit both lower levels of emotion regulation and higher levels of lability/negativity (H3c). As our outcome variables were generated via a data-driven approach, we did not formulate specific hypotheses about emotion regulation and lability/negativity in relation to psychopathology classes. However, we expected that higher lability/negativity would be associated with latent classes of psychopathology characterized by externalizing symptomology, while lower levels of emotion regulation would be associated with a latent class of psychopathology characterized by higher levels of internalizing symptomology.
Methods
Participants
Participants (N = 413) were from a longitudinal follow-up study of emerging adults who participated in a research summer camp program as children. The original study (wave 1 [W1]) included 659 low-income maltreated (n = 339) and non-maltreated (n = 320) children aged 10 to 12. The original sample was racially and ethnically diverse (71.6% Black, 11.8% White, 12.6% Latinx, 4.0% biracial, 1% other race) and evenly distributed by gender (50.1% male). Most children were from single parent families (68.7%) with a history of receiving public assistance (96.1%). At wave 2 (W2), emerging adults were on average 19.68-years-old (SD = 1.15), 51.1% female, 53.5% (n=207) maltreated, and identified as Black (68.5%), White (9.2%), Latinx (12.6%), biracial (6.1%), and other (3.7%). W2 participants did not significantly differ from the W1 participants lost to attrition on maltreatment status, χ2 = .14 (1), p = .71, Cramér’s V = .014; sex χ2 = .50 (1), p = .48, Cramér’s V = .027; income, F = 2.76 (679), p = .10, η2 = .005; child lability/negativity, F = .78 (679), p = .38, η2 = .001; or emotion regulation, F = .08 (679), p = .78, η2 = .00.
Procedure
All study procedures were approved by the Institutional Review Board at the University of Rochester. W1 participants were recruited for a summer research camp from 2004–2007. Children in the maltreated group had substantiated investigations of child maltreatment according to Department of Human Services (DHS) Child Protective Services (CPS) records. Children without CPS involvement were recruited from families receiving Temporary Assistance to Needy Families (TANF) to ascertain a sociodemographically-comparable sample of children without maltreatment experiences. A DHS liaison identified eligible families and contacted a random sample from both groups via mail. If families elected to participate, their contact information was shared with research staff.
Parents who chose to enroll their children in the research summer camp provided signed consent to study procedures. During the camp, camp counselors facilitated recreational activities with the same groups of 8–10 children (35 hours of direct contact and observation). Children also provided assent to study procedures. Children self-reported on their functioning and camp counselors provided independent ratings of childhood functioning after the end of the week. Maltreatment status was unknown to camp counselors. For information on summer research camp procedures, see Cicchetti and Manly (1990). At W2 (~eight years after W1), a variety of strategies were used to relocate and recruit W1 participants for a follow-up study during emerging adulthood. Records of last known addresses, extensive public internet searches (e.g., LexisNexis), contact information from medical records, and neighborhood canvasing were part of a comprehensive recruitment design. Interested participants completed signed consents and then participated in three research visits.
Measures
Childhood maltreatment (W1).
The Maltreatment Classification System (MCS; Barnett et al., 1993), a reliable and validated measure of coding maltreatment (Manly, 2005), was used to code CPS records from birth until W1. The MCS yields information regarding exposures to various subtypes of maltreatment, including physical abuse, sexual abuse, emotional maltreatment, and neglect, as well as other maltreatment dimensions. To derive a dimensional categorization of maltreatment, participants were coded as being exposed to threat only (exposure to physical or sexual abuse without neglect), deprivation only (exposure to neglect without abuse exposure), or both threat and deprivation (exposure to abuse and neglect). There were 14 cases of children who experienced emotional maltreatment only in their records; these children were excluded from the analyses because we did not have clarity regarding whether the exposure was emotional abuse or emotional neglect, and thus, we were unable to categorize them as threat or deprivation. There were also another 14 maltreated children who did not have subtype-level information. Among children exposed to maltreatment who were included in the threat/deprivation categorization (N = 193), 23 (11.9%) were included in the threat only group, 59 (30.6%) in the deprivation only group, and 111 (57.5%) in the threat and deprivation group. Children without maltreatment histories were classified as “non-maltreated” (n = 192).
Emotion regulation and lability/negativity (W1).
The ERC (Shields & Cicchetti, 1997) was used to assess emotional regulation and lability/negativity in childhood. The ERC is a well-validated (Shields & Cicchetti, 1997, 1998) and reliable (Kim-Spoon et al., 2013) scale that relies on other-reporters (i.e., camp counselors) to rate children on a 4-point scale indicating their displays of affective behavior. For the present study we used a shortened version of the ERC developed within a similar sample of low-SES urban children (Shields & Cicchetti, 1998). Two subscales of the ERC were used. The emotion regulation subscale consisted of four items regarding the child’s appropriate emotional displays and recognition of emotions (e.g., “Can say when s/he is feeling sad, angry or mad, fearful or afraid”; α = .82). The lability/negativity subscale consisted of three items regarding mood lability and dysregulation (e.g., “Can recover quickly from episodes of upset or distress”, reverse scored; α = .88). Higher scores on emotion regulation indicate superior regulatory skills and higher scores on lability/negativity denote more labile and reactive affective responses1. As discussed prior, the ERC has been used by investigators to examine distinct associations between emotion regulation and lability/negativity both with childhood adversity and consequent psychopathology (Crespo et al., 2017; Kim-Spoon et al., 2013; Shields & Cicchetti, 1998; Shipman et al., 2005).
To determine whether the emotion regulation and lability/negativity scales were indeed distinct factors, we used confirmatory factor analysis to compare a one-factor model against a two-factor model. In doing so, we found that the two-factor model had significantly better model fit compared to the one-factor model, Δχ2 = 130.778 (Δdf = 1), p < .001. These results are consistent with prior investigations (e.g., Kim & Cicchetti, 2013) which also support the two-factor structure of the ERC.
Adult Self-Report (W2; Achenbach & Rescorla, 2003).
The Adult Self-Report (ASR) is a 123-item self-report scale that includes items relating to emotional and behavioral functioning for adults. For each item, participants rated their symptoms over the last six months on a scale of 0 = not true, 1 = somewhat or sometimes true, or 2 = very true or often true. The ASR produces several normed scales (e.g., gender and age) related to problematic functioning. The ASR has strong psychometric properties, including strong test-retest reliability (Achenbach & Rescorla, 2003). The current study used the following problem scales (T scores) for internalizing: depressed/anxious, withdrawn, somatic; and the following problem scales (T scores) for externalizing: aggressive, rule-breaking, intrusive, substance use.
Diagnostic Interview Schedule for DSM-IV (W2; Robins et al., 1995).
The Diagnostic Interview Schedule for DSM-IV (DIS-IV) is a structured clinical interview administered in person with the help of a computer system to provide clinical psychiatric diagnoses and symptom counts based on DSM-IV criteria (APA, 1994). In the current study, modules of the DIS-IV were conducted with participants in a private room by administrators trained on this measure. Dichotomous scores indicating the presence or absence of past-year diagnosis were used for each of the following for internalizing: post-traumatic stress disorder (PTSD), suicidal ideation, major depressive disorder (MDD); and for externalizing: antisocial personality disorder (ASPD), and alcohol/marijuana abuse.
Analytic Plan
All analyses were performed with Mplus version 8.4 (Muthén & Muthén, 2010). The percentage of missing data in the emerging adult sample ranged from 0 to 6.8%. Little’s MCAR (i.e., missing completely at random) test was non-significant, indicating that data were missing completely at random, χ2 = 15.23 (10), p = .12. Full information maximum likelihood (FIML) estimation was used to account for missing data in the latent profile analysis (LPA) and path analysis models. First, we used LPA to investigate classes of comorbid psychopathology in emerging adulthood (W2) with seven continuous indicators (i.e., problem scales from the ASR) and five dichotomous indicators (i.e., past year diagnosis from the DIS, note that alcohol abuse and marijuana abuse were combined into one indicator of substance abuse). Means were allowed to vary between classes and variances were constrained. We tested models with two through six classes and compared them using a variety of fit indices and established conventions (Wickrama et al., 2016). The probability of accurate classification was determined with entropy, with values close to 1.0 considered to have good entropy (Wickrama et al., 2016). In addition, information criterion statistics including the Bayesian information criterion (BIC), sample-size adjusted BIC (ssBIC), and the Akaike information criterion (AIC) were used. For these indicators, lower values indicate a better fitting class solution. Furthermore, a Lo-Mendell-Rubin likelihood ratio test (LMR-LRT) was utilized to test the class solution (k) against the null hypothesis class solution (k-1). Significant results on the LMR-LRT indicate that the k class solution better fits the data as compared to the k-1 class solution. We also considered prior empirical work, theory, and interpretability to choose the best class solution, as recommended by Wickrama et al (2016).
Once the most appropriate class solution was chosen, we tested predictors using the three-step method (Lanza et al., 2013). This method allowed us to examine predictors of class solutions without altering the original properties of the class solutions (Wickrama et al., 2016). Predictors of the categorical psychopathology classes were tested using a multinomial logistic regression framework. We ran three multinomial regression models. First, control variables (race and sex) were entered. Second, dimensions of childhood maltreatment (threat only, deprivation only, and both, dummy coded with non-maltreated as the reference group) were entered, controlling for race and sex. Third, emotion regulation and lability/negativity were entered, also controlling for race and sex (without controlling for dimensions of childhood maltreatment).
Last, we tested the role of emotion regulation and lability/negativity as mediators in the pathways from childhood maltreatment dimensions to comorbid psychopathology classes. To do so, we first saved class solutions as a new variable. This was justified in this case, as the average latent class probabilities for most likely latent class membership ranged from .91 to .95. Following, a path analysis framework was used to test our mediation hypothesis. Predictors included threat only, deprivation only, and both threat/deprivation experiences. These predictors were dummy coded with non-maltreated as the reference group. Emotion regulation and lability/negativity were entered as competing mediators. Control variables included race (dummy coded as 1 = Black and 0 = other) and sex (coded as 1 = male and 2 = female). Confidence intervals for indirect effects were constructed using the delta method (MacKinnon et al., 2007).
Results
Descriptive Statistics
See Table 1 for bivariate correlations and descriptive statistics for all study variables. Threat-only had a significant association with ASPD (r = .11, p < .05), and deprivation-only had a significant association with anxiety/depression (r = .12, p < .05). There were no other significant associations between child maltreatment dimensions and psychopathology indicators.
Table 1.
Bivariate correlations and descriptive statistics (N = 413)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | ||
| 1. | Threat only | |||||||||||||||||||
| 2. | Dep. only | - | ||||||||||||||||||
| 3. | Threat & Dep. | - | - | |||||||||||||||||
| 4. | Lability/Neg | 0.00 | 0.03 | .18*** | ||||||||||||||||
| 5. | Emotion Reg | 0.02 | −0.08 | −0.08 | −.54*** | |||||||||||||||
| 6. | Anx/Dep | 0.00 | .12* | 0.01 | 0.00 | 0.00 | ||||||||||||||
| 7. | Withdrawn | −0.09 | 0.09 | 0.04 | .12 | −0.08 | .64*** | |||||||||||||
| 8. | Somatic | −0.03 | 0.02 | 0.04 | 0.03 | 0.05 | .59*** | .47*** | ||||||||||||
| 9. | Aggressive | 0.04 | 0.04 | 0.08 | .12* | −0.04 | .62*** | .63*** | .54*** | |||||||||||
| 10. | Rulebreaking | −0.04 | 0.06 | 0.08 | .10* | −0.07 | .43*** | .45*** | .36*** | .59*** | ||||||||||
| 11. | Intrusive | 0.03 | −0.01 | 0.04 | 0.04 | 0.07 | .33** | .24*** | .31*** | .41*** | .42*** | |||||||||
| 12. | Sub. Use | 0.06 | 0.06 | 0.00 | 0.08 | 0.02 | .12* | .18*** | .18*** | .27*** | .51*** | .14** | ||||||||
| 13. | PTSD | 0.02 | 0.07 | 0.10 | 0.03 | 0.09 | .21*** | .20*** | .26*** | .19*** | .11* | 0.09 | 0.10 | |||||||
| 14. | ASPD | .11* | 0.00 | −0.01 | 0.03 | 0.03 | 0.06 | 0.07 | 0.04 | .19*** | .32*** | .11* | .32*** | 0.04 | ||||||
| 15. | Sub Abuse | 0.07 | 0.01 | −0.01 | −0.06 | 0.00 | −0.06 | −0.05 | 0.04 | 0.08 | .23*** | 0.07 | .28*** | 0.03 | .24*** | |||||
| 16. | Depression | −0.01 | 0.02 | 0.03 | 0.02 | 0.02 | .32*** | .22*** | .34*** | .31*** | .24*** | .18*** | .12* | .32*** | 0.06 | −0.02 | ||||
| 17. | SI | 0.02 | 0.06 | −0.03 | −0.01 | 0.08 | .36*** | .22*** | .32*** | .33*** | .23*** | .25*** | .12* | .29*** | 0.08 | −0.07 | .62*** | |||
| 18. | Race | −0.04 | 0.06 | −0.05 | .11* | −.14** | −0.07 | 0.00 | −.15** | −0.08 | −0.09 | −0.09 | −0.04 | −0.09 | −0.03 | −0.03 | −.13* | −.12* | ||
| 19. | Sex | 0.05 | 0.02 | −0.01 | −.10* | 0.04 | 0.09 | .14** | .14** | .16** | −0.02 | −0.01 | 0.02 | .13** | −0.03 | −.13** | .22*** | .14** | −0.01 | |
| Mean | 1.94 | 3.01 | 55.67 | 59.43 | 57.34 | 57.54 | 57.09 | 54.93 | 57.63 | |||||||||||
| SD | .60 | .51 | 7.46 | 8.50 | 7.88 | 7.32 | 6.97 | 6.26 | 8.64 | |||||||||||
| % | 5.6 | 14.3 | 26.9 | 6.1 | 22.0 | 5.8 | 15.3 | 7.0 | 71.7 | 51.1 |
Note. Dep = deprivation; Neg = negativity; Reg = regulation; Anx/Dep = anxious/depressed; Sub. = substance; SI = suicidal ideation. Race is coded as 1 = Black and 0 = Other. Sex is coded as 1 = male and 2 = female.
p < .05;
p < .01;
p < .001
Class Solutions
See Table 2 for the fit indices of class solutions with two through six classes. The three-class solution was chosen as the superior class solution based on fit indices and interpretability. As expected, AIC, BIC, and ssBIC values decreased for each k+1 solution and were the lowest in the six-class solution. However, the five and six class solutions each included a class with less than 3.0% of the sample, limiting interpretability of these solutions. The LMR-LRT test was significant for the three-class solution, indicating that this solution was superior to the two-class solution. Additionally, the LMR-LRT test was non-significant for the four-class solution. Further, the four-class solution included two classes that were similar on all measures of psychopathology and thus this solution was theoretically uninterpretable. Consequently, the three-class solution was selected and utilized for all subsequent analyses.
Table 2.
Fit Statistics for the Latent Class Analysis (N = 413)
| Class size (%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Classes | LL | AIC | BIC | Adj BIC | Entropy | LRT (p) | C1 | C2 | C3 | C4 | C5 | C6 |
| 2 | −9971.42 | 20006.84 | 20135.59 | 20034.05 | .88 | < .001 | 70.0% | 30.0% | ||||
| 3 | -9827.48 | 19744.95 | 19926.01 | 19783.21 | .86 | .04 | 57.5% | 32.0% | 10.6% | |||
| 4 | −9749.73 | 19615.46 | 19848.82 | 19664.78 | .88 | .45 | 54.3% | 24.6% | 10.9% | 10.3% | ||
| 5 | −9668.98 | 19479.96 | 19765.63 | 19540.33 | .92 | .22 | 53.0% | 21.3% | 12.1% | 11.3% | 2.2% | |
| 6 | −9626.69 | 19421.38 | 19759.35 | 19492.80 | .92 | .42 | 48.6% | 17.7% | 14.4% | 8.8% | 8.4% | 2.2% |
Note. LL = Loglikelihood; AIC = Akaike information criterion; BIC = Bayesian information criteria; LMR-LRT= Vuong-Lo-Mendell-Rubin Likelihood ratio test. Lower values of AIC and BIC and higher values of entropy indicate better model fit. The selected class is shown in bold.
The characteristics of the three-class solution are displayed in Table 3 and Figure 1. The low psychopathology class consisted of 57.5% of the sample, the severe/comorbid psychopathology class consisted of 10.6% of the sample, and the high externalizing class consisted of 32.0% of the sample. Classes were significantly different on all indicators of psychopathology (see Table 3). Notably, the severe/comorbid psychopathology class had significantly higher scores on all continuous measures of psychopathology except for substance use (the high externalizing class had a significantly higher mean score on substance use compared to the comorbid and low psychopathology classes) than the low psychopathology and high externalizing classes. On dichotomous diagnostic indicators, the severe/comorbid class had a higher probability of PTSD, depression, suicidal ideation, and ASPD compared to the low psychopathology class, while the high externalizing class had a higher probability of PTSD, Depression, ASPD, and substance use compared to the low psychopathology class. Additionally, the severe/comorbid class had a higher probability of depression and suicidal ideation compared to the high externalizing class.
Table 3.
Means and Probabilities for the Three-class Model.
| Mean (SE) for Continuous Indicators | |||||
|---|---|---|---|---|---|
| Indicators | Low Psychopathology (1) (57.5%) | Severe/Comorbid Psychopathology (2) (10.6%) | High Externalizing (3) (32.0%) | Sig. contrastsa | F statistic |
| Anxious/Depressed | 51.74 (.49) | 71.51 (1.57) | 57.41 (.86) | 2>1, 2>3, 3>1 | 407.55*** |
| Withdrawal | 54.59 (.70) | 71.36 (.95) | 64.08 (1.11) | 2>1, 2>3, 3>1 | 206.62*** |
| Somatic | 53.68 (.42) | 69.82 (2.06) | 59.70 (.88) | 2>1, 2>3, 3>1 | 158.32*** |
| Aggressive | 53.08 (.46) | 69.83 (1.48) | 61.40 (.91) | 2>1, 2>3, 3>1 | 319.04*** |
| Rule Breaking | 53.48 (.35) | 64.27 (1.32) | 61.14 (1.26) | 2>1, 2>3, 3>1 | 127.63*** |
| Intrusive | 53.01 (.35) | 61.22 (1.64) | 56.25 (.73) | 2>1, 2>3, 3>1 | 43.99*** |
| 54.69 (.52) | 59.33 (1.60) | 62.45 (1.70) | 2>1, 3>2, 3>1 | 42.47*** | |
| Probabilities (SE) for Dichotomous Indicators | Sig. contrastsb | χ2 statistic | |||
| PTSD | .02 (.01) | .19 (.07) | .10 (.03) | 2>1, 3>1 | 22.74*** |
| Depression | .06 (.02) | .48 (.11) | .22 (.04) | 2>1, 3>1, 2>3 | 57.88*** |
| Suicidal ideation | .01 (.01) | .33 (.10) | .10 (.03) | 2>1, 2>3, 3>1 | 56.25*** |
| ASPD | .14 (.03) | .28 (.07) | .36 (.06) | 2>1, 3>1 | 28.55*** |
| Substance abuse | .04 (.01) | .04 (.03) | .11 (.03) | 3>1 | 6.44* |
Note.
Bonferroni correction used to account for multiple comparisons.
Significance at p < .05 determined with latent class odds ratio results by 95% confidence intervals that do not overlap with 1.
p < .05,
p < .001.
Figure 1.
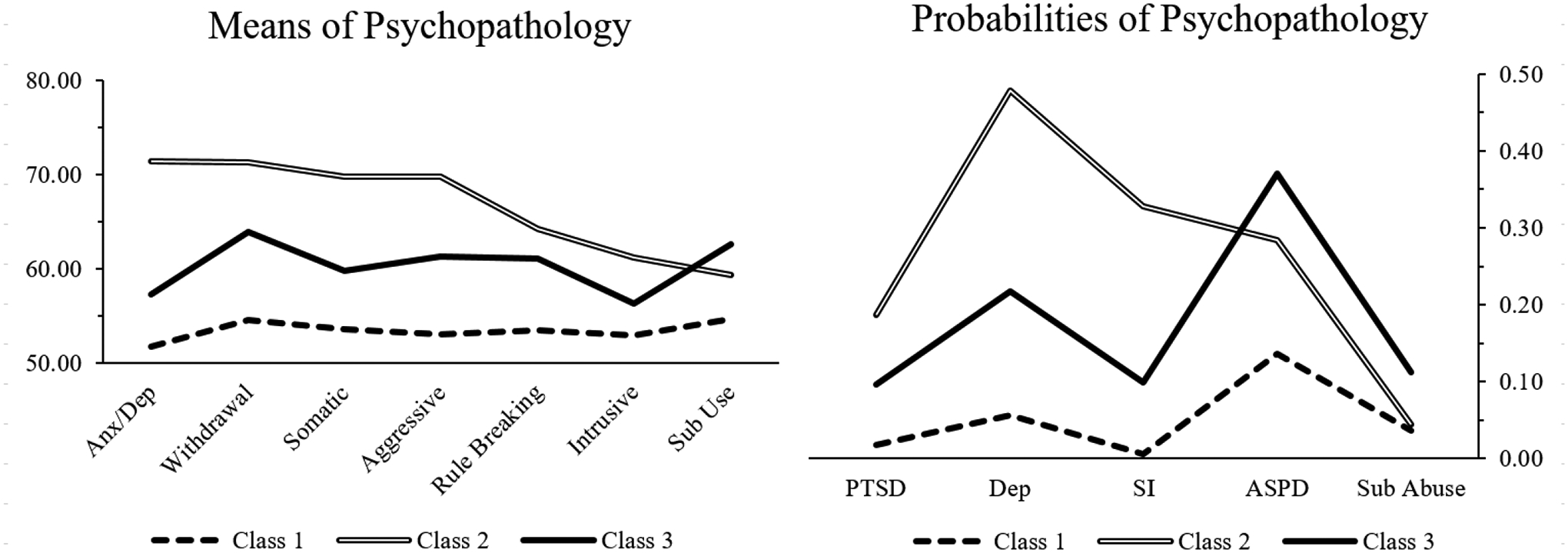
Classes of psychopathology during emerging adulthood (N = 413). There were 57.5% of the sample in Class 1 (Low psychopathology), 10.6% in Class 2 (Severe/Comorbid psychopathology), and 32.0% in Class 3 (High externalizing psychopathology).
Note. PTSD = Post-traumatic stress disorder; Dep = Depression; SI = Suicidal ideation; ASPD = Antisocial personality disorder, Sub = Substance abuse.
Predictors
Predictors of psychopathology classes were tested in a multinomial logistic regression framework (see Table 4). Emerging adults who identified as Black were significantly less likely to be classified in the severe/comorbid class compared to the low psychopathology class (OR = .47, 95% CI [.24, .96]) and compared to the high externalizing class (OR = .39, 95% CI [.18, .87]). Females were significantly more likely to belong to the high externalizing class compared to the low class (OR = 1.72, 95% CI [1.04, 2.85]) and were marginally more likely to belong to the severe/comorbid psychopathology class compared to the low class (OR = 1.92, 95% CI [.95, 3.87]). Child maltreatment experiences characterized by deprivation only (compared to no exposure to maltreatment) were associated with a 3.12-fold (95% CI [1.15, 8.45]) and 4.00-fold (95% CI [1.28, 12.48]) increase in risk for comorbid psychopathology compared to the low psychopathology class and the high externalizing class, respectively. Lability/negativity in childhood was associated with membership in the high externalizing class versus the low psychopathology class (OR = 1.76, 95% CI [1.05, 2.93]).
Table 4.
Logistic Regression ORs and CIs for Predictors
| Comorbid psychopathology vs. Low (c) | High externalizing vs. Low (c) | Comorbid psychopathology vs. High externalizing (c) | ||||
|---|---|---|---|---|---|---|
| Model Predictors | Logit (OR) | 95% CI | Logit (OR) | 95% CI | Logit (OR) | 95% CI |
| Model 1: Control variables | ||||||
| Race | −.75 (.47)* | [.24, .96] | .20 (1.22) | [.68, 2.17] | −.94 (.39)* | [.18, .87] |
| Sex | .65 (1.92)† | [.95, 3.87] | .54 (1.72)* | [1.04, 2.85] | .11 (1.12) | [.51, 2.43] |
| Model 2: Maltreatment dimensions a | ||||||
| Threat only | 1.06 (2.88) | [.79, 10.52] | −.33 (.72) | [.21, 2.46] | 1.39 (4.01)† | [.84, 19.26] |
| Deprivation only | 1.14 (3.12)* | [1.15, 8.45] | −.25 (.78) | [.35, 1.73] | 1.39 (4.00)* | [1.28, 12.48] |
| Threat and deprivation | .61 (1.84) | [.73, 4.62] | −.32 (.73) | [.39, 1.36] | .93 (2.53)† | [.91, 6.99] |
| Model 3: Emotion regulation | ||||||
| Lability-negativity | .42 (1.52) | [.80, 2.89] | .56 (1.76)* | [1.05, 2.93] | −.14 (.87) | [.44, 1.73] |
| Emotion regulation | −.08 (.92) | [.36, 2.35] | .10 (1.10) | [.61, 1.99] | −.18 (.84) | [.30, 2.36] |
Note. Race is coded as 1 = Black and 0 = Other. Sex is coded as 1 = male and 2 = female. ‘C’ refers to the comparison group.
Maltreatment dimensions were dummy coded and entered simultaneously with the non-maltreated group as the reference category.
The predictors for each model are listed below the model number. Models 2 and 3 also contained control variables (race and sex).
p < .10;
p < .05;
p < .01;
p < .001.
Mediation via Emotion Regulation and Lability/Negativity
Last, we used a path analysis framework to test the indirect pathway between childhood maltreatment dimensions and emerging adult psychopathology via emotion regulation and lability/negativity. See Figure 2 for a depiction of the final model2. Due to the estimation method used to account for the categorical outcomes, traditional fit indices (e.g., CFI, RMSEA) were not provided in Mplus. Fit indices were AIC = 4030.52, BIC = 4212.22, LL = −1975.26. Experiences of threat only, deprivation only, and both (compared to no exposure to maltreatment), all significantly predicted lability/negativity at W1. Experiences of deprivation only, and both threat and deprivation, significantly predicted emotion regulation at W1. In turn, higher lability/negativity predicted membership in the high externalizing psychopathology class at W2 compared to the low psychopathology class. There was also a direct association between experiences of deprivation only in childhood and membership in the severe/comorbid psychopathology class at W2 compared to the low psychopathology class. The indirect effect from both threat and deprivation to membership in the high externalizing psychopathology class at W2 via lability/negativity at W1 was significant, α*β = .03, SE = .02, p < .05.
Figure 2.
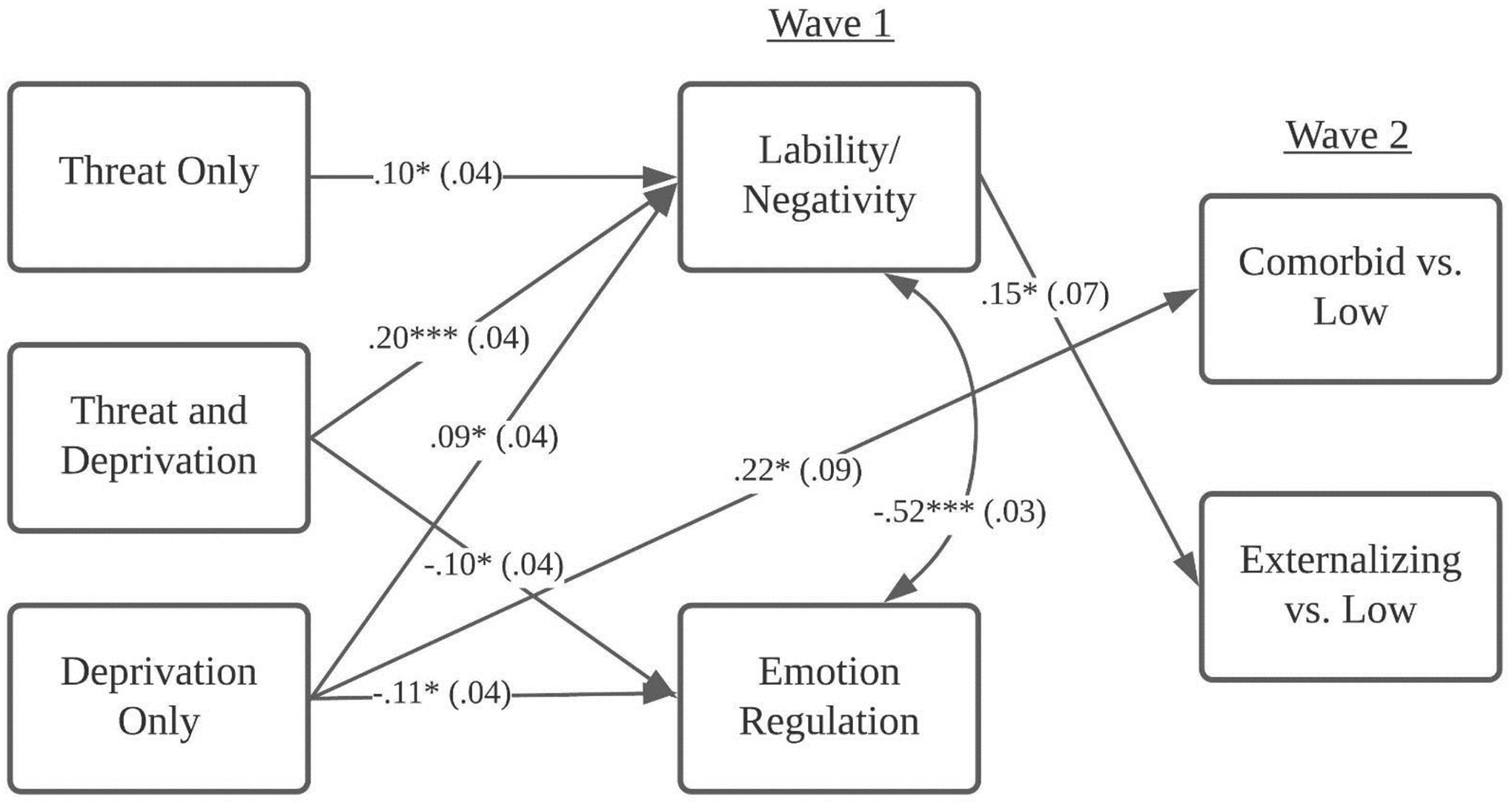
Path model testing the mediating role of emotion regulation and lability/negativity.
Note. Threat only, threat and deprivation, and deprivation only were dummy coded with non-maltreated as the reference group.
*p < .05; **p < .01; ***p < .001
Sensitivity Analysis
We examined a second mediation model that used threat and deprivation as continuous predictors. Threat was operationalized as the maximum number of developmental periods that an individual had experienced emotional abuse, physical abuse, or sexual abuse, and deprivation was operationalized as the maximum number of developmental periods that an individual had experienced neglect (range: 0 to 4). There were no direct associations between the chronicity of threat and deprivation with psychopathology outcomes. More chronic deprivation experiences had a marginally significant effect on emotion regulation, β = −.09, SE = .05, p = .08, and a significant effect on lability/negativity, β = .11, SE = .05, p < .05. More chronic threat conditions had a marginally significant effect on lability/negativity, β = .09, SE = .05, p = .06. There were no significant indirect effects.
Discussion
There were several notable findings of the present study. First, we found three distinct profiles of symptomology which showed both homotypic comorbidity (i.e., within the internalizing and externalizing spectrums) and heterotypic comorbidity (i.e., across the internalizing and externalizing spectrums). The classes that emerged in the present sample differ from other studies that have used a person-centered approach to investigate psychopathology in adolescent and young adult samples, which have identified classes of psychopathology characterized by a high-internalizing symptom class, a high-externalizing symptom class, and a comorbid internalizing and externalizing class (e.g., Olino et al., 2012). Specifically, we did not find a class of psychopathology characterized by high-internalizing symptoms only. This finding might be attributed to the age of our sample and the fact that comorbidity tends to accumulate over time (see Caspi et al., 2020). Thus, it is possible that youth who exhibited internalizing symptoms in childhood eventually developed comorbid externalizing symptoms later in adolescence and young adulthood. Our findings are also consistent with a study using a different, national sample of maltreated and non-maltreated, low-SES children and adolescents, which also failed to find an internalizing-only latent class (Duprey et al., 2020). Thus, the latent structure of psychopathology we found in our sample might be unique to populations of youth with high rates of childhood adversity exposure.
A second aim for our study was to identify specific dimensions of child maltreatment, namely threat and deprivation, as predictors of psychopathology classes in emerging adulthood. We used the MCS to code records of child maltreatment, which we then categorized into threat only, deprivation only, and threat and deprivation combined. Notably, we found that most of the maltreated children in our CPS-involved sample were exposed to both threat and deprivation (57.5%), rather than only one of these dimensions. It is important to note that exposure to emotional maltreatment did not clearly fit in either the threat or deprivation category due to the heterogeneous nature of this type of maltreatment. These findings highlight potential future directions for studies using the dimensional model of childhood maltreatment, as well as the limitations inherent in such models.
We found that childhood maltreatment exposure characterized by deprivation-only was significantly associated with comorbid internalizing and externalizing psychopathology, while exposure to threat-only and exposure to both threat and deprivation did not exhibit the same association. This is consistent with the dimensional model of psychopathology and with other studies that have highlighted the detrimental impact of neglect. The lack of developmentally expected environmental stimuli, such as interactions with stable and nurturing caregivers, can have devastating impacts on a child’s socioemotional development. For instance, in a similar sample of maltreated and non-maltreated demographically matched children, physical neglect during early childhood (infancy through preschool age) was associated with significantly higher scores on externalizing and internalizing behaviors, while controlling for the effects of other types of maltreatment (Manly et al., 2001). Surprisingly, the threat and deprivation category was unrelated to any classes of psychopathology. It is possible that other characteristics of the maltreatment exposure play a role in this finding. For instance, deprivation experiences may be characterized by more severe and/or earlier onset of maltreatment.
We also found that sex was related to the likelihood of membership in the high externalizing class versus the low psychopathology class, such that girls (versus boys) were more likely to belong to the high externalizing class. This result was somewhat surprising given the greater prevalence of externalizing disorders among boys (Mayes et al., 2020) and emerging adult men (Hicks et al., 2007). However, the high externalizing class did have significantly higher mean scores on internalizing symptomology compared to the low psychopathology class, which may have led to this finding.
A third aim of our study was to test emotion regulation and lability/negativity as distinct mechanisms linking exposure to threat and deprivation in childhood to emerging adult psychopathology profiles. We were specifically interested in these mediators due to their underpinnings of cognitive processing and emotion processing, which have been proposed as mechanisms from deprivation and threat exposure, respectively, in the dimensional model of adversity and psychopathology (McLaughlin et al., 2021). Our results presented some evidence for distinct associations between threat and deprivation with emotion regulation and lability/negativity. In our structural model, exposure to threat-only (as compared to no exposure to maltreatment) was associated with increases in emotion lability/negativity in childhood but was unrelated to cognitive emotion regulation skills. Indeed, the dimensional model of psychopathology proposes that threat specifically leads to deficits in emotional processing (including emotional reactivity) that subsequently predicts psychopathology. Thus, our results showing the associations between child maltreatment dimensions and emotion regulation and lability/negativity are in line with prior theory (McLaughlin & Sheridan, 2016). Alternatively, deprivation exposure (including overlapping threat and deprivation) was associated with both higher levels of emotion lability/negativity and lower levels of emotion regulation skills. Youth who are exposed to deprivation are often neglected by their caregivers, and thus may not develop emotion regulation skills that many children do via social learning and modeling from their parents (Kim & Cicchetti, 2009; Weissman et al., 2019). This finding is also consistent with the dimensional model of psychopathology, which puts forth executive functioning as a key mechanism linking deprivation exposure to psychopathology (McLaughlin, 2016). Aspects of executive functioning, such as inhibitory control, underlie higher level emotion regulation skills like cognitive reappraisal (for a review, see Schmeichel & Tang, 2015).
Finally, we found a significant indirect effect between exposure to both threat and deprivation (compared to no exposure to maltreatment) and psychopathology characterized by externalizing symptoms, via increased lability/negativity in childhood. This finding mirrors previous work that has uncovered associations between child maltreatment and lability-negativity (Kim-Spoon et al., 2013), and between emotion reactivity and externalizing symptoms in adolescent samples (Uink et al., 2018). Indeed, emotional lability has been suggested as an underlying feature of homotypic externalizing comorbidity (Beauchaine & McNulty, 2013). Our results extend this work by showing that lability-negativity serves as a developmental mechanism underlying childhood maltreatment and externalizing psychopathology in emerging adulthood, and by characterizing the childhood environments that are likely to lead to this risky developmental trajectory.
Despite this, we did not find evidence of emotion regulation or lability/negativity as mechanisms linking childhood maltreatment with comorbid internalizing and externalizing psychopathology. It is likely that other distinct developmental processes are implicated in the development of comorbid symptomology in emerging adulthood. According to the developmental psychopathology framework, failure to attain certain developmental salient socioemotional tasks throughout childhood, such as the ability to form healthy relationships or the ability to self-regulate, can respectively lead to internalizing and externalizing psychopathology later in life (Cicchetti, 2016; Oland & Shaw, 2005). It is possible that comorbid internalizing and externalizing psychopathology may result from the convergence of multiple socioemotional deficits including social processes and self-regulation processes. Further research that tests these hypotheses will facilitate greater understanding on the nature of internalizing and externalizing comorbidity as a distinct pattern of psychopathology.
There are several limitations of the present study. First, we used a sample of emerging adults who were recruited into the study in childhood based on exposure to maltreatment and/or socioeconomic adversity, and who primarily resided in an urban area of the Northeast United States. Consequently, these results may not generalize to other samples of emerging adults in different geographic areas or who have different levels of exposure to childhood maltreatment. Second, we modeled comorbidity using a person-centered approach. It is possible that there were more classes of psychopathology that existed in the sample, which could not be identified based on our sample size (i.e., more classes could emerge if using a larger sample). Third, we were unable to categorize emotional maltreatment experiences into either threat or deprivation for 14 children in the sample. Emotional maltreatment, as it was measured in the current study, could have included aspects of deprivation such as emotional neglect, or aspects of threat such as denigrating the child. Thus, as we did not have information on the specific experiences that comprised emotional maltreatment, this contributed to missing data on maltreatment dimensions. Finally, there are several limitations of our measurement strategy. We used CPS records to code child maltreatment exposure, which is limited due to the under-reporting of maltreatment. Certain types of maltreatment, such as emotional maltreatment, are especially difficult to detect and tend to go under-reported by CPS. Thus, it is possible that the child maltreatment categories we used in the present study do not truly reflect the occurrence of abuse and neglect that occurred in our sample. Additionally, there are limitations to our measure of emotion regulation and lability/negativity. Children were assessed in a camp setting and thus it is possible that their observed ability to regulate may be specific to this context. The emotion regulation scale of the ERC also does not assess specific regulation strategies that the child uses, and the lability/negativity subscale of the ERC addresses only one aspect of emotion reactivity (i.e., mood lability).
Another major limitation of the present study was the inability to examine the impact of racism and discrimination on developmental outcomes. Most participants in our sample were from racial and ethnic groups that are historically marginalized in the United States. Further, our sample was recruited from the child welfare system, a system that is imbedded with structural racism and in which Black children are overrepresented (Hyunil Kim et al., 2017), and most families resided in low-income neighborhoods. Consequently, the children and families in our sample experienced heightened oppression that likely contributed to various adverse psychopathology outcomes. Future research must consider the role of race and systemic oppression in shaping developmental outcomes among maltreated children and youth.
In conclusion, our results highlight the comorbid nature of psychopathology among a sample of emerging adults who were reared in low-SES environments, and in which approximately half were involved in child maltreatment investigations. There are several implications for clinical practice and prevention that should be considered based on our findings. We found that deprivation-only experiences were associated with higher rates of comorbid internalizing and externalizing psychopathology among emerging adults. This result underscores the need for primary prevention of child maltreatment, and namely the prevention of childhood neglect. Preventive interventions that work with parents and infants to increase parenting skills, provide necessary resources, and prevent child maltreatment, such as the Building Healthy Children program (Demeusy et al., 2021) and the Nurse-Family Partnership (Olds, 2008), may have downstream effects on ameliorating rates of psychopathology for adolescents and emerging adults (for a review, see Toth et al., 2016). Additionally, we found that youth exposed to environments characterized by both threat and deprivation were at risk for developing higher lability-negativity, which in turn led to an increased likelihood of exhibiting externalizing symptoms in emerging adulthood. Clinical interventions that address emotional lability and increase emotional coping skills may be particularly salient for children and adolescents who experience multiple dimensions of child maltreatment.
Acknowledgements:
We are grateful to the Jacobs Foundation (to Dante Cicchetti), National Institute on Drug Abuse (R01-DA01774 to Fred A. Rogosch and Dante Cicchetti), and National Institute on Child Health and Human Development (P50-HD096698 to Dante Cicchetti and Sheree Toth) for their support of this work. Erinn Duprey’s work was also supported by the National Institute on Mental Health (T32-MH020061, PI: Conwell).
Funding:
This work received financial support from the Jacobs Foundation (to Dante Cicchetti), National Institute on Drug Abuse (R01-DA01774 to Fred A. Rogosch and Dante Cicchetti), and National Institute on Child Health and Human Development (P50-HD096698 to Dante Cicchetti and Sheree Toth).
Footnotes
Conflicts of interest/Competing interests: There are no conflicts of interests or competing interests to disclose.
Ethical approval: Approval was obtained from the ethics committee of University of Rochester. The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent to Participate: Informed consent was obtained from legal guardians of minors in the study. Informed consent was obtained from all adult participants in the study.
We removed two items from the ERC (one from the emotion regulation subscale, “is a cheerful child”, and one from the lability/negativity subscale, “is easily frustrated”) due to overlap with internalizing and externalizing psychopathology. The emotion regulation and lability/negativity scales retained good reliability (α = .75 and α = .84, respectively). Results remained the same after this modification. Thus, we decided to retain our results using the original measure.
In a sensitivity analysis, we ran the path analysis including the 14 cases that were dropped due to vagueness of the emotional maltreatment they experienced. The significance of parameters and the overall interpretation of results did not change.
References
- Achenbach TM, & Rescorla LA (2003). Manual for the ASEBA adult forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Aldao A, Gee DG, De Los Reyes A, & Seager I (2016). Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Development and Psychopathology, 28(4), 927–946. 10.1017/S0954579416000638 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469–480. 10.1037//0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Barnett D, Manly JT, & Cicchetti D (1993). Defining child maltreatment: The interface between policy and research. In Cicchetti D, & Toth SL (Eds.), Child abuse, child development, and social policy. Norwood, NJ: Ablex. [Google Scholar]
- Beauchaine TP, & McNulty T (2013). Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Development and psychopathology, 25(4pt2), 1505–1528. 10.1017/S0954579413000746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunford N, Evans SW, Zoccola PM, Owens JS, Flory K, & Spiel CF (2017). Correspondence between heart rate variability and emotion dysregulation in children, including children with ADHD. Journal of Abnormal Child Psychology, 45, 1325–1337. 10.1007/s10802-016-0257-2 [DOI] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Ambler A, Danese A, Elliott ML, Hariri A, Harrington HL, Hogan S, Poulton R, Ramrakha S, Rasmussen LJH, Reuben A, Richmond-Rakerd L, Sugden K, Wertz J, Williams BS, & Moffitt TE (2020). Longitudinal assessment of mental health disorders and comorbidities across 4 decades among participants in the dunedin birth cohort study. JAMA Network Open, 3(4), e203221. 10.1001/jamanetworkopen.2020.3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, Meier MH, Ramrakha S, Shalev I, Poulton R, & Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2(2), 119–137. 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan YF, Dennis ML, & Funk RR (2008). Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment, 34(1), 14–24. 10.1016/j.jsat.2006.12.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D (2016). Socioemotional, personality, and biological development: Illustrations from a multilevel developmental psychopathology perspective on child maltreatment. Annual Review of Psychology, 67(1), 187–211. doi: 10.1146/annurev-psych-122414-033259 [DOI] [PubMed] [Google Scholar]
- Cicchetti D, & Banny A (2014). A developmental psychopathology perspective on child maltreatment. In Lewis M & Rudolph KD (Eds.), Handbook of Developmental Psychopathology (pp. 723–741). Springer US. doi: 10.1007/978-1-4614-9608-3_37 [DOI] [Google Scholar]
- Cicchetti D, & Manly JT (1990). A personal perspective on conducting research with maltreating families: Problems and solutions. In Brody G & Sigel I (Eds.), Methods of family research: Families at risk (Vol. 2, pp. 87–133). Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Coates AA, & Messman-moore TL (2014). A structural model of mechanisms predicting depressive symptoms in women following childhood psychological maltreatment. Child Abuse & Neglect, 38(1), 103–113. 10.1016/j.chiabu.2013.10.005 [DOI] [PubMed] [Google Scholar]
- Crespo LM, Trentacosta CJ, Aikins D, & Wargo-Aikins J (2017). Maternal emotion regulation and children’s behavior problems: The mediating role of child emotion regulation. Journal of Child and Family studies, 26(10), 2797–2809. 10.1007/s10826-017-0791-8 [DOI] [Google Scholar]
- Demeusy EM, Handley ED, Manly JT, Sturm R, & Toth SL (2021). Building Healthy Children: A preventive intervention for high-risk young families. Development and Psychopathology, 1–16. 10.1017/S0954579420001625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dugré JR, Dumais A, Dellazizzo L, & Potvin S (2020). Developmental joint trajectories of anxiety-depressive trait and trait-aggression: Implications for co-occurrence of internalizing and externalizing problems. Psychological Medicine, 50(8), 1338–1347. 10.1017/S0033291719001272 [DOI] [PubMed] [Google Scholar]
- Duprey EB, Oshri A, & Liu S (2020). Developmental pathways from child maltreatment to adolescent suicide-related behaviors: The internalizing and externalizing comorbidity hypothesis. Development and Psychopathology, 32(3). doi: 10.1017/S0954579419000919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvir Y, Ford JD, Hill M, & Frazier JA (2014). Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. Harvard Review of Psychiatry, 22(3), 149–161. 10.1097/HRP.0000000000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Racusin R, Ellis CG, Daviss WB, Reiser J, Fleischer A, & Thomas J (2000). Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment, 5(3), 205–217. 10.1177/1077559500005003001 [DOI] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Reboussin BA, Mayfield A, Frazier PH, & Treadway SL (2009). Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: Developmental changes. Journal of Consulting and Clinical Psychology, 77(2), 281–290. 10.1037/a0014732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruhn MA, & Compas BE (2020). Effects of maltreatment on coping and emotion regulation in childhood and adolescence: A meta-analytic review. Child Abuse & Neglect, 103, 104446. [DOI] [PubMed] [Google Scholar]
- Hagan MJ, Roubinov DS, Mistler AK, & Luecken LJ (2014). Mental health outcomes in emerging adults exposed to childhood maltreatment: The moderating role of stress reactivity. Child Maltreatment, 19, 156–167. 10.1177/1077559514539753 [DOI] [PubMed] [Google Scholar]
- Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, & McGue M (2007). Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: A longitudinal twin study. Journal of Abnormal Psychology, 116(3), 433–447. 10.1037/0021-843X.116.3.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 62(6), 593. 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kim-Spoon J, Cicchetti D, & Rogosch FA (2013). A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development, 84, 512–527. 10.1111/j.1467-8624.2012.01857.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Hyunil, Wildeman C, Jonson-Reid M, & Drake B (2017). Lifetime prevalence of investigating child maltreatment among US children. American Journal of Public Health, 107(2), 274–280. 10.2105/AJPH.2016.303545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Hyunsik, & Eaton NR (2017). A hierarchical integration of person-centered comorbidity models: structure, stability, and transition over time. Clinical Psychological Science, 5(4), 595–612. 10.1177/2167702617704018 [DOI] [Google Scholar]
- Kim J, & Cicchetti D (2009). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. 10.1111/j.1469-7610.2009.02202.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annual Review of Clinical Psychology, 2, 111–133. 10.1146/annurev.clinpsy.2.022305.095213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, & Bray BC (2013). Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling: A Multidisciplinary Journal, 20(1), 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavi I, Katz LF, Ozer EJ, & Gross JJ (2019). Emotion reactivity and regulation in maltreated children: A meta-analysis. Child Development, 90(5), 1503–1524. 10.1111/cdev.13272 [DOI] [PubMed] [Google Scholar]
- Leaberry KD, Walerius DM, Rosen PJ, Fogleman ND (2017) Emotional lability. In: Zeigler-Hill V, Shackelford T (eds) Encyclopedia of Personality and Individual Differences. Springer, Cham. 10.1007/978-3-319-28099-8_510-1 [DOI] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology, 58(1), 593–614. 10.1146/annurev.psych.58.110405.085542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly JT (2005). Advances in research definitions of child maltreatment. Child Abuse & Neglect, 29(5), 425–439. 10.1016/j.chiabu.2005.04.001 [DOI] [PubMed] [Google Scholar]
- Manly JT, Kim JE, Rogosch FA, & Cicchetti D (2001). Dimensions of child maltreatment and children’s adjustment: Contributions of developmental timing and subtype. Development and Psychopathology, 13(4), 759–782. [PubMed] [Google Scholar]
- Martin RE, & Ochsner KN (2016). The neuroscience of emotion regulation development: Implications for education. Current opinion in behavioral sciences, 10, 142–148. 10.1016/j.cobeha.2016.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayes SD, Castagna PJ, & Waschbusch DA (2020). Sex differences in externalizing and internalizing symptoms in ADHD, autism, and general population samples. Journal of Psychopathology and Behavioral Assessment, 1–8. [Google Scholar]
- McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, & Viding E (2011). Heightened neural reactivity to threat in child victims of family violence. Current Biology, 21, R947–R948. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA (2016). Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child and Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Winter W, Fox NA, Zeanah CH, & Nelson CA (2014). Widespread reductions in cortical thickness following severe early-life deprivation: a neurodevelopmental pathway to attention-deficit/hyperactivity disorder. Biological Psychiatry, 76, 629–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, Humphreys KL, Belsky J, & Ellis BJ (2021). The value of dimensional models of early experience: Thinking clearly about concepts and categories. Perspectives on Psychological Science, 16, 1463–1472. 10.1177/1745691621992346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AB, Machlin L, McLaughlin KA, & Sheridan MA (2021). Deprivation and psychopathology in the Fragile Families Study: A 15-year longitudinal investigation. Journal of Child Psychology and Psychiatry and Allied Disciplines, 62(4), 382–391. 10.1111/jcpp.13260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller RT, Vascotto NA, Konanur S, & Rosenkranz S (2013). Emotion regulation and psychopathology in a sample of maltreated children. Journal of Child & Adolescent Trauma, 6, 25–40. 10.1080/19361521.2013.737441 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus User’s Guide: Statistical Analysis with Latent Variables: User’s Guide. Muthén & Muthén. [Google Scholar]
- Oland AA, & Shaw DS (2005). Pure versus co-occurring externalizing and internalizing symptoms in children: The potential role of socio-developmental milestones. Clinical Child and Family Psychology Review, 8(4), 247–270. 10.1007/s10567-005-8808-z [DOI] [PubMed] [Google Scholar]
- Olds DL (2008). Preventing child maltreatment and crime with prenatal and infancy support of parents: The Nurse‐Family Partnership. Journal of Scandinavian Studies in Criminology and Crime Prevention, 9(sup1), 2–24. 10.1080/14043850802450096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Farmer RF, Seeley JR, & Lewinsohn PM (2012). Examination of the structure of psychopathology using latent class analysis. Comprehensive Psychiatry, 53(4), 323–332. 10.1016/j.comppsych.2011.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öner S (2018). Neural substrates of cognitive emotion regulation: A brief review. Psychiatry and Clinical Psychopharmacology, 28(1), 91–96. 10.1080/24750573.2017.1407563 [DOI] [Google Scholar]
- Oshri A, Rogosch FA, & Cicchetti D (2013). Child maltreatment and mediating influences of childhood personality types on the development of adolescent psychopathology. Journal of Clinical Child & Adolescent Psychology, 42(3), 287–301. doi.org/ 10.1080/15374416.2012.715366 [DOI] [PubMed] [Google Scholar]
- Pavlova B, Perroud N, Cordera P, Uher R, Dayer A, & Aubry JM (2016). Childhood maltreatment and comorbid anxiety in people with bipolar disorder. Journal of Affective Disorders, 192, 22–27. 10.1016/j.jad.2015.12.002 [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler L, Bucholz K, Compton W, North CS, & Rourke KM (1995). Diagnostic interview schedule for DSM-IV. St Louis, MO: Washington University Press. [Google Scholar]
- Rogosch FA, Oshri A, & Cicchetti D (2010). From child maltreatment to adolescent cannabis abuse and dependence: A developmental cascade model. Development and Psychopathology, 22(04), 883–897. 10.1017/S0954579410000520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmeichel BJ, & Tang D (2015). Individual differences in executive functioning and their relationship to emotional processes and responses. Current Directions in Psychological Science, 24(2), 93–98. 10.1177/0963721414555178 [DOI] [Google Scholar]
- Shields A, & Cicchetti D (1997). Emotion regulation among school-age children: The development and validation of a new criterion Q-sort scale. Developmental Psychology, 33(6), 906–916. 10.1037/0012-1649.33.6.906 [DOI] [PubMed] [Google Scholar]
- Shields A, & Cicchetti D (1998). Reactive aggression among maltreated children: The contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology, 27(4), 381–395. [DOI] [PubMed] [Google Scholar]
- Shipman K, Edwards A, Brown A, Swisher L, & Jennings E (2005). Managing emotion in a maltreating context: A pilot study examining child neglect. Child Abuse & Neglect, 29(9), 1015–1029. doi: 10.1016/j.chiabu.2005.01.006 [DOI] [PubMed] [Google Scholar]
- Toth SL, Petrenko CLM, Gravener-Davis JA, & Handley ED (2016). Advances in prevention science: A developmental psychopathology perspective. In Cicchetti D (Ed.), Developmental Psychopathology (Volume Fou, pp. 1–59). John Wiley & Sons, Inc. 10.1002/9781119125556.devpsy416 [DOI] [Google Scholar]
- U.S. Department of Health & Human Services, Administration for Children and Families, Administration on Children, Youth and Families, C. B. (2021). Child Maltreatment 2019.
- Uink B, Modecki KL, Barber BL, & Correia HM (2018). Socioeconomically disadvantaged adolescents with elevated externalizing symptoms show heightened emotion reactivity to daily stress: An experience sampling study. Child Psychiatry and Human Development, 49(5), 741–756. 10.1007/s10578-018-0784-x [DOI] [PubMed] [Google Scholar]
- Warmingham JM, Handley ED, Rogosch FA, Manly JT, & Cicchetti D (2019). Identifying maltreatment subgroups with patterns of maltreatment subtype and chronicity: A latent class analysis approach. Child Abuse & Neglect, 87, 28–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, & McLaughlin KA (2019). Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Development and Psychopathology, 31(3), 899–915. 10.1017/S0954579419000348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama KKAS, Lee TK, O’Neal CW, & Lorenz FO (2016). Higher-Order Growth Curves and Mixture Modeling with Mplus: A Practical Guide. Routledge. [Google Scholar]
- Willner CJ, Gatzke-Kopp LM, & Bray BC (2016). The dynamics of internalizing and externalizing comorbidity across the early school years. Development and Psychopathology, 28(4pt1), 1033–1052. 10.1017/S0954579416000687 [DOI] [PMC free article] [PubMed] [Google Scholar]


