Abstract
Background:
The literature comparing open and arthroscopic repair of subscapularis tendon (ST) tears is insufficient.
Purpose:
To compare the clinical results of open versus arthroscopic repair of ST tears with or without concomitant supraspinatus tears.
Study Design:
Retrospective cohort study.
Methods:
We retrospectively evaluated 70 patients treated for isolated ST tears and ST tears with concomitant supraspinatus tendon tears at a single center between 2011 and 2019. Patients were divided into 2 groups: those who underwent open ST repairs (group O) and those with an arthroscopic ST repair (group A). Range of motion (ROM), liftoff and belly-press tests, and Constant-Murley (CM) scores were included in the pre- and postoperative functional evaluations. The minimal clinically important difference was calculated using the anchor-based method for changes in CM score. Tear size was evaluated according to the Lafosse classification. The categorical data were assessed using the Pearson chi-square, Fisher exact, and Fisher-Freeman-Halton tests. The parametric and nonparametric data were evaluated using the Student t test and Mann-Whitney U test, respectively. The dependent groups (for nonnormally distributed data) were evaluated using the Wilcoxon signed rank test.
Results:
Group O included 34 patients, and group A included 36 patients. The mean age was 62.9 years, and the mean follow-up period was 66.7 months. Even though group O exhibited a significantly better preoperative CM score (53.7 ± 4.6 vs 48.9 ± 6.8 [mean ± SD]; P = .001), group A had a significantly better postoperative CM score (88.7 ± 4.7 vs 84.6 ± 2.9; P < .001). Our measurements revealed a minimal clinically important difference of 11.5 points for the CM score. Group A had significantly greater postoperative ROM in abduction (153° vs 143.9°; P = .005) and forward elevation (159.1° vs 149.7°; P = .005), as well as significantly greater postoperative improvement in positive belly-press test results (P = .028). Complications occurred in 4 patients in group O and in 1 patient in group A.
Conclusion:
The study findings indicated that arthroscopic ST repair was more advantageous than open repair in terms of ROM and functional outcomes.
Keywords: subscapularis, rotator cuff tear, arthroscopic repair, open repair, shoulder
Tears of the subscapularis tendon (ST) were first described by Smith 39 in a cadaveric study in 1834. Hauser 22 carried out the first study on ST repair in 1954. Although ST injuries have been described historically, studies on the repair of this tendon are relatively few, given the presence of critical neurovascular structures in its vicinity and the lower chance of injury to it than the other tendons forming the rotator cuff. 34 In the past, it was thought that ST tears were not as common as those of the other tendons that make up the rotator cuff. 14,16,40 However, today it is known that ST tears are at least as common as infraspinatus tears. 1 ST tears may cause arthrosis in the glenohumeral joint attributed to pain as well as loss of internal rotation strength and anterior stability in the long term. 34
During arthroscopic and open repair of ST tears, the axillary artery and nerve, musculocutaneous nerve, and lateral cord of the brachial plexus are at risk because of the location of the tendon. 5 Three unique aspects of ST tears can make repair particularly difficult. First, a chronic ST tear tends to retract to a much greater extent than the rest of the rotator cuff, making the tendon extremely complicated to repair. Second, mobilizing the retracted tendon can be quite challenging given its proximity to the aforementioned anatomic structures. Third, arthroscopic vision and repair in the tightly constricted subcoracoid space can be tricky. 5
Although some authors have stated that open repair is the standard, 3 successful arthroscopic repair has been reported in recent years and has become the preferred method. 1,6,29,35 However, the literature comparing open and arthroscopic repair of ST tears is insufficient.
This study aimed to compare the clinical results of open and arthroscopic repair of ST tears. Our hypothesis was that the range of motion (ROM) and functional scores of patients who underwent arthroscopic repair would be better than those of patients who underwent open repair.
Methods
We obtained institutional review board approval before starting the study. Informed consent was obtained from all the participants included in the study. This retrospective study evaluated patients who underwent rotator cuff tear repair between 2011 and 2019. The study included patients aged 35 to 75 years with isolated ST tears and concomitant supraspinatus tendon tears. The study excluded patients with massive rotator cuff tears with >5 cm of retraction of the supraspinatus and infraspinatus muscles, pseudoparalysis, previous shoulder surgery, concomitant Bankart or superior labrum anterior-posterior lesion, history of shoulder infection, arthrosis of the glenohumeral joint, and follow-up <1 year.
Patients who met the study inclusion criteria were divided into 2 groups: patients who underwent open repair (group O) and those who underwent arthroscopic repair (group A). Functional evaluations of the patients with a follow-up period >1 year were assessed in the final examination.
Surgical Procedure and Rehabilitation
The operations were performed by 3 surgeons with a minimum of 5 years of experience in shoulder arthroscopy and rotator cuff repairs. In both surgical methods, the patients were prepared in the beach-chair position. Open repair was performed using a deltopectoral incision, whereas arthroscopic repair was conducted using the posterior, lateral, anterosuperior, and anteroinferior portals. Depending on the experience and preference of the operating surgeon, metal and bioabsorbable anchors were used. Single-row repair was performed in all patients who underwent open or arthroscopic ST repair. Supraspinatus repair was applied as a single or double row according to the preference of different surgeons. After examination of the biceps tendon, tenodesis or tenotomy was performed considering the level of tendinopathy and the patient’s age, daily activity level, and postoperative expectation.
In the repair of the ST according to the single-row repair technique, 2 anchors were used in patients with complete detachment, and 1 anchor was used in patients with partial tears (those involving one-third and two-thirds of the tendon). In the repair of the supraspinatus tendon, at least 2 anchors were used in a single- or double-row repair technique.
The patients who underwent arthroscopic repair were discharged the day after surgery. For our patients who underwent open surgery, the drain placed in the incision area was removed on postoperative day 1, and they were discharged on postoperative day 2 after verification that no hematoma had formed in the surgical area. Postoperatively, all patients wore a shoulder arm sling at 30° of abduction for the first 6 weeks. Active ROM and strengthening exercises were initiated by a physical therapist at our hospital. Wrist and elbow movements were initiated in patients whose tenodesis was not performed on the long head of the biceps muscle. Pendulum movement commenced in postoperative week 4, and active ROM exercises were started at the end of postoperative week 6. Strengthening exercises were initiated in postoperative week 12.
Outcome Measures
The preoperative data of the patients were retrieved from their medical records (mechanism of injury, history of physical therapy, time from onset of symptoms or trauma to surgery). The patients were evaluated by an independent investigator who was not part of the surgical team. ROM, liftoff and belly-press tests, and Constant-Murley (CM) scores were used for the pre- and postoperative functional evaluations. 8,17,18 For the belly-press test, the patient is asked to press the palm of the hand against the abdomen, through shoulder internal rotation. The test result is positive for subscapularis muscle dysfunction if the patient compensates the movement using wrist flexion, shoulder adduction, and shoulder extension. This unconscious compensatory movement would result in the elbow’s dropping behind the trunk. The liftoff test evaluates whether the patient’s hand can be actively lifted from the back. If the patient is unable to actively separate the hand from the back, the liftoff test result is considered positive and is indicative of subscapularis rupture or dysfunction.
The CM score was the primary outcome measure. 2,13 We calculated minimal clinically important difference (MCID) values for the pre- to postoperative improvement in CM score. Two methods can be used in the calculation of MCID: anchor based and distribution based. In our study, we used the anchor-based calculation method, which was performed by asking patients a simple 2-stage question: Is the shoulder better or worse after the operation? We used the responses to this question as an indicator of patient satisfaction and as an anchor to calculate the MCID for the CM score.
The receiver operating characteristic (ROC) curve approach was used to estimate the MCID using the value with the highest Youden index to allow the best discrimination between the satisfied and dissatisfied patients. 28,41 It is possible to use an ROC curve to identify the optimal cutoff point for the change in the CM score by determining the optimum relationship between sensitivity and specificity (ie, where the ROC curve is as close as possible to the left upper corner). This point most accurately corresponds to the change identified as the MCID. 20
The tears were graded according to the method defined by Lafosse et al, 29 based on the preoperative magnetic resonance imaging and intraoperative data. 32 Moreover, concomitant biceps pathologies and applied treatment methods were obtained from the surgical data. According to the Lafosse classification, type 1 indicates a partial tear in the upper one-third of the tendon; type 2, a full-thickness tear in the upper one-third of the tendon; type 3, a full-thickness tear in the upper two-thirds of the tendon; type 4, a complete tear in which the entire tendon is not retracted medially to the medial glenohumeral joint; and type 5, a complete tear with the tendon retracted medially from glenoid to coracoid.
Statistical Analysis
The data were analyzed using SPSS Statistics Software (Version 23.0; IBM Corp). The distribution of the data was evaluated using the Kolmogorov-Smirnov test. The categorical data were assessed using the Pearson chi-square, Fisher exact, and Fisher-Freeman-Halton tests. The parametric and nonparametric data were evaluated using the Student t test and Mann-Whitney U test, respectively. For nonnormally distributed data, the dependent groups were evaluated using the Wilcoxon signed rank test. P < .05 was considered significant for all analyses.
A prestudy power analysis based on previous data determined that a sample size of 31 patients would be adequate to reach the desired power >0.8.
Results
We identified 82 patients who underwent ST repairs during the study period. Twelve patients did not want to participate; thus, 70 patients were included in this study. The mean age of the patients was 62.9 ± 10.1 years (range, 35-75 years), and the mean follow-up period was 66.7 months (range, 12-103 months). Group O comprised 34 patients (17 female and 17 male), and group A comprised 36 patients (19 female and 17 male). Table 1 compares the patient and tear characteristics between the groups. We found that 23 patients in group O and 28 in group A had a history of trauma before symptoms appeared. Eighteen (25.7%) patients sustained a high-velocity trauma, and 33 (47.1%) sustained a fall from standing height. The remaining 19 (27.1%) reported shoulder problems unrelated to any previous injury. The mean interval from trauma to surgery was 12.6 ± 12.5 months (range, 1-48 months) in group O and 9 ± 11 months (range, 1-51 months) in group A (P = .067). It was noted that 45 patients received physical therapy before surgery. There were no records of preoperative injections.
Table 1.
Patient and Tear Characteristics of the Study Groups a
| Open Repair (n = 34) | Arthroscopic Repair (n = 36) | P Value | |
|---|---|---|---|
| Age, y | 60.6 ± 11 | 65.1 ± 8.7 | .060 |
| Sex, female:male | 17:17 | 19:17 | .816 |
| Follow-up period, mo | 61.7 ± 31.4 | 71.3 ± 26.0 | .317 |
| Side affected, right:left | 31:3 | 23:13 | .007 |
| Tendon tears, isolated:combined | 7:27 | 1:35 | .026 |
| History of trauma, yes:no | 23:13 | 28:8 | .134 |
| History of physiotherapy | 22 | 23 | .565 |
| Duration of symptoms, mo | 12.6 ± 12.5 | 9 ± 11 | .067 |
| Tear size, Lafosse classification | .269 | ||
| Type 1 | 0 | 0 | |
| Type 2 | 20 | 14 | |
| Type 3 | 11 | 16 | |
| Type 4 | 3 | 6 | |
| Type 5 | 0 | 0 |
a Data are presented as mean ± SD or No. of patients. Bold P values indicate statistically significant difference between groups (P < .05).
When ST repair was performed, bioabsorbable anchors were used in 42 patients, whereas metal anchors were used in 28 patients. Eight patients had isolated ST tears (7 in group O and 1 in group A), while 62 presented with concomitant supraspinatus tendon tears. Analysis of the detachment sizes of the ST ruptures is given in Table 1. No significant difference was observed in the preoperative Lafosse classification between the groups (P = .269).
Surgery for the biceps tendon was performed in 43 patients (tenotomy, 14 patients; tenodesis, 29 patients). During surgery, the biceps tendon was intact in 21 patients and ruptured in 6 patients (Table 2).
Table 2.
Biceps Tendon Procedures Chart a
| Open Repair (n = 34) | Arthroscopic Repair (n = 36) | |
|---|---|---|
| Tenodesis | 13 (38.3) | 16 (45.5) |
| Tenotomy | 5 (14.8) | 9 (25) |
| Ruptured | 4 (11.7) | 2 (5.5) |
| Intact | 12 (35.2) | 9 (25) |
a Data are presented as No. (%) of patients.
A significant difference was noted in the pre- and postoperative CM scores between the groups. Even though group O exhibited a significantly better preoperative CM score (53.7 ± 4.6 vs 48.9 ± 6.8; P = .001), group A had a significantly better postoperative CM score (88.7 ± 4.7 vs 84.6 ± 2.9; P < .001) (Table 3). The mean change in CM score of the patients who were satisfied with the surgery was 11.5 points (95% CI, 0.630-0.938Confidence interval of the area under the curve). In ROC analysis, the optimal MCID for the change in the CM score was 4 points (area under the curve, 0.78) (Figure 1).
Table 3.
Comparison of Constant-Murley Scores Between Groups a
| Score | Overall | Open Repair | Arthroscopic Repair | P Value |
|---|---|---|---|---|
| Preoperative | 51.28 ± 6.3 | 53.7 ± 4.6 | 48.9 ± 6.8 | .001 |
| Postoperative | 86.74 ± 4.4 | 84.6 ± 2.9 | 88.7 ± 4.7 | <.001 |
a Data are presented as mean ± SD. Bold P values indicate statistically significant difference between groups (P < .05).
Figure 1.
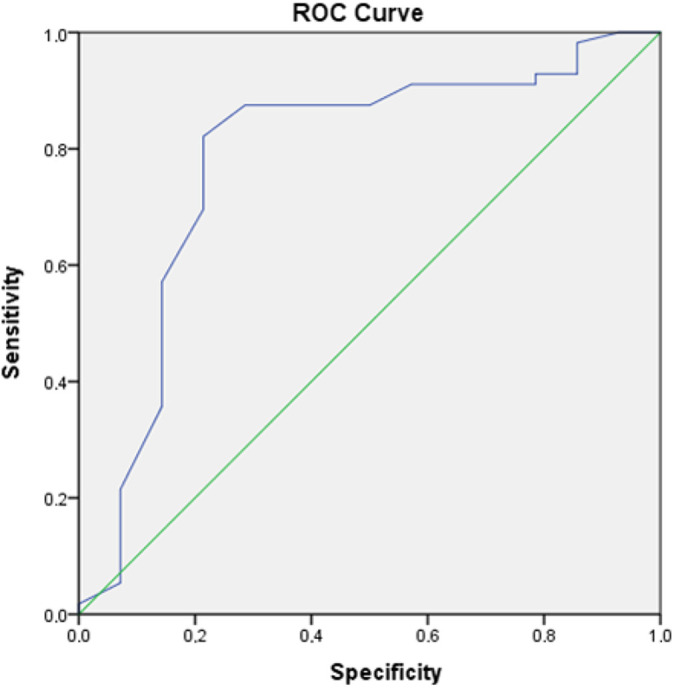
Receiver operating characteristic (ROC) analysis. The optimal minimal clinically important difference for the change in the Constant-Murley score was 4 points (ie, where the ROC curve is as close as possible to the left upper corner). Area under the ROC curve, 0.78. Blue line, satisfaction rate after repair; green line, random classifier.
When ROM was compared, group A had significantly better results for abduction (P = .005) and forward elevation (P = .005) (Table 4). The results of the postoperative belly-press test were also statistically significantly better for group A (P = .028) (Table 5).
Table 4.
Comparison of Range of Motion Between Groups a
| Open Repair | Arthroscopic Repair | P Value | |
|---|---|---|---|
| Abduction, deg | |||
| Preoperative | 95.5 ± 16.1 | 94.4 ± 17.7 | .780 |
| Postoperative | 143.9 ± 15.9 | 153 ± 20.5 | .005 |
| Forward elevation, deg | |||
| Preoperative | 127.6 ± 27.5 | 131.1 ± 20.7 | .552 |
| Postoperative | 149.7 ± 16.2 | 159.1 ± 18.2 | .005 |
| External rotation, deg | |||
| Preoperative | 28 ± 5.5 | 29 ± 7.3 | .549 |
| Postoperative | 39.8 ± 5.9 | 41.1 ± 8.2 | .518 |
| Internal rotation, level of spine | |||
| Preoperative | L3 | L4 | .722 |
| Postoperative | L2 | L2 | .340 |
a Data are presented as mean ± SD. Bold P values indicate statistically significant difference between groups (P < .05).
Table 5.
Patients’ Change With Positive Liftoff and Belly-Press Test Results Before and After the Operation a
| Open Repair | Arthroscopic Repair | ||||||
|---|---|---|---|---|---|---|---|
| Positive | Pre | Post | Change | Pre | Post | Change | P Value |
| Liftoff | 29 | 11 | 18 | 20 | 7 | 13 | .155 |
| Belly-press | 8 | 5 | 3 | 18 | 3 | 15 | .028 |
a Bold P value indicates statistically significant difference between groups regarding pre- to postoperative change (P < .05). Pre, preoperative; Post, postoperative.
Moreover, 11.8% of the patients in group O presented with complications, while the corresponding rate in group A was 2.8%. These complications included superficial wound infection, deep tissue infection (septic arthritis), and rerupture. Three patients in group O and 1 in group A developed superficial wound infections. They were treated with antibiotherapy. Septic arthritis, which was detected in 1 patient from group O, was treated with debridement. The debridement was conducted arthroscopically, the repair line was evaluated as intact, and the infection was treated with antibiotherapy. A rerupture was detected after completion of the septic arthritis treatment in the patient during an evaluation for ROM limitation. The rerupture in this patient was repaired using an open procedure.
Discussion
Our study showed that the repair of ST tears had successful results in both groups. Postoperatively, the CM score (P < .001) and ROM in abduction (P = .005) and forward flexion (P = .005) were significantly better in group A than group O. In addition, the number of patients with a positive belly-press test result significantly decreased in group A (P = .028).
The literature contains many studies on open ST repair. Deutsch et al 12 reported 2-year follow-up outcomes for 13 patients who underwent surgery for isolated ST tears. They found that the internal rotation strength increased for all patients, the liftoff tests showed negative results in the final follow-up, and 10 of the 13 patients returned to sports activities. Other studies 3,13,17,27 assessing open repairs of ST tears evaluated patients for periods ranging from 12 to 46 months and noted that the CM scores as well as the forward elevation and external rotation of the patients increased, while the results of the liftoff tests turned negative. When the results of our patients who underwent open repair were examined, the increase in CM scores and the improvement in the liftoff test were similar to results of these studies.
Burkhart and Tehrany, 6 who were the first to study arthroscopic repair of the ST, observed significant improvement in the functional results and joint ROM at a mean 10.7 months postoperatively. Later, other studies assessing the short- and midterm results of arthroscopic repair reported the procedure to be successful. 23,26,29 In our patients who underwent arthroscopic repair, there was a significant increase in joint ROM at the end of at least 1 year of follow-up, consistent with the literature, and improvement in liftoff and belly press tests, which are specific tests for ST tears. We believe that the greater improvement in shoulder ROM in patients who have undergone arthroscopic repair is because of better tendon healing, as noted by Neviaser et al, 35 and less joint stiffness is because of smaller incisions and less dissection.
Studies reporting outcomes after arthroscopic and/or open repair have revealed similar rates of success (Table 6). 21,38 However, while the increase in ROM was greater in the arthroscopic repair group as compared with its open repair counterpart, the CM scores were similar for both groups. 34,35 When we compared the changes in ROM between the groups in our study, we observed that patients who underwent arthroscopic repair had a greater increase in abduction and anterior elevation movements, which was consistent with the literature. 3,30 Consistent with Neviaser et al, 35 the results of the belly-press test showed a significant improvement in the arthroscopic repair group as compared with the open repair group. When the CM scores were assessed, we noted that although the scores of the patients who had undergone arthroscopic repair were lower than those of the open repair group in preoperative terms, arthroscopic repair group had higher CM scores than open repair group postoperatively. It is thought that patients who underwent arthroscopic repair had better recovery since better results were obtained in the ROM, CM scores, and belly-press test in the arthroscopic repair group.
Table 6.
Studies on Arthroscopic and Open Repair a
| Burkhart (2002) 6 | Adams (2008) 1 | Flury (2006) 14 | Lafosse (2007) 30 | Bartl (2011) 2 | Deutsch (1997) 12 | Kreuz (2005) 27 | Neviaser (2020) 35 | Present Study | |
|---|---|---|---|---|---|---|---|---|---|
| No. of patients (female:male) | 25 (17:8) | 40 (28:12) | 61 (53:8) | 17 (13:4) | 30 (26:4) | 14 (8:6) | 16 (14:2) | 57 (35:22) | 70 (36:34) |
| Age, b y | 60.7 (41-78) | 66 (13-81) | 56 (28-75) | 47 (29-59) | 43.1 (15-64) | 38 (18-64) | 46 (27-64) | 65 | 62.9 (31-84) |
| Follow-up, b mo | 10.7 | 60 | 35 | 29 | 46 | 24 | 36 | 34 | 66.7 |
| Surgical technique | Arthroscopic | Arthroscopic | Open | Arthroscopic | Open | Open | Open |
|
|
| Tendon involvement |
|
|
|
Isolated SSC | Isolated SSC | Isolated SSC | Isolated SSC |
|
|
| Biceps tendon situation | 8 R, 6 D | 6 R, 5 PR, 15 D/S | 36 Biceps tenodesis | 2 R, 9 PR/D | 16 Tenodesis, 7 repair | 1 R, 6 PR/D | — | 28 R/S | 6 R, 29 Tenodesis, 14 tenotomy |
| Tests | 6 Liftoff, 9 Napoleon | 6 Liftoff, 3 bearhug, 24 Napoleon | 61 Liftoff | 16 Liftoff, 9 belly- press | 17 Liftoff, 27 belly-press | 2 Liftoff | 13 Liftoff, 10 Napoleon | 31 Liftoff, 32 belly-press | 49 Liftoff, 26 belly- press |
| ROM changes | Increased FE, decreased ER | Increased FE and elevation | Increased abduction and IR | Increased elevation and IR | Decreased ER | Decreased ER | — | Increased FE | Increased FE and abduction |
| Score b,c | UCLA: 10.7 → 30.5 |
|
CM: 55 → 83 |
|
CM: 51 → 84.2 | — | CM: 44 → 89 | ASES: 42 → 80 | CM: 51.2 → 86.7 |
a Dashes indicate not available. ASES, American Shoulder and Elbow Surgeons; CM, Constant-Murley score; D, dislocated; ER, external rotation; FE, forward elevation; IR, internal rotation; PR, partial rupture; R, rupture; ROM, range of motion; S, subluxated; SSC, subscapularis; SSP, supraspinatus; UCLA, University of California, Los Angeles; VAS, visual analog scale.
b Mean or mean (range).
c Preoperative → postoperative.
The MCID was first described by Jaeschke et al in 1989. 24 Their argument was that although statistically significant changes often occurred during use of instruments that measured change after intervention, in some cases the significant change had little clinical significance. 9,24 The first study investigating the MCID of CM changes of patients who underwent surgery for a rotator cuff tear was published by Kukkonen et al 28 in 2013. In this study, the MCID of patients who were satisfied with the surgery was calculated as 10.4 points. At the end of 1 year, approximately 90% of the patients reported that they were satisfied with the surgery. In a recent study by Cvetanovich et al, 10 the MCID for the CM score was calculated as 5.5 points. The MCID score of our patients was 11.5 points. The changes in both groups were clinically and statistically significant with this result. It was observed that the initial CM score of our patients who underwent arthroscopic repair was lower than that of the patients who underwent open repair at the final follow-up. When the amount of CM changes between the groups was examined, the total increase difference between the groups was 8.9 points. Although there is no publication comparing the repair of a rotator cuff tear with 2 different methods on the MCID, the difference between the groups seems to be consistent with the value of 5.5 points found by Cvetanovich et al.
ST tears were classified by Lafosse et al 31 in 2010 according to the amount of avulsion at the binding site. The classification contains 5 subtypes. None of our patients presented with type 1 or 5 tears, and types 3 and 4 tears were observed in 14 (41%) patients in the open repair group and 22 (61%) patients in the arthroscopic repair group. Many authors have assessed the effects of the tear types on the results of their studies. Some reported that tear size does not exert a negative effect on the results. 35,37 Another study showed that complete tears had better outcomes. 27 In our study, although more patients in the arthroscopic repair group presented with a high Lafosse classification tear level as compared with those in the open repair group, the improvement in CM scores, belly-press test results, and ROM was better for those patients than their counterparts in the open repair group.
The sheath of the biceps tendon is an extension of the synovium of the shoulder joint and is in close relationship with the rotator cuff. Inflammation that occurs here can be a source of pain by reflecting on the rotator cuff. 36 The ST contributes to medial support of the bicipital groove, and the incidence of biceps tendinopathy increases in ST ruptures. 1,33 While the rate of tendinopathy accompanying ST tears reaches 60%, it has been observed to be as low as 19% in patients without ST tears. 1,7,12 Treatment of biceps tendon pathologies affects the CM scores and subjective results in the postoperative period. Edwards et al 13 recommended tenodesis or tenotomy when performing ST repair regardless of the condition of the biceps. Of the patients evaluated in our study, 70% presented with subluxation, dislocation, or a tear in the biceps tendon. Tenodesis or tenotomy was performed in 43 patients because of the pathology of the biceps tendon. As stated in the studies in this direction in the literature, in both groups we think that patients who underwent biceps tendon procedures indirectly contributed to the improvement in CM scores to be significant.
In terms of complications observed after ST repair, a rerupture rate of 13% has been reported in some publications. 4,11,13,15,19,25,38 One of the 101 patients who underwent open repair in the study of Edwards et al 13 and 1 of the 26 patients who underwent arthroscopic repair in the study of Grueninger et al 19 experienced an infection requiring debridement. No infections were reported by Denard et al 11 and Fox et al. 15 One patient developed rupture with deep tissue infection in our study. Not surprisingly, infectious complications and subsequent rupture complications were more common in the open surgical group.
Limitations
Our study was not without limitations. The retrospective nature of our study and the operations performed by different surgeons influenced the choice of open and arthroscopic repair methods, double- or single-row repairs, and the use and distribution of anchors; therefore, standardization was not possible and may have introduced biases. The fact that the number of patients who underwent tenodesis or tenotomy was not the same in our patients included in the study may have influenced the results in the postoperative period. Although pain assessment is included in the CM scoring system, our patients were not evaluated pre- and postoperatively using an objective pain scoring system. Finally, factors that may have directly influenced functional outcomes, such as systemic disease and preoperative steroid injections, increased the risk of bias. Despite the homogeneous demographic distribution between groups, the retrospective nature of the study and the collection of descriptive data from records may not have clearly documented nonoperative treatment modalities and systemic diseases, with the exception of physical therapy performed in patients before surgery, which increased the risk of bias. In addition to the limiting factors mentioned here, the standard single-row repair of ST tears and the fact that the study consisted of patients with a long follow-up period are the strengths of our study.
Conclusion
The study findings showed that when an ST tear is evaluated in terms of its degree, satisfactory results can be achieved via arthroscopic repair even if the tear size is large. Arthroscopic repair may be a more advantageous method than open repair in terms of ROM and functional outcomes.
Footnotes
Final revision submitted March 15, 2022; accepted May 17, 2022.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Tokat Gaziosmanpaşa University (No. 20-KAEK-106).
References
- 1. Adams CR, Schoolfield JD, Burkhart SS. The results of arthroscopic subscapularis tendon repairs. Arthroscopy. 2008;24(12):1381–1389. [DOI] [PubMed] [Google Scholar]
- 2. Bartl C, Salzmann GM, Seppel G, et al. Subscapularis function and structural integrity after arthroscopic repair of isolated subscapularis tears. Am J Sports Med. 2011;39(6):1255–1262. [DOI] [PubMed] [Google Scholar]
- 3. Bartl C, Scheibel M, Magosch P, Lichtenberg S, Habermeyer P. Open repair of isolated traumatic subscapularis tendon tears. Am J Sports Med. 2011;39(3):490–496. [DOI] [PubMed] [Google Scholar]
- 4. Bennett WF. Arthroscopic repair of anterosuperior (supraspinatus/subscapularis) rotator cuff tears. Arthroscopy. 2003;19(1):21–33. [DOI] [PubMed] [Google Scholar]
- 5. Burkhart SS, Brady PC. Arthroscopic subscapularis repair: surgical tips and pearls A to Z. Arthroscopy. 2006;22(9):1014–1027. [DOI] [PubMed] [Google Scholar]
- 6. Burkhart SS, Tehrany AM. Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy. 2002;18(5):454–463. [DOI] [PubMed] [Google Scholar]
- 7. Chen C-H, Hsu K-Y, Chen W-J, Shih C-H. Incidence and severity of biceps long-head tendon lesion in patients with complete rotator cuff tears. J Trauma Acute Care Surg. 2005;58(6):1189–1193. [DOI] [PubMed] [Google Scholar]
- 8. Constant C, Murley A. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 9. Cook CE. Clinimetrics corner: the minimal clinically important change score (MCID)—a necessary pretense. J Man Manip Ther. 2008;16(4):e82–e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cvetanovich GL, Gowd AK, Liu JN, et al. Establishing clinically significant outcome after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2019;28(5):939–948. [DOI] [PubMed] [Google Scholar]
- 11. Denard PJ, Jiwani AZ, Lädermann A, Burkhart SS. Long-term outcome of a consecutive series of subscapularis tendon tears repaired arthroscopically. Arthroscopy. 2012;28(11):1587–1591. [DOI] [PubMed] [Google Scholar]
- 12. Deutsch A, Altchek DW, Veltri DM, Potter HG, Warren RF. Traumatic tears of the subscapularis tendon: clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med. 1997;25(1):13–22. [DOI] [PubMed] [Google Scholar]
- 13. Edwards TB, Walch G, Sirveaux F, et al. Repair of tears of the subscapularis. J Shoulder Elbow Surg. 2005;87(4):725–730. [DOI] [PubMed] [Google Scholar]
- 14. Flury MP, John M, Goldhahn J, Schwyzer H-K, Simmen BR. Rupture of the subscapularis tendon (isolated or in combination with supraspinatus tear): when is a repair indicated? J Shoulder Elbow Surg. 2006;15(6):659–664. [DOI] [PubMed] [Google Scholar]
- 15. Fox JA, Noerdlinger MA, Romeo AA. Arthroscopic subscapularis repair. Tech Shoulder Elb Surg. 2003;4(4):154–168. [Google Scholar]
- 16. Frankle M, Cofield R, eds. Rotator cuff tears including the subscapularis. In: Proceedings of the Fifth International Conference on Surgery of the Shoulder. International Shoulder and Elbow Society; 1992. [Google Scholar]
- 17. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon: results of operative repair. J Shoulder Elbow Surg. 1996;78(7):1015–1023. [DOI] [PubMed] [Google Scholar]
- 18. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle: clinical features in 16 cases. J Bone Joint Surg Br. 1991;73(3):389–394. [DOI] [PubMed] [Google Scholar]
- 19. Grueninger P, Nikolic N, Schneider J, et al. Arthroscopic repair of traumatic isolated subscapularis tendon lesions (Lafosse type III or IV): a prospective magnetic resonance imaging—controlled case series with 1 year of follow-up. Arthroscopy. 2014;30(6):665–672. [DOI] [PubMed] [Google Scholar]
- 20. Guzik A, Drużbicki M, Wolan-Nieroda A, Turolla A, Kiper P. Estimating minimal clinically important differences for knee range of motion after stroke. J Clin Med. 2020;9(10):3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harrison A, Shatsky J, Parsons B, Flatow E. Outcomes of open and arthroscopic subscapularis repairs (SS-18). Arthroscopy. 2011;27(5):e38–e39. [Google Scholar]
- 22. Hauser ED. Avulsion of the tendon of the subscapularis muscle. J Shoulder Elbow Surg. 1954;36(1):139–141. [PubMed] [Google Scholar]
- 23. Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Shoulder Elbow Surg. 2007;89(11):2378–2388. [DOI] [PubMed] [Google Scholar]
- 24. Jaeschke R, Singer J, Guyatt GH. Measurement of health status: ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–415. [DOI] [PubMed] [Google Scholar]
- 25. Jeong JY, Pan H-L, Song SY, Lee SM, Yoo JC. Arthroscopic subscapularis repair using single-row mattress suture technique: clinical results and structural integrity. J Shoulder Elbow Surg. 2018;27(4):711–719. [DOI] [PubMed] [Google Scholar]
- 26. Kim S-H, Oh I, Park J-S, Shin S-K, Jeong W-K. Intra-articular repair of an isolated partial articular-surface tear of the subscapularis tendon. Am J Sports Med. 2005;33(12):1825–1830. [DOI] [PubMed] [Google Scholar]
- 27. Kreuz P, Remiger A, Lahm A, Herget G, Gächter A. Comparison of total and partial traumatic tears of the subscapularis tendon. J Bone Joint Surg Br. 2005;87(3):348–351. [DOI] [PubMed] [Google Scholar]
- 28. Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Äärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–1655. [DOI] [PubMed] [Google Scholar]
- 29. Lafosse L, Brozska R, Toussaint B, Gobezie R. The outcome and structural integrity of arthroscopic rotator cuff repair with use of the double-row suture anchor technique. J Shoulder Elbow Surg. 2007;89(7):1533–1541. [DOI] [PubMed] [Google Scholar]
- 30. Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Shoulder Elbow Surg. 2007;89(6):1184–1193. [DOI] [PubMed] [Google Scholar]
- 31. Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. 2010;96(8):S99–S108. [DOI] [PubMed] [Google Scholar]
- 32. Lee J, Shukla DR, Sánchez-Sotelo J. Subscapularis tears: hidden and forgotten no more. JSES Open Access. 2018;2(1):74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lo IK, Burkhart SS. The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy. 2003;19(10):1142–1150. [DOI] [PubMed] [Google Scholar]
- 34. Mall NA, Chahal J, Heard WM, et al. Outcomes of arthroscopic and open surgical repair of isolated subscapularis tendon tears. Arthroscopy. 2012;28(9):1306–1314. [DOI] [PubMed] [Google Scholar]
- 35. Neviaser AS, Charen DA, Cotter JM, Harrison AK, Cagle PJ, Flatow EL. Retrospective review of open and arthroscopic repair of anterosuperior rotator cuff tears with subscapularis involvement: a single surgeon’s experience. J Shoulder Elbow Surg. 2020;29(5):893–897. [DOI] [PubMed] [Google Scholar]
- 36. Nho SJ, Strauss EJ, Lenart BA, et al. Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18(11):645–656. [DOI] [PubMed] [Google Scholar]
- 37. Nové-Josserand L, Hardy M-B, Ogassawara RLN, Carrillon Y, Godenèche A. Clinical and structural results of arthroscopic repair of isolated subscapularis tear. J Shoulder Elbow Surg. 2012;94(17):e125. [DOI] [PubMed] [Google Scholar]
- 38. Saltzman BM, Collins MJ, Leroux T, et al. Arthroscopic repair of isolated subscapularis tears: a systematic review of technique-specific outcomes. Arthroscopy. 2017;33(4):849–860. [DOI] [PubMed] [Google Scholar]
- 39. Smith JG. Pathological appearances of seven cases of injury of the shoulder joint, with remarks. London Med Gaz. 1834;14:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Warner JJ, Higgins L, Parsons I IV, Dowdy P. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg. 2001;10(1):37–46. [DOI] [PubMed] [Google Scholar]
- 41. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. [DOI] [PubMed] [Google Scholar]


