Abstract
Background
TFMT stems are modular porous coated stems widely used in revision hip arthroplasty. Although TFMT stems are popular due to its proven advantage in the setting of severe bone deficiency, subsidence is a concern in these stem designs. We used two TFMT stems between 2013 and 2019, ARCOS(Zimmer Biomet) and Reclaim(Depuy Synthes). We reviewed our results and compared these stems.
Aim
The primary aim was a) look for early to mid-term stem survival b) radiological outcome measuring subsidence, secondary aim was to measure proximal femoral bone stock changes.
Materials and methods
Data was collected retrospectively. There were 51 patients in Arcos and 57 patients in Reclaim cohort. Both cohorts were comparable with respect to gender, side, BMI, paprosky defect, indications for surgery, ETO and stem length. The mean age group was 78.03 in Arcos and 73.75 in Reclaim.
Results
At a mean follow up of 5 years both cohorts showed excellent stem survival, 96.4% in Reclaim cohort as compared to 100% in Arcos. Subsidence was observed in both but none required a revision due to subsidence. There was a significant difference (p = 0.017) between the cohorts with mean of 2.3 mm(0–12 mm) in Arcos as compared to 4.5 mm(0–25 mm) in Reclaim. Both cohorts showed excellent restoration of proximal femoral bone stock.
Conclusion
Our data shows promising results using TFMT stems at 5 year follow up with more than 95% stem survival, minimal subsidence and good restoration of proximal femoral bone stock. The difference in subsidence between these stems may be attributed to stem geometry and difference in taper.
Keywords: TFMT stems, Hip, Arthroplasty, Revision hip arthroplasty, Stem taper
1. Introduction
There is a steady increase in the number of hip and revision hip surgeries performed in United Kingdom. The 17th NJR annual reported 1,191,253 primary and 7,791 revision hip replacements in 2019. There is an increase in the number of re revisions (N = 3,916) in 2019 as compared (N = 3365) to 2018. The risk of re-revision rate is strongly associated with time of first revision after primary, 12.69% of primary hips revised in first year needed re-revision in next 3 years as compared to 7% in primary hips that lasted for at least 5 years. Revision and re revision surgeries pose huge financial burden1. Commonest indications for revision and re revision are aseptic loosening followed by dislocation/subluxation, adverse soft tissue reaction to particulate debris, infection and pain1.
Goals of femoral revision include initial stability, lower complication rates, maintaining or restoring proximal femoral bone stock and predictable long term osseous integration. To address these issues, many techniques and implant designs have been described. Whilst monoblock cylindrical stem designs have shown good long term outcome, studies reveal high incidence of intraoperative fractures (8–30%) and long term stress shielding of proximal femur (6–16.7%).2, 3, 4 They are technically difficult to use in severe femoral defects and have high (21–37.5%) mechanical failure in paprosky type 4 defects.5
Use of Tapered fluted modular titanium (TFMT) stems, have gained popularity over the past few years with promising long term outcomes.6,7 Bohm et al. reported low rates of intra operative fractures (1.5%) with 129 tapered stems.8 Due to line to line reaming of femoral canal, distal stem insertion is safer and has reduced risk of intra operative fractures. Splines provide initial stability and resistance to torque. Modularity facilitates the intraoperative adjustment of leg length, horizontal offset, and neck version independent of distal stem. Abdel et al. reported 96% survivorship in their large series of 519 TFMT stems at a mean follow up of 10years.9 Despite excellent results, there are concerns regarding subsidence especially in periprosthetic fractures. Reported rates vary from 10% to 43%.10, 11, 12
In our unit, two different TFMT (Arcos and Reclaim) stems were used. Arcos is relatively new stem in U K, introduced for widespread use in 2012. Results for Arcos and Reclaim stem are published separately but there has been no comparison between these two stem designs to the best of our knowledge.13,14
We aimed to study and compare early to mid-term survivorship and radiological outcome of both stems. Secondary outcome measure included preservation and or restoration of proximal femoral bone stock.
2. Materials and methods
We carried out a retrospective cross-sectional cohort comparison of 108 patients operated with one of the two femoral component designs between August 2013 and November 2019. Patient demographic data were collected and compared including age at the time of revision, gender, side, body mass index (BMI), and indications for revision surgery. Data was also collected regarding paprosky grading, extended trochanteric osteotomy (ETO), cables used and stem length. Implants were chosen according to surgeon's preference and familiarity. All data were obtained using hospital episode statistics and theatre registry. Informed consent from patients and Institutional ethics board approval was attained. (Ref-200727Pawar).
2.1. Stems
TFMT stems are made of titanium which minimizes stress shielding due to lower modulus of elasticity. The tapered geometry achieves axial stability and rotational stability is achieved by cutting flutes. In Arcos stem (Zimmer biomet, Warsaw, Indiana, USA) proximal cone is porous plasma sprayed for initial scratch fit and biological fixation. Distal stem is grit blasted with 3° spline taper. In Reclaim stem (Depuy Synthes., Warsaw, Indiana, USA) both proximal cone and distal stem both are grit blasted for bony apposition. The distal stem has a 2.5° spline taper (Fig. 1).
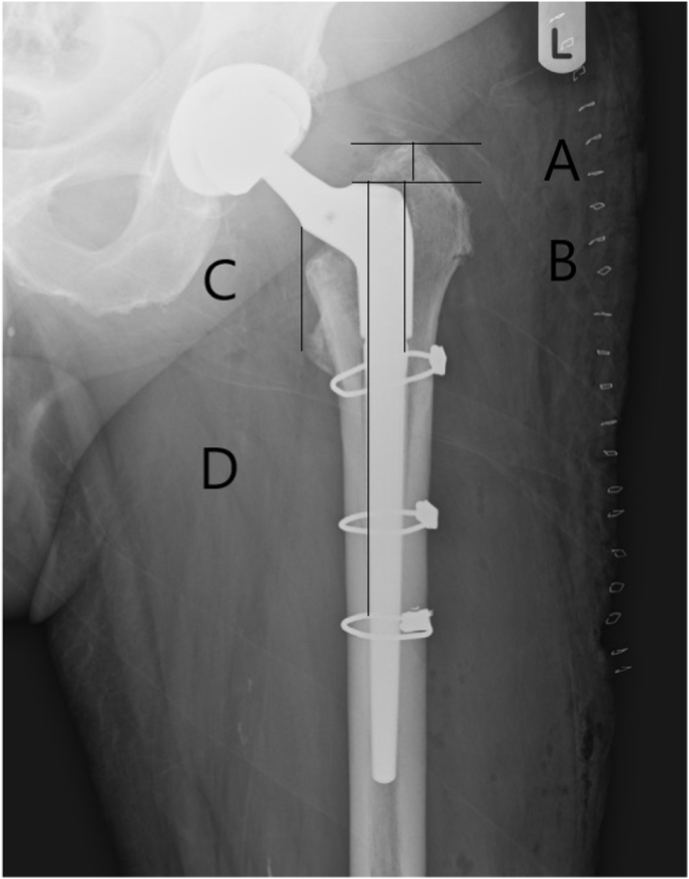
Fig. 1.
TFMT(Tapered Fluted Modular Titanium) stems.
2.2. Surgical technique
Posterolateral surgical approach was used in both cohorts. An extended trochanteric osteotomy was used to prevent bone loss where there was difficulty in retrieving the original stem. For most patients in Arcos (48 of 51) and in Reclaim (49 of 57) cohort, a prophylactic cerclage wire was placed distal to the extended trochanteric osteotomy or the periprosthetic fracture to decrease the risk of intraoperative fracture and allow insertion of largest possible stem diameter. Postoperatively, patients were allowed to toe touch weight bear for first six weeks followed by graduated weight bearing until 3 months. They were allowed full weight bearing at 3 months guided by radiological osseous integration. Patients who had an extended trochanteric osteotomy were advised not to do active abduction for the initial 6 weeks.
2.3. Radiological assessment
Preoperative evaluation for all patients included a standard AP pelvis, cross-table lateral hip, AP and lateral radiographs of the femur. All had pre-operative grading of the femoral defects using the Paprosky classification.15 Proximal femoral bone quality was graded according to classification described by Bohm et al.16 The images were calibrated with the known head size. All measurements were made using digital patient archiving and communication system (GE software). Subsidence and proximal femur bone quality was measured from initial post-operative radiograph and compared with the most recent radiographs The subsidence was measured at 4 different points on the AP radiographs and an average was obtained, modified from the technique described by Girard et al.12 Four points were measured as described. First reference (point A) was the distance from the tip of Greater trochanter to the shoulder of the proximal body. Second reference (point B) was the distance from shoulder of proximal body to the proximal cerclage cable. Third (point C) was from medial border of the proximal body to the center of lesser trochanter and the fourth (point D) was from shoulder of proximal body to distal most cable if present (Fig. 2). Measurements were taken on the last and first radiograph, the difference was calculated at all four points. The mean was taken as measure of subsidence.
Fig. 2.
Measurement points on AP x ray.
Proximal femoral bone stock was classified into a) increasing defects, b) constant defects and c) osseous restoration after comparison of first and last radiographs as described by Bohm et al. To avoid bias, 2 colleagues, not involved in the original surgery measured the subsidence and proximal bone stock.
2.4. Statistical analysis
The data was analyzed and processed by IBMS SPSS Statistics 19.0 software. Continuous variables were analyzed using independent samples t-test. Categorical variables were analyzed using the Pearson chi-square test. The correlation between two ordinal categorical variables was analyzed by Spearman's rank correlation coefficient test. P value α was set at 0.05, and P < 0.05 was considered statistically significant.
3. Results
There were 51 patients in Arcos and 57 patients in Reclaim cohort. There were 22 males, 29 females in Arcos and 22 males, 35 females in Reclaim cohort. Mean age was 78.03 (54–93) in Arcos and 73.75 (36–97) in Reclaim cohort. Mean BMI was 29.04 and 28.3 in Arcos and Reclaim cohort respectively. Most patients in Arcos (41 of 51) and Reclaim (42 of 57) cohort were either in grade IIIA or IIIB of paprosky grading for proximal femoral bone stock.
Both cohorts were comparable with respect to sex, BMI and femoral bone loss, however there was a difference in age group with relatively younger age group in Reclaim cohort. Extended trochanteric osteotomy (ETO) was performed in 12/51 and 14/57 patients in Arcos and Reclaim cohort respectively. In majority of patients, Arcos (29/51) and Reclaim (36/57), a stem length of less than or equal to 150 mm was used. Periprosthetic fracture followed by aseptic loosening were most common indications in both cohorts (Table 1).
Table 1.
Patient demographics.
| Arcos (N = 51) | Reclaim(N = 57) | P value | |
|---|---|---|---|
| Age | 78.03(54–93) | 73.75(36–97) | 0.03a |
| Sex(M/F) | 22/29 | 22/35 | 0.63a |
| Side (R/L) | 27/24 | 37/20 | 0.20b |
| BMI | 29.04(19–36) | 28.3(21–41) | 0.19a |
| ETO(Y/N) | 12/39 | 14/43 | 0.90b |
| Paporysky Defect | 0.25b | ||
| I | 1 | 1 | |
| II | 8 | 13 | |
| IIIA | 21 | 31 | |
| IIIB | 20 | 11 | |
| IV | 1 | 1 | |
| Revision indication | 0.67b | ||
| Periprosthetic fracture | 27 | 24 | |
| Aseptic loosening | 16 | 22 | |
| Infection | 4 | 7 | |
| Instability/Dislocation | 4 | 4 | |
| Stem length | 0.50b | ||
| <150 mm | 29 | 36 | |
| >150 mm | 22 | 21 |
BMI = Body Mass Index.
ETO = Extended Trochanteric Osteotomy.
= Independent t-test.
= Chi-squared test.
The mean follow up in the Arcos cohort was 34 months (12–56) as compared to 47 months (12–83) in the Reclaim cohort. Minimum follow up period in both cohorts was 12 months to identify maximal subsidence.
We found a statistical difference in the maximal subsidence between two cohorts. The mean subsidence in Arcos cohort was 2.3 (0–12 mm) as compared to 4.5 (0–25 mm) in Reclaim cohort with p value of 0.017 (Table 2).
Table 2.
Subsidence.
| Subsidence(mm) | Arcos | Reclaim | P value |
|---|---|---|---|
| Overall subsidence | 2.3(0–12) | 4.5(0–25) | 0.017 |
We further analyzed the cause of difference in subsidence. Chi-squared test did not show any statistical difference in subsidence in subgroups based on indication (periprosthetic fractureVs Other), BMI (above or below 30), stem length (above or below 150 mm), use of prophylactic cables and whether an ETO was performed or not (Table 3). One way Anova test did not show any statistical difference in subsidence between the paprosky groups in both the cohorts. (Table 4.
Table 3.
Comparison of subsidence in subgroups.
| Sub Groups |
P value | ||
|---|---|---|---|
| Indication | Periprosthetic | Others | |
| Arcos N = 51 | 27 | 24 | 0.17 |
| Reclaim N = 57 | 24 | 33 | 0.30 |
| ETO | Yes | No | |
| Arcos N = 51 | 12 | 39 | 0.48 |
| Reclaim N = 57 | 14 | 43 | 0.49 |
| BMI | <30 | >30 | |
| Arcos N = 51 | 28 | 23 | 0.32 |
| Reclaim N = 57 | 30 | 27 | 0.16 |
| Stem length | <150 | >150 | |
| Arcos N = 51 | 29 | 22 | 0.58 |
| Reclaim N = 57 | 36 | 21 | 0.6 |
Table 4.
Comparison of subsidence in paprosky defects.
| Paprosky Defect | Arcos | Reclaim |
|---|---|---|
| I | 1 | 1 |
| II | 8 | 13 |
| IIIA | 21 | 31 |
| IIIB | 20 | 11 |
| IV | 1 | 1 |
| P value | 0.14 | 0.08 |
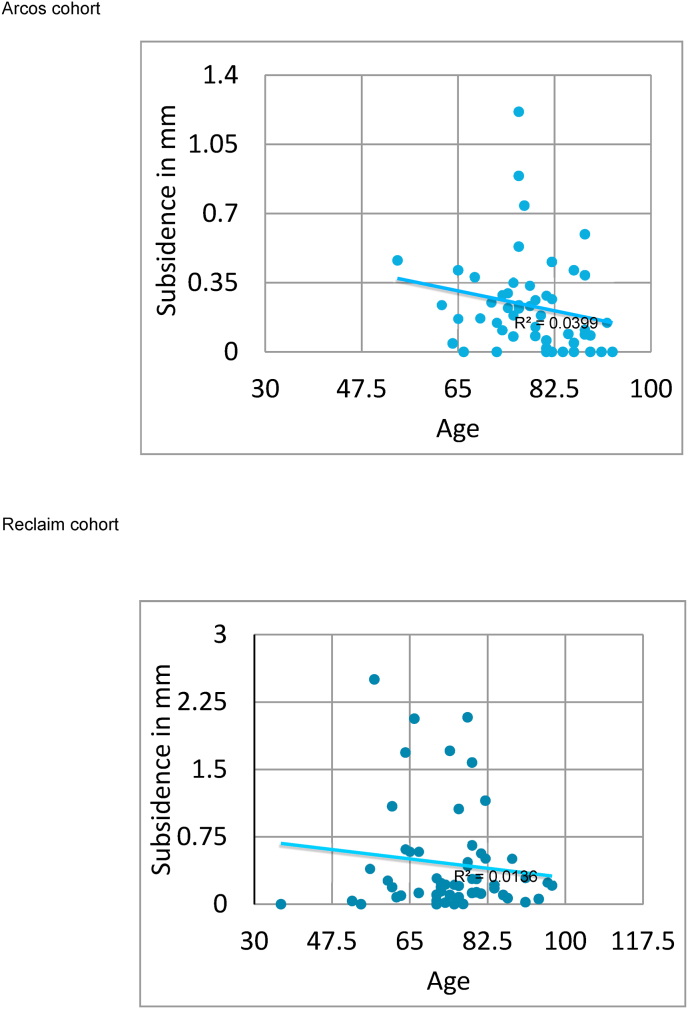
Linear regression analysis for association between the age and subsidence showed no correlation with R2 of 0.03 in Arcos group and .01 in Reclaim group (Fig. 3).
Fig. 3.
Correlation chart for age and subsidence.
We found no statistical difference (p = 0.11) in restoration of proximal bone stock, 43/51 (84%) in Arcos cohort and 40/57(70%) in Reclaim cohort had excellent restoration of bone stock at final follow up (Table 5).
Table 6.
Complications.
| Post op complication | Arcos | Reclaim |
|---|---|---|
| Dislocation | 3 | 3 |
| Infection | 1 | 2 |
| ETO Non union | 1 | 0 |
| Foot drop | 0 | 1 |
| Abductor insufficiency | 1 | 0 |
| Fatigue failure of stem | 0 | 1 |
Table 5.
Proximal femoral bone stock changes according to Bohm and Bischel et al.
| Proximal femoral bone stock | Arcos | Reclaim | P value |
|---|---|---|---|
| 0.11 | |||
| Increasing defects | 3 | 11 | |
| Constant defects | 5 | 6 | |
| Osseous restoration | 43 | 40 |
At final follow up none of Arcos stems were revised for any reason in with 100% survival and 2 stems had to be revised in Reclaim cohort with survivorship of 96.4%. There was no significant difference with p value of 0.18 on log-rank test.
4. Complications
3 patients (5.8%) in the Arcos cohort had recurrent dislocations. 2 cases settled with closed reduction and bracing and one had to be revised to a dual mobility. One of the reduced hips had subsidence greater than 5 mm. 1 (2%) patient developed superficial infection which needed washout. There was 1 (2%) patient with abductor weakness following procedure and 1 (2%) with non-union at ETO site, neither of them required surgical intervention.
3 patients (5%) in the Reclaim cohort had recurrent dislocations. 1 settled with closed reduction and 2 needed revision to dual mobility articulation. All of these stems had subsided more than 5 mm. There was 1 superficial infection which resolved with wash out and long term antibiotics and 1 deep infection which needed excision arthroplasty after multiple failed wash outs. 1 (1.6%) patient was found to have foot drop following surgery, which resolved in 6 months. 1 patient developed fatigue failure of junction between cone and distal stem at 8 months, which was revised to a longer Reclaim stem and excluded from further study.
5. Discussion
Failure of the femoral component after a primary or revision THA is usually associated with significant femoral bone loss. Depending on the proximal femoral bone quantity and quality, femoral stem revision can be challenging. Choice of components is vital owing to bone loss and distorted anatomy. Implants are designed and engineered so as to maximize primary host bone contact fixation, early secondary biological fixation and long term implant survival without significant subsidence. Subsidence of stem is one of the important causes of instability and subsequent revision of prosthesis in hip arthroplasty. Many authors report, up to 5% of stems subside more than 10 mm in revision surgeries.17,18
TFMT stem designs have shown promising early and mid-term survivorship.19,20 Our study looked at results of two TFMT stems, Arcos and Reclaim.
Factors that influence subsidence of uncemented stems include age, gender, BMI, postoperative weight bearing protocol, preoperative bone loss, periprosthetic fractures, stem length, ETO and stem designs.21, 22, 23
In our study we observed subsidence in both the cohorts. 5/51(10%) patients in Arcos cohort and 17/57 (30%) patients in Reclaim cohort had subsidence more than 5 mm. We could not explain the differences in subsidence to any variables other than stem geometry. We hypothesized that this could be due to the difference in the degree of taper. Pierson et al. compared stems two spline configurations (Narrow 0.4–0.5 mm and Broad 0.9–1.0 mm) with five taper angle groups per spline configuration (2.5°, 3.0°, 3.5°, 4.0°, 5.0°). They measured resistance to stem subsidence and axial stability and concluded that higher degrees of taper angle and broad spline geometry were superior.24 Haddad et al. reported good osseous integration and low subsidence (4.5%) using a 3° tapered femoral stem at 4 years in 23 patients with type III paprosky defects.25
Bohm et al. suggested that subsidence in femoral revision correlated with the extent of preoperative femoral bone loss and degree of osteoporosis15. In our study we found no difference in the subsidence between different paprosky grades in both cohorts. Koster G et al. and Park MS et al. also reported no correlation between stem subsidence and the extent of preoperative bone loss.11,17 Tangsataporn et al. reported increased subsidence of 14.1% with increased body weight more than 80 kg and with short stems.26 In our study there was no correlation to BMI or stem length used in both cohorts.
Munro et al. observed subsidence in 24% of patients who had revision for periprosthetic femur fractures, of which only one required revision.27 In their study by Neumann et al., 2 out of 53 revisions for periprosthetic fractures had to be re revised for pain and instability following subsidence greater than 5 mm.28 In our study no stems were revised for subsidence and also there was no difference in subsidence based on indication for revision.
Park et al. reported stem subsidence of more than 5 mm in non ETO group (4/30 hips, 13%) as compared to ETO group (0/32 hips, 0%) (P = 0.049).20 Our results showed no significant difference in both cohorts.
We acknowledge the limitation of our study, this is a non-randomized retrospective design. Radiographic methods to measure subsidence are not as accurate as radio isometric analysis. Strengths of our study is that it is from a single center and is the only study comparing two TFMT design.
6. Conclusion
Our study shows excellent mid-term survivorship and restoration of proximal femoral bone stock with both TFMT stems. Although Subsidence was observed in both cohorts, no stems have been revised for subsidence. Comparison between the stems revealed a statistically significant increased subsidence in Reclaim cohort which could not be attributed to any other variables apart from stem geometry.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Institutional ethical committee approval
Informed consent from patients and Institutional ethics board approval was attained. (Ref-200727Pawar).
Author contribution
Dr Rajesh Pawar: Writing - Original Draft, Data Curation, Formal analysis.
Dr Rye Yap: Data Curation, Formal analysis.
Miss Jody Blow: Data Curation, Resources.
Dr Mohanrao Garabadi: Data Curation, Resources.
Mr Mark Rowsell: Supervision.
Mr Hasnat Minhas: Supervision.
Mr Prasad Antapur: Conceptualization, Writing - Review & Editing, Supervision.
Declaration of competing interest
None.
Acknowledgement
None.
References
- 1.Ben-Shlomo Y., Blom A., Boulton C., et al. London: National Joint Registry; 2019. The National Joint Registry 16th Annual Report [Internet] Dec. PMID: 32744812. [PubMed] [Google Scholar]
- 2.Weeden S.H., Paprosky W. Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty. 2002;17(4 Suppl 1):134–137. doi: 10.1054/arth.2002.32461. Jun. [DOI] [PubMed] [Google Scholar]
- 3.Meek R.M., Garbuz D.S., Masri B.A., Greidanus N.V., Duncan C.P. Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am. 2004;86(3):480–485. doi: 10.2106/00004623-200403000-00004. Mar. [DOI] [PubMed] [Google Scholar]
- 4.Moreland J.R., Bernstein M.L. Femoral revision hip arthroplasty with uncemented, porous-coated stems. Clin Orthop Relat Res. 1995;(319):141–150. Oct. [PubMed] [Google Scholar]
- 5.Sporer S.M., Paprosky W.G. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. Dec. [DOI] [PubMed] [Google Scholar]
- 6.Munro J.T., Garbuz D.S., Masri B.A., Duncan C.P. Role and results of tapered fluted modular titanium stems in revision total hip arthroplasty. J Bone Joint Surg Br. 2012;94(11 Suppl A):58–60. doi: 10.1302/0301-620X.94B11.30612. Nov. [DOI] [PubMed] [Google Scholar]
- 7.Amanatullah D.F., Howard J.L., Siman H., Trousdale R.T., Mabry T.M., Berry D.J. Revision total hip arthroplasty in patients with extensive proximal femoral bone loss using a fluted tapered modular femoral component. Bone Joint Lett J. 2015;97-B(3):312–317. doi: 10.1302/0301-620X.97B3.34684. Mar. [DOI] [PubMed] [Google Scholar]
- 8.Böhm P., Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;(420):148–159. Mar. [PubMed] [Google Scholar]
- 9.Abdel M.P., Cottino U., Larson D.R., Hanssen A.D., Lewallen D.G., Berry D.J. Modular fluted tapered stems in aseptic revision total hip arthroplasty. J Bone Joint Surg Am. 2017;99(10):873–881. doi: 10.2106/JBJS.16.00423. May 17. [DOI] [PubMed] [Google Scholar]
- 10.Parry J.A., Hernandez N.M., Berry D.J., Abdel M.P., Yuan B.J. Risk factors for subsidence of modular fluted tapered stems used during revision total hip arthroplasty for periprosthetic hip fractures. J Arthroplasty. 2018;33(9):2967–2970. doi: 10.1016/j.arth.2018.05.006. Sep. [DOI] [PubMed] [Google Scholar]
- 11.Köster G., Walde T.A., Willert H.G. Five- to 10-year results using a noncemented modular revision stem without bone grafting. J Arthroplasty. 2008;23(7):964–970. doi: 10.1016/j.arth.2007.08.024. Oct. [DOI] [PubMed] [Google Scholar]
- 12.Girard J., Roche O., Wavreille G., Canovas F., Le Béguec P. Stem subsidence after total hip revision: 183 cases at 5.9 years follow-up. Orthop Traumatol Surg Res. 2011;97(2):121–126. doi: 10.1016/j.otsr.2010.10.006. Apr. [DOI] [PubMed] [Google Scholar]
- 13.Dyreborg K., Petersen M.M., Balle S.S., Kjersgaard A.G., Solgaard S. Observational study of a new modular femoral revision system. World J Orthoped. 2020;11(3):167–176. doi: 10.5312/wjo.v11.i3.167. 2020 Mar 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hancock D.S., Sharplin P.K., Larsen P.D., Phillips F.T. Early radiological and functional outcomes for a cementless press-fit design modular femoral stem revision system. Hip Int. 2019;29(1):35–40. doi: 10.1177/1120700018760277. Jan. [DOI] [PubMed] [Google Scholar]
- 15.Paprosky WG, Lawrence J, Cameron H. Femoral defect classification, (1990) Clinical application. Orthop Rev, 19(suppl 9):9-17.
- 16.Bohm Böhm P., Bischel O. Femoral revision with the Wagner SL revision stem: evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am. 2001;83(7):1023–1031. Jul. [PubMed] [Google Scholar]
- 17.Park M.S., Lee J.H., Park J.H., Ham D.H., Rhee Y.K. A distal fluted, proximal modular femoral prosthesis in revision hip arthroplasty. J Arthroplasty. 2010;25(6):932–938. doi: 10.1016/j.arth.2009.06.031. Sep. [DOI] [PubMed] [Google Scholar]
- 18.Rodriguez J.A., Deshmukh A.J., Klauser W.U., Rasquinha V.J., Lubinus P., Ranawat C.S. Patterns of osseointegration and remodeling in femoral revision with bone loss using modular, tapered, fluted, titanium stems. J Arthroplasty. 2011;26(8):1409–1417.e1. doi: 10.1016/j.arth.2011.06.021. Dec. [DOI] [PubMed] [Google Scholar]
- 19.McInnis D.P., Horne G., Devane P.A. Femoral revision with a fluted, tapered, modular stem seventy patients followed for a mean of 3.9 years. J Arthroplasty. 2006;21(3):372–380. doi: 10.1016/j.arth.2005.08.022. Apr. [DOI] [PubMed] [Google Scholar]
- 20.Park Y.S., Moon Y.W., Lim S.J. Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty. 2007;22(7):993–999. doi: 10.1016/j.arth.2007.03.017. Oct. [DOI] [PubMed] [Google Scholar]
- 21.Murphy S.B., Rodriguez J. Revision total hip arthroplasty with proximal bone loss. J Arthroplasty. 2004;19(4 Suppl 1):115–119. doi: 10.1016/j.arth.2004.04.001. Jun. [DOI] [PubMed] [Google Scholar]
- 22.Palumbo B.T., Morrison K.L., Baumgarten A.S., Stein M.I., Haidukewych G.J., Bernasek T.L. Results of revision total hip arthroplasty with modular, titanium-tapered femoral stems in severe proximal metaphyseal and diaphyseal bone loss. J Arthroplasty. 2013;28(4):690–694. doi: 10.1016/j.arth.2012.08.019. Apr. [DOI] [PubMed] [Google Scholar]
- 23.Bottner F., Zawadsky M., Su E.P., et al. Implant migration after early weightbearing in cementless hip replacement. Clin Orthop Relat Res. 2005;436:132–137. doi: 10.1097/01.blo.0000160380.15429.fb. Jul. [DOI] [PubMed] [Google Scholar]
- 24.Pierson J.L., Small S.R., Rodriguez J.A., Kang M.N., Glassman A.H. The effect of taper angle and spline geometry on the initial stability of tapered, splined modular titanium stems. J Arthroplasty. 2015;30(7):1254–1259. doi: 10.1016/j.arth.2015.01.054. Jul. [DOI] [PubMed] [Google Scholar]
- 25.Ngu A.W.T., Rowan F.E., Carli A.V., Haddad F.S. Single 3° tapered fluted femoral stems demonstrate low subsidence at mid-term follow-up in severe bony deficiency. Ann Transl Med. 2019;7(23):725. doi: 10.21037/atm.2019.12.19. Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tangsataporn S., Safir O.A., Vincent A.D., Abdelbary H., Gross A.E., Kuzyk P.R. Risk factors for subsidence of a modular tapered femoral stem used for revision total hip arthroplasty. J Arthroplasty. 2015;30(6):1030–1034. doi: 10.1016/j.arth.2015.01.009. Jun. [DOI] [PubMed] [Google Scholar]
- 27.Munro J.T., Garbuz D.S., Masri B.A., Duncan C.P. Tapered fluted titanium stems in the management of Vancouver B2 and B3 periprosthetic femoral fractures. Clin Orthop Relat Res. 2014;472(2):590–598. doi: 10.1007/s11999-013-3087-3. Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neumann D., Thaler C., Dorn U. Management of Vancouver B2 and B3 femoral periprosthetic fractures using a modular cementless stem without allografting. Int Orthop. 2012;36:1045–1050. doi: 10.1007/s00264-011-1371-y. [DOI] [PMC free article] [PubMed] [Google Scholar]