Highlights
-
•
US college students’ simultaneous alcohol and marijuana (SAM) use rate was rising.
-
•
There was an upward trend of SAM use among Black college students (2006–2019).
-
•
Hispanic and Asian American/Pacific Islander students’ trend remained stable.
Keywords: Simultaneous use, Alcohol, Marijuana, College students, National survey, Trends
Abstract
Objective
Simultaneous alcohol and marijuana (SAM) use exposes college students to a myriad of adverse consequences. However, there is no recent nationally representative study on SAM use among college students in the United States (US). To provide an update to the literature, the present study aimed to examine the trends, prevalence, and correlates of SAM use among US college students between 2006 and 2019, using nationally representative data.
Method
We used data from the 2006–2019 National Survey on Drug Use and Health (NSDUH) and the analytic sample was limited to the 55,669 full-time college student respondents (ages 18–22). Using logistic regression analysis, we assessed trends in SAM use prevalence and examined sociodemographic and psycho-social-behavioral correlates of SAM use.
Results
The proportion of US college students who reported SAM use increased significantly from 8.13% (2006–2010) to 8.44% (2015–2019). However, examination by race/ethnicity revealed that the increasing trend was largely driven by Black college students, whose SAM use prevalence increased significantly from 5.50% (2006–2010) to 9.30% (2015–2019), reflecting a 69.09% increase. SAM use rates did not change significantly among other racial/ethnic groups.
Conclusions
This study uncovered an upward trend and prevalence of SAM use among US college students, calling for more research and public health interventions in this area. At-risk subgroups that warrant more attention include college students who are Black, female, above the legal drinking age, have a lower than $20,000 household income, and reside in small metropolitan areas.
1. Introduction
The 2020 Monitoring the Future results show alcohol misuse among college students in the United States (US) decreased significantly (e.g., binge drinking: 24 % in 2020 compared to 32 % in 2019) (Schulenberg et al., 2021). In contrast, rates of marijuana use among college students are increasing. In 2020, the prevalence of past-year marijuana use among college students—44 percent— was the highest it has been in the past 35 years (Schulenberg et al., 2021). Importantly, previous research shows that most users of alcohol and marijuana use these simultaneously (Brière et al., 2011, Pape et al., 2009, Subbaraman and Kerr, 2015). Simultaneous alcohol and marijuana (SAM) use is often defined as using alcohol and marijuana at the same time such that their effects overlap (Patrick et al., 2018, Subbaraman and Kerr, 2015). In the present study, SAM use is specifically defined as using marijuana at the same time or within a couple of hours of one’s last alcohol use (Substance Abuse and Mental Health Services Administration, 2021). Given the opposite prevalence trends in alcohol and marijuana use, it is unclear whether SAM use is on the rise or decline among college students in the US.
SAM use may expose college students to more adverse consequences than single-substance or concurrent use (i.e., using alcohol and marijuana on separate occasions within a given period) (Patrick et al., 2018, Subbaraman and Kerr, 2015). Indeed, past research show that compared to college students who are alcohol-only, marijuana-only, and concurrent alcohol and marijuana users, SAM users experience a greater number of consequences, such as blackouts, impaired control, driving under the influence, vomiting, psychical dependence, risk behaviors, and cognitive, social, academic, and occupational consequences (Davis et al., 2021, Jackson et al., 2020, Mallett et al., 2019, Sokolovsky et al., 2020).
Despite its importance, there are few nationally representative studies on the recent trends, prevalence, and correlates of SAM use among college students in the US. Recent studies on similar topics and populations suggest that SAM use among college students might be high and rising. One recent nationally representative study examined non-disordered alcohol and marijuana co-use, which was defined as use of both alcohol and marijuana without meeting disorder criteria in the past year, and found that co-use increased between 2002 and 2018 among both college students and non-college young adults (McCabe et al., 2021). Another recent representative study focused on SAM use among young adults below the legal drinking age and found the odds of SAM use were particularly high for young adults attending college full-time (Patrick et al., 2019). Their findings also suggest that more than one in five of young adults aged 19–20 reported past-year SAM use and the prevalence remained generally stable from 2007 to 2016 (Patrick et al., 2019). Among young adult alcohol users, another study found the SAM use prevalence between 2014 and 2016 was approximately 30 % (ages 19/20 and 21/22) and 20–25 % (ages 23/24 through 29/30) (Terry-McElrath et al., 2018). Another study surveyed college students who used alcohol and marijuana in the past year in three state universities and the past-year, past-three-month, and past-month SAM use prevalence rates were 73 %, 59 %, and 50 %, respectively (White et al., 2019).
To better characterize changes in SAM use among US college students, the present study aimed to use nationally representative data from the National Survey on Drug Use and Health (NSDUH) to answer two research questions: (a) what are the trends and prevalence of SAM use among the traditionally aged college student population (i.e., 18–22; Adams and Corbett, 2010) between 2006 and 2019? (b) what are the demographic and psycho-social-behavioral correlates of SAM use in this population?
To answer the second research question, we selected several potentially salient correlates based on findings from past research. Specifically, we examined factors that have been found by past research to be correlated to SAM use among young adults/adolescents: gender (males might have higher risks than females; example OR from prior studies = 1.31–1.57), race/ethnicity (Black/AA and Hispanic Americans might have higher risks than White Americans; example ORBlack/AA = 0.42–0.44, ORHispanic = 0.59–0.66) (Patrick et al., 2019, Terry-McElrath et al., 2013), religiosity (lower religiosity might be associated with higher risks; example ORmedium religiosity = 1.56, ORlow religiosity = 1.58 compared to high religiosity) (Terry-McElrath et al., 2013), delinquency (higher delinquency-higher risk; example OR = 1.4) (Brière et al., 2011), other substance use (higher risk; example OR = 1.9–4.5) (Brière et al., 2011, Patrick et al., 2017), criminal justice involvement and substance use disorders (higher risk) (Green et al., 2016). We also explored other factors that have been commonly found to be associated with substance use among young adults/adolescents as potential correlates of SAM use, such as age, household income, psychological distress, risk propensity, substance accessibility, and risk perception (Cohn et al., 2018, Hai, 2018, Vaughn et al., 2016).
2. Method
2.1. Data and sample
This study used public-use NSDUH data collected between 2006 and 2019. NSDUH provides population estimates for an array of behavioral health variables in the general US population. It uses multistage area probability sampling methods and computer-assisted interviewing. Each independent, cross-sectional NSDUH sample is considered representative of the noninstitutionalized population ages 12 and older. This study’s analytic sample was limited to the 55,669 full-time college student respondents (ages 18–22). We chose the 2006–2019 timeframe and the age group of 18–22 mainly for practical reasons—in NSDUH, the SAM use variable was only available after 2006, 2019 was the last year of complete data available, and college enrollment status was only inquired among young adults ages 18–22. A detailed description of NSDUH procedures can be found elsewhere (Substance Abuse and Mental Health Services Administration, 2021).
2.2. Measures
2.2.1. SAM use
SAM use was assessed by asking respondents whether they used marijuana/hashish at the same time or within a couple of hours of their last alcohol use in the past 30 days (no, yes).
2.2.2. Psychosocial and behavioral correlates
We examined correlates in the domains of psychological factors, marijuana/alcohol specific factors, illegal behaviors, and substance use.
Psychological Factors. These included past-year major depressive episodes, serious psychological distress, risk propensity, and religiosity. We used a dichotomous measure of one or more major depressive episodes in the past 12 months (0 = no episode, 1 = one or more episodes), which was based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) (American Psychiatric Association, 2000). Serious psychological distress was reflected by a score of 13 or higher on the widely used K6 scale (0 = K6 score <13, 1 = score >=13) (Kessler et al., 2003).
Risk propensity and religiosity were created with methods in line with previous studies (e.g., Vaughn et al., 2016). Responses to two dichotomous items: “How often do you like to test yourself by doing something a little risky?” and “How often do you get a real kick out of doing things that are a little dangerous?” (0 = never/seldom, 1 = sometimes/always) were summed to create an ordinal scale of low-, medium-, and high-risk propensity. Religiosity, as a continuous variable, was generated by summing four dichotomous items: (a) past-year religious service attendance frequency (“During the past 12 months, how many times did you attend religious services?” 1 = 25 times or more, 0 = fewer than 25 times), (b) the importance (“Your religious beliefs are a very important part of your life.” 1 = strongly agree, 0 = strongly disagree/disagree/agree) and (c) influence of religious beliefs (“Your religious beliefs influence how you make decisions in your life.” 1 = strongly agree, 0 = strongly disagree/disagree/agree), and (d) the importance of shared religious beliefs with friends, with religiosity score ranging from 0 to 4 (“It is important that your friends share your religious beliefs.” 1 = strongly agree, 0 = strongly disagree/disagree/agree).
Marijuana/Alcohol-Specific Factors. These included (a) marijuana accessibility (1 = fairly/very easy to obtain, 0 = otherwise), (b) perceived marijuana use risk (1 = perceived great risk with smoking marijuana 1–2 times/week, 0 = otherwise), and (c) perceived alcohol use risk (1 = perceived great risk with having 5 or more alcohol drinks 1–2 times/week, 0 = otherwise).
Illegal Behaviors. These were measured in terms of one or more instances of self-reported (a) drug selling (“During the past 12 months, how many times have you sold illegal drugs?” 1 = 1or more times, 0 = 0 times), (b) theft (“During the past 12 months, how many times have you stolen or tried to steal anything worth more than $50?” 1 = 1or more times, 0 = 0 times), (c) violent attack (“During the past 12 months, how many times have you attacked someone with the intent to seriously hurt them?” 1 = 1or more times, 0 = 0 times), and driving under the influence of (d) alcohol (1 = yes, 0 = no) or (e) marijuana (1 = yes, 0 = no).
Substance Use. This was examined via four dichotomous variables, including past-month binge drinking (i.e., drinking 5 [male]/4 [female] or more drinks on the same occasion on at least one day in the past 30 days), past-year illicit drug use (other than marijuana), past-year alcohol use disorder, and marijuana use disorder (no, yes). Past-year alcohol/marijuana use disorder was measured based on the criteria in the DSM-IV (American Psychiatric Association, 2000).
2.2.3. Demographic factors
This study examined key demographic factors commonly included as control variables in NSDUH-based studies, including age (18, 19, 20, 21, 22), gender (female, male), race/ethnicity (non-Hispanic White [hereafter White], non-Hispanic Black/African American [hereafter Black/AA], Hispanic/Latino/Latinx [hereafter Hispanic], non-Hispanic Asian/Pacific Islander [AAPI], and Other [Non-Hispanic Native American/Alaska Native and Non-Hispanic more than one race]), annual household income (< $20,000, $20,000-$39,999, $40,000-$74,999, >= $75,000), and urbanicity (large metro, small metro, non-metro).
2.3. Statistical analyses
All statistical analyses were weighted to account for the NSDUH’s stratified cluster sampling design and carried out using Stata 16SE. First, we assessed trends in SAM use prevalence between 2006 and 2019, using survey-adjusted logistic regression analysis following the Center for Disease Control and Prevention’s (CDCP) guidelines for secular trend analysis (CDCP, 2020). Specifically, SAM use was specified as the dichotomous dependent variable, survey year was specified as the continuous independent variable, and demographic variables were included as control variables. Second, for the examination of the sociodemographic and psycho-social-behavioral correlates, we conducted multivariable regression analyses controlling for sociodemographic factors using the most recent NSDUH data from 2015 to 2019 (Hidalgo & Goodman, 2013).
3. Results
3.1. Trends in SAM Use, 2006–2019
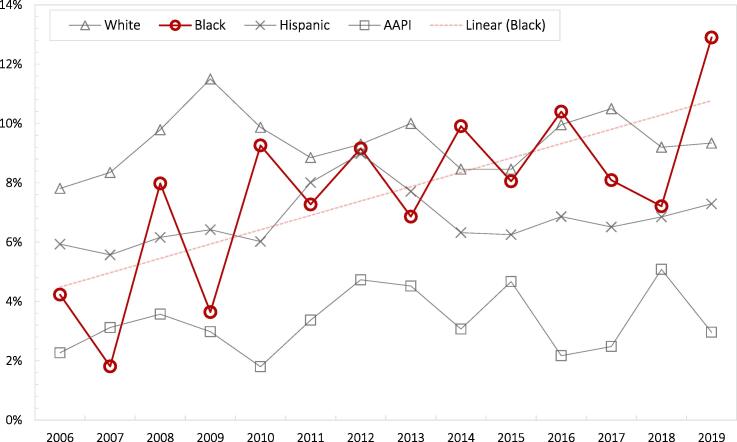
Table 1 presents the prevalence and trends of SAM use among the full sample and demographic subgroups (2006–2019). Overall, the proportion of US college students ages 18–22 who reported SAM use increased annually from 2006 to 2019 (adjusted odds ratio [AOR] = 1.01, 95 % CI = 1.00, 1.03). However, a closer look at SAM use prevalence trends by race/ethnicity revealed that the increasing trend was largely driven by Black/AA students. SAM use prevalence among Black/AA students increased from 5.50 % in 2006–2010 to 9.30 % in 2015–2019, reflecting a 69.09 % increase (the largest increase among all demographic subgroups) (yearly trend AOR = 1.07, 95 % CI = 1.04, 1.10). On the other hand, SAM use rates did not change significantly among other racial/ethnic groups. Fig. 1 presents the year-by-year trend estimates of SAM use in racial/ethnic subgroups.
Table 1.
Trends and sociodemographic correlates of simultaneous alcohol and marijuana use among college students in the United States, NSDUH 2006–2019.
| 2006–2010 |
2015–2019 |
Δ pp (% change) |
Correlates (2015–2019) | |||
|---|---|---|---|---|---|---|
| % | (95 % CI) | % | (95 % CI) | AOR (95 % CI) | ||
| Overall SAM Rate | 8.13 | (7.59–8.72) | 8.44 | (7.82–9.11) | 0.31 (3.81 %)* | – |
| Age | ||||||
| 18 | 7.13 | (6.19–8.20) | 6.49 | (5.42–7.76) | −0.64 (−8.98 %) | – |
| 19 | 7.87 | (6.90–8.96) | 8.04 | (6.83–9.45) | 0.17 (2.16 %) | 1.23 (0.94–1.60) |
| 20 | 9.04 | (7.90–10.34) | 8.25 | (7.06–9.63) | −0.79 (−8.74 %) | 1.22 (0.95–1.57) |
| 21 | 8.35 | (7.02–9.91) | 10.16 | (8.83–11.66) | 1.81 (21.68 %)* | 1.52 (1.20–1.92) |
| 22 | 8.25 | (7.01–9.67) | 9.52 | (8.12–11.13) | 1.27 (15.39 %)* | 1.43 (1.11–1.85) |
| Gender | ||||||
| Male | 10.64 | (9.84–11.50) | 9.93 | (8.92–11.03) | −0.71 (−6.67 %) | – |
| Female | 5.80 | (5.21–6.46) | 7.15 | (6.39–7.99) | 1.35 (23.28 %)* | 0.69 (0.58–0.82) |
| Race/Ethnicity | ||||||
| White | 9.48 | (8.79–10.21) | 9.49 | (8.51–10.57) | 0.01 (0.11 %) | – |
| Black/African American | 5.50 | (4.60–6.58) | 9.30 | (7.82–11.03) | 3.80 (69.09 %)* | 1.00 (0.78–1.28) |
| Hispanic | 6.04 | (4.52–8.04) | 6.78 | (5.70–8.04) | 0.74 (12.25 %) | 0.72 (0.57–0.93) |
| AAPI | 2.74 | (1.91–3.93) | 3.45 | (2.34–5.06) | 0.71 (25.91 %) | 0.32 (0.20–52) |
| Other | 11.67 | (8.34–16.09) | 13.59 | (10.58–17.28) | 1.92 (16.45 %) | 1.52 (1.11–2.08) |
| Household Income | ||||||
| <$20,000 | 9.20 | (8.24–10.25) | 10.66 | (9.56–11.88) | 1.46 (15.87 %)* | – |
| $20,000–$39,999 | 5.71 | (5.02–6.50) | 6.69 | (5.53–8.07) | 0.98 (17.16 %)* | 0.66 (0.51–0.84) |
| $40,000–$74,999 | 7.47 | (6.24–8.91) | 7.20 | (5.79–8.91) | −0.27 (−3.61 %) | 0.69 (0.52–0.91) |
| ≥$75,000 | 8.66 | (7.62–9.82) | 7.35 | (6.40–8.43) | −1.31 (−15.13 %) | 0.67 (0.54–0.81) |
| Urbanicity | ||||||
| Large Metro | 8.31 | (7.60–9.07) | 8.04 | (7.10–9.09) | −0.27 (−3.25 %) | – |
| Small Metro | 8.44 | (7.55–9.42) | 9.41 | (8.23–10.74) | 0.97 (11.49 %)* | 1.01 (0.81–1.25) |
| Non-Metro | 6.75 | (5.73–7.93) | 7.45 | (5.84–9.46) | 0.70 (10.37 %) | 0.75 (0.55–1.04) |
Notes. Survey year was included as a continuous independent variable in trend analysis. Five years were aggregated (2006–2010, 2015–2019) only in this table for clearer presentation and more representative prevalence rates. SAM = simultaneous alcohol and marijuana use. AAPI = Asian American and Pacific Islander. AOR = Adjusted odds ratios. Δ pp = percentage point change from 2006 to 2010 to 2015–2019. % change determined by dividing the pp change by the 2006–2010 value and multiplying by 100. Δ pp and % change values with * signify a significant linear trend change (p <.05). Tests of trends and correlate tests with pooled data were conducted while controlling for all sociodemographic factors, including age, gender, race/ethnicity, household income, and urbanicity. Estimates adjusted for complex sampling design.
Fig. 1.
Year-by-year rates of simultaneous alcohol and marijuana use among college students in the United States, NSDUH 2006–2019. Notes. Linear trend in simultaneous alcohol and marijuana use prevalence by race: White (adjusted odds ratio [AOR] = 1.01, 95 % confidence interval [CI] = 0.99, 1.02), Black (AOR = 1.07, 95 % CI = 1.04, 1.10), Hispanic (AOR = 1.00, 95 % CI = 0.97, 1.04), AAPI (AOR = 1.02, 95 % CI = 0.96, 1.07).
Black/AA students’ SAM use rate jumped from 7.21 % in 2018 to 12.90 % in 2019 (a 79 % increase) and became the highest prevalence rate among all racial/ethnic groups (White: 9.34 %, Hispanic: 7.29 %, and AAPI: 2.96 %). Given this jump, we performed a sensitivity analysis to test the SAM use trend between 2006 and 2018 (excluding 2019) to see if the significant trend between 2006 and 2019 was skewed by the sharp increase between 2018 and 2019. Results indicated that there was still a statistically significant upward trend in Black/AA students’ SAM use prevalence between 2006 and 2018 (AOR = 1.06, 95 % CI = 1.03, 1.09).
Significant SAM use trend increases were also observed among college students who (a) were 21 (21.68 % increase) and 22 years old (15.39 % increase), (b) identified as female (23.28 % increase), (c) had household incomes of <$20,000 (15.87 % increase) and $20,000-$39,999 (17.16 % increase), and (d) resided in small metro areas (11.49 % increase).
3.2. Correlates of SAM Use, 2015–2019
Table 1 also presents the demographic correlates of SAM use among US college students. College students who reported SAM use were more likely to be older and from the “Other racial/ethnic group”. They were less likely to be female, Hispanic, AAPI, and have higher household incomes.
Table 2 shows the psycho-social-behavioral correlates of SAM use among college students in the US. SAM use was significantly associated with major depressive episodes, serious psychological distress, higher risk propensity, easy access to marijuana, and all of the illegal and substance use behaviors: drug selling, theft, violent attack, driving under the influence of alcohol and marijuana, binge drinking, illicit drug use (other than marijuana), alcohol use disorder, and marijuana use disorder. Higher religiosity, and perceiving great risk with smoking marijuana and having 5 or more alcohol drinks 1–2 times/week were associated with lower likelihood of SAM use.
Table 2.
Correlates of simultaneous alcohol and marijuana use among college students in the United States, NSDUH 2015–2019.
| % or Mean (95 % CI) |
Logistic Regression |
|||
|---|---|---|---|---|
| No SAM use (N = 50,815) |
SAM use (N = 4,552) |
AOR | 95 % CI | |
| Psychological Factors | ||||
| Major Depressive Episode | ||||
| No | 86.97 (86.19–87.72) | 76.52 (73.34–79.42) | 1.00 | – |
| Yes | 13.03 (12.28–13.81) | 23.48 (20.58–26.66) | 2.16 | (1.78–2.61) |
| Serious Psychological Distress | ||||
| No | 76.27 (75.41–77.11) | 64.83 (61.31–68.21) | 1.00 | – |
| Yes | 23.73 (22.89–24.59) | 35.17 (31.79–38.69) | 1.84 | (1.57–2.16) |
| Risk Propensity | ||||
| Low | 63.43 (62.340–64.5) | 36.35 (32.51–40.36) | 1.00 | – |
| Medium | 17.35 (16.43–18.30) | 23.45 (20.43–26.77) | 2.29 | (1.84–2.85) |
| High | 19.23 (18.45–20.03) | 40.20 (36.90–43.60) | 3.48 | (2.97–4.08) |
| Religiosity (mean) | 1.00 (0.97–1.03) | 0.44 (0.37–0.51) | 0.65 | (0.60–0.71) |
| Marijuana/Alcohol Specific Factors | ||||
| Marijuana Fairly/Very Easy to Obtain | ||||
| No | 23.48 (22.47–24.53) | 1.75 (0.93–3.28) | 1.00 | – |
| Yes | 76.52 (75.47–77.53) | 98.25 (96.72–99.07) | 15.58 | (7.93–30.61) |
| Perceived Great Risk Smoking Marijuana 1–2 Times/Week | ||||
| No | 81.72 (80.89–82.51) | 99.14 (98.05–99.62) | 1.00 | – |
| Yes | 18.28 (17.49–19.11) | 0.87 (0.38–1.96) | 0.04 | (0.02–0.10) |
| Perceived Great Risk Having 5 + Drinks 1–2 Times/Week | ||||
| No | 63.25 (62.04–64.44) | 76.43 (73.47–79.15) | 1.00 | – |
| Yes | 36.75 (35.56–37.96) | 23.57 (20.85–26.53) | 0.57 | (0.48–0.69) |
| Illegal Behaviors (Past Year) | ||||
| Sold Drugs | ||||
| No | 97.94 (97.54–98.27) | 80.78 (78.02–83.26) | 1.00 | – |
| Yes | 2.06 (1.73–2.46) | 19.22 (16.74–21.98) | 10.43 | (7.78–13.99) |
| Theft | ||||
| No | 98.82 (98.55–99.04) | 93.89 (91.92–95.40) | 1.00 | – |
| Yes | 1.18 (0.96–1.45) | 6.11 (4.60–8.09) | 5.11 | (3.50–7.45) |
| Violent Attack | ||||
| No | 98.84 (98.56–99.07) | 95.70 (93.60–97.13) | 1.00 | – |
| Yes | 1.16 (0.93–1.44) | 4.30 (2.87–6.40) | 3.68 | (2.26–6.00) |
| Drove Under the Influence of Alcohol | ||||
| No | 92.58 (91.86–93.24) | 36.70 (32.98–40.58) | 1.00 | – |
| Yes | 7.42 (6.76–8.14) | 63.30 (59.42–67.02) | 20.71 | (17.04–25.18) |
| Drove Under the Influence of Marijuana | ||||
| No | 93.14 (92.54–93.70) | 75.91 (72.83–78.74) | 1.00 | – |
| Yes | 6.86 (6.30–7.46) | 24.09 (21.26–27.17) | 3.95 | (3.24–4.81) |
| Substance use | ||||
| Past-Month Binge Drinking | ||||
| No | 68.14 (67.00–69.26) | 21.67 (19.43–24.09) | 1.00 | – |
| Yes | 31.86 (30.74–33.00) | 78.33 (75.91–80.57) | 7.83 | (6.71–9.14) |
| Past-Year Illicit Drug Use (other than marijuana) | ||||
| No | 84.98 (83.99–85.93) | 37.79 (35.04–40.61) | 1.00 | – |
| Yes | 15.02 (14.07–16.01) | 62.21 (59.39–64.96) | 8.90 | (7.86–10.07) |
| Past-Year Alcohol Use Disorder* | ||||
| No | 91.42 (90.82–91.98) | 72.80 (69.87–75.55) | 1.00 | – |
| Yes | 8.58 (8.03–9.18) | 27.20 (24.45–30.13) | 3.62 | (3.03–4.33) |
| Past-Year Marijuana Use Disorder* | ||||
| No | 97.15 (96.62–97.61) | 65.60 (62.28–68.77) | 1.00 | – |
| Yes | 2.85 (2.39–3.39) | 34.40 (31.23–37.72) | 17.00 | (13.52–21.38) |
Notes. Data from years 2015–2019 are pooled. Adjusted Odds ratios (AOR) were estimated with sociodemographic factors adjusted for (age, gender, race/ethnicity, household income, and urbanicity). AOR and confidence intervals (95 % CI) in bold are statistically significant at p <.05. All estimates adjusted for the NSDUH’s complex sampling design. *Data from years 2016–2019 were pooled because these variables were not comparable before and after 2015.
4. Discussion
Drawing from a large national sample, the present study aimed to shed greater light on SAM use among college students in the US. We examined the trend and prevalence of SAM use in the traditionally aged college student population and by sociodemographic subgroups. Additionally, we identified several important psycho-social-behavioral correlates of SAM use. Below we highlight several key findings.
First, we found a slight but significant rising trend of SAM use among college students in the US. Importantly, a closer inspection by race/ethnicity revealed that the increasing SAM use trend was driven by Black/AA college students, while trends among AAPI, Hispanic, and White college students remained largely stable between 2006 and 2019 (Fig. 1). 2006–2019 was a period when more and more states in the US legalized marijuana use and previous research indicated medical marijuana use laws were linked to increases in marijuana use among US adolescents and young adults (Yu et al., 2020). It is unclear whether and how these laws may have differential impacts on college students from different racial/ethnic groups and further investigation is needed.
Albeit with some fluctuations, SAM use rates among Black/AA college students generally followed an upward trend over the past decade (2006–2019). Of note, there was a large increase in Black/AA college students’ SAM use prevalence between 2018 (7.21 %) and 2019 (12.90 %), indicating a nearly 80 % increase. Although in keeping with the upward trend in previous years, this sharp increase in 2019 roughly coincided with and could possibly be attributable to the beginning of the widespread attention to racism and police brutality and the concomitant rise of feelings of distress around these issues in the Black/AA community (Sterling, 2020). Given the risks and negative consequences related to SAM use, further research on SAM use among Black/AA students is warranted.
Second, we tested SAM use prevalence among socio-demographically-defined subgroups of US college students. Results suggested that about 1 in 10 college students ages 21 and 22 engaged in SAM use, which was significantly higher than the prevalence rate among college students who were 18 years old (SAM use rate 2015–2019: 6 %). This is likely related to 21 being the legal drinking age: there are more alcohol drinkers among college students ages 21 and above and/or college students who were under the legal drinking age were less likely to report SAM use even if they had engaged in this behavior. Consistent with previous findings (e.g., Arterberry et al., 2017), our results show that female college students were less likely to report SAM use. However, while SAM use prevalence remained stable for male college students, we found a significant upward trend for female college students, with a 23 % increase between 2006 and 2019 (from 5.80 % in 2006–2010 to 7.15 % in 2015–2019). One possible explanation of this finding is that male adolescents might be more susceptible to peer pressure for deviant behaviors than females and thus as marijuana use was perceived less and less “deviant” in the past decade, male adolescent/young adults’ SAM use prevalence remained stable while females’ was catching up (Mccoy et al., 2019).
With regards to racial/ethnic differences in SAM use, prior findings were mixed. For example, Patrick et al. (2019) shows Black/AA and Hispanic young adults were less likely to report SAM use compared to White young adults, while Arterberry et al. (2017) found no racial/ethnic differences among college students. Our finding is somewhere in between. We found that Hispanic and AAPI college students had significantly lower SAM use rates than White students, whereas there was no significant difference between Black/AA and White college students in recent years (2015–2019). In 2019, Black/AA college students’ SAM use prevalence reached a historic high, with approximately 13 % of Black college students reporting using marijuana at the same time or shortly after their last alcohol use. In comparison, about 9 % of White students, 7 % of Hispanic students, and 3 % of AAPI students reported SAM use in 2019. If the rising SAM use trend among Black/AA students continues, future research may soon consistently find Black/AA college students to have significantly higher SAM use rates than other racial/ethnic college subgroups. In addition, we found that the SAM use prevalence of college students in the “other” race/ethnicity was higher than that of White students. It is unclear which racial/ethnic subgroup contributed to this result and further investigation is needed.
Besides racial/ethnic differences, this study also identified disparities related to income. Compared to college students with a less than $20,000 household income, students from higher-income households were less likely to engage in SAM use. Furthermore, our trend test results suggested that the gap in SAM use rates between higher and lower income groups could be expanding. The SAM use prevalence had been increasing among the lower-income subgroups (<$20,000 and $20,000-$39,999) while remained stable among the higher-income subgroups ($40,000-$74,999 and ≥$75,000) between 2006 and 2019. In addition, while we did not find the urbanicity of college students’ residence (large metro, small metro, non-metro) to influence their SAM use, there was indication that the SAM use rates of college students residing in small metropolitan areas have followed an upward linear trend and became relatively high in recent years (9.4 %).
Third, we examined several potential psycho-social-behavioral correlates of SAM use. In line with previous research, we found that a higher likelihood of SAM use among college students in general was associated with a wide range of mental health (major depressive episodes, serious psychological distress), risk taking and illegal behaviors (higher risk propensity, easy marijuana access, drug selling, theft, violent attack, driving under the influence of alcohol or marijuana), and other substance misuse (binge drinking, illicit drug use (other than marijuana), alcohol use disorder, and marijuana use disorder). Lower odds of SAM use were linked to protective factors such as religiosity and higher marijuana and alcohol use risk perception. Preventions/interventions for college SAM use are recommended to take these factors into consideration. Additionally, it is worth pointing out that although alcohol and marijuana use disorders were linked to higher odds of SAM use, the majority of SAM users did not meet criteria for an alcohol use disorder (72.8 %) or marijuana use disorder (65.6 %). Therefore, our findings have implications for the broader college student population and not just the small subgroups who meet clinical diagnostic criteria for substance use disorders.
The present study’s findings should be interpreted in light of several limitations. First, NSDUH data offer consistent assessment of cohorts over a number of years, they are cross-sectional, precluding causal inference and the examination of within-person change. Second, all responses were drawn from self-reports, which could introduce recall and social desirability biases especially when it pertains to reporting substance use. Third, we face limitations related to measured constructs. This study relied on a binary measure of SAM use (used marijuana at the same time or a few hours after the last alcohol use or not) and thus may not capture important nuance related to the degree of SAM use. Similarly, given that college enrollment status was only inquired among young adults ages 18–22 in NSDUH, we could not examine SAM use among older college students. In addition, we could not examine some sociocultural factors unavailable in the NSDUH data but are potentially important to Black/AA and other minoritized student groups, such as racism, immigration status, racial socialization, ethnic identity, cultural values, adverse childhood experiences, and extended family support (Forster et al., 2018, Giordano et al., 2021, Neblett et al., 2010, Rich and Grey, 2011, Schwartz et al., 2011). Fourth, due to the high heterogeneity of the “other” racial/ethnic group, we were unable to make specific implications for this group. However, the high prevalence of SAM use demonstrated by the “other” racial/ethnic group is consistent with past literature that suggests a high risk for substance use problems among multiracial (Goings et al., 2017) and Native American/Alaska Native young people (Swaim & Stanley, 2018).
It is also important to note that due to measurement differences, our SAM use prevalence estimates appear smaller than those in some of the past research. For example, Patrick et al. (2019) found that almost 25 % of young adults attending four-year college full time (aged 19–20) reported SAM use (2007–2016), whereas in the present study, the SAM use rate among college students aged 19/20 was around 8–9 % (2006–2019). This discrepancy might be largely attributable to differences in the operational definitions of SAM use. While Patrick et al. (2019) measured past-year SAM use, the NSDUH SAM use measure we used focused on SAM use during/soon after the respondent’s last alcohol use and therefore may mainly capture frequent SAM users. Nevertheless, the SAM use prevalence rates this study uncovered are consistent with past studies and document surprising sharp increases, warranting more public health attention.
5. Conclusions
This study uncovered an increasing trend of SAM use among US college students, calling for more research and public health interventions in this area. Specifically, between 2006 and 2019, there was an upward trend of SAM use among Black/AA college students, while trends among college students from other racial/ethnic groups remained generally stable. In 2019, Black/AA college students replaced White students as the racial/ethnic subgroup with the highest prevalence of SAM use (13 %). Besides Black/AA college students, other subgroups that warrant more attention include college students who are female, above the legal drinking age, have a lower than $20,000 household income, and reside in small metropolitan areas.
Research Support
This research received no external financial or non-financial support.
Relationships
There are no additional relationships to disclose.
Patents and Intellectual Property
There are no patents to disclose.
Other Activities
There are no additional activities to disclose.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Audrey Hang Hai: Conceptualization, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Kate B. Carey: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. Michael G. Vaughn: Conceptualization, Methodology, Supervision, Writing – review & editing. Christina S. Lee: Conceptualization, Writing – review & editing. Cynthia Franklin: Writing – review & editing. Christopher P. Salas-Wright: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Audrey Hang Hai, Email: ahai@tulane.edu.
Kate B. Carey, Email: kate_carey@brown.edu.
Michael G. Vaughn, Email: michael.vaughn@slu.edu.
Christina S. Lee, Email: leecs@bu.edu.
Cynthia Franklin, Email: cfranklin@austin.utexas.edu.
Christopher P. Salas-Wright, Email: christopher.salas-wright@bc.edu.
References
- Adams J., Corbett A. Experiences of Traditional and Non-Traditional College Students. Perspectives. 2010;2 [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed. Te). Amer Psychiatric Pub Inc.
- Arterberry, B. J., Treloar, H., & Mccarthy, D. M. (2017). Empirical Profiles of Alcohol and Marijuana Use, Drugged Driving, and Risk Perceptions. Journal of Studies on Alcohol and Drugs, November, 889–898. [DOI] [PMC free article] [PubMed]
- Brière F.N., Fallu J.S., Descheneaux A., Janosz M. Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addictive Behaviors. 2011;36(7):785–788. doi: 10.1016/j.addbeh.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Interpretation of YRBS trend data. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm.
- Cohn A.M., Johnson A.L., Rose S.W., Pearson J.L., Villanti A.C., Stanton C. Population-Level Patterns and Mental Health and Substance Use Correlates of Alcohol, Marijuana, and Tobacco Use and Co-Use in US Young Adults and Adults: Results From the Population Assessment for Tobacco and Health. The American Journal on Addictions. 2018;27(6):491–500. doi: 10.1111/ajad.12766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C.N., Dash G.F., Miller M.B., Slutske W.S. Past year high-intensity drinking moderates the association between simultaneous alcohol and marijuana use and blackout frequency among college students. Journal of American College Health. 2021 doi: 10.1080/07448481.2021.1880415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster M., Grigsby T.J., Rogers C.J., Benjamin S.M. The relationship between family-based adverse childhood experiences and substance use behaviors among a diverse sample of college students. Addictive Behaviors. 2018;76:298–304. doi: 10.1016/J.ADDBEH.2017.08.037. [DOI] [PubMed] [Google Scholar]
- Giordano A.L., Prosek E.A., Henson R.K., Silveus S., Beijan L., Reyes A., Molina C., Agarwal S.M. Effects of Vicarious Racism Exposure via the Media on College Students of Color: Exploring Affect and Substance Use. Journal of College Counseling. 2021;24(1):4–17. doi: 10.1002/JOCC.12173. [DOI] [Google Scholar]
- Goings T.C., Salas-Wright C.P., Howard M.O., Vaughn M.G. Substance use among bi/multiracial youth in the United States: Profiles of psychosocial risk and protection. The American Journal of Drug and Alcohol Abuse. 2017;44(2):206–214. doi: 10.1080/00952990.2017.1359617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green K.M., Musci R.J., Johnson R.M., Matson P.A., Reboussin B.A., Ialongo N.S. Outcomes associated with adolescent marijuana and alcohol use among urban young adults: A prospective study. Addictive Behaviors. 2016;53:155–160. doi: 10.1016/j.addbeh.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hai A.H. Gender Differences in the Relationships among Young Adults’ Religiosity, Risk Perception, and Marijuana Use: A Moderated Mediation Model. Substance Use and Misuse. 2018;53(8):1377–1386. doi: 10.1080/10826084.2017.1409242. [DOI] [PubMed] [Google Scholar]
- Hidalgo B., Goodman M. Multivariate or multivariable regression? American Journal of Public Health. 2013;103(1):39–40. doi: 10.2105/AJPH.2012.300897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson K.M., Sokolovsky A.W., Gunn R.L., White H.R. Consequences of alcohol and marijuana use among college students: Prevalence rates and attributions to substance-specific versus simultaneous use. Psychology of Addictive Behaviors. 2020;34(2):370–381. doi: 10.1037/adb0000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Barker P.R., Colpe L.J., Epstein J.F., Gfroerer J.C., Hiripi E., Howes M.J., Normand S.L.T., Manderscheid R.W., Walters E.E., Zaslavsky A.M. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Mallett K.A., Turrisi R., Trager B.M., Sell N., Linden-Carmichael A.N. An examination of consequences among college student drinkers on occasions involving alcohol-only, marijuana-only, or combined alcohol and marijuana use. Psychology of Addictive Behaviors. 2019;33(3):331–336. doi: 10.1037/adb0000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe S.E., Arterberry B.J., Dickinson K., Evans-Polce R.J., Ford J.A., Ryan J.E., Schepis T.S. Assessment of Changes in Alcohol and Marijuana Abstinence, Co-Use, and Use Disorders Among US Young Adults From 2002 to 2018. JAMA Pediatrics. 2021;175(1):64–72. doi: 10.1001/JAMAPEDIATRICS.2020.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mccoy, S. S., Dimler, L. M., Samuels, D. v, & Natsuaki, M. N. (2019). Adolescent Susceptibility to Deviant Peer Pressure: Does Gender Matter? Adolescent Research Review, 4, 59–71. https://doi.org/10.1007/s40894-017-0071-2.
- Neblett E.W., Jr., Terzian M., Harriott V. From Racial Discrimination to Substance Use: The Buffering Effects of Racial Socialization. Child Development Perspectives. 2010;4(2):131. doi: 10.1111/J.1750-8606.2010.00131.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pape H., Rossow I., Storvoll E.E. Under double influence: Assessment of simultaneous alcohol and cannabis use in general youth populations. Drug and Alcohol Dependence. 2009;101(1–2):69–73. doi: 10.1016/j.drugalcdep.2008.11.002. [DOI] [PubMed] [Google Scholar]
- Patrick M.E., Kloska D.D., Terry-McElrath Y.M., Lee C.M., O’Malley P.M., Johnston L.D. Patterns of simultaneous and concurrent alcohol and marijuana use among adolescents. American Journal of Drug and Alcohol Abuse. 2018;44(4):441–451. doi: 10.1080/00952990.2017.1402335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M.E., Terry-McElrath Y.M., Lee C.M., Schulenberg J.E. Simultaneous alcohol and marijuana use among underage young adults in the United States. Addictive Behaviors. 2019;88:77–81. doi: 10.1016/j.addbeh.2018.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick M.E., Veliz P.T., Terry-McElrath Y.M. High-intensity and simultaneous alcohol and marijuana use among high school seniors in the United States. Substance Abuse. 2017;38(4):498–503. doi: 10.1080/08897077.2017.1356421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich J.A., Grey C.M. Pathways to Recurrent Trauma Among Young Black Men: Traumatic Stress, Substance Use, and the “Code of the Street”. American Journal of Public Health. 2011;95(5):816–824. doi: 10.2105/AJPH.2004.044560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulenberg, J. E., Patrick, M. E., Johnston, L. D., O’malley, P. M., Bachman, J. G., & Miech, R. A. (2021). Monitering the Future national survey results on drug use 1975-2020: Volume II, Collegestudents andadults ages 19–60. http://monitoringthefuture.org/pubs.html#monographs.
- Schwartz S.J., Weisskirch R.S., Zamboanga B.L., Castillo L.G., Ham L.S., Huynh Q.-L., Park I.J.K., Donovan R., Kim S.Y., Vernon M., Davis M.J., Cano M.A. Dimensions of Acculturation: Associations With Health Risk Behaviors Among College Students From Immigrant Families. Journal of Counseling Psychology. 2011;58(1):27. doi: 10.1037/A0021356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sokolovsky A.W., Gunn R.L., Micalizzi L., White H.R., Jackson K.M. Alcohol and marijuana co-use: Consequences, subjective intoxication, and the operationalization of simultaneous use. Drug and Alcohol Dependence. 2020;212 doi: 10.1016/j.drugalcdep.2020.107986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling, A. (2020). Police Killed Over 1,000 American Civilians In 2019. Forbes. https://www.forbes.com/sites/amysterling/2020/07/01/police-killed-over-1000-american-civilians-in-2019/?sh=196c6def667e.
- Subbaraman M.S., Kerr W.C. Simultaneous versus concurrent use of alcohol and cannabis in the national alcohol survey. Alcoholism: Clinical and Experimental Research. 2015;39(5):872–879. doi: 10.1111/acer.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2021). What is NSDUH?https://nsduhweb.rti.org/respweb/homepage.cfm.
- Swaim R.C., Stanley L.R. Substance Use Among American Indian Youths on Reservations Compared With a National Sample of US Adolescents. JAMA Network Open. 2018;1(1):e180382–e. doi: 10.1001/JAMANETWORKOPEN.2018.0382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath Y.M., O’Malley P.M., Johnston L.D. Simultaneous alcohol and marijuana use among US high school seniors from 1976 to 2011: Trends, reasons, and situations. Drug and Alcohol Dependence. 2013;133(1):71–79. doi: 10.1016/j.drugalcdep.2013.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath Y.M., Patrick M.E., O’Malley P.M., Johnston L.D. The end of convergence in developmental patterns of frequent marijuana use from ages 18 to 30: An analysis of cohort change from 1976–2016. Drug and Alcohol Dependence. 2018;191:203–209. doi: 10.1016/J.DRUGALCDEP.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughn M.G., Nelson E.J., Salas-Wright C.P., Qian Z., Schootman M. Racial and ethnic trends and correlates of non-medical use of prescription opioids among adolescents in the United States 2004–2013. Journal of Psychiatric Research. 2016;73:17–24. doi: 10.1016/j.jpsychires.2015.11.003. [DOI] [PubMed] [Google Scholar]
- White H.R., Kilmer J.R., Fossos-Wong N., Hayes K., Sokolovsky A.W., Jackson K.M. Simultaneous Alcohol and Marijuana Use Among College Students: Patterns, Correlates, Norms, and Consequences. Alcoholism: Clinical and Experimental Research. 2019;43(7):1545–1555. doi: 10.1111/acer.14072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu B., Chen X., Chen X., Yan H. Marijuana legalization and historical trends in marijuana use among US residents aged 12–25: Results from the 1979–2016 National Survey on drug use and health. BMC Public Health. 2020;20(1) doi: 10.1186/s12889-020-8253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]