Highlights
-
•
Videoconferencing allows for face-to-face interactions and visual aids for patient education.
-
•
Patients were highly satisfied with videoconferencing for virtual patient education.
-
•
Radiation Therapists reported videoconferencing and in-person patient education were comparable.
Keywords: Patient Education, Virtual Care, Videoconferencing, Radiation therapist
Abstract
Purpose
Pre-radiotherapy patient education led by Radiation Therapists (RTT) has been shown to improve patients’ distress and overall experiences. In an effort to offer a remote delivery method while allowing for visual learning and face-to-face communication, this pilot project evaluated the feasibility and acceptability of using virtual videoconferencing for patient education.
Methods
This prospective pilot study integrated virtual patient education into standard care. This workflow consisted of a one-on-one, 45-minute tele-education session with an RTT on the day prior to CT-simulation. For this study, patients were offered the option to complete the session using web-based videoconferencing if they had the capability for it. Feasibility was evaluated as the proportion of patients who agreed to and completed virtual education. To evaluate acceptability, patients and RTTs were then emailed post-intervention surveys evaluating their satisfaction with virtual patient education.
Results
Over three months 106 of 139 patients (76%) approached consented to virtual education. The median (range) age was 65 (27–93), 69% were male and most had genitourinary (38%) or head-and-neck (29%) cancers. Ninety patients (85%) completed virtual education as planned, with incompletions due to scheduling (8) or patient technical issues (7), or treatment cancellation (1). Sixty-eight patients completed surveys, with the vast majority agreeing virtual education was clear (94%) and helped them prepare (100%), they were comfortable with the technology (96%) and they were satisfied overall (99%). Twelve RTTs responded, suggesting overall that virtual education was higher quality though less feasible than tele-education, and comparable to in-person education.
Conclusion
Offering individual, RTT-led virtual education using videoconferencing to patients pre-radiotherapy was feasible and acceptable in this pilot study, and is therefore being recommended as an option for all our patients. Future work will directly compare the effectiveness of in-person versus virtual education, and incorporate individual patient needs and preferences.
Introduction
Nearly 50% of patients with cancer experience increased anxiety and distress prior to radiotherapy [1]. From the patients’ perspective, this can result in unpreparedness, a lack of engagement, reduced ability to self-manage care, and unwillingness to adhere to evidenced-based radiotherapy regimes that improve clinical outcomes [1]. Unprepared patients also result in re-scheduled or lengthened appointments, and repeated procedures which drain resources and decrease capacity of RTTs to treat patients. However, conducting patient education traditionally during the first appointment in the radiotherapy pathway, typically CT-simulation, can be ineffective as it requires patients to learn new information while unwell, overwhelmed, and anxious [2]. A patient education needs assessment by Li et al., showed that most patients prefer to receive information about the radiotherapy pathway well in advance of the first radiotherapy appointment [3]. Ensuring appropriate and timely education is delivered to patients may reduce anxiety and distress prior to radiotherapy, and could resolve the associated impacts to patients and clinical resources.
Pre-radiotherapy education sessions have traditionally been conducted in-person, the reputed gold standard. Halkett et al. reported on a randomized trial demonstrating improved patient knowledge and preparedness, and reduced patient anxiety with pre-radiotherapy education conducted with a radiation therapist (RTT) in-person [1]. However, in-person care is resource intensive and requires additional visits to cancer centres which may add barriers to equitable patient education as over 40% report needing unpaid work leave to attend [2]. The 2020 coronavirus pandemic also compelled centres to rapidly limit on-site clinic visits while minimizing disruptions to patient care. Berlin et al. reported how a large academic cancer centre increased the proportion of ambulatory clinic visits using virtual medical care from <1% pre-pandemic to 68% with high patient and practitioner satisfaction [4]. These results included virtual care via telephone (81%) or videoconferencing (19%), with the latter being more likely to be considered a suitable replacement for in-person care and to be requested for future visits [4]. There is a paucity of research reporting experiences of virtual care by RTT specifically, including virtual education.
Several other technology-focused strategies, described below, aimed at streamlining patient education have been prospectively evaluated and been shown to be beneficial. Virtual reality tools allow for immersive and interactive patient sensory experiences of the treatment room prior to treatment commencing [5], [6], [7], although availability of this technology is a barrier to widespread use. More simplistic videos demonstrating didactic material and patient narratives, ranging from 7 to 23 min in length, can also be effective [8], [9]. However, alone they do not allow for patient-provider communication, assessing comprehension and the opportunity for patients to ask questions. The acceptability of these interventions can also vary widely with radiotherapy patient demographics and even individual preferences [3]. In comparison, RTT-led education delivered one-on-one remains a flexible, patient-centered approach [10], that may be further enhanced with current technological advances and social norms.
Given the prospective trials described above that support RTT-delivered patient education, and recent growth and acceptance of remote education for non-patient learners and educators, we aimed to address the gap in virtual education for cancer patients receiving radiotherapy. This pilot study integrated web-based videoconferencing for virtual patient education, and evaluated its feasibility and acceptability by RTTs and patients. It was hypothesised that this strategy could offer the benefits of remote delivery and visual aides previously used for in-person education, to provide the best patient-centered care.
Methods
Project overview
This prospective, single-institution project aimed to integrate virtual patient education into routine radiotherapy care. Hereafter virtual education is defined as being delivered with videoconferencing. It was formally approved (ID# 21-0320) as a quality improvement (QI) project and exempt from research ethics board review. A plan-do-study-act approach was used over the 3-month pilot phase to gain experience, refine workflows and expand to additional staff and patient groups. RTTs were encouraged to give ad hoc feedback, which in addition to patient feedback (see Section ‘Evaluation’), was reviewed biweekly by the project team.
The standard practice at our institution beginning with the coronavirus pandemic in 2020 was for all new patients to have a one-on-one, tele-education with an RTT the day prior to CT-simulation. The sessions are tailored to the patients’ specific tumor site for which their RTT is a specialist in its technique and management. Generally, RTTs review technical procedures, preparation, scheduling, side effects, supportive care and allow for patients to ask questions. These telephone appointments were booked for up to 45-minutes. For this project, patients were given the option to complete the session virtually using video conferencing.
Implementation
Each RTT received individual training on the video-conferencing platform, workflows, and institutional best-practice guidelines for virtual care. The interim process to screen for eligible patients was performed by project team members as follows. Patients were included if they were pre-booked for standard care tele-education, and had consented to the use of email and virtual care as indicated in their electronic medical chart. Patients were excluded if they had a previous radiotherapy course, as they would have already been familiar with radiotherapy. Patients with low or absent English proficiency were included as they typically had English-speaking caregivers participate, or had an interpreter provided by the institution as per standard practice..
Those eligible were contacted 2 days before their scheduled tele-education and offered the option to switch to virtual education if they had the capability, which is defined as access to computer/tablet/laptop with microphone, webcam, and internet connection. Patients who did not meet the criteria, did not have the capability or who declined, proceeded with the standard tele-education.
Virtual patient education
Patients who agreed to virtual education were emailed appointment details and basic instructions on how join the session (Microsoft Bookings v1.5, Microsoft Corp., Redmond USA). They were informed they could share the email with others they wished to join (e.g. caregivers). A reminder email was sent one day prior to the appointment.
Virtual education was performed using a web-based videoconferencing application (Microsoft Teams v1.5). Patients and RTTs used microphones and webcams to allow for virtual face-to-face communication. At the beginning of the session RTTs confirmed the patient’s identity, their consent for other participants joining (if applicable), privacy risks inherit with virtual care, requested they not record the session and their verbal consent to proceed. The RTTs covered site-specific material, similar to tele-education, and additionally projected a visual presentation (Microsoft PowerPoint) composed of graphical aids, photos and plain language text. These visual educational materials were initially developed by RTTs at our institution for in-person education prior to the pandemic, and were repurposed and updated for virtual education.
If for any reason it was not possible to perform virtual education (e.g., technical difficulties) the RTTs completed the session over the telephone per standard practice.
Evaluation
Basic demographic data (age, sex, and tumor site) was extracted from the charts (Mosaiq v2.83, Elekta Inc, Sunnyvale, USA) for all patients scheduled for education. The primary operational metrics to assess feasibility were the proportion of patients who were eligible for virtual education, agreed to virtual education, and completed it as planned within the 45 min session. It was estimated that 15–20% of all patients could participate in virtual care based on published data from our institution [4] and this threshold should be met to sustain RTT skills for this initiative long term.
To primarily assess acceptability, patients and RTTs who completed a virtual education session were given the option to anonymously complete paper or web-based (REDCap v12.0.25, Vanderbilt University, USA) stakeholder surveys adapted from Berlin et al. [4]. Questions gauged perceived feasibility (e.g., efficacy, integration of processes/technology) and acceptability (e.g., satisfaction, intent to continue) using 5-point Likert scale responses, plus an opportunity to provide open-ended feedback (see Appendix). Patients were offered their survey within one week of completing their session while RTTs were offered their survey after one- and three-months of the pilot period. All quantitative data were analyzed using descriptive statistics.
Results
Clinical operations
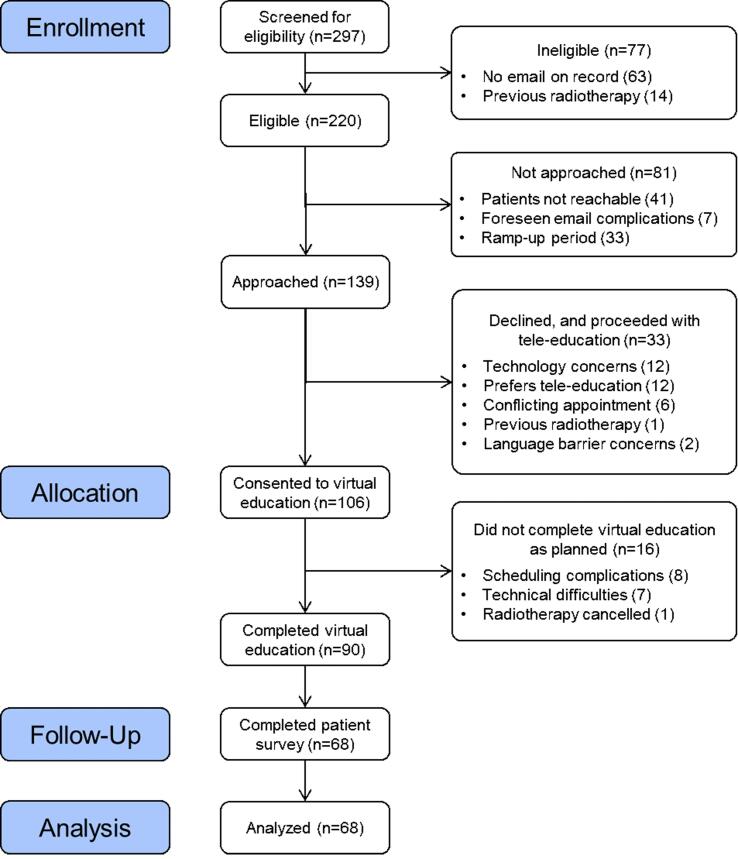
This pilot was initiated in one of four clinical teams and then expanded to a second after 1 month, with these teams focusing on pelvic, and head and neck cancers respectively. Some eligible patients were intentionally not approached to allow for a ramp-up period and for RTTs to gain comfort with procedures. The patient flow over the 3-month pilot is shown in Fig. 1 and patient demographics in Table 1. As a result of the continuous improvement process and RTT feedback, minor updates to the visual presentations were made and RTTs were provided functionality to host virtual education remotely (i.e. working from home) when scheduling permitted it. The pilot was not expanded to the remaining teams and patient groups due to the limited pilot resources and interim booking process (e.g. difficulty reaching patients by phone).
Fig. 1.
Patient flow diagram.
Table 1.
Patient demographics.
| Demographic Data | Allocation During Pilot Project |
||
|---|---|---|---|
| Consented to virtual education (n = 106) |
All others (n = 191) |
||
| Age, median (range) | 65 (27–93) | 67.5 (24–95) | |
| Tumor site, No. (%) | Endocrine | 2 (2%) | 4 (2%) |
| Head and neck | 31 (29%) | 55 (29%) | |
| Eye | 2 (2%) | 3 (2%) | |
| Genitourinary | 40 (38%) | 70 (37%) | |
| Gynecological | 13 (12%) | 24 (12%) | |
| Lower gastrointestinal | 12 (11%) | 25 (13%) | |
| Skin | 6 (6%) | 10 (5%) | |
| Sex, No. (%) | Male | 73 (69%) | 142 (74%) |
| Female | 33 (31%) | 49 (26%) | |
Over three months, 74% (200/297) of patients pre-booked for tele-education were eligible for virtual education. Of the patients approached, 76% (106/139) opted to switch to the virtual education option. In the minority who declined, the most common reasons given by patients were technology concerns (i.e. availability, or computer literacy) or preference to continue with tele-education. Eighty-five percent of patients (90/106) completed virtual education as planned. Those that were not completed were largely due to unforeseen scheduling issues with either the patient or RTT, or, technical patient difficulties with video-conferencing. In total, 30% of all patients scheduled for pre-radiotherapy education (90/297) completed it virtually during the pilot period.
The average (range) time to complete the sessions was 36 (12–80) minutes, with 75% of sessions being completed within ≤45 min. In 7% (6/90) of sessions additional participants, such as support family and friends, joined remotely from a device separate to that of the patient.
Patient survey results
A 76% survey response rate (68/90) was received for those who completed virtual education (Fig. 2). The vast majority responded positively (agree or strongly agree) to statements that it helped their understanding/preparation of radiation (100%), they were comfortable with the technology (96%) and asking questions (97%), the procedural information was clear (94%), that it should continue to be offered (100%) and they were satisfied overall (99%). Results varied when responding to whether they still had outstanding questions about radiotherapy. When asked what the best method of patient education is, 100% selected virtual education over telephone or in-person delivery. Patients commented, “Because I'm a visual learner, I appreciated the PowerPoint presentation. [It] made it easy to understand” – Patient 1, “[It] worked very well for us and we believe it was better than a phone call for sure. We were able to ask questions, and all was explained to us very well” – Patient 2, and “Nowadays, video conferencing is the norm. It's putting a real person behind the voice. [It was] much more personable. This is definitely the way to go if patients are used to the technology” – Patient 3.
Fig. 2.
Patient survey responses on virtual education (N = 68).
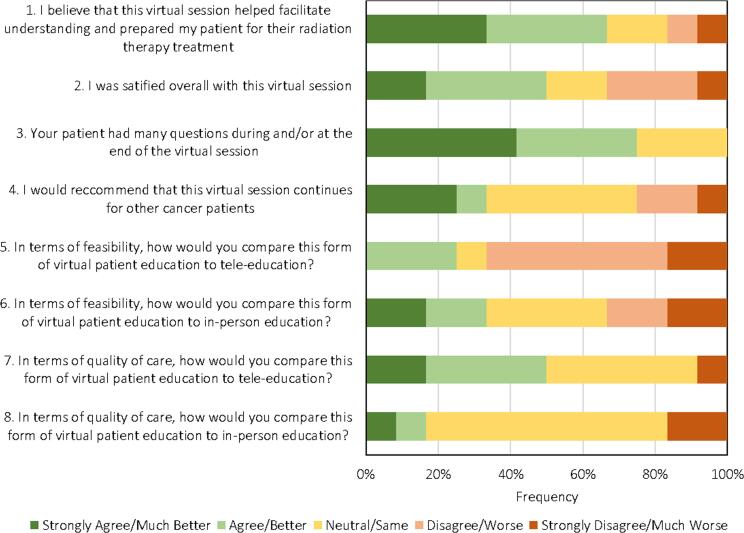
RTT survey results
Fifteen RTTs were trained and hosted one or more virtual patient education sessions. Twelve survey responses were received in total (7 after 1 month, 5 after 3 months) and these were combined for analysis (Fig. 3). The majority were either positive or neutral in regard to virtual education when responding to whether it helped patient understanding/preparation, whether patients asked questions, that it should continue to be offered, and overall satisfaction. The majority of responses indicated virtual education was either ‘much better’, ‘better’ or the ‘same’ with respect to quality of care compared to in-person or tele-education, and with respect to feasibility compared to in-person education. However, the majority indicated it was ‘worse’ or ‘much worse’ in terms of feasibility compared to tele-education. RTTs commented on the positive aspects, for example “[The] ability to show pictures makes it easier to explain and describe procedures (ie- mask making, daily treatments, etc.). [It is a] more personalized experience for the patient”. Some comments questioned the feasibility of virtual education when compared to tele-education, noting that there are more technical issues to navigate and patients appeared to ask more questions which resulted in exceeding the appointment time allocated.
Fig. 3.
RTT survey responses on virtual education (N = 12).
Discussion
This study demonstrated that virtual pre-radiotherapy patient education sessions enhanced understanding and preparedness for radiotherapy, was highly acceptable to patients, and preferred over in-person and tele-education. For patients’ who had the capability and agreed to virtual education, there was a high completion rate with minimal technical issues. RTTs reported good acceptability, suggested it was comparable to in-person education, and also identified opportunities to further streamline workflows. To our knowledge, this is the first report on the feasibility and acceptability of virtual education delivered to cancer patients receiving radiotherapy using videoconferencing, in a one-to-one setting with an RTT.
A potential barrier with virtual education is equitable access, for example, in older demographics who are less likely to have access to digital health tools [11]. In this study however, most patients were eligible to participate and only a small proportion perceived or experienced technology-related issues and this barrier may not be as significant as previously thought [11], [12]. Providing options for patients and considering individual preferences, including in-person or tele-education, would ensure equitable access and patient-centered care.
The high acceptability by patients with respect to RTT-led virtual education is similar to that reported for virtual cancer care by Berlin et al. [4]. In this study patients were noted to have many questions during the virtual education session, with RTTs indicating this occurred more frequently than tele-education. This suggests a more active exchange of information between RTTs and patients, a motivation for patients to learn radiotherapy concepts and increased patient engagement [13]. The content of these pre-radiotherapy education sessions, which was not the focus of the current study, may require refinement or individualization as a sizable minority of patients still had unanswered questions.
Virtual care and education has been associated with positive outcomes in other heath professions, similar to the present study. Within chronic disease management education and occupational therapy, the majority of participants preferred virtual over in-person care, with the virtual care being feasible, accessible and easy to operate [14], [15]. Virtual care in nutrition, nursing, and physical therapy has reduced in-person visits for individuals with chronic illnesses while maintaining clinical standards [16], [17]. Although virtual care has been catalyzed from the pandemic, one report in the field of dermatology showed that a vast majority of patients will continue to prefer virtual care in a post pandemic world [18]. These comparisons suggest that outside of radiotherapy, virtual care and education is being implemented to a similar high degree of acceptability and feasibility and may warrant continued use as an increasing expectation by patients. Maintaining progression through technological advances and social norms is also essential to provide the best patient-centred care.
An ideal future state may be one where RTTs can also recommend the most effective education delivery method based on patient factors. Unfortunately, a recent systematic review reported that direct comparisons between virtual and in-person cancer care are currently limited and generally lower quality evidence [19]. Prospective comparisons between videoconferencing-education, tele-education, and in-person education are required to evaluate effectiveness. Virtual education is likely to play a pivotal role in providing options to equitable education which can result in better patient-centered care in the future.
Limitations
This pilot study included only specific tumor sites and patient groups which limits its generalizability. Similarly, patients had to have existing capability for virtual education and agree to participation, which may have added selection bias and impacted the high patient satisfaction results. Only a small number of RTTs participated and they may have experienced recall bias at the time of the survey completion. Interpreters were not required for any of the patients who participated in virtual education in this pilot, however their inclusion would expected to be seamless given that patients’ had caregivers join from additional devices. Although these are all potential limitations of the current work, this strategy does advance patient education by offering individuals more choice in their care [2], [3].
Conclusion
Offering individual, RTT-led virtual education to patients pre-radiotherapy was feasible and acceptable in this pilot study. Web-based videoconferencing education allows for both visuals and personable patient-RTT interactions, while being done remotely, and is therefore being recommended as an option for all our patients. Future research is needed to evaluate effectiveness of different patient education modalities.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors thank the Virtual Care and IT/Digital teams at UHN for their support, and the radiation therapists for performing the project procedures and their feedback
Appendix.
 |
 |
 |
 |
References
- 1.Halkett G., O’Connor M., Jefford M., Aranda S., Merchant S., Spry N., et al. RT prepare: A radiation therapist-delivered intervention reduces psychological distress in women with breast cancer referred for radiotherapy. Br J Cancer. 2018;118(12):1549–1558. doi: 10.1038/s41416-018-0112-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Giuliani M., Papadakos T., Papadakos J. Propelling a new era of patient education into practice—cancer care post–covid-19. Int J Radiat Oncol Biol Phys. 2020;108(2):404–406. doi: 10.1016/j.ijrobp.2020.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li W., Hill C., Cashell A., Hindle D., Feuz C., Rosewall T. Could knowledge of patient demographics facilitate a personalized approach to radiation therapy patient education? J Med Imag Radiat Sci. 2022;53(1):41–50. doi: 10.1016/j.jmir.2021.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Berlin A., Lovas M., Truong T., Melwani S., Liu J., Liu Z.A., et al. Implementation and outcomes of virtual care across a tertiary cancer center during COVID-19. JAMA Oncol. 2021;7(4):597. doi: 10.1001/jamaoncol.2020.6982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jimenez Y.A., Cumming S., Wang W., Stuart K., Thwaites D.I., Lewis S.J. Patient education using virtual reality increases knowledge and positive experience for breast cancer patients undergoing radiation therapy. Support Care Cancer. 2018;26(8):2879–2888. doi: 10.1007/s00520-018-4114-4. [DOI] [PubMed] [Google Scholar]
- 6.Tennant M., Anderson N., Youssef G.J., McMillan L., Thorson R., Wheeler G., et al. Effects of immersive virtual reality exposure in preparing pediatric oncology patients for radiation therapy. Tech Innov Patient Support Radiat Oncol. 2021;19:18–25. doi: 10.1016/j.tipsro.2021.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang L., Casto B., Luh J.Y., Wang S.J. Virtual reality-based education for patients undergoing radiation therapy. J Cancer Educ. 2020;37(3):694–700. doi: 10.1007/s13187-020-01870-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matsuyama R.K., Lyckholm L.J., Molisani A., Moghanaki D. The value of an educational video before consultation with a radiation oncologist. J Cancer Educ. 2013;28(2):306–313. doi: 10.1007/s13187-013-0473-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar K.A., Balazy K.E., Gutkin P.M., Jacobson C.E., Chen J.J., Karl J.J., et al. Association between patient education videos and knowledge of radiation treatment. Int J Radiat Oncol Biol Phys. 2021;109(5):1165–1175. doi: 10.1016/j.ijrobp.2020.11.069. [DOI] [PubMed] [Google Scholar]
- 10.Arden J.D., Rutka E., Ye H., Robertson J.M. A personalized patient teaching session at the time of radiation simulation may improve patient satisfaction scores. Adv Radiat Oncol. 2021;6(1):100570. doi: 10.1016/j.adro.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lam K., Lu A.D., Shi Y., Covinsky K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Internal Med. 2020;180(10):1389. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dixit N., Van Sebille Y., Crawford G.B., Ginex P.K., Ortega P.F., Chan R.J. Disparities in telehealth use: How should the supportive care community respond? Support Care Cancer. 2021;30(2):1007–1010. doi: 10.1007/s00520-021-06629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palis A.G., Quiros P.A. Adult learning principles and presentation pearls. Middle East Afr J Ophthalmol. 2014;21(2):114. doi: 10.4103/0974-9233.129748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maheswaranathan M., English J.A., Cunningham M.A., Kamen D.L. Development and implementation of a virtual Lupus Patient Education Event during the COVID-19 pandemic. Lupus Sci Med. 2021;8(1):e000493. doi: 10.1136/lupus-2021-000493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chetty L. Client satisfaction with virtual consultations during the COVID-19 pandemic at an occupational health physical therapy clinic. Workplace Health Saf. 2022;70(4):220–223. doi: 10.1177/21650799211061146. [DOI] [PubMed] [Google Scholar]
- 16.Lovo S., Harrison L., O’Connell M.E., Rotter T., Bath B. A physical therapist and nurse practitioner model of care for chronic back pain using telehealth: Diagnostic and management concordance. J Telemed Telecare. 2022 doi: 10.1177/1357633x221098904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cloutier A., Bond A., Taylor M.I., Ablett J., Teubner A., Farrer K., et al. Successful implementation of remote video consultations for patients receiving home parenteral nutrition in a national UK centre. Frontline Gastroenterol. 2020;11(4):280–284. doi: 10.1136/flgastro-2019-101257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kutner A., Love D., Markova A., Rossi A., Lee E., Nehal K., et al. Supporting virtual dermatology consultation in the setting of covid-19. J Digit Imaging. 2021;34(2):284–289. doi: 10.1007/s10278-021-00425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh S., Fletcher G.G., Yao X., Sussman J. Virtual care in patients with cancer: a systematic review. Curr Oncol. 2021;28(5):3488–3506. doi: 10.3390/curroncol28050301. [DOI] [PMC free article] [PubMed] [Google Scholar]